Abstract
One of the most important benign tumors in neurofibromatosis type 1 (NF1) is plexiform neurofibroma, and there is a risk of developing malignant peripheral nerve sheath tumor (MPNST) throughout life approximately 10%. However lesion characterization by anatomical imaging methods are not possible. Because of that most of cases goes to biopsy. Using of fluorodeoxyglucose-positron emission tomography/computed tomography (FDG-PET/CT) for lesion characterization can be helpful in NF1 patients. We aimed to present an example of the efficacy of FDG-PET/CT in distinguishing benign neurofibroma from MPNST. A 6-year-old male patient who had NF1 admitted to emergency service due to high fever. Acute upper respiratory tract infection was diagnosed; antipyretic and abundant fluid intake was suggested. When high fever continued, the patient referred to our hospital on detection of axillary lymphadenopathy. Leukocytosis was detected in patient's blood count. Sedimentation was 54 mm/h, C-reactive protein 166 g/L, and lactate dehydrogenase 276U/L. Blood and throat cultures did not show pathogenic bacteria. In serological tests, VZV-IgG, EBV-VCA-IgG, and CMV-IgG were avidite positive; Hepatitis B Ag, Anti-HIV, Anti-HAV IgG and IgM, Anti-HCV, EBV-VCA IgM, and VZV-IgM were negative. Based on these results, cervical and thoracic contrast-enhanced computed tomography was performed on preliminary diagnosis of MPNST. Solid lesions with rounded margins, large one being 49 mm in size, that extend from superior mediastinum to posterior mediastinum, left axillary region, and left part of neck were detected, and they were surrounding the vascular structures. Since neurofibroma, MPNST, and lymphoma could not be distinguished, patient referred to FDG-PET/CT scanning. In FDG-PET/CT, highest lesion maximum standardized uptake value (SUVmax) was 1.5; SUVmax lesion/SUVmax liver 1.0, and SUVmax/ SUV mean liver 1.5. Biopsy from mediastinal and axillary region did not have LN structure and was positive for S-100 immunostaining, and patient was diagnosed as benign neurofibroma. We believe that there is no need for biopsy in lesions considered benign based on FDG-PET/CT parameters.
Keywords: Malignant peripheral nerve sheath tumor, neurofibromatosis, positron-emission tomography/computed tomography
INTRODUCTION
Neurofibromatosis type 1 (NF1) is an autosomal dominant disease with 1/3500 prevalence and associated with malignant or benign tumors. One of the most important benign tumors in the NF1 patients is plexiform neurofibroma, and there is a risk of developing malignant peripheral nerve sheath tumor (MPNST). This risk is 1.6/1000 per annum, and MPNST develops throughout the life of approximately 10% of the cases diagnosed with NF1. About 80% of cases are males and more frequently seen in ages between 20 and 50.[1,2,3]
There are no any specific findings in physical examination and imaging is required most of time in these patients characterization. Anatomical imaging methods can be used, but they are not effective enough in distinguishing malignant from benign lesions.[4] Therefore, some researchers describe lesion characterization without histopathologic examination as “challenging” in these cases.[5] Biopsy, especially from deeply located lesions, is a laborious process both for the patient and surgeon. Recent studies reported that use of flourodeoxyglucose-positron emission tomography/computed tomography (FDG-PET/CT) for lesion characterization can be helpful.[3,6] In NF1 patients, ability of FDG-PET/CT to distinguish malignant from benign lesions with high accuracy can reduce the number of invasive procedures for diagnosis, thereby patient will be spared from unnecessary invasive procedures and their possible complications; there won’t be any loss of time and cost for the health professionals as well as the insurance system.
We aimed to present an example of the efficacy of FDG-PET/CT in distinguishing benign neurofibroma from MPNST.
Case Report
A 6-year-old male patient who had NF1 was admitted to emergency service due to high fever. Acute upper respiratory tract infection was diagnosed; antipyretic and abundant fluid intake was suggested. Since high fever continued, the patient was referred to our hospital on detection of axillary lymphadenopathy. Leukocytosis was detected in patient's blood count. Sedimentation was 54 mm/h, C-reactive protein 166 g/L, and lactate dehydrogenase 276 U/L. Blood and throat cultures did not show pathogenic bacteria. In serological tests, VZV-IgG, EBV-VCA-IgG, and CMV-IgG were avidite positive; Hepatitis B Ag, Anti-HIV, Anti-HAV IgG and IgM, Anti-HCV, EBV-VCA IgM and VZV-IgM were negative. Based on these results, cervical and thoracic contrast-enhanced computed tomography (CT) was performed on preliminary diagnosis of MPNST. Solid lesions with rounded margins, the large one being 49 mm in size, that extend from superior mediastinum to posterior mediastinum, left axillary region, and left part of the neck were detected, and they were surrounding the vascular structures in CT [Figure 1]. Since neurofibroma to MPNST could not be distinguished, the patient was referred to FDG-PET/CT scanning. In FDG-PET/CT, highest lesion maximum standardized uptake value (SUVmax) was 1.5; SUVmax lesion/SUVmax liver 1.0, and SUVmax/mean SUV (SUVmean) liver 1.5 [Figure 2]. Since material from the biopsy from mediastinal and axillary region did not have LN structure and was positive for S-100 immunostaining, the patient was diagnosed as benign neurofibroma.
Figure 1.
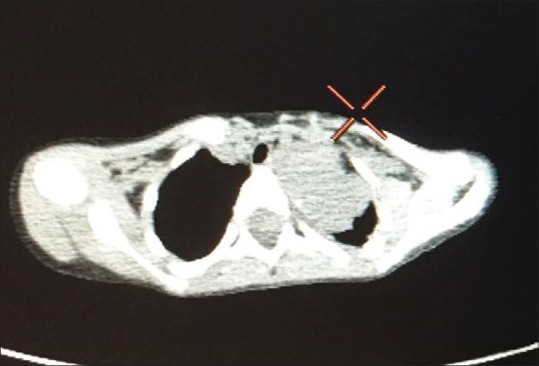
Computed tomography imaging of neurofibroma in mediastinum and axilla
Figure 2.
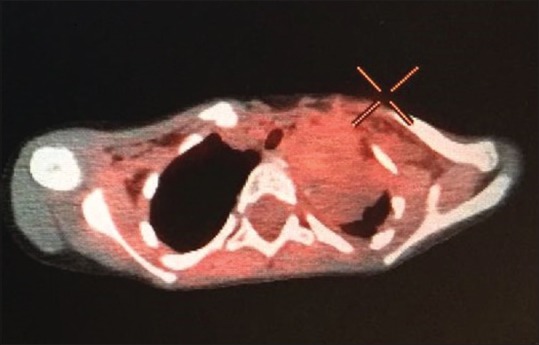
Positron emission tomography/computed tomography imaging of neurofibroma in mediastinum and axilla
DISCUSSION
NF1 is an autosomal dominant disease, and incidence of malignancy in these patients is considerably higher than normal population. As reported by Walker et al., risk of malignancy in NF1 patients under 20 years of age is about 28 times greater than normal population.[3] MPNST is a common malignancy in these patients, with 8.3% of patients with neurofibromas or MPNST have tumoral tissues in the thorax, and malignant potentials of neurofibromas located in deep tissues of the body are reported to be higher.[7,8] Therefore, it is of great importance to characterize lesion as quickly as possible with noninvasive methods.
An irregular contour or contrast agent enhancement, which are among the symptoms visualized by anatomic imaging methods suggesting malignancy, can also be observed in plexiform neurofibromas.[4,9] When the relationship between lesion size and malignancy is examined, an overlap between studies is noteworthy. For example, while Matsumine et al. reported mean benign tumor size as 69 mm, Demehri et al. reported it as 39 mm and the mean MPNST size as 63 mm.[8,9] It is noteworthy that value given for malignant tumors in the second study is rather small compared to the value given for benign tumors in the first study. The largest lesion in our study is approximately 5.0 cm, making it difficult to make a clear distinction with respect to size. Studies have been undertaken especially in recent years regarding the usefulness of FDG-PET/CT in this regard. Tovmassian et al. found that mean SUVmax of benign neurofibromas was 1.93 and MPNST was 7.48.[4] Similarly, Ferner et al. reported mean value of SUVmax as 1.5 for plexiform neurofibromas and 5.7 for MPNST.[6] This difference suggests that a cutoff can be given for plexiform neurofibroma and MPNST distinction. On this subject, Warbey et al. reported SUVmax cutoff value of 3.5 would be an appropriate approach.[5] However Salomon et al. suggested >5.5 as a cut-off for SUVmax. With this cut-off they found 95% sensitivity and 85% specificity. SUVmax of 1.5 detected in our case was evaluated as compatible with the benign lesion, based on all of the cutoff values given above.
Apart from SUVmax, some other parameters have also analyzed for lesion characterization. In lesions with a SUVmax tumor/liver <1.5, Combemale et al. calculated 98.8% negative predictive value. On the other hand, in the same study, 25 of 65 lesions with the ratio >1.5 were found to be benign tumors.[7] In a study that looked at SUVmax lesion/SUVmean liver, cutoff >2.6 was suggested. In this study, sensitivity was 100% and specificity was 87%.[10] SUVmax lesion/liver and SUVmax lesion/SUVmean liver of our case were below all of the abovementioned cutoffs, and lesions in our patient were benign according to FDG-PET/CT. Histopathological examination confirmed this result.
CONCLUSION
We think that there is no need for biopsy in lesions considered benign based on FDG-PET/CT parameters in the differential diagnosis of benign neurofibroma from MPNST. Thus, by not performing any invasive procedures, patient comfort can be ensured, time and cost savings can be achieved.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hersh JH American Academy of Pediatrics Committee on Genetics. Health supervision for children with neurofibromatosis. Pediatrics. 2008;121:633–42. doi: 10.1542/peds.2007-3364. [DOI] [PubMed] [Google Scholar]
- 2.Kransdorf MJ. Malignant soft-tissue tumors in a large referral population: Distribution of diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164:129–34. doi: 10.2214/ajr.164.1.7998525. [DOI] [PubMed] [Google Scholar]
- 3.Walker L, Thompson D, Easton D, Ponder B, Ponder M, Frayling I, et al. A prospective study of neurofibromatosis type 1 cancer incidence in the UK. Br J Cancer. 2006;95:233–8. doi: 10.1038/sj.bjc.6603227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tovmassian D, Abdul Razak M, London K. The role of [18F] FDG-PET/CT in predicting malignant transformation of plexiform neurofibromas in neurofibromatosis-1hindawi publishing corporation. Int J Surg Oncol. 2016;2016:7. doi: 10.1155/2016/6162182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warbey VS, Ferner RE, Dunn JT, Calonje E, O’Doherty MJ. [18F] FDG PET/CT in the diagnosis of malignant peripheral nerve sheath tumours in neurofibromatosis type-1. Eur J Nucl Med Mol Imaging. 2009;36:751–7. doi: 10.1007/s00259-008-1038-0. [DOI] [PubMed] [Google Scholar]
- 6.Ferner RE, Golding JF, Smith M, Calonje E, Jan W, Sanjayanathan V, et al. [18F] 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG PET) as a diagnostic tool for neurofibromatosis 1 (NF1) associated malignant peripheral nerve sheath tumours (MPNSTs): A long-term clinical study. Ann Oncol. 2008;19:390–4. doi: 10.1093/annonc/mdm450. [DOI] [PubMed] [Google Scholar]
- 7.Combemale P, Valeyrie-Allanore L, Giammarile F, Pinson S, Guillot B, Goulart DM, et al. Utility of 18F-FDG PET with a semi-quantitative index in the detection of sarcomatous transformation in patients with neurofibromatosis type 1. PLoS One. 2014;9:e85954. doi: 10.1371/journal.pone.0085954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsumine A, Kusuzaki K, Nakamura T, Nakazora S, Niimi R, Matsubara T, et al. Differentiation between neurofibromas and malignant peripheral nerve sheath tumors in neurofibromatosis 1 evaluated by MRI. J Cancer Res Clin Oncol. 2009;135:891–900. doi: 10.1007/s00432-008-0523-y. [DOI] [PubMed] [Google Scholar]
- 9.Demehri S, Belzberg A, Blakeley J, Fayad LM. Conventional and functional MR imaging of peripheral nerve sheath tumors: Initial experience. AJNR Am J Neuroradiol. 2014;35:1615–20. doi: 10.3174/ajnr.A3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salamon J, Papp L, Tóth Z, Laqmani A, Apostolova I, Adam G, et al. Nerve sheath tumors in neurofibromatosis type 1: Assessment of whole-body metabolic tumor burden using F-18-FDG PET/CT. PLoS One. 2015;10:e0143305. doi: 10.1371/journal.pone.0143305. [DOI] [PMC free article] [PubMed] [Google Scholar]


