Abstract
Background
Studies investigating bladder cancer risk in pioglitazone-treated type 2 diabetes mellitus patients report conflicting results. Previous meta-analyses on this topic utilized publications prior to 2013. More long-term observational studies have been published since then. We reviewed the accumulated evidence and updated findings from previous meta-analyses.
Methods
This meta-analysis was based on a systematic review of peer-reviewed observational studies published prior to September 30, 2016. Eligible studies were identified using a specified MEDLINE search. References from included studies and from previous meta-analyses were screened for additional records. Meta-analysis hazards ratios were derived using a random-effects model. Several sensitivity analyses including hierarchical Bayesian meta-analysis with country-specific effects were conducted.
Results
Of 363 identified records, 23 studies were included in this review and 18 in the actual meta-analyses. For bladder cancer outcome, the estimated effect size for ever vs. never use of pioglitazone was 1.16 [95% confidence interval (CI), 1.04–1.28]. In the cumulative dose and duration analyses, highest effect was observed in the highest/longest exposure group, but substantial heterogeneity was present. In the sensitivity analysis, only studies adjusted for lifestyle-related factors were included and the frequentist effect size was 1.18 (95% CI, 1.00–1.40, p = 0.054). However, the risk was not verified in the Bayesian framework with an effect size of 1.17 [95% credible interval (CrI), 0.94–1.54].
Conclusions
In line with previous meta-analyses, we observed a small but statistically significant association between ever (vs. never) use of pioglitazone and bladder cancer risk; however, causality is not established and alternative explanations cannot be ruled out.
Electronic supplementary material
The online version of this article (10.1007/s13340-018-0360-4) contains supplementary material, which is available to authorized users.
Keywords: Bladder cancer, Meta-analysis, Pioglitazone, Review, Observational studies
Introduction
The burden of diabetes has been rising with its increasing prevalence. Currently, type 2 diabetes mellitus (T2DM) presents a global public health problem not only in industrialized countries, but across the globe. An estimated 422 million individuals or 8.5% of the world’s population had diabetes in 2014 [1]. It is estimated that 29.1 million people had diabetes in the United States (US) in 2014; including 21 million diagnosed and 8.1 million undiagnosed cases [2]. In the US alone, direct medical costs of $176 billion and indirect costs of $69 billion were spent on diabetic patients care in 2012 [3].
Pioglitazone is an agonist of peroxisome proliferator activated receptor-γ (PPAR γ) in the class of thiazolidinedione and is used to treat T2DM. Pioglitazone has effective glycemic control in both diabetic and pre-diabetic populations. The Actos Now for Prevention of Diabetes (ACT NOW) clinical trial showed that pioglitazone reduced the risk of T2DM conversion in adults with impaired glucose tolerance by 72% [4, 5]. Pioglitazone has been shown to be efficacious in glycemic control in T2DM patients alone or in combination with metformin, sulfonylurea, or insulin [6–9].
The use of pioglitazone raised a safety concern after an increased number of bladder cancer cases were observed in exposed male rats, though the effect was not observed in female rats or mice of both sexes [10]. Several observational studies have been published investigating the possible risk of bladder cancer in pioglitazone users with conflicting results [11–17]. It is plausible that limitations, methodological differences, residual confounding, and other biases may have contributed to discrepancies between the findings of these studies. Furthermore, several meta-analyses of published studies have suggested that pioglitazone use is associated with a small increase in the risk of bladder cancer [18–23]. All previous meta-analyses were conducted using studies published prior to 2013 and more observational studies have been published since then [24–26].
Recently, a 10-year follow-up study in the US with a diabetic cohort of 193,099 persons from 1997–2002 until December 2012 was published [24]. This study found no statistically significant association between pioglitazone use and risk of bladder cancer [adjusted hazard ratio (aHR), 1.06; 95% confidence interval (CI), 0.89–1.26]. The same study also included a nested case–control analysis of 928 persons with complete bladder cancer-related medical history which found no statistically significant association either [adjusted odds ratio (aOR), 1.18; 95% CI, 0.78–1.80]. Another recent cohort study pooled six large European databases and selected 56,337 eligible pioglitazone users matched to 56,337 non-users [27]. No association was observed in this study (aOR, 0.99; 95% CI, 0.75–1.30). Meanwhile, a study from the United Kingdom (UK) found that pioglitazone was associated with increased bladder cancer risk in comparison to other antidiabetic drugs among 145,806 diabetic patients [26].
New data since the recent meta-analyses [18–23] have not been incorporated in the latest observational knowledge by meta-analysis methods. There are also some limitations to the previous meta-analyses. For instance, in the Turner et al. review [21], only eight observational studies were included for pioglitazone. Of the studies included, one observational US-based study (KPNC study13) has more recent data following completion of longer-term follow-up.26 The updated KPNC results did not show an increased risk of bladder cancer with any duration of pioglitazone use. In addition, a meta-analysis may be subject to publication bias, as articles of non-significant results tend to be published later than those with significant results. Turner et al. [21] did not evaluate publication bias due to small sample size. In addition, they used a fixed-effect model for analysis based on small I2 statistic for heterogeneity, which is heavily biased by small sample size [28]. Furthermore, three of the eight observational studies included were from Taiwan. As a result, patients in the Taiwanese population could have a disproportionally higher contribution than patients in other populations. The other meta-analyses reviewed the association of the risk of bladder cancer and pioglitazone with slightly different methods [18–20, 22, 23]. However; all these meta-analyses largely utilized the same relatively small number of studies, underlining the need to update knowledge with observational data from newer studies.
The objective of this meta-analysis was to assess the association between risk of bladder cancer and exposure to pioglitazone among subjects with T2DM in a meta-analysis of observational studies and to update the findings reported in previously published meta-analyses by extending the accumulated evidence prior to 2013 with subsequently published studies up to September 30, 2016. The primary research question was whether T2DM patients treated with pioglitazone had a higher risk of bladder cancer compared to those who were not treated with pioglitazone. The secondary research question was whether an increased cumulative duration or dose of pioglitazone was associated with higher risk of bladder cancer.
Methods
Selection of studies
This meta-analysis was based on a comprehensive literature review that identified eligible observational studies from peer-reviewed scientific journals. Studies published prior to September 30, 2016 were identified using a MEDLINE search strategy and the inclusion criteria (Table 1, Supplementary Table 1). Observational studies presenting a measure of association between risk of bladder cancer and pioglitazone use in type 2 diabetes mellitus patients were eligible for inclusion in this meta-analysis. The references of each included study and from previous meta-analyses were screened for additional records. After removing duplicates, titles and abstracts yielded by the search were independently screened against the inclusion criteria by two review authors. Disagreement between the reviewers was resolved through a discussion.
Table 1.
Criteria for considering studies in this review
| Types of studies | Observational studies, e.g., cohort studies, case–control studies, nested case–control studies (open label extensions of clinical trials were not eligible) |
|---|---|
| Types of participants | Human subjects with T2DM |
| Types of comparisons | Pioglitazone users vs. non-users (including users of other diabetes medications), and/or, increasing duration of pioglitazone exposure, and/or increasing cumulative pioglitazone dose (reference group defined as never use of pioglitazone including use of any other antidiabetic medications) |
| Type of outcome | Incident bladder cancer |
| Published results | Full text available, i.e., fully published article in a peer-reviewed journal |
| Data on outcome | A measure of association between bladder cancer and pioglitazone use (odds ratio [OR], relative risk [RR] or hazard ratio [HR]), or sufficient data to enable estimation of HR |
| Language | Abstract should be available in English |
The MEDLINE search strategy is presented in Supplementary Table 1
Data collection and variables
All included studies were searched to extract the following variables: authorship, year of publication, country or region of source data, setting (database used), study design (e.g., cohort, case–control, nested case–case control), study period, inclusion and exclusion criteria, study population size, follow-up time, age, proportion of male subjects, outcome identification, number of bladder cancer cases, type(s) of pioglitazone exposure studied, estimated effect sizes for pioglitazone–bladder cancer association, adjusting covariates, and any additional information that might guide the reviewers when assessing the risk of bias within individual studies.
Assessment of bias
The risk of bias in the included studies was evaluated regarding potential confounding by indication/channeling bias, immortal time bias, and information bias by addressing pre-specified questions detailed in the supplement. For each eligible study, a judgement as to the possible risk of bias was made for each of the pre-specified questions based on the extracted information and rated as ‘high risk’ or ‘low risk’. The risk of bias was judged ‘unclear’ if there was insufficient detail reported in the study.
Study conduct
The study was conducted according to a study protocol developed following the code of conduct of the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). The study protocol is registered and available at the ENCePP E-Register of Studies, no EUPAS16082.
Statistical methods
Primary and secondary analyses
As the primary analysis, the pooled HR for the risk of incident bladder cancer with pioglitazone use (ever) vs. no use (never) was estimated. In the first secondary analysis, among studies where the results for cumulative dose were available, the pooled HR was estimated in the following subgroups and compared to never use category: < 10,500, 10,500–28,000, and > 28,000 mg. In the second secondary analysis, among studies where the results for cumulative exposure duration of pioglitazone were available, the pooled HR was estimated in the following subgroups and compared to never use category: < 12 months, 12–24 months, and > 24 months. Random-effects model was used in both primary and secondary analyses. Most comprehensively adjusted results were used from each study. For multi-country studies reporting both country-specific and overall effect sizes (combining all countries), the overall estimate was used.
Assessment of heterogeneity
Heterogeneity across studies was assessed using the I2 statistic [29, 30] with pre-specified categorization including 0–40%: might not be important; 30–60%: may represent moderate heterogeneity; 50–90%: may represent substantial heterogeneity; 75–100%: considerable heterogeneity. Heterogeneity with a significance level of 0.1 was tested using the Chi squared test.
Assessment of publication bias
Publication bias was studied with the funnel plot [31] and tested using Begg’s rank correlation test [32] and Egger’s regression test [33].
Sensitivity analyses
Regarding the never vs. ever exposure for pioglitazone use and bladder cancer risk, the following sensitivity analyses were conducted. First, studies considered prone to high risk of bias were excluded. Second, the pooled HR was estimated using a Bayesian random-effects model. Third, the pooled HR was estimated using a Bayesian random-effects model with extra level of hierarchy (study country). This approach combines study-specific estimates from the same country into country-specific estimates that in turn contribute to the estimation of the overall effect. This provides a potential solution to account for the possible correlation between studies within the same country caused by the overlapping study subjects. Model details are presented in the supplement. Fourth, the primary analysis was repeated using a fixed-effect model. Fifth, studies excluded in the original primary analysis due to not reporting results for never vs. ever exposure in the total population were included by first estimating the overall effect with a fixed-effect meta-analysis model. Sixth, separate meta-analysis was performed for case–control and cohort studies.
Results
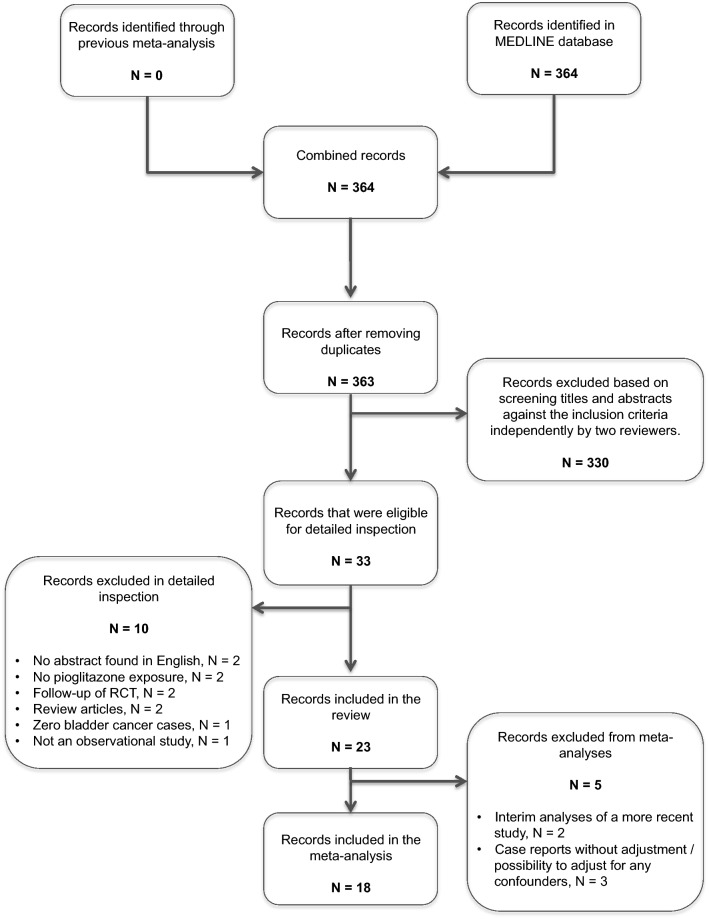
After a systematic review of 363 identified records, 23 studies were included in this review and 18 studies in the actual meta-analysis. Among the 5 studies excluded from the meta-analysis, 2 studies were interim analysis of a more recently published study with updated data. Only the most recent published results were included in the meta-analysis. Three studies failing to adjust for any confounding variables and reporting only crude estimates were judged as having a high risk of bias and excluded from the meta-analysis. Figure 1 shows a flowchart describing the selection of studies. A summary of 23 studies included in this review, including 5 that were excluded from the actual meta-analysis, is provided in Table 2. The total population size was 3,499,600 patients, ranging from 28,514 to 1,491,060 patients per study. The study periods were between 1988 and 2014 and the average follow-up varied between 2 and 7.9 years. Study-specific effect sizes are presented in Supplementary Table 2. Among the 18 studies included in the meta-analysis, 2 involved a nested case–control setting within a cohort study [25, 34]. The main reason for having the nested case–control setting was the ability to control for more confounding variables among specific study subjects. In the primary analysis, we selected the use of the nested case–control study results from Jin et al. [34] instead of the cohort study results, because the latter was only adjusted for age and sex. Conversely, even though the Lewis et al. [25] case–control study had complete information on certain adjusting variables, we used the cohort study in the primary analysis since it was also adjusted for several variables.
Fig. 1.
Flowchart diagram showing results of the electronic search, screening of studies against the inclusion criteria for eligibility, and final number of included studies
Table 2.
Characteristics of reviewed studies
| References | Year | Country | Database | Period | Size | Follow-up years | Age | Male (%) | Cases | Controls | Exposure |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case–control studies (N = 6) | |||||||||||
| Azoulay [15] | 2012 | UK | GPRD | 1988–2009 | 115,727 | 4.8 | 69 | 81 | 376 | 6,699 | Never/ever, cumulative dose, cumulative duration |
| Chang [39] | 2012 | Taiwan | NHIRD | 2000–2007 | 606,583 | 7.9 | 71 | 67 | 1,583 | 6,308 | Never/ever, cumulative dose, cumulative duration |
| Song [17] | 2012 | South Korea | Severance Hospital, Yonsei | 2005–2011 | 53,569 | NR | 69 | 84 | 329 | 658 | Never/ever |
| Hsiao [35] | 2013 | Taiwan | NHIRD | 1997–2008 | NR | 3.6 | 66 | 68 | 3,412 | 17,060 | Never/current/recent/past, cumulative duration |
| Kuo [40] | 2014 | Taiwan | NHIRD | 1997–2009 | 64,745 | NR | 70 | 62 | 259 | 1,036 | Never/ever, cumulative dose |
| Han [41] | 2016 | South Korea | NHIS-NSC | 2002–2013 | 47,738 | 7.9 | 70–79 | 81 | 85 | 850 | Never/ever |
| Nested case–control studies within cohort studies (N = 2) | |||||||||||
| Jin [34] | 2014 | South Korea | Severance Hospital, St. Mary | 2005–2011 | 113,193 | >2 | 69 | 55 | 208 | 620 | Never/ever > 6 months use |
| Lewis [25] | 2015 | USA | KPNC | 1997–2012 | 193,099 | 6 | 70–79 | 85 | 464 | 464 | Never/ever, cumulative dose, cumulative duration |
| Cohort studies (N = 12) | |||||||||||
| Mamtami [42] | 2012 | UK | THIN | 2000–2010 | 28,514 | Pio: 2.4, no pio: 4.4 | 62 | 57 | 127 | Never/ever, cumulative duration | |
| Neumann [14] | 2012 | France | PMSI-SNIIRAM | 2006–2009 | 1,491,060 | 3.1 | 63 | 53 | 2,016 | Never/ever, cumulative dose, cumulative duration | |
| Tseng [43] | 2012 | Taiwan | NHI | 2006–2009 | 54,928 | <4 | NR | NR | 165 | Never/ever, cumulative dose, cumulative duration | |
| Wei [44] | 2013 | UK | GPRD | 2001–2010 | 207,714 | Pio: 3.5, no pio: 5.3 | 65 | 54 | 869 | Never/ever | |
| Vallarino [45] | 2013 | USA | i3 InVision Data Mart | 2000–2010 | 56,536 | Pio: 2.2, no pio: 1.9 | 59 | 57 | 128 | Never/ever | |
| Jin [34] | 2014 | South Korea | Severance Hospital, St. Mary | 2005–2011 | 113,193 | 3.8 | 63 | 53 | 267 | Never/ever | |
| Lee [46] | 2014 | Taiwan | NHI | 2003–2009 | 34,970 | NR | >60 | 48 | 84 | Never/ever, cumulative dose, cumulative duration | |
| Levin [24] | 2015 | Canada, Europe | Several | 1999 – | 1,007,596 | 4.0–7.4 | 60–64 | 50–56 | 3,248 | Never/ever, cumulative duration | |
| Scotland | 252,269 | 5.7 | 64 | 54 | 797 | ||||||
| England | CPRD | 156,443 | 5.2 | 64 | 54 | 599 | |||||
| Finland | 426,767 | 5.1 | 64 | 51 | 1,329 | ||||||
| Canada | British Columbia | 153,862 | 4 | 61 | 53 | 472 | |||||
| Netherlands | Rotterdam | 6,694 | 5.4 | 64 | 50 | 15 | |||||
| England | Manchester | 11,561 | 7.4 | 60 | 56 | 36 | |||||
| Lewis [25] | 2015 | USA | KPNC | 1997–2012 | 193,099 | Pio: 6.1, no pio: 7.2 | 60 | 53 | 1,261 | Never/ever, cumulative dose, cumulative duration | |
| Korhonen [27] | 2016 | Europe (FIN, SWE, UK, NL) | Several | 2000–2011 | 112,674 | Pio: 2.9, no pio: 2.8 | 64 | 54 | 183 | Never/ever, cumulative dose, cumulative duration | |
| MacKenzie [36] | 2016 | USA | Medicare | 2006–2012 | Prev.: 1,161,443 Incid.: 320,090 |
Prev.: 3.5 Incid.: 3.1 |
Prev.: 75 Incid: 77 |
Prev.: 38 Incid.: 38 |
Prev.: 4,433 Incid.: 1,159 |
Cumulative duration | |
| Tuccori [26] | 2016 | UK | CPRD | 2000–2014 | 145,806 | 4.7 | 64 | 57 | 622 | Never/ever, cumulative dose, cumulative duration | |
| Excluded studies (N = 5) | |||||||||||
| References | Year | Country | Database | Period | Size | Reason for exclusion | |||||
| Lewis [12] | 2011 | USA | KPNC | 1997–2008 | 193,099 | Interim analysis of a more recent study | |||||
| Piccini [11] | 2011 | USA | FDA AERS | 2004–2009 | NA | Case report without possibility to adjust for any confounders | |||||
| Fujimoto [16] | 2012 | Japan | MRI Kitano hospital | 2000–2011 | 21,335 | Not adjusted for any confounders | |||||
| Balaji [47] | 2014 | India | NR | NR | 1077 | Case report without possibility to adjust for any confounders | |||||
| Lewis [48] | 2014 | USA | KPNC | 2000–2010 | 193,099 | Interim analysis of a more recent study | |||||
NR not reported, Pio. Pioglitazone exposed, No pio no pioglitazone exposure, Prev. prevalent cases, Incid. incident cases
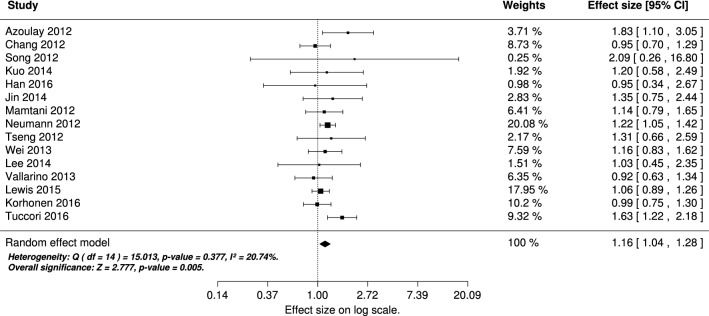
Figure 2 shows the association estimates between ever vs. never use of pioglitazone and bladder cancer among the individual studies, and the overall effect derived using a random-effects model in the meta-analysis (effect size, 1.16; 95%, CI 1.04–1.28). The figure also presents the heterogeneity assessment, which indicated no heterogeneity across individual studies (I2 = 21%, p = 0.377).
Fig. 2.
Meta-analysis results for the association of ever exposure (vs. never) to pioglitazone and bladder cancer. Studies included in the meta-analysis are shown with the adjusted risk estimates, 95% confidence interval (CI), and the relative weight in the meta-analysis. The meta-analysis result was derived using a random effect model
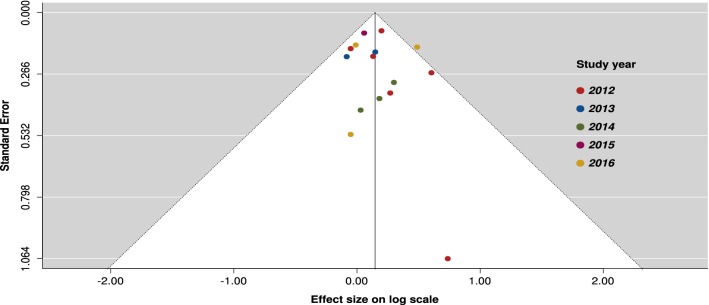
Figure 3 shows the funnel plot assessing possible publication bias among individual studies. Overall, the figure does not indicate clear asymmetry, i.e., publication bias. The regression test for asymmetry yielded test statistic z = 0.58 with a p value of 0.565. The rank correlation test yielded Kendall’s tau value of 0.03 with a p value of 0.923. Based on these results, there was no sign of publication bias.
Fig. 3.
Funnel plot of studies included in the meta-analysis assessing the association of ever exposure (vs. never) of pioglitazone use and bladder cancer
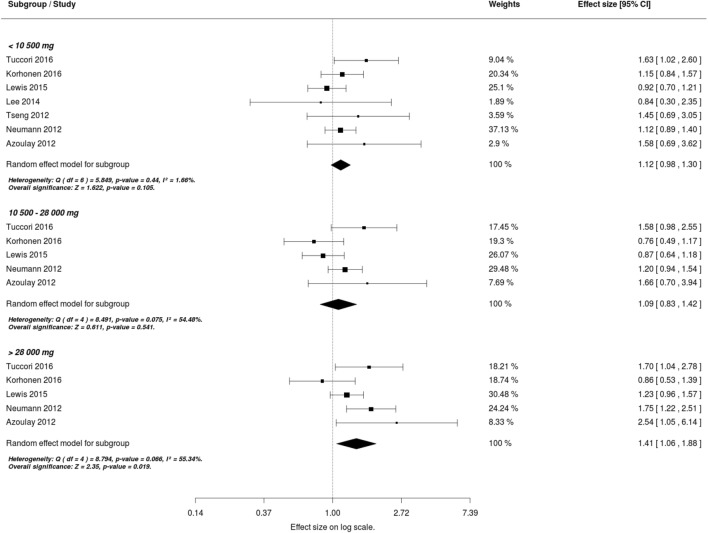
Figure 4 shows the estimates of association between cumulative dose of pioglitazone exposure and bladder cancer among the individual studies and the overall effect derived using a random-effects model. Among cumulative exposure categories < 10,500, 10,500–28,000, and > 28,000 mg, the overall effect size for risks of bladder cancer against never use were 1.12 (95%, CI 0.98–1.30), 1.09 (95% CI, 0.83–1.42), and 1.41 (95% CI, 1.06–1.88), respectively. In contrast to ever exposure (Fig. 2) and < 10,500 mg (Fig. 4, upmost part) exposure categories, substantial heterogeneity was found in the 10,500–28,000 and > 28,000 mg groups (I2 = 54%, p = 0.075 and I2 = 55%, p = 0.066, respectively).
Fig. 4.
Meta-analysis results for the association of cumulative dose exposure (vs. never use) to pioglitazone and bladder cancer. Studies included in the meta-analysis are shown with the adjusted risk estimates, 95% CI and the relative weight in the meta-analysis. The meta-analysis results were derived using a random effect model
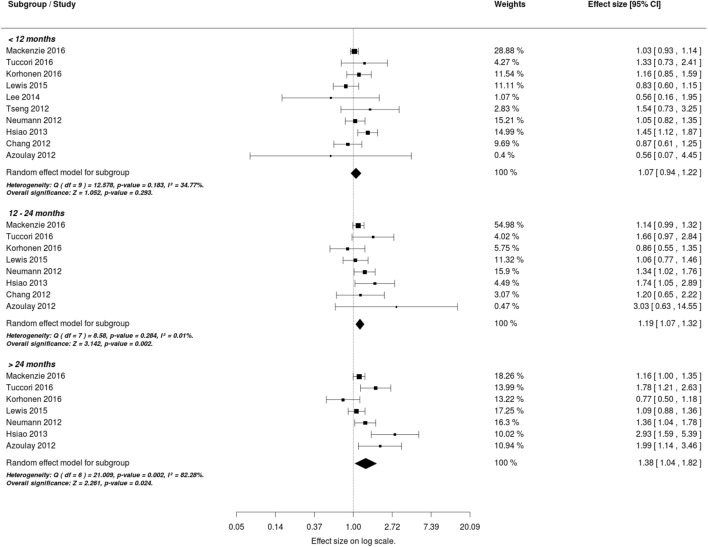
Figure 5 shows the estimates of association between cumulative duration of pioglitazone exposure and bladder cancer among the individual studies, and the overall effect derived using a random-effects model. Among cumulative duration categories < 12 months, 12–24 months, and > 24 months, the overall effect sizes for risks of bladder cancer against never use were 1.07 (95% CI, 0.94–1.22), 1.19 (95% CI, 1.07–1.32), and 1.38 (95% CI, 1.04–1.82), respectively. Substantial heterogeneity was only found in the > 24 months exposure group across individual study results (I2 > 82%, p = 0.002).
Fig. 5.
Meta-analysis results for the association of cumulative exposure duration (vs. never use) random to pioglitazone and bladder cancer. Studies included in the meta-analysis are shown with the adjusted risk estimates, 95% CI, and the relative weight in the meta-analysis. The meta-analysis results were derived using a random-effects model
Sensitivity analyses
In sensitivity analysis 1, all studies that were unable to adjust for lifestyle-related factors such as smoking and obesity were excluded. In addition, the result from the Korhonen study [27] adjusted for these factors (all countries not included, HR, 0.83; 95% CI, 0.54–1.28) was used. The effect size in this analysis was similar to that in the original primary analysis (effect size, 1.18; 95% CI, 1.00–1.40), but the treatment effect size was not statistically significant (p = 0.054). Full results are presented in Supplementary Fig. 1.
In sensitivity analysis 2 (Supplementary Fig. 2), the Bayesian random-effects model yielded similar results to the original primary approach.
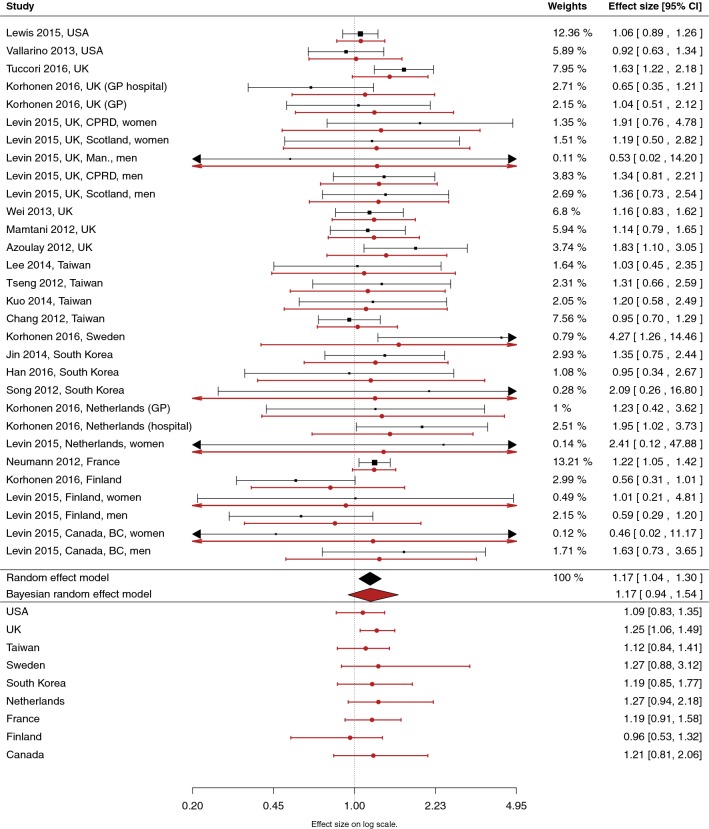
The results from sensitivity analysis 3 are shown in Fig. 6. In a hierarchical Bayesian model, the overall effect size had similar magnitude (effect size, 1.17) to the primary analysis, but the 95% credible interval [CrI]: (0.94–1.54) crossed 1.0. Country-specific effects in this analysis resulted in overlapping posterior CrIs with small differences in the posterior median. The Netherlands and Sweden had the highest posterior median value (1.27) and Finland the lowest (0.96). From the nine country-specific effects, only the UK had a 95% posterior CrI that did not cross with 1.
Fig. 6.
Bayesian hierarchical random-effects meta-analysis results for the association of ever (vs. never) use of pioglitazone and bladder cancer. The Bayesian model involves study and country-specific hierarchical levels. The Bayesian posterior median and 95% credible interval for the individual studies, country-level effects, and for the overall effect are shown in red. Original individual study results and the (frequentist) random-effects meta-analysis results are shown in black
Sensitivity analysis 4, using a fixed-effect model, yielded a similar association of ever use of pioglitazone and bladder cancer (effect size, 1.16; 95% CI, 1.04–1.28) to the original random-effects model.
In the primary analysis, two studies that had only cumulative exposure results [35, 36]. and one study reporting results separately for men and women [24] were excluded. In sensitivity analysis 5, the results within these studies were combined using a fixed-effect model. After this, the original random-effects meta-analysis was re-performed with a result of 1.19 (95% CI, 1.08–1.32), similar to the original primary analysis. However, in the three studies that were originally excluded, the effect size after combining results using a fixed-effect model were generally higher than in other studies. This also led to moderate heterogeneity across studies (I2 = 50%, p = 0.039). Full results are presented in Supplementary Fig. 3.
In sensitivity analysis 6, random-effects meta-analysis was performed separately for case–control and cohort studies (Supplementary Fig. 4). The overall effect size for case–control studies (effect size: 1.20; 95% CI, 0.95–1.52) was higher than those among cohort studies (effect size: 1.15; 95% CI, 1.04–1.28). However, the confidence interval for the overall effect among case–control studies was clearly wider (p = 0.128) than among cohort studies (p = 0.007).
Discussion
In this review, we included 23 studies and 18 studies in the actual meta-analyses. For the bladder cancer outcome, the estimated overall effect size for ever vs. never use of pioglitazone was 1.16 (95% CI, 1.04–1.28). In the sensitivity analysis excluding studies that did not adjust for lifestyle-related factors the treatment effect size was 1.18 (95% CI, 1.00–1.40), but the result was no longer statistically significant (p = 0.054). These new results are in line with a previously published meta-analysis [21] that covered 8 of the 18 studies included in this analysis showing a small but significant association between pioglitazone use and bladder cancer with an effect size of 1.21 (95% CI, 1.09–1.35).
A major challenge for meta-analyses studying pioglitazone use and bladder cancer risk is inclusion of overlapping studies, i.e., a potential duplication of some individuals in several studies that have used the same database. As a result, spurious associations and bias may arise if overlap between studies is not controlled for. To account for this challenge, a Bayesian random-effects model with study country as one extra level of hierarchy was utilized (sensitivity analysis 3). The effect size of the Bayesian analysis was 1.17 (95% CrI, 0.94–1.54, crossing 1.0). In our view, this approach provides a sound solution to account for the possible correlation between studies caused by the overlapping subjects; thus, our results become more robust and precise.
To put the results into perspective, it is important to consider the strength of an association. Generally accepted values by epidemiologists show that an RR of 1–2 is a ‘weak’ or ‘small’ association, 2–4 a ‘moderate’ association, and 5 or larger a ‘strong’ association [37]. The observed association between pioglitazone exposure and bladder cancer risk in the ever vs. never use of pioglitazone meta-analysis was less than 2 and found to be relatively small (16%); thus, can be considered a weak/small association. Since the effect size was small and the bladder cancer outcome rare, this type of association may be difficult to observe, even in a large single study.
It is also important to note that the meta-analytic method provides evidence extracted and integrated from a number of primary observational studies, not from a random sampling. Hence, causality is not established and alternative explanations cannot be ruled out [38].
Systematic reviews and meta-analyses can provide credible and consistent evidence relevant to questions of interest. The conclusions from meta-analysis are especially clear when the results of the included studies show clinically important effects of similar magnitude. The conclusions are much less clear, however, when the included studies have differing results. The degree of heterogeneity across individual study results was found to increase by cumulative duration and cumulative exposure of pioglitazone. In the cumulative dose and duration analyses, the high I2 value shows that most of the variability across studies is due to heterogeneity rather than chance. In addition, the number of studies included in the cumulative dose analysis was only 5. These factors reduce the confidence of the estimated effect sizes and reduce the degree to which conclusions might be generalized to situations outside of these investigated studies.
This study has several strengths. This is one of the largest and most comprehensive meta-analysis of observational studies evaluating a potential bladder cancer risk with pioglitazone use both in terms of number of studies and sample size. We also investigated cumulative dose and duration. Furthermore, we conducted several specific sensitivity analyses. However, there are also some limitations. First, in our analysis we focused and included only observational studies since randomized controlled trials are difficult to conduct because of the rarity of bladder cancer incidence. Second, the evidence and conclusions generated by this meta-analysis strongly depend on the quality of the studies identified and included to estimate the pooled effect. For instance, many previous individual observational studies did not account for all parameters known to be associated with bladder cancer, such as smoking and occupational exposures, and thus might have substantially confounded the presented study results as meta-analyses cannot resolve confounding factors. Third, details on cumulative dose and duration of pioglitazone therapy were not complete in several included studies, thus restricting those results to a subset of the studies.
Conclusions
In line with previous meta-analyses, we observed a small but statistically significant association between ever (vs. never) use of pioglitazone and bladder cancer risk; however, causality is not established and one cannot rule out alternative explanations. In the cumulative dose and duration analyses, the highest effect size was observed in the highest/longest exposure group, but substantial heterogeneity across individual studies was present. Importantly, when studies without adjustment for lifestyle factors were excluded, the effect size was not statistically significant. Also, when the imbalance in number of studies per country/overlap in subjects was addressed in the Bayesian sensitivity analysis, the 95% CrI of the treatment effect size crossed 1.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This study was sponsored by Takeda Pharmaceuticals Company Limited.
Author contributions
DB and YY conceived and designed the study and wrote a first protocol outline. JM, HK, PK, and FH critically reviewed the outline and developed a full protocol. JM, HK, PK, YY, and FH participated in the development of the literature search strategy, conducted literature search, and abstracted and compiled the data. JM, HK, PK, and FH performed the analyses. All authors participated in the discussion and interpretation of the study findings. JM, HK, PK, and FH drafted the manuscript. All authors critically reviewed, revised, and approved the final version submitted for publication.
Conflict of interest
YY and DB are employees of Takeda Pharmaceutical Company Limited. JM, HK, FH, and PK are employees of EPID Research Oy, which is a contract research organization that performs commissioned pharmacoepidemiologic studies, and thus its employees have been and currently are working in collaboration with several pharmaceutical companies.
Ethics approval
This systematic literature review does not involve any animal or human subjects, including research on identifiable human material and data.
References
- 1.World Health Organization. Global Report on Diabetes. 2016. http://apps.who.int/iris/bitstream/10665/204871/1/9789241565257_eng.pdf?ua=1. Accessed 23 Aug 2016.
- 2.Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed 23 Aug 2016.
- 3.American Diabetes Association Economic Costs of Diabetes in the US in 2012. Diabetes Care. 2013;36:1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeFronzo RA, Banerji M, Bray GA, et al. Actos now for the prevention of diabetes (ACT NOW) study. BMC Endocr Disord. 2009 doi: 10.1186/1472-6823-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeFronzo RA, Tripathy D, Schwenke DC, et al. Pioglitazone for diabetes prevention in impaired glucose tolerance. N Engl J Med. 2011;364:1104–1115. doi: 10.1056/NEJMoa1010949. [DOI] [PubMed] [Google Scholar]
- 6.Kipnes MS, Krosnick A, Rendell MS, et al. Pioglitazone hydrochloride in combination with sulfonylurea therapy improves glycemic control in patients with type 2 diabetes mellitus: a randomized, placebo-controlled study. Am J Med. 2001;111:10–17. doi: 10.1016/S0002-9343(01)00713-6. [DOI] [PubMed] [Google Scholar]
- 7.Einhorn D, Rendell M, Rosenzweig J, et al. Pioglitazone hydrochloride in combination with metformin in the treatment of type 2 diabetes mellitus: a randomized, placebo-controlled study. The Pioglitazone 027 Study Group. Clin Ther. 2000;22:1395–1409. doi: 10.1016/S0149-2918(00)83039-8. [DOI] [PubMed] [Google Scholar]
- 8.Rosenstock J, Einhorn D, Hershon K, et al. Efficacy and safety of pioglitazone in type 2 diabetes: a randomised, placebo-controlled study in patients receiving stable insulin therapy. Int J Clin Pract. 2002;56:251–257. [PubMed] [Google Scholar]
- 9.Schernthaner G, Matthews DR, Charbonnel B, et al. Efficacy and safety of pioglitazone versus metformin in patients with type 2 diabetes mellitus: a double-blind, Randomized Trial. J Clin Endocrinol Metab. 2004;89:6068–6076. doi: 10.1210/jc.2003-030861. [DOI] [PubMed] [Google Scholar]
- 10.Takeda Pharmaceuticals America, Inc. Actos (Pioglitazone Hydrochloride) Tablets: Full Prescribing Information. 2009. http://www.actos.com/actospro/home.aspx. Accessed 12 Aug 2016.
- 11.Piccinni C, Motola D, Marchesini G, Poluzzi E. Assessing the association of pioglitazone use and bladder cancer through drug adverse event reporting. Diabetes Care. 2011;34(6):1369–1371. doi: 10.2337/dc10-2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lewis JD, Ferrara A, Peng T, et al. Risk of bladder cancer among diabetic patients treated with pioglitazone: interim report of a longitudinal cohort study. Diabetes Care. 2011;34:916–922. doi: 10.2337/dc10-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tseng C-H. Pioglitazone and bladder cancer: a population-based study of Taiwanese. Diabetes Care. 2012;35:278–280. doi: 10.2337/dc11-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neumann A, Weill A, Ricordeau P, et al. Pioglitazone and risk of bladder cancer among diabetic patients in France: a population-based cohort study. Diabetologia. 2012;55:1953–1962. doi: 10.1007/s00125-012-2538-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Azoulay L, Yin H, Filion KB, et al. The use of pioglitazone and the risk of bladder cancer in people with type 2 diabetes: nested case-control study. BMJ. 2012;344:e3645. doi: 10.1136/bmj.e3645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fujimoto K, Hamamoto Y, Honjo S, et al. Possible link of pioglitazone with bladder cancer in Japanese patients with type 2 diabetes. Diabetes Res Clin Pract. 2013;99:e21–e23. doi: 10.1016/j.diabres.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Song SO, Kim KJ, Lee B-W, et al. The risk of bladder cancer in korean diabetic subjects treated with pioglitazone. Diabetes Metab J. 2012;36:371–378. doi: 10.4093/dmj.2012.36.5.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colmers IN, Bowker SL, Majumdar SR, et al. Use of thiazolidinediones and the risk of bladder cancer among people with type 2 diabetes: a meta-analysis. CMAJ Can Med Assoc J J Assoc Medicale Can. 2012;184:E675–E683. doi: 10.1503/cmaj.112102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bosetti C, Rosato V, Buniato D, et al. Cancer risk for patients using thiazolidinediones for type 2 diabetes: a meta-analysis. Oncologist. 2013;18:148–156. doi: 10.1634/theoncologist.2012-0302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferwana M, Firwana B, Hasan R, et al. Pioglitazone and risk of bladder cancer: a meta-analysis of controlled studies. Diabet Med. 2013;30:1026–1032. doi: 10.1111/dme.12144. [DOI] [PubMed] [Google Scholar]
- 21.Turner RM, Kwok CS, Chen-Turner C, et al. Thiazolidinediones and associated risk of bladder cancer: a systematic review and meta-analysis: thiazolidinediones and bladder cancer. Br J Clin Pharmacol. 2014;78:258–273. doi: 10.1111/bcp.12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu Z, Shen Z, Lu Y, et al. Increased risk of bladder cancer with pioglitazone therapy in patients with diabetes: a meta-analysis. Diabetes Res Clin Pract. 2012;98:159–163. doi: 10.1016/j.diabres.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 23.He S, Tang Y, Zhao G, et al. Pioglitazone prescription increases risk of bladder cancer in patients with type 2 diabetes: an updated meta-analysis. Tumour Biol J Int Soc Oncodevelopmental Biol Med. 2014;35:2095–2102. doi: 10.1007/s13277-013-1278-x. [DOI] [PubMed] [Google Scholar]
- 24.Levin D, Bell S, Sund R, et al. Pioglitazone and bladder cancer risk: a multipopulation pooled, cumulative exposure analysis. Diabetologia. 2015;58:493–504. doi: 10.1007/s00125-014-3456-9. [DOI] [PubMed] [Google Scholar]
- 25.Lewis JD, Habel LA, Quesenberry CP, et al. Pioglitazone use and risk of bladder cancer and other common cancers in persons with diabetes. JAMA. 2015;314:265. doi: 10.1001/jama.2015.7996. [DOI] [PubMed] [Google Scholar]
- 26.Tuccori M, Filion KB, Yin H, et al. Pioglitazone use and risk of bladder cancer: population based cohort study. BMJ. 2016;352:i1541. doi: 10.1136/bmj.i1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Korhonen P, Heintjes EM, Williams R, et al. Pioglitazone use and risk of bladder cancer in patients with type 2 diabetes: retrospective cohort study using datasets from four European countries. BMJ. 2016 doi: 10.1136/bmj.i3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Hippel PT. The heterogeneity statistic I 2 can be biased in small meta-analyses. BMC Med Res Methodol. 2015 doi: 10.1186/s12874-015-0024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 30.Higgins JPT. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis. J Clin Epidemiol. 2001;54:1046–1055. doi: 10.1016/S0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 32.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 33.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jin S-M, Song SO, Jung CH, et al. Risk of bladder cancer among patients with diabetes treated with a 15 mg pioglitazone dose in Korea: a multi-center retrospective cohort study. J Korean Med Sci. 2014;29:238. doi: 10.3346/jkms.2014.29.2.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hsiao F-Y, Hsieh P-H, Huang W-F, et al. Risk of bladder cancer in diabetic patients treated with rosiglitazone or pioglitazone: a nested case-control study. Drug Saf. 2013;36:643–649. doi: 10.1007/s40264-013-0080-4. [DOI] [PubMed] [Google Scholar]
- 36.Mackenzie TA, Zaha R, Smith J, et al. Diabetes pharmacotherapies and bladder cancer: a medicare epidemiologic study. Diabetes Ther. 2016;7:61–73. doi: 10.1007/s13300-016-0152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shapiro S. Causation, bias and confounding: a hitchhiker’s guide to the epidemiological galaxy part 2. Principles of causality in epidemiological research: confounding, effect modification and strength of association. J Fam Plann Reprod Health Care. 2008;34:185–190. doi: 10.1783/147118908784734873. [DOI] [PubMed] [Google Scholar]
- 38.Greco T, Zangrillo A, Biondi-Zoccai G, et al. Meta-analysis: pitfalls and hints. Heart Lung Vessels. 2013;5:219–225. [PMC free article] [PubMed] [Google Scholar]
- 39.Chang C-H, Lin J-W, Wu L-C, et al. Association of thiazolidinediones with liver cancer and colorectal cancer in type 2 diabetes mellitus. Hepatology. 2012;55:1462–1472. doi: 10.1002/hep.25509. [DOI] [PubMed] [Google Scholar]
- 40.Kuo H-W, Tiao M-M, Ho S-C, et al. Pioglitazone use and the risk of bladder cancer. Kaohsiung J Med Sci. 2014;30:94–97. doi: 10.1016/j.kjms.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 41.Han E, Jang S-Y, Kim G, et al. Rosiglitazone use and the risk of bladder cancer in patients with type 2 diabetes. Medicine (Baltimore) 2016;95:e2786. doi: 10.1097/MD.0000000000002786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mamtani R, Haynes K, Bilker WB, et al. Association between longer therapy with thiazolidinediones and risk of bladder cancer: a cohort study. JNCI J Natl Cancer Inst. 2012;104:1411–1421. doi: 10.1093/jnci/djs328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tseng C-H. Pioglitazone and bladder cancer: a population-based study of Taiwanese. Diabetes Care. 2012;35:278–280. doi: 10.2337/dc11-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wei L, MacDonald TM, Mackenzie IS. Pioglitazone and bladder cancer: a propensity score matched cohort study. Br J Clin Pharmacol. 2013;75:254–259. doi: 10.1111/j.1365-2125.2012.04325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vallarino C, Perez A, Fusco G, et al. Comparing pioglitazone to insulin with respect to cancer, cardiovascular and bone fracture endpoints, using propensity score weights. Clin Drug Investig. 2013;33:621–631. doi: 10.1007/s40261-013-0106-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee M-Y, Hsiao P-J, Yang Y-H, et al. The association of pioglitazone and urinary tract disease in type 2 diabetic Taiwanese: bladder cancer and chronic kidney disease. PLoS One. 2014;9:e85479. doi: 10.1371/journal.pone.0085479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Balaji V, Seshiah V, Ashtalakshmi G, et al. A retrospective study on finding correlation of pioglitazone and incidences of bladder cancer in the Indian population. Indian J Endocrinol Metab. 2014;18:425. doi: 10.4103/2230-8210.131223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lewis JD, Habel L, Quesenberry C, et al. Proteinuria testing among patients with diabetes mellitus is associated with bladder cancer diagnosis: potential for unmeasured confounding in studies of pioglitazone and bladder cancer: proteinuria and bladder cancer diagnosis. Pharmacoepidemiol Drug Saf. 2014;23:636–645. doi: 10.1002/pds.3619. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.