Abstract
Background
This study was performed to determine survival and morbidity rates in very low birth weight infants (VLBWIs) in the Korean Neonatal Network (KNN), and to compare neonatal outcomes with those in other countries.
Methods
Data were collected for 8,269 VLBWIs with gestational age (GA) ≥ 22 weeks who were born between January 1, 2013 and December 31, 2016, and admitted to the neonatal intensive care units of the KNN.
Results
The survival rate of all VLBWIs and of infants with GA 22–23, 24–25, 26–27, 28–29, 30–32, and > 32 weeks were 86% (total), 33%, 65%, 84%, 94%, 97%, and 98%, respectively. The bronchopulmonary dysplasia (BPD) rates of all VLBWIs and of infants with GA 22–23, 24–25, 26–27, 28–29, 30–32, and > 32 weeks were 30% (total), 88%, 64%, 47%, 26%, 14%, and 5%, respectively. The intraventricular hemorrhage rates (≥ grade III) of all VLBWIs and of infants with GA 22–23, 24–25, 26–27, 28–29, 30–32, and > 32 weeks were 10% (total), 45%, 27%, 12%, 5%, 2%, and 1%, respectively. In an international comparison, the survival rate of VLBWIs with GA 24–27 weeks in KNN was lower, and the BPD rate of VLBWIs in the KNN was higher than that of the neonatal networks of other countries.
Conclusion
Despite overall improvements in neonatal outcomes, the survival and morbidity rates of more immature infants with GA 22–27 weeks need further improvement. Therefore, it would be necessary to develop more optimal treatment strategies and perform more active quality improvement to further improve neonatal outcomes of VLBWIs in Korea.
Keywords: Infant, Premature; Infant, Very Low Birth Weight; Infant Mortality; Bronchopulmonary Dysplasia
Graphical Abstract
INTRODUCTION
Despite advances in neonatal intensive care, very low birth weight infants (VLBWIs) who are born weighing < 1,500 g, remain at high risk of mortality and morbidities of serious complications.1 Complications related to preterm birth are the leading cause of mortality in children younger than 5 years overall, including the neonatal period.2 In addition, preterm infants require active health care in the long term as well as in the neonatal period owing to various complications.3 These outcomes in VLBWIs are accepted as an index reflecting the quality of newborn care in each country.4,5 Many developed countries have already established neonatal networks and are seeking to improve neonatal care by accumulating and presenting population-based data on high-risk newborns, such as VLBWIs. In addition, these networks are making efforts to find ways to improve the care of newborns in their countries through comparisons with other countries.6,7
The survival rate of VLBWIs in Korea has been improving in the past half century,8 reaching 84.8% according to a recent report.9 However, few studies have reported on population-based neonatal outcomes, including survival rates along with serious morbidities such as bronchopulmonary dysplasia (BPD), intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), and retinopathy of prematurity (ROP). The Korean Neonatal Network (KNN), which was established by the Korean Society of Neonatology and Korea Centers for Disease Control and Prevention in 2013, has been collecting nationwide population-based data for improving the outcomes of VLBWIs in Korea.10
Therefore, this study was performed to determine the survival and morbidity rates of VLBWIs in Korea, and to compare the neonatal outcomes with those in other countries.
METHODS
Data collection
Of 8,291 VLBWIs born in or transferred within 28 days after birth to the participating neonatal intensive care units (NICUs) of the KNN between January 1, 2013 and December 31, 2016, this study enrolled 8,269 infants born at gestational age (GA) ≥ 22 weeks. From 2013 to 2016, a total of 49, 55, 60, and 66 NICUs participated annually and registered 1,396, 2,123, 2,392, and 2,358 VLBWIs, in the registry of the KNN, respectively. The population in this study included about two-thirds of the annual VLBWIs born in Korea except 2013. This study was based on data from annual reports of the KNN from 2013 to 2016.11,12,13,14
The definitions of collected data were guided by the manual of operations of the KNN. GA was determined thorough obstetric examination with ultrasonography early during pregnancy or, if early ultrasonography was unavailable, by way of historical review of the last menstrual period. BPD was defined as the need for supplemental oxygen support at corrected GA of 36 weeks.15 Necrotizing enterocolitis (NEC) was defined as Bell's stage II or higher.16 IVH (≥ grade III)17 and cystic PVL on cranial ultrasonography were based on the Papile grading system.
The neonatal outcomes data of other countries were collected and modified with published studies.6,7,18,19 The data of other countries were collected by the national neonatal research networks of countries that participated in the International Network for Evaluating Outcomes (iNeo) of Neonate and the National Institute of Child Health and Human Development (NICHD) Neonatal Research Network.
Data analysis
Subgroup analysis for survival and morbidity rates in the KNN was performed according to GA; 22–23, 24–25, 26–27, 28–29, 30–32, and > 32 weeks. International comparison of survival rates was conducted with VLBWIs born at GA 24–29 weeks, whereas the comparison with morbidity rates was conducted with VLBWIs born at GA 24–31 weeks.
Demographic data and neonatal outcomes were presented as percent (range of probability; 95% confidence interval). The statistical significance for unadjusted comparisons was analyzed with the χ2 or Fisher's exact test. All statistical analyses were performed using R software (R Foundation for Statistical Computing, Vienna, Austria).20
RESULTS
Demographic characteristics
Of all the VLBWIs in this study, 35% were born from multiple births and 34% of mothers were older than 35 years. Antenatal steroid was given to 76% of mothers and 77% of the infants were born via cesarean section. Maternal diabetes and hypertension were present in 8% and 21%, respectively, during the pregnancy.
Fewer mothers of VLBWIs with GA 22–23 weeks and GA > 32 weeks received antenatal steroid than mothers of other VLBWI subgroups. Fewer VLBWIs with GA 22–23 weeks were born via cesarean section than VLBWIs of other subgroups, and more VLBWIs with GA 30–32 weeks and > 32 weeks were born via cesarean section than VLBWIs of other subgroups. Maternal diabetes and hypertension showed a tendency to increase with increasing GA of the VLBWIs. Demographic data of VLBWIs enrolled in this study are shown in Table 1.
Table 1. Demographic data of VLBWIs of KNN (2013–2016).
| Variables | GA, wk | |||||||
|---|---|---|---|---|---|---|---|---|
| 22–23 (n = 372) | 24–25 (n = 1,156) | 26–27 (n = 1,644) | 28–29 (n = 2,191) | 30–32 (n = 2,078) | > 32 (n = 828) | Total (n = 8,269) | ||
| Sex, male | 52 (47–58) | 52 (49–55) | 53 (50–55) | 51 (49–53) | 47 (45–50) | 47 (44–50) | 50 (49–51) | |
| Multiple birth | 39 (34–44) | 34 (31–36) | 29 (27–31) | 34 (32–36) | 41 (39–43) | 38 (35–42) | 35 (34–36) | |
| Maternal age, yr | ||||||||
| < 20 | 0 (0–2) | 1 (0–1) | 0 (0–1) | 0 (0–1) | 0 (0–1) | 0 (0–1) | 0 (0–1) | |
| > 35 | 30 (26–35) | 32 (30–35) | 36 (34–38) | 32 (31–35) | 34 (32–36) | 35 (32–39) | 34 (33–35) | |
| Antenatal steroid | 63 (58–68) | 79 (76–81) | 82 (80–84) | 81 (79–83) | 80 (79–82) | 45 (42–49) | 76 (75–77) | |
| Cesarean section | 49 (43–54) | 71 (68–74) | 74 (71–76) | 77 (75–79) | 85 (83–86) | 88 (86–90) | 77 (76–78) | |
| Maternal diabetes | 2 (1–4) | 5 (4–6) | 9 (8–10) | 10 (9–12) | 10 (9–11) | 8 (6–10) | 8 (8–9) | |
| Maternal hypertension | 3 (2–6) | 8 (7–10) | 13 (12–15) | 17 (15–18) | 33 (31–35) | 38 (34–41) | 21 (20–21) | |
Data are presented as percentage (range of probability: 95% confidence interval). There is a significant difference among groups if the probability ranges do not overlap with each other.
VLBWIs = very low birth weight infants, KNN = Korean Neonatal Network, GA = gestational age.
Neonatal outcomes
The survival rate of all VLBWIs in this study was 86%, and the survival rates were much lower in more immature VLBWIs (GA 22–23, 24–25, 26–27 weeks) than in infants with GA ≥ 28 weeks.
Of all the VLBWIs in this study, 78% and 30% were diagnosed as having respiratory distress syndrome (RDS) and moderate to severe BPD, respectively. The RDS rates decreased abruptly in VLBWIs with GA 30–32 weeks and GA > 32 weeks. The BPD rates were much higher in VLBWIs with GA 22–23, 24–25, and 26–27 weeks than VLBWIs with GA ≥ 28 weeks.
Of the total VLBWIs in this study, 7% were diagnosed as having NEC and 8% needed therapy for ROP before discharge from the NICU. The rate of NEC in VLBWIs with GA 22–23 weeks was 20% which decreased as the subgroup GA increased. The rate of therapy for ROP in VLBWIs with GA 24–25 weeks was the highest at 25% which also decreased as the subgroup GA increased.
Sepsis occurred in 21% of all VLBWIs in this study during the stay in the NICU; specifically, the rates of sepsis in VLBWIs with GA 22–23, 24–25, and 26–27 weeks were much higher than those of VLBWIs with GA ≥ 28 weeks.
IVH (≥ grade III) was diagnosed in 10% of all VLBWIs in this study, and the rates of IVH (≥ grade III) were much higher in VLBWIs with GA 22–23 and 24–25 weeks than in VLBWIs with GA ≥ 26 weeks. The neonatal outcomes of VLBWIs enrolled in this study are shown in Table 2.
Table 2. Neonatal outcomes of VLBWIs of KNN (2013–2016).
| Variables | GA, wk | ||||||
|---|---|---|---|---|---|---|---|
| 22–23 (n = 372) | 24–25 (n = 1,156) | 26–27 (n = 1,644) | 28–29 (n = 2,191) | 30–32 (n = 2,078) | > 32 (n = 828) | Total (n = 8,269) | |
| Survival rate | 33 (28–38) | 65 (62–67) | 84 (82–85) | 94 (93–95) | 97 (96–98) | 98 (97–99) | 86 (85–87) |
| RDS | 98 (95–99) | 98 (97–99) | 96 (95–97) | 89 (88–91) | 60 (58–62) | 21 (18–23) | 78 (77–79) |
| BPD | 88 (80–93) | 64 (61–68) | 47 (44–49) | 26 (24–28) | 14 (13–16) | 5 (4–7) | 30 (29–31) |
| ROP Tx. | 20 (16–25) | 25 (23–28) | 11 (9–12) | 3 (2–4) | 1 (0–1) | 0 (0–1) | 8 (7–8) |
| NEC ≥ IIa | 20 (16–25) | 15 (13–17) | 9 (8–11) | 4 (3–5) | 3 (2–3) | 2 (1–4) | 7 (6–7) |
| Sepsis | 38 (33–43) | 36 (33–39) | 31 (29–33) | 18 (16–19) | 11 (9–12) | 6 (4–8) | 21 (20–22) |
| Drug for PDA | 39 (34–45) | 52 (49–55) | 48 (45–50) | 34 (32–36) | 21 (19–23) | 9 (7–11) | 34 (33–35) |
| Ligation of PDA | 18 (14–23) | 25 (23–28) | 18 (16–20) | 7 (6–9) | 3 (3–4) | 2 (1–3) | 11 (10–12) |
| IVH (≥ grade III) | 45 (39–51) | 27 (25–30) | 12 (11–14) | 5 (4–6) | 2 (1–3) | 1 (0–2) | 10 (9–10) |
| PVL | 15 (11–20) | 12 (10–15) | 11 (9–12) | 8 (7–9) | 5 (4–6) | 2 (1–3) | 8 (7–9) |
Data are presented as percentage (range of probability: 95% confidence interval). There is a significant difference among groups if the probability ranges do not overlap with each other.
VLBWIs = very low birth weight infants, KNN = Korean Neonatal Network, GA = gestational age, RDS = respiratory distress syndrome, BPD = bronchopulmonary dysplasia, moderate to severe, ROP Tx. = therapy for retinopathy of prematurity before discharge from the neonatal intensive care unit, NEC = necrotizing enterocolitis, PDA = patent ductus arteriosus, IVH (≥ grade III) = grade III or more intraventricular hemorrhage, PVL = periventricular leukomalacia, cystic.
Annual trends of neonatal outcomes in the KNN from 2013 to 2016
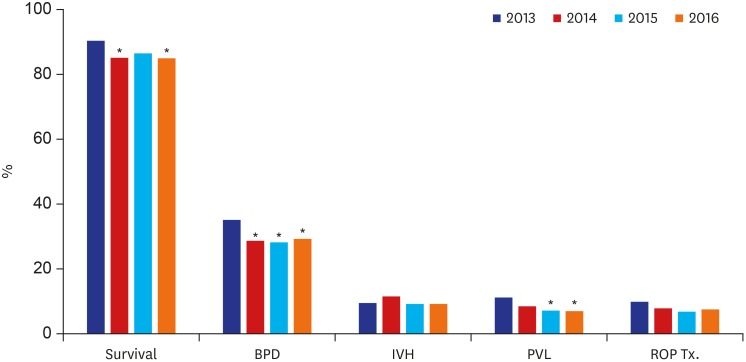
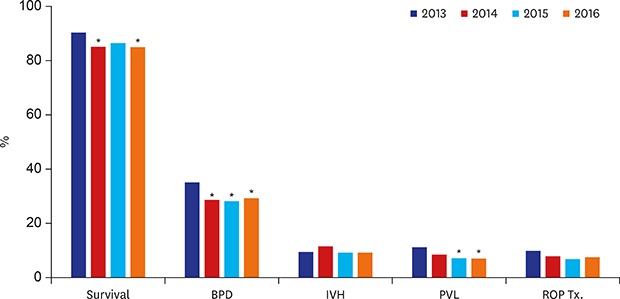
The annual survival rates for 2013, 2014, 2015, and 2016 were 90% (88%–92%), 85% (84%–87%), 86% (85%–88%) and 85% (83%–87%), respectively. The annual BPD rates for 2013, 2014, 2015 and 2016 were 35% (32%–38%), 29% (26%–31%), 28% (26%–30%) and 29% (27%–31%), respectively. The annual trends of neonatal outcomes in the KNN from 2013 to 2016 are shown in Fig. 1.
Fig. 1. Annual trends of neonatal outcomes of VLBWIs of KNN (2013–2016).
VLBWIs = very low birth weight infants, KNN = Korean Neonatal Network, BPD = bronchopulmonary dysplasia, moderate to severe, IVH (≥ grade III) = grade III or more intraventricular hemorrhage, PVL = periventricular leukomalacia, cystic, ROP Tx. = therapy for retinopathy of prematurity.
*P value < 0.05 evaluated with χ2 Fisher's exact test, compared with outcomes in 2013.
International comparison of neonatal outcomes
The survival rates of VLBWIs born at GA 24–29 weeks are shown by country in Table 3. The overall survival rate of VLBWIs in the KNN was 84% (83%–85%). In contrast, the survival rates in the Neonatal Research Network of Japan (NRNJ), the Australia and New Zealand Neonatal Network, and the Canadian Neonatal Network (CNN) were higher than those in other neonatal networks including the KNN; the rates in the SwissNeoNet and United Kingdom Neonatal Collaborative were comparable to those in the KNN. The differences in survival rates between the KNN and the networks in countries with better survival rates became more prominent in the comparison based on less mature infants with GA 24–26 weeks.
Table 3. International comparison of survival rates of VLBWIs (24–29 weeks' gestation).
| GA, wk | KNNa | ANZNNb | CNNb | NICHDc | INNb | NRNJb | SEN1500b | SwissNeoNetb | UKNCd |
|---|---|---|---|---|---|---|---|---|---|
| 24 | 56 (51–60) [478] | 65 (62–67) [1,229] | 62 (59–65) [1,191] | 62 (60–65) [1,241] | 35 (31–39) [482] | 84 (82–85) [2,082] | 36 (33–39) [866] | 58 (50–65) [186] | 64 (62–66) [2,053] |
| 25 | 71 (67–74) [678] | 80 (78–82) [1,655] | 79 (77–81) [1,829] | 77 (75–80) [1,391] | 57 (54–61) [664] | 89 (88–90) [2,413] | 60 (57–62) [1,200] | 67 (62–72) [319] | 77 (75–78) [2,366] |
| 26 | 79 (76–82) [774] | 88 (86–89) [2,117] | 87 (85–88) [2,043] | 85 (83–86) [1,513] | 78 (75–81) [847] | 93 (92–94) [2,850] | 73 (71–75) [1,568] | 84 (80–87) [458] | 85 (84–86) [3,091] |
| 27 | 88 (86–90) [870] | 92 (91–93) [2,346] | 92 (90–93) [2,412] | 90 (89–92) [1,733] | 85 (83–88) [947] | 94 (94–95) [3,301] | 82 (80–84) [1,842] | 91 (88–93) [478] | 90 (89–91) [3,657] |
| 28 | 93 (91–95) [1,072] | 95 (94–96) [2,939] | 95 (94–95) [2,703] | 94 (93–95) [1,886] | 92 (90–93) [1,156] | 96 (96–97) [3,850] | 89 (87–90) [2,210] | 95 (93–96) [581] | 93 (92–94) [4,383] |
| 29 | 95 (94–96) [1,119] | 97 (97–98) [2,953] | 97 (96–98) [2,710] | - | 94 (93–96) [1,345] | 97 (96–97) [3,925] | 92 (91–93) [2,540] | 98 (96–99) [653] | 96 (95–97) [4,425] |
| 24–29 | 84 (83–85) [4,991] | 89 (88–90) [13,239] | 88 (87–89) [12,888] | 83 (83–84) [7,764] | 80 (79–81) [5,441] | 93 (93–94) [17,192] | 78 (77–79) [10,226] | 87 (86–88) [2,675] | 87 (86–87) [19,975] |
Data are presented as survival rate (range of probability: 95% confidence interval) [numbers of group]. There is a significant difference among groups if the probability ranges do not overlap with each other.
VLBWIs = very low birth weight infants, GA = gestational age, KNN = Korean Neonatal Network, ANZNN = Australia and New Zealand Neonatal Network, CNN = Canadian Neonatal Network, NICHD = National Institute of Child Health and Human Development, INN = the Israel Neonatal Network, NRNJ = Neonatal Research Network of Japan, SEN1500 = Spanish Neonatal Network, UKNC = United Kingdom Neonatal Collaborative.
a2013–2016; b2007–2013; c2008–2012; d2008–2013.
The demographic data and morbidity rates of VLBWIs by country are shown in Table 4. Most of the characteristics of the VLBWIs in the KNN, including multiple births, male, antenatal steroid use and cesarean section, showed similar trends with those of VLBWIs in other networks. With regard to morbidities, the BPD rate in the KNN was higher than that in other networks.
Table 4. International comparison of demographics and morbidities of VLBWIs (24–31 weeks' gestation).
| Variables | KNNa (n = 6,620) | ANZNNb (n = 9,643) | CNNb (n = 8,666) | INNb (n = 4,481) | NRNJb (n = 12,608) | SEN1500b (n = 8,063) | SwissNeoNetb (n = 2,034) | UKNCc (n = 10,325) |
|---|---|---|---|---|---|---|---|---|
| Multiple birth | 35 (33–36) | 31 (30–32) | 31 (30–32) | 42 (41–44) | 24 (23–25) | 33 (32–34) | 34 (32–36) | 28 (27–29) |
| Sex, male | 51 (50–52) | 51 (50–52) | 52 (51–53) | 52 (51–54) | 52 (51–53) | 52 (51–53) | 52 (49–54) | 51 (50–52) |
| Antenatal steroid | 81 (80–82) | 90 (89–90) | 84 (84–85) | 75 (74–77) | 49 (49–50) | 84 (84–85) | 89 (88–90) | 82 (81–83) |
| Cesarean section | 77 (76–78) | 64 (63–65) | 62 (61–63) | 73 (72–75) | 77 (76–77) | 67 (66–68) | 84 (83–86) | 47 (46–48) |
| BPD | 33 (32–34) | 24 (23–25) | 25 (24–26) | 14 (13–15) | 19 (18–20) | 15 (14–16) | 13 (11–15) | 32 (31–33) |
| IVH (≥ grade III) | 10 (9–11) | 6 (6–7) | 10 (9–11) | 12 (11–13) | 4 (4–5) | 10 (9–11) | 8 (7–9) | 6 (6–6) |
| PVL | 7 (6–9) | 3 (2–3) | 6 (5–7) | 5 (4–6) | 4 (4–4) | 6 (6–7) | 2 (2–3) | 2 (2–2) |
| ROP Tx. | 8 (8–9) | 3 (3–3) | 4 (4–4) | 3 (3–4) | 16 (16–17) | 4 (4–5) | 2 (1–3) | 2 (2–3) |
Data are presented as survival rate (range of probability: 95% confidence interval). There is a significant difference among groups if the probability ranges do not overlap with each other.
VLBWIs = very low birth weight infants, BPD = bronchopulmonary dysplasia, moderate to severe, IVH (≥ grade III) = grade III or more intraventricular hemorrhage, PVL = periventricular leukomalacia, cystic, ROP Tx. = therapy for retinopathy of prematurity before discharge from the neonatal intensive care unit, KNN = Korean Neonatal Network, ANZNN = Australia and New Zealand Neonatal Network, CNN = Canadian Neonatal Network, INN = the Israel Neonatal Network, NRNJ = Neonatal Research Network of Japan, SEN1500 = Spanish Neonatal Network, UKNC = United Kingdom Neonatal Collaborative.
a2013–2016; b2007–2010; c2008–2010.
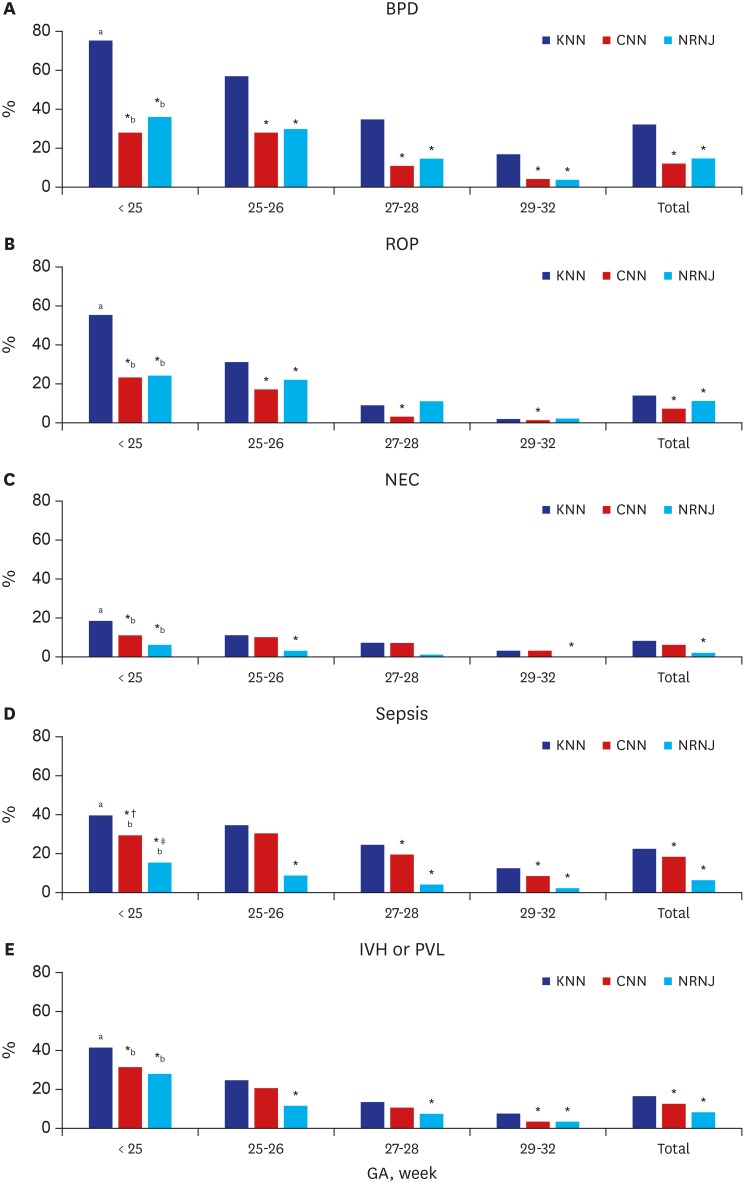
The rates of BPD, ROP, NEC, sepsis, IVH or PVL in VLBWIs with GA ≤ 32 weeks in the KNN, CNN, and NRNJ are shown in Fig. 2. The rates of morbidities of infants in the KNN were higher than those in the CNN and NRNJ, and these differences were more pronounced in the comparison based on less mature infants with GA < 25 weeks and 25–26 weeks and in the comparison of BPD and ROP rates.
Fig. 2. International comparison of moderate to severe BPD, severe ROP (≥ stage III), NEC (≥ stage IIa), sepsis, and IVH (≥ grade III) or cystic PVL in VLBWIs with 22–32 weeks' gestation.
BPD = bronchopulmonary dysplasia, ROP = retinopathy of prematurity, NEC = necrotizing enterocolitis, IVH = intraventricular hemorrhage, PVL = periventricular leukomalacia, VLBWIs = very low birth weight infants, KNN = Korean Neonatal Network, CNN = Canandian Neonatal Network, NRNJ = Neonatal Research Network of Japan.
*P value < 0.05 evaluated with χ2 Fisher's exact test, compared with outcomes of the KNN; †sepsis at ≥ 3 days of life; ‡sepsis at ≥ 7 days of life; a2013–2016; b2006–2008.
DISCUSSION
The present study is the first to evaluate the survival rates along with rates of major morbidities of VLBWIs using a population-based study in Korea. Our data showed that the survival rate of VLBWIs in the KNN enrolled from January 1, 2013 to December 31, 2016, was 86% and that the rates of RDS, BPD, IVH and PVL were 78%, 30%, 10%, and 8% respectively. These data according to GA would help to provide useful information to both physicians and parents and could facilitate studies to improve neonatal outcomes in Korea.
The survival rate of VLBWIs in Korea, which had reached about 40% from 1960 to the mid-1980s, showed dramatic improvement owing to the rapid development of neonatal intensive care medicine, increasing to 85% in 2005–2009. The statistical differences among the survival rates of VLBWIs according to GA from surveillance data in the 2000s were analyzed and the survival rates were significantly lower in infants with GA < 30 weeks in 2002, GA < 29 weeks in 2007, and GA < 27 weeks in 2013–2014, indicating that the survival rate of less mature VLBWIs has improved over time.9 In the present study, the survival rates of VLBWIs with GA 22–23, 24–25, and 26–27 weeks were also much lower than those of infants with GA ≥ 28–29 weeks. These prominent differences in the survival rate according to GA were also found in a comparison with other developed countries. In the present study, the overall survival rates of VLBWIs with GA between 24 and 29 weeks of GA in the KNN was 84%; this rate was comparable to that in most other countries; however, the overall survival rates of less mature infants with GA between 24 and 26 weeks in the KNN were much lower than those in many other countries. The annual survival rates in 2014 and 2016 were significantly lower than those in 2013 in this study. However, these results may be attributed to the quantitative increase of NICUs participating in the data registry of the KNN during the study period and the deaths of some infants before enrollment in the data registry of 2013, rather than to the deterioration of neonatal intensive care for these high-risk infants.
Perinatal and neonatal care has focused on improving neonatal outcomes by reducing major morbidities, in addition to increasing survival rate in extremely preterm infants. Antenatal steroid use is known to be one of the most effective perinatal care for improving neonatal outcomes of preterm infants.21,22 Mori et al.23 found that antenatal steroid exposure was associated with a significant decrease in mortality of preterm infant born at GA 22 or 23 weeks. Although the frequency of antenatal steroid use for overall VLBWIs in the KNN was comparable to that of networks in other countries, the frequency of antenatal steroid use in infants with GA 22–23 weeks was still much lower than that in infants with GA ≥ 24 weeks in this study. In addition, only 49% of infants with GA 22–23 weeks were born via cesarean section, and this rate is much lower than the cesarean section rate of all the VLBWIs in the present study. There has been a wide variation of opinions among obstetricians regarding routine use of electronic fetal monitoring or consideration of cesarean section for infants with GA < 24 weeks.24 Although the risks and benefits should be taken into account when deciding whether to use antenatal steroid and cesarean section for extremely preterm infants at the limit of viability, these may be necessary to improve neonatal survival and reduce major morbidity rates.
BPD, a representative chronic lung disease in newborn infants, results in higher mortality and longer hospitalization. Infants with BPD have increased risks of cardiovascular impairment, pulmonary sequelae, growth failure, and neurodevelopmental delay.25,26,27 The BPD rate in VLBWIs with GA 23–31 weeks increased from 17.8% in 2007–2008 to 33% in 2013–2014 in Korea.28 The studies in other countries also showed that the increase in the survival rate of infants with more immature GA and lower birth weight, which are risk factors for BPD, leads to an unavoidable increase in the rate of BPD.18,19,29,30 In the present study, the annual BPD rate for 2013 was 35% (32%–38%), but significantly decreased to 29% (26%–31%), 28% (26%–30%) and 29% (27%–31%) in 2014, 2015, and 2016, respectively. These conflicting results may also be attributed to the exclusion of infants who died before enrollment in the data registry for 2013. In addition, the variation of incidence of BPD among countries may be caused by the difference in definition of BPD with regard to whether or not to include use of heated humidified high-flow nasal cannula for respiratory support.
The development of severe IVH or cystic PVL is of great importance in that it is likely to induce long-term neurodevelopmental impairment. In the study by the NICHD, the IVH rate was decreased in VLBWIs with GA 26–28 weeks from 1993 to 2012 but not in infants with GA 22–25 weeks.18 The cystic PVL rate was also decreased in VLBWIs GA 26–28 weeks during the last 20 years in that study.18 In the present study, IVH and PVL rates in infants with GA ≤ 27 weeks were also much higher than those in infants with GA > 27 weeks. Cho et al.31 reported that intensive resuscitation with cardiac compression and/or epinephrine administration at birth resulted in greater early mortality at less than 7 days, increased IVH, and increased PVL, and suggested that quality improvement in delivery room management would result in reduced morbidity and early death in vulnerable VLBWIs. In the present study, the annual PVL rate for 2015 and 2016 was significantly lower than that for 2013. However, the baseline characteristics such as GA, birth weight, use of antenatal steroids, need for intensive resuscitation at birth, and the PVL rate according to GA were not different from 2013 to 2016 (data not shown). This difference may also result from the composition of infants enrolled in 2013.
The NRNJ, which has the best VLBWI survival rate among the neonatal networks of other countries, showed a remarkable difference from others, especially in the survival rate of less mature infants with GA ≤ 26 weeks and the lower rates of IVH, PVL, NEC, and late-onset sepsis.32,33 The excellent neonatal outcomes of VLBWIs in Japan have been attributed to social consensus on the limit of viability and to care guidelines and active support for the treatment of more immature infants.34,35 Smith et al.36 reported that NICUs with higher rates of antenatal steroid use in extremely low birth weight infants (ELBWIs) at GA 22 to 24 weeks showed reduced rates of death, death or ROP, death or late-onset sepsis, death or NEC, and death or neurodevelopmental impairment in ELBWIs at GA 25–27 weeks. This suggested that physicians' willingness to provide care to extremely low GA infants, as measured by the frequency of antenatal steroid use, could be associated with improved outcomes for more mature infants. Kim et al.37 reported that improved survival in extremely premature infants with GA 23–24 weeks was associated with a higher rate of antenatal steroid use, an improved 5-minute Apgar score and a decrease in BPD rate in infants at GA 25–26 weeks. This finding was associated with early weaning from intubation, prolonged use of less-invasive continuous positive airway pressure, and reduced supplemental oxygen. The results of these studies demonstrate that an active approach to perinatal and neonatal care can improve outcomes in extremely preterm infants.
The strength of the present study lies in analyzing prospectively collected data from a large population and clearly showing nationwide survival and major morbidity rates in Korean VLBWIs according to GA. However, we could not analyze details such as risk factors for mortality and morbidity because the present study was based on data from the KNN annual reports. Moreover, regarding international network comparisons, there may be an actual difference for comparison because the data collected from the cohorts in other networks were not for the same years, rather were older than those of the KNN. Further studies are needed to clarify these differences.
Despite improvements in neonatal outcomes of VLBWIs during the last 20 years, survival and morbidity rates of more immature infants with GA 22–27 weeks need further improvement in Korea. Therefore, it would be necessary to develop more optimal treatment strategies and perform more active quality improvement to further improve neonatal outcomes of VLBWIs in Korea.
Footnotes
Funding: This research was supported by a fund (2016-ER6307-02#) by Research of Korea Centers for Disease Control and Prevention.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Lee JH, Chang YS.
- Data curation: Lee JH, Chang YS.
- Formal analysis: Lee JH, Noh OK.
- Methodology: Lee JH, Noh OK, Chang YS.
- Writing - original draft: Lee JH, Noh OK, Chang YS.
- Writing - review & editing: Lee JH, Chang YS.
References
- 1.Patel RM, Kandefer S, Walsh MC, Bell EF, Carlo WA, Laptook AR, et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med. 2015;372(4):331–340. doi: 10.1056/NEJMoa1403489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385(9966):430–440. doi: 10.1016/S0140-6736(14)61698-6. [DOI] [PubMed] [Google Scholar]
- 3.Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261–269. doi: 10.1016/S0140-6736(08)60136-1. [DOI] [PubMed] [Google Scholar]
- 4.Bartels DB, Wypij D, Wenzlaff P, Dammann O, Poets CF. Hospital volume and neonatal mortality among very low birth weight infants. Pediatrics. 2006;117(6):2206–2214. doi: 10.1542/peds.2005-1624. [DOI] [PubMed] [Google Scholar]
- 5.Chung JH, Phibbs CS, Boscardin WJ, Kominski GF, Ortega AN, Needleman J. The effect of neonatal intensive care level and hospital volume on mortality of very low birth weight infants. Med Care. 2010;48(7):635–644. doi: 10.1097/MLR.0b013e3181dbe887. [DOI] [PubMed] [Google Scholar]
- 6.Helenius K, Sjörs G, Shah PS, Modi N, Reichman B, Morisaki N, et al. Survival in very preterm infants: an international comparison of 10 national neonatal networks. Pediatrics. 2017;140(6):140. doi: 10.1542/peds.2017-1264. [DOI] [PubMed] [Google Scholar]
- 7.Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M, et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatr. 2016;177:144–152.e6. doi: 10.1016/j.jpeds.2016.04.083. [DOI] [PubMed] [Google Scholar]
- 8.Hahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: in comparison with Japan and the USA. J Korean Med Sci. 2011;26(4):467–473. doi: 10.3346/jkms.2011.26.4.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shim JW, Jin HS, Bae CW. Changes in survival rate for very-low-birth-weight infants in Korea: comparison with other countries. J Korean Med Sci. 2015;30(Suppl 1):S25–34. doi: 10.3346/jkms.2015.30.S1.S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang YS, Park HY, Park WS. The Korean neonatal network: an overview. J Korean Med Sci. 2015;30(Suppl 1):S3–S11. doi: 10.3346/jkms.2015.30.S1.S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Executive Committee of Korean Neonatal Network. 2013 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 12.The Executive Committee of Korean Neonatal Network. 2014 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 13.The Executive Committee of Korean Neonatal Network. 2015 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 14.The Executive Committee of Korean Neonatal Network. 2016 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 15.Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116(6):1353–1360. doi: 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- 16.Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33(1):179–201. doi: 10.1016/S0031-3955(16)34975-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529–534. doi: 10.1016/s0022-3476(78)80282-0. [DOI] [PubMed] [Google Scholar]
- 18.Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314(10):1039–1051. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Isayama T, Lee SK, Mori R, Kusuda S, Fujimura M, Ye XY, et al. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics. 2012;130(4):e957–65. doi: 10.1542/peds.2012-0336. [DOI] [PubMed] [Google Scholar]
- 20.R Development Core Team. R: a language and environment for the statistical computing. [Updated 2018]. [Accessed March 15, 2018]. https://www.R-project.org/
- 21.Gilstrap LC NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. Effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA. 1995;273(5):413–418. doi: 10.1001/jama.1995.03520290065031. [DOI] [PubMed] [Google Scholar]
- 22.Carlo WA, McDonald SA, Fanaroff AA, Vohr BR, Stoll BJ, Ehrenkranz RA, et al. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22 to 25 weeks' gestation. JAMA. 2011;306(21):2348–2358. doi: 10.1001/jama.2011.1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mori R, Kusuda S, Fujimura M Neonatal Research Network Japan. Antenatal corticosteroids promote survival of extremely preterm infants born at 22 to 23 weeks of gestation. J Pediatr. 2011;159(1):110–114.e1. doi: 10.1016/j.jpeds.2010.12.039. [DOI] [PubMed] [Google Scholar]
- 24.McElrath TF, Norwitz ER, Nour N, Robinson JN. Contemporary trends in the management of delivery at 23 weeks' gestation. Am J Perinatol. 2002;19(1):9–15. doi: 10.1055/s-2002-20176. [DOI] [PubMed] [Google Scholar]
- 25.Van Marter LJ. Epidemiology of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009;14(6):358–366. doi: 10.1016/j.siny.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Kinsella JP, Greenough A, Abman SH. Bronchopulmonary dysplasia. Lancet. 2006;367(9520):1421–1431. doi: 10.1016/S0140-6736(06)68615-7. [DOI] [PubMed] [Google Scholar]
- 27.Majnemer A, Riley P, Shevell M, Birnbaum R, Greenstone H, Coates AL. Severe bronchopulmonary dysplasia increases risk for later neurological and motor sequelae in preterm survivors. Dev Med Child Neurol. 2000;42(1):53–60. doi: 10.1017/s001216220000013x. [DOI] [PubMed] [Google Scholar]
- 28.Jo HS, Cho KH, Cho SI, Song ES, Kim BI. Recent changes in the incidence of bronchopulmonary dysplasia among very-low-birth-weight infants in Korea. J Korean Med Sci. 2015;30(Suppl 1):S81–S87. doi: 10.3346/jkms.2015.30.S1.S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–456. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ancel PY, Goffinet F, Kuhn P, Langer B, Matis J, Hernandorena X, et al. Survival and morbidity of preterm children born at 22 through 34 weeks' gestation in France in 2011: results of the EPIPAGE-2 cohort study. JAMA Pediatr. 2015;169(3):230–238. doi: 10.1001/jamapediatrics.2014.3351. [DOI] [PubMed] [Google Scholar]
- 31.Cho SJ, Shin J, Namgung R. Initial resuscitation at delivery and short term neonatal outcomes in very-low-birth-weight infants. J Korean Med Sci. 2015;30(Suppl 1):S45–S51. doi: 10.3346/jkms.2015.30.S1.S45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Futagi Y, Toribe Y, Ogawa K, Suzuki Y. Neurodevelopmental outcome in children with intraventricular hemorrhage. Pediatr Neurol. 2006;34(3):219–224. doi: 10.1016/j.pediatrneurol.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 33.Fitzgibbons SC, Ching Y, Yu D, Carpenter J, Kenny M, Weldon C, et al. Mortality of necrotizing enterocolitis expressed by birth weight categories. J Pediatr Surg. 2009;44(6):1072–1075. doi: 10.1016/j.jpedsurg.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Nishida H, Sakuma I. Limit of viability in Japan: ethical consideration. J Perinat Med. 2009;37(5):457–460. doi: 10.1515/JPM.2009.112. [DOI] [PubMed] [Google Scholar]
- 35.Yamaguchi F, Tamura M. Report on the results of a bioethical study in neonatal care: first part: handling of infants with a gestational age of 22 weeks. J Jpn Soc Perinat Neonat Med. 2009;45:864–871. [Google Scholar]
- 36.Smith PB, Ambalavanan N, Li L, Cotten CM, Laughon M, Walsh MC, et al. Approach to infants born at 22 to 24 weeks' gestation: relationship to outcomes of more-mature infants. Pediatrics. 2012;129(6):e1508–e1516. doi: 10.1542/peds.2011-2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim JK, Chang YS, Sung S, Ahn SY, Yoo HS, Park WS. Trends in survival and incidence of bronchopulmonary dysplasia in extremely preterm infants at 23–26 weeks gestation. J Korean Med Sci. 2016;31(3):423–429. doi: 10.3346/jkms.2016.31.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]