Abstract
Purpose: The aim of this retrospective study was to report the clinical and radiographic results of the biodegradable subacromial spacer (InSpace Balloon®) implantation in patients with massive irreparable rotator cuff tears. Materials and methods: From February 2014 to October 2015, 30 patients affected by massive irreparable rotator cuff tears were treated with the implantation of InSpace Balloon®. Clinical evaluation (Constant Score and VAS), X-rays and MR imaging were performed preoperatively in all patients and 3, 6, 12 and 24 months after surgery, dividing patients in different groups according to the time elapsed from surgery. Results: Constant Score increased from 39.89 to 62.33 points (p 0.0002) in the 6 months group and from 41.66 to 65.38 points (p< 0.0001) in the 12 months group. ROM (Range of Movement) and ADL (Activity of Daily Living) significantly improved with the contemporary reduction of VAS and pain at 12 months and, furthermore, an increase of functional performance with reduction of pain was registered at 24 months. Conclusions: Our results supported the surgical procedure of the arthroscopic implantation of biodegradable subacromial InSpace Balloon® for irreparable massive cuff tears in worker patients and with recreational activities’ demands in order to recover the shoulder function with a reduction of the pain. (www.actabiomedica.it)
Keywords: massive irreparable cuff rotator tears, subacromial biodegradable spacer, shoulder arthroscopy, Constant Scores
Introduction
Rotator cuff tears (RCTs) are age-dependent common injuries affecting millions of people (1). Repair of these lesions is performed safely with arthroscopic techniques and leads to proven clinical benefit. Large lesions are associated with poor results and failure (2). Regarding classifications, in literature there is a distinction between massive and irreparable rotator cuff tears (IRCTs) (3). Massive tears are considered those more than 5 cm, involving two or more tendons, while IRCTs are lesions that cannot be repaired back to the native footprint or that, once repaired, almost certainly lead to a structural failure (4). In clinical diagnosis of IRCTs, static anterosuperior subluxation and associated pseudoparalysis on anterior elevation are suggestive. At the imaging, superior migration of the humeral head with acromiohumeral interval less than 7 mm at x-rays and grade 3 and 4 fatty infiltration according to the Goutallier classification (5) at CT scans is observed.
Several surgical options are available for the treatment of IRCT with the intent of reducing pain and improving functions. These options includes subacromial decompression or debridement, partial tendon repair, tendon transfer, muscle-tendon slide procedures, the use of rotator cuff allograft and synthetic grafts, arthrodesis, hemiarthroplasty and reverse total shoulder arthroplasty (6-7).
One recent arthroscopic alternative is the implant of a biodegradable subacromial spacer, the InSpace balloon (OrthoSpace, Kfar Saba, Israel), initially described by Savarese and Romeo (8), which permits better gliding restoring shoulder kinematics with low rate of complications (9).
Our purpose was to confirm the good results described in the literature with this recently-introduced surgical technique.
Materials and methods
Patient recruitment
This retrospective study is a case series performed in single Institute. From February 2014 to October 2015, 30 patients (17 females, 13 males; mean age 65.7 years) affected by massive irreparable rotator cuff tears (IRCT) were treated with the implantation of InSpace Balloon®.
All patients were fully informed on the characteristics of treatment and gave their written informed consent.
The indication for surgery was made on clinical signs of IRCT and MR imaging (Goutallier3–4) (5) in patients who has persistent pain for at least 6 months after the failure of conservative treatment. Exclusion criteria included shoulder osteoarthritis, glen humeral instability, prior shoulder surgery and shoulder infection.
Patients were divided into 4 different groups based on the follow up’s time: 8 patients were evaluated at 3 months after surgery, 9 patients at 6 months, 8 patients at 12 months, 5 patients at 24 months.
Surgical technique and postoperative management
The same surgeon completed all the procedures. A standard arrangement for arthroscopic rotator cuff repair was used with the patient in a beach-chair position. Standard arthroscopic portals were performed, with biceps tenotomy, sub acromial bursectomy and acromioplasty in all cases. Patients were under general anaesthesia and interscalene block.
The preoperative instrumental diagnosis of irreparable massive rotator cuff tears was confirmed during arthroscopy in all cases. We measured the subacromial space using an arthroscopic probe (provided in the InSpace Balloon System® kit); then we selected the correct implant size choosing between small, medium and large. We prepared the inflating system and filled syringe with 0.9% saline solution pre-heated to 40 degrees Celsius. After Balloon inflation, we verified its stability through full ROM. After surgery patients wore a sling for one week and began full active assisted range of motion and early active ROM at low level; overhead activity was avoided for 6 weeks.
Outcome assessment
The same orthopaedic team performed pre- and post-operatively clinical evaluation. X-rays and MR imaging was performed preoperatively and, depending on groups, at 3, 6, 12 and 24 months after surgery. Clinical evaluation was conducted using the Constant Score (10) and pain was recorded with VAS. Subacromial space was measured on standard AP X-rays (5) by the same senior radiologist.
Statistical analysis
Study data were analysed using SPSS program for Macintosh (20.0 version) and the differences of mean results were evaluated with Wilcoxon T test. P values <0.05 were considered statistically significant.
Results
Clinical preoperative values of Total Constant Score (TCS), pain, Range of Movement (ROM), strength in abduction with dynamometer, ADL (Activity of daily living) and VAS showed no significative differences between groups (Table 1A).
Table 1 .
| A | ||||||||
|---|---|---|---|---|---|---|---|---|
| p value | TCS | PAIN | ROM | Strenght | ADL | VAS | SAS | |
| 3 months | 0,0001 | 0,0037 | 0,0002 | 0,2564 | 0,0037 | 0,0005 | <0,0001 | |
| 6 months | 0,0002 | 0,0153 | 0,0001 | 0,3755 | 0,0001 | 0,0019 | 0,0004 | |
| 12 months | <0,0001 | 0,0032 | <0,0001 | 0,0633 | 0,0074 | 0,0001 | 0,0067 | |
| 24 months | <0,0001 | 0,0072 | <0,0001 | 0,0943 | 0,0462 | 0,0019 | 0,0007 | |
| B | ||||||||
| TCS | Pain | ROM | Strenght | ADL | VAS | SAS | SIZE (CM) | |
| PRE | 39,75 | 2,5 | 33 | 3,5 | 0,75 | 6,13 | 6,61 | |
| PRE | 39,89 | 4,44 | 30 | 4,3 | 1,1 | 6,45 | 6,63 | |
| PRE | 41,66 | 3,75 | 32,5 | 3,88 | 1,75 | 6,25 | 6,45 | |
| PRE | 41,8 | 4 | 32,4 | 3,8 | 1,6 | 6,6 | 6,67 | |
| 3 months | 55,63 | 8,13 | 40,75 | 5 | 3 | 3,38 | 7,99 | 4x7 |
| 6 months | 62,33 | 9,44 | 43,56 | 5,67 | 3,56 | 3,67 | 8,16 | 2,5x7 |
| 12 months | 65,38 | 10,63 | 44,75 | 5,75 | 3,5 | 2,86 | 7,09 | 3x6,5 |
| 24 months | 66,8 | 12 | 45,6 | 6,2 | 3,6 | 2,8 | 7,94 | - |
TCS: Total Costant Score; ROM: Range of motion; SAS: Subacromial space; VAS: Visual analogue scale for pain;
Table 1B shows the mean results for each group of follow-up. We focused on temporary variation of values between preoperative and postoperative outcomes at 3, 6, 12 and 24 months after surgery.
Clinical results
After 3 months we observed a statistically significative improvement of Constant Total Score (from 39.75 to 55.63 points) with positive results in pain, ADL and VAS, without any significative evidence.
Otherwise, we obtained a significative improvement in pain reduction and function at 6 and 12 months. After 6 months the mean TCS significantly improved from 39.89 to 62.33 points (p 0.0002) with a reduction of pain (from 4.44 to 9.44 points, p 0.0153), improvement of ADL (from 1.1. to 3.56 points, p 0.0001); VAS decreased from 6.45 to 3.67 points (p 0.0019).
Size: balloon size measured by MRI; ADL: activity of dayly living
A further increase of values was observed after 12 months, with a mean TCS of 65.38 points (p< 0.0001), a reduction of pain (from 3.75 to 10.63 points, p 0.0032), an increase of ADL (from 1.75 to 3.5 points, p 0.0074) and the statistical improvement of VAS (from 6.23 to 2.86 points, p 0.0001).
After 24 months we registered another slight increase of results: TCS increased to 66.8 points (p<0.0001), there was reduction of pain (score from 4 to 12, p 0.00072), increase of ADL (from 1.6 to 3.6, p<0.046) and VAS (from 6.6 to 2.8, p 0.0019) (Fig. 1).
Figure 1.
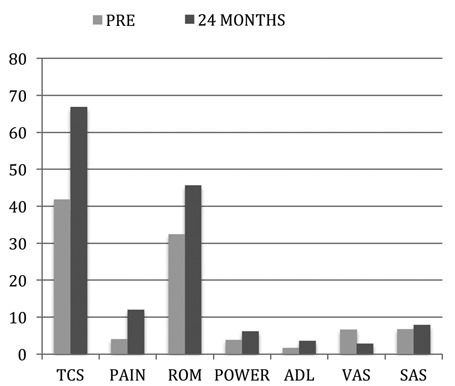
TCS: Total Costant Score; ROM: Range of motion; SAS: Subacromial space; VAS: Visual analogue scale for pain; SIZE: balloon size measured by MRI; ADL: activity of dayly living
Radiographic results
The X-rays analysis showed that acromiohumeral interval raised from 6.61 to 7.99 at 3 months (p<0.0001), from 6.63 to 8.16 at 6 months (p 0.0004), from 6.45 to 7.09 at 12 months (p 0.00067) and from 6.67 to 7.94 at 24 months (p 0.0007).
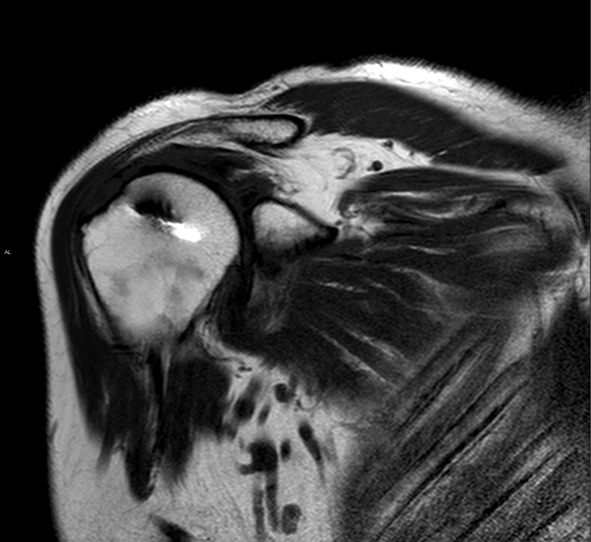
MRI results
We decided to complete the study with the MR description of spacer. At 3 months the implant was evident in subacromial space with a mean width of 4 cm and a thickness of 7 mm (Fig. 2). The radiologist described effusion joint strata at 6 months, while the spacer appeared significantly reduced in volume at 12 months (width decreased to 3 cm and thickness was reduced to 6.5 mm). At the end of follow-up the implant was not recognizable, replaced by a layer of fibrosis with a mean width of 2 cm and a thickness of 4 mm (Fig. 3).
Figure 2.

MRI at 3 months follow up
Figure 3.
MRI at 24 months follow up
Functional results
At 3 months we observed positive results in ROM (from 33 to 40,75 points, p 0.0002) and in strength (from 3.5 to 5 points). After 6 months the improvement of ROM was from 30 to 43.56 points, p< 0.0001 and strength increased from 4.3 to 5.67 points. Moreover a further development of ROM was registered at 12 months (from 32.5 to 44.75 points, p< 0.0001) with strength from 3.88 to 5.7 points. After 24 months there was a slight increase of ROM (from 32.4 to 45.6 points, p< 0.0001) and strength (from 3.8 to 6.2)
Discussion
Based on our results, spacer improves functional outcomes and pain reduction, with a significant increase of Constant Score values (p< 0.002 at 6 months) and VAS (p< 0.015 at 6 months, 2 points at 12 months, p< 0.038), the good outcomes continuing to be maintained at 24 months.
Our results are in line with Senekovic et al (9) that reported an increase of Total Constant Score from 33.4 to 65.4 points on 20 patients treated with InSpace Balloon®, with an evident improvement of power at 18 months (p< 0.003) and of function at 3 years. Similar outcomes were obtained by Naggar et al (11). In a mean follow-up of 24 months good and excellent results were reported in 86% of patients, with pain relief and a recovery often after six weeks. Furthermore he registered an increase of active and painless ROM. The Constant Score almost doubled and the improvement continued up to 18 months after surgery. These authors support the advantages of subacromial spacer described by Szollosy et al in 2014 (12).
Analyzing X-ray and MR imaging, all patients presented before surgery an acromiohumeral distance less than 6 mm and grade lesion 3–4 according to Goutallier, while postoperative the space always was > 7 mm. The same measures were reported on Australian Safety and Efficacy Register of New International Procedures-Surgical in December 2014 end March 2015 (13). However, to complete this data we analysed MR imaging in the postoperative period. From 6 to 12 months the spacer was visible but progressively smaller-sized, and contemporary inflammatory stratus absorption was obseved. Furthermore, we observed that the degradation process started over 12 months to be completed at 24 months, like Savarese et al argued in 2012 (8). These radiological data can support clinical trends observed in our study and they can complete results described by Senekovic and Naggar (9-11).
In literature there are other different surgical options proposed to treat IRCT when no-operative solutions have failed.
Neviaser et al were the first that used the graft interposition with good or excellent clinical results (14) but other authors criticized this procedure for the lack of pain relief and poor clinical outcomes (15).
Rockwood and Kempf studied the outcomes of debridement with or without biceps tenotomy (16-17); although they found good clinical results, a variety of studies showed no advantages in osteoarthritis progression (4).
In 1993 Burkhart et al (18) introduced the partial repair of rotator cuff with the concept of “suspension bridge”. This option obtained improvements in active elevation (from 59.6° to 150.4°) and in the UCLA Score (from 9.8 to 27.6 points). Afterwards Duralde et al reported significant increase in ASES Index, pain and activation (19).
Another technique is the “interval slide” proposed by Tauro and Lo (20-21). Nevertheless Kim el al found 91% of retear rate and patients who underwent this operation did not showed significative reduction of pain or improve of functional outcomes (22).
The arthroscopic superior capsule reconstruction recently described by Mihata (23) was preferred to the graft that can develop an interposition to the torn tendon with a consequent impingement.
Unfortunately all these studies were conducted on small cohort of patients without control group.
Further researches are necessaries to provide definitive guidelines in the treatment of IRCT, a challenging condition that reduces life performance of adult with working and recreational demands.
Despite lack of strong evidences about the superiority of one technique, the implantation of a biodegradable spacer (InSpace technology) could be the last and functional solution (24-25).
Conclusions
This study shows that subacromial biodegradable spacer is a minimally invasive procedure with good mid term clinical and instrumental results in irreparable rotator cuff tears. The improvement of Constant Score, VAS and shoulder function allows to assert that InSpace Balloon® can be considered as a valid surgical option in patients with irreparable rotator cuff tears especially in order to postpone more invasive procedures.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Tonino PM, Gerber C, Itoi E, Porcellini G, Sonnabend D, Walch G. Complex shoulder disorders: evaluation and treatment. J Am Acad Othop Surg. 2009;17:125–36. doi: 10.5435/00124635-200903000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Flurin PH, Landreau P, Gregory T, et al. Arthroscopic repair of full-thickness cuff tears: A multicentric retrospective study of 576 cases with anatomical assessment. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:31–42. doi: 10.1016/s0035-1040(05)84503-9. [in French] [DOI] [PubMed] [Google Scholar]
- 3.Omid R, Lee B. Tendon transfers for irreparable rotator cuff tears. J Am Acad Orthop Surg. 2013;21:492–501. doi: 10.5435/JAAOS-21-08-492. [DOI] [PubMed] [Google Scholar]
- 4.Gerber C, Wirth SH, Farshad M. Treatment options for massive rotator cuff tears. J Shoulder Elbow Surg. 2011;20:S20–S29. doi: 10.1016/j.jse.2010.11.028. [DOI] [PubMed] [Google Scholar]
- 5.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 6.Moser M, Jablonski MV, Horodyski M, Wright TW. Functional outcome of surgically treated massive rotator cuff tears:A comparison of complete repair, and debridment. Orthopedics. 2007;30:479–82. doi: 10.3928/01477447-20070601-05. [DOI] [PubMed] [Google Scholar]
- 7.Goutallier D, Le Guilloux P, Postel JM, Radier C, Bernageau J, Zilber S. Acromio humeral distance less than six millimeter: its meaning in full-thickness rotator cuff tear. Orthopaedics & Traumatology: Surgery & Research. 2011;97:246–51. doi: 10.1016/j.otsr.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Savarese E, Romeo R. New solution for massive, irreparable rotator cuff tears: the subacromial “biodegradable spacer”. Arthrosc Tech. 2012;1:e69–e74. doi: 10.1016/j.eats.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Senekovic V, Poberaj B, Kovacic L, Mikek M, Adar E, Dekel A. Prospective clinical study of a novel biodegradable sub-acromial spacer in treatment of massive irreparable rotator cuff tears. Eur J Orthop Surg Traumatol. doi: 10.1007/s00590-012-0981-4. doi 10.1007/s00590-012-0981-4. [DOI] [PubMed] [Google Scholar]
- 10.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Othop and Relat Res. 1987;214:160–4. [PubMed] [Google Scholar]
- 11.Naggar L. The balloon, a new revolutionary technique for massive irreparable rotator cuff tears: preliminary results at 1 year follow-up, after balloon degradation. Swiss Medical Weekly [serial on the Internet] 2013;(Supp. 198):143. [Google Scholar]
- 12.Szollosy G, Rosso C, Fogerty S, Petkin K, Lafosse L. Subacromial spacer placement for protection of rotator cuff repair. Arthrosc Tech. 2014;5:e605–e609. doi: 10.1016/j.eats.2014.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Australian Safety and Efficacy Register of New Interventional Procedures-Surgical (ASERNIP-S) March 2015. Available from: http://www.health.qld.gov.au/healthpact .
- 14.Neviaser JS, Neviaser RJ, Neviaser TJ. The repair of chronic massive ruptures of the rotator cuff of the shoulder by use of a freeze-dried rotator cuff. J Bone Joint Surg Am. 1978;60:681–4. [PubMed] [Google Scholar]
- 15.Nasca RJ. The use of freeze-dried allograft in the management of global rotator cuff tears. Clin Orthop Relat Res. 1988;228:218–26. [PubMed] [Google Scholar]
- 16.Rockwood CA, Williams GR, Burkhead WZ. Debridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am. 1995;77:857–66. doi: 10.2106/00004623-199506000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Kempf JF, Gleyze P, Bonnomet F, Walch G, Mole D, Frank A, Beaufils P, Levigne C, Rio B, Jaffe A. A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy. 1999;15:56–66. doi: 10.1053/ar.1999.v15.015005. [DOI] [PubMed] [Google Scholar]
- 18.Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder’s “suspension bridge”. Arthroscopy. 1993;9:611–6. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 19.Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14:121–7. doi: 10.1016/j.jse.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 20.Tauro JC. Arthroscopic “interval slide” in the repair of large rotator cuff tears. Arthroscopy. 1999;15:527–30. doi: 10.1053/ar.1999.v15.0150521. [DOI] [PubMed] [Google Scholar]
- 21.Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004;20:22–3. doi: 10.1016/j.arthro.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 22.Kim SJ, Kim SH, Lee SK, Seo JW, Chun YM. Arthroscopic repair of massive contracted rotator cuff tears: aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Joint Surg Am. 2013;95:1482–8. doi: 10.2106/JBJS.L.01193. [DOI] [PubMed] [Google Scholar]
- 23.Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Kinoshita M. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–70. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 24.Sartoretti C, Sartoretti-Schefer S, duff C, Buchmann P. Angioplasty balloon catheters used for distraction of the ankle joint. Arthroscopy. 1996;12:82–6. doi: 10.1016/s0749-8063(96)90224-8. [DOI] [PubMed] [Google Scholar]
- 25.Kilinc AS, Ebrahimzadeh MH, Lafosse L. Subacromial internal spacer for rotator cuff tendon repair: “The balloon technique”. Arthoscopy. 2009;25:921–4. doi: 10.1016/j.arthro.2009.02.017. [DOI] [PubMed] [Google Scholar]


