Abstract
Bark extracts from the Amazonian rain forest tree Geissospermum vellosii (pao pereira), enriched in α-carboline alkaloids have significant anticancer activities in certain preclinical models. Because of the predominance of prostate cancer as a cause of cancer-related morbidity and mortality for men of Western countries, we preclinically tested the in vitro and in vivo effects of a pao pereira extract against a prototypical human prostate cancer cell line, LNCaP. When added to cultured LNCaP cells, pao pereira extract significantly suppressed cell growth in a dose-dependent fashion and induced apoptosis. Immunodeficient mice heterotopically xenografted with LNCaP cells were gavaged daily with pao pereira extract or vehicle control over 6 weeks. Tumor growth was suppressed by up to 80% in some groups compared with tumors in vehicle-treated mice. However, we observed a striking U-shaped dose-response curve in which the highest dose tested (50 mg/kg/d) was much less effective in inducing tumor cell apoptosis and in reducing tumor cell proliferation and xenograft growth compared with lower doses (10 or 20 mg/kg/d). Although this study supports the idea that a pao pereira bark extract has activity against human prostate cancer, our in vivo results suggest that its potential effectiveness in prostate cancer treatment may be limited to a narrow dose range.
Keywords: pao pereira, preclinical, prostate cancer
Numerous chemotherapeutic agents used in the treatment of cancer were originally derived from plants. Such agents include the vinka alkaloids, extracted from the Madagascar periwinkle; taxanes, extracted from Pacific yew tree bark; etoposide, extracted from the may-apple plant; and irinotecan and topotecan, extracted from Camptotheca acuminata. In a similar manner, Beljanski and Crochet proposed that extracts of the bark of an Amazonian rain forest tree, Geissospermum vellosii Allemão (familiarly known as pao pereira), used medicinally by South American Indian tribes, might have activity against human tumors.1–3 In preliminary investigations, Beljanski and Crochet demonstrated that pao pereira bark extract suppressed the in vitro growth of several human cancer cell lines, including ones derived from melanoma and glioblastoma.1–3 Pao Pereira bark extract is enriched for alkaloids of the β-carboline family. These types of alkaloids have been shown to be cytotoxic for cancer cells, and their mechanism of action may involve the targeting of cyclin-dependent kinases (CDKs).3–5 None of the previous studies on pao pereira bark extracts involved human prostate cancer cell lines, so here we report our preclinical studies to test whether a standardized extract of pao pereira bark might affect the in vitro or in vivo growth of a prototypic human prostate cancer cell line, LNCaP.
Our focus on prostate cancer derives from the predominance of this cancer as a health concern for men in Western countries. Prostate cancer is the most frequently diagnosed malignancy in males and a leading cause of cancer deaths in men.6 Given the relatively high frequency with which prostate cancer occurs, prevention offers the most likely means to reduce the health risk to men posed by the disease. If pao pereira bark extract has tumor-suppressing activity for prostate cancer without overt toxicity, one can consider the possibility that it might be used as a preventive agent as a dietary supplement. Moreover, there is a great need for better therapeutic agents to treat advanced (metastatic) prostate cancer. Although hormone therapy is the standard for men with this stage of disease, it is mainly a palliative treatment that loses effectiveness over time. Once prostate cancer progresses to the hormone-refractory stage, few chemotherapeutic agents are known to affect patient survival. Recently, it was shown that a combination of docetaxel, a paclitaxel (Taxol) derivative, with estramustine does offer some therapeutic advantage for hormone-refractory prostate cancer patients, but the survival gained is limited to a few months at most.7 Therefore, there is good reason to consider whether natural agents that act by mechanisms different from the chemotherapeutics now in use might help prostate cancer patients. In this regard, we had previously used LNCaP cells to identify the anti–prostate cancer activity of a β-carboline alkaloid–rich extract of another medicinal plant, Rauwolfia vomitoria.8 In contrast to our findings with Rauwolfia extracts, however, we report herein results showing a striking discrepancy involving the effectiveness of escalated doses of pao pereira extract for in vivo tumor growth inhibition. Our results suggest that the pao pereira extract might differ fundamentally from the β-carboline-rich extracts of other medicinal plants.
Methods and Materials
Pao Pereira Extracts
All experiments were conducted with a proprietary extract of pao pereira bark enriched in β-carboline alkaloids (Natural Source International, Ltd., New York, NY). A single batch of the extract, which was determined by high-performance liquid chromatrography analysis to contain 54% β-carboline alkaloids, was used. The pao pereira extract was dissolved in 6% dimethyl sulfoxide (DMSO) in water and was filtered through a 0.2 μm membrane. The final concentration of DMSO following dilution in cell culture was 0.12%. A stock solution of 6% DMSO was used for vehicle controls.
Cell Culture
The androgen-sensitive human prostate cancer LNCaP cells were obtained from the American Type Culture Collection (Manassas, VA) and were grown in RPMI-1640 medium with l-glutamine (GIBCO Invitrogen Corp., Carlsbad, CA), supplemented with 10% fetal bovine serum and 100 mg/L erythromycin (Sigma-Aldrich, St. Louis, MO). The cells were maintained at 37°C in a humidified atmosphere of 95% air and 5% CO2.
Cell Growth Assays
LNCaP cells were seeded in 96-well plates at a density of 5,000 cells per well in a final volume of 100 μL. Twenty-four hours later, the medium was replaced with 100 μL of fresh medium containing different concentrations of pao pereira extract (100, 250, and 500 μg/mL) or vehicle (n = 8 for each condition). WST-1 labeling solution (WST-1 Cell Proliferation Assay Kit, Roche Diagnostics, Indianapolis, IN) was added at 24, 48, or 72 hours following the addition of the extract. Three hours later, formazan product was detected at 420 nm in a spectrophotometric plate reader (Tecan, Männedorf, Switzerland). Each experiment was repeated in triplicate.
Cell Cycle Analysis
Cultured LNCaP prostate cancer cells were exposed to various concentrations of pao pereira extract for 24 hours. Adherent cells were trypsinized and pooled with the cells in suspension, centrifuged, and washed twice with ice-cold phosphate-buffered saline. A fraction of washed cells was stained with trypan blue and counted. The cells were adjusted to 1 million cells per milliliter and fixed in a 2:1 ratio (vol/vol) of chilled ethanol overnight before staining with propidium iodide in the presence of ribonuclease. Cell cycle distribution was analyzed on a Becton Dickinson Flow Cytometer (BD Biosciences, San Jose, CA), and 10,000 cells were analyzed for each experimental condition. Data analysis was performed using the CellQuest cell cycle analysis software (BD Biosciences).
Generation of Tumor Xenografts and Oral Gavage with Pao Pereira Extract
LNCaP tumor xenografts were generated in 4- to 5-week-old male athymic nude mice (nu/nu; Harlan Inc., Indianapolis, IN). Mice were randomized into four groups of eight each. Following 3-day acclimation, freshly harvested LNCaP cells were xenografted subcutaneously over the right flank of the mice as previously described.8 Oral gavage (0.5 mL) was initiated 48 hours following xenografting, as follows: (1) vehicle control (0.12% DMSO); (2) 10 mg/kg pao pereira extract; (3)20 mg/kg pao pereira extract; or (4) 50 mg/kg pao pereira extract. Gavage was performed 6 days per week at the same time per day for 6 weeks. Tumor volumes were calculated one to two times per week using caliper measurements of length, width, and depth [volume = (πxh) × (h2 + 3a2)/6, a = (L + W)/4].9 Mice were injected subcutaneously with a 10 mM solution of bromodeoxyuridine (BrdU) at a dose of 15 μL/g body weight 4.5 hours prior to euthanasia. Tumors were then removed, fixed for 24 hours in 10% formalin solution, paraffin embedded, and sectioned onto glass slides for immunohistochemical analyses.
Immunohistochemical Analysis of Tumor Xenografts
Tumor sections were stained for BrdU incorporation using the In Situ Cell Proliferation Kit II POD (Roche Applied Sciences, Indianapolis, IN) and were counterstained with methyl green. TUNEL immunostaining was conducted on sequential sections using the In Situ Cell Death Detection Kit POD (Roche Applied Sciences, Indianapolis, IN). Sections were counterstained with Harris hematoxylin. Slides were imaged under a light microscope (×200 magnification), and images were captured using a SPOT insight color digital camera and analysis software (Diagnostic Instruments). Positive nuclei were counted to determine the apoptotic and proliferation indices, as previously described.8
Statistical Evaluation of Data
Statistical methods used to analyze the data consisted of the Student t-test, analysis of variance (ANOVA) techniques, and the Kruskal-Wallis test. All tests were two-sided and conducted at the .05 level of significance.
For the in vitro studies, the outcomes of interest were cell growth, cell cycle progression, and cell death. The Student t-test was used to determine if the pao pereira extract induced significant effects on these outcomes in comparison with the control conditions. For the in vivo study, outcomes of interest were rate of change in log tumor volume over time, change in final log tumor volume from baseline, baseline and final tumor volume, and percent positive staining nuclei per total cells for the BrdU and TUNEL assays. Owing to the skewed nature of some of the tumor volume–related outcomes, the Kruskal-Wallis test was applied to assess differences among the dose groups where appropriate. Log tumor volume measurements over time for the different treatment groups were also presented graphically. Differences in percent positive staining nuclei per total cells between control and pao pereira–treated mice for both BrdU and TUNEL assays were assessed using a Student t-test.
Results
Effects of Pao Pereira Extract on LNCaP Cell Growth and Apoptosis In Vitro
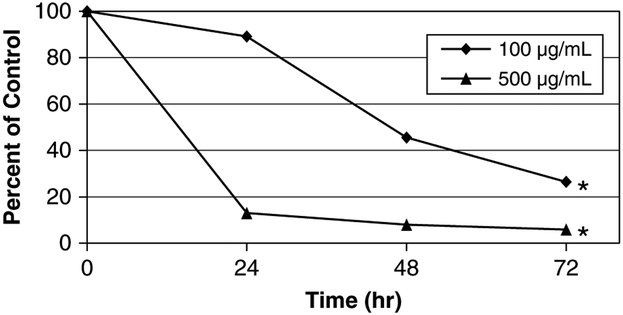
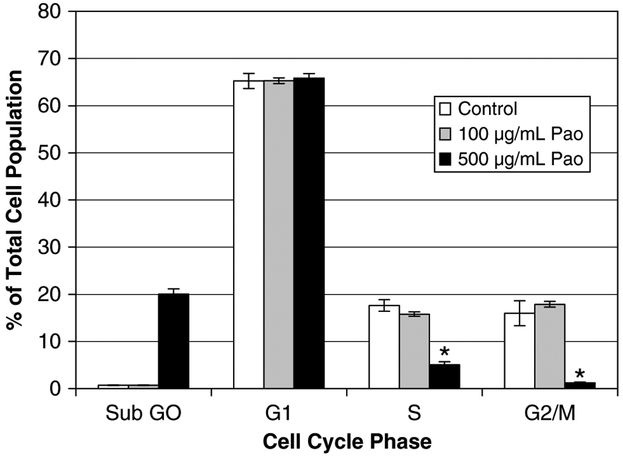
In vitro growth of LNCaP cells was significantly reduced following treatment with 100 or 500 μg/mL pao pereira extract (p < .001, Student t-test) compared with vehicle-treated cells (Figure 1). There was a striking dose-dependent difference in growth inhibition between the 100 and 500 μg/mL doses, with a greater than 90% suppression of growth at the 500 μg/mL dose. Fluorescence-activated cell sorter (FACS) analysis showed that there was no significant effect on the overall cell cycle distribution of cells treated at 100 μg/mL; however, at 500 μg/mL, there was a significant reduction in the percentage of cells in the S and G2/M phases of the cell cycle and increased accumulation in the sub-G1/G0 population (cells containing subgenomic levels of deoxyribonucleic acid [DNA]) (Figure 2). The increased number of cells in sub-G1/G0 indicated that the 500 μg/mL dose induced cell death that was not observed at 100 μg/mL. To determine if the cell death was the consequence of apoptosis, protein lysates from pao pereira–treated (500 μg/mL) or control cells were analyzed for the presence of cleaved poly (adenosine diphosphate [ADP]-ribose) polymerase (PARP) by Western blot analysis. Extensive PARP cleavage was observed in cells treated for 24 hours with pao pereira but not in control cells (data not shown).
Figure 1.
Pao pereira extract suppresses in vitro cell growth in the human prostate cancer cell line LNCaP. *p < .001, Student t-test.
Figure 2.
Analysis of LNCaP cell cycle progression following 24-hour treatment with pao pereira extract. *p < .01, Student t-test.
In Vivo Effects of Pao Pereira on LNCaP Xenograft Volume and Tumor Cell Proliferation or Apoptosis
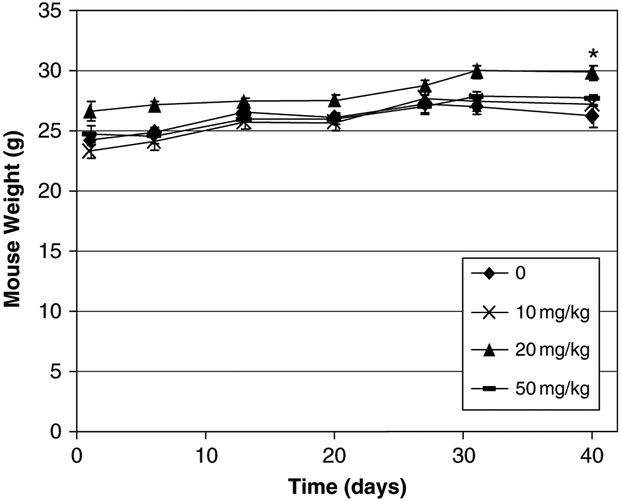
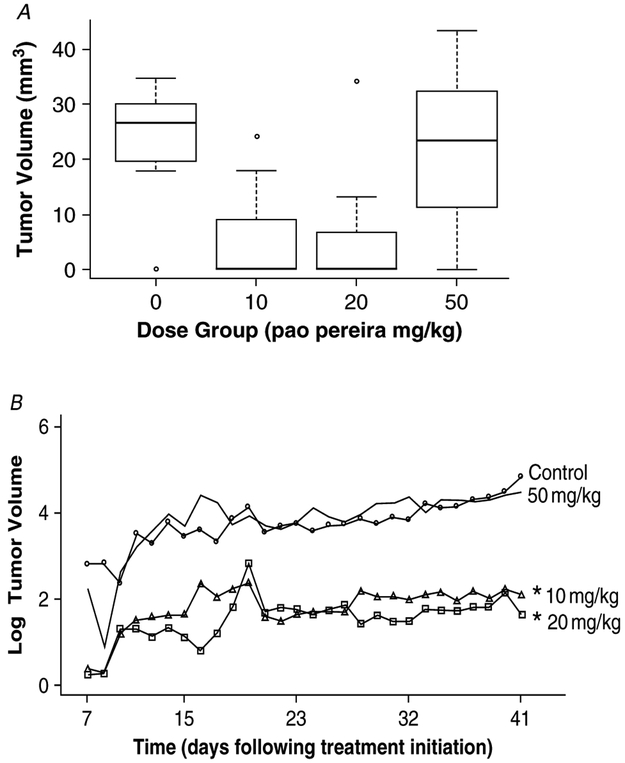
To determine if the pao pereira extract could suppress the in vivo growth of LNCaP tumor xenografts, male immuno-deficient mice were subcutaneously xenografted with 1 × 106 LNCaP cells and the mice were randomly divided into groups, each of which was gavaged daily with vehicle or with 10, 20, or 50 mg/kg/d of the pao pereira extract. The extract did not appear to affect the overall health of the mice as no significant difference in weight was observed over the study period across the treatment or control groups (ANOVA-based F-test, p = .3852) (Figure 3). However, the tumor volumes at the first measurement were already significantly lower in the 10 and 20 mg/kg treated groups (Figure 4; Kruskal-Wallis test, p = .025). Also, by the end of the experiment, median tumor volumes in the 10 and 20 mg/kg treatment groups were decreased by 80% and 75%, respectively, compared with the vehicle control group (Kruskal-Wallis test, p = .021). The tumor-suppressing effect of the pao pereira extract was apparently lost at the highest dose (50 mg/kg/d) as the distribution of tumor volume at both baseline and the end of the study in this group was not statistically different from that of vehicle-treated controls.
Figure 3.
Average mouse weights of the pao pereira treatment and control groups. *p = .3852, ANOVA-based F-test.
Figure 4.
Effect of pao pereira extract (10, 20, and 50 mg/kg) on LNCaP tumor xenograft growth in immunodeficient mice A, Box plot of baseline tumor volumes for control and pao pereira treatment groups. A statistically significant difference was observed across all dose groups (p = .025, Kruskal-Wallis test). B, Overall tumor volume in mouse xenografts was reduced in 10 mg/kg and 20 mg/kg pao pereira–treated mice. *p = .005, ANOVA (median log tumor volume).
Change in tumor volume over time was evaluated by considering both the rate of change in log tumor volume and the difference in final log tumor volume from baseline (see Figure 4B). There was no evidence of differences in tumor volume behavior over time across the dosing groups for these two outcomes (p = .792 and p = .682, respectively). These results then suggest that the 10 mg/kg and 20 mg/kg doses slowed the ability of the tumor cells to establish themselves and grow within the subcutaneous environment of the mice compared with the control or the 50 mg/kg treatment group.
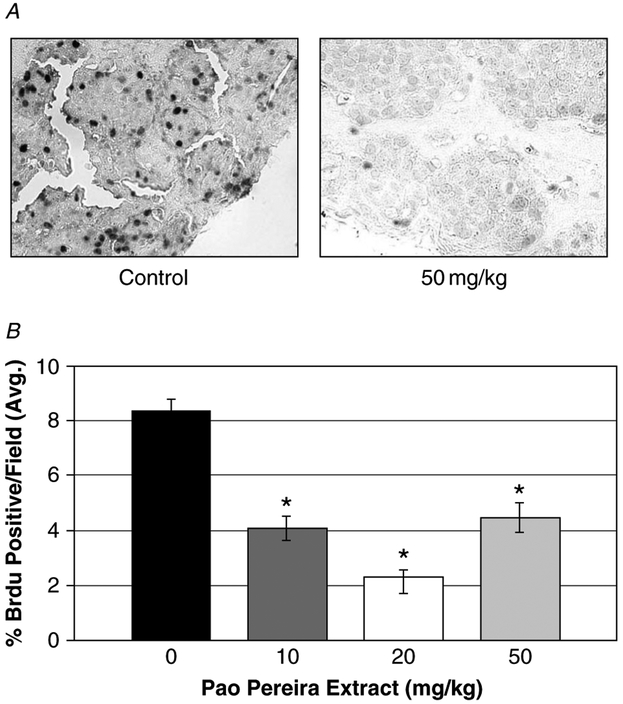
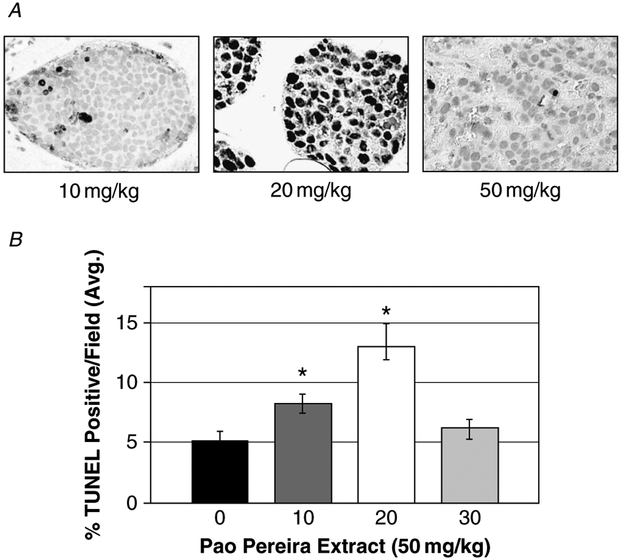
The effect of the extract on tumor cell proliferation was analyzed by immunohistochemical detection of BrdU incorporation into tumor cell nuclei. A quantitative assessment of the average number of BrdU-positive nuclei revealed that all treatment groups induced statistically significant reductions in overall tumor cell BrdU incorporation, as shown in Figure 5 (Student t-test, p < .001). The 10 mg/kg and 20 mg/kg extract reduced tumor cell proliferation by 52% and 73%, respectively. Although the 50 mg/kg dose inhibited tumor cell proliferation by 46% compared with the control group (Student t-test, p < .001), the effect was not different from that caused by the 10 mg/kg dose, supportive of a biphasic dose response. Additionally, tumor sections from all mice were analyzed by TUNEL staining to detect cells undergoing apoptosis (Figure 6A). As illustrated in Figure 6B, TUNEL-positive nuclei were significantly increased by 1.6-fold and 2.6-fold in the 10 mg/kg and 20 mg/kg groups, respectively, compared with control levels (Student t-test, p < .05). The 50 mg/kg dose did not induce tumor cell apoptosis over control levels (p > .05). Again, a trend toward a biphasic dose response was evident, suggesting that the 50 mg/kg pao pereira was beyond the optimal dose required to induce maximal tumor cell apoptosis.
Figure 5.
Inhibition of proliferation in LNCaP tumor xenografts following 6-week gavage of pao pereira extract. A, Cells stained dark blue represent proliferating cells (BrdU incorporation; ×200 magnification). B, Quantification of proliferating cells in LNCaP tumor xenografts. Errors bars indicate ± SEM; *p < .05, Student t-test.
Figure 6.
Six-week oral dosing of pao pereira extract–induced apoptosis in LNCaP tumor xenografts. A, Cells undergoing apoptosis stained brown (TUNEL staining; ×200 magnification). B, Quantification of apoptotic cells in LCNaP tumor xenografts from each treatment group. Error bars indicate ± SEM; *p < .05, Student t-test.
Discussion
Prostate cancer is a problematic human disease whose burden to health in the United States could be decreased by a suitable preventive agent or treatment, especially one that might be used as a nutritional supplement. Here we tested whether a β-carboline-rich extract of pao pereira bark might have any efficacy in suppressing in vitro or in vivo growth of a prototypic human prostate cancer cell line, LNCaP. Our results showed that this extract, when added to the medium of cultured LNCaP cells, suppressed their growth and induced apoptosis in a dose-dependent manner. Furthermore, when pao pereira extract was gavaged into mice that had been xenografted with LNCaP cells, tumor size was significantly smaller in two of three groups of treated mice compared with the tumor size in vehicle-treated mice over the experimental period. To some extent, this response was similar to our previous finding that a β-carboline-rich extract of another medicinal plant, R. vomitoria, also suppressed LNCaP growth in vitro and in vivo, and it supports the idea that other plants rich in β-carbolines might also be natural sources of prostate cancer preventive or therapeutic agents.
Although we do not understand the mechanism(s) through which the pao pereira extract affects prostate cancer cell growth and survival, we presume that the effects of this agent might be related to the β-carboline alkaloids. β-Carboline alkaloids suppress CDK activity5 that is needed to drive normal and cancerous cells through the cell cycle, but they also bind to DNA and may cause other cellular anomalies specific to cancer cells that suppress cell division or induce cell death. In our previous work with R. vomitoria extract, we used a targeted microarray analysis approach to evaluate the effects of the extract on gene expression patterns in LNCaP cells, especially on genes involved in DNA damage repair.8 We reported that numerous genes involved in DNA damage and repair were modulated by this extract. We did perform a similar but preliminary (unvalidated) analysis using the same DNA damage and repair microarray to compare gene expression in pao pereira–treated (100 μg/mL) LNCaP cells with that in control (vehicle treated) cells, but much fewer and different genes were affected in this pathway compared with treatment with the Rauwolfia extract. In our assay using pao pereira–treated cell complementary DNA, we observed particularly strong upregulation of the DNA repair response genes BRCA1 (24.67-fold) and DDIT3 (14.6-fold change) compared with vehicle-treated cells. More striking, however, were the changes in the expression of genes associated with the apoptosis pathway, where BAX (13-fold), TNFRSF11B (a member of the tumor necrosis factor receptor family; 12-fold), and APAF1 (9.5-fold) were most strongly upregulated. These results, although not yet validated by polymerase chain reaction studies, suggest that the Rauwolfia and pao pereira extracts may have different mechanisms of action that might even be complementary with regard to an anticancer effect.
One of the most striking and enigmatic results of our study, however, was the finding that the greatest effect of pao pereira extract on in vivo tumor growth (size) occurred at the lower doses tested (10 and 20 mg/kg/d). In these groups, pao pereira extract treatment reduced tumor volume by 80% and 75%, respectively. In contrast, mice gavaged with a 50 mg/ kg/d dose actually had mean tumor volumes at the end of the experiment that were similar to those of vehicle-treated mice. These discrepant results were also reflected by our analysis of the effects of pao pereira extract on tumor cell apoptosis (measured by TUNEL staining). Whereas the 20 mg/kg/d dose of pao pereira extract increased tumor cell apoptosis in the LNCaP xenografts by > 2.5-fold, the 50 mg/kg/d dose did not significantly increase apoptosis.
At this time, we do not understand the reason(s) for this unusual treatment effect. All groups were gavaged daily at the same times by the same investigators, and the doses were made from the same stock of pao pereira extract dissolved in 6% DMSO. Although there was no difference in tumor size in vehicle-treated versus 50 mg/kg/d extract–treated groups, treatment at the high dose did significantly suppress proliferation of the tumor cells, so the treated mice were experiencing some effects of the extract, but these were not sufficient to influence tumor size. Other potential explanations for this effect might include gastrointestinal consequences at the higher dose that suppresses uptake of active agents. We note here again that the mice did not suffer weight loss, which might reflect a general failure of gastrointestinal absorption at higher doses, nor did we notice other symptoms of gastrointestinal distress, such as diarrhea, in any treated group. It is also possible that high concentrations of pao pereira extract could induce metabolic enzymes, potentially altering the chemical profile of the bioactive compounds to an inactive state. The effects of the pao pereira preparation on mice are likely a composite of the effects of the extract in multiple organ systems, unlike single cells in cell culture. Finally, we must consider the possibility that the complex nature of pao pereira extract allows for the potential presence of ingredients that oppose the actions of any cancer-suppressing agent(s) present and that the tumor cell–protective effect is manifest at the higher doses of the extract.
According to the Mertz model, a U-shaped dose-response relationship exists between essential nutrients and their biologic impact; therefore, the optimal concentration of these agents required to achieve their desired biologic effects is in the midrange of the dose-response curve.10 Several studies have reported that this relationship also applies to anticancer nutritional agents,11–13 and our data using pao pereira extract also appear to validate this idea. Regardless, our data demonstrate the anti–prostate cancer activities of the pao pereira extract in both in vitro and in vivo prostate cancer cell model systems, and this work indicates the need for continued exploration into its use in the prevention and/or treatment of prostate cancer.
Acknowledgments
Financial disclosure of authors: This research was supported by The Center for Holistic Urology at Columbia University Medical Center, The Charles Royce Foundation, and Natural Source International, Ltd.
Financial disclosure of reviewers: None reported.
Contributor Information
Debra L. Bemis, Department of Urology, College of Physicians and Surgeons, Columbia University Medical Center, New York, NY.
Jillian L. Capodice, Department of Urology, College of Physicians and Surgeons, Columbia University Medical Center, New York, NY.
Manisha Desai, Department of Biostatistics, Mailman School of Public Health, Columbia University Medical Center, New York, NY.
Aaron E. Katz, Department of Urology, College of Physicians and Surgeons, Columbia University Medical Center, New York, NY.
Ralph Buttyan, The Ordway Research Institute, Albany, NY..
References
- 1.Beljanski M, Crochet S. The selective anticancer agents PB-100 and BG-8 are active against human melanoma cells, but do not affect non malignant fibroblasts. Int J Oncol 1996;8:1143–8. [DOI] [PubMed] [Google Scholar]
- 2.Beljanski M, Crochet S. The selective anticancer agent PB-100 inhibits interleukin-6 induced enhancement of glioblastoma cell proliferation in vitro. Int J Oncol 1994;5:873–9. [DOI] [PubMed] [Google Scholar]
- 3.Beljanski M The anticancer agent PB-100, selectively active on malignant cells, inhibits multiplication of sixteen malignant cell lines, even multidrug resistant. Genet Mol Biol 2000;23:29–33. [Google Scholar]
- 4.Beljanski M, Beljanski MS. Three alkaloids as selective destroyers of cancer cells in mice: synergy with classic anticancer drugs. Oncology 1986;43:198–203. [DOI] [PubMed] [Google Scholar]
- 5.Cao R, Peng W, Wang W, Xu A. betal-carboline alkaloids: biochemical and pharmacological functions. Curr Med Chem 2007;14:479–500. [DOI] [PubMed] [Google Scholar]
- 6.American Cancer Society. Cancer facts and figures 2008. Atlanta: American Cancer Society, 2008. [Google Scholar]
- 7.Caffo O, Sava T, Comploj E, et al. Docetaxel, with or without estramustine phosphate, as first-line chemotherapy for hormone-refractory prostate cancer: results of a multicentre, randomized phase II trial. BJU Int 2008;May 15 [Epub]. [DOI] [PubMed] [Google Scholar]
- 8.Bemis DL, Capodice JL, Gorroochurn P, et al. Antiprostate cancer activity of a beta-carboline alkaloid enriched extract from Rauwolfia vomitoria. Int J Oncol 2006;29:1065–73. [PubMed] [Google Scholar]
- 9.Taguchi A, Blood DC, del Toro G, et al. Blockade of RAGE-amphoterin signalling suppresses tumour growth and metastases. Nature 2000;405:354–60. [DOI] [PubMed] [Google Scholar]
- 10.Mertz W The essential trace elements. Science 1981; 213:1332–8. [DOI] [PubMed] [Google Scholar]
- 11.Waters DJ, Shen S, Glickman LT, et al. Prostate cancer risk and DNA damage: translational significance of selenium supplementation in a canine model. Carcinogenesis 2005;26:1256–62. [DOI] [PubMed] [Google Scholar]
- 12.Leitzmann MF, Stampfer MJ, Wu K, et al. Zinc supplement use and risk of prostate cancer. J Natl Cancer Inst 2003;95:1004–7. [DOI] [PubMed] [Google Scholar]
- 13.Nyberg F, Hou SM, Pershagen G, et al. Dietary fruit and vegetables protect against somatic mutation in vivo, but low or high intake of carotenoids does not. Carcinogenesis 2003;24:689–96. [DOI] [PubMed] [Google Scholar]