Abstract
Femoral neck stress fractures (FNSFs) in healthy young subjects are uncommon and most prevalent among long-distance runners and military recruits. Women seem to be at higher risk of developing stress fractures because of possible eating disorders followed by amenorrhea and osteoporosis. This case report describes four young and middle-aged, active female recreational runners who developed stress fractures of the femoral neck. In three of them, with a clinical history of persistent pain in the groin region, which worsened during training, early diagnosis by MRI was considered essential in detecting the fractures. The patients were clinically, metabolically and radiographically evaluated; they were then treated and followed-up at our institution. Only one case was treated conservatively, while the others underwent surgical internal fixation using a screw-plate (DHS®). All of them returned to sport physical activity after a recovery period. Regarding the challenging management of FNSFs, our report highlights the importance of groin pain, especially in athletic females, an early diagnosis by MRI, and a proper classification of these injuries for a correct choice of treatment in order to prevent further dislocation and avoid avascular necrosis of the femoral head. (www.actabiomedica.it)
Keywords: fracture bone, femoral neck fractures, stress fractures, hip pain, MRI, running sports
Introduction
Femoral neck stress fractures (FNSFs) are uncommon injuries that were reported by Asalin, a German military surgeon first in 1905 (1) and then in 1936 (2), while Devas in 1958 (3) described these injuries in athletes. They currently account for between 1% and 7.2% of all stress fractures in healthy subjects; the femoral neck is involved in 11% of them (4). Nowadays, running is considered a main cause for sport-related stress fractures, especially in the lower extremity (5). FNSFs are more common in young women, especially runners, other endurance athletes or female military recruits as opposed to male ones (6), as well as in individuals with metabolic disorders. Most FNSFs in athletes are fatigue fractures caused by repetitive loading of normal bone with abnormal forces (7). Hence, potential risk factors include female gender, age, smoking, low aerobic conditioning, a sudden reduction in weight and lower extremity muscle mass combined with daily training (8), decreased femoral BMD and bone strength (9), gluteus medium weakness, coxa vara alignment (10) and femoral acetabular impingement (11). These fractures are also found in patients with an abnormal femoral anatomy, renal osteodystrophy, use of corticosteroids, amenorrhea and osteomalacia (12-18).
At present, the most commonly used classification system for FNSFs is that of Fullerton & Snowdy (19), based on both plain radiographs and bone scans, which divides them into 3 groups: Type I fractures, developed on the tension-side of the femoral neck; Type II fractures on the compression-side; and Type III displaced fractures. A fourth category, superiorly based incomplete tension-type fractures, originally added by Provencher (20), are routinely missed on plain radiographs, while they are usually detected with magnetic resonance imaging (MRI). More recently, an MRI-based classification system was proposed by Arendt & Griffth to predict the outcome of FNSFs, dividing them into 4 grades: Grade 1, signal change on STIR sequencing; Grade 2, change on STIR and T2; Grade 3, change on STIR, T1, and T2 but with no fracture line present; Grade 4, change on STIR, T1, and T2 with a fracture line present (21, 22).
The typical presenting complaint in FNSFs is gradual onset hip or groin pain, increased by activity and weight-bearing and reduced or ceased with rest. Symptoms can be located in the anterior groin region, thigh, gluteal region or radiating to the knee. The pain is often associated with increased intensity or duration of normal physical exercise. Initially, it is noted in the latter part of prolonged exercise, and later, it can be present at night and at rest, always associated with antalgic gait. Further, the presence of “cracking” or “popping” sensations during exercise is often associated with complete and displaced fractures (19, 23-25).
Since it is particularly difficult to diagnose FNSFs from history and physical exam, imaging is fundamental to get a correct and early diagnosis, even if plain radiographs do not show any clear finding (26). For this reason, although hip and pelvis bone scans and CT are very useful to get a proper diagnosis, the gold standard for the diagnosis of these injuries is considered MRI (27). Besides giving a better anatomic definition of the fracture, it can provide further information on the fracture outcome, as pointed out previously (21, 22, 28).
This mono-centre report describes the clinical, diagnostic and therapeutic approaches to treating four cases of FNSFs that occurred in young and middle-aged, active female recreational runners between January 2011 and December 2016. At our institution, the patients were treated and followed-up by the same single surgeon (A.B.), according to the newest evidence-based knowledge reported in the literature. In fact, they were assessed clinically and radiographically, and underwent bone metabolism and endocrinological evaluation by blood tests of vitamin D cholecalcipherol, calcium, phosphorus, alkaline phosphatase (ALP), serum protein electrophoresis, parathyroid hormone (PTH), tumor markers (CEA, CA125, CA19–9, CA15–3, AFP), and by urine calcium level test.
Case report 1
A 42-year-old female, accountant by profession, recreational runner of approximately 30 kilometers per week, presented a 4-week history of deep, intense pain in the right groin, which appeared after usually 30 minutes of running. She denied any symptoms of the left hip. There was no history of trauma, alcohol abuse, steroid use, metabolic disorder or any relevant diseases. Her body height was 163 cm with body weight 51 kg, and her BMI was 19.2 Kg/m2. She had born two children and had a normal menstrual cycle. At the beginning of symptoms, she took analgesics with partial clinical improvement. However, due to persistence of pain, she was evaluated by her general practitioner (GP) who suggested x-rays and MRI of the pelvis and hip joints.
At the orthopaedic visit, physical examination revealed a slight ROM reduction of the right hip due to pain compared to the contralateral: flexion limited to 90°, extension 20°, external rotation 40°, internal rotation 10°, flexion-abduction 45° and adduction 30°. The neurovascular examination showed normal results of both lower extremities. The values of tumor markers, urine calcium level test and all blood tests prescribed in that occasion resulted normal except for vitamin D and PTH (Table 1). Radiographic examination including plain pelvis x-rays (antero-posterior and lateral views) did not revealed any bone alteration or sign of fractures (Figure 1a and 1b), while the MRI showed edema of the spongy bone in the femoral neck base and a suspicious fracture line in the inferior margin of the femoral neck (Figures 2a and 2b). The diagnosis was an FNSF at the right femoral neck base, which was classified according to Fuellerton and Snowdy as a Type II, compression-side, incomplete FNSF.
Table 1.
Vitamin D and PTH blood values at diagnosis and after 6 months of supplemental therapy
| Vitamin D (75-250 nmol/L) | PTH (4.6-26.8 ng/L) | ||
|---|---|---|---|
| Case 1 | At diagnosis | 38 | 79 |
| At 6-month follow-up | Therapy: CHOLECALCIFEROL 30.000 U.I./month 70 | 32 | |
| Case 2 | At diagnosis | 76 | 17 |
| At 6-month follow-up | Therapy: DIBASE ® 50.000 U.I./month 89 | 14 | |
| Case 3 | At diagnosis | 53 | 66 |
| At 6-month follow-up | Therapy: CHOLECALCIPHEROL 100.000 U.I./month 75 | 17 | |
| Case 4 | |||
| At diagnosis | 25 | 51.3 | |
| At 6-month-follow-up | Therapy: CHOLECALCIPHEROL 60.000 U.I./month 76 | 54 |
Figure 1.
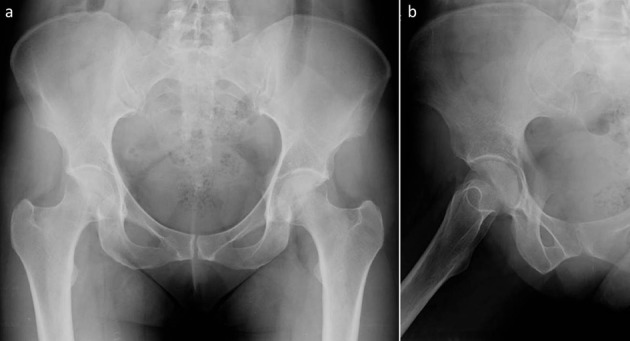
Case 1. Radiographic images at 4 weeks after onset of symptoms showing a Type II, compression-side FNSF: (a) panoramic anteroposterior view of the pelvis and (b) lateral view of right hip
Figure 2.
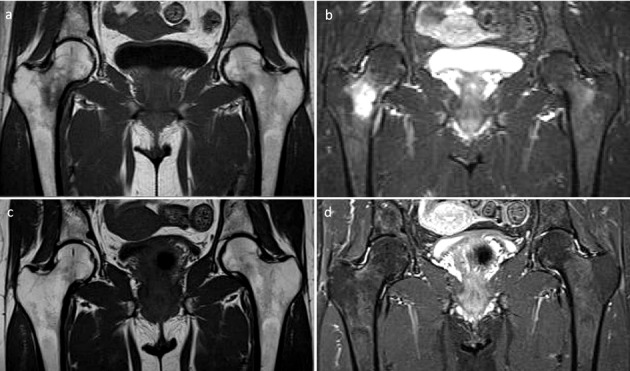
Case 1. Pelvis MRI images at 4 weeks after onset of symptoms showing the consolidation of the FNSF: (a) T1 weighted image, (b) T2 weighted image. Pelvis MRI images at 12-month FU, showing the FNSF healing: (c) T1 image and (d) T2 image
Discussing the MRI results with the patient, a conservative treatment was proposed, advising rest, using elbow crutches to avoid load on her right left limb for 30 days, then for further 20 days with assisted loading by crutches and finally, full weight-bearing at 2-month follow-up. Further, the patient was advised to take non-steroidal anti-inflammatory drugs (NSAIDs) for pain control and Cholecalcipherol 30.000 U.I./month to improve vitamin D levels.
During the rehabilitation period, the patient underwent physiokinesis and magnetic therapy cycles. She was followed at 3, 6 and 12 months following the injury, being clinically, metabolically and radiographically assessed. At 3-month follow-up she was completely pain free with full right hip ROM on clinical examination. She was able to walk with complete load without pain, starting only stationary cycling and swimming, while a month later, she started normal physical activity, without complaint. The new x-ray imaging studies performed showed callus formation on the inferior aspect of the femoral neck. At 6-month follow-up, the blood level of vitamin D and PTH improved almost to normal values (Table 1). The 12-month follow-up MRI showed no signs of avascular necrosis (AVN), and there was radiographic evidence of a healed stress fracture (Figures 2c and 2d).
Case report 2
The patient was a 28-year-old female, physician by profession, recreational runner, physically active non-smoker who complained of 2-week deep left groin pain during usual exercise of 60 minutes running 2–3 times per week. She had no allergies to medications. She did not drink or smoke and denied any drug use. She did not report specific history of previous trauma, also in her right hip. She had no past medical history except for polycystic ovary syndrome (POS).
As her symptoms did not abate taking NSAIDs regularly, she came to our outpatient department. At the time of presentation, her height was 164 cm and her weight 57 kg (BMI 21.2 Kg/m2). Clinical examination revealed no deformities or shortening either lower limb, and excellent capillary refill and good pulses. No neurological deficit was identified. Her left hip ROM was complete, comparable with the contralateral and with no pain limitations. However, the symptoms started and increased with load. The iliopsoas test and those for labral pathology were negative. The contralateral hip did not present any pathology. Tumor markers, a urine calcium level test and all blood tests prescribed resulted normal. As vitamin D was just at the normal limit (Table 1), Cholecalcipherol 50.000 U.I./month was suggested. Imaging studies were performed including first pelvis and x-rays of the hips (antero-posterior and lateral views), which did not show any alteration (Figures 3a and 3b). The MRI of her pelvis was performed 6 days later (Figure 3c), identifying a left femoral neck stress fracture on the medial side without cortical bone involvement and with surrounding edema of the spongy bone. Following Fuellerton and Snowdy, the injury was classified as a Type II, compression-side, incomplete, FNSF with a good prognosis. On the basis of clinical signs and radiographic results, the patient was treated conservatively and advised to rest, use walking aids to avoid full weight-bearing on her left lower limb. Unfortunately, when at 2-month-follow-up assisted loading by crutches was permitted, the pain increased suddenly. Immediate hip-x-rays were performed with a suspect of a Type II, compression-side, complete FNSF, which was radiologically confirmed as a superior neck margin fracture with cortical bone involvement. Hence, surgical treatment was proposed, and the patient underwent an internal fixation procedure on her proximal left femur using a DHS® DePuy-Synthes plate. After surgery, she was discharged with assisted loading by elbow crutches. After 30 days, she was able to walk with complete load, without aids and pain, starting stationary cycling and swimming. Finally, the patient was followed at 3, 6 and 12 months following the injury, being clinically, metabolically and radiographically assessed. At 6-month follow-up, the blood level of vitamin D and PTH were improved (Table 1), and at the last follow-up, the plain x-rays (Figures 4a and 4b) and MRI showed evidence of a healed stress fracture without signs of AVN (Figure 4c).
Figure 3.
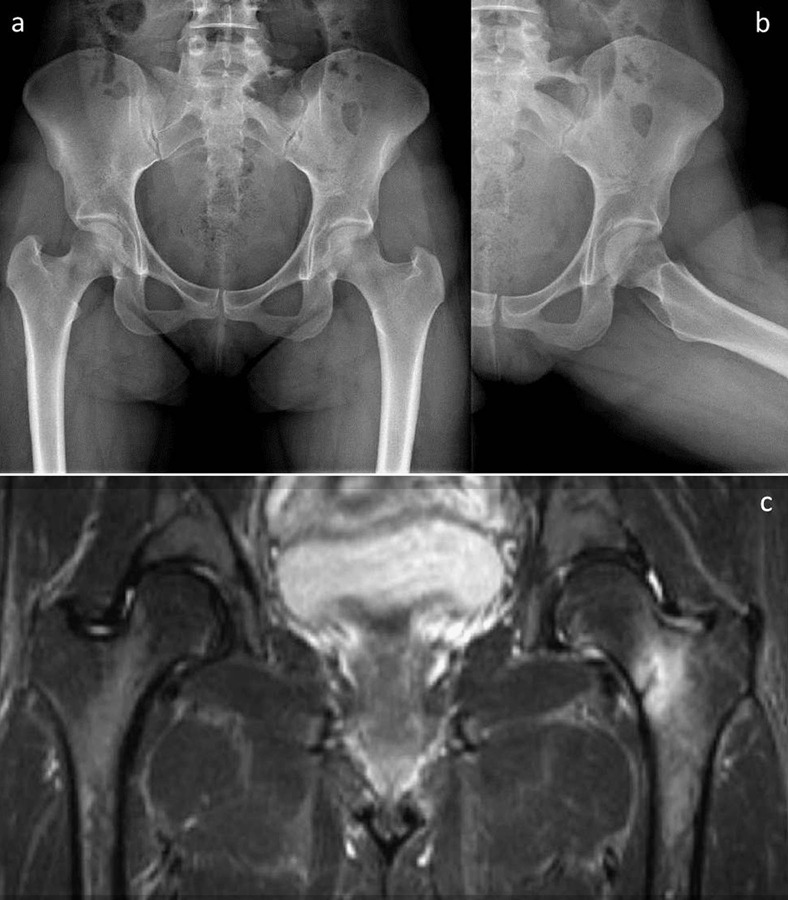
Case 2. Radiographic images at 2 weeks after onset of symptoms, showing a Type II, compression-side FNSF: (a) panoramic anteroposterior view of the pelvis and (b) lateral view of left hip. Pelvis MRI image at the same period: (c) T2 image
Figure 4.

Case 2. Radiographic images of left hip at 12-month FU showing the FNSF healing: (a) anteroposterior and (b) lateral views. MRI images at the same follow-up: (c) T1 weighted image
Case report 3
The patient was a33-year-old female, administration employee, physically active, non-professional runner. However, she had been training for a previous period of 3 months in preparation for a marathon with 3 hours running per day, 4–5 times a week. She denied allergies to medications, drinking or smoking, diabetes and any drug or corticosteroid use. Her height was 168 cm and weight 58 kg (BMI 20.5 Kg/m2). At the time of presentation, the patient suffered POS, dysmenorrhea and had previous history of anorexia with amenorrhea. However, she did not report specific history of previous trauma. She complained of a 4-week history of deep left groin pain during physical exercise, treated with partial relief by taking NSAIDs after every training session. Unfortunately, during a 20-kilometer running competition, she had intense pain in the left groin and was forced to abandon the race. After that, she came to the outpatient department of our institution for a first opinion.
Physical examination revealed no deformities of either hip. However, there was evidence of atraumatic mild pain of the left hip, complete ROM with moderate pain in passive motion, which increased with load and walking with discrete limping, and functional impairment, especially in internal rotation. On the right side, full range of motion was observed. The values of tumor markers, a urine calcium level test and all blood tests taken later resulted in normal ranges except for vitamin D and PTH (Table 1). Therapy with Cholecalcipherol 100.000 U.I./month was started to improve vitamin D levels. Pelvis and hip x-ray images (Figure 5a and 5b) showed an undisplaced femoral neck fracture, while the following CT scan (Fig. 5c and 5d) revealed a left femoral basicervical fracture, incomplete in the posterior-distal part, without bone callus. The MRI confirmed a complete fracture of the neck base of the left femur and the presence of intra-articular fluid (Figures 5e and 5f). Following Fuellerton and Snowdy, it was classified as a Type II, compression-side, complete FNSF.
Figure 5.

Case 3. Radiographic images at initial presentation, showing a Type II, compression-side FNSF: (a) panoramic anteroposterior view of the pelvis and (b) lateral view of left hip. Hip CT performed during hospitalisation, (c) coronal and (d) axial views. Pelvis MRI at the same period: T1 image (e) and T2 weighted image (f)
On the basis of the patient’s clinical presentation and radiographic examination, surgical treatment was proposed and performed using a DHS® S DePuy-Synthes plate (Figures 6a and 6b). The post-operative course was uneventful, and the patient was discharged and advised to walk with assisted loading with crutches for 30 days. After 60 days from the operation, she was able to walk with complete load, without crutches and pain free. She followed the same clinical, metabolic and radiographic post-operative protocol. At 6-month follow-up, the blood levels of vitamin D and PTH were normal (Table 1). At 12-month follow-up, she was completely pain free and demonstrated full range of motion of her left hip upon clinical examination, while the x-rays showed evidence of a healed stress fracture without signs of AVN (Figures 6c and 6d).
Figure 6.

Case 3. Radiographic images immediately after surgery at post-operative period: (a) anteroposterior and (b) lateral views of left hip. Radiographic images of the same hip at 12-month FU: (c) anteroposterior and (d) lateral views showing the FNSF healing
Case report 4
A 48-year-old female, public administration employee, thin physical build and non-smoker with no history of metabolic diseases or use of corticosteroids, having born two children, complained of 4-week left groin pain. At the beginning, it was dull and not radiated, of low intensity, and presented only during running activity. She denied any history of symptoms of the right hip. There was no habitual dietary abnormality that could include osteoporosis. She had started running regularly for 30 minutes, training 2 times per week just 3 months before the appearance of symptoms. Despite them, she decided to continue her physical activity with a worsening of pain and with a limp. She started a cycle of physical therapy with a further worsening of pain that started to radiate into the posterior aspect of the left lower limb.
After 10 days of increasing symptoms, she came to the outpatient department of our institution. Clinically, her left hip ROM was limited by pain: flexion 80°, extension 20°, external rotation 30°, internal rotation 10°, flexion-abduction 35° and adduction 20°. The neurovascular examination showed normal results of both lower extremities. At the time of presentation, her height was 170 cm and weight 56 kg with a BMI of 19.3 Kg/m2. As for metabolic investigations, the patient presented a low blood value of vitamin D and a high level of PTH (Tab. 1), while all other urinary and blood tests and tumor markers were in normal range. Thus 60.000 U.I./month of Cholecalcipherol were suggested. She then underwent radiographic evaluation including x-rays and a CT scan of the pelvis and hip (Figure 7a, 7b and 7c) which revealed a complete and displaced left femoral neck base stress fracture, Type III, according to Fuellerton and Snowdy. As the diagnosis had already been determined by radiography MRI was not necessary. Hence, surgical internal fixation by a DHS® DePuy-Synthes plate and a 7 mm-cannulated screw was proposed and performed (Figures 8a and 8b).
Figure 7.
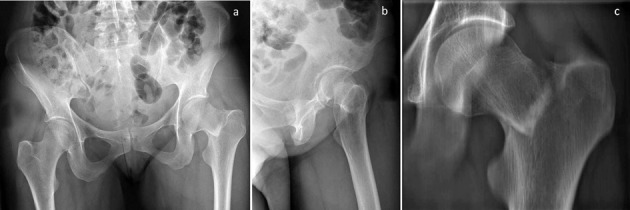
Case 4. Radiographic images at early diagnosis showing a Type III, complete and displaced FNSF: (a) panoramic anteroposterior view of the pelvis and (b) lateral view of left hip. Left hip CT at the same period (c)
Figure 8.
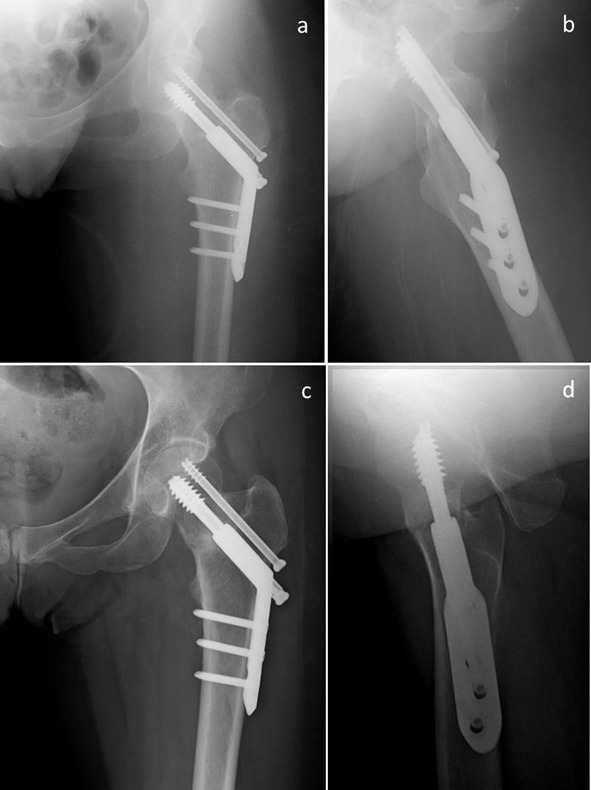
Left hip radiographic images immediately after surgery at post-operative period: (a) anteroposterior and (b) lateral view. Radiographic images of the same hip at 12-month FU: (c) anteroposterior view and (d) lateral view, showing signs of FNSF consolidation
After discharge, the patient was advised to use crutches, avoiding load on the left lower limb for 30 days; thereafter, assisted loading with crutches was authorized for another 20 days and complete load after that. She was assessed by the same clinical, metabolic and radiographic post-operative protocol. At 3-month follow-up, she was able to walk without crutches; she was completely pain free and had started stationary cycling and swimming. At 6-month follow-up, the blood level of cholecalcipherol was in normal range, while those of PTH persisted high (Table 1). At 12-month follow-up, the x-rays showed signs of FNSF consolidation without AVN (Fig. 8d and 8c).
Discussion
FNSFs, although uncommon injuries, are a known cause of groin, thigh or knee pain, often reducing at rest, in athletes at all levels of competition. They can also occur in children and adolescents. Multiple risk factors can be involved, including nutritional and dietary aspects (20). It was reported that FNSFs are more common in women with limited caloric intake, with avoidance of dairy products and high fat products, especially in women who have low BMI and eating disorders during adolescence (29, 30). Female athletes with amenorrhea have 2–4 times higher risk of FNSFs compared to those ones with eumenorrhea (31). In our report, all patients were female, recreational runners, with thin body build and low BMI. Two of them had polycystic ovary syndrome, and one of them suffered also from an eating disorder during adolescence. Another important finding was that all patients had a low vitamin D blood level and high PTH (Tab.1). Osteoporosis also causes a higher risk of fracture (32, 33). Bone stock and fracture risk is inverse and continuous. Femoral fractures are 2.6 times more common for every reduction of 1 standard deviation of femoral bone mineral density (BMD) (34).
Because of vague presentation of symptoms (35, 36) and non-specific physical examination (37), the clinical diagnosis of FNSFs is difficult, and approximately 75% of them may be misdiagnosed or undiagnosed on physical examination (20). As the hip and the surrounding tendons are overstressed and often overloaded, especially in athletes (38), these patients are often treated for muscle strain or hip tendinopathies during preparation for a marathon or other sport event (37). Although radiographs are appropriate as an initial screening, they have been reported to have low sensitivity for early detection (15%) and at follow-up (50%) (39). Hence, if clinical suspicion is high, further imaging is recommended from the initial presentation. In particular, a bone scan is more sensitive in high bone remodelling areas, but it lacks specificity due to similar uptake in case of infection, osteonecrosis and tumors (40). MRI evaluation is the most sensitive and specific imaging exam for the diagnosis of FNSFs (41); it can detect early, low-grade bony changes associated with FNSFs, such as periosteal, muscle and bone marrow edema (42-43). In agreement with Naik (44), who stated that additional tests and radiographic examination are not necessary to confirm the diagnosis when the fractures are evident in the initial standard radiographs, including CT scan, also in our series, MRI was performed at our institution in only 3 of 4 cases; there was no need to carry out MRI in the fourth Type III fracture case, as the standard x-rays and CT scan of the pelvis and hip were sufficient for diagnosis. Only for case 3, a better study of the fracture was required with MRI after CT, however without changes related to previous radiographic classification and surgical indication.
Although FNSFs are often a matter of debate in the community of orthopedic surgeons, at our institution, a clinical approach based on Fullerton and Snowdy radiographic classification was used for their management. For both Type I, compression-side, undisplaced fractures, and for Type II, incomplete, tension-side fractures, a conservative treatment is indicated, even though, for the latter, a prophylactic surgical fixation is advocated (45). In fact, for case 2, the second option of treatment by surgery was necessary. On the contrary, for Type II, tension-side fractures, some complete and all displaced fractures, and for those cases of patients not compliant with conservative treatment or in those with persisting pain after 4-week conservative treatment, surgical fixation and early ambulation are necessary, especially for young individuals.
Currently, the best surgical option is considered the screw-plate as opposed to cannulated screws or intramedullary nailing due to the best support for axial load (41). Further, it is still considered the preferred treatment equivalent of cannulated screw and screw-plate internal fixation (42). For these reasons, a screw-plate system was preferred in our surgically treated cases; a further de-rotation cannulated screw was added in the fourth case, providing a more stable construction and reducing the risk of rotating the femoral head during cephalic screw insertion, which could limit the femoral head blood supply (46).
Among the several complications reported such as refracture, varus collapse, or pseudoarthrosis (47), the major surgical risk, even in the correct treatment of FNSF, remains the avascular necrosis of the femoral head. Different studies reported a percentage of AVN between 18 and 25% after FNSF surgical treatment (48, 49). Obviously, the risk is correlated to the grade of displacement, the kind of internal fixation used, fracture-treatment timing and proper anatomic reduction (50). The most important risk factor in order to predict the AVN of the femoral head in these injuries is delaying their surgical treatment. Its incidence is estimated up to 3/10 patients with a treatment delay of over 4 weeks from the appearance of symptoms (51). In contrast, if the treatment is performed in the first 6 hours after the start of symptoms, AVN incidence is limited to 10.5–20% (52, 53). Finally, there are both significant morbidity and cost in the treatment of these fractures.
A better understanding of causes could improve prevention in these risk categories of patients through routine evaluation of their bone and endocrinological metabolism. We suggest specific blood and urine testing, including also a full blood count, erythrocyte sedimentation rate and C-reactive protein levels (47, 54), and an additional hormone profile for females as performed in our cases.
Conclusions
On the basis of the literature and supported by our experience, although limited to the 4 cases presented, we believe the success in management of FNSFs is related to:
- avoiding the underrating of groin pain persisting more than 3 weeks when correlated in young and middle-aged sports subjects, especially if female;
- bone markers and hormone profile screening of women and starting medical treatment if necessary;
- early evaluation of the pelvis and hip first by standard x-rays and then, if negative, by MRI (gold standard); in this way, it is possible to avoid any delay in diagnosis, often cause of further fracture displacement and possible AVN of femoral head;
- classifying the FNSF according to the radiological prognostic system proposed in the literature for a proper choice between conservative or surgical treatment;
- when the treatment indication is surgical, performing a perfect reduction, anatomic or in slight valgus, associated with a stable and rigid internal synthesis to avoid AVN, followed by a specific recovery period.
Author contribution
C.B. and A.C.: study concept and design; drafting the paper;
A.B.: operated and followed-up the patients;
C.M. and G.T.: data collection, analysis and discussion of data;
P.R.: final approval of the version to be published.
Declarations
Ethics approval and consent to participate
This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2000. The patients received a thorough explanation of this study and gave their oral and written informed consent to be included in this analysis.
Consent for publication
The patients gave their oral and written informed consent to the publication of their anonymous and clustered data and anonymous pictures.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Belcher A. Ueber den Einfluss des Parademarches auf die Entstehung der Fussgeschwulst. Med Klin. 1905;1:305–306. [Google Scholar]
- 2.Asal D. Uberlastungsschaden am Knochensystem bei Soldaten. Arch für Klinische Chirurgie. 1936;186:511–522. [Google Scholar]
- 3.Devas M. B. Stress fractures of the femoral neck. J Bone Joint Surg Br 47.4. 1965:728–738. [PubMed] [Google Scholar]
- 4.Scott M, Finnoff J, Davis B. Femoral neck stress fracture presenting as gluteal pain in a marathon runner: case report. Arch Phys Med Rehabil. 1999;80:236–38. doi: 10.1016/s0003-9993(99)90127-2. [DOI] [PubMed] [Google Scholar]
- 5.Cichy B., Roche S. J., Wozniak A. Atypical femoral neck stress fracture in a marathon runner: a case report and literature review. Irish journal of medical science 181.3. 2012:427–429. doi: 10.1007/s11845-010-0599-7. [DOI] [PubMed] [Google Scholar]
- 6.Warden SJ, Burr DB, Brukner PT. Stress fractures: pathophysiology, epidemiology, and risk factors. Curr Osteoporos Rep. 2006 Sep;4(3):103–9. doi: 10.1007/s11914-996-0029-y. [DOI] [PubMed] [Google Scholar]
- 7.Behrens SB, Deren ME, Matson A, Fadale PD, Monchik KO. Stress fractures of the pelvis and legs in athletes: a review. Sports Health. 2013;5:165–174. doi: 10.1177/1941738112467423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armstrong DW, Rue JPH, Wilckens JH, Frassica FJ. Stress fracture injury in young military men and women. Bone. 2004;35(3):806–816. doi: 10.1016/j.bone.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 9.Pouilles JM, Bernard J, Tremollieres F, Louvet JP, Ribot C. Femoral bone density in young male adults with stress fractures. Bone. 1989;10(2):105–108. doi: 10.1016/8756-3282(89)90006-9. [DOI] [PubMed] [Google Scholar]
- 10.Carpintero P, Leon F, Zafra M, Serrano-Trenas JA, Roman M. Stress fractures of the femoral neck and coxa vara. Archives of orthopaedic and trauma surgery. 2003;123(6):273–277. doi: 10.1007/s00402-003-0514-z. [DOI] [PubMed] [Google Scholar]
- 11.Goldin M, Anderson CN, Fredericson M, Safran MR, Stevens KJ. Femoral neck stress fractures and imaging features of femoroacetabular impingement. PM&R. 2015;7(6):584–592. doi: 10.1016/j.pmrj.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Werntz JR, Lane JM. The biology of pathologic fracture repair. In: Lane JM, Healey JH, editors. Diagnosis and management of pathologic fractures. New York: Raven; 1993. p. 1-11. [Google Scholar]
- 13.Daffner RH, Pavlov H. Stress fractures: current concepts. Am J Roentgenol. 1992;159(2):245–52. doi: 10.2214/ajr.159.2.1632335. [DOI] [PubMed] [Google Scholar]
- 14.Romani WA, Gieck JH, Perrin DH, Saliba EN, Kahler DM. Mechanisms and management of stress fractures in physically active persons. J Athl Train. 2002;37(3):306–14. [PMC free article] [PubMed] [Google Scholar]
- 15.Simpson PJ, Lucchesi BR. Free radicals and myocardial ischemia and reperfusion injury. J Lab Clin Med. 1987;110(1):13–30. [PubMed] [Google Scholar]
- 16.Pihlajamäki HK, Ruohola JP, Weckström M, Kiuru MJ, Visuri TI. Long-term outcome of undisplaced fatigue fractures of the femoral neck in young male adults. J Bone Joint Surg Br. 2006;88(12):1574–9. doi: 10.1302/0301-620X.88B12.17996. [DOI] [PubMed] [Google Scholar]
- 17.Talbot JC, Cox G, Townend M, Langham M, Parker PJ. Femoral neck stress fractures in military personnel – a case series. J R Army Med Corps. 2008;154(1):47–50. doi: 10.1136/jramc-154-01-13. [DOI] [PubMed] [Google Scholar]
- 18.>Umans H, Pavlov H. Stress fractures of the lower extremities. Semin Roentgenol. 1994;29(2):176–93. doi: 10.1016/s0037-198x(05)80063-x. [DOI] [PubMed] [Google Scholar]
- 19.Fullerton JR, LeRoy R, Snowdy HA. Femoral neck stress fractures. The American journal of sports medicine 16.4. 1988:365–377. doi: 10.1177/036354658801600411. [DOI] [PubMed] [Google Scholar]
- 20.Provencher MT, Baldwin AJ, Gorman JD, Gould MT, Shin AY. Atypical tensile-sided femoral neck stress fractures the value of magnetic resonance imaging. The American journal of sports medicine. 2004;32(6):1528–1534. doi: 10.1177/0363546503262195. [DOI] [PubMed] [Google Scholar]
- 21.Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clinics in sports medicine 16.2. 1997:291–306. doi: 10.1016/s0278-5919(05)70023-5. [DOI] [PubMed] [Google Scholar]
- 22.Ramey LN, McInnis KC, Palmer WE Femoral Neck Stress Fracture: Can MRI Grade Help Predict Return-to-Running Time? The American journal of sports medicine 44.8. 2016:2122–2129. doi: 10.1177/0363546516648319. [DOI] [PubMed] [Google Scholar]
- 23.Egol KA, Koval KJ, Kummer F, Frankel VH. Stress fractures of the femoral neck. Clinical orthopaedics and related research. 1998;348:72–78. [PubMed] [Google Scholar]
- 24.Neubauer T, Brand J, Lidder S, Krawany M. Stress fractures of the femoral neck in runners: a review. Research in Sports Medicine. 2016;24(3):283–297. doi: 10.1080/15438627.2016.1191489. [DOI] [PubMed] [Google Scholar]
- 25.Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. Journal of the American Academy of Orthopaedic Surgeons 5.6. 1997:293–302. doi: 10.5435/00124635-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Webber BJ, Trueblood WE, Tchandja JN, Federinko SP, Cropper TL. Concurrent bilateral femoral neck stress fractures in a military recruit: a case report. Military medicine. 2015;180(1):e134–e137. doi: 10.7205/MILMED-D-14-00289. [DOI] [PubMed] [Google Scholar]
- 27.Niva M, Mattila V, Kiuru M, Pihlajamaki H. Bone stress injuries are common in female military trainees. Clin Orthop Relat Res. 2009;467:2962–69. doi: 10.1007/s11999-009-0851-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nguyen JT, Peterson JS, Biswal S, Beaulieu CF, Fredericson M. Stress-related injuries around the lesser trochanter in long-distance runners. AJR. 2008;190:1616–1620. doi: 10.2214/AJR.07.2513. [DOI] [PubMed] [Google Scholar]
- 29.Frusztajer NT, Dhuper S, Warren MP, Brooks-Gunn J, Fox R P. Nutrition and the incidence of stress fractures in ballet dancers. The American journal of clinical nutrition. 1990;51(5):779–783. doi: 10.1093/ajcn/51.5.779. [DOI] [PubMed] [Google Scholar]
- 30.Bennell K, Malcolm SA, Thomas SA, Ebeling PR, McCrory PR, Wark JD, Brukner PD. Risk factors for stress fractures in female track-and-field athletes: a retrospective analysis. 1995. [DOI] [PubMed]
- 31.Bennel K, Matheson G, Meeuwisse W, Brukner P. Risk factors for stress fractures. Sport Med. 1999;28:91–122. doi: 10.2165/00007256-199928020-00004. [DOI] [PubMed] [Google Scholar]
- 32.Consensus development conference. Diagnosis, prophylaxis and treatment of osteoporosis. Am J Med. 1991;90:107–110. [Google Scholar]
- 33.Consensus Development Conference V. Diagnosis, prophylaxis and treatment of Osteoporosis. Ann J Med. 1994;90:646–650. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 34.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. Br Med J. 1996;312:1254–1259. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lassus J, Tulikoura I, Konttinen YT, Salo J, Santavirta S. Bone stress injuries of the lower extremity: a review. Acta Orthop Scand. 2002;73(3):359–68. doi: 10.1080/000164702320155392. [DOI] [PubMed] [Google Scholar]
- 36.Naranje S, Sezo N, Trikha V, Kancherla R, Rijal L, Jha R. Simultaneous bilateral femoral neck stress fractures in a young military cadet: a rare case report. Eur J Orthop Surg Traumatol. 2012;1(22 Suppl):103–6. doi: 10.1007/s00590-011-0864-0. [DOI] [PubMed] [Google Scholar]
- 37.Neubauer T, Brand J, Lidder S, Krawany M. Stress fractures of the femoral neck in runners: a review. Res Sports Med. 2016 doi: 10.1080/15438627.2016.1191489. doi:10.1080/15438627.2016.1191489 1-15. [DOI] [PubMed] [Google Scholar]
- 38.Frizziero A, Vittadini F, Pignataro A, Gasparre G, Biz C, Ruggieri P, Masiero S. 201 Conservative management of tendinopathies around hip. Muscles, Ligaments and Tendons Journal 6. 6(3):281. doi: 10.11138/mltj/2016.6.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maffulli N, Longo UG, Denaro Umile Giuseppe. Femoral neck stress fractures. Operative Techniques in Sports Medicine 17.2. 2009:90–93. [Google Scholar]
- 40.Katsougrakis Ilias, Alexandros P. Apostolopoulos, Samantha Z. Tross. Conservative Management of a Femoral Neck Stress Fracture in a Female Athlete. A Case Report and Review of the Literature. Journal of Long-Term Effects of Medical Implants 26.1. 2016 doi: 10.1615/JLongTermEffMedImplants.2016011991. [DOI] [PubMed] [Google Scholar]
- 41.Shin AY, Morin WD, Gorman JD, Jones SB. The superiority of magnetic resonance imaging in differentiating the cause of hip pain in endurance athletes. Am J Sports Med. 1996;22:168–176. doi: 10.1177/036354659602400209. [DOI] [PubMed] [Google Scholar]
- 42.Blair B, Koval KJ, Kummer F, Zuckerman JD. Basicervical fractures of the proximal femur. A biomechanical study of 3 internal fixation techniques. Clin Orthop. 1994;306:256–263. [PubMed] [Google Scholar]
- 43.Clark DI, Crofts CE, Saleh M. Femoral neck fracture fixation. Comparison of a sliding screw with lag screws. J Bone Joint Surg [Br] 1990;72:797–800. doi: 10.1302/0301-620X.72B5.2211759. [DOI] [PubMed] [Google Scholar]
- 44.Naik MA, Sujir P, Tripathy SK, Vijayan S, Hameed S, Rao SK. Bilateral stress fractures of femoral neck in non-athletes: a report of four cases. Chin J Traumatol. 2013;16(2):113–7. [PubMed] [Google Scholar]
- 45.Pouilles JM, Bernard J, Tremollieres F, Louvet JP, Ribot C. Femoral bone density in young male adults with stress fractures. Bone. 1989;10(2):105–108. doi: 10.1016/8756-3282(89)90006-9. [DOI] [PubMed] [Google Scholar]
- 46.Enocson A, Lapidus LJ. The vertical hip fracture – a treatment challenge. A cohort study with an up to 9 year follow-up of 137 consecutive hips treated with sliding hip screw and antirotation screw. BMC Musculoskelet Disord. 2012;13:171. doi: 10.1186/1471-2474-13-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robertson GA, Wood AM. Femoral Neck Stress Fractures in Sport: A Current Concepts Review. Sports Medicine International Open 1.02. 2017:E58–E68. doi: 10.1055/s-0043-103946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Visuri T, Vara A, Meurman KO. Displaced stress fractures of the femoral neck in young male adults: a report of twelve operative cases. J Trauma. 1988;28:1562–9. doi: 10.1097/00005373-198811000-00007. [DOI] [PubMed] [Google Scholar]
- 49.Johansson C, Ekenman I, Tornkvist H, Eriksson E. Stress fractures of the femoral neck in athletes: the consequence of a delay in diagnosis. The American journal of sports medicine. 1990;18(5):524–528. doi: 10.1177/036354659001800514. [DOI] [PubMed] [Google Scholar]
- 50.Lee C-H, Huang G-S, Chao K-H, Jean J-L, Wu S-S. Surgical treatment of displaced stress fractures of the femoral neck in military recruits: a report of 42 cases. Archives of Orthopaedic and Trauma Surgery. 2003;123(10):527–533. doi: 10.1007/s00402-003-0579-8. [DOI] [PubMed] [Google Scholar]
- 51.Myburgh KH, Hutchins J, Fataar AB, Hough SF, Noakes TD. Low bone density is an etiologic factor for stress fractures in athletes. Annals of internal medicine. 1990;113(10):754–759. doi: 10.7326/0003-4819-113-10-754. [DOI] [PubMed] [Google Scholar]
- 52.Manninger J, Kazar GY, Fekete GY, Nagy E, Zolczer L, Frenyo S. Avoidance of avascular necrosis of the femoral head following fractures of the femoral neck, by early reduction and internal fixation. Injury. 1985;16:437–448. doi: 10.1016/0020-1383(85)90162-7. [DOI] [PubMed] [Google Scholar]
- 53.Manninger J, Kazar G, Fekete G, Fekete K, Frenyo S, Gyarfas F, Salacz T, Varga A. Significance of urgent (within 6 h) internal fixation in the management of fractures of the neck of the femur. Injury. 1989;20:101–105. doi: 10.1016/0020-1383(89)90152-6. [DOI] [PubMed] [Google Scholar]
- 54.Goolsby MA, Barrack MT, Nattiv A. A displaced femoral neck stress fracture in an amenorrheic adolescent female runner. Sports Health. 2012;4:352–356. doi: 10.1177/1941738111429929. [DOI] [PMC free article] [PubMed] [Google Scholar]


