Abstract
Background
In order to provide essential scientific evidence on the population's health status and social health determinants as well as the current capacity of the health care system in Vietnam to health policy makers and managers, Vietnam Ministry of Health, Hanoi University of Public Health, Hanoi Medical University, and Ho Chi Minh University of Medicine and Pharmacy collaborated with Seoul National University (Korea) and conducted a health system survey in the Quoc Oai district (of Hanoi capital) that represented northern rural Vietnam.
Methods
The study design was a cross-sectional study. The survey covered different topics (more than 200 questions) and was administered in three separate questionnaires: 1) Basic information of all household members; 2) Household characteristics; and 3) Individual characteristics. Socio-demographic characteristics among the households and individuals were collected from 2,400 households sampled by multi-stage cluster sampling method: more than 200 questions.
Results
The household size of Quoc Oai was larger than the national average and there was no significant difference in gender composition. In addition, the proportions of pre-elderly, age 55–64, and elderly group (65 years old and over) were higher than the national population statistics. In this context, demographic transition has begun in Quoc Oai.
Conclusion
This study design description provides the basic information about a baseline survey of a future prospective cohort (as a part of a collaborative project on strengthening the health system in Vietnam) to the prospective data user of this survey.
Keywords: Baseline Survey, Health System Strengthening, Vietnam
Graphical Abstract
INTRODUCTION
Together with the changes in the socioeconomic situation of the country, Vietnam is undergoing rapid epidemiological transitions, demonstrated by a double burden of communicable (tuberculosis, human immunodeficiency virus and acquired immune deficiency syndrome [HIV/AIDS], malaria, etc.) and non-communicable diseases (cardiovascular diseases, cancers, diabetes, etc.). Non-communicable diseases, which have been the leading causes of death in the country, rose from 427,000 deaths in 2012 to 521,000 deaths in 2015.1,2 As a result, Vietnam's health care system is also undergoing reforms to solve both the traditional and new health problems.3
As the process of health system reform is well underway in Vietnam, it is crucial for health policy makers and managers to have scientific evidence on the local population's health profiles and social determinants as well as evidence on the current capacity of health care providers in Vietnam.
To generate scientific evidence for the above-mentioned purposes, Vietnam Ministry of Health (MoH), Hanoi University of Public Health (HUPH), Hanoi Medical University (HMU), and Ho Chi Minh University of Medicine and Pharmacy (UMP) of Vietnam have worked together with Seoul National University (SNU) from Korea to conduct a health system survey in two districts of Vietnam (one in the North and one in the South). This collaboration between global south and north benefited both parties by mutual learning as well as increasing quality of research work.4,5 This paper reports the methods and key socio-demographic characteristics of households and individuals captured by the survey conducted in Quoc Oai district of Hanoi capital (in the North of Vietnam) in 2016, which will be developed into a prospective cohort in the near future.
METHODS
Study design
This was a cross-sectional study.
Study setting
Quoc Oai is a rural district located in the North of Vietnam, 20 km west of Hanoi capital. Quoc Oai district covers an area of 147 km2, including lowlands and mountains as it spreads over 20 communes and a town. The number of households and population of Quoc Oai in 2014 were 46,455 and 175,835, respectively. Per capita income of Quoc Oai in 2014 was VND 26,000,000 (USD 1,100).6 The health care system in Quoc Oai includes the district health bureau, district hospital, district center for preventive medicine, district center for population and 21 commune health stations. Ninety percent of commune health stations in Quoc Oai had medical doctors, all of which had midwives or obstetric and pediatric assistant doctors, and most had sufficient essential drugs.7
Quoc Oai was selected as the research site in the North of Vietnam because it is a typical northern Vietnam district with respect to socioeconomic characteristics and health status. Furthermore, local authorities and health leaders were strongly supportive and committed to the project, which created favorable conditions to construct and develop this project.
Sample size
The sample size for this survey was estimated based on the WHO formula8 for estimating the proportion of households incurring catastrophic medical payment, defined as when a household's total out-of-pocket health payments equal or exceed 40% of the household's capacity to pay, an important indicator for measuring universal health coverage. In order to estimate the sampling size using the expected proportion of households in the district incurring catastrophic expenditure of 3%, we have calculated that 2,400 households were needed to detect the effect size at 5% significance level with absolute precision of 1%, design effect as 2 and allowing non-response rate of about 10% in the above example.
Sampling
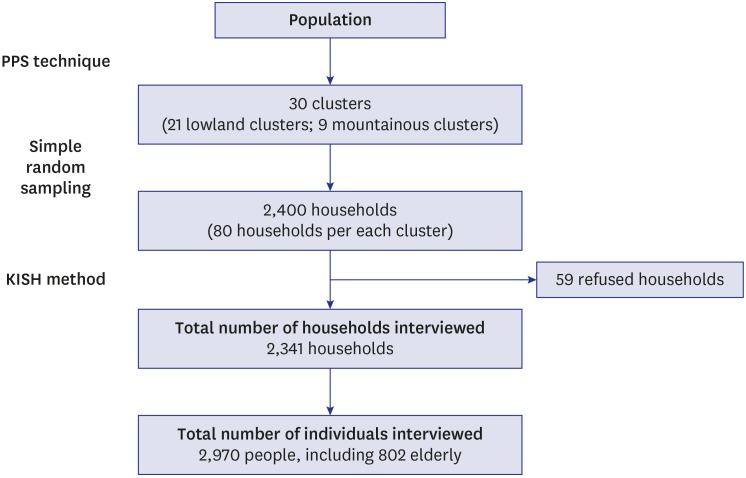
Multistage cluster sampling method was applied. First, to select the sample clusters for the study, the district was divided into 2 strata (lowland and mountain). We randomly selected 30 clusters (villages) from the 2 strata (21 lowland clusters and 9 mountainous clusters). Second, in each cluster, 80 households were chosen by using the simple random sampling technique (total of 2,400 households). The interviews on household characteristics were completed with the heads of the selected households. Third, for the individual level characteristics, the interviews on self-reported health problems, including chronic non-communicable diseases, were conducted with up to 2 individuals per household (one person aged 15–59 and one person aged 60 and above). The selection of participants for interviews on self-reported health problems among household members per each selected household was done using the Kish method.9 The sampling method and the distribution of the study sample are presented in Fig. 1 and Table 1, respectively.
Fig. 1. Survey process.
Table 1. Number of clusters and households selected and completed in the survey.
| Variables | No. of selected communes | No. of selected clusters | No. of selected households | No. of surveyed households | |
|---|---|---|---|---|---|
| Low land area | 15 | 21 | 1,680 | 1,645 | |
| Sub-urban area | 1 | 2 | 160 | 158 | |
| Rural area | 14 | 19 | 1,520 | 1,487 | |
| Mountainous area | 2 | 9 | 720 | 696 | |
| Total | 17 | 30 | 2,400 | 2,341 | |
Survey questionnaires
The survey questionnaires were developed by members of the team based on their own survey experiences. The survey covered different topics (more than 200 questions) and was administered in three separate questionnaires: 1) Basic information of all household members; 2) Household characteristics; and 3) Individual characteristics. The first questionnaire asked the head of household or decision maker to provide information on each member of the household. The questions focused on five topics: demographic information, self-reported chronic diseases, healthcare service utilization, self-treatment and health care expenditure. The second questionnaire captured household level characteristics such as household income/expenditure, fixed assets, durable goods, hygiene practices in livestock and agriculture activities. The individual questionnaire focused on acute symptoms, smoking, use of alcohol, access to health promotion information, and quality of life, etc. Quality of life data were captured for respondents aged 60 and older. All questionnaires were pre-tested to ensure ease of understanding and local cultural applicability.
Data collection and quality assurance
Data were collected based on face-to-face household interviews. Interviews were conducted by 20 local data collectors, who marked respondent data directly onto the paper survey. The data collectors (local health collaborators with good interviewing skills) were trained in a two-day workshop, which included classroom lectures, discussions, role-play, mock interviews, and field practice. The research team from HUPH supervised data collection in the field. Eight field supervisors accompanied data collectors to interviews and/or randomly checked on-going interviews.
Data management and analysis
Collected data were entered into a database using Epi Data 3.1. Both descriptive and analytical statistics were performed. Data were cleaned, edited, and analyzed using Stata statistical software version 12 (StataCorp LP, College Station, TX, USA). In this paper, only descriptive analyses were performed.
Ethics statement
This survey was approved by the ethics committee at the HUPH (Certificate No. 003/2016/YTCC‐HD3). All participants were informed about background information and rationale of the survey and of their rights to refuse participation without consequences.
RESULTS
Of the 2,400 sampled households, 2,341 of the households responded, resulting in a response rate of 97.5%. Household heads or decision makers were interviewed and provided general information on the household and each of its members. As a result, data on 10,031 individuals from 2,341 households were collected. A total of 2,970 individuals aged 15 years old or above were interviewed using an individual interview questionnaire. Of the 2,970 interviewees, 802 individuals were 60 years old and over.
The average household size was four and the median annual household income was VND 98,751,740 (USD 4,369.5). Households spent an average of VND 4,288,384 (USD 189.7) per month on regular expenses (e.g., food, electricity, water and daily necessities), and VND 49,134,730 (USD 2,174.1) per year on irregular expenses (e.g. tuition fees, clothing, jewelry, furniture, and tax).
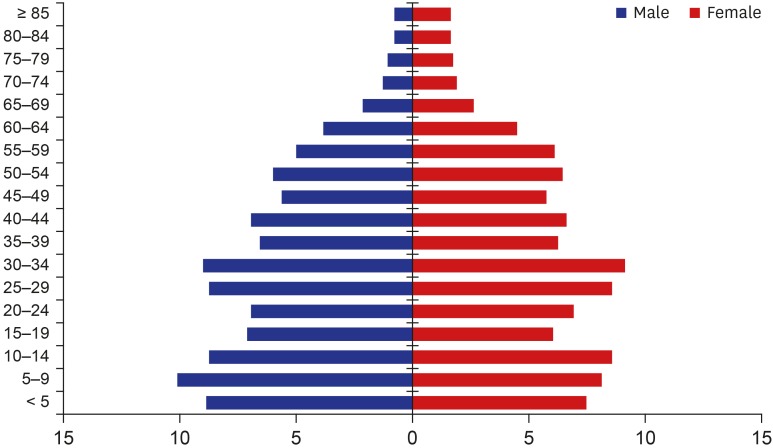
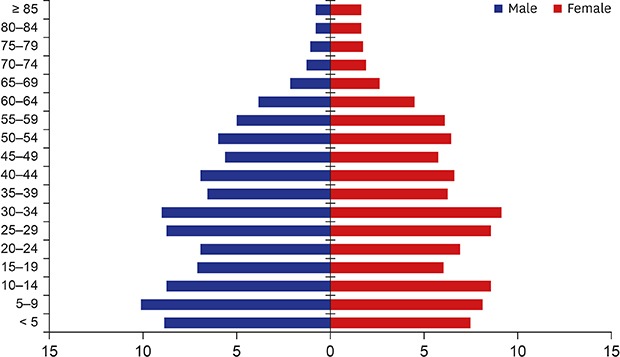
Fig. 2 and Table 2 show the socio-demographic characteristics of the respondents. Of the study population, 49.9% were men and 50.1% were women. The ethnic majority in this particular area was the Kinh (75.3%) vs. other minority ethnicities were (24.7%). Almost all (97.5%) respondents reported not having a religion. By age group, individuals aged 25–34 accounted for the biggest share (17.3%). The majority of the study population (25 years old and over) reported that they completed secondary education (39.5%). People with an undergraduate or postgraduate degree accounted for 13.7% of the study population. The proportion of married people was 80%, in which the proportion of people currently having a wife/husband accounted for 71.8%. The proportion of widow/divorce/separation was 8.2%. About one-third of the study population (33.2%) reported that their main job was a farmer or fisherman. Government officials accounted for merely 1.6% and the unemployed/retired occupied 4.9%. The proportion of people having health insurance was approximately 75.0%.
Fig. 2. Age structure of Quoc Oai populations in 2016.
Table 2. Socio-demographic characteristics of the respondents.
| Variables | Count, No. (%) | |
|---|---|---|
| Overall | 10,031 (100.0) | |
| Sex | ||
| Male | 5,001 (49.9) | |
| Female | 5,030 (50.1) | |
| Age group, yr | ||
| < 5 | 1,009 (10.1) | |
| 5–14 | 1,725 (17.2) | |
| 15–24 | 1,410 (14.1) | |
| 25–34 | 1,739 (17.3) | |
| 35–44 | 1,323 (13.2) | |
| 45–54 | 1,167 (11.6) | |
| 55–64 | 922 (9.2) | |
| ≥ 65 | 736 (7.3) | |
| Highest education level completed 25 years old and over | 6,061 (100.0) | |
| Primary school or lower | 1,730 (28.5) | |
| Secondary school | 2,391 (39.5) | |
| High school | 1,110 (18.3) | |
| College/university/post-graduate | 830 (13.7) | |
| Ethnicity | ||
| Kinh people | 7,549 (75.3) | |
| Ethnic minority | 2,482 (24.7) | |
| Religion | ||
| No religion | 9,780 (97.5) | |
| Other | 251 (2.5) | |
| Main occupation | ||
| Small/pupil/student | 3,384 (33.7) | |
| Government official | 165 (1.6) | |
| Workers | 952 (9.5) | |
| Farmer/fishermen | 3,329 (33.2) | |
| Unemployed/retired | 490 (4.9) | |
| Other | 1,711 (17.1) | |
| Marital status 15 years old and over | 7,420 (100.0) | |
| Single | 1,477 (19.9) | |
| Married | 5,324 (71.8) | |
| Widowed/separated/divorced | 608 (8.2) | |
| Missing | 11 (0.1) | |
| Have health insurance | ||
| Yes | 7,519 (75.0) | |
| No | 2,512 (25.0) | |
DISCUSSION
This paper presents the study design and key socio-demographic characteristics of households and individuals from our health system research site in the North of Vietnam. This is comprehensive additional information collection to similar contents from a health and demographic surveillance system, which is established in a defined population to collect longitudinal population-based data in limited resource settings.10 The findings from the paper can be used as background information for future health system research by relevant researchers and our follow-up surveys such that this survey will facilitate the start of evidence-based health planning and management process in the study setting.
The response rate of this baseline survey was 97.5%, higher than that of the 2016 CHILILAB Health and Demographic Surveillance System (HDSS) in Vietnam (95.6%).11 It was also higher than the response rates of 95% of Matlab HDSS in Bangladesh and Purworejo HDSS in Indonesia but lower than the rate of 100% in Kanchanaburi HDSS in Thailand.12
The household size in the 2016 Quoc Oai baseline survey was higher than that of the 2016 CHILILAB HDSS survey (4.3 compared to 3.1 per household).11 It was also bigger than the census data collected for the Red River Delta and the whole country (3.5 and 3.7 per household respectively).13 This difference can be explained by the fact that in Quoc Oai, many people still maintain the tradition of living in large households (four or more members), and multiple generations living under one roof. However, in recent years, the shift of household size from large families to small-scale families is becoming more common in Quoc Oai district in accordance with the general trend of the country.
As for ethnicity, the percentage of Kinh people in Quoc Oai district was lower than that of Chi Linh district (75.3% compared to 99.7%).11 In Quoc Oai, there are two communes named Dong Xuan and Phu Man which belong to the mountainous area, where some minority ethnic groups live together such as the Muong, Thai, and Tay people, etc. lived together. Meanwhile, almost the entire area of CHILILAB HDSS was based in the lowland area.
We observed no significant differences in the gender composition in this study compared to the survey in Chi Linh in 2016 (48.5% men and 51.5% women).11 It also remained on par with data of the Red River Delta and the national census data (49.0% men and 51.0% women; 49.3% men and 50.7% women respectively).14
Generally speaking, the 2016 Quoc Oai age structure was quite similar to the national figures reported by the most recent Vietnam Population and Housing Census in 2014. However, there still were some slight differences. The proportion of the 15–24 age group in Quoc Oai was lower than the national figure (14.1% compared to 17.6%).14 This difference may be a consequence of our definition of household resident. As such, a person would be counted as a household resident and be included in the survey if he or she has lived and eaten at the household for at least the last 3 months. The young aged 15 to 24 years often study or work in Hanoi or other provinces or even abroad so they were not included in the survey. On the other hand, the proportion of 55–64 age-group and the elderly group (65+) were higher than the national data.14 The Quoc Oai population is starting an “aging” trend.
Therefore, it is very important to address this demographic transition through research and interventions, namely, by developing health care systems for the elderly, enhancing the quality of life for the elderly, and providing recommendations to improve pension and health insurance policies. A cross-sectional study design is an insufficient approach to construct a base for the evidence-based health policy formation. If this study continues towards a longitudinal cohort study as planned, future research will be able to serve a stronger base for developing evidence-based policy by showing empirical evidence and/or by suggesting pilot study ideation. There are no strong evidence yet to show the similarities and differences between high-income nation and in low- and middle-income countries (LMICs) using longitudinal data due to a few community based longitudinal studies in LMICs. This new cohort study can address which risk factors among well-known risk factors from the high-income nations are evident in Vietnam or whether Vietnamese national health insurance enrollment is working similarly or differently compared to other countries. In this sense, this comprehensive study setting is worthwhile to be a longitudinal cohort in the near future such that stronger evidence could be disclosed to make more promising policy formation.
The highest education level completed by Quoc Oai residents who were 25 years old and over was quite similar to CHILILAB people from the same age group. In both surveys, individuals who completed secondary school accounted for the largest proportion (39.5% in Quoc Oai and 40.5% in Chi Linh respectively). Meanwhile, the proportion of residents holding a college, university or post-graduate degree occupied 13.7% and 15.2% respectively.11
Our analysis of data captured from the 6,315 respondents in working age (15–60 years) suggested an unemployment rate of 1.98%. This was higher than the CHILILAB 2016 rate (0.75%) but lower than that observed in the Red River Delta in 2014 (2.82%).11,14 The proportion of people currently having a wife/husband in Quoc Oai 2016 was similar to CHILILAB 2016 (75.6%) but higher than that of Red Delta River (67.6%).11,13
In the study, the 2016 average household income per year (VND 98,751,740) was significantly lower than that reported in the 2016 CHILILAB HDSS Survey (VND 112,019,000) and the Red River Delta in 2012 (VND 101,827,992).15 Each Quoc Oai household spent less money on regular expenses per month than those in Chi Linh households (VND 4,288,384 compared to VND 4,487,023 per month) but spent more money on irregular expenses per year than each CHILILAB household (VND 49,134,730 compared to VND 31,118,230 per year).11 Furthermore, the monthly total consumption expenditure per capita in Quoc Oai in 2016 (VND 1,949,756) was higher than those of the Red River Delta and the whole country (VND 1,889,000 and VND 1,603,000 respectively).15
There was no significant differences observed between the percentage of people having health insurance in this baseline survey and the 2016 CHILILAB HDSS baseline survey (75% and 76.4% respectively).11 Even though this survey would help evidence-based health policy by prospective health system research based on this survey data, this data could not represent all the Vietnamese context considering these data collection is from a rural district.
In conclusion, this study design description provides the basic information about a baseline survey of a future prospective cohort (as a part of a collaborative project on strengthening the health system in Vietnam) to the prospective data user of this survey. The researchers who are willing to contribute for improving people's health and healthcare system of Vietnam should be welcomed and encouraged to be the prospective data user of this survey. This comprehensive baseline data preparation with a number of variables across various aspects will serve to find out potential enablers and barriers to better population health in the near future through planned future cohort follow-up of individual risk factors and health system factors. Data access can be obtained by prospective users will be given to the prospective users through four institutions (HUPH, HMU, UMP of Ho Chi Minh City, Vietnam; and SNU College of Medicine, School of Public Health, College of Nursing, and School of Dentistry).
ACKNOWLEDGMENTS
This research was financially supported by the JW LEE Center for Global Medicine of Seoul National University College of Medicine, Seoul, South Korea. This project is part of a collaborative project by Hanoi University of Public Health, Hanoi Medical University, University of Medicine and Pharmacy of Ho Chi Minh City and the JW LEE Center for Global Medicine of Seoul National University College of Medicine, Seoul, South Korea. Authors wait and thank in advance for any possible future research grant opportunity, which enable this baseline survey to become a successful future prospective cohort as a continuing part of a collaborative project on strengthening the health system in Vietnam. If authors get future grant agency support, follow-up round surveys will be conducted in regular intervals such as every 2 or 3 years with successful collaboration of stakeholders. Death, new disease incidence, and risk factor changes will be followed up to construct a prospective longitudinal cohort. The data will be publicly available for research purpose as one of the public goods to improve Vietnamese health and population health in other LMICs.
Footnotes
Funding: This research was supported by Vietnam Health System Strengthening Project of JW LEE Center for Global Medicine, Seoul National University College of Medicine (2015-2019).
Disclosure: The authors have no potential conflict of interest to disclose.
- Conceptualization: Hoang VM, Oh J, Tran TG.
- Data curation: Hoang VM, Oh J, Ngueyn BN, Dat LM.
- Formal analysis: Honag VM, Ngueyn BN.
- Investigation: Hoang VM, Oh J.
- Methodology: Hoang VM, Oh J, Nguyen VH, Le QC.
- Project administration: Hoang VM, Oh J, Lee JK, Tran TG, Lee SP, Le QC, Luu NH.
- Writing - original draft: Hoang VM, Oh J.
- Writing - review & editing: Hoang VM, Oh J, Ngueyn BN, Dat LM, Lee JK, Tran TG, Nguyen VH, Lee SP, Bang KS, Cho Y, Kim SY, Lee HY, Choi N, Dinh TS, Luu NH.
References
- 1.Hoa NP, Rao C, Hoy DG, Hinh ND, Chuc NT, Ngo DA. Mortality measures from sample-based surveillance: evidence of the epidemiological transition in Viet Nam. Bull World Health Organ. 2012;90(10):764–772. doi: 10.2471/BLT.11.100750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santosa A, Wall S, Fottrell E, Hogberg U, Byass P. The development and experience of epidemiological transition theory over four decades: a systematic review. Glob Health Action. 2014;7:23574. doi: 10.3402/gha.v7.23574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministry of Health, Vietnam, Health Partnership Group. Join Annual Health Review 2011: Strengthening Management Capacity and Reforming Health Financing to Implement the Five-year Health Sector Plan 2011–2015. Hanoi: Ministry of Health; 2011. [Google Scholar]
- 4.Macfarlane SB, Jacobs M, Kaaya EE. In the name of global health: trends in academic institutions. J Public Health Policy. 2008;29(4):383–401. doi: 10.1057/jphp.2008.25. [DOI] [PubMed] [Google Scholar]
- 5.Busse H, Aboneh EA, Tefera G. Learning from developing countries in strengthening health systems: an evaluation of personal and professional impact among global health volunteers at Addis Ababa University's Tikur Anbessa Specialized Hospital (Ethiopia) Global Health. 2014;10:64. doi: 10.1186/s12992-014-0064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quoc Oai People Committee. Overview of Quoc Oai District. Hanoi: Quoc Oai People Committee; 2016. [Google Scholar]
- 7.Quoc Oai District Health Center. Annual Report of Quoc Oai District Health Center. Hanoi: Quoc Oai District Health Center; 2016. [Google Scholar]
- 8.Lwanga SK, Lemeshow S. Sample Size Determination in Health Studies: a Practical Manual. Geneva: World Health Organization; 1991. [Google Scholar]
- 9.Kish L. A procedure for objective respondent selection within the household. J Am Stat Assoc. 1949;44(247):380–387. [Google Scholar]
- 10.Sankoh O, Byass P. The INDEPTH Network: filling vital gaps in global epidemiology. Int J Epidemiol. 2012;41(3):579–588. doi: 10.1093/ije/dys081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minh HV, Ngan TT, Ngoc NB, Kien VD, Mai VQ, Phuong TB, et al. Methods for the 2016 socioeconomic and health survey in Chi Linh Health and Demographic Surveillance System (Chililab HDSS) Asia Pac J Public Health. 2017;29(5 Suppl):9S–17S. doi: 10.1177/1010539517709068. [DOI] [PubMed] [Google Scholar]
- 12.Ng N, Van Minh H, Juvekar S, Razzaque A, Huu Bich T, Kanungsukkasem U, et al. U sing the INDEPTH HDSS to build capacity for chronic non-communicable disease risk factor surveillance in low and middle-income countries. Glob Health Action. 2009 doi: 10.3402/gha.v2i0.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.General Statistical Office (VN) The 2014 Vietnam Population and Housing Census. Hanoi: CPaHCS Committee, General Statistical Office; 2014. [Google Scholar]
- 14.General Statistical Office (VN) Statistic Yearbook of Vietnam Year 2014. Hanoi: General Statistical Office; 2014. [Google Scholar]
- 15.General Statistical Office (VN) Results of the Viet Nam Household Living Standards Survey 2012. Hanoi: General Statistical Office; 2012. [Google Scholar]