Abstract
Background and aim of the work: Intramuscular paravertebral injections of ozone are minimally invasive, safe and efficacy in reducing pain and disability. The aim of this paper is to present the early results of paravertebral lumbar ozone injections in the treatment of low back pain. Methods: Between February 2011 and December 2015, a total of 109 patients underwent intramuscular paravertebral lumbar injections of ozone due to low back pain. Of them, 42 interrupted the treatment at a medium of 5.4 injections and were lost to follow-up. Of the 67 remaining patients, only 24 answered to our questionnaire. Local and radiating pain was assessed using a 10-cm horizontal Visual Analogue Scale. Perceived functional status and disability were evaluated using the Oswestry Disability Index, administered before treatment and one month after the last injection. Results: Visual Analogue Scale reduction was demonstrated in 23 out of 29 cycles (79%) of ozone therapy. Regarding disability evaluation, Oswestry Disability Index score reduction was assessed in all except one. No complications were recorded. Our results are similar to the other reports: 79% of patients had VAS reduction of 2.3 points and all except one patient reported ODI reduction (average reduction of 9%). Conclusions: Lumbar paravertebral oxygen-ozone injections are minimally invasive, safe, cheaper and effective in relieving pain as well as disability. This technique is easy to perform, it doesn’t need computed-tomography or anesthesiologist support. We suggest its application in low back pain as first choice to replace intradiscal computed-tomography-guided infiltrations and to avoid or delay surgery. (www.actabiomedica.it)
Keywords: low back pain, oxygen-ozone therapy, minimally invasive technique
Introduction
The efficacy of oxygen-ozone therapy in medicine is nowadays well defined and demonstrated in several fields, such as vascular diseases, infections, orthopedics and odontoiatry. Nevertheless, due to an improper empirical use by some practitioners, lack of standardization, ozone generators without appropriate photometer, and scarcity of scientific data, orthodox medicine tends to refuse ozone therapy.
The rational of its use is based on the exploitation of the chemical properties of ozone, an unstable allotropic form of oxygen. Ozone therapy has a direct (mechanical) and indirect (anti-inflammatory) effect (1). The direct effect consists in the lysis of the proteoglicans composing the disc’s nucleus pulposus, which results in the release of water molecules and the subsequent cell degeneration of the matrix, which is then replaced by fibrous tissue, leading to a reduced disc volume (2). The indirect effect is realized by altering the breakdown of arachidonic acid to inflammatory prostaglandins. As result, by reducing the inflammatory components, there is a subsequent decrease in pain (3).
Regarding its use in orthopedic field, ozone can be administered through several ways, such as intramuscular, intradiscal, intraforaminal and periradicular. Usually, except for intramuscular way, the other need to be computed-tomography (CT)-guided and to be performed with anesthesiologist support.
Intramuscular lumbar paravertebral injections of ozone are minimally invasive, safe and efficacy in reducing pain, as well as disability and intake of analgesic drugs (2). The aim of this paper is to present the early results of paravertebral lumbar ozone injections in the treatment of low back pain (LBP) caused by several pathologies, such as discal bulging, disk herniation (DH), spondylolisthesis and lumbar stenosis.
Methods
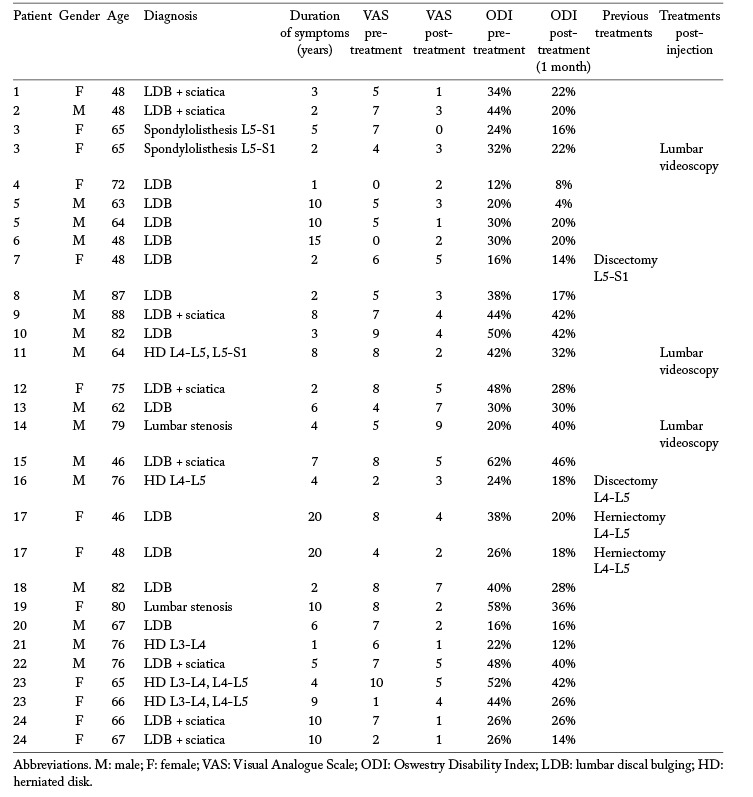
Between February 2011 and December 2015, a total of 109 patients underwent intramuscular paravertebral lumbar injections of ozone due to LBP. Of them, 42 interrupted the treatment at a medium of 5.4 injections and were lost to follow-up. Seventeen of them had a reduced VAS, 14 had an increased VAS and 11 were stable. Finally, a total of 67 patients completed the 12 injections of ozone and were followed before and after treatment. Unfortunately, of the 67 patients, only 24 answered to our questionnaire. Their data, clinical aspects and results are summarized in table 1. There were 9 females and 15 males, with an average age of 66.2 years (range 46-88 years). All patients were studied with clinical evaluation, standard x-rays and Magnetic Resonance Imaging (MRI). All patients had a long clinical history, with an average of 6.5 years of LBP (range 1-20 years). Four of them underwent lumbar herniectomy before our treatment. LBP was due in 10 patients to lumbar discal bulging (LDB). Seven cases had LDB associated with sciatica without neurological deficits. Four patients had lumbar DH, 2 had lumbar stenosis and 1 had spondylolisthesis. Five of them underwent 2 cycles of injections.
Table 1.
Inclusion criteria were: LBP with or without sciatica (congruous with the level of pathology detected with MRI), VAS greater than 0 or in alternative ODI greater than 10%. Exclusion criteria were: neurological deficits, cauda equine syndrome, diabetic neuropathy, pregnancy and favism, in which ozone therapy is contraindicated. All patients were orally informed of the potential risks of treatment and written informed consent was obtained from all the subjects.
All procedures were performed in the outpatient clinic without anesthesiologist support. Each patient received 12 intramuscular injections (2/week) of an oxygen-ozone mixture (20 ml) with an ozone concentration of 27 ug/ml, obtained by means of a Multiossigen 98 HCPS generator (Multiossigen s.r.l., Gorle, Bergamo, Italy). The intramuscular injection was administered in the paraspinal lumbar muscles of the corresponding affected level, bilaterally (20 ml for each side), using an extraspinal lateral approach, under sterile conditions, with a 22-gauge needle. An injection time of 15 seconds was used, since longer injection time was deemed unsuitable because of the instability of ozone, which starts decaying after about 20 seconds (2). In order to promote homogeneous distribution of the gas through the muscular fibers, the injection site was gently massaged at the end of the procedure.
Local and radiating pain were assessed using a 10-cm horizontal Visual Analogue Scale (VAS), with 0 cm labeled “no pain” and 10 cm “worst pain I have ever had”, administered before and after treatment. Perceived functional status and disability were evaluated using the Oswestry Disability Index (ODI), administered before treatment and one month after the last injection.
Results
All patients were retrospectively evaluated with VAS and ODI scale. The mean pre-treatment VAS score was 5.6 (range 0-10), while the mean pre-treatment ODI score was 34% (range 12-62%). After treatment, we obtained a reduction of 2.3 point of the VAS scale (mean value was 3.3) and of 9% of the ODI score (mean value 25%). Three patients underwent lumbar videoscopy after treatment, because of persistent LBP, of which 1 was a 79 year-old man with severe lumbar stenosis, 1 was a 65 year-old female with spondylolisthesis L5-S1 and the last was a 64 year-old man with multiple DH.
VAS reduction was demonstrated in 23 out of 29 cycles (79%) of ozone therapy (mean VAS score reduction 2.3); 6 of them had a VAS score increase (mean VAS score increase 2.5).
Regarding disability evaluation, ODI score reduction was assessed in all except one patient (a 79 year-old man with severe lumbar stenosis). No complications were recorded.
Conclusions
LBP with or without sciatic nerve involvement affects roughly 70-80% of the population at least once in their lifetime (4). Until 15 years ago, surgery was the treatment of choice, but conservative measures are now preferred in the wake of unsatisfactory surgical outcomes (5). The natural history of DH tends to be favorable in most cases; spontaneous regression of DH in longitudinal imaging studies has been reported (6) and a spontaneous resolution of pain within the acute phase (from 6 to 12 weeks after pain onset) has been documented in 60-80% of patients with sciatica (7). Nowadays, surgery is indicated only in patients with intolerable pain, progressive neurological deficits or risk of cauda equine syndrome (8). Surgical treatment of DH is reported to have a short-term success rate of 85-90%. The success rate tends to decrease to 70-80% during long-term follow-up (more than 6 months) as a result of the appearance of symptoms related to failed back surgery syndrome (9). Neurosurgeons have consequently tended to adopt a more conservative approach, and it is estimated that only 3-4% of all patients affected by LBP and/or sciatica receive surgical treatment in the United States (10).
Minimally invasive methods have been developed (such as corticosteroid and anesthetic injections, acupuncture, mesotherapy) in addition to physiotherapy and vertebral manipulation to treat LBP. Among them, there has been increasing use of oxygen-ozone therapy. Ozone has a double effect, direct and indirect, or mechanical and anti-inflammatory. Ozone has an oxidizing action and breaks down some of the glycosaminoglycans chains in the nucleus pulposus and reduces their ability to hold water, diminishing the size of herniation and subsequently contributing to reduce hernia impingement on the venus and arterial flow. This causes hyper-oxygenation and reduces pain by direct and indirect mechanism. Besides, ozone has an effect on the inflammatory cascade by altering the breakdown of arachidonic acid to inflammatory prostaglandins (3). Finally, the stimulation of fibroblastic activity by ozone results in the initiation of the repair process by stimulating collagen deposition (11,12).
Among minimally invasive methods, ozone can be administered through intradiscal way, intraforaminal, intramuscular (2,13,14) and periradicular. Several papers have already demonstrated good results with low costs and very rare collateral effects (1,2,13-19). While intradiscal injections seem to exploit mechanical and anti-inflammatory effect, paravertebral intramuscular injections probably use only the anti-inflammatory mechanism (3).
Periradicular and intradiscal injections have been proposed since the late 1990s as a treatment for lumbar DH (20-23). Since then, several retrospective and randomized controlled studies have been published confirming clinical success in 70-80% of patients (20-23). In 2003 Andreula et al. (1) reported the results of a study involving 600 patients, treated with intradiscal and periganglionic CT-guided injections of oxygen-ozone versus corticosteroid and anesthetic plus oxygen-ozone. They had better results in the last group with a success rate at 6 months of 78.3% and statistically significant difference between the 2 groups. In 2005 Bonetti et al. (16) described the outcomes of a randomized controlled study, reporting better results for oxygen-ozone intraforaminal injections versus periradicular infiltration of steroids. Muto et al. (17) in 2010 presented a retrospective clinical study involving 2900 patients with LBP and treated with intradiscal-intraforaminal oxygen-ozone CT-guided injections. At 1 year follow-up, they reported success rate of 75-80% for soft DH, 70% for multiple DH and 55% for failed back surgery syndrome.
We found only 3 papers dealing with intramuscular oxygen-ozone injections in LBP. The advantage of this kind of procedure is that can be performed free-hand in the outpatient clinic, without premedication or anesthesiologist support. The disadvantage is that it exploits only the anti-inflammatory effect of ozone. Melchionda et al. (14) reported the results of a matched pair study between paravertebral lumbar oxygen-ozone injections versus anti-inflammatory analgesic drugs. They had 80% success rate for oxygen-ozone treatment at 6 months follow-up versus 50% for the anti-inflammatory analgesic drug group. Paoloni et al. (2) conducted a multicenter, randomized, double-blind, simulated therapy-controlled clinical trial. Thirty-six patients received intramuscular-paravertebral ozone injections whereas 24 received simulated lumbar intramuscular-paravertebral injections with false needle. Patients who received ozone had significant lower pain scores (VAS was 0.66 in the study group and 4.0 in the control group) compared to patients who received simulated therapy. Sixty-one patients became pain-free at a medium follow-up of 6 months. More recently, Apuzzo et al. (13) confirmed efficacy of intramuscular ozone injections in LBP: according their results, oxygen-ozone therapy was associated with better results in the short-term follow-up, whereas global postural re-education, alone or in combination with ozone, seemed to be associated with a further reduction in pain over time. Our results are similar to the other reports: 79% of patients had VAS reduction of 2.3 points and all except one patient reported ODI reduction (average reduction of 9%).
Our study has certain limitations: first of all the short term follow-up (1 month), second the small number of patients, due to a reduced compliance during treatment.
Lumbar paravertebral oxygen-ozone injections in the treatment of LBP are minimally invasive, safe, cheaper and effective in relieving pain as well as disability. In literature only a very small percentage of patients are reported to present side effects. This technique is easy to perform, it doesn’t need CT or anesthesiologist support. We suggest its application in LBP (due to lumbar discal bulging, lumbar stenosis, spondylolisthesis and DH) as first choice to replace intradiscal CT-guided infiltrations and to avoid or delay surgery.
Level of Evidence: Level 4 retrospective study.
References
- 1.Andreula CF. Simonetti L. De Santis F. Agati R. Ricci R. Leonardi M. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. AJNR Am J Neuroradiol. 2003;24(5):996–1000. [PMC free article] [PubMed] [Google Scholar]
- 2.Paoloni M. Di Sante L. Cacchio A, et al. Intramuscular oxygen-ozone therapy in the treatment of acute back pain with lumbar disc herniation: a multicenter, randomized, double-blind, clinical trial of active and simulated lumbar paravertebral injection. Spine (Phila Pa 1976) 2009;34(13):1337–44. doi: 10.1097/BRS.0b013e3181a3c18d. doi: 10.1097/BRS.0b013e3181a3c18d. [DOI] [PubMed] [Google Scholar]
- 3.Rahimi-Movaghar V. Eslami V. The major efficient mechanisms of ozone therapy are obtained in intradiscal procedures. See comment in PubMed Commons below Pain Physician. 2012;15(6):E1007–8. [PubMed] [Google Scholar]
- 4.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 5.Davis RA. A long-term outcome analysis of 984 surgically treated herniated lumbar discs. J Neurosurg. 1994;80(3):415–21. doi: 10.3171/jns.1994.80.3.0415. [DOI] [PubMed] [Google Scholar]
- 6.Sakai T. Tsuji T. Asazuma T. Yato Y. Matsubara O. Nemoto K. Spontaneous resorption in recurrent intradural lumbar disc herniation. Case report. J Neurosurg Spine. 2007;6(6):574–8. doi: 10.3171/spi.2007.6.6.11. [DOI] [PubMed] [Google Scholar]
- 7.Peul WC. van Houwelingen HC. van der Hout WB, et al. Prolonged conservative treatment or ‘early’ surgery in sciatica caused by a lumbar disc herniation: rationale and design of a randomized trial [ISRCT 26872154] BMC Musculoskelet Disord. 2005;6:8. doi: 10.1186/1471-2474-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Awad JN. Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:183–97. doi: 10.1097/01.blo.0000198724.54891.3a. [DOI] [PubMed] [Google Scholar]
- 9.Gangi A. Dietemann JL. Mortazavi R. Pfleger D. Kauff C. Roy C. CT-guided interventional procedures for pain management in the lumbosacral spine. Radiographics. 1998;18(3):621–33. doi: 10.1148/radiographics.18.3.9599387. [DOI] [PubMed] [Google Scholar]
- 10.van Tulder MW. Koes BW. Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomized controlled trials of the most common interventions. Spine (Phila Pa 1976) 1997;22(18):2128–56. doi: 10.1097/00007632-199709150-00012. [DOI] [PubMed] [Google Scholar]
- 11.Sagai M. Bocci V. Mechanisms of Action Involved in Ozone Therapy: Is healing induced via a mild oxidative stress? Med Gas Res. 2011 Dec 20;1(29) doi: 10.1186/2045-9912-1-29. doi: 10.1186/2045-9912-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borrelli E. Mechanism of action of oxygen ozone therapy in the treatment of disc herniation and low back pain. Acta Neurochir Suppl. 2011;108:123–5. doi: 10.1007/978-3-211-99370-5_19. doi: 10.1007/978-3-211-99370-5_19. [DOI] [PubMed] [Google Scholar]
- 13.Apuzzo D. Giotti C. Pasqualetti P. Ferrazza P. Soldati P. Zucco GM. An observational retrospective/horizontal study to compare oxygen-ozone therapy and/or global postural re-education in complicated chronic low back pain. Funct Neurol. 2014;29(1):31–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Melchionda D. Milillo P. Manente G. Stoppino L. Macarini L. Treatment of radiculopathies: a study of efficacy and tollerability of paravertebral oxygen-ozone injections compared with pharmacological anti-inflammatory treatment. J Biol Regul Homeost Agents. 2012;26(3):467–74. [PubMed] [Google Scholar]
- 15.Gallucci M. Limbucci N. Zugaro L, et al. Sciatica: treatment with intradiscal and intraforaminal injections of steroid and oxygen-ozone versus steroid only. Radiology. 2007;242(3):907–13. doi: 10.1148/radiol.2423051934. [DOI] [PubMed] [Google Scholar]
- 16.Bonetti M. Fontana A. Cotticelli B. Volta GD. Guindani M. Leonardi M. Intraforaminal O(2)-O(3) versus periradicular steroidal infiltrations in lower back pain: randomized controlled study. AJNR Am J Neuroradiol. 2005;26(5):996–1000. [PMC free article] [PubMed] [Google Scholar]
- 17.Muto M. Ambrosanio G. Guarnieri G, et al. Low back pain and sciatica: treatment with intradiscal-intraforaminal O(2)-O (3) injection. Our experience. Radiol Med. 2008;113(5):695–706. doi: 10.1007/s11547-008-0302-5. doi: 10.1007/s11547-008-0302-5. [DOI] [PubMed] [Google Scholar]
- 18.Lu W. Li YH. He XF. Treatment of large lumbar disc herniation with percutaneous ozone injection via the posterior-lateral route and inner margin of the facet joint. World J Radiol. 2010;2(3):109–12. doi: 10.4329/wjr.v2.i3.109. doi: 10.4329/wjr.v2.i3.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leonardi M. Simonetti L. Raffi L. Cenni P. Barbara C. Mini-invasive treatment of herniated disc by oxygen-ozone injection. Interv Neuroradiol. 2003;9(Suppl 2):75. doi: 10.1177/15910199030090S211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D’Erme M. Scarchilli A. Artale AM. Pasquali Lasagni M. Ozone therapy in lumbar sciatic pain. See comment in PubMed Commons below Radiol Med. 1998;95(1-2):21–4. [PubMed] [Google Scholar]
- 21.Paradiso R. Alexandre A. The different outcomes of patients with disc herniation treated either by microdiscectomy, or by intradiscal ozone injection. Acta Neurochir Suppl. 2005;92:139–42. doi: 10.1007/3-211-27458-8_30. [DOI] [PubMed] [Google Scholar]
- 22.Muto M. Andreula C. Leonardi M. Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen-ozone (O2-O3) injection. J Neuroradiol. 2004;31(3):183–9. doi: 10.1016/s0150-9861(04)96989-1. [DOI] [PubMed] [Google Scholar]
- 23.Muto M. Avella F. Percutaneous treatment of herniated lumbar disc by intradiscal oxygen-ozone injection. Interv Neuroradiol. 1998;4(4):279–86. doi: 10.1177/159101999800400403. [DOI] [PubMed] [Google Scholar]


