Abstract
Purpose
We assessed the effectiveness of a worksite management intervention (the 3W program) for overweight and obese hotel employees.
Design
The program was tested in a 2-year cluster-randomized trial involving 30 hotels that employed nearly 12,000 individuals.
Setting
All participating hotels were on Oahu, Hawaii. The intervention was implemented within hotel worksites.
Subjects
Participants were included in the analysis if they had an initial body mass index (BMI) ≥ 25, were assessed at least twice, were not missing other data needed for the analysis, and did not switch to employment at a hotel in a different experimental condition. Of the 6519 employees we assessed, data from 1207 individuals (intervention: 598; control: 610) met these criteria and contributed to the analysis.
Intervention
The intervention had two components: (1) group meetings and (2) a workplace environment intervention.
Measures
Weight and waist to height ratio (WHtR) were measured at three annual assessments.
Analysis
The effect of the intervention on change in BMI and WHtR was estimated in hierarchical mixed regression models using full maximum likelihood to estimate model parameters.
Results
The effects on change in BMI and WHtR were in the expected direction but were not statistically significant.
Conclusion
The 3W program was not effective. The low intensity of the intervention may have contributed to its ineffectiveness.
Keywords: Weight Control, Worksite Intervention, Randomized Trial, Prevention Research
PURPOSE
We report the main results of the Work, Weight, and Wellness (3W) study, a 2-year trial of a worksite weight management program for overweight and obese workers living on Oahu, Hawaii.
Obesity is associated with heart disease, diabetes, and musculoskeletal problems that cause suffering for workers and negative economic consequences for their employers.1 Worksite health promotion programs can improve these individuals’ health and lessen the economic consequences of their condition.2
Hawaii’s hotel industry employs a large representative sample of the state’s racially diverse population in positions that range widely in their physical activity requirements.3 The 3W study examined the effectiveness of proven approaches to weight management in hotel worksites.
METHODS
Design
The design and sampling plan are described elsewhere.3 The primary outcomes were rate of change in body mass index (BMI: kg/m2) and waist to height ratio (WHtR) of overweight (BMI ≥ 25 and < 30) and obese (BMI ≥ 30) employees. Hotels were the unit of randomization. Individual employees were the unit of analysis.
Sample
Thirty hotels employing nearly 12,000 workers were randomly assigned to control or intervention conditions within pairs define by a combination of union status (unionized = 9), luxury rating (range = 2–4 stars), and number of employees (range = 18–1518). Of 38 hotels expressing initial interest, one declined owing to union issues, six owing to acquisitions, and two others merged. Managers gave informed written consent for hotels to participate.
All employees were invited to three annual assessments where they gave informed written consent and received a $10 gift card. Once assessed, they were not committed to attend future study-related activities. The Kaiser Permanente-Hawaii Institutional Review Board approved the study.
Measures
Employees’ height, weight, and waist circumference were measured in three waves: at baseline, 12 months, and 24 months. Assessments included a questionnaire covering demographics, health behaviors, intake of foods that are high or low in calorie density, the Godin Leisure-Time Exercise Questionnaire,4 attitude toward work and employer, and stage of change for physical activity and diet.
Attributes of all hotel’s physical environment and policies related to health behaviors were measured at baseline and at 12, 24, and 30 months. The Checklist of Health Promotion Environments at Worksites was used to measure attributes of buildings, grounds, and neighborhoods that affect diet and physical activity.5 Kaiser Permanente Hawaii’s Policy Assessment Checklist was used to measure policy support for healthy behaviors.
Intervention
The intervention sought to increase physical activity and promote a healthy low-fat and low-calorie diet. Strategies for influencing behavior were based on the Social Ecological Model and on Chapman’s framework of workplace obesity control.6 The approach was modeled on successful interventions in Stanford and Pawtucket,7 the Weight Loss Maintenance Trial,8 and the Dietary Approaches to Stop Hypertension (DASH) diet.9
Feasibility of implementation helped determine how the intervention was tailored to individual hotels. Hotel employees served as coordinators of 3W program activities. Their positions at hotels varied widely, from clerical staff to director of human resources.
The 3W program had two components: group sessions and a workplace environment intervention. Group sessions led by trained nutritional counselors offered interpersonal support and instruction about diet and physical activity choices. The 48-week curriculum was adapted from its original 1-hour format to the 30 minutes available during shift changes and meals. The longer format was shown to effectively promote sustained weight loss in the Weight Loss Maintenance Trial.8 Nutritional advice was consistent with the DASH diet9: high fruit and vegetable intake, low fat and sugar intake.
The Worksite Environment Intervention was designed to be pervasive but not intrusive. It delivered health-supportive messages to employees in two ways: (1) displays in employee-only areas including cafeterias, break rooms, halls, stairways, and elevators; (2) newsletters and fliers in pay envelopes or employee mailboxes.
The messages reinforced group sessions’ curriculum content, publicized group sessions, and promoted healthy food choices in cafeterias and vending machines. Study staff worked with cafeteria chefs to promote healthy modifications of common regional recipes. An entire cookbook of healthy versions of Filipino recipes (the most prevalent group) was created and distributed.
Analysis
Intervention effects were estimated in mixed effects models that accommodate the covariation of repeated measurements within employees and of employees within hotels. The intervention and covariates were fixed effects, and time was the random effect. Rate of change in outcomes was modeled as the interaction between fixed effects and time. Covariates were retained if they were significant at p < .1.
Participants were included in the analysis if they had an initial BMI ≥ 25, were assessed at least twice, were not missing other data needed for the analysis, and did not switch to employment at a hotel in a different experimental condition. The potential for bias from incomplete data (fewer than three measurements) was assessed by comparing results when uncollected data were missing to five equivalent models that used imputed values for uncollected data.10
RESULTS
Participation
We assessed 6519 (54.3%) of the approximately 12,000 total hotel employees. Of these, 1207 (intervention: 598; control: 610) met criteria for inclusion in the analysis (Table).
Table.
Baseline Sample Characteristics and Hypothesis Test Results*
| Baseline Sample Characteristics | Hypothesis Test Results | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Control (N - 610) |
Intervention (N - 598) |
Outcome | ||||||
|
| ||||||||
| BMI | WHtR | |||||||
|
|
|
|||||||
| β† | SE | p | β† | SE | p | |||
| Characteristic | ||||||||
| BMI‡, mean (SD) | 29.25 (4.02) | 29.38 (3.93) | ||||||
| WHR§, mean (SD) | 0.56 (0.06) | 0.56 (0.06) | ||||||
| Age, y, mean (SD) | 46.11 (10.16) | 46.00 (9.65) | ||||||
| Race = white, % | 9.02 | 5.69 | ||||||
| Gender = male, % | 49.84 | 46.66 | ||||||
| Effects | ||||||||
| Annual rate of change | ||||||||
| Time (assessment year) | 0.33 | 0.13 | <0.01 | −0.73 | 0.10 | <0.0001 | ||
| Study condition‖ (intervention) | −0.10 | 0.07 | 0.18 | −0.18 | 0.13 | 0.14 | ||
| Patient age (y) | −0.01 | 0.00¶ | <0.0001 | - | - | - | ||
| Baseline | ||||||||
| Study condition (intervention) | −0.04 | 0.18 | 0.81 | −0.16 | 0.03 | 0.57 | ||
| Race‖ (Filipino) | −1.55 | 0.21 | <0.0001 | −0.29 | 0.30 | 0.34 | ||
| Race‖ (non-Filipino Asian) | −1.15 | 0.22 | <0.0001 | −1.03 | 0.31 | <0.01 | ||
| Race‖,§ (Pacific Islander) | 1.76 | 0.22 | <0.0001 | 1.85 | 0.32 | <0.0001 | ||
| Physical activity (MET) | −0.00¶ | 0.00¶ | <0.0001 | −0.00¶ | 0.00¶ | <0.0001 | ||
| Calorie-dense diet | 0.17 | 0.02 | <0.0001 | 0.28 | 0.03 | <0.0001 | ||
| Patient age (y) | - | - | - | 0.11 | 0.01 | <0.0001 | ||
The following variables did not meet p < 0.1 retention criteria for inclusion in the regression model: rate of change effects–job category, gender; baseline effects–job category, race: other, age. BMI indicates body mass index; WHtR, waist to height ratio; and MET, Metabolic Equivalent Task.
Parameter estimate in a covariate-adjusted hierarchical regression model.
Weight (kg)/height (m)2.
Waist circumference (cm)/height (cm).
Reference categories: study condition: control; race: Caucasian.
< 0.01 and >−0.01.
Among these, 378 (31.3%) had an initial BMI ≥ 30 (intervention: 32.8%; control: 29.8%), and 173 (14.1%) were assessed in all three waves (intervention: 13.0%; control: 15.1%). Among those in the intervention condition who contributed to the analysis, 48% attended group sessions. The average number of sessions they attended was 5.4.
Baseline Sample Characteristics
The prevalence of obesity and overweight was similar across study conditions at baseline. The distribution of BMI by gender and job type at baseline is given elsewhere.3 The ethnicity of assessed employees at baseline was 42% Filipino, 32% other Asian, 13% Pacific Islander, 9% white, 1% African-American, and 3% other. Greater age, greater daily intake of calorie-dense food, and Pacific Islander ancestry were associated with higher baseline WHtR.
Intervention Effects
The effects of the 3W program on change in BMI and WHtR were in the expected direction, but were not statistically significant. Relative to the control condition, BMI in the intervention condition decreased by .10 per year (p = .18) and WHtR decreased by .18 per year (p = .14) during 2 years.
Sensitivity Analysis
Equivalent analyses conducted after missing data were replaced by imputed data10 did not substantially alter the magnitude or direction of results.
Average Change in BMI and WHtR
At control hotels, employees’ mean BMI was virtually unchanged during 12 months and increased by .12 during 24 months. At intervention hotels, employees’ mean BMI decreased by .10 during 12 months and by .28 during 24 months. Mean WHtR decreased among employees in both study arms: by .28 and .17 during 12 and 24 months, respectively, at control hotels, and by larger amounts at intervention hotels, .55 during 12 months and .72 during 24 months.
Covariate Effects
Employees’ age was the only covariate associated with rate of change in BMI (β= .1; p < .0001). No covariates were associated with rate of WHtR change.
Post Hoc Exploration of Intervention Intensity
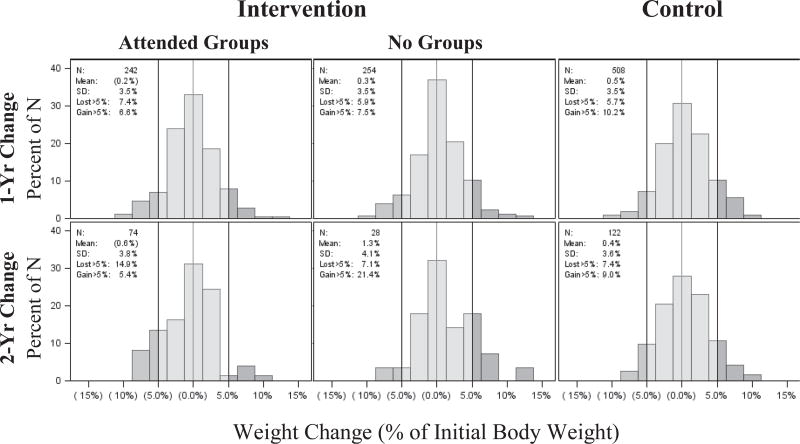
We explored intervention intensity in descriptive post hoc analyses. The Figure shows the distribution of weight change expressed as a percentage of initial body weight of individuals included in the main analysis. Vertical lines define the portions that lost or gained a clinically significant percent (5%) of initial body weight during 1 year and 2 years. The two intervention distributions are distinguished by individuals’ attendance of any group sessions. More attendees lost and fewer gained a clinically significant percentage of their baseline body weight than either nonattendees at intervention hotels or employees of control hotels.
Figure.
Distribution of Weight Change From Baseline as a Percentage of Initial Body
DISCUSSION
Summary
The intervention was associated with a rate of change in both BMI and WHtR that was in the expected direction but was not statistically significant.
Limitations
We had to modify the intervention in ways that diminished its intensity. Our use of briefer group sessions, for example, may help explain the differences between our findings and the Weight Loss Maintenance Trial, which used hour-long versions of the 3W group session curriculum. Although nearly all employees were exposed to the program’s environmental intervention, only 47.5% of the target population whose data contributed to the analysis attended at least one group session.
Management changes and employment fluctuations affected employers’ commitment to the study and our assessment and group session participation rates. Nearly half of participating hotels were sold or changed management during the intervention.
Significance
The 3W program did not reduce the BMI or WHtR of overweight and obese hotel employees.
SO WHAT? Implications for Health Promotion Practitioners and Researchers.
What is already known on this topic?
Worksites are a promising setting for weight control programs.2 The interventions that the Work, Weight, and Wellness (3W) Program was modeled on were effective in other populations and settings.7–9
What does this article add?
The ineffectiveness of the 3W program is inconsistent with research on similar worksite weight control programs and with the evidence basis for the 3W intervention. It suggests that similar interventions may need to be more intense and receive more consistent support from employers to be effective.
What are the implications for health promotion practice or research?
Practitioners should consider alternatives to the approach used in the 3W program. Future trials should address factors that affected our research. They should select worksites with stable ownership and low employee turnover and employers who guarantee full program implementation and full support for their employees’ participation.
Acknowledgments
The Work, Weight, and Wellness Program was funded by NHLBI Grant No. 5R01HL079505. The authors thank the following persons for important contributions: Myrissa Jerves, Mark Schmidt, Carol Nichols, Aleli Vinoya, Gloria Renda, Jonathan Lai, Vivian Guzman-Aniban, Aileen R. Uchida, Chuhe Chen, and the entire staff of the 3W program.
Contributor Information
Andrew E. Williams, Kaiser Permanente Center for Health Research, Honolulu, Hawaii.
Victor J. Stevens, Kaiser Permanente Center for Health Research, Portland, Oregon.
Cheryl L. Albright, University of Hawaii, Honolulu, Hawaii.
Claudio R. Nigg, University of Hawaii, Honolulu, Hawaii.
Richard T. Meenan, Kaiser Permanente Center for Health Research, Portland, Oregon.
Thomas M. Vogt, Kaiser Permanente Center for Health Research, Honolulu, Hawaii.
References
- 1.Finkelstein EA, DiBonaventura M, Burgess SM, Hale BC. The costs of obesity in the workplace. J Occup Environ Med. 2010;52:971–976. doi: 10.1097/JOM.0b013e3181f274d2. [DOI] [PubMed] [Google Scholar]
- 2.Goetzel RZ, Anderson DR, Whitmer RW, et al. The relationship between modifiable health risks and health care expenditures: an analysis of the multi-employer HERO health risk and cost database. J Occup Environ Med. 1998;40:843–854. doi: 10.1097/00043764-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Williams AE, Vogt TM, Stevens VJ, et al. Work, Weight, and Wellness: the 3W Program: a Worksite Obesity Prevention Trial among hotel workers. Obes Res. 2007;15(1S):16S–26S. doi: 10.1038/oby.2007.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Godin G, Shephard R. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–146. [PubMed] [Google Scholar]
- 5.Oldenburg B, Sallis JF, Harris D, Owen N. Checklist of Health Promotion Environments at Worksites (CHEW): development and measurement characteristics. Am J Health Promot. 2002;16:288–299. doi: 10.4278/0890-1171-16.5.288. [DOI] [PubMed] [Google Scholar]
- 6.Chapman LS. Reducing obesity in work organizations [discussion in Am J Health Promot. 2004;19(1):suppl 12] Am J Health Promot. 2004;19(suppl):1–8. [PubMed] [Google Scholar]
- 7.Carleton RA, Lasater TM, Assaf AR, et al. The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. Am J Public Health. 1995;85:777–785. doi: 10.2105/ajph.85.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299:1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 9.Vogt T, Appel J, Obarzanek E, et al. Dietary Approaches to Stop Hypertension (DASH): rationale, design, and methods. J Am Diet Assoc. 1999;99(suppl):S12–S18. doi: 10.1016/s0002-8223(99)00411-3. [DOI] [PubMed] [Google Scholar]
- 10.Gullion CM, Chen C, Maltesen GT. A Method of Using Multiple Imputation in Clinical Data Analysis. Portland, Ore: Center for Health Research; 2008. [Google Scholar]