Abstract
Background and aim: Healthcare workers (HCWs) employed in Emergency Departments (EDs) frequently face with patients becoming violent because of long wait or diseases or under the influence of alcohol or drugs. Globally, workplace violence (WPV) in EDs is a major challenge to safety for HCWs, involving significant consequences to the victims, patients, and healthcare organizations. We reviewed the current literature with the aim to explore the topics focused on and to detect new evidences about approaching the issue of WPV toward HCWs in EDs. Methods: A search for articles regarding WPV toward HCWs employed in EDs and published from January 2007 through December 2017 was performed; using predetermined criteria for inclusion, selected articles were reviewed and qualitatively assessed for the aims of the review. Results: We found 60 papers which matched our inclusion criteria; the topics, discussed in order of frequency from highest to lowest, were: “Risk Assessment”, “Occurrence Rates”, “Risk Management”, and “Physical/non Physical Consequences”. Dementia, schizophrenia, anxiety, acute stress reaction, suicidal ideation, and alcohol and drug intoxication were found as predictors of physical violence perpetrated by patients against HCWs. Conclusion: A strategic way to the effective management of WPV should prioritize training courses focused on: constructing HCW-patient relationship, improving the workers’ communication skills, accurate reporting of each violent incident, and improving the labor context through management commitment and employee involvement in WPV prevention programs. A special effort is required in implementing workplace design effective in minimizing stressful conditions in waiting rooms which turned out to be the most frequent site of assaults.
Keywords: assault, occupational risk, safety measures, risk assessment, risk management
Introduction
Workplace violence against healthcare workers (HCWs) employed in Emergency Departments (EDs) is a major challenge to HCWs’ workplace safety and health worldwide, involving significant consequences to the victims, patients, and healthcare organizations. EDs are high-risk settings for WPV, compared to all health care settings (1-6); by literature, ED HCWs face many acute and chronic, often unpredictable, stressors every day, including sudden death, trauma and hospital overcrowding and frequently deal with patients with grat potential for violent behavior due to their disease state, long waits or drug and alcohol intoxication (1, 8-9). In a recent research, Ferri et al. (1) showed that in an italian ED the 63% of violent events occurred in the waiting room, hypothesizing that there is a relationship between WPV and high level of anxiety and stress endured by both patients and their carers or relatives that is compounded by long waits. Long waits and the stress of waiting in combination with substance abuse and psychiatric comorbidities of patients can lead to WPV (10, 11).
Sequelae of violent attacks against HCWs may include not only somatic injuries but also psychological consequences, in fact, anger, fear or anxiety, post-traumatic stress disorder symptoms, guilt, self-blame and shame, decreased job satisfaction and increased intent to leave the organization, lowered health-related quality of life (HRQoL), were found as frequent consequences of workers’ (short or long-term) exposure to WPV (12, 13). The psychic consequences of WPV for ED HCWs who have been the victims of WPV often lead to absenteeism, poor morale and decreased productivity (14-16). More specifically, research examining the effect of WPV on ED nurse productivity revealed that ED nurses exposure to violent events significantly decreased productivity in the areas of Cognitive Demands and Support/Communication Demands in contrast to their feelings that they were able to maintain their work performance and provided safe and competent care (17).
The aims of this review were to explore the most common themes raised in the literature on WPV committed by patients and visitors against HCWs in EDs in the last 10 years. Although WPV against HCWs is a global problem, to date there is no general agreement among researchers on the definition; for the purposes of the present review, WPV was defined: “Any incident in which a person is abused, threatened or assaulted in circumstances relating to their work; this can include verbal abuse or threats as well as physical attacks”, according to the definition adopted by the Health and Safety Executive (HSE) (18).
Methods
A search for articles regarding WPV toward HCWs employed in EDs and published from January 2007 through December 2017 was performed using two common literature databases: PubMed and Web of Science; selected keywords were used to search articles for the aims of this review. The keywords were: Violence, Emergency Department, Healthcare worker, Assault, Prediction, Prevalence, Occupational Risk, Safety Measures, Risk Assessment and Risk Management. The keywords were systematically combined together to conduct the search. For example, “Healthcare worker,” AND “Violence” AND “Occupational risk” was one combination. Our search was aimed to identify original research articles (i.e. non-reviews) using the above- mentioned keywords with the following exclusion criteria: (1) not written in English; (2) not published after January 2007 (the year 2007 was chosen, with the aim to analyze the research studies of the last 10 years); (3) studies not regarding EDs, and (4) not full reports (i.e. letters to the editor). The screening of articles was carried out in two phases. In the first phase, articles were screened on the basis of title and abstract. Two independent reviewers (G.d and V.P.) assessed the abstracts and categorized them as relevant, not relevant and possibly relevant. In the second phase, the full-text articles were evaluated for eligibility. Two reviewers (G.d. and V.P.) independently applied inclusion and exclusion criteria to potentially eligible papers and both reviewers then independently extracted data from the original articles. Any disagreements were independently checked by a third reviewer (M.M.) and discussed with the other reviewers until consensus was reached. Every full-text article that met the inclusion criteria was reviewed and categorized into one or more of the following four categories based on its subject matter: Risk assessment (articles addressed to the examination of WPV perpetrated by patients as well as the probability that they will occur), Risk management (articles aimed at detecting effective interventions to minimize the WPV risk to an acceptable level to protect workers), Occurrence rates (e.g. incidence or prevalence of patient violence), Physical/non physical consequences (e.g. injuries or mental disorder following patient violence).
Results
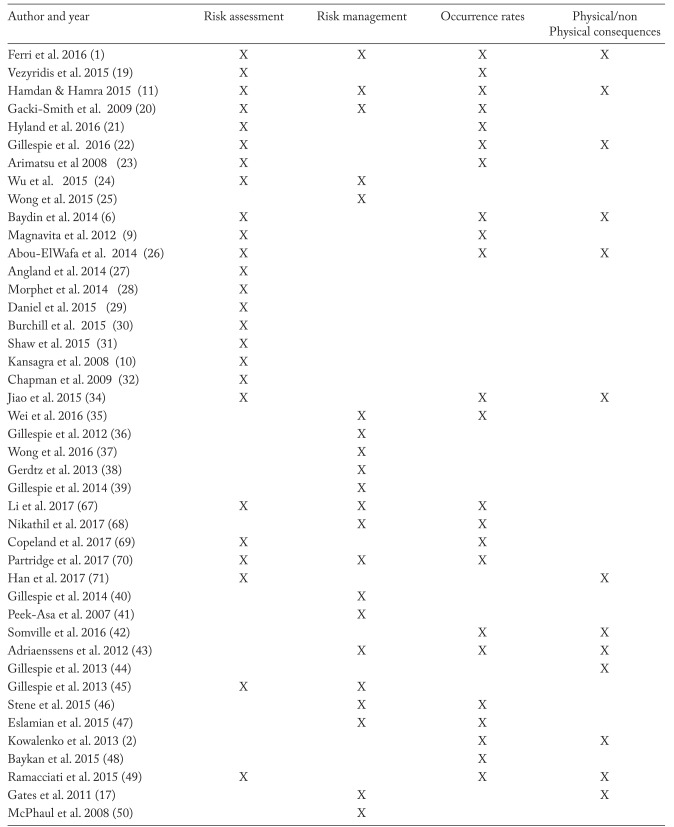
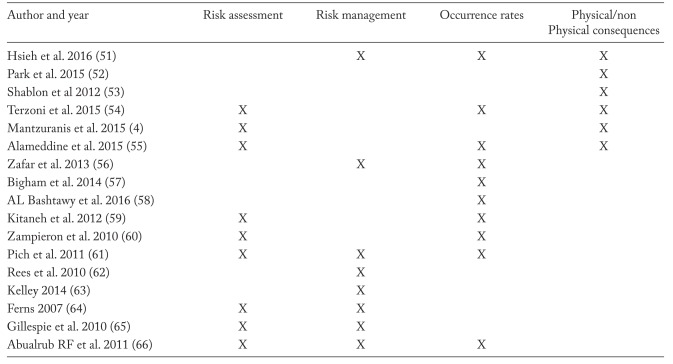
Our search of the two literature databases resulted in a total of 653 publications that matched our inclusion criteria. Of those, 593 were removed because they did not meet inclusion criteria (e.g. conference proceedings or not concerning HCWs of EDs). Therefore, 60 papers remained in the study. The topics, discussed in order of frequency from most frequent to least frequent, were: “Risk Assessment”, “Occurrence Rates”, “Risk Management”, and “Physical/non Physical Consequences”. 34 papers focused on “Risk Assessment”; 32 papers on “Occurrence Rates”; 29 papers on “Risk Management”; 19 papers on “Physical/Non Physical consequences”. Seven papers discussed both “Occurrence Rates” and “Risk Assessment”; four papers focused on both “Risk Assessment” and “Risk Management”, two papers were addressed to all the 4 topics.
Table 1.
Summary of literature review findings and articles categorization based on addressed topics
Discussion
Risk Assessment of WPV
The results of the present literature review show that in the last 10 years, the main topic of the checked papers was focused on “Risk Assessment”, with the aim to examine the risk factors of WPV perpetrated by patients against HCWs, as well as the risk that WPV will occur. The checked papers relating to “Risk Assessment” focused on: the predictors of violence perpetrated by patients; the determinants within the EDs; the perceived risk of violence among HCWs. Regarding the predictors of violence perpetrated by patients, Ferri et al. (1) reported that verbal violence was frequently perpetrated by patients in a lucid and normal state of consciousness; dementia, schizophrenia, anxiety, acute stress reaction, suicidal ideation, and alcohol and drug intoxication were found as predictors of physical violence perpetrated by patients against HCWs. These findings are consistent with the workplace violence literature (5, 19-27, 34-36) that showed an higher perceived risk of physical violence among ED HCWs facing patients affected by mental health disease or disorder or under the influence of drugs or alcohol, than facing patient in a lucid and normal state of consciousness. These evidences support the need for EDs to have action plans aimed to assess prior every patient for the risk of being violent and to make known to colleagues that a patient is at risk for becoming violent (34). Chapman et al. (28) developed the STAMPEDAR assessment tool to identify patients and visitors at risk for violent behaviors, based on the work of Luck et al. who developed the STAMP acronym (29). The acronym STAMPEDAR stands for staring, tone and volume of voice, assertiveness, mumbling, pacing, emotions, disease process, anxiety, and resources. Though the tool does not allow to predict whether the patient will become violent or not, STAMPEDAR is effective to alert ED HCWs on behavioral precursors to violence (e.g., staring, tone and volume of voice, assertiveness, emotions, disease process). This approach is aimed to preventing WPV through early detection of potentially violent patient and it is in line with literature which evidenced the need to implement procedures to identify in advance the patients as well as being in alert if the patients were to return to the ED in the future.
With regard to the determinants of violence within the EDs, they were most frequently identified as: inadequate HCW-patient relationship, high anxiety level among the staff, poorer perceived safety climates, high job demands, long waiting times for patients. HCWs’ characteristics that were associated with the experience of physical WPV included, but were not limited to age less than 30 years and female gender (20). Although these evidences, Kansagra et al. (10) showed that staff who had worked more than 5 years perceived less safe than staff who had worked shorter periods of time. This finding may be due to the fact that staff felt less safe and able to manage violent patients as they have been witness of many epysodes of WPV in the past.
Organizational factors were evidenced as frequent determinants of WPV. In particular, Wu et al. (20) demonstrated the relationship between high job demand and WPV; in fact, an excessive service volume, high-stress situations, and overload of physicians in daily practice were related to poor-quality medical care and, consequently, to dissatisfied patients, which revealed being the main cause of WPV against physicians. In the light of these findings, organizational interventions aimed at managing the job demand and at improving the safety climate should be adopted as a strategic way in increasing worker safety and in protecting HCWs from WPV and its negative consequences.
By literature, the surveys targeted on the staff perception of safety were detected as a valuable strategy to assess WPV risk and to achieve the gool of WPV risk reduction. In fact, Shaw et al. (27) found that among nurses of a pediatric ED, the assessment of perceived safety leaded to detect improvement interventions based on HCWs’ suggestions and consisting in increased presence from hospital security staff (55%) and local police (71%). This finding is consistent with WPV literature; in the past, Burchill C. (26) developed the Personal Workplace Safety Instrument for Emergency Nurses (PWSI EN) and revealed its effectiveness in measuring the perception of safety in EDs’ nurses and in finding solutions for managing WPV. Based on perceived safe assessment in EDs, Kansagra et al. (10) showed that nurses perceived less safe than the other HCWs in EDs, and interpreted this finding as a consequence of the close association between ED nurses and patients throughout the visit which may expose them to higher risk of violence and, consequently, lead them to perceive themselves less safe. This finding is in line with other studies which have shown that nurses experienced more physical assaults than other HCWs (21).
Risk management of WPV
Among the 29 papers focusing this topic, 19 papers discussed the management interventions targeted to the staff (e.g. training, improvement of skills in de-escalation approach to violent patients, teamworking, reporting WPV incidents); 10 papers addressed the worksite analysis with the aim to eliminate or minimize potential hazards for WPV.
With regard to training, the selected papers focused most frequently on: contructing the HCW-patient relationship, improving the workers’communication skills, accurate reporting of each violent incident, and improving the labor context through management committment and employee involvment in a WPV prevention program. Wu et al. (20) showed that training based only on lectures was less effective in preventing WPV compared to WPV training programs in hospital settings based on interactive and dynamic learning methods for ED workers (e.g. teaching strategies such as small-group learning, interactive learning, and simulation exercises may be applied during training in medical schools. In line with this findings, Wong et al (21, 31) found that an interprofessional simulation-based team-training curriculum successfully increased staff ability to manage factors impacting the care of potentially aggressive patients in the ED. Training revealed effective also to minimizing the fenomenon of under-reporting WPV incidents; in fact, Stene et al. (37) showed increased compliance of HCWs to report these violent incidents, after educational program for WPV, aimed to encourage HCWs to WPV reporting.
With regard to worksite analysis, several measures have been purposed to remove the hazards from the workplace or to prevent contact between HCWs and hazards identified by the workplace security analysis. The main security measures evaluated to minimize WPV risk were: alarm systems and other security devices, panic buttons, hand-held alarms or noise devices, cellular phones and private channel radios where risk is apparent or may be anticipated; closed-circuit video recording for high-risk areas on a 24-hour basis; employee “safe rooms” for use during emergencies; shatter-proof glass in reception, triage and admitting areas or client service rooms; with regard to waiting room, should be prioritized interventions to make them comfortable and to minimize stress, in fact Ferri et al. (1) showed that 63% of violent events perpetrated by patients took place in the waiting room, and were related to intolerance for long waiting times, and misunderstanding in communications or missing information; these findings are consistent with WPV literature. In particular, Angland et al. (23) suggested that to prevent the aggression that may arise from waiting times, electronic boards indicating approximate waiting times may be useful. Also, information guides and videotapes on the patient’s journey through the ED may be of benefit, and communication training for ED staff is also recommended.
Many authors showed the importance of limiting access through security officers, which can manage the access to the patient treatment area; in fact, patients’ and visitors’ possibility to access the patient treatment area was felt by ED workers as threat to the safety of ED workers (23, 42, 43); in particular, Gillepsie et al. (43) demonstrated that if access were not always controlled and violent patients and visitors were able to enter the treatment area, emergency nurses felt unsafe and perceived an high risk of suffering a physical assault. It is also important that early communication between security officers and ED workers takes place before violent events occur.
Physical/non-physical consequences of WPV
All the 19 studies focused on this topic evaluated the psychic repercussions of the attacks; the main consequences reported by abused or assaulted professionals, especially those verbally abused, were to mental health and well-being of the workers in terms of fear, irritation, anger, depression, anxiety, guilt, humiliation, feelings of helplessness, and disappointment. These sequelae, as reported in the literature, can reduce the ability of HCWs to share and understend the patients’ needs and, sometimes, are predictors of burnout (1, 45). Moreover, Gates et al. (17) revealed that ninety-four percent of nurses experienced at least one posttraumatic stress disorder (PTSD) symptom after a violent event, 17% suffered for probable PTSD, and found that such symptoms consequent to physical violence had a negative impact on the cognitive ability of emergency nurses to perform their work compared to their ability before a violent incident.
The detrimental effects of stress symptoms suffered by assaulted HCWs involve all the staff; in fact, lost productivity was found in assaulted HCWs suffering stress symptoms, due to absenteeism, and difficulties in approaching patients; in particular, Hamdan & Hamra (11) found that after an epysode of WPV, 26.4% of physicians and 21.8% of the nurses victim of WPV minimized contacts with patients and their companions and 13.6% and 14.5%, respectively, minimized the time of patient care, as well as 11.8% and 8.2%, respectively, avoided taking decisions that might involve medical risks.
Occurrence of WPV
The 32 checked studies showed that between 24% and 88,8% of HCWs on EDs have been victim of violence by a patient at some stage in the past 12 months; verbal assaults affected from 46,3 to 72.5% of HCWs; physical assaults from 16,5 to 48% of HCWs; sexual harassment from 8.6 to 14% of HCWs. Gacki-Smith et al. (46) revealed that 25% of emergency nurses recruited into a cross-sectional study on WPV, reported experiencing physical violence more than 20 times in the past 3 years, and almost 20% reported experiencing verbal abuse more than 200 times during the same period. Kowalenko et al (2) showed that average violence exposition rate per person per 9 months was 4.15; six hundred one events were physical threats (3.01 per person); two hundred twenty six events were assaults (1.13 per person); more than two-thirds of physicians have experienced WPV during their career, and more than 50% of physicians have experienced WPV in the previous year.
With regard to the professionals assaulted in EDs, no occupation revealed to be not affected by assaults and threats, although with differences among occupations (1). A recent study by Kitaneh and Hamdan (47) did not riveal statistical differences in exposure to WPV between physicians and nurses, in the past 12 months in Palestinian public hospitals; this finding was confirmed by Guglielmetti et al. (48) which detected nurses and physicians as exposed to the same risk of WPV. On the contrary, Magnavita et al. (9) showed that physicians were more exposed to WPV, compared to other occupations, and hypotisized that the finding was related to their decision-making role and to frequently working alone with patients.
WPV occurrence data suffer of under-reporting WPV by assaulted HCWs; in fact Ferri et al. (1) reported that 84% of HCWs did not report violent events, in line with literature which indicates many reasons for under-reporting of WPV: fear of retaliation from aggressor and his/her family, feelings of shame related to being the subject of aggression, or addiction to WPV considered an integral part of job.
Limitations
There are several limitations in this study. Firstly, because of the definition of violence is not unique, some selected papers analyzed only physical violence, others both physical and verbal; secondly, the occurrence of the WPV may be underestimated; in fact, several studies showed that in many cases the episodes of WPV are not reported by assaulted workers. In view of the above, to carefully analyze the WPV risk, we used the violence definition made by the HSE, which is comprehensive of both physical and non-physical attacks; moreover, we think that the phenomenon of underreporting of WPV is mitigated by the considerable number of papers which studied the topic of “occurrence rate” and held into account the above limitation.
Implications for emergency healthcare workers
A special effort is required in implementing workplace design effective in: ensuring the safe egress by staff away from the violent patient or visitor until help can respond, and in minimizing stressful conditions in waiting rooms rooms which turned out to be the most frequent site of assaults against HCWs. A strategic way to the effective management of WPV should also prioritize training courses focused on contructing the HCW-patient relationship, improving the workers’communication skills, accurate reporting of each violent incident, and improving the labor context through management committment and employee involvment in a WPV prevention program; in fact, the HCW attitudes in assessing and managing WPV showed determinant in minimizing the risk. Wong et al. (21,31) demonstrated the effectiveness in improving HCWs’ attitudes toward patients with behavioral emergencies through a better understanding of factors contributing to patient aggression. All HCWs should be also trained to behave carefully toward colleagues when WPV occurs; in fact, assaulted workers frequently suffer feelings of fear, anger, guilt, irritation and helplessness. These sequelae, as reported by the literature, can reduce the empathy capacity of health care workers and, sometimes, constitutes causes of burnout.
Interventions targeted at preventing WPV should consider the post-incident reports of assaults, with the aim to analyze incidents, including the characteristics of assailants and victims, an account of what happened before and during the incident, and the relevant details of the situation and its outcome, processes and procedures that put employees at risk of assault, including how often and when. The analysis of each assault helps to identify new or unknown risk factors and deficiencies or failures in work practices, procedures or controls. Also, the analysis helps to design measures through engineering or work practices to prevent or control these hazards. To date, most of the checked papers highlighted the phenomenon of under-reporting the incidents by assaulted HCWs; educational programs showed effective in encouraging HCWs to WPV reporting; Stene et al. demonstrated that after the ED staff were given the education aimed to report assaults, the ED staff began reporting those violent incidents that occurred within the ED (37).
Conclusion
The findings of the present review show that the patients’ violence towards HCWs is a major problem for HCWs, healthcare organizations and patients; dementia, schizophrenia, anxiety, acute stress reaction, suicidal ideation, and alcohol and drug intoxication were found as predictors of physical violence perpetrated by patients against HCWs in EDs; despite this evidence, the short-term prediction of behavioral emergencies in an ED, based on such predictors, has limited value compared to community settings; in fact, in the admittance of acute patients such predictors are frequently unknown (5, 8-10).
We found a lack of evidence about the long-term psychic consequences of violence towards HCWs in EDs; in fact, many authors revealed that among HCWs both forms of violence, physical and non-physical, were significantly correlated, in the short-term period, with symptoms of burnout (emotional exhaustion, depersonalisation and inefficacy) and with experience distressing emotions. In particular, Gates et al (17) found high risk of PTSD among ED nurses assaulted and suggested immediate interventions, during the first hours or days after a trauma, to provide the victim with the support system composed of peers and administrative representatives; in fact, workers supported by such interventions would have an opportunity to process the event and put it into perspective, thus minimizing the short and long-term symptoms related to stress and anxiety. According to these findings, we suggest the need to analyze the long-term psychological sequelae of WPV towards assaulted HCWs, with the purpose of designing the effective interventions to assist the victims of violence and to prevent psychological consequences.
References
- 1.Ferri P, Silvestri M, Artoni C, Di Lorenzo R. Workplace violence in different settings and among various health professionals in an Italian general hospital: a cross-sectional study. Psychology Research and Behavior Management. 2016;9:263–75. doi: 10.2147/PRBM.S114870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kowalenko T, Gates D, Gillespie GL, Succop P, Mentzel TK. Prospective study of violence against ED workers. Am J Emerg Med. 2013;31:197–205. doi: 10.1016/j.ajem.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Edward KL, Ousey K, Warelow P, Lui S. Nursing and aggression in the workplace: a systematic review. Br J Nurs. 2014;23:653–9. doi: 10.12968/bjon.2014.23.12.653. [DOI] [PubMed] [Google Scholar]
- 4.Mantzuranis G, Fafliora E, Bampalis VG, Christopoulou I. Assessment and analysis of workplace violence in a Greek tertiary hospital. Arch Environ Occup Health. 2015;70:256–264. doi: 10.1080/19338244.2013.879564. [DOI] [PubMed] [Google Scholar]
- 5.Spector PE, Zhou ZE, Che XX. Nurse exposure to physical and nonphysical violence, bullying, and sexual harassment: a quantitative review. Int J Nurs Stud. 2014;51:72–84. doi: 10.1016/j.ijnurstu.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Baydin A, Erenler AK. Workplace violence in emergency department and its effects on emergency staff. Int J Emerg Ment Health. 2014;16:288–90. doi: 10.4172/1522-4821.1000112. [DOI] [PubMed] [Google Scholar]
- 7.d’Ettorre G, Greco M. Assessment and Management of Work-Related Stress in Hospital Emergency Departments in Italy. J Med Pract Manage. 2016;31:280–3. [PubMed] [Google Scholar]
- 8.Hallin K, Danielson E. Registered nurses’ experiences of daily work, a balance between strain and stimulation: a qualitative study. Int J Nurs Stud. 2007;44:1221–1230. doi: 10.1016/j.ijnurstu.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Magnavita N, Heponiemi T. Violence towards health care workers in a Public Health Care Facility in Italy: a repeated cross-sectional study. BMC Health Serv Res. 2012;12:108. doi: 10.1186/1472-6963-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kansagra S, Rao S, Sullivan A, et al. A Survey of Workplace Violence Across 65 U.S. Emergency Departments. Acad Emerg Med. 2008;15:1268–74. doi: 10.1111/j.1553-2712.2008.00282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamdan M, Abu Hamra A. Workplace violence towards workers in the emergency departments of Palestinian hospitals: a cross-sectional study. Hum Resour Health. 2015;13:28. doi: 10.1186/s12960-015-0018-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nolan P, Dallender J, Soares J, Thomsen S, Arnetz B. Violence in mental health care: the experiences of mental health nurses and psychiatrists. J Adv Nurs. 1999;30:934–41. doi: 10.1046/j.1365-2648.1999.01163.x. [DOI] [PubMed] [Google Scholar]
- 13.Sofield L, Salmond S. Workplace violence: A focus on verbal abuse and intent to leave the organization. Orthop Nurs. 2003;22:274–83. doi: 10.1097/00006416-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Chen C, Huang C, Chen C. The relationship of health-related quality of life to workplace physical violence against nurses by psychiatric patients. Qual Life Res. 2010;19:1155–61. doi: 10.1007/s11136-010-9679-4. [DOI] [PubMed] [Google Scholar]
- 15.Richter D, Berger K. Post-traumatic stress disorder following patient assaults among staff members of mental health hospitals: a prospective longitudinal study. BMC Psychiatry. 2006;6:15. doi: 10.1186/1471-244X-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inoue M, Tsukano K, Muraoka M, et al. Psychological impact of verbal abuse and violence by patients on nurses working in psychiatric departments. Psychiatry Clin Neurosci. 2006;60:29–36. doi: 10.1111/j.1440-1819.2006.01457.x. [DOI] [PubMed] [Google Scholar]
- 17.Gates DM, Gillespie GL, Succop P. Violence against nurses and its impact on stress and productivity. Nurs Econ. 2011;29:59–66. [PubMed] [Google Scholar]
- 18.Health and Safety Executive (UK) [Internet] Work-related violence. 2016 [cited 2017 dec 28]. Available from: http://www.hse.gov.uk/violence/index.htm .
- 19.Vezyridis P, Samoutis A, Mavrikiou PM. Workplace violence against clinicians in Cypriot emergency departments: a national questionnaire survey. J Clin Nurs. 2015;24:1210–22. doi: 10.1111/jocn.12660. [DOI] [PubMed] [Google Scholar]
- 20.Wu JC, Tung TH, Chen PY, Chen YL, Lin YW, Chen FL. Determinants of workplace violence against clinical physicians in hospitals. J Occup Health. 2015;57:540–7. doi: 10.1539/joh.15-0111-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong AH, Wing L, Weiss B, Gang M. Coordinating a Team Response to Behavioral Emergencies in the Emergency Department: A Simulation-Enhanced Interprofessional Curriculum. West J Emerg Med. 2015;16:859–65. doi: 10.5811/westjem.2015.8.26220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abou-ElWafa HS, El-Gilany AH, Abd-El-Raouf SE, et al. Workplace violence against emergency versus non-emergency nurses in Mansoura university hospitals, Egypt. J Interpers Violence. 2015;30:857–72. doi: 10.1177/0886260514536278. [DOI] [PubMed] [Google Scholar]
- 23.Angland S, Dowling M, Casey D. Nurses’ perceptions of the factors which cause violence and aggression in the emergency department: a qualitative study. Int Emerg Nurs. 2014;22:134–9. doi: 10.1016/j.ienj.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 24.Morphet J, Griffiths D, Plummer V, et al. At the crossroads of violence and aggression in the emergency department: perspectives of Australian emergency nurses. Aust Health Rev. 2014;38:194–201. doi: 10.1071/AH13189. [DOI] [PubMed] [Google Scholar]
- 25.Daniel C, Gerdtz M, Elsom S, et al. Feasibility and need for violence risk screening at triage: an exploration of clinical processes and public perceptions in one Australian emergency department. Emerg Med J. 2015;32:457–62. doi: 10.1136/emermed-2013-202979. [DOI] [PubMed] [Google Scholar]
- 26.Burchill C. Development of the Personal Workplace Safety Instrument for Emergency Nurses. Work. 2015;51:61–6. doi: 10.3233/WOR-141889. [DOI] [PubMed] [Google Scholar]
- 27.Shaw J. Staff perceptions of workplace violence in a pediatric emergency department. Work. 2015;51:39–49. doi: 10.3233/WOR-141895. [DOI] [PubMed] [Google Scholar]
- 28.Chapman R, Perry L, Styles I, Combs S. Predicting patient aggression against nurses in all hospital areas. Br J Nurs. 2009;18:478–83. doi: 10.12968/bjon.2009.18.8.41810. [DOI] [PubMed] [Google Scholar]
- 29.Luck L, Jackson D, Usher K. STAMP: components of observable behaviour that indicate potential for patient violence in emergency departments. J Adv Nurs. 2007 Jul;59(1):11–9. doi: 10.1111/j.1365-2648.2007.04308.x. [DOI] [PubMed] [Google Scholar]
- 30.Gillespie GL, Gates DM, Miller M, Howard PK. Emergency department workers’ perceptions of security officers’ effectiveness during violent events. Work. 2012;42:21–7. doi: 10.3233/WOR-2012-1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong AH, Combellick J, Wispelwey BA, et al. The Patient Care Paradox: An Interprofessional Qualitative Study of Agitated Patient Care in the Emergency Department. Acad Emerg Med. 2017;24:226–2. doi: 10.1111/acem.13117. [DOI] [PubMed] [Google Scholar]
- 32.Gerdtz MF, Daniel C, Dearie V, et al. The outcome of a rapid training program on nurses’ attitudes regarding the prevention of aggression in emergency departments: a multi-site evaluation. Int J Nurs Stud. 2013;50:1434–45. doi: 10.1016/j.ijnurstu.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 33.Gillespie GL, Gates DM, Kowalenko T, et al. Implementation of a comprehensive intervention to reduce physical assaults and threats in the emergency department. J Emerg Nurs. 2014;40:586–91. doi: 10.1016/j.jen.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Peek-Asa C, Casteel C, Allareddy V, et al. Workplace violence prevention programs in hospital emergency departments. J Occup Environ Med. 2007;49:756–63. doi: 10.1097/JOM.0b013e318076b7eb. [DOI] [PubMed] [Google Scholar]
- 35.Gillespie GL, Bresler S, Gates DM, Succop P. Posttraumatic stress symptomatology among emergency department workers following workplace aggression. Workplace Health Saf. 2013;61:247–54. doi: 10.1177/216507991306100603. [DOI] [PubMed] [Google Scholar]
- 36.Gillespie L, Gates D, Berry P. Stressful Incidents of Physical Violence Against Emergency Nurses. OJIN: The Online Journal of Issues in Nursing. 2013;18:2. [PubMed] [Google Scholar]
- 37.Stene J, Larson E, Levy M, Dohlman M. Workplace Violence in the Emergency Department: Giving Staff the Tools and Support to Report. Perm J. 2015;19:e113–7. doi: 10.7812/TPP/14-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eslamian J, Akbarpoor A, Hoseini SA. Quality of work life and its association with workplace violence of the nurses in emergency departments. Iran J Nurs Midwifery Res. 2015;20:56–62. [PMC free article] [PubMed] [Google Scholar]
- 39.Baykan Z, Öktem İS, Çetinkaya F, Naçar M. Physician exposure to violence: a study performed in Turkey. Int J Occup Saf Ergon. 2015;21:291–7. doi: 10.1080/10803548.2015.1073008. [DOI] [PubMed] [Google Scholar]
- 40.Rees S, Evans D, Bower D, Norwick H, Morin T. A program to minimize ED violence and keep employees safe. J Emerg Nurs. 2010;36:460–5. doi: 10.1016/j.jen.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 41.Kelley EC. Reducing violence in the emergency department: a rapid response team approach. J Emerg Nurs. 2014;40:60–4. doi: 10.1016/j.jen.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 42.Ferns T. Considering theories of aggression in an emergency department context. Accid Emerg Nurs. 2007;15:193–200. doi: 10.1016/j.aaen.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 43.Gillespie GL, Gates DM, Miller M, Howard PK. Workplace violence in healthcare settings: risk factors and protective strategies. Rehabil Nurs. 2010;35:177–84. doi: 10.1002/j.2048-7940.2010.tb00045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abualrub RF, Al-Asmar AH. Physical violence in the workplace among Jordanian hospital nurses. J Transcult Nurs. 2011;22:157–65. doi: 10.1177/1043659610395769. [DOI] [PubMed] [Google Scholar]
- 45.Li Z, Yan CM, Shi L, et al. Workplace violence against medical staff of Chinese children›s hospitals: A cross-sectional study. PLoS One. 2017 Jun 13;12(6):e0179373. doi: 10.1371/journal.pone.0179373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gacki-Smith J, Juarez AM, Boyett L, Homeyer C, Robinson L, MacLean SL. Violence against nurses working in US emergency departments. J Nurs Adm. 2009;39:340–9. doi: 10.1097/NNA.0b013e3181ae97db. [DOI] [PubMed] [Google Scholar]
- 47.Kitaneh M, Hamdan M. Workplace violence against physicians and nurses in Palestinian public hospitals: a cross-sectional study. BMC Health Serv Res. 2012;12:469. doi: 10.1186/1472-6963-12-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guglielmetti C, Gilardi S, Licata M, De Luca G. The healthcare operators’ experience with aggressive patients and their visitors: a cross-sectional study in four clinical departments. Med Lav. 2016;107:223–234. [PubMed] [Google Scholar]