Abstract
We introduce the National Institute on Minority Health and Health Disparities (NIMHD) research framework, a product that emerged from the NIMHD science visioning process.
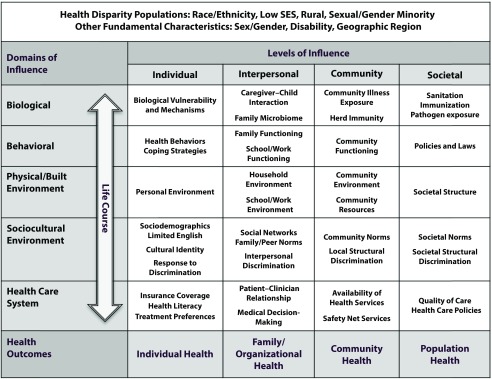
The NIMHD research framework is a multilevel, multidomain model that depicts a wide array of health determinants relevant to understanding and addressing minority health and health disparities and promoting health equity. We describe the conceptual underpinnings of the framework and define its components.
We also describe how the framework can be used to assess minority health and health disparities research as well as priorities for the future. Finally, we describe how fiscal year 2015 research project grants funded by NIMHD map onto the framework, and we identify gaps and opportunities for future minority health and health disparities research.
Understanding and addressing health disparities in all of their complexity and promoting health equity requires applying a multidimensional research lens.1 The National Institute on Minority Health and Health Disparities (NIMHD) research framework (hereafter “the framework”) is a tool for conceptualizing and depicting the wide array of determinants that promote or worsen minority health or cause, sustain, or reduce health disparities. These determinants may reflect etiological factors related to health outcomes as well as intervention targets to improve minority health or reduce disparities. NIMHD considers the framework to be a work in progress and may change it in response to changes in research conceptualizations or terminology as well as feedback from the extramural community and other stakeholders.
DEFINITIONS
NIMHD defines minority health as all aspects of health and disease in one or more racial/ethnic minority populations as defined by the Office of Management and Budget, including Blacks/African Americans, Hispanics/Latinos, Asians, American Indians/Alaska Natives, and Native Hawaiians/other Pacific Islanders.2 NIMHD defines a health disparity as a health difference, on the basis of one or more health outcomes, that adversely affects disadvantaged populations. According to the legislation that created NIMHD,3 a health disparity population is characterized by a pattern of poorer health outcomes, indicated by the overall rate of disease incidence, prevalence, morbidity, mortality, or survival in the population as compared with the general population. Current NIMHD-designated health disparity populations include Office of Management and Budget–defined racial/ethnic minorities, socioeconomically disadvantaged populations, underserved rural populations, and sexual and gender minorities (which include lesbian, gay, bisexual, transgender, and gender-nonbinary or gender-nonconforming individuals).
ORGANIZATION OF THE FRAMEWORK
The framework reflects a hybrid of two existing models: the National Institute on Aging (NIA) health disparities research framework4 and the socioecological model.5 The NIA framework organizes levels of analysis of health disparities relevant to aging research into several domains, including biological, behavioral, sociocultural, and environmental. The NIMHD framework expands on the NIA framework to include one additional domain (the health care system) and uses slightly different labels for two other domains (sociocultural environment and physical or built environment). Although the health care system domain can be considered a subset of both the sociocultural environment (e.g., cultural competence, clinician bias) and the physical and built environment (e.g., access to specialty care, availability of bilingual providers), we used it as a separate domain in the framework because of its relevance to health disparities.
The NIMHD framework further extends the NIA framework by categorizing domains of determinants according to levels of the socioecological model. The socioecological model, first introduced by Bronfenbrenner,5 posits that health and human development are influenced by factors at multiple levels, from the individual to the macro or societal level. The resulting graphic representation of the framework (Figure 1) is a matrix with two axes, with the y-axis depicting domains of influence on health (biological, behavioral, physical and built environment, sociocultural environment, health care system) and the x-axis depicting levels of influence on health (individual, interpersonal, community, societal). The societal level may encompass states, regions within a country, or entire nations or world regions.
FIGURE 1—
The National Institute on Minority Health and Health Disparities Research Framework: 2017
Note. SES = socioeconomic status. Available at: https://www.nimhd.nih.gov/about/overview/research-framework.html. Accessed February 19, 2018.
The combination of these dimensions produces 20 cells that each reflect a unique set of determinants that may be relevant for any particular minority health outcome or health disparity. For example, racial/ethnic disparities in lung cancer mortality may be driven by genetic risk (individual–biological), smoking behavior (individual–behavioral), exposure to secondhand smoke in the home or at work (physical and built environment–interpersonal), neighborhood-level exposure to environmental toxins (physical and built environment–community), engagement in early screening (health care system–individual), access to high quality cancer treatment (health care system–community), state policies regarding Medicaid coverage of lung cancer screening and treatment (health care system–societal), and state laws regarding cigarette taxes and smoking bans (behavioral–societal).
Examples of factors within each cell are provided in Figure 1; these are not intended to constitute a comprehensive listing. At the societal level, we conceptualize policies and laws, such as those related to immigration, civil rights, worker protections, or environmental protections, as falling into the behavioral domain because of their time-limited or modifiable nature. We place societal structure, such as the organization of the government, educational, and criminal justice systems, under the physical and built environment domain because these structures are more stable over time. However, we recognize that there is conceptual overlap in these two cells.
In addition to health disparities determinants, the framework specifies that health outcomes can also span multiple levels (individual, family and organizational, community, and population). Health outcomes beyond the individual level reflect collective or aggregate outcomes (e.g., prevalence of smoking among individuals within a school or workplace, incidence of adolescent pregnancy within communities or tribes, or rates of psychiatric rehospitalization within US states or territories). Also included in the framework are the demographic characteristics associated with the currently designated National Institutes of Health (NIH) health disparity populations (race/ethnicity, socioeconomic status, rural vs urban status, and sexual or gender minority status). Sex or gender (biological or self-identification as male or female), disability status, and geographic region of residence (referring to distinct areas of the United States, such as the South, or of other countries) are included as other fundamental characteristics, as these factors may interact with race/ethnicity, socioeconomic status, rural/urban status, and sexual or gender minority status to produce unique health determinants or health outcomes.
Finally, the framework identifies the importance of a life course perspective,6 including consideration of early adverse events, chronic and cumulative social and environmental exposures, transgenerational transmission of risk and resilience, and the critical or sensitive period when environmental exposures may have heightened impact when examining determinants across domains of influence. To reflect this, a bidirectional life course perspective arrow cuts across the domains of influence column in the framework.
IMPORTANCE OF THE FRAMEWORK
The framework, developed in 2015 as part of the NIMHD science visioning process, was intended as a vehicle to convey NIMHD’s philosophy and priorities for minority health and health disparities research. The framework communicates that conducting research entirely within one cell of the framework—including within the individual–biological or individual–behavioral cells, which characterize a significant portion of traditional health research—may result in research knowledge that is incomplete because it does not address the cumulative or interactive effects of multiple determinants. The framework also depicts the need for attention to both biological and social determinants of health rather than an exclusive focus on one or the other. Finally, the framework recognizes both risk and resilience factors, as the determinants in any cell in the framework may have a positive or negative impact on minority health or health disparities.
It is NIMHD’s hope that, in addition to serving as a representation of NIMHD’s philosophy, the framework will also be used by researchers, educators, and others to further encourage a multidomain, multilevel approach to health disparities research. NIMHD encourages the public to download the framework from its Web site (https://www.nimhd.nih.gov/about/overview/research-framework.html) for use in courses, presentations, and articles, either in its original form or adapted to apply to a particular research question or population. The framework is also intended to be used as a tool to assess the state of current research and identify gaps and opportunities for future research, including those identified in the NIMHD science visioning recommendations discussed elsewhere in this journal supplement.7 This can be done by mapping funded grant projects onto the framework to assess the distribution and coverage of health determinants and health outcomes examined across the cells of the framework.
MAPPING NIMHD GRANTS ONTO THE FRAMEWORK
To determine the inclusion of multidomain, multilevel determinants in NIH-supported minority health and health disparities research grants, NIMHD undertook an analysis of the 90 NIMHD research project grant (R01) awards active in fiscal year (FY) 2015, the year the framework was developed. Our analysis did not cover all mechanisms that may support minority health and disparities research at NIMHD, but R01 grants were selected because they are the primary mechanism for funding fully powered, hypothesis-driven research projects.
The authors of this commentary reviewed the specific aims and research strategy sections of the competing grant applications of the 90 R01 awards and coded them according to which determinants of health disparities were included, whether the project used a life course approach, and the level of health outcomes. To establish standardization of coding, two staff members independently reviewed 50 of the 90 grants and compared coding; discrepancies were discussed to reach agreement on the appropriate coding. J. A. coded the remaining 40 grants. We considered determinants within a cell to be present if they were identified as a factor to explain or address minority health or health disparities and were explicitly measured in the project or included as an intervention element. We did not code factors that were generic determinants of health and not specific to minority health or health disparities. Coding did not capture the number of determinants or outcomes present within each cell.
The results of the coding are shown in Table 1, which indicates the number and proportion of NIMHD grants including at least one determinant in each cell of the framework, as well as the number and proportion including health outcomes at each level. Results are purely descriptive in nature; we did not perform any statistical testing. The median number of cells covered per R01 was five. Individual-level determinants were more common than were determinants at higher levels, with particularly low levels of community-level or societal-level determinants.
TABLE 1—
Determinants and Health Outcomes of Fiscal Year 2015 National Institute on Minority Health and Health Disparities R01 Awards: United States
| Domains of Influence | Levels of Influence, No (%) |
|||
| Individual | Interpersonal | Community | Societal | |
| Biological | 64 (71) | 10 (11) | 0 (0) | 0 (0) |
| Behavioral | 54 (60) | 28 (31) | 20 (22) | 3 (3) |
| Physical/built environment | 15 (17) | 7 (8) | 20 (22) | 2 (2) |
| Sociocultural environment | 61 (68) | 26 (29) | 10 (11) | 5 (6) |
| Health care system | 58 (64) | 38 (42) | 33 (37) | 20 (22) |
| Health outcomes | 78 (87) | 16 (18) | 18 (20) | 20 (22) |
Note. Population size was n = 90. Grants could include more than one type of determinant or outcome, so percentages across rows or columns may exceed 100%.
Nearly all (91%) grants included at least one individual-level determinant, compared with 64%, 50%, and 27% including at least one interpersonal, community-level, and societal-level determinant, respectively (percentages not shown in Table 1). Biological, behavioral, sociocultural, and health care determinants were commonly represented, particularly at the individual level, with physical and built environment determinants being less frequently included. Seventy-four percent of grants included at least one health care determinant, followed by 71% with at least one biological determinant, and 69% with at least one behavioral determinant. Only 32% included at least one physical and built environment factor (percentages not shown in Table 1). Health outcomes were typically limited to individuals, with much less measurement of interpersonal, community-level, and societal-level health outcomes. Only 13% of grants included a life course perspective (data not shown in Table 1).
IDENTIFYING FUTURE OPPORTUNITIES
This analysis provides a snapshot of NIMHD R01 grants at the time the framework was developed. Limitations of this analysis include the exclusion of grants funded by other NIH institutes and centers or other types of NIMHD grants that involve research projects and the lack of examination of patterns of determinants that may be more relevant for some populations, health conditions, or research questions than others. Nonetheless, results from this analysis point to areas of research that warrant further emphasis in future NIMHD-funded research:
-
•
All levels of physical and built environmental determinants. The physical spaces that individuals occupy to live, work, and play are increasingly recognized as critical to understanding health and health disparities, both independently and in combination with the social environment and population demographics.8 It is also recognized that interventions that focus primarily on individual behavior, such as diet, physical activity, or alcohol consumption, have shown little progress in reducing health disparities, in part because members of health disparity populations often live in environments that are not conducive to maintaining behavioral changes.9 Despite this knowledge, physical and built environmental determinants appear underrepresented in NIMHD R01 grants relative to other domains. Examination of societal-level determinants reflecting structure of the political, educational, criminal justice, and other systems were virtually absent from NIMHD R01s.
-
•
Community- and societal-level determinants across domains. Neighborhood-level or community-level factors, whether they are related to behavior (e.g., social cohesion, social capital), built environment (e.g., access to healthy food choices, residential segregation), sociocultural environment (e.g., community attitudes), or the health care system (e.g., access to specialty care), are robust predictors of health outcomes.10–12 Despite evidence that these factors are relevant to health disparities, they were infrequently included in FY2015 grants. Similarly, despite evidence of the impact of societal-level policies, laws, structures, norms, and attitudes on health outcomes,13 these factors were rarely included in R01 awards, with the exception of projects examining state and federal policies on health care provision and health insurance.
-
•
Life course issues beyond maternal and child health. The bulk of R01 awards using a life course perspective focused on the transmission of disease risk from mother to infant, either through biological (e.g., maternal gestational weight gain, vaginal microbiome of mother) or behavioral factors (alcohol, tobacco, or drug use; breastfeeding behavior). Fewer projects emphasized life course issues related to developmental periods after infancy, timing or accumulation of exposures across the lifespan, the mechanisms of social or cultural transmission of risk or resilience, or critical developmental periods or life stages on which to target interventions. These areas all have documented or theoretical implications for health disparities.14–17
-
•
Community- and population-level health outcomes. Even for R01 projects that examined multiple determinants across domains and levels, studies focused primarily on individual-level outcomes (i.e., how different constellations of multidomain, multilevel factors affect the health or health risks of an individual). This approach, which reflects the underlying principle of precision medicine approaches, may have limited potential to eliminate health disparities and may exacerbate them if access to individualized treatments are not equally accessible to all individuals.18 By definition, health disparities do not reflect variations in health among individuals but among populations. It therefore follows that attempts to reduce disparities must also take a population health approach.
CONCLUSIONS
The analysis of NIMHD R01 awards in FY2015 provides a useful foundation on which to build. Gaps and opportunities identified from this analysis are consistent with many of the NIMHD science vision recommendations.7 NIMHD has implemented several strategies to promote multilevel, multidomain research, including dissemination of the framework through NIMHD’s Web site, conference and workshop presentations by NIMHD staff, and NIMHD-sponsored funding opportunity announcements. Future analyses of NIMHD R01s and other awards made since FY2015 will determine whether these and other strategies have resulted in greater “coverage” of determinants across domains and levels of the framework. It also is clear that NIMHD needs to take a more active role in fostering and supporting research that addresses interpersonal, community-level, and societal-level health outcomes in areas beyond health services research. In addition, NIMHD plans to analyze minority health and health disparities grants across the NIH using the framework and hopes that other NIH institutes and centers and other health research funders conduct their own analyses as well.
Research done within specific individual cells of the framework has established an important foundation on which to develop the building blocks for future research. It is imperative that the next generation of research examines and addresses the interaction of determinants from different domains and levels to inform efforts to reduce disparities. These interactions are likely to be critical to understanding health disparities and strategies to address them. For example, using agent-based modeling to understand the impact of violence-prevention interventions, Cerda et al.19 found that reducing disparities in violent victimization required the elimination of residential segregation. Another simulation modeling study20 found that individual (mail reminders) and community-level (mass media messages) communication strategies were more effective in increasing colorectal cancer screening rates among rural and African American populations than was a structural strategy (expanding the number of endoscopy facilities). Without the inclusion of factors across domains and levels in these studies, important linkages across determinants and between determinants and health outcomes would have been missed.
Much work remains to be done to improve minority health, reduce health disparities, and promote health equity. It is NIMHD’s hope that the framework can serve to facilitate meaningful research progress toward these efforts.
ACKNOWLEDGMENTS
This work was supported by the National Institute on Minority Health and Health Disparities (NIMHD).
This work resulted from an NIMHD-led workshop, including external experts, to address intervention science for health disparities research.
Note. The final content is the responsibility of the authors and does not necessarily represent the perspective of the US government.
CONFLICTS OF INTEREST
No conflicts of interest.
REFERENCES
- 1.Cooper LA, Ortega AN, Ammerman AS et al. Calling for a bold new vision of health disparities intervention research. Am J Public Health. 2015;105(suppl 3):S374–S376. doi: 10.2105/AJPH.2014.302386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. 1997. Available at: https://obamawhitehouse.archives.gov/omb/fedreg_1997standards. Accessed October 5, 2018.
- 3.US Government Publishing Office. Public Law 106–525. Available at: https://www.gpo.gov/fdsys/pkg/PLAW-106publ525/pdf/PLAW-106publ525.pdf. Accessed October 5, 2018.
- 4.Hill CV, Pérez-Stable EJ, Anderson NA, Bernard MA. The National Institute on Aging health disparities research framework. Ethn Dis. 2015;25(3):245–254. doi: 10.18865/ed.25.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–531. [Google Scholar]
- 6.Fine A, Kotelchuck M. Rethinking MCH: the life course model as an organizing framework. Available at: http://www.hrsa.gov/ourstories/mchb75th/images/rethinkingmch.pdf. Accessed October 5, 2018.
- 7.Jones N, Breen N, Farhat T, Das R, Palmer R. Cross-cutting themes to advance the science of minority health and health disparities. Am J Public Health. 2019;109(suppl 1):S48–S55. doi: 10.2105/AJPH.2019.304950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tung EL, Cagney KA, Peek ME, Chin MH. Spatial context and health inequity: reconfiguring race, place, and poverty. J Urban Health. 2017;94(6):757–763. doi: 10.1007/s11524-017-0210-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baum F, Fisher M. Why behavioural health promotion endures despite its failure to reduce health inequities. Sociol Health Illn. 2014;36(2):213–225. doi: 10.1111/1467-9566.12112. [DOI] [PubMed] [Google Scholar]
- 10.Wong MS, Chan KS, Jones-Smith JC, Colantuoni E, Thorpe RJ, Jr, Bleich SN. The neighborhood environment and obesity: understanding variation by race/ethnicity. Prev Med. 2018;111:371–377. doi: 10.1016/j.ypmed.2017.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuma-Guerrero PJ, Cubbin C, von Sternberg K. Neighborhood social cohesion as a mediator of neighborhood conditions on mothers’ engagement in physical activity: results from the geographic research on wellbeing study. Health Educ Behav. 2017;44(6):845–856. doi: 10.1177/1090198116687537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Topmiller M, Zhen-Duan J, Jacquez FJ, Vaughn LM. Place matters in non-traditional migration areas: exploring barriers to healthcare for Latino immigrants by region, neighborhood, and community health center. J Racial Ethn Health Disparities. 2017;4(6):1214–1223. doi: 10.1007/s40615-016-0329-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hahn RA, Truman BI, Williams DR. Civil rights as determinants of public health and racial and ethnic health equity: health care, education, employment, and housing in the United States. SSM Popul Health. 2018;4:17–24. doi: 10.1016/j.ssmph.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dixon B, Peña MM, Taveras EM. Lifecourse approach to racial/ethnic disparities in childhood obesity. Adv Nutr. 2012;3(1):73–82. doi: 10.3945/an.111.000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fox M, Entringer S, Buss C, DeHaene J, Wadhwa PD. Intergenerational transmission of the effects of acculturation on health in Hispanic Americans: a fetal programming perspective. Am J Public Health. 2015;105(suppl 3):S409–S423. doi: 10.2105/AJPH.2015.302571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giesinger I, Goldblatt P, Howden-Chapman P, Marmot M, Kuh D, Brunner E. Association of socioeconomic position with smoking and mortality: the contribution of early life circumstances in the 1946 birth cohort. J Epidemiol Community Health. 2014;68(3):275–279. doi: 10.1136/jech-2013-203159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shields AE. Epigenetic signals of how social disadvantage “gets under the skin”: a challenge to the public health community. Epigenomics. 2017;9(3):223–229. doi: 10.2217/epi-2017-0013. [DOI] [PubMed] [Google Scholar]
- 18.Ramaswami R, Bayer R, Galea S. Precision medicine from a public health perspective. Annu Rev Public Health. 2018;39:153–168. doi: 10.1146/annurev-publhealth-040617-014158. [DOI] [PubMed] [Google Scholar]
- 19.Cerdá M, Tracy M, Ahern J, Galea S. Addressing population health and health inequalities: the role of fundamental causes. Am J Public Health. 2014;104(suppl 4):S609–S619. doi: 10.2105/AJPH.2014.302055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hassmiller Lich K, Cornejo DA, Mayorga ME et al. Cost-effectiveness analysis of four simulated colorectal cancer screening interventions, North Carolina. Prev Chronic Dis. 2017;14:E18. doi: 10.5888/pcd14.160158. [DOI] [PMC free article] [PubMed] [Google Scholar]