Highlights
-
•
Hydatid cyst represents the parasitic infection by Genus Echenococcus Granulosis. The disease involves mainly Liver followed by lungs and rare involvement is seen in CNS.
-
•
When it is found in Brain it is usually present in supratentorial compartment rather than infratentorial compartment. The usual area is intracerebral hemisphere. They can be isolated cyst or multicystic. Involvement of Infratentorial compartment of CNS is extremely rare.
-
•
In this case report we are presenting a rare case of Multiple Hydatid cysts involving the peripontomedullary area and extending all the way down to the foramen magnum.
Keywords: Hydatid cyst, Peripontomedullary area
Abstract
Introduction: Hydatid cyst represents the parasitic infection by Genus Echenococcus Granulosis. This disease usually involves liver followed by lungs and rarely the CNS. The CNS involvement by the Hydatid Cyst is present in 1–2% of all hydatidosis. Even when it is found in the Brain it presents usually in the supratentorial compartment. However this case was unique in having the Hydatid cyst within the infratentorial fossa. With multiple small cysts, causing mass effect and challenging for surgical resection.
Presentation: A 44 years female presented with headache, diplobia and bulbar symptoms, followed by ataxia. Full examination, proper investigations showed the peripontomedullary hydatid cysts. Surgical management is illustrated.
Discussion: It is still challenging for the neurosurgeons to operate on these lesions in spite of modern technologies and fancy approaches due to its delicate nature, associated risk of allergic reaction, cyst’s material dissemination and irreversible injury of multiple neurological structure due to prolonged compression of cranial nerves crossing the cerebellopontine angle.
Conclusion: In this case report we are presenting a rare case of Multiple Hydatid cysts involving a rare location in the brain; peripontomedullary area and extending all the way down to the foramen magnum. Supported with a literature review in relation to disease etiology, epidemiology, clinical presentation and management.
1. Introduction
CNS involvement in the Hydatid Cyst disease is an uncommon entity in the field of Neurosurgery. It can be reviewed from literature that the involvement of CNS is found in about 1–2% of all the cases of Hydatid disease [1]. Fifty to 75% cases of Intracranial hydatid cyst are seen in children [2]. Involvement of infratentorial compartment is rarely seen [3] in about 1% cases of Hydatid Cyst disease and they are difficult to manage when the cyst are multiple and present in the area which is difficult to approach or involving delicate neurovascular structures in the small vicinity of infratentorial compartment of brain. The rarity of spread of the hydatid cyst to brain is related to the blood supply of brain that it shares with the other organs of body. The involvement of Brain is uncommon as compared to cases of liver 60% and lung 20% [4]. In the brain involvement of the supratentorial compartment greater than the infratentorial compartment is again due to spread of disease to former by the middle cerebral artery which is about 75%–80% of the blood supply of brain [5].
Hydatid cyst is a disease spreads by the larval stage of the worm Echinococcus granulosis [6] in this case man act as the intermediate host while dogs are the definitive hosts. The eggs were found in the faeces of dogs that leads to contamination of the vegetations and accidentally ingested by the man and retaken by the sheep and cattle in their feed. In the blood stream the larva of the genus found their way through the blood stream in the body and can reach to any organ of the body and make the cysts. These cysts can be single solitary lesion or multiple, the clinical presentation depends upon the type of organ involved and specially in brain these cyst present as the space occupying lesions. In our case the multiple cysts were found in the retro clival, precisely in parapontomedullary cistern and involving both cerebellopontine angles and going down to the length of clivus at the edge of foramen magnum. It is referred case from a peripheral hospital to our institution which is a tertiary care and research center accepting complicated cases from all around the country.
2. Case study
A 44 year-old female, presented through the out patient department with the history of Headache, Diplopia for the last 2 years the symptoms were gradually progressive in course she developed disturbance of gait and balance after 6 months of the appearance of first symptoms. She noticed the weakness and deviation of mouth to the right side. On examination she was conscious oriented with time place and person. Her GCS was 15/15. The cranial nerve examination revealed the involvement of the V–IX, XI and XII nerves on the left side with loss of coordination on the left side and slurred speech. The patient was investigated with MRI that revealed the presence of multiple cystic SOL in the subarachnoid space of the prepontine cistern in relation to the retroclival area. The lesion was extending to both CP angles and also in cranio-caudal length to the foramen magnum. This cyst was hypointense on T1 weighted images and hyperintense on T2 weighted images this lesion was not taking contrast and presenting a clear source of pressure over the pons and medulla, indenting the surface of pons (Fig. 1). The most probable differential diagnosis made was dermoid or epidermoid cyst, neurenteric cyst or hydatid cyst of parapontomedullary area. Patient was booked for elective surgery on 23rd of September 2013. A retromastoid suboccipital craniotomy was done on the left side to reach the lesion it was also kept in mind that this lesion might require staged surgery from other side because it was extending away from the midline. The left side was selected because the main burden of the disease was on the left side and all the nerves involved were on the left side. After craniotomy the dura was incised, and arachnoid space was opened, the cerebellum was retracted medially to reach the tumor. The first look of tumor was glistening white, which was almost avascular on further dissection as expected it was found that it is a multicystic SOL with delicate cyst wall. Therefore careful dissection was made to remove these cystic structures from the left sided CP angle region these cysts were compressing all the exiting nerve roots coming out of left CP angle namely VI, VII, VIII and basal cranial nerves. The cysts were found close to the pons indenting the anterolateral surface of it at multiple levels and reaching to the anterior edge of Foramen magnum. One by one the cysts were removed and during removal after observation it was found that the cysts were containing sand like particles scolices, therefore further care was taken to avoid dissemination of these particles in the CSF spaces. Using the Normal saline irrigation maximum approachable cysts were removed, few cysts were not approachable from this side were left behind for possible second surgery. During surgery there was no unusual event occurred except small bleeding from the left transverse sinus, which was secured, using surgicil and gentle pressure. After securing the hemostasis the dura was closed primarily followed by the closure of wound in layers. Limitations of our approach is having a midline extension of the lesion, that is difficult to be approached laterally without too much retraction, significant stretch over the lower cranial nerves, bilateral representations of the lesion, inability to perform en block resection as the lesion is diffused ventrally and multicystic. After closure the patient was shifted intubated to the surgical ICU for post operative monitoring. On first post operative day CT scan brain was done revealed Hydrocephalus therefore External Ventricular Drain was introduced. Ischemic changes in the region of left cerebellum was also observed. As there was a spasm in the arteries of the posterior circulation due to reaction against the contents of the hydatid cyst. The patient remained in the ICU, gentle extubation was successful then she has recovered slowly. The EVD was removed and no changes in the ventricular size were observed after removal of EVD. Patient was returned back to ward with NGT feeding. Her conscious level had improved to 10/15. The barium swallow was performed to see the swallowing reflex but it was found that the patient needs long term tubal feed, therefore PEG tube (percutaneous endoscopic gastric tube) was inserted. She was also offered a long term physiotherapy program for the following 2 years.
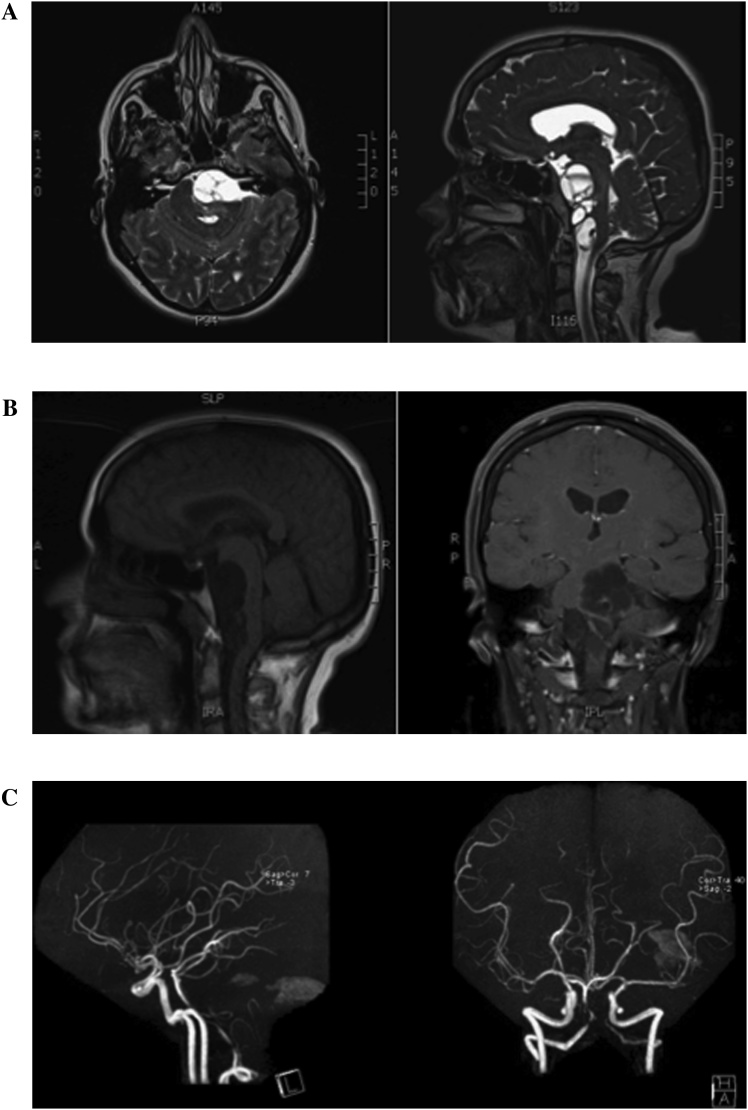
Fig. 1.
(A): MRI T2WI Axial and sagittal planes, showing the prepontomedullary multicystic hyperintense lesion, indented over the brainstem causing mass effect and narrowing of the foramen magnum. (B): MRI T1WI Sagittal and coronal planes, showing the multicystic hypointense lesion at the prepontine cistern. With no gadolinium enhancement. (C): CT-Angiography to evaluate the posterior circulation post-operatively as there were areas of ischemia post op suspected from a vasospasm, due to a reaction from the cyst content.
After 2 weeks the post operative MRI Brain with and without contrast revealed that due to excision of the cysts from left petroclival area and prepontine cistern the pressure over the brain stem was relieved but still some lesions were present which were actually not approachable from the left side (Fig. 2).
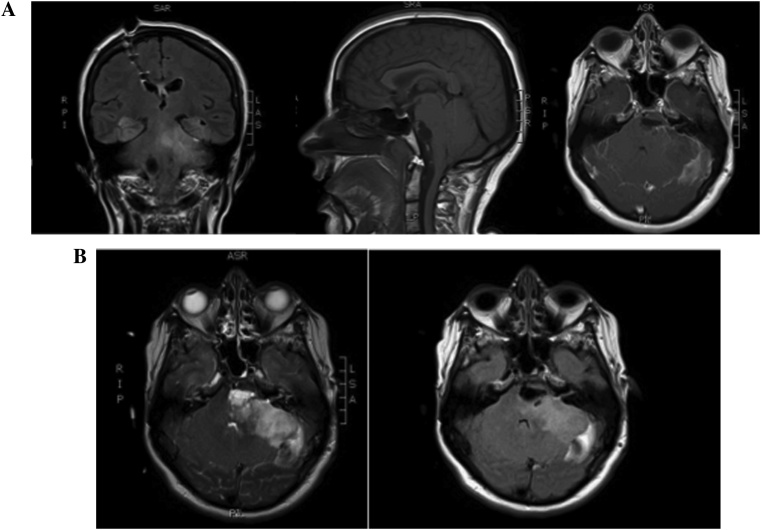
Fig. 2.
(A): Post-operative MRI T1WI with and without contrast, revealed some relieve of the pressure from the brainstem, after excision of the cysts from the left petroclival and prepontine areas. (B): Some residual in the midline at the prepontomeduulary cistern, which is difficult to be reached by the left retrosigmoid suboccipital approach.
The histopathology report confirmed the result of Hydatid cyst. MRI chest, abdomen and pelvis was performed to diagnose any other cysts and a second cyst was found in the liver. Infectious disease’s team were consulted and patient was started on the recommended doses of Albendazol 400 mg, GT, BID for 6 months. Follow up in the clinic after 1 month revealed good healing of the wound edges, GCS 15/15. Improved in gate, but persistence of the lower cranial nerves deficits on the left side. Another neurosurgical clinic visit after 1 year showed improvement clinically with occupational and physiotherapy. MRI showed subtle improvement regarding the mass effect with persistence of gliotic changes within the peripontomedullary cistern and the cerebeloopontine angle. During this time she was on regular follow up with infectious disease clinic for monitoring the body response to medications.
3. Discussion
Hydatid cyst is classified in the list of Zoonoses, Dog is the definitive host [7], which harbors the disease by eating the infected intestine of sheep, goats and other parts of flesh of different animals. Contaminated food is accidentally taken by the human, who served as intermediate host. The sheep, horse and other cattle take this through infected vegetation they eat as food. The larval stage enters the blood and then finally develops cysts in different organ of body. In human being the larva enter in the blood and reach to different organs especially with rich blood supply. Therefore the maximum spread occur to the liver then second organ affected is lung, while CNS spread is seen as rare but third most common area to be affected. Then following is the list of organs where hydatid cyst can be spread naming a few muscles, orbit, heart, adrenal gland, thyroid, submandibular gland, kidneys, intestine, internal acoustic canal, jugular foramen and spine [[7], [8], [9]]. Radiologically the Hydatid cyst can be best diagnosed with MRI with contrast study there is no enhancement. The images also revealed that the cyst can be solitary or multiple [10]. The clinical signs and symptoms are dependent on the area of brain involvement and it varies from Headache to focal neurological deficit in the area involved when the cyst is present in the posterior fossa the exiting nerve from the brain stem are affected and usually patient have multiple cranial nerves involvement and it is also possible to get signs of cerebellar disturbance and signs of brain stem involvement. Hydrocephalus may occur if the ventricular system is blocked in the latter stages [10]. Histopathological diagnosis of hydatid cyst is confirmatory by observing scolices (the sand) in the cyst fluid. Once diagnosed the treatment of choice is surgical excision of cyst both in solitary and multiple types because it will ensure the disease free host and relief the compression on the affected organs. During surgery Saline is used to do dissection of Hydatid cyst and with this method usually the cysts are delivered out. Dowling method is commonly practiced when there is large single solitary cyst present in or near the supratentorial region but when these cyst are present in odd situation then this modality is not successful and microscopic dissection is done with care of avoiding the spillage of cyst contents in the surrounding areas. In such situation some authors adequate the aspiration of the cysts first followed by the dissection and removal of the cyst [11]. During surgery full coverage of steroid is given to avoid any anaphylactic shock secondary to spillage of cyst contents in the CSF spaces. Once the diagnosis of hydatid disease is confirmed the Anti parasitic treatment Albendazole is given 400 mg orally BID for 3–6 months. The other body parts, which are the usual area of spread, needs to be addressed. Proper scanning of the body with CT Scan and MRI Scan control and contrast will give the lesions if present in other parts of the body. The spillage of cyst material may result in the spasm of the local arteries and can result in infarction of the affected area.
Reviewing the literature over the past ten years up to date from 2008 till 2018, using pubmed searching engine we found that some geographical distribution of this disease mainly involving the Middle East and developing countries [14,16,17]. The majority of the reported cases are from Asia and Africa [12,13,15,18]. Clinical information was gathered on a summarized Table 1, obviously all the cases are children or young adults. No significant gender difference, presentation usually raised ICP in the posterior fossa setting. What unique about our case is the anterior location within the posterior fossa, whereas most of the reported cases are laterally at cerebellopontine angles or involving the cerebellar hemispheric in location. Treatment plan is almost always the same with big hydatid cyst intracranially. Careful surgical resections with pharmacological medication, most cases are treated with Albendazole for at least 6 months.
Table 1.
Geographical distribution of the hydatid cyst reported cases in the past ten years.
| Author | Year | Geographic Location | Age | Gender | Multiplicity | Location | Presentation | Treatment |
|---|---|---|---|---|---|---|---|---|
| Saqui et al. | 2017 | Morocco | 12 year-old | Male | Solitary | Posterior fossa | Raised ICPa | Surgery +Albendazole |
| Lakhdar et al. | 2010 | Morocco | 37 year-old | Male | Multiple | Posterior fossa | Raised ICPa | Surgery +Albendazole |
| Bhaskar et al. | 2012 | India | 40 year-old | Female | Multiple | Posterior fossa | Raised ICPa | Surgery +Albendazole |
| Gazzaz et al. | 2000 | Morocco | 5 year- old | Male | Solitary | Posterior fossa | Torticollis | Surgery + Albendazole |
| Karakoc et al. | 2016 | Turkey (Iraqi patient) | 14 year- old | Female | Multiple | Bilateral CP Anglesa | Respiratory Distress + Quadriparesis | Surgery + Albendazole |
| Fakhouri et al. | 2015 | Syria | 5 year-old | Female | Solitary | Right cerebellar hemisphere | Raised ICP | Surgery + Albendazole |
| Raynham et al. | 2008 | South Africa | 25 year- old | Female | Multiple | Left CP Anglea | Limbs/face weakness | Surgery + Albendazole |
ICP: Intracranial Pressure, CP Angle: Cerebellopontine Angle.
4. Conclusion
Hydatid cyst disease is not uncommon in our area, within the Middle East specifically the gulf area. Rarely patients with hydatosis present with CNS complaint, but still the intracranial dissemination of the disease can happen. The posterior fossa involvement is even much more rare. Specially peripontomedullary cistern, it should be kept in mind while skimming the imaging scans of weird looking lesions at this location. To be prepared pre- and intra-operatively with the required caution, not to implement spillage of the cyst content while operating. Treatment of the Hydatid cyst with surgical resection and Albendazole has good outcome, together with treatment of the associated hydrocephalus if present especially with posterior fossa cysts.
Conflict of interest
All authors declare that there is no conflict of interest regarding the publication of this article.
Funding
This work was completed without financial support.
Ethical approval
The Institutional Review Board (IRB) committee at our institute has given the ethical approval. With reference number RCJ/455/39.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contribution
Afnan Alkhotani, Babar But, Muhammed Khalid, Mohammed Binmahfoodh: Management of the case.
Afnan Alkhotani, Babar Butt: Study Design, data collection and Manuscript writing, submission for publication.
Mohammed Binmahfoodh: Revision of manuscript.
Registration of research studies
Not Applicable on this case report.
Guarantor
Dr. Mohammed Binmahfoodh.
Dr. Afnan Alkhotani.
Provenance and peer review
Not commissioned, externally peer-reviewed
SCARE guidelines
This work has been reported in line with the SCARE criteria [19].
References
- 1.Ali M. Hydatid cysts of the brain. J. Ayub Med. Coll. Abbottabad. 2009;21(July–September (3)):152–154. [PubMed] [Google Scholar]
- 2.Ersahin Y. A case of thalamic hydatid cyst. Clin. Neurol. Neurosurg. 1995;97(November (4)):321–323. doi: 10.1016/0303-8467(95)00052-l. [DOI] [PubMed] [Google Scholar]
- 3.Sanli A. Hydatid cyst of the ambient cistern radiologically mimicking an arachnoid cyst. J. Neurosurg. Pediatr. 2012;10(September (3)):186–188. doi: 10.3171/2012.6.PEDS11562. Epub 2012 July 13. [DOI] [PubMed] [Google Scholar]
- 4.Vavra P. Surgical treatment of complicated hepatic echinococcosis in two Bulgarian citizens at two surgical departments in the Czech Republic. Rozhl. Chir. 2012;91(July (7)):381–387. [PubMed] [Google Scholar]
- 5.Lindegaard K.F. Variation in middle cerebral artery blood flow investigated with noninvasive transcranial blood velocity measurement. Stroke. 1987;18:1025–1030. doi: 10.1161/01.str.18.6.1025. [DOI] [PubMed] [Google Scholar]
- 6.Taratuto A.L., Venturiello S.M. Echinococcosis. Brain Pathol. 1997;7(January (1)):673–679. doi: 10.1111/j.1750-3639.1997.tb01082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geramizadeh Bita. Unusual locations of the hydatid cyst: a review from Iran. Iran. J. Med. Sci. 2013;38(1):2–14. [PMC free article] [PubMed] [Google Scholar]
- 8.Wani R.A. Hydatid disease at unusual sites. Int. J. Case Rep. Imag. 2012;3(6):1–6. [Google Scholar]
- 9.Akdemir G. Hydatid cysts of the internal acoustic canal and jugular foramen. J. Clin. Neurosci. 2007;14(April (4)):394–396. doi: 10.1016/j.jocn.2006.04.007. Epub 2007 Jan 30. [DOI] [PubMed] [Google Scholar]
- 10.Alexandra O., Bogdan O.P. Intracranial cysts: an imagery diagnostic challenge. Sci. World J. 2013 doi: 10.1155/2013/172154. Published online May 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muthusubramanian V. Surgical management of brain stem hydatid cyst—an unusual site. Surg. Neurol. 2009;71(January (1)):103–106. doi: 10.1016/j.surneu.2007.06.077. discussion 106, Epub 2008 February 11. [DOI] [PubMed] [Google Scholar]
- 12.Saqui A.E., Aggouri M., Benzagmout M., Chakour K., Faizchaoui M.E. Kyste hydatique de la fosse cérébralepostérieure. Pan Afr. Med. J. 2017;26:133. doi: 10.11604/pamj.2017.26.133.8363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lakhdar F., Arkha Y., Bougrine M., Derraz S., El Ouahabi A., El Khamlichi A. Kyste hydatique intra- et extracrânien de la fosse cérébrale postérieure (à propos d’un cas) Neurochirurgie. 2010;1699(October (5)):363–428. doi: 10.1016/j.neuchi.2010.01.001. ISSN 0028-3770. [DOI] [PubMed] [Google Scholar]
- 14.Bhaskar S., Choudhary A., Singh A.K. Posterior fossa extradural hydatid cyst with septae and calcification. NeurolIndia. 2012;60:242–243. doi: 10.4103/0028-3886.96426. http://www.neurologyindia.com/text.asp?2012/60/2/242/96426 [cited 2018Jul18] Available from: [DOI] [PubMed] [Google Scholar]
- 15.Kyste hydatique extradural de la fosse cérébrale postérieure, 1101 (4) (2000) 339–409, ISSN 0028-3770, https://doi.org/JNG-09-2000-46-4-0028-3770-101019-ART97. [PubMed]
- 16.Karakoc Z.C. A life-threatening brainstem compression by cerebral Echinococcus granulosus, 2016. Infez. Med. 2016;24(1):62–66. [PubMed] [Google Scholar]
- 17.Fakhouri F., Ghajar A., Mahli N., Shoumal N. Giant hydatid cyst in the posterior fossa of a child. Asian J. Neurosurg. 2015;10(4):322–324. doi: 10.4103/1793-5482.162719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raynham O.W., Mulwafu W., Fagan J.J. Hydatid disease of the skull base: report of three cases and a literature review. Skull Base. 2009;19(2):171–175. doi: 10.1055/s-0028-1096207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]