Abstract
Localized malignant pleural mesothelioma (LMPM) is an extremely rare tumor. We report the case of a 40-year-old Japanese male with an LMPM mimicking an anterior mediastinal tumor due to invasion to the anterior mediastinum, and we discuss mainly the differentiation of LMPM from an anterior mediastinal tumor. The present tumor had a long shape along the pleura, and LMPM could be one of the differential diagnoses.
Keywords: Pleural mesothelioma, Localized, Pleural tumor, Radiology, LMPM
1. Introduction
Localized malignant pleural mesothelioma (LMPM) was first reported by Crotty et al. in 1994 [1]. The World Health Organization (WHO) classified LMPM as a distinct diagnosis in the 2004 WHO Classification of Tumors of the Pleura. LMPM is defined as a localized nodular lesion with no diffused invasion, both macroscopically and microscopically. In terms of histology and immunohistology as well as microstructure, no significant differences are observed between localized (LMPM) and diffuse malignant pleural mesothelioma (DMPM) [2]. We report a case of LMPM mimicking an anterior mediastinal tumor due to invasion to anterior mediastinum and discuss mainly about differentiation from an anterior mediastinal tumor.
2. Case report
A 40-year-old Japanese man underwent an annual medical check-up, and an abnormal shadow was detected on his chest radiograph. A CT examination revealed an anterior mediastinal mass. The patient was referred to our hospital for further assessment. Contrast-enhanced CT demonstrated a multi-nodular and heterogeneous mass 5.4 cm in max. dia. located mainly in the anterior mediastinum (Fig. 1). The mass was broadly adjacent to the pleura and right lung, suggesting invasion.
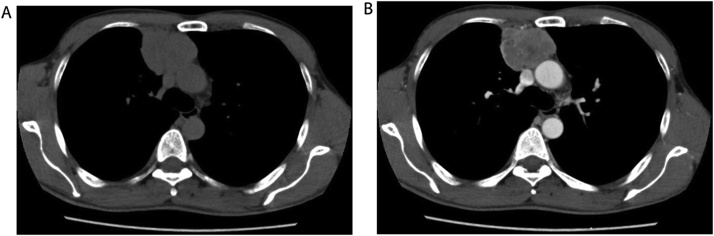
Fig. 1.
Axial view of pre-contrast (a) and contrast-enhanced (b) CT demonstrated a multi-nodular tumor with heterogeneous enhancement in the anterior mediastinum.
An MR examination was performed with a 1.5-T scanner. The mass showed isointensity relative to muscles on T1-weighted images (Fig. 2a) and hypointensity on T2-weighted images (Fig. 2b). Diffusion-weighted imaging (DWI) was performed using a multisection spin-echo single-shot echo-planar sequence in the axial plane with b-values of 0, 500, and 1000s/mm2. Thereafter, apparent diffusion coefficient (ADC) maps were generated. This lesion showed hyperintensity on the DWI (Fig. 2c), and the ADC values ranged from 0.7 to 0.9 × 0.10−3 mm2/s (Fig. 2d).
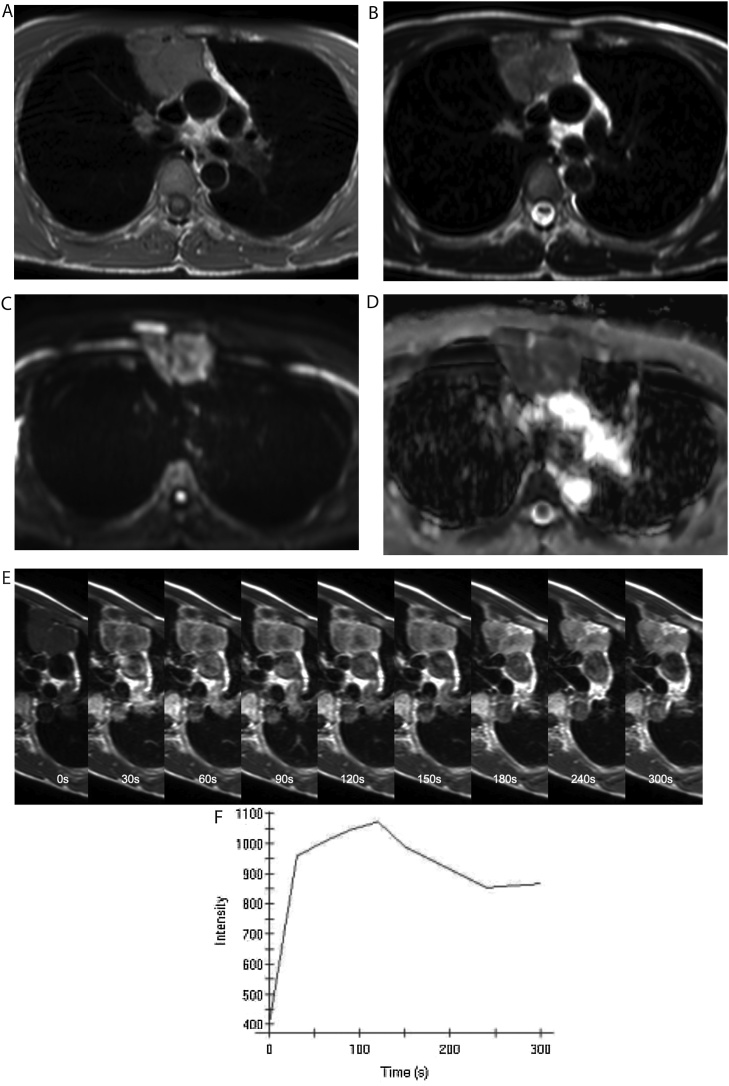
Fig. 2.
MRI revealed a mass with iso-signal intensity relative to muscles on a T1-weighted image (a) and low signal intensity on a T2-weighted image (b). This lesion showed hyperintensity on DWI with a b-value of 1000s/mm2 (c), and the ADC values ranged from 0.7 to 0.9 × 10−3 mm2/s (d). The dynamic contrast-enhancement study revealed a rapid-plateau pattern (e,f).
For a dynamic contrast-enhancement study, gadopentetate dimeglumine (0.2 mL/kg of body weight) was administered intravenously at a rate of 2 mL/s. MR images were sequentially obtained before and every 30 s for 5 min after the contrast material administration. Regions of interest (ROIs) were manually drawn for signal intensity measurement. We then plotted the average signal intensity within the ROI against time, and a time-intensity curve (TIC) was constructed which revealed a rapid-plateau pattern (Fig. 2e,f). An 18-fluorodeoxyglucose (FDG)-PET examination revealed abnormal uptake in this tumor with a maximal standardized uptake (SUVmax) value of 9.66 (Fig. 3). No other lesion was observed at any site.
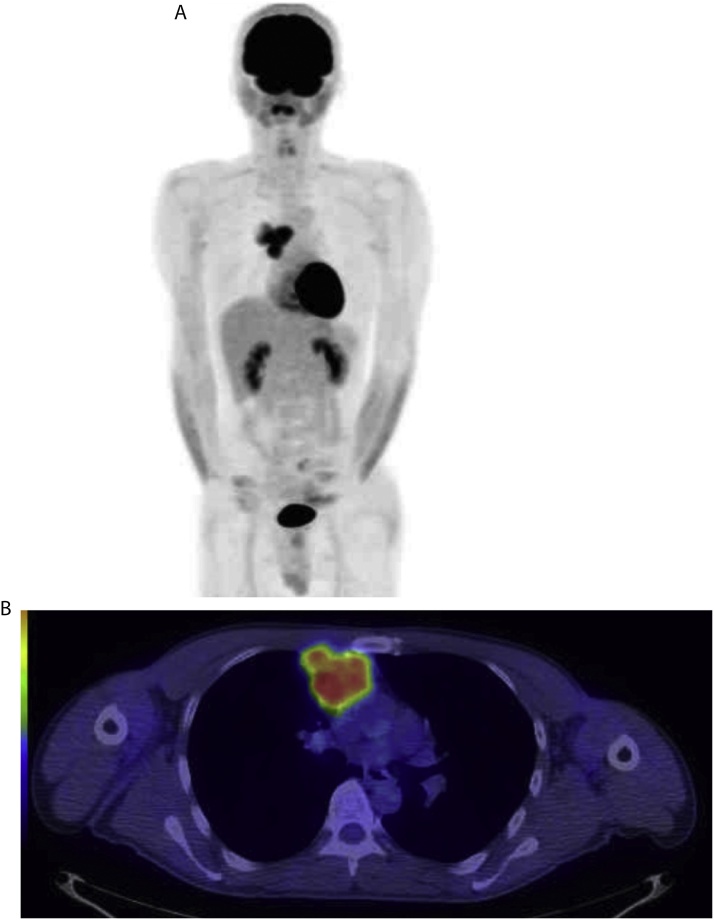
Fig. 3.
18F-FDG-PET/CT showed a high accumulation of FDG with a maximum standardized uptake value of 9.88 (a). No other abnormal uptake was observed (b).
From these findings, the differential diagnosis included mediastinal tumors such as invasive thymoma, thymic cancer, and malignant lymphoma. A CT-guided biopsy was performed, and adenocarcinoma was suspected. Immunohistochemically, the tumor cells were negative for the markers TTF-1 and Napsin A. These results are not consistent with lung adenocarcinoma. Based on the diagnosis of thymic cancer, neoadjuvant chemoradiotherapy was performed: 40 Gy, 2.0 Gy per fraction (20 fractions); CBDCA AUC6 and PTX, 45 mg/m2 daily, 4 days per week. However, significant volume reduction of the tumor was not obtained.
Surgical resection followed the chemoradiotherapy. The tumor displaced a normal thymus and infiltrated to the pericardium, rib, and right lung. Histopathologically, both epithelioid and sarcomatous components were identified (Fig. 4). The pleura adjacent to the tumor were thickened pathologically. On immunohistochemistry, AE1/AE3, vimentin, CAM2.5, calretinin, D2-40, and thrombomodulin were positive, but TTF-1, Napsin, S-100, CD5, and alpha-SM actin were negative. Thus, the diagnosis of malignant pleural mesothelioma with a biphasic pattern was pathologically confirmed.
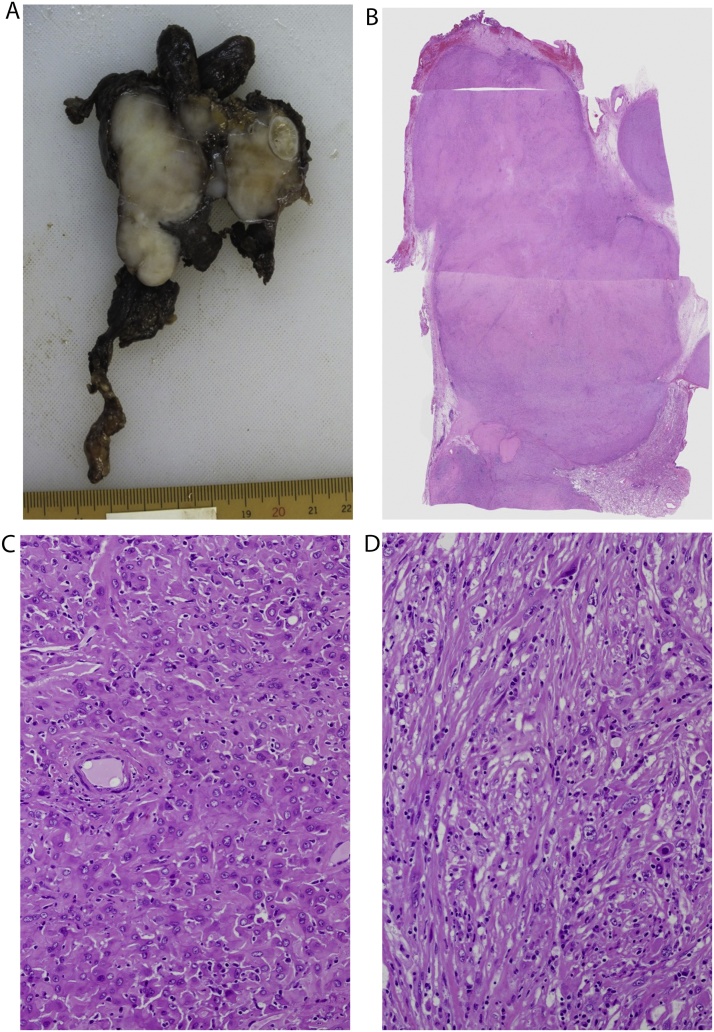
Fig. 4.
Macroscopically, the tumor was circumscribed and solid. Partial infiltration toward the right upper lobe was observed (a,b). Microscopically, polygonal, spindle, or epithelioid-shaped cells with bizarre nuclei proliferated in a sheet, storiform, or fascicular pattern. Fibrous, hyalinized and myxomatous stroma was also seen. Both epithelioid (c) and sarcomatous (d) components were observed. These findings indicated a malignant mesothelioma with a biphasic pattern.
A small nodule was observed in the anterior mediastinum on CT performed 12 months after the tumor's resection. At 18 months after the surgery, the size of the nodule had increased, and it was considered to be local recurrence. Chemotherapy (CDDP and PEM) was administered, but a suppression of the nodule's increase could not be obtained. The recurrent nodule/tumor was still progressive, and pleural dissemination arose. The patient died 44 months after the original surgery.
3. Discussion
LMPM is a rare tumor; about 50 cases have been reported [3]. The mean age of the reported LMPM patients is early 60 s. This tumor has rarely occurred before the age of 40 years. More than 90% of localized malignant melanomas arise from the pleura, but a few cases have originated from the peritoneum. The sex ratio of the reported cases is approx. 2:1 (male/female) [4]. Only about 20%–40% of cases involved asbestos exposure, but this rate might have been underestimated due to an obscure medical history or delayed onset [4,5].
LMPM is often found unexpectedly with nonspecific symptoms such as chest pain, dyspnea, malaise, fever, and night sweats, which can cause the misdiagnosis of other respiratory disease [4,6]. LMPMs show frequent local recurrence or distant metastasis. The reported overall survival of patients with an LMPM ranges from 8 months to several years. This survival rate is much better than that of DMPM (5–7months) [3,4,7].
Chest high-resolution CT scan is the most common modality for the assessment of LMPMs [8]. LMPM is demonstrated as a circumscribed mass based on pleura. Although the internal characteristics of LMPMs vary, the large mass tends to be heterogeneous on contrast-enhanced CT. This may reflect the degree of necrosis or degeneration [[9], [10], [11]]. Pleural plaques were observed in 20% of patients with MPM, but these details are unknown in LMPM [10]. Some cases showed cyst formation [12]. The median reported diameter of the LMPM mass is 5–6 cm; this tumor is sometimes found as a mass >10 cm [4,11]. LMPM is locally aggressive, and thus it can invade the chest wall, ribs, mediastinum, pericardium, and diaphragm. A CT scan cannot provide a definitive diagnosis but it is useful for identifying the tumor size, metastasis, and stage, and for guiding biopsy sites [13,14].
MRI is not routinely used to assess MPMs. The MR signals of an MPM are nonspecific. MPMs show iso-intensity or slight hyperintensity on T1-weighted images and moderately hyperintense on T2-weighted images. Delayed Gd-enhanced MRI is more useful in identifying the precise extent of the tumor or invasion [11]. Some reports described that early contrast enhancement was observed and peaked at 4.5 min. Although DWI for evaluating MPM has been used in a few studies, it is possible that a DWI histogram is useful for evaluating the tumor's response to treatment [15].
FDG-positron emission tomography CT can predict lymph node and distant metastasis or recurrence better than other modalities. It has higher sensitivity and specificity for staging, especially for patients whose tumor is at an advanced stage [[16], [17], [18]]. Although the cut-off value of the SUVmax for LMPM has not been determined, some studies have reported that malignant pleural disease (including MPMs) showed higher SUVmax values [19,20]. It was also reported that the SUVmax was related to the overall survival of patients with MPM [21].
The differential diagnosis of LMPM includes other pleural tumors such as solitary fibrous tumor, synovial sarcoma, and epithelioid angiosarcoma. If an LMPM invades the anterior mediastinum, it can mimic a mediastinal mass as in our patient's case [13,22]. We suspected that his tumor was an anterior mediastinal tumor and did not originally consider the possibility of a pleural tumor. We thus sent the specimen from the CT-guided biopsy to the pathologists as an anterior mediastinal tumor, and the pathological diagnosis was suspicious for thymic adenocarcinoma. If we had mentioned the possibility of a pleural tumor, a correct diagnosis could have been obtained based on the CT-guided biopsy results.
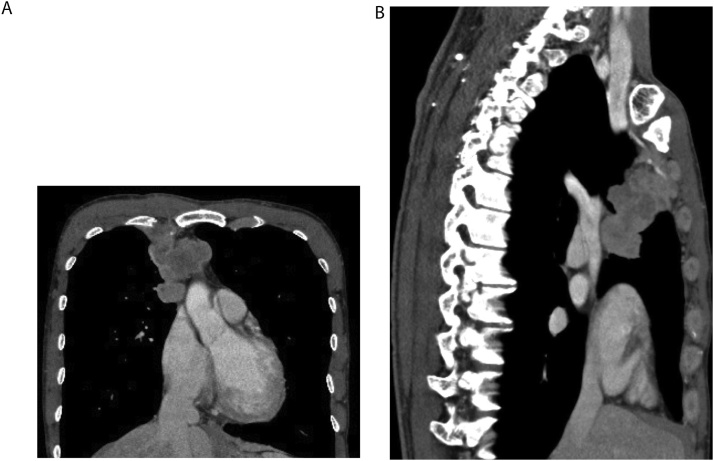
Retrospectively, this tumor was vertically long along the right pleura. The additionally reconstructed curved multi-planer reconstruction CT images demonstrated the multinodular mass with a long shape along the right pleura (Fig. 5). We suspect that this shape is atypical for mediastinal tumors and might be helpful for the differentiation of LMPMs from mediastinal tumors.
Fig. 5.
Curved-MPR views of contrast-enhanced CT demonstrated the multinodular mass with a long shape along the right pleura.
In conclusion, we have described the imaging features of a case of LMPM mimicking an anterior mediastinal tumor. LMPM should be considered in the differential diagnosis of a mediastinal mass with a long shape along the pleura. Multi-planar views might be useful for the diagnosis of LMPM.
Conflict of interest
The authors have no conflicts of interest or financial support associated with this manuscript.
References
- 1.Crotty T.B., Myers J.L., Katzenstein A.L., Tazelaar H.D., Swensen S.J., Chrug A. Localized malignant mesothelioma. A clinicopathologic and flow cytometric study. Am. J. Surg. Pathol. 1994;18:357–363. https://www.ncbi.nlm.nih.gov/pubmed/7511353 [PubMed] [Google Scholar]
- 2.Travis W.D., Brambilla E., Burke A.P., Marx A., Nicholson A.G. 4th ed. 2015. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart. [DOI] [PubMed] [Google Scholar]
- 3.Gelvez-Zapata S.M., Gaffney M., Scarci M., Cooner A.S. What is the survival after surgery for localized malignant pleural mesothelioma? Interact. Cardiovasc. Thorac. Surg. 2003;16:533–537. doi: 10.1093/icvts/ivs542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allen T.C., Cagle P.T., Churg A.M., Colby T.V., Gibbs A.R., Hammar S.P., Corson J.M., Grimes M.M., Ordonez N.G., Roggli V., Travis W.D., Wick M.R. Localized malignant mesothelioma. Am. J. Surg. Pathol. 2005;29:866–873. doi: 10.1097/01.pas.0000165529.78945.dc. https://insights.ovid.com/crossref?an=00000478-200507000-00003 [DOI] [PubMed] [Google Scholar]
- 5.Asioli S., Dal Piaz G., Damiani S. Localised pleural malignant mesothelioma. Report of two cases simulating pulmonary carcinoma and review of the literature. Virchows Arch. 2004;445:206–209. doi: 10.1007/s00428-004-1062-9. [DOI] [PubMed] [Google Scholar]
- 6.British Thoracic Society Standards of Care Committee BTS statement on malignant mesothelioma in the UK, 2007. Thorax. 2007;62:ii1–ii19. doi: 10.1136/thx.2007.087619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim K.C., Ko H.P. Localized malignant pleural sarcomatoid mesothelioma misdiagnosed as benign localized fibrous tumor. J. Thorac. Dis. 2016;8:E379–84. doi: 10.21037/jtd.2016.03.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samuel G.A., 3rd, Ee Labby Z., Coolen J., Klabatsa A., Feigem M., Persigehl T., Gill R.R. Imaging in pleural mesothelioma: a review of the 11th international conference of the international mesothelioma interest group. Lung Cancer. 2013;32:190–196. doi: 10.1016/j.lungcan.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Nakano T., Hamanaka R., Oiwa K., Nakazato K., Masuda R., Iwazaki M. Localized malignant pleural mesothelioma. Gen. Thorac. Cardiovasc. Surg. 2012;60:468–474. doi: 10.1007/s11748-012-0025-3. [DOI] [PubMed] [Google Scholar]
- 10.Erdogan E., Demirkazik F.B., Guslin M., Ariyurek M., Emri S., Sak S.D. Incidental localized (solitary) mediastinal malignant mesothelioma. BJR. 2005;78:858–861. doi: 10.1259/bjr/19513813. [DOI] [PubMed] [Google Scholar]
- 11.Yao W., Yang H., Huang G., Yan Y., Wang H., Sun D. Massive localized malignant pleural mesothelioma (LMPM): manifestations on computed tomography in 6 cases. Int. J. Clin. Exp. Med. 2015;8:18367–18374. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4694340/pdf/ijcem0008-18367.pdf [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Z.F., Reddy G.P., Gotway M.P., Higgins C.B., Jablons D.M., Ramaswamy M., Hawkins R.A., Webb W.R. Malignant pleural mesothelioma: evaluation with CT, MR imaging and PET. Radiographics. 2004;24:105–119. doi: 10.1148/rg.241035058. [DOI] [PubMed] [Google Scholar]
- 13.Hassan I., Goolam-Mahomed A. An unusual cause of anterior mediastinal mass. Respir. Med. Case Rep. 2014;12:52–54. doi: 10.1016/j.rmcr.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scherpereela A. French speaking society for chest medicine (SPLF) experts group. Guidelines of the French speaking society for chest medicine for management of malignant pleural mesothelioma. Respir. Med. 2007;101:1265–1276. doi: 10.1016/j.rmed.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Armato S.G., 3rd, Blyth K.G., Keating J.J., Katz S., Tsim S., Coolen J., Gudmundsson E., Opitz I., Nowak A.K. Imaging in pleural mesothelioma: a review of the 13th International Conference of the International Mesothelioma Interest Group. Lung cancer. 2016;101:48–58. doi: 10.1016/j.lungcan.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharif S., Zahid I., Routledge T., Scarci M. Does positron emission tomography offer prognostic information in malignant pleural mesothelioma? Interact. Cardiovasc. Thorac. Surg. 2011;12:806–811. doi: 10.1510/icvts.2010.255901. [DOI] [PubMed] [Google Scholar]
- 17.Basu S., Saboury B., Torigian D.A., Alavi A. Current evidence base of FDG-PET/CT imaging in the clinical management of malignant pleural mesothelioma: emerging significance of image segmentation and global disease assessment. Mol. Imaging Biol. 2011;13:801–811. doi: 10.1007/s11307-010-0426-6. [DOI] [PubMed] [Google Scholar]
- 18.van Zandwijk N., Clarke C., Henderson D., Musk A.W., Fong K., Nowak A., Loneragan R., McCaughan B., Boyer M., Feigen M., Currow D., Schofield P., Nick Pavlakis B.I., McLean J., Marshall H., Leong S., Keena V., Penman A. Guidelines for the diagnosis and treatment of malignant pleural mesothelioma. J. Thorac. Dis. 2013;5:E254–E307. doi: 10.3978/j.issn.2072-1439.2013.11.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dimarakis I., Rehman S., Machaal A., Shah R. PET-CT in the diagnosis of localized malignant pleural mesothelioma. Clin. Imaging. 2011;35:476–477. doi: 10.1016/j.clinimag.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Kadota K., Kachala S.S., Nitadori J., Suzuki K., Dunphy M.P., Sima C.S., Travis W.D., Rusch V.W., Adusumilli P.S. High-SUVmax on FDG-PET indicates pleomorphic subtype in epithelioid malignant pleural mesothelioma: supportive evidence to reclassify pleomorphic as non-epithelioid histology. J. Thorac. Oncol. 2012;7:1192–1197. doi: 10.1097/JTO.0b013e3182519d96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gerbaudo V.H., Mamede M., Trotman-Dickenson B., Hatabu H., Sugarbaker D.J. FDG PET/CT patterns of treatment failure of malignant pleural mesothelioma: Relationship to histologic type, treatment algorithm, and survival. Eur. J. Nucl. Med. Mol. Imaging. 2011;38:810–821. doi: 10.1007/s00259-010-1704-x. [DOI] [PubMed] [Google Scholar]
- 22.Inafuku T., Morohashi T., Adachi H., Koumori K., Tsuura Y., Masuda M. A resected case of localized malignant pleural mesothelioma that was preoperatively diagnosed as lung cancer. JJRC. 2016;56:1040–1045. (in Japanese) [Google Scholar]