Abstract
Perineural invasion (PNI) can be found in a variety of malignant tumors. It is a sign of tumor metastasis and invasion and portends the poor prognosis of patients. The pathological description and clinical significance of PNI are clearly understood, but exploration of the underlying molecular mechanism is ongoing. It was previously thought that the low-resistance channel in the anatomic region led to the occurrence of PNI. However, with rapid development of precision medicine and molecular biology, we have gradually realized that the occurrence of PNI is not the result of a single factor. The latest study suggests that PNI of cancer is a continuous and multistep process. A specific peripheral microenvironment, also called the perineural niche, is formed by neural cells, supporting cells, recruited inflammatory cells, altered extracellular matrix, blood vessels, and immune components in the background of carcinoma. Various soluble signaling molecules and their receptors comprise a complex signal network, which achieves the interaction between nerve and tumor. Nerve cells and tumor cells can interact directly or through the opening and closing of the signal transduction pathways and/or the recognition and response of the ligands and receptors. The information is transferred to the targets accurately and effectively, leading to the specific interactions between the nerve cells and the malignant tumor cells. PNI occurs through changes in nerve cells and supporting cells in the background of cancer; change and migration of the perineural matrix; enhancement of the viability, mobility, and invasiveness of the tumor cells; injury and regeneration of nerve cells; interaction, chemotactic movement, contact, and adherence of the nerve cells and the tumor cells; escape from autophagy, apoptosis, and immunological surveillance of tumor cells; and so on. Certainly, exploring the mechanism of PNI clearly has great significance for blocking tumor progression and improving patient survival. The current review aims to elucidate the cellular and molecular mechanisms of PNI, which may help us find a strategy for improving the prognosis of malignant tumors.
Keywords: PNI, cancer, perineural niche, molecular mechanism, autophagy
Introduction
Invasion and metastasis are two of the most characteristic biological behaviors of malignant tumors. In addition to the three typical routes of invasion and metastasis (i.e., partial invasion, blood metastasis, and lymphatic metastasis), in 1985 Batsakis defined perineural invasion (PNI) for the first time: the invasion, surrounding, or passing through nerve of tumor cells. The neurolemma is composed of three layers of connective tissues from the outside to the inside, that is, epineurium, perineurium, and endoneurium. The epineurium is rich in collagen and elastin, surrounding the blood; the perineurium is composed of endothelial cells and basement membrane, which closely bind together have barrier functions of permeability and selectivity; and the endoneurium surrounds single axons and Schwann cells. There are various descriptions of nerve growth patterns in the direction of the tumor, including all surrounding, partial surrounding, concentric lamella structure, tangency contacting, and this makes the definitions of PNI inconsistent. Bockman et al. proposed that only the tumor cells surrounding the nerve by more than 33% can be labeled as PNI. Liebig [1] synthesized the past definitions and presented a definition of PNI consisting of cancer cells in nerves or surrounding or pass-through nerves, tumor cells closely contacting the nerve and surrounding at least 33% of the nerve periphery, or tumor cells invading any of the three layers of the neurolemma structure.
PNI can exist independently when there is no lymph or blood invasion, and it may be the sole metastasis method for some tumors. PNI can occur in several tumors, such as pancreatic ductal adenocarcinoma, gastric carcinoma, colorectal cancer, prostate cancer, head and neck cancer, biliary tract tumor, and cervical cancer. It is an important factor influencing the pathological characteristics and prognosis of malignant tumors, presenting a low survival rate and bad prognosis, and its clinical significance is summarized in Table 1.
Table 1.
Clinical implications of perineural invasion (PNI) in several cancers
| Cancer type | Percentage of patients with PNI | Effect of survival | Other clinical outcomes | Refs |
|---|---|---|---|---|
| Pancreatic ductal adenocarcinoma | 70.0%-100.0% | Independent prognosis factor of overall survival and disease-free survival, indicating the high recurrence rate, progress, and poor prognosis of tumor. | Closely related to the occurrence of ache. | [2-6] |
| An important danger factor for independent survival in addition to AJCC-TNM tumor staging. PNI can be included in patient stratification factors to direct different diagnosis schemes. | ||||
| Gastric carcinoma | 6.8%-75.6% | Independent prognosis factor of overall survival and disease-free survival, and patients with PNI have a poor prognosis. It is also a reference index for postoperative adjuvant treatment. | The 5-year survival of patients with PNI passing through the subserosa tissue or serosa is 50%, obviously lower than 64% of patients with PNI restricted to submucosa or nerves at the muscularis propria. | [7-10] |
| Biliary tract tumor | 56.0%-88.0% | PNI is an independent prognostic factor of overall survival of biliary tract cancer. The 5-year overall survival of patients with PNI is 28%, whereas that of patients without PNI is 74%. | Radical treatment is difficult, the 5-year survival is low, and tumor is likely to relapse. | [11-14] |
| In gall bladder cancer, PNI is related to the high staging and low overall survival. | ||||
| Prostate cancer | 12.4%-83.6% | A meta-analysis involving 13,412 patients showed that the occurrence of PNI is related to the increase in biochemistry recurrence of prostate cancer after radical operation or radiotherapy (rise of specific antigen of prostate) and is the biological prediction factor of poor prognosis. | Related to the partial or general progress of the tumor, being an independent prognosis influence factor. | [15-17] |
| PNI positive can reduce survival, but the classification of PNI degree by percentages has more precise predictive value than a simple positive or negative dichotomy. | ||||
| Head and neck cancer | 5.2%-90.0% | Poor prognosis factor of oropharynx squamous cell carcinoma tongue; occurrence of PNI indicates the decrease in overall survival and disease-free survival and increase in distant recurrence rate. | Strong predictive factor of lymphatic metastasis. | [18-21] |
| Malignant tumor of parotid gland indicates later TNM staging, high-risk pathology. | Causes facial paralysis and ache. | |||
| Low survival of laryngeal cancer patients after surgical treatment. | ||||
| Colorectal cancer | 15.7%-38.9% | Predictive factor of death rate increase within 1 year, and patients with PNI have high a postoperative recurrence rate and low survival rate, indicating poor prognosis. | Independent risk factor of recurrence, indicating worse phenotype of tumor. | [22-25] |
| The 5-year overall survival and disease-related survival decrease obviously. | PNI state shall be considered in pathological classification of colorectal cancer. | |||
| Cervical cancer | 8.6%-31.3% | Patients with PNI have short disease-free survival and overall survival, and PNI is a poor prognosis factor of cervical cancer. | More likely to have adverse histopathological characteristics, e.g., increase of tumor, increase in depth of stromal invasion, lymph node invasion, lymphatic vessel invasion, and lymphatic metastasis. It can guide the operation and the postoperative adjuvant treatment. | [26-28] |
| PNI is an independent prognostic factor of cervical cancer and indicates poor prognosis in early or terminal cervical cancer. |
Because of technical restrictions, the initial explanations of PNI are focused on the direct observation of the microstructure, and it is thought that the adjacency of the tumor to neuroanatomy is an important factor for PNI. Thus, the hypothesis of the “low-resistance channel” is presented, based on the idea that the tumor spreads to the nerve sheath along the lymphatic system and is likely to invade the perineural space, which is a kind of cracklike, low-resistance, and cell-free space between the nerve tract and the surrounding connective tissues. However, upon further study, researchers have gradually recognized that the occurrence of PNI is not the result of a single factor, and its formation is a continuous multistep process with several contributing factors. The pathological description and clinical significance of PNI are understood clearly, but exploration of the underlying molecular mechanism is ongoing. This paper summarizes the latest studies of molecular mechanisms of PNI to help us gain an in-depth understanding of the PNI of cancer and determine some corresponding precise therapeutic targets.
The concept of tumor-neural connect and perineural niche
Scuteri A et al. [29] presented the concept of tumor-neural connect (TNC) to comprehensively investigate the interactive relationship and molecular network between tumor and nerves. This is similar to the concept of the perineural niche presented by some scholars. We consider that the nerves, surrounding supporting cells, recruited inflammatory cells, altered extracellular matrix, blood vessels, and immune components form a specific peripheral microenvironment in the tumor background, and various soluble signal molecules and their receptors (see below) constitute a complex signal network in which the nerves and tumor interact. Jeffus SK et al. [30] studied 143 cases of squamous cell carcinoma with vulva invasion, defined as a “fiber bonding matric reaction”, with immature collagen and fibroblast forming the extracellular matrix, isolating and surrounding the tumor cells, and found that tumors with these changes are more likely to result in PNI and cause poor prognosis, indicating the effect of the interaction among nerves, tumors, and supporting cells on the progress and recurrence of such tumors. Hypoxia, high glucose levels, inflammatory reaction, and sympathetic system activation also constitute the specific microenvironment background of PNI [31]. Low oxygen in a solid tumor may promote the expression of hypoxia inducible factor-1α (HIF-1α) by activating the hypoxia-responsive element in the promoter of the target gene, thus upregulating vascular endothelial growth factor (VEGF) and stem cell factor by inducing CXCL12, CXCR4, and CX3CR1 expression and accelerating the neogenesis of tumor blood vessel; upregulating glucoamylase GLU1 (GLU-1) to increase the transfer of glucose and induce the expression of glycolytic enzyme; and upregulating human telomerase reverse transcriptase (hTERT) and survivin to promote cell proliferation and resist apoptosis, thus promoting the occurrence of PNI. In pancreatic ductal adenocarcinoma (PDAC), a tumor microenvironment with high glucose levels can promote the high expression of nerve growth factor (NGF) and its receptor and synergistically promote the occurrence of PNI [32]. Nigri J [33] et al. confirmed through an in vivo experiment that acinous cells in the tumor microenvironment of PDAC generate pancreatitis-related albumen PAP and ReG3A, and the activation of janus kinase (JAK)/signal transducer and activator of transcription (STAT) signal pathway makes for the occurrence of PNI and indicates poor prognosis. In patients with prostate cancer whose aspiration biopsy is positive, acute and chronic prostatitis are related to the low morbidity of PNI. This shows that the inflammation and immunoregulation alleviate the PNI of patients with prostate cancer through certain mechanisms [34]. Armaiz-Pena GN discovered that with tumor occurrence, the norepinephrine level in the tumor microenvironment increases because of the chronic activation of the sympathetic nervous system, and such activation can initiate the upregulation of the downstream tumor chemotactic promoter through the β-adrenergic receptor signal transduction pathway to promote tumor growth and progression [35]. All of these studies found that a certain microenvironment plays an important role in the progress of tumor PNI. The presentation of the TNC and the perineural niche concept helps to consider various factors taking part in PNI progress, and this builds foundation for further study on the changes of cells and molecules.
PNI is a continuous and multistep process
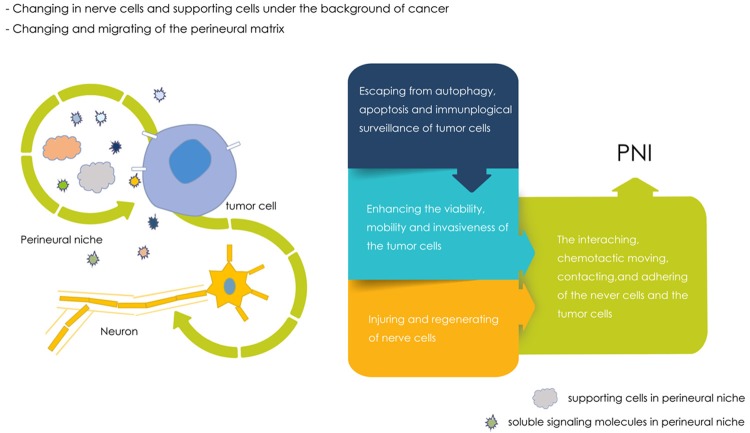
The PNI of tumor is a continuous multistep process [36]. In the perineural niche, the nerves and tumor cells are able to make the information accurately and effectively interact on the target site through direct contact between cells or through the opening and closing of the signal transduction pathway, as well as initiate the recognition and response of the ligand and receptor. They then produce a specific interaction between nerves and the malignant tumor cell. The study by Moran Amit [31] demonstrated that PNI goes through seven steps: survival of tumor cells, formation of a neural steady state, inflammatory reaction, recruiting of tumor cells to nerves, neogenesis of nerves, adhesion of tumor cells and neurolemma, and nerve invasion. We believe that PNI finally occurs after proceeding through the following important steps: changes in nerve cells and supporting cells under the tumor background; changes and metastasis of the perineural matrix; enhancement of the viability, mobility, and invasion of tumor cells; injury and regeneration of nerves; interaction, chemotactic movement, contact, and adhesion of nerve cells and tumor cells; and escape, autophagy, apoptosis, and immunological surveillance of tumor cells (the pattern is shown in Figure 1). However, these steps do not happen simply in sequence; rather, it is an interactional, complex closed-loop system, and they cannot be separated mechanically nor can their interaction be neglected. From this, it can be seen that changing the microenvironment and blocking the associated molecular pathway undoubtedly play important roles in terminating the occurrence of PNI and further improving tumor prognosis. The following discusses the changes in cells and molecules in PNI, respectively.
Figure 1.
Main Steps in PNI.
Cells in PNI
Schwann cells
Schwann cells are also called neurogliocytes and are given attention during the process of PNI, as they promote the survival of damaged nerve cells and the regeneration of axons. Research shows that Schwann cells can migrate inwards to the tumor before the occurrence of PNI, which indicates that the tumor microenvironment and Schwann cells play a role during the PNI initiation process [37]. In an in vitro experiment, Deborde [38] discovered that Schwann cells of glial fibrillary acidic protein (+) can destroy the connection among tumor cell lines. This causes the spherically shaped cancer cell line to morph into a chain structure and highly express neural cell adhesion molecule 1 (NCAM1) at the cell contact to promote tumor cells to form a projection and migrate toward the Schwann cells. Subsequently, Schwann cells further insert and destroy the connection among tumor cells, enhance the invasive power of the tumor, and assist the tumor cells in spreading from the cancer cell group to invade toward the nerves. Schwann cells can also regulate the growth, survival, and repair of nerve cells, and after being activated and dedifferentiated in the tumor environment, they become a subtype more likely to migrate, promote the remodeling of matric components by means of direct contact and secretion of soluble signal molecules, and promote the targeting of newborn nerves by means of inducing the extension of axons [39]. After cultivating salivary adenoid cystic carcinoma (SACC) cells and Schwann cells together in vitro, Shan found that Schwann cells can induce SACC cells through the brain-derived nerve growth factor (BDNF)/tropomyosin receptor kinase B (TrkB) axle to change into a mesenchymal form, which is associated with greater metastasis and invasion, and promote the process of epithelial-mesenchymal transition (EMT) [40,41]. After cultivating pancreatic cancer cells and Schwann cells together in vitro, Yoko Fuji-Nishimura detected relevant expressions of mesenchymal-epithelial transition (MET) markers and discovered that in the area with PNI, the interaction of Schwann cells and tumor cells increased the membrane expression of E-cadherin and reduced the expression of SMAD3 and vimentin. Downregulated SMAD3 is a key substance in the activation of the transforming growth factor-β (TGF-β) signal pathway, while MET is the secondary process of colonization after EMT occurs and tumor cells migrate to the distance, which indicates that Schwann cells play an important role during the tumor MET process [42].
Macrophages
Endoneurial macrophages are a macrophage subgroup that maintain the steady state and regeneration of nerves after nerve injuries. It has been verified that macrophage colony-stimulating factor 1, secreted by pancreatic cancer cells, can cause chemotaxis of endoneurial macrophages, and the generated glial cell line-derived neurotrophic factor (GDNF) has a role in promoting PNI [43]. The tumor microenvironment in PDAC is characterized by a dense tumor matrix and vast tumor-associated macrophages (TAMs). TAMs can secrete proinflammatory factors (such as interleukin-8 [IL-8]) to activate PDAC cells and promote PNI through the matrix metalloproteinase 1 (MMP-1)-protease-activated receptors 1-extracellular signal-regulated kinases1/2 (ERK1/2) pathway.
Stellate cells and fibroblast
In pancreatic cancer, tumor cells in the microenvironment are surrounded by pancreatic stellate cells and fibroblasts. Sonic Hedgehog (SHH) of pancreatic tumor cells can activate pancreatic stellate cells in the adjacent cell matrix and then start the transcription of downstream genes to promote tumor progression. SHH can also induce the rise in expression levels of MMP-2, MMP-9, and NGF and promote PNI through different pathways. SHH protein from tumor plays a vicious role in reducing patient survival and promoting the invasion and drug resistance of tumor cells [44]. Fibroblasts can synthesize specific growth factors and chemotactic factors, which indirectly causes cancer invasion. Perineurium originates from fibroblasts, and as a result, the change in fibroblasts in the tumor microenvironment can lead to changes in the permeability of perineurium and protection from injury, which directly affects the occurrence of PNI.
Molecules in PNI
Molecules leading tumor and neuron cell changes
Neurotrophin factors
Neurotrophin factors are a kind of protein molecule necessary for the growth and survival of nerve cells. They are generated by nerve-governed tissues and astrocytes or tumor cells (e.g., NGF, BDNF, neurotrophic factor-3 [NT-3] and neurotrophic factor-4/5 [NT-4/5], insulin-like growth factor, ciliary neurotrophic factor, GDNF, etc.), and they are important substance molecules that regulate and control the signal pathway generated by the tumor nerve. By integrating with high-affinity Trk receptors and low-affinity p75 neurotrophin receptor (p75NTR), NGF is highly expressed in several types of tumor cells and in the nerve sheath, takes part in important processes of survival and differentiation of nerve cells as well as the formation of axons, and plays an important role in PNI [45-47]. In pancreatic cancer, NGF activates and inhibits the effects on pancreatic cancer cells, and these actions depend on the expression level of NGF and the specific value of TrkA and p75NTR. The overexpression of NGF can strengthen a TrkA combined signal and reduce the apoptosis of pancreatic cancer cells, activate the p44/42-mitogen-activated protein kinase (MAPK) signal pathway, and increase MMP-2 or cause PNI of pancreatic cancer cells by inducing the proliferation of PNI nerves [32]. In an in vitro experiment, AA Bapat verified that the NGF-TrkA pathway can promote the survival of cancer cells and assist them in migrating to the dorsal root ganglia, where they inhibit the pathway through small interfering RNA, neutralizing antibodies, or downregulating p75NTR, all of which can reduce the occurrence of PNI [48]. BDNF and its high-affinity receptors TrkB, NT-3, and receptor TrkC have expressions in several types of tumor cells and promote the invasion, proliferation, and progress of tumor by activating tumor cells to produce MMP-2, thus causing poor prognosis. Blocking NT3 inhibited the growth and progress of prostatic and pancreatic cancer in a mouse heterograft model [49-52]. The GDNF family includes four proteins: GDNF, neurturin (NTN), artemin (ART), and persephin (PSP), and each type corresponds to one special GDNF receptor-α (GFRα). GDNF is related to several signal pathways of growth and differentiation, growth of nerve axons, and the survival of cells. Iwahashi et al. verified that GDNF and its receptors GFRα1/RET have high expression in several tumors. They also found that the generated PNI effect showed a dosage association with GDNF, and blocking GFR can reduce the occurrence of PNI [53,54]. GDNF secreted by nerves and supporting cells (including macrophages) binds with soluble GFRα1 secreted by nerves to produce the GDNF-GFRα1 compound. This compound binds with RET of cancer cell expression and initiates the signal transduction pathway to activate the downstream MAPK pathway to control the direction of tumor cell metastasis, induce the massive excitation of MMPs (e.g., MMP-9), significantly enhance the invasion of cells, and promote the formation of axons, so as to facilitate the interactive invasion and growth of cancer cells and nerves [36,43,55,56]. GNDF can also induce the expression of programmed death-ligand 1 (PD-L1) by the JAK2-STAT1 signal pathway, and PD-L1 thus plays a key role in immunosuppression by binding with its receptors, thus inducing the immunologic inadequacy of cells and the escape of tumor cells on immunological surveillance [36]. Other studies have found that the expressions of artemin and its receptor GFRα3 increase in the pancreatic cancer cell line, which is related to the generation of PNI [52].
TGF
Tumor cells can produce a kind of polypeptide growth factor, which can stimulate cells that are growing in static mode to grow in a nonstatic mode. This factor is called TGF and includes TGF-α and TGF-β. Pancreatic cancer tissues highly express TGF-α, and the binding of TGF-α and its receptor, epidermal growth factor receptor (EGFR), can activate a series of signal transduction pathways to induce the proliferation of pancreatic cancer cells. After contacting the nerve cells, the proliferated tumor cells promote nerve tissues to highly express TGF-α. This vicious circle causes PNI of pancreatic cancer. TGF-β1 can improve the activity of nerve cells in vitro, promote the proliferation of Schwann cells, secrete plenty of collagen IV, and induce the formation of axons and myelin, thus facilitating PNI.
Molecules that promote tumor cell metastasis
Midkine
Midkine (MK) is a newly discovered heparin binding growth factor family, composed of pleiotrophin (PTN) and medkine (MDK). PTN is overexpressed in several human cancers and promotes the generation and expansion of blood vessel as well as the growth and transfer of tumor cells. N-syndecan is a high-affinity receptor of PTN and is also an important component for the growth of nerve axons. Its high expression indicates the occurrence and poor prognosis of PNI [57,58]. In pancreatic cancer, cancer cells expressing PTN penetrate and invade the pancreatic nerve tract, injure nerve cells, damage the steady state of nerves, and cause nerve cells and Schwann cells to release N-syndecan. The high-affinity function of PTN and N-syndecan can attract PTN-positive cancer cells to reach the damaged nerve. The increased PTN/N-syndecan expression level again injures nerves, thus forming a vicious circle of PNI [59]. Syndecan-3 is a high-affinity receptor of MDK, and studies confirm that the MDK/syndecan-3 pathway plays an important role in nerve invasion of tumors. Meanwhile, MDK can be used as a biological marker, and its high expression indicates the occurrence of PNI, advanced tumor, lymphatic metastasis, and poor prognosis [58].
MMP
The MMP family is a type of endopeptidase family with extracellular matrix degradation and tissue remodeling function, and it has 26 members so far. According to different structures and functioned matrix, MMPs can be divided into collagenases, gelatinases, MMP, membrane-type metalloprotein, and matrix degradation enzyme. To date, studies have mostly focused on MMP-2, MMP-3, MMP-5, MMP-7, and MMP-9. In recent years, studies have found that the promoter region of the MMP gene has polymorphic sites, which can affect gene expression and thus the tumor susceptibility. The MMP family has upregulated expression in most malignant tumors of breast cancer, esophageal cancer, colorectal cancer, gastric cancer, lung cancer, liver cancer, oral squamous cell carcinoma, prostatic cancer, pancreatic cancer, cholangiocarcinoma, head and neck neoplasms, and malignant lymphoma, and it is closely related to the occurrence of PNI, tumor progression, and poor prognosis [60-62]. In colorectal cancer, β6 integrin can induce the phosphorylation of ETS1 through the ERK/MAPK signal pathway and induce the expression of MMP-3 and MMP-9 [63]. Chen Q et al. [64] found that in liver cancer, microRNA29a negatively controls the expression of ten-eleven translocation family members to deactivate the ectogenic suppressor of cytokine signaling 1 and then trigger the STAT3 signal pathway, resulting in upregulation of MMP-9 expression. Xu L et al. [65] found that the nuclear Drosha upregulates the expression of phosphorylated EGFR, ERK1/2, and MMP-7 through the EGFR/ERK1/2-MMP-7 signal pathway to promote the proliferation of cells and take part in PNI progression of gastric cancer. The mechanism of high-expression MMP promoting PNI is summarized [66-74] as follows: 1) Degrade the extracellular matrix and reduce the conglutination of tumor cells to enhance the invasion of tumor cells and provide conditions for the spreading of tumor cells. 2) Promote the proliferation activity of tumor cells and inhibit their apoptosis. 3) Degrade associated cell factors, e.g., integrin β4, pro-TGFβ, pro-IL1b, pro-TNFα, and other MMP propeptides, to activate some cell factors for EMT. 4) Activate other cell factors that promote tumor cell metastasis, e.g., insulin-like growth factor binding protein, growth factor receptors, and other associated cell factors. 5) Promote vascular remodeling and the chemotaxis of new vessels to tumor tissues.
Molecules guiding chemotactic movement of tumors and neuron cells
Axon guidance factors
Axon guidance factors exist widely in the microenvironment of nerves and mainly include the Netrins family, Ephrins family, Semaphorins family, and Slit family, as they have both promotion and inhibition effects on nerve guidance. Nerve guidance is the synthesized complex result of factors having attraction and rejection functions. The Eph/ephrin signal pathway takes part in the neogenesis of tumor vessels in several tumors. Among Eph receptor members, EphA2 has the most powerful contact with cancer progression, and its expression is closely related to the occurrence of PNI. Studies by Ding Y found that the expression of semaphorin 4F in human prostatic cancer is related to PNI, and the in vitro experiment verifies that the overexpression of semaphorin 4F in prostatic cancer can be induced through NF-κB and then promote the growth and invasion of tumor cells [75]. Sema3C is highly expressed in gastric cancer and breast cancer and promotes the development of tumor through vessels in the tumor. As a kind of common signal transduction system, Sema4D and its high-affinity receptor plexin-B1 take part in the regulation of motion and adhesion of different cells. Studies show that Sema4D/plexin-B1 are highly expressed in tumor cells and nerves, respectively, and mutually attract and affect each other by means of Rho/Rho kinase dependency. They subsequently promote PNI of head and neck squamous cell carcinoma, breast cancer, prostatic cancer, and colon cancer [76]. Slit molecule is a factor that plays a guidance role in the growth of axons and the metastasis of nerve cells. Slit2, secreted by tumor cells, can attract vascular endothelial cells to migrate in the direction of the tumor, induce the neogenesis of tumor vessels, and provide necessary nutrition for tumor growth. In pancreatic cancer, the recovery of the Slit2 signal is effective for inhibiting the pancreatic cancer to move toward the known chemotactic factor, indicating that the occurrence of PNI not only has one-way chemical chemotaxis but also the comprehensive effect of deactivation of partial pathways [77].
Chemokines
Chemokines are a type of protein family that forms a concentration gradient and then regulates cell migration. They can be divided into four subfamilies of CC, CXC, XC, and CX3C, which in total include more than 50 types. The interaction of chemokines and their receptors can induce several effects, and chemokines may be one of the core mechanisms controlling PNI. Table 2 summarizes the most recent research.
Table 2.
Major PNI-Related Chemokine Proteins and Mechanisms of PNI
| Chemokines | Receptor | Mechanisms in PNI | Refs |
|---|---|---|---|
| CCL2 (MCP-1) | CCR2 | Inflammatory mononuclear cells of CCR2(+) are recruited to the area of the PNI by CCL2 released by Schwann cells. They are differentiated from macrophages and promote the occurrence of PNI through the process of Akt induction. | [78,79] |
| The CCL2-CCR2 pathway activates P42/MAPK through G-protein-coupled receptors to regulate the adhesion and movement of macrophages. | |||
| In the in vitro experiment of mouse dorsal root ganglion (DRG) in prostatic cancer, nerves injured by tumor invasion promote the release of CCL2, generate an inflammatory reaction of nerve restoration, and induce CCR2 cancer cells to migrate to these nerves. By activating the MAPK and Akt pathways in pc3 cells, they promote the occurrence of PNI. | |||
| CCL5 | CCR5 | In salivary adenoid cystic carcinoma (SACC), the CCL5-CCR5 axis stimulates SACC cells after being activated and causes the Ca2+ concentration of the sarcoplasmic reticulum to rise, resulting in high-level actin polymerization and recombination of the cytoskeleton, forming a pseudopod to enhance the invasion capability of tumor cells, which plays a key role in PNI. | [80] |
| CCL21 | CCR7 | CCL21-CCR7 promotes the proliferation and migration of CD133+ pancreatic cancer cells by regulating EMT and ERK/NF-κB. | [81] |
| CXCL5 | CXCR2 | The CXCL5-CXCR2 pathway can activate and promote the migration of hepatocellular carcinoma EMT and tumor through PI3K/Akt/GSK-3β/Snail signal transduction. | [82] |
| CXCL12 (SDF-1) | CXCR4 | Overexpressed CXCR4 in bile duct carcinoma and pancreatic cancer is closely related to PNI, lymphatic metastasis, TNM staging, and vessel invasion. | [83-86] |
| CXCR4 promotes VEGF expression, the mitosis and proliferation of vascular endothelial cells, and tumor to generate new vessels. It also promotes the specific growth tendency of axons and increases nerve-tumor contact. | |||
| The CXCL12-CXCR4 axis can upregulate MAPK, Rho family protein CDC42, PAK, and Akt through arrestin; promote the synthesis of intracellular golgiosome microtubules and microfilament; increase their contractility and contraction frequency to promote EMT; enhance the transformation and moving ability of tumor cells; and increase the migration ability and invasion of tumor cells. | |||
| Enhance the anti-apoptosis of tumor cells through the Akt/Bcl-2/NF-κB pathway and by reducing the expression level of caspase, downregulate the MHC-I level to induce tumor cells to escape from the immune surveillance of mechanism. | |||
| As chemotherapeutics, the retardant AMD3100 (Mozobil, plerixafor) of the CXCL12/CXCR4 axis and CTCE-9908 have achieved antitumor effects in solid tumors, but they need to be further researched. | |||
| CXCL12 (SDF-1) | CXCR7 | Studies of Dona E demonstrate that besides CXCR4, CXCR7 can be used as the second receptor of CXCL12. By chelating with CXCL12, the CXCR7 ligand can regulate and change the overall availability, distribution, and concentration gradient of CXCL12 in the tumor microenvironment and the synergism of CXCR4 to cause PNI. | [87] |
| CX3CL1 (Fractalkine) | CX3CR1 | CX3CR1 and CX3CL1 constitute a high-affinity signal pathway and can be highly expressed in early pancreatic cancer and prostatic cancer. CX3CR1 activates and induces the adhesion molecule through G-protein dependency and β1 integrin, to take part in the adhesion of nerve cells and induction of the tendency for nerve growth of tumor cells. | [88] |
Molecules promoting cell adhesion
Adhesion molecules and cadherin
Cell adhesion molecules are a group of transmembrane proteins that play a role in inducing cell-cell adhesion as well as adhesion between the cell and extracellular matrix by means of receptor and ligand binding. In the occurrence of PNI, the cell adhesion molecules interact with Schwann cells and produce various effects. Followings are several types of adhesion molecules closely related to PNI.
NCAMs play an important role in cell adhesion, nerve growth, tumor invasion, and tumor growth. Studies have confirmed that NCAM is expressed in tumor and nerves in PNI. NCAM may undergo transmembrane changes under the action of polysialic acid and then influence the adhesion ability of E-cadherin; they also promote induction of cancer cells by Schwann cells to spread and invade and play an important role in the occurrence of PNI [38]. Mucin 1 (MUC1) is a kind of transmembrane mucoprotein that affects cell adhesion, and in pancreatic cancer patients with PNI, MUC1 interacts with myelin-associated glycoprotein expressed by oligodendroglia cells and Schwann cells. Tumor cells with overexpressed MUC1 have an adhesion advantage and can improve the survival ability in nerves. The expression of MUC1 can downregulate the expression of E-cadherin, which reduces its inhibition function in tumor metastasis and is one of the steps in the enhancement of tumor cell invasion [58]. Cadherin is a transmembrane single-chain glycoprotein and is an important factor affecting the metastasis of various epithelium-derived malignant tumors of lung cancer, colorectal cancer, gastric cancer, breast cancer, and bile duct cancer and causes poor prognosis in patients with tumors. The cadherin family has three members (E-cadherin, N-cadherin, and P-cadherin), of which E-cadherin is widely distributed on the surface of epithelial cells and plays an important role in promoting mutual adhesion among cells, maintaining the integrity of the cell skeleton, and maintaining the polarity arrangement of epithelial cells. Low expression, deficiency, or excitation of the E-cadherin gene may cause decreased adhesion and a disordered polarity arrangement of epithelial cells. This can lead to exposure of endothelial cells, changes in EMT, and finally tumor occurrence. After losing the polarity arrangement, the epithelial cells will promote tumor cells to break through the extracellular matrix, leading to partial invasion and metastasis of the tumor. Other studies have confirmed that as a kind of transmembrane protein, the expression of the L1 cell adhesion molecule is related to tumor progress and metastasis of various cancers, and it promotes the occurrence of PNI by influencing the migration of nerve cells [89].
In addition to the above factors, recent studies have also found other signal molecules to be highly expressed in PNI-associated tumor progression. These molecules may coordinate with the above-described typical signal molecules to enhance the invasion of tumor cells or indirectly regulate the development of PNI through multiple signal pathways, but their specific mechanism still requires further research. These other molecules are summarized in Table 3.
Table 3.
Other molecules related to PNI
| Molecules | Mechanism of PNI | Other clinical features | Refs |
|---|---|---|---|
| SP (Substance P) | Activate MAPK and ERK1/2 to promote the differentiation of cells and induce the migration of cells after being bound with the receptor NK-1R and its subtypes. Accelerate the secretion of MMP-2 and the formation of new vessels and then promote the occurrence of PNI. | Substance P and its receptor NK-1R are highly expressed in several tumors and are related to the pains caused by cancer. | [90] |
| NK1 receptor antagonist can block the mitogenic function of substance P and produce apoptosis-promoting function in vitro and in vivo. | |||
| Galanin | Activate NFAT (nuclear factor of activated T cells) after being bound with GAL-R2 and promote the transcription of cyclooxygenase-2 (COX-2) and GAL in tumor cells under the induction of calcineurin dephosphorylation. COX-2 promotes the generation of prostaglandin E2 (PGE2) and promotes the invasion of tumor. | To be released after nerve cells are injured or have inflammation, having three receptors of GAL-R1, GAL-R2, and GAL-R3. | [91,92] |
| The newly transcribed GAL can induce neurogenesis and promote PNI. When this indicates PNI, there is not only invasion of tumor to nerves but also neurogenesis in tumor tissues. | |||
| Slug | Upregulate MMP-inducing factors and downregulate E-cadherin to promote the EMT process of tumor cells. | Slug belongs to important members of the zinc finger transcription factor family, and its expression level in tumor tissues with PNI is obviously higher than that in normal tissues. | [93,94] |
| Promote PNI and distant metastasis of tumor cells through the MAPK signal pathway, and such processes can be blocked by the targeted inhibitor MicroRNA-181a of the MAPK pathway. | |||
| NPY (Neuropeptide Y) | Synthesized and released in tumor cells and sympathetic nervous system nerves. NPY has a function of promoting growth and can be changed due to receptors of tumor-specific expression. | NPY and its receptors are expressed in cells and vessels of various tumors and play a complex role. | [95] |
| As an angiogenesis factor, NPY can powerfully induce the proliferation, differentiation, and migration of endothelial cells; promote the generation of vessels; and then promote the growth of tumor in the PNI process. | |||
| Survivin | Survivin is a type of anti-apoptosis factor that has recently been gradually recognized. It can directly block the apoptosis of cells by blocking the apoptosis of receptors and inhibiting the activity of mitochondria, and studies show that it takes part in the anti-apoptosis function in PNI. | When pancreatic cancer is accompanied by PNI, there is always high expression of survivin. | [33] |
Interaction of nerve and tumor
Previously, people thought of PNI as a one-way process of tumor cell invasion into nerves, that is, with the nerves in a passive position. However, studies on tumor neurogenesis have overturned this view. Seifert et al. was the first to find nerves in the epithelial cell adenoma on an eyelash-like body and later discovered tumor neurogenesis successively in breast cancer, bladder cancer, pancreatic cancer, and colorectal cancer. An increasing amount of evidence has shown that the process of tumor neurogenesis is another key driving force of cancer progression [96]. Current studies postulate that the occurrence and development of PNI are the interactive processes of nerves and tumor, and the nerve cells in the tumor background can enhance the contact and adhesion with the tumor cells through the growth and lengthening of the axon and the thickening of the nerve fiber, so as to promote neurogenesis. In malignant tumors with PNI features, tumor cells, by their interaction with nerves, can promote cell factors (especially neurotrophic factors and axon-induction factors) that regulate nerve growth. This growth induces the upregulation of nerve survival-related protein expression, increases neurite quantity and the lengthening of the axon, increases the density of nerve tissues, and finally leads to new nerves in the tumor. However, new nerves can induce the immune escape and survival advantage of tumor cells in special steady state with nerve regeneration after nerve injury by changing the invasion of tumor cells [92]. On the other hand, innervation has a significant effect on the occurrence of cancer. Yates C observed the histological changes and genetic expression mode of mouse prostatic epithelial cells that were undergoing innervation loss and found that the methods of regulating cellular energy metabolism (e.g., mitochondrial pathway, mitochondrial adenosine triphosphate [ATP] synthesizing coupling proton transport, mitochondrial proton transporting ATP synthase complex, glycolysis, and electron transfer chain) were downregulated. Denervation can reduce the tumor occurrence rate or the volume of the tumor and cause reduced tumor cytoplasm and karyopyknosis, finally leading to cell apoptosis. This confirms that nerves provide the microenvironment that promotes tumor occurrence. The interaction between nerves and tumor cells is a key factor in the survival and invasion of tumor cells. From this, it is speculated that cancer and tumor development may be fundamentally affected by the integral nerve [97]. Magnon C clearly verified that nerve cells take part in the promotion of cancer progression, and the formation of autonomic nerves has important significance in the regulation of the growth and metastasis of mouse prostatic cancer [85]. Zhao CM also verified that in a mouse gastric cancer model, stomach denervation can reduce the occurrence rate and growth of tumor while improving the resistance reaction of chemotherapy. On the other hand, the downregulation of muscarinic acetylcholine receptor M3 inhibits the occurrence of tumor [98]. Fromont et al. confirmed that nerve-surrounded tumor cells of PNI in prostatic cancer have a greater active proliferation ability than tumor cells that are not near the nerves. In addition, the expression levels of proliferating cell nuclear antigen (ki-67) and CD74 are obviously higher than cancer cells without PNI, and this indicates that nerves not only promote tumor metastasis but also influence the proliferation of tumor cells by means of paracrine, which makes the tumor more likely to relapse [99]. These findings show that the nerves actively take part in tumor progression, and studies show that they can promote the proliferation and invasion of tumor through neurotransmitter signaling pathways and receptor induction and play an important role in the occurrence of PNI.
Neurotransmitter and PNI
Neurotransmitter released by peripheral nerves can directly enter the microenvironment of the tumor. They can activate corresponding receptors and then regulate the occurrence and progression of the tumor. This may well explain the long-lasting influence of psychological factors on cancer and the relationship between the nerves and emotion and the occurrence of cancer. The adrenergic fibers of the sympathetic nervous system have a role in the initial stage of tumor progression, while the cholinergic fibers of the parasympathetic nervous system with tumor invasion are the basis of tumor cell invasion and metastasis invasion [98]. Epinephrine and noradrenaline can control several mechanisms related to tumor development, increase the secretion of VEGF and IL-6 by activating the β-adrenergic receptor-cyclic adenosine monophosphate-protein kinase A pathway, and promote vessel generation, tumor proliferation, VEGF, and IL-6 [100]. Dopamine or dopamine receptor agonists can inhibit the phosphorylation of VEGF receptor 2 and block the activation of MAPK, so as to inhibit the generation of vessels. On the other hand, dopamine can inhibit the mobilization of bone marrow endothelial progenitor cells, thus inhibiting tumor development and metastasis. Overexpression of γ-aminobutyric acid (GABA) or its receptor agonists can produce different effects due to the difference in cancer types or in GABA receptors. For example, in rat, it can reduce the occurrence rate of gastric cancer, inhibit the metastasis of mouse colon cancer cells, and inhibit the growth of liver cancer cells in vitro and in vivo but promote the growth and metastasis of cancer cells in prostatic cancer. Muscarinic acetylcholine receptor, in the acetylcholine receptor family, can induce the growth of colon cancer by transactivation of the EGFR/ERK pathway [101]. The activation of nicotinic acetylcholine receptors (N-AchRs) induces the growth of mesothelioma and colon cancer cells. N-AChRs induce the generation of vessels through PG-E2 activation and cyclooxygenase-2 as well as an increase in VEGF induced by nicotine [102]. Recent studies have demonstrated that the nerve cell protein families neurexins and neuroligins can produce multiple effects, including vasotonia and morphogenesis, by affecting various forms of intercellular communications [103,104]. One subtype of neuroligin, NLGN1, affects the glutamic acid reaction by regulating ionotropic glutamate receptors expressed on neurons surfaces and cancer cells, and another subtype of neuroligin, NLGN2, can take effect by controlling the release of catecholamine from peripheral nerves [102].
Autophagy and PNI
Autophagy of cells is a steady-state mechanism that buffers metabolic stress by degrading the aggregated protein or cell organelle. By recycling intracellular components, autophagy can complete the cell organelle update. The autophagy process plays a large role in physiological and pathological processes, but its significance in tumors is not yet clear, which has made the study of autophagy and PNI a hot new field. Studies by Fuji S et al. found that typical markers of autophagy (e.g., microtubule-associated protein 1A/1B-light chain 3 [LC3]) have a high expression in cancer cells around PNI. A high autophagy level may assist cancer cells in escaping from stress-induced apoptosis in the PNI environment and promote the survival of tumor cells, tumor invasion, and tumor metastasis. It is also an independent risk factor for occurrence and poor prognosis of PNI [5,42]. Studies on cutaneous squamous cell carcinoma found that the expression of autophagy-related genes has a close correlation with the occurrence of tumor, and autophagy-related high-pression Beclin1 and LC3 as well as low-level p62/sequestosome-1 play key roles in controlling the occurrence and progression of cutaneous squamous cell carcinoma as well as lymphatic metastasis. However, the expressions of Notch, Integrin, tumor protein p53, and EGFR are related to the occurrence of PNI, and autophagy-related genes are expected to become the therapeutic targets of skin cancer [105-107]. The clinical PNI of head and neck cancer may be related to autophagy-related genes of HIF1A, MAPK8, mTOR, BCL2L1, and Rab23. Gene analysis results showed that the change in the p53 gene pathway plays an important role in PNI of head and neck cancer and is a potential therapeutic target, whereas the signal pathways of tumor necrosis factor induction and the functional defect of autophagy are important factors of tumor progress and invasion [18]. The relationship between autophagy and PNI requires further study. Research on the relationship between autophagy and tumors has important significance and is expected to become a new specificity target.
lncRNA, miRNA, and PNI
Long noncoding RNA (lncRNA) is noncoding RNA with a length of more than 200 nucleotides, whereas microRNA (miRNA) is a kind of small RNA with the length of about 20 to 24 nucleotides. Both have important regulation function in cells, involving multiple important steps of cell cycle control and differentiation as well as the occurrence of tumor, and they are hot topics of current studies. Studies by Wei W [108] showed that lncRNA-X-inactive specific transcript (XIST) has high expression in pancreatic carcinoma tissues and is negatively correlated with the expression of miR-133a. XIST may promote the proliferation of pancreatic carcinoma cells by upregulating the expression of EGFR and is related to the occurrence and poor prognosis of PNI. Tan [109] observed that lncRNA-metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) has abnormal expression in multiple tumor issues and takes part in the occurrence and progression of several tumors. He also verified that lncRNA-MALAT1 is specifically upregulated in hilar cholangiocarcinoma tissues and cell lines and is related to the volume increase, metastasis, and invasion of tumor as well as the occurrence of PNI. Its mechanism may be related to the regulation of miR-204-dependent CXCR4. In colon cancer issues [110], the expression level of lncRNA-MALAT1 is 2.26 times higher than that in noncancer tissues and is positively correlated with the occurrence rate of PNI, indicating poor prognosis. In renal carcinoma [111], lncRNA-MALAT1 has high expression and reduces the expression of E-cadherin through the interaction with miR-205. It then promotes EMT, which is related to the proliferation and invasion of renal carcinoma cells as well as to the low survival of patients. Studies by Tan L et al. [112] found that the level of lncRNA-gastric cancer-associated transcript 2 (GACAT2) in the plasma of patients with gastric carcinoma before operation was significantly higher than that after operation and significantly related to the occurrence of PNI. Thus, plasma-based GACAT2 can be developed as a tumor marker to screen for and predict the prognosis of patients with gastric carcinoma. The level of lncRNA-AA174084 in gastric carcinoma tissues is obviously lower than that in the adjacent normal tissues and indicates the occurrence and poor prognosis of PNI [113]. However, the level of AA174084 in gastric juice of patients with gastric carcinoma is higher, and this is similar to the observation that the level of some noncoding RNA (e.g., miR-200a, miRNA-21, and miR-106a) in body fluid is inconsistent with the level in tissues [114]. We believe the high level of AA174084 in gastric juice may be secreted by an exosome or other means. Gezer U [115] showed that exosomes can transfer noncoding RNA into the body liquid. Exosomes are increasingly recognized as important media of intercellular communication. They can transfer receptor, protein, and RNA into the target cells through the interaction with cells and then produce a specific targeting effect. Data from En-Hao Yu [116] confirmed that in oral squamous cell carcinoma, the expression of miR-21 is negatively correlated with the expression of phosphatase and tensin homolog deleted on chromosome ten (PTEN; also called mutated in multiple advanced cancers 1). The high expression of miR-21 assists cancer cells in invading the nerve tract and dispersing, promotes the occurrence of PNI, influences the survival of patients, and is an independent prognosis factor of oral squamous cell carcinoma and multiple solid tumors, whereas the expression reduction of PTEN is also used as an indicator of poor prognosis of several cancers. Studies by Sousa LO [117] showed that miRNA takes part in the malignant transformation process of head and neck squamous cell carcinoma; the rise in miR-21 level; the reduction in miR-100, miR-125b, and PTEN level; the following influence on protein level, which controls the tumor marker and provides high proliferation ability to head and neck squamous cell carcinoma; apoptosis; and the occurrence of PNI. Based on breast cancer studies, Sim J [118] confirmed that the upregulation of miR-370 in breast cancer is related to the progression of breast cancer and the occurrence of PNI, indicating poor prognosis, and that miR-370 may play a role as an oncogene. According to current studies, the expressions of lncRNA and microRNA are closely related to the occurrence of PNI and have become new gene regulation factors and prognosis markers of several cancers. They can be used as preoperation and intraoperation diagnosis markers of PNI, which plays an important role in predicting the clinical outcomes. However, the specific mechanisms of lncRNA, microRNA, and exosomes, including promoting transportation of cell information, require further research. We believe lncRNA and microRNA will become promising chemotherapy targets during the inhibition of PNI and tumor progression pathways.
Conclusion
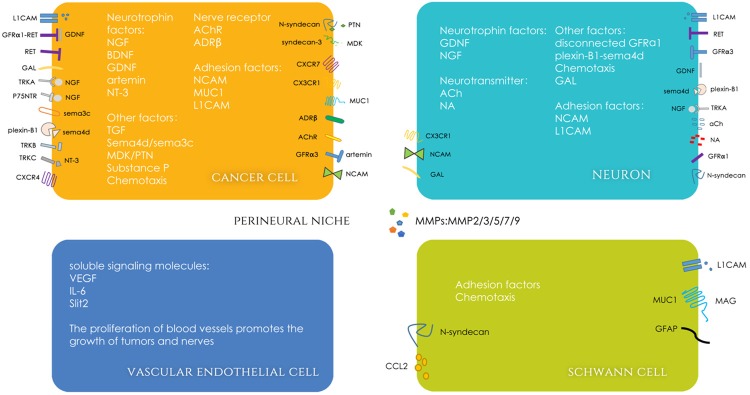
The exploration of the molecular mechanisms of tumor occurrence is of great interest to researchers, especially today, due to the rapid development of precision medicine and molecular biology. PNI is common in various malignant tumors. It promotes the metastasis and invasion of tumor and causes poor prognosis in patients. Although studies on the relationship between tumor and nerves have been carried out for decades, progress in this field is slow. Past views regarded the generation of PNI as caused by low-resistance channel on anatomy, and the latest study showed that in the tumor background environment of oxygen deficit, high glucose level, inflammatory reaction, and sympathetic system activation, tumor cells, nerve cells, supporting cells, recruited inflammatory cells, blood vessels, immune cells, lncRNA, miRNA, and various soluble signaling molecules and their receptors in a perineural niche interact with each other and induce various signal pathways to form complex network regulation. These views are summarized in the pattern diagram (Figure 2). Various associated molecules of neurotrophic factors, such as TGF, MMPs, adhesion molecules, cadherin, MK, axon guidance factors, chemotactic factors, and neurotransmitters, transfer the information to the targets accurately and effectively through the opening and closing of the signal transduction pathways and/or the recognition and response of the ligands and receptors, leading to the specific interactions between the nerve cells and the malignant tumor cells. Then, PNI occurs through multiple steps of nerve and supporting cell changes; changes and migration of the perineural matrix; enhancement of the viability, mobility, and invasiveness of the tumor cells; injuring y and regeneration of nerve cells; chemotactic movement; contact and adherence of the nerve cells and the tumor cells; and escape from autophagy, apoptosis, and immunological surveillance of tumor cells. As an increasing number of molecular mechanisms of the PNI process are clarified, we will gain more molecular targets, and blocking these pathways will provide a brand new strategy for tumor therapy. Meanwhile, through the systematic and integral concept of perineural niche, we have more new ideas of ways to prevent tumor occurrence, tumor development, and PNI, and we provide solutions for drug resistance of tumor. The applications of genome-wide expression analysis will help to discover more potential genes that take part in PNI. The application of immunostaining technologies (e.g., antibody glucose transporter-1) can significantly improve the detection rate of PNI [119]. By enhancing magnetic resonance imaging, the motion of tumor cells using the iron oxide nanoparticle marker can be directly observed [90]. By injecting the homologous pancreatic cancer cell line PANC02-H7 into the ischiadic nerve of mouse, S Deborde constituted the in vivo model of PNI of pancreatic cancer [120]. All these efforts will help to further explain the molecular mechanism of PNI. The newly discovered PNI powerful predicting factor (e.g., insulin-like growth factor II mRNA binding protein 3), can provide great help in early prediction and treatment strategy formation of PNI [121].
Figure 2.
Molecular signaling of perineural niche. Four major cells (tumor cell, neuron, vascular endothelial cell, Schwann cell) in the perineural niche and various soluble signaling molecules and their receptors comprise a complex signal network, which achieves the interaction between nerve and tumor. Abbreviations: ADRβ, β-adrenergic receptor; AChR, acetylcholine receptor; GAL, galanin; NA, noradrenaline.
With more study, the molecular mechanism of PNI will be further confirmed. This is a milestone event that can block the occurrence of PNI and lead to specific tumor treatments. At that time, we can confirm the optimum treatment strategy for each patient through the concept of precision medicine and overcome the tumor.
Acknowledgements
This work was supported by the National Science Foundation of China (No. 81272362).
Disclosure of conflict of interest
None.
References
- 1.Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer. 2009;115:3379–3391. doi: 10.1002/cncr.24396. [DOI] [PubMed] [Google Scholar]
- 2.Bapat AA, Hostetter G, Von Hoff DD, Han H. Perineural invasion and associated pain in pancreatic cancer. Nat Rev Cancer. 2011;11:695–707. doi: 10.1038/nrc3131. [DOI] [PubMed] [Google Scholar]
- 3.Deshmukh SD, Willmann JK, Jeffrey RB. Pathways of extrapancreatic perineural invasion by pancreatic adenocarcinoma: evaluation with 3D volume-rendered MDCT imaging. Ajr Am J Roentgenol. 2010;194:668–674. doi: 10.2214/AJR.09.3285. [DOI] [PubMed] [Google Scholar]
- 4.Demir IE, Friess H, Ceyhan GO. Nerve-cancer interactions in the stromal biology of pancreatic cancer. Front Physiol. 2012;3:97. doi: 10.3389/fphys.2012.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang YH, Liu JB, Gui Y, Lei LL, Zhang SJ. Relationship between autophagy and perineural invasion, clinicopathological features, and prognosis in pancreatic cancer. World J Gastroenterol. 2017;23:7232–7241. doi: 10.3748/wjg.v23.i40.7232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schorn S, Demir IE, Haller B, Scheufele F, Reyes CM, Tieftrunk E, Sargut M, Goess R, Friess H, Ceyhan GO. The influence of neural invasion on survival and tumor recurrence in pancreatic ductal adenocarcinoma-A systematic review and meta-analysis. Surg Oncol. 2017;26:105–115. doi: 10.1016/j.suronc.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Jiang N, Deng JY, Liu Y, Ke B, Liu HG, Liang H. Incorporation of perineural invasion of gastric carcinoma into the 7th edition tumor-node-metastasis staging system. Tumour Biol. 2014;35:9429–9436. doi: 10.1007/s13277-014-2258-5. [DOI] [PubMed] [Google Scholar]
- 8.España-Ferrufino A, Lino-Silva LS, Salcedo-Hernández RA. Extramural perineural invasion in pT3 and pT4 gastric carcinomas. J PatholTransl Med. 2018;52:79–84. doi: 10.4132/jptm.2017.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aurello P, Berardi G, Tierno SM, RampioniVinciguerra GL, Socciarelli F, Laracca GG, Giulitti D, Pilozzi E, Ramacciato G. Influence of perineural invasion in predicting overall survival and disease-free survival in patients with locally advanced gastric cancer. Am J Surg. 2017;213:748–753. doi: 10.1016/j.amjsurg.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 10.Deng J, You Q, Gao Y, Yu Q, Zhao P, Zheng Y, Fang W, Xu N, Teng L. Prognostic value of perineural invasion in gastric cancer: a systematic review and meta-analysis. PLoS One. 2014;9:e88907. doi: 10.1371/journal.pone.0088907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oven Ustaalioglu BB, Bilici A, Seker M, Kefeli U, Aydin D, Celik S, Demir T, Erkol B. Prognostic factors for operated gallbladder cancer. J Gastrointest Cancer. 2018 doi: 10.1007/s12029-018-0099-y. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Feo CF, Cossu ML, Ginesu GC, Ginesu GC, Fancellu A, Scanu AM, Piras N, Cherchi G, Cossu A, Sotgiu G, Pazzona M, Porcu A. Perineural infiltration as a prognostic factor in surgically treated gallbladder cancer: a single center experience and literature review. Ann Ital Chir. 2017;88:485–490. [PubMed] [Google Scholar]
- 13.Murakami Y, Uemura K, Sudo T, Hashimoto Y, Kondo N, Nakagawa N, Muto T, Sasaki H, Urabe K, Sueda T. Perineural invasion in extrahepatic cholangiocarcinoma: prognostic impact and treatment strategies. J Gastrointest Surg. 2013;17:1429–1439. doi: 10.1007/s11605-013-2251-0. [DOI] [PubMed] [Google Scholar]
- 14.Wellner UF, Shen Y, Keck T, Jin W, Xu Z. The survival outcome and prognostic factors for distal cholangiocarcinoma following surgical resection: a meta-analysis for the 5-year survival. Surg Today. 2017;47:271–279. doi: 10.1007/s00595-016-1362-0. [DOI] [PubMed] [Google Scholar]
- 15.Tollefson MK, Karnes RJ, Kwon ED, Lohse CM, Rangel LJ, Mynderse LA, Cheville JC, Sebo TJ. Prostate cancer Ki-67 (MIB-1) expression, perineural invasion, and gleason score as biopsy-based predictors of prostate cancer mortality: the Mayo model. Mayo Clin Proc. 2014;89:308–318. doi: 10.1016/j.mayocp.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Zhang LJ, Wu B, Zha ZL, Qu W, Zhao H, Yuan J, Feng YJ. Perineural invasion as an independent predictor of biochemical recurrence in prostate cancer following radical prostatectomy or radiotherapy: a systematic review and meta-analysis. BMC Urol. 2018;18:5. doi: 10.1186/s12894-018-0319-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lubig S, Thiesler T, Müller S, Vorreuther R, Leipner N, Kristiansen G. Quantitative perineural invasion is a prognostic marker in prostate cancer. Pathology. 2018;50:298–304. doi: 10.1016/j.pathol.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Schmitd LB, Scanlon CS, D’Silva NJ. Perineural invasion in head and neck cancer. J Dent Res. 2018;97:742–750. doi: 10.1177/0022034518756297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cracchiolo JR, Xu B, Migliacci JC, Katabi N, Pfister DG, Lee NY, Patel SG, Ghossein RA, Wong RJ. Patterns of recurrence in oral tongue cancer with perineural invasion. Head Neck. 2018;40:1287–1295. doi: 10.1002/hed.25110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huyett P, Duvvuri U, Ferris RL, Johnson JT, Schaitkin BM, Kim S. Perineural invasion in parotid gland malignancies. Otolaryngol Head Neck Surg. 2018;158:1035–1041. doi: 10.1177/0194599817751888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albergotti WG, Schwarzbach HL, Abberbock S, Ferris RL, Johnson JT, Duvvuri U, Kim S. Defining the prevalence and prognostic value of perineural invasion and angiolymphatic invasion in human papillomavirus-positive oropharyngeal carcinoma. Jama Otolaryngol Head Neck Surg. 2017;143:1236–1243. doi: 10.1001/jamaoto.2017.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quintana JM, González N, Lázaro S, Baré M, Fernández-de-Larrea N, Redondo M, Briones E, Escobar A, Sarasqueta C, García-Gutierrez S, Antón-Ladislao A REDISSEC-CARESS/CCR group. Predictors of one and two year mortality in patients with rectal cancer. Colorectal Dis. 2018;20:676–687. [Google Scholar]
- 23.Zare-Bandamiri M, Fararouei M, Zohourinia S, Daneshi N, Dianatinasab M. Risk Factors predicting colorectal cancer recurrence following initial treatment: a 5-year cohort study. Asian Pac J Cancer Prev. 2017;18:2465–2470. doi: 10.22034/APJCP.2017.18.9.2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang Y, He L, Dong D, Yang C, Liang C, Chen X, Ma Z, Huang X, Yao S, Liang C, Tian J, Liu Z. Individualized prediction of perineural invasion in colorectal cancer: development and validation of a radiomics prediction model. Chin J Cancer Res. 2018;30:40–50. doi: 10.21147/j.issn.1000-9604.2018.01.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kinugasa T, Mizobe T, Shiraiwa S, Akagi Y, Shirouzu K. Perineural invasion is a prognostic factor and treatment indicator in patients with rectal cancer undergoing curative surgery: 2000-2011 data from a single-center study. Anticancer Res. 2017;37:3961–3968. doi: 10.21873/anticanres.11780. [DOI] [PubMed] [Google Scholar]
- 26.Zhu Y, Zhang G, Yang Y, Cui L, Jia S, Shi Y, Song S, Xu S. Perineural invasion in early-stage cervical cancer and its relevance following surgery. Oncol Lett. 2018;15:6555–6561. doi: 10.3892/ol.2018.8116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cui L, Shi Y, Zhang GN. Perineural invasion as a prognostic factor for cervical cancer: a systematic review and meta-analysis. Arch GynecolObstet. 2016;292:13–9. doi: 10.1007/s00404-015-3627-z. [DOI] [PubMed] [Google Scholar]
- 28.Vural C, Bayrak BY, Muezzınoglu B, Yucesoy I. Perineural invasion is a valuable prognostic factor in advanced stage and/or Node (+) cervical cancer. Indian J Pathol Microbiol. 2017;60:27–32. doi: 10.4103/0377-4929.200021. [DOI] [PubMed] [Google Scholar]
- 29.Scuteri A, Miloso M, Foudah D, Orciani M, Cavaletti G, Tredici G. Mesenchymal stem cells neuronal differentiation ability: a real perspective for nervous system repair? Curr Stem Cell Res Ther. 2011;6:82–92. doi: 10.2174/157488811795495486. [DOI] [PubMed] [Google Scholar]
- 30.Jeffus SK, Gehlot A, Holthoff E, Stone R, Spencer H, Kelly T, Post SR, Quick CM. A fibromyxoid stromal response is associated with an infiltrative tumor morphology, perineural invasion, and lymph node metastasis in squamous cell carcinoma of the vulva. Am J Surg Pathol. 2016;39:1226–1233. doi: 10.1097/PAS.0000000000000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amit M, Na’Ara S, Gil Z. Mechanisms of cancer dissemination along nerves. Nat Rev Cancer. 2016;16:399. doi: 10.1038/nrc.2016.38. [DOI] [PubMed] [Google Scholar]
- 32.Li J, Ma J, Han L, Xu Q, Lei J, Duan W, Li W, Wang F, Wu E, Ma Q, Huo X. Hyperglycemic tumor microenvironment induces perineural invasion in pancreatic cancer. Cancer Biol Ther. 2015;16:912–921. doi: 10.1080/15384047.2015.1040952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nigri J, Gironella M, Bressy C, Vila-Navarro E, Roques J, Lac S, Bontemps C, Kozaczyk C, Cros J, Pietrasz D. PAP/REG3A favors perineural invasion in pancreatic adenocarcinoma and serves as a prognostic marker. Cell Mol Life Sci. 2017;74:4231–4243. doi: 10.1007/s00018-017-2579-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuang AG, Nickel JC, Andriole GL, Castro-Santamaria R, Freedland SJ, Moreira DM. Both acute and chronic inflammation are associated with lower perineural invasion in men with prostate cancer on repeat biopsy. BJU Int. 2019;123:91–97. doi: 10.1111/bju.14428. [DOI] [PubMed] [Google Scholar]
- 35.Armaiz-Pena GN, Cole SW, Lutgendorf SK, Sood AK. Neuroendocrine influences on cancer progression. Brain BehavImmun. 2013;30(Suppl):S19–S25. doi: 10.1016/j.bbi.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bakst RL, Wong RJ. Mechanisms of perineural invasion. J Neurol Surg Part B Skull Base. 2016;77:096–106. doi: 10.1055/s-0036-1571835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Demir IE, Boldis A, Pfitzinger PL, Teller S, Brunner E, Klose N, Kehl T, Maak M, Lesina M, Laschinger M, Janssen KP, Algül H, Friess H, Ceyhan GO. Investigation of Schwann cells at neoplastic cell sites before the onset of cancer invasion. J Natl Cancer Inst. 2014;106 doi: 10.1093/jnci/dju184. [DOI] [PubMed] [Google Scholar]
- 38.Deborde S, Omelchenko T, Lyubchik A, Zhou Y, He S, McNamara WF, Chernichenko N, Lee SY, Barajas F, Chen CH, Bakst RL, Vakiani E, He S, Hall A, Wong RJ. Schwann cells induce cancer cell dispersion and invasion. J Clin Invest. 2016;126:1538–1554. doi: 10.1172/JCI82658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Azam SH, Pecot CV. Cancer’s got nerve: Schwann cells drive perineural invasion. J Clin Invest. 2016;126:1242. doi: 10.1172/JCI86801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tanaka K, Okugawa Y, Toiyama Y, Inoue Y, Saigusa S, Kawamura M, Araki T, Uchida K, Mohri Y, Kusunoki M. Brain-derived neurotrophic factor (BDNF)-induced tropomyosin-related kinase B (Trk B) signaling is a potential therapeutic target for peritoneal carcinomatosis arising from colorectal cancer. PLoS One. 2014;9:e96410. doi: 10.1371/journal.pone.0096410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shan C, Wei J, Hou R, Wu B, Yang Z, Wang L, Lei D, Yang X. Schwann cells promote EMT and the Schwann-like differentiation of salivary adenoid cystic carcinoma cells via the BDNF/TrkB axis. Oncol Rep. 2016;35:427–435. doi: 10.3892/or.2015.4366. [DOI] [PubMed] [Google Scholar]
- 42.Fujii-Nishimura Y, Yamazaki K, Masugi Y, Douguchi J, Kurebayashi Y, Kubota N, Ojima H, Kitago M, Shinoda M, Hashiguchi A, Sakamoto M. Mesenchymal-epithelial transition of pancreatic cancer cells at perineural invasion sites is induced by Schwann cells. Pathol Int. 2018;68:214–223. doi: 10.1111/pin.12641. [DOI] [PubMed] [Google Scholar]
- 43.Cavel O, Shomron O, Shabtay A, Vital J, Trejo-Leider L, Weizman N, Krelin Y, Fong Y, Wong RJ, Amit M, Gil Z. Endoneurial macrophages induce perineural invasion of pancreatic cancer cells by secretion of GDNF and activation of RET tyrosine kinase receptor. Cancer Res. 2012;72:5733–5743. doi: 10.1158/0008-5472.CAN-12-0764. [DOI] [PubMed] [Google Scholar]
- 44.Tang D, Wang D, Yuan Z, Xue X, Zhang Y, An Y, Chen J, Tu M, Lu Z, Wei J, Jiang K, Miao Y. Persistent activation of pancreatic stellate cells creates a microenvironment favorable for the malignant behavior of pancreatic ductal adenocarcinoma. Int J Cancer. 2013;132:993–1003. doi: 10.1002/ijc.27715. [DOI] [PubMed] [Google Scholar]
- 45.Shen WR, Wang YP, Chang JY, Yu SY, Chen HM, Chiang CP. Perineural invasion and expression of nerve growth factor can predict the progression and prognosis of oral tongue squamous cell carcinoma. J Oral Pathol Med. 2014;43:258–264. doi: 10.1111/jop.12133. [DOI] [PubMed] [Google Scholar]
- 46.Mancino M, Ametller E, Gascón P, Almendro V. The neuronal influence on tumor progression. Biochim Biophys Acta. 2011;1816:105–118. doi: 10.1016/j.bbcan.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 47.Doebele RC, Davis LE, Vaishnavi A, Le AT, Estrada-Bernal A, Keysar S, Jimeno A, Varella-Garcia M, Aisner DL, Li Y, Stephens PJ, Morosini D, Tuch BB, Fernandes M, Nanda N, Low JA. An oncogenic NTRK fusion in a patient with soft-tissue sarcoma with response to the tropomyosin-related kinase inhibitor LOXO-101. Cancer Discov. 2015;5:1049–1057. doi: 10.1158/2159-8290.CD-15-0443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bapat AA, Munoz RM, Von Hoff DD, Han H. Blocking nerve growth factor signaling reduces the neural invasion potential of pancreatic cancer cells. PLoS One. 2016;11:e0165586. doi: 10.1371/journal.pone.0165586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jia S, Wang W, Hu Z, Shan C, Wang L, Wu B, Yang Z, Yang X, Lei D. BDNF mediated TrkB activation contributes to the EMT progression and the poor prognosis in human salivary adenoid cystic carcinoma. Oral Oncol. 2015;51:64–70. doi: 10.1016/j.oraloncology.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 50.Okugawa Y, Tanaka K, Inoue Y, Kawamura M, Kawamoto A, Hiro J, Saigusa S, Toiyama Y, Ohi M, Uchida K, Mohri Y, Kusunoki M. Brain-derived neurotrophic factor/tropomyosin-related kinase B pathway in gastric cancer. Br J Cancer. 2013;108:121–130. doi: 10.1038/bjc.2012.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Amit M, Na’ara S, Sharma K, Ramer N, Ramer I, Agbetoba A, Glick J, Yang X, Lei D, Bjoerndal K, Godballe C, Mücke T, Klaus-Dietrich W, Eckardt AM, Copelli C, Sesenna E, Palmer F, Ganly I, Gil Z. Elective neck dissection in patients with head and neck adenoid cystic carcinoma: an international collaborative study. Ann Surg Oncol. 2015;22:1353–1359. doi: 10.1245/s10434-014-4106-7. [DOI] [PubMed] [Google Scholar]
- 52.Gao L, Bo H, Wang Y, Zhang J, Zhu M. Neurotrophic factor artemin promotes invasiveness and neurotrophic function of pancreatic adenocarcinoma in vivo and in vitro. Pancreas. 2015;44:134–143. doi: 10.1097/MPA.0000000000000223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bakst RL, Lee N, He S, Chernichenko N, Chen CH, Linkov G, Le HC, Koutcher J, Vakiani E, Wong RJ. Radiation impairs perineural invasion by modulating the nerve microenvironment. PLoS One. 2012;7:e39925. doi: 10.1371/journal.pone.0039925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.He S, Chen CH, Chernichenko N, He S, Bakst RL, Barajas F, Deborde S, Allen PJ, Vakiani E, Yu Z, Wong RJ. GFRα1 released by nerves enhances cancer cell perineural invasion through GDNF-RET signaling. Proc Natl Acad Sci U S A. 2014;111:E2008–E2017. doi: 10.1073/pnas.1402944111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DeLancey JO, Wood DP Jr, He C, Montgomery JS, Weizer AZ, Miller DC, Jacobs BL, Montie JE, Hollenbeck BK, Skolarus TA. Evidence of perineural invasion on prostate biopsy specimen and survival after radical prostatectomy. Urology. 2013;81:354–357. doi: 10.1016/j.urology.2012.09.034. [DOI] [PubMed] [Google Scholar]
- 56.Chuang JY, Tsai CF, Chang SW, Chiang IP, Huang SM, Lin HY, Yeh WL, Lu DY. Glial cell line-derived neurotrophic factor induces cell migration in human oral squamous cell carcinoma. Oral Oncol. 2013;49:1103–1112. doi: 10.1016/j.oraloncology.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 57.Yao J, Li WY, Gao SG. The advances of Midkine with peripheral invasion in pancreatic cancer. Am J Cancer Res. 2015;5:2912–2917. [PMC free article] [PubMed] [Google Scholar]
- 58.Yao J, Li WY, Li SG, Feng XS, Gao SG. Midkine promotes perineural invasion in human pancreatic cancer. World J Gastroenterol. 2014;20:3018–3024. doi: 10.3748/wjg.v20.i11.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yao J, Zhang LL, Huang XM, Li WY, Gao SG. Pleiotrophin and N-syndecan promote perineural invasion and tumor progression in an orthotopic mouse model of pancreatic cancer. World J Gastroenterol. 2017;23:3907–3914. doi: 10.3748/wjg.v23.i21.3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen P, Cescon M, Bonaldo P. The role of collagens in peripheral nerve myelination and function. Mol Neurobiol. 2015;52:216–225. doi: 10.1007/s12035-014-8862-y. [DOI] [PubMed] [Google Scholar]
- 61.Guo D, Sun W, Zhu L, Zhang H, Hou X, Liang J, Jiang X, Liu C. Knockdown of BDNF suppressed invasion of HepG2 and HCCLM3 cells, a mechanism associated with inactivation of RhoA or Racl and actin skeleton disorganization. APMIS. 2012;120:469–476. doi: 10.1111/j.1600-0463.2011.02855.x. [DOI] [PubMed] [Google Scholar]
- 62.Cossa G, Gatti L, Cassinelli G, Lanzi C, Zaffaroni N, Perego P. Modulation of sensitivity to antitumor agents by targeting the MAPK survival pathway. Curr Pharm Des. 2013;19:883–894. [PubMed] [Google Scholar]
- 63.Gao H, Peng C, Liang B, Shahbaz M, Liu S, Wang B, Sun Q, Niu Z, Niu W, Liu E, Wang J, Lin P, Wang J, Niu J. β6 integrin induces the expression of metalloproteinase-3 and metalloproteinase-9 in colon cancer cells via ERK-ETS1 pathway. Cancer Lett. 2014;354:427–437. doi: 10.1016/j.canlet.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 64.Chen Q, Yin D, Zhang Y, Yu L, Li XD, Zhou ZJ, Zhou SL, Gao DM, Hu J, Jin C, Wang Z, Shi YH, Cao Y, Fan J, Dai Z, Zhou J. MicroRNA-29a induces loss of 5-hydroxymethylcytosine and promotes metastasis of hepatocellular carcinoma through a TET SOCS1-MMP9 signaling axis. Cell Death Dis. 2017;8:e2906. doi: 10.1038/cddis.2017.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xu L, Hou Y, Tu G, Chen Y, Du YE, Zhang H, Wen S, Tang X, Yin J, Lang L, Sun K, Yang G, Tang X, Liu M. Nuclear Drosha enhances cell invasion via an EGFR-ERK1/2-MMP7 signaling pathway induced by dysregulated miRNA-622/197 and their targets LAMC2 and CD82 in gastric cancer. Cell Death Dis. 2017;8:e2642. doi: 10.1038/cddis.2017.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xiang T, Xia X, Yan W. Expression of matrix metalloproteinases-2/-9 is associated with microvessel density in pancreatic cancer. Am J Ther. 2017;24:E431–E434. doi: 10.1097/MJT.0000000000000424. [DOI] [PubMed] [Google Scholar]
- 67.Klimczak-Bitner AA, Kordek R, Bitner J, Musiał J, Szemraj J. Expression of MMP9, SERPINE1 and miR-134 as prognostic factors in esophageal cancer. Oncol Lett. 2016;12:4133–4138. doi: 10.3892/ol.2016.5211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Juchniewicz A, Kowalczuk O, Milewski R, Laudański W, Dzięgielewski P, Kozłowski M, Nikliński J. MMP-10, MMP-7, TIMP-1 and TIMP-2 mRNA expression in esophageal cancer. Acta Biochim Pol. 2017;64:295–299. doi: 10.18388/abp.2016_1408. [DOI] [PubMed] [Google Scholar]
- 69.Li Q, Wang Y, Lai Y, Xu P, Yang Z. HspB5 correlates with poor prognosis in colorectal cancer and prompts epithelial mesenchymaltransition through ERK signaling. PLoS One. 2017;12:e0182588. doi: 10.1371/journal.pone.0182588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Klupp F, Neumann L, Kahlert C, Diers J, Halama N, Franz C, Schmidt T, Koch M, Weitz J, Schneider M, Ulrich A. Serum MMP7, MMP10 and MMP12 level as negative prognostic markers in colon cancer patients. BMC Cancer. 2016;16:494. doi: 10.1186/s12885-016-2515-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lu L, Ma GQ, Liu XD, Sun RR, Wang Q, Liu M, Zhang PY. Correlation between GDF15, MMP7 and gastric cancer and its prognosis. Eur Rev Med Pharmacol Sci. 2017;21:535–541. [PubMed] [Google Scholar]
- 72.Han Y, Wu Z, Wu T, Huang Y, Cheng Z, Li X, Sun T, Xie X, Zhou Y, Du Z. Tumor-suppressive function of long noncoding RNA MALAT1 in glioma cells by downregulation of MMP2 and inactivation of ERK/MAPK signaling. Cell Death Dis. 2016;7:e2123. doi: 10.1038/cddis.2015.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang TF, Guo L, Wang Q. Meta-analysis of associations between four polymorphisms in the matrix metalloproteinases gene and gastric cancer risk. Asian Pac J Cancer Prev. 2014;15:1263–1267. doi: 10.7314/apjcp.2014.15.3.1263. [DOI] [PubMed] [Google Scholar]
- 74.Du J, Zhang L. Analysis of salivary microRNA expression profiles and identification of novel biomarkers in esophageal cancer. Oncol Lett. 2017;14:1387–1394. doi: 10.3892/ol.2017.6328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ding Y, He D, Florentin D, Frolov A, Hilsenbeck S, Ittmann M, Kadmon D, Miles B, Rowley D, Ayala G. Semaphorin 4F as a critical regulator of neuroepithelial interactions and a biomarker of aggressive prostate cancer. Clin Cancer Res. 2013;19:6101–6111. doi: 10.1158/1078-0432.CCR-12-3669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Binmadi NO, Yang YH, Zhou H, Proia P, Lin YL, De Paula AM, Guimarães AL, Poswar FO, Sundararajan D, Basile JR. Plexin-B1 and semaphorin 4D cooperate to promote perineural invasion in a RhoA/ROK-dependent manner. Am J Pathol. 2012;180:1232–1242. doi: 10.1016/j.ajpath.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 77.Göhrig A, Detjen KM, Hilfenhaus G, Körner JL, Welzel M, Arsenic R, Schmuck R, Bahra M, Wu JY, Wiedenmann B. Axon guidance factor SLIT2 inhibits neural invasion and metastasis in pancreatic cancer. Cancer Res. 2014;74:1529–1540. doi: 10.1158/0008-5472.CAN-13-1012. [DOI] [PubMed] [Google Scholar]
- 78.He S, He S, Chen CH, Deborde S, Bakst RL, Chernichenko N, McNamara WF, Lee SY, Barajas F, Yu Z, Al-Ahmadie HA, Wong RJ. The chemokine (CCL2-CCR2) signaling axis mediates perineural invasion. Mol Cancer Res. 2015;13:380–390. doi: 10.1158/1541-7786.MCR-14-0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bakst RL, Xiong H, Chen CH, Deborde S, Lyubchik A, Zhou Y, He S, McNamara W, Lee SY, Olson OC, Leiner IM, Marcadis AR, Keith JW, Al-Ahmadie HA, Katabi N, Gil Z, Vakiani E, Joyce JA, Pamer E, Wong RJ. Inflammatory monocytes promote perineural invasion via CCL2-mediated recruitment and cathepsin B expression. Cancer Res. 2017;77:6400. doi: 10.1158/0008-5472.CAN-17-1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gao T, Shen Z, Ma C, Li Y, Kang X, Sun M. The CCL5/CCR5 chemotactic pathway promotes perineural invasion in salivary adenoid cystic carcinoma. J Oral Maxillofac Surg. 2018;76:1708–1718. doi: 10.1016/j.joms.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 81.Sukhanova KY, Harhun MI, Bouryi VA, Gordienko DV. Mechanisms of Ca2+ elevation following P2X receptor activation in the guinea-pig small mesenteric artery myocytes. Pharmacol Rep. 2013;65:152–163. doi: 10.1016/s1734-1140(13)70973-3. [DOI] [PubMed] [Google Scholar]
- 82.Shen Z, Li T, Chen D, Jia S, Yang X, Liang L, Chai J, Cheng X, Yang X, Sun M. The CCL5/CCR5 axis contributes to the perineural invasion of human salivary adenoid cystic carcinoma. Oncol Rep. 2014;31:800. doi: 10.3892/or.2013.2920. [DOI] [PubMed] [Google Scholar]
- 83.Zaitseva L, Murray MY, Shafat MS, Lawes MJ, MacEwan DJ, Bowles KM, Rushworth SA. Ibrutinib inhibits SDF1/CXCR4 mediated migration in AML. Oncotarget. 2014;5:9930–9938. doi: 10.18632/oncotarget.2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li J, Ma Q, Liu H, Guo K, Li F, Li W, Han L, Wang F, Wu E. Relationship between neural alteration and perineural invasion in pancreatic cancer patients with hyperglycemia. PLoS One. 2011;6:e17385. doi: 10.1371/journal.pone.0017385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Li X, Ma Q, Xu Q, Liu H, Lei J, Duan W, Bhat K, Wang F, Wu E, Wang Z. SDF-1/CXCR4 signaling induces pancreatic cancer cell invasion and epithelial-mesenchymal transition in vitro through non-canonical activation of Hedgehog pathway. Cancer Lett. 2012;322:169–176. doi: 10.1016/j.canlet.2012.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pitts TM, Kulikowski GN, Tan AC, Murray BW, Arcaroli JJ, Tentler JJ, Spreafico A, Selby HM, Kachaeva MI, McPhillips KL, Britt BC, Bradshaw-Pierce EL, Messersmith WA, Varella-Garcia M, Eckhardt SG. Association of the epithelial-to-mesenchymal transition phenotype with responsiveness to the p21-activated kinase inhibitor, PF-3758309, in colon cancer models. Front Pharmacol. 2013;4:35. doi: 10.3389/fphar.2013.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Donà E, Barry JD, Valentin G, Quirin C, Khmelinskii A, Kunze A, Durdu S, Newton LR, Fernandez-Minan A, Huber W, Knop M, Gilmour D. Directional tissue migration through a self-generated chemokine gradient. Nature. 2013;503:285–289. doi: 10.1038/nature12635. [DOI] [PubMed] [Google Scholar]
- 88.Bauman J, McVary K. Autonomic nerve development contributes to prostate cancer progression. Asian J Androl. 2013;15:713–714. doi: 10.1038/aja.2013.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ben QW, Wang JC, Liu J, Zhu Y, Yuan F, Yao WY, Yuan YZ. Positive expression of L1-CAM is associated with perineural invasion and poor outcome in pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2010;17:2213. doi: 10.1245/s10434-010-0955-x. [DOI] [PubMed] [Google Scholar]
- 90.Huang C, Li Y, Guo Y, Zhang Z, Lian G, Chen Y, Li J, Su Y, Li J, Yang K, Chen S, Su H, Huang K, Zeng L. MMP1/PAR1/SP/NK1R paracrine loop modulates early perineural invasion of pancreatic cancer cells. Theranostics. 2018;8:3074–3086. doi: 10.7150/thno.24281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Scanlon CS, Banerjee R, Inglehart RC, Liu M, Russo N, Hariharan A, van Tubergen EA, Corson SL, Asangani IA, Mistretta CM, Chinnaiyan AM, D’Silva NJ. Galanin modulates the neural niche to favour perineural invasion in head and neck cancer. Nat Commun. 2015;6:6885. doi: 10.1038/ncomms7885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Olar A, He D, Florentin D, Ding Y, Wheeler T, Ayala G. Biological correlates of prostate cancer perineural invasion diameter. Hum Pathol. 2014;45:1365–1369. doi: 10.1016/j.humpath.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mallini P, Lennard T, Kirby J, Meeson A. Epithelial-to-mesenchymal transition: what is the impact on breast cancer stem cells and drug resistance. Cancer Treat Rev. 2014;40:341–348. doi: 10.1016/j.ctrv.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 94.He Q, Zhou X, Li S, Jin Y, Chen Z, Chen D, Cai Y, Liu Z, Zhao T, Wang A. MicroRNA-181a suppresses salivary adenoid cystic carcinoma metastasis by targeting MAPK Snai2 pathway. Biochim Biophys Acta. 2014;1830:5258–5266. doi: 10.1016/j.bbagen.2013.07.028. [DOI] [PubMed] [Google Scholar]
- 95.Tilan J, Kitlinska J. Neuropeptide Y (NPY) in tumor growth and progression: lessons learned from pediatric oncology. Neuropeptides. 2016;55:55–66. doi: 10.1016/j.npep.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hassan S, Karpova Y, Baiz D, Yancey D, Pullikuth A, Flores A, Register T, Cline JM, D’Agostino R Jr, Danial N, Datta SR, Kulik G. Behavioral stress accelerates prostate cancer development in mice. J Clin Invest. 2013;123:874–886. doi: 10.1172/JCI63324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yates C. Influence of tumor microenvironment on the molecular regulation of prostate cancer progression. Eur Neuropsychopharm. 2011;13:S96–S97. [Google Scholar]
- 98.Zhao CM, Hayakawa Y, Kodama Y, Muthupalani S, Westphalen CB, Andersen GT, Flatberg A, Johannessen H, Friedman RA, Renz BW, Sandvik AK, Beisvag V, Tomita H, Hara A, Quante M, Li Z, Gershon MD, Kaneko K, Fox JG, Wang TC, Chen D. Denervation suppresses gastric tumorigenesis. Sci Transl Med. 2014;6:250ra115. doi: 10.1126/scitranslmed.3009569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fromont G, Godet J, Pires C, Yacoub M, Dore B, Irani J. Biological significance of perineural invasion (PNI) in prostate cancer. Prostate. 2012;72:542–548. doi: 10.1002/pros.21456. [DOI] [PubMed] [Google Scholar]
- 100.Kim-Fuchs C, Le CP, Pimentel MA, Shackleford D, Ferrari D, Angst E, Hollande F, Sloan EK. Chronic stress accelerates pancreatic cancer growth and invasion: a critical role for beta-adrenergic signaling in the pancreatic microenvironment. Brain BehavImmun. 2014;40:40–47. doi: 10.1016/j.bbi.2014.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Saloman JL, Albers KM, Rhim AD, Davis BM. Can stopping nerves, stop cancer? Trends Neurosci. 2016;39:880–889. doi: 10.1016/j.tins.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Arese M, Bussolino F, Pergolizzi M, Bizzozero L, Pascal D. Tumor progression: the neuronal input. Ann Transl Med. 2018;6:89. doi: 10.21037/atm.2018.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Samarelli AV, Riccitelli E, Bizzozero L, Silveira TN, Seano G, Pergolizzi M, Vitagliano G, Cascone I, Carpentier G, Bottos A, Primo L, Bussolino F, Arese M. Neuroligin 1 induces blood vessel maturation by cooperating with the α6 integrin. J Biol Chem. 2014;289:19466–19476. doi: 10.1074/jbc.M113.530972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Graziano S, Marchiò S, Bussolino F, Arese M. A peptide from the extracellular region of the synaptic protein α Neurexin stimulates angiogenesis and the vascular specific tyrosine kinase Tie2. Biochem Biophys Res Commun. 2013;432:574–579. doi: 10.1016/j.bbrc.2013.02.045. [DOI] [PubMed] [Google Scholar]
- 105.Echarri MJ, Lopez-Martin A, Hitt R. Targeted therapy in locally advanced and recurrent/metastatic head and neck squamous cell carcinoma (LA-R/M HNSCC) Cancers (Basel) 2016;8 doi: 10.3390/cancers8030027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yoshihara N, Takagi A, Ueno T, Ikeda S. Inverse correlation between microtubule-associated protein 1A/1B-light chain 3 and p62/sequestosome-1 expression in the progression of cutaneous squamous cell carcinoma. J Dermatol. 2014;41:311–315. doi: 10.1111/1346-8138.12439. [DOI] [PubMed] [Google Scholar]
- 107.Zheng LQ, Li SY, Li CX. Expression profiling analysis of autophagy-related genes in perineural invasion of cutaneous squamous cell carcinoma. Oncol Lett. 2018;15:4837–4848. doi: 10.3892/ol.2018.7971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wei W, Liu Y, Lu Y, Yang B, Tang L. LncRNA XIST promotes pancreatic cancer proliferation through miR-133a/EGFR. J Cell Biochem. 2017;118:3349–3358. doi: 10.1002/jcb.25988. [DOI] [PubMed] [Google Scholar]
- 109.Tan X, Huang Z, Li X. Long Non-Coding RNA MALAT1 interacts with miR-204 to modulate human hilar cholangiocarcinoma proliferation, migration, and invasion by targeting CXCR4. Cell Biochem. 2017;118:3643–3653. doi: 10.1002/jcb.25862. [DOI] [PubMed] [Google Scholar]
- 110.Zheng HT, Shi DB, Wang YW, Li XX, Xu Y, Tripathi P, Gu WL, Cai GX, Cai SJ. High expression of lncRNA MALAT1 suggests a biomarker of poor prognosis in colorectal cancer. Int J Clin Exp Pathol. 2014;7:3174–3181. [PMC free article] [PubMed] [Google Scholar]
- 111.Hirata H, Hinoda Y, Shahryari V, Deng G, Nakajima K, Tabatabai ZL, Ishii N, Dahiya R. Long noncoding RNA MALAT1 promotes aggressive renal cell carcinoma through Ezh2 and interacts with miR-205. Cancer Res. 2015;75:1322–1331. doi: 10.1158/0008-5472.CAN-14-2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tan L, Yang Y, Shao Y, Zhang H, Guo J. Plasma lncRNA-GACAT2 is a valuable marker for the screening of gastric cancer. Oncol Lett. 2016;12:4845–4849. doi: 10.3892/ol.2016.5297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shao Y, Ye M, Jiang X, Sun W, Ding X, Liu Z, Ye G, Zhang X, Xiao B, Guo J. Gastric juice long noncoding rna used as a tumor marker for screening gastric cancer. Cancer. 2014;120:3320–3328. doi: 10.1002/cncr.28882. [DOI] [PubMed] [Google Scholar]
- 114.Cui L, Zhang X, Ye G, Zheng T, Song H, Deng H, Xiao B, Xia T, Yu X, Le Y, Guo J. Gastric juice microRNAs as potential biomarkers for the screening of gastric cancer. Cancer. 2013;119:1618–1626. doi: 10.1002/cncr.27903. [DOI] [PubMed] [Google Scholar]
- 115.Gezer U, Özgür E, Cetinkaya M, Isin M, Dalay N. Long non-coding RNAs with low expression levels in cells are enriched in secreted exosomes. Cell Biol Int. 2014;38:1076–1079. doi: 10.1002/cbin.10301. [DOI] [PubMed] [Google Scholar]
- 116.Yu EH, Tu HF, Wu CH, Yang CC, Chang KW. MicroRNA-21 promotes perineural invasion and impacts survival in patients with oral carcinoma. J Chin Med Assoc. 2017;80:383–388. doi: 10.1016/j.jcma.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 117.Sousa LO, Sobral LM, Matsumoto CS, Saggioro FP, López RV, Panepucci RA, Curti C, Silva WA Jr, Greene LJ, Leopoldino AM. Lymph node or perineural invasion is associated with low miR-15a, miR-34c and miR-199b levels in head and neck squamous cell carcinoma. BBA Clin. 2016;6:159–164. doi: 10.1016/j.bbacli.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sim J, Ahn H, Abdul R, Kim H, Yi KJ, Chung YM, Chung MS, Paik SS, Song YS, Jang K. High MicroRNA-370 expression correlates with tumor progression and poor prognosis in breast cancer. J Breast Cancer. 2015;18:323–328. doi: 10.4048/jbc.2015.18.4.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ueno H, Shirouzu K, Eishi Y, Yamada K, Kusumi T, Kushima R, Ikegami M, Murata A, Okuno K, Sato T, Ajioka Y, Ochiai A, Shimazaki H, Nakamura T, Kawachi H, Kojima M, Akagi Y, Sugihara K Study Group for Perineural Invasion projected by the Japanese Society for Cancer of the Colon and Rectum (JSCCR) Characterization of perineural invasion as a component of colorectal cancer staging. Am J Surg Pathol. 2013;37:1542–1549. doi: 10.1097/PAS.0b013e318297ef6e. [DOI] [PubMed] [Google Scholar]
- 120.Deborde S, Yu Y, Marcadis A, Chen CH, Fan N, Bakst RL, Wong RJ. An in vivo murine sciatic nerve model of perineural invasion. J Vis Exp. 2018 doi: 10.3791/56857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tarsitano A, Asioli S, Morandi L, Monti V, Righi A, MorselliLabate AM, Nardi E, Foschini MP, Marchetti C. Laminin-5 and insulin-like growth factor-II mRNA binding protein-3 (IMP3) expression in preoperative biopsy specimens from oral cancer patients: their role in neural spread risk and survival stratification. J Craniomaxillofac Surg. 2016;44:1896–1902. doi: 10.1016/j.jcms.2016.07.012. [DOI] [PubMed] [Google Scholar]