Abstract
Background:
Chronic diseases are prevalent and the leading causes of mortality. Comorbidity of substance use disorders (SUDs) and chronic diseases is understudied to inform behavioral healthcare integration.
Objectives:
This study leveraged electronic health record (EHR) data of 211,880 adults from a large health system to examine prevalence and correlates of comorbidity of SUDs and nine chronic disease groups and to determine their association with hospitalization.
Methods:
Logistic regression analyses were conducted to estimate associations between chronic diseases and SUDs. To control for severity of diagnosis, analyses of associations between SUD and hospitalization were stratified by the number of chronic conditions.
Results:
In the sample, 48.3% had ≥1 chronic condition (hypertension 33.7%, arthritis 16.2%, diabetes 13.7%, chronic kidney disease 9.9%, asthma 9.1%, chronic obstructive pulmonary disease 8.9%, ischemic heart disease 8.3%, cancer 4.6%, and hepatitis 1.3%). Prevalence of SUD (overall 13.3%) among patients increased with multiple chronic conditions (14.3% having SUD among patients with one condition; 21.2% having SUD among patients with two to three conditions; and 32.5% having SUD among patients with 4–9 conditions). Chronic conditions were associated with increased odds of SUDs. For all SUD groups, hospitalization was more prevalent among patients with SUD than those without it; prevalence of hospitalization increased with the number of comorbid chronic conditions.
Conclusions:
Findings reveal a striking pattern of multicomorbidity of SUD and chronic diseases and its positive association with hospitalization. Behavioral healthcare integration should consider efforts to assess and treat comorbid SUD and chronic diseases, especially among adults with multiple chronic conditions.
Keywords: Chronic disease, comorbidity, electronic health records, hospitalization, substance use disorder
1. Introduction
The comorbidity of substance use disorders (SUDs) and chronic disease represents double jeopardy in terms of disease burden and healthcare costs (Thorpe et al., 2017). It is imperative to better characterize their comorbid patterns in order to inform behavioral healthcare integration efforts (Laderman, 2015). Specifically, chronic substance misuse and/or SUD could affect a wide range of organs and systems in the body, which may lead to multiple medical problems and an increased risk for contracting infectious diseases (Brick, 2012). The presence of SUD, such as alcohol or drug use disorder, may also interfere with an individual’s self-care behaviors, affect adherence to treatment regimen, or exacerbate existing medical diseases, thereby increasing disease complications, healthcare resource utilization (e.g., hospitalization), or mortality (Ducat et al., 2014; Ghitza et al., 2013; McLellan et al., 2014; Thorpe et al., 2017). In particular, drug misuse problems (e.g., illicit opioids, stimulants) and the opioid epidemic have been escalating in the United States (CDC, 2018; Seth et al., 2018). Opioid use disorder in the United States was the 11th leading cause of disability in 1990, and it became the seventh leading cause in 2016 (U.S. Burden of Disease Collaborators, 2018). The continued increases in substance-involved overdoses demonstrate an urgent need to study comorbid alcohol/drug use disorders and chronic diseases to inform healthcare services for improving alcohol/drug use disorder care and outcomes in medical settings (Hedegaard et al., 2017; Hoge et al., 2014; Vivolo-Kantor et al., 2018).
Of note, chronic diseases are prevalent and account for the vast majority of the total healthcare expenditures (Gerteis et al., 2014). Several chronic diseases, such as cancer, ischemic heart disease, diabetes, and chronic obstructive pulmonary disease (COPD), are among the leading causes of the deaths (U.S. Burden of Disease Collaborators, 2018). The 2010 Medical Expenditure Panel Survey data showed that 52% of Americans had ≥1 chronic condition (e.g., hypertension, arthritis, diabetes, asthma, heart disease, COPD), and 32% had multiple chronic conditions (Gerteis et al., 2014). As high as 86% of the total U.S. healthcare spending in 2010 was for patients with ≥1 chronic condition (Gerteis et al., 2014). Thus, failing to treat comorbid SUD and chronic diseases not only misses the opportunity for prevention and treatment, but also increases excess healthcare costs due to inefficiently delivered services to manage treatment compliance, medical complications, or hospitalizations (IOM, 2013; McLellan et al., 2014; Wu et al., 2012). Moreover, the top 10% of the U.S. population with poorer health or multicomorbidity accounts for an estimated 66% of total expenditures (Cohen, 2014). Developing effective service models to optimize healthcare outcomes for people with complex healthcare needs is a high priority (Blumenthal and Abrams, 2016). The Triple-Aim reform approach seeks to address the healthcare crisis by targeting improvement in the patient’s healthcare experience and population health as well as the reduction in healthcare cost per capita (Berwick et al., 2008). Inadequately managed alcohol/drug use disorders and related comorbidities are key drivers of excess healthcare costs (Thorpe et al., 2017). Hence, behavioral healthcare integration in medical settings to mitigate behavioral contributors (e.g., alcohol/drug use disorders) to healthcare costs is an essential component of the Triple-Aim reform (Laderman, 2015; Levey et al., 2012).
Data from healthcare settings are needed to characterize people with multicomorbidity in order to better inform integrated healthcare efforts for high-need, high-cost patients (Powers et al., 2015). Data on multicomorbidity or patients with complex healthcare need are generally unavailable from survey studies of SUDs. Therefore, patients’ electronic health records (EHR) data are needed to study the patterns of multicomorbidity and healthcare utilization in medical settings (SAMHSA 2017; Wu et al., 2018). In this study, we leverage patients’ EHR data of adults aged ≥18 years from a large health system to investigate the prevalence and correlates of multicomorbidity of SUD and chronic diseases and to determine their association with hospitalization.
2. Methods
2.1. Study sample
We analyzed the EHR data of adult patients from the Duke Medicine Enterprise Data Warehouse (EDW) between January 1, 2007 and December 31, 2014. The study sample included 211,880 adult patients aged ≥18 years (as of January 1, 2007) living in Durham County, North Carolina, who had at least two encounters between 2007 and 2014 (i.e., receiving the health care during the study period) and information about race/ethnicity and sex. The encounters included ambulatory visits, emergency department (ED) visits, hospitalizations, and other visits (e.g., procedure visit). The EDW stores the EHR data generated in the healthcare delivery of patients in the Duke University Health System (DUHS) (Horvath et al., 2014). A single, seamless EHR has been used by three hospitals and over 300 ambulatory clinics. The EDW employs a formal extract, transform, and load procedure to integrate data from source systems on a nightly basis to ensure consistency and quality and to minimize redundancy (Danford et al., 2013). Compared with the overall U.S. population, Durham County, North Carolina has a lower proportion of the “white alone” (non-Hispanic, single-race) population (77% vs. 54%), a higher proportion of the “Black/African American alone” (non-Hispanic, single-race) population (13% vs. 38%) and a lower proportion of the “Hispanic/Latino” population (18% vs. 14%) (U.S. Census Bureau, 2018). This study was approved by the DUHS Institutional Review Board (IRB).
2.2. Study variables
Demographic variables included age (as of January 1, 2007), sex, patient-identified race and ethnicity (Caucasian/White, African American/Black, Hispanic, Asian, multiracial, others). Diagnostic variables were based on ICD-9-CM codes (CMS, 2014). Common chronic conditions related to leading causes of death were examined: diabetes (type 1 or 2), COPD, hypertension, ischemic heart disease, chronic kidney disease, cancer (breast, endometrial, colorectal, lung, or prostate), arthritis (osteoarthritis or rheumatoid), hepatitis (viral B or C), and asthma (CMS, 2017; Heron, 2016). A categorical variable was created to define multicomorbidity based on the number of the nine chronic conditions. The main focus of healthcare utilization variable was inpatient hospitalization.
SUD diagnosis variables included: any SUD (alcohol, tobacco, or drug), alcohol use disorder, tobacco use disorder, drug use disorder (cannabis, opioids/heroin, cocaine/amphetamines, hallucinogens, sedatives, hypnotics, or anxiolytics, and unspecified drugs). A patient was considered to have a given diagnosis if an ICD-9-CM code for the condition was found in the list of discharge or final diagnosis codes during 2007–2014. Diagnosis grouping for each variable was defined to be consistent with those from the Agency for Healthcare Research and Quality (AHRQ)’s Clinical Classification Software (AHRQ, 2016) and Military Health System (MHS)’s surveillance case definitions (MHS, 2015). Any mood or anxiety disorder diagnosis was included in the logistic regression models as a control variable (Wu et al., 2015).
2.3. Statistical analysis
We examined frequencies of demographics, SUDs, chronic conditions, and healthcare utilization to provide the medical context. We then examined prevalence of SUDs by chronic conditions. We conducted separate logistic regression analyses of individual SUD to determine demographic and medical correlates of each SUD. We then produced the prevalence of hospitalization by SUD status and stratified the analysis by the number of chronic conditions. Finally, we conducted logistic regression analyses, stratified by the number of chronic conditions (0, 1, 2–3, 4–9), to further determine whether SUD was associated with elevated odds of hospitalization, adjusting for age, sex, race/ethnicity, and any mood/anxiety disorder. Analyses were conducted with Stata 15.1 (StataCorp, 2017).
3. Results
3.1. Demographic and medical characteristics (Table 1)
Table 1.
Demographic and clinical characteristics of the study sample (N=211,880)*
| Variables | N | Column % (SE) |
|---|---|---|
| Age group in years | ||
| 18–25 | 47,445 | 22.4 (0.09) |
| 26–34 | 43,869 | 20.7 (0.09) |
| 35–49 | 55,367 | 26.1 (0.10) |
| 50–64 | 40,844 | 19.3 (0.09) |
| 65+ | 24,355 | 11.5 (0.07) |
| Age in years, mean (SD) | --- | 41.3 (17.53) |
| Sex | ||
| Male | 87,573 | 41.3 (0.11) |
| Female | 124,307 | 58.7 (0.11) |
| Race/ethnicity | ||
| Caucasian/White | 105,917 | 50.0 (0.11) |
| African American/Black | 76,168 | 35.9 (0.10) |
| Hispanic | 12,976 | 6.1 (0.05) |
| Asian | 7,750 | 3.7 (0.04) |
| Multiracial | 2,846 | 1.3 (0.03) |
| Others | 6,223 | 2.9 (0.04) |
| Substance use disorder diagnosis, yes | ||
| Tobacco | 21,085 | 10.0 (0.07) |
| Alcohol | 7,377 | 3.5 (0.04) |
| Any drug | 8,244 | 3.9 (0.04) |
| Cannabis | 2,152 | 1.0 (0.02) |
| Opioids/heroin | 2,093 | 1.0 (0.02) |
| Cocaine/amphetamines | 3,483 | 1.6 (0.03) |
| Other drugs | 4,724 | 2.2 (0.03) |
| Any substance listed above | 28,247 | 13.3 (0.07) |
| Chronic condition diagnosis, yes | ||
| Hypertension | 71,466 | 33.7 (0.10) |
| Arthritis† | 34,388 | 16.2 (0.08) |
| Diabetes, type 1 or 2 | 28,967 | 13.7 (0.07) |
| Chronic kidney disease | 21,049 | 9.9 (0.06) |
| Asthma | 19,228 | 9.1 (0.06) |
| Chronic obstructive pulmonary disease | 18,902 | 8.9 (0.06) |
| Ischemic heart disease | 17,685 | 8.3 (0.06) |
| Cancer‡ | 9,656 | 4.6 (0.05) |
| Hepatitis viral B or C | 2,737 | 1.3 (0.02) |
| Any chronic condition listed above | 102,324 | 48.3 (0.11) |
| Any substance use disorder or chronic condition listed above, yes | 109,861 | 51.9 (0.11) |
| Number of the 9 chronic conditions listed above | ||
| None (other conditions) | 109,556 | 51.7 (0.11) |
| 1 | 43,279 | 20.4 (0.09) |
| 2–3 | 41,613 | 19.6 (0.09) |
| 4–9 | 17,432 | 8.2 (0.06) |
| Mood or anxiety disorder diagnosis, yes | 47,189 | 22.3 (0.09) |
| Inpatient hospitalization, yes | 64,124 | 30.3 (0.10) |
| The number of total encounters§, mean (SD) | --- | 33.9 (52.56) |
The study sample included patients aged 18 or older and with at least two encounters between 2007 and 2014 in the EHR data.
Arthritis: osteoarthritis or rheumatoid arthritis.
Cancer: breast, endometrial, colorectal, lung, or prostate cancer.
The total encounters included ambulatory visits, emergency department admissions, inpatient hospitalizations, and other visits (e.g., tele-medication, procedure visit).
SD: standard deviation. SE: standard error.
The mean age of the sample on January 1, 2007 was 41.3 years (SD=17.53). Of the sample, 58.7% were female, and 50.0% were non-Caucasian/White (African American/Black 35.9%, Hispanic 6.1%, Asian 3.7%, multiracial 1.3%, and other 2.9%).
The prevalence of any SUD diagnosis in the overall sample was 13.3% (tobacco 10.0%, alcohol 3.5%, any drug 3.9%, cannabis 1.0%, opioids/heroin 1.0%, cocaine/amphetamines 1.6%, and other drugs 2.2%). Overall, 48.3% of the sample had any of the nine chronic conditions (1 condition 20.4%, 2–3 conditions 19.6%, and 4–9 conditions 8.2%). Hypertension (33.7%), arthritis (16.2%) and diabetes (13.7%) were more common than others (chronic kidney disease 9.9%, asthma 9.1%, COPD 8.9%, ischemic heart disease 8.3%, cancer 4.6%, and hepatitis viral B/C 1.3%). In the sample, 30.3% had any inpatient hospitalization recorded in the EHRs during 01/01/2007–12/31/2014. The mean number of total encounters (ambulatory visits, ED admissions, hospitalizations, and other visits, e.g., procedure visit) was 33.9 (SD=52.56).
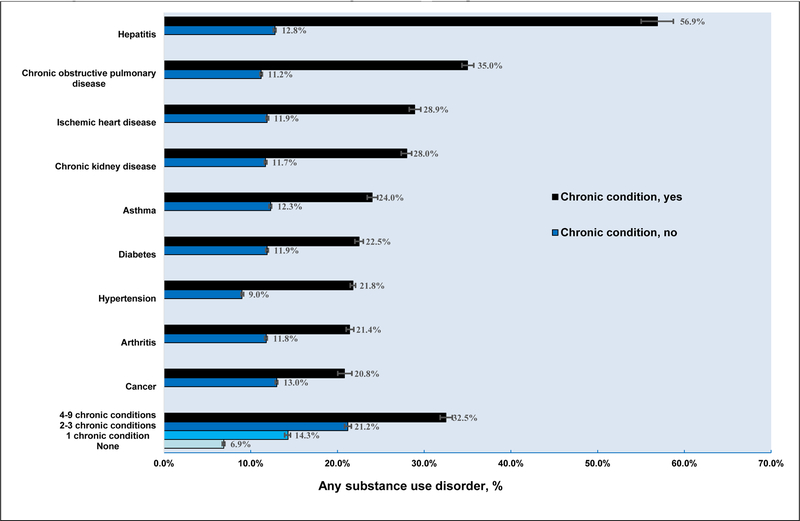
3.2. Prevalence of SUDs by chronic disease (Table 2 and Fig. 1)
Table 2.
Prevalence of substance use disorder diagnoses by chronic conditions among adult patients
| Substance use disorder, yes | ||||
|---|---|---|---|---|
| Any substance* | Tobacco | Alcohol | Any drug | |
| Prevalence of substance use disorder % | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) |
| Overall | 13.3 (13.19–13.48) | 10.0 (9.82–10.08) | 3.5 (3.40–3.56) | 3.9 (3.81–3.97) |
| Hypertension | ||||
| Yes | 21.8 (21.48–22.09) | 17.1 (16.87–17.42) | 5.7 (5.50–5.83) | 6.4 (6.18–6.54) |
| No | 9.0 (8.88–9.18) | 6.3 (6.17–6.42) | 2.4 (2.29–2.45) | 2.6 (2.55–2.72) |
| Arthritis† | ||||
| Yes | 21.4 (21.01–21.88) | 16.5 (16.11–16.90) | 4.8 (4.61–5.07) | 7.2 (6.89–7.44) |
| No | 11.8 (11.61–11.91) | 8.7 (8.55–8.81) | 3.2 (3.14–3.30) | 3.3 (3.18–3.34) |
| Diabetes, type 1 or 2 | ||||
| Yes | 22.5 (22.02–22.99) | 17.7 (17.30–18.18) | 5.1 (4.90–5.40) | 7.0 (6.69–7.28) |
| No | 11.9 (11.73–12.03) | 8.7 (8.59–8.85) | 3.2 (3.14–3.30) | 3.4 (3.32–3.49) |
| Chronic kidney disease | ||||
| Yes | 28.0 (27.35–28.56) | 21.0 (20.43–21.53) | 8.1 (7.77–8.51) | 10.7 (10.28–11.11) |
| No | 11.7 (11.58–11.86) | 8.7 (8.61–8.86) | 3.0 (2.89–3.05) | 3.1 (3.06–3.22) |
| Asthma | ||||
| Yes | 24.0 (23.44–24.65) | 19.5 (18.95–20.07) | 5.1 (4.84–5.46) | 9.0 (8.57–9.38) |
| No | 12.3 (12.12–12.41) | 9.0 (8.87–9.13) | 3.3 (3.24–3.40) | 3.4 (3.30–3.47) |
| Chronic obstructive pulmonary disease | ||||
| Yes | 35.0 (34.36–35.72) | 30.4 (29.73–31.04) | 7.5 (7.16–7.91) | 9.9 (9.50–10.35) |
| No | 11.2 (11.07–11.35) | 8.0 (7.83–8.07) | 3.1 (3.01–3.16) | 3.3 (3.22–3.38) |
| Ischemic heart disease | ||||
| Yes | 28.9 (28.28–29.61) | 23.3 (22.70–23.95) | 6.8 (6.48–7.22) | 9.2 (8.74–9.59) |
| No | 11.9 (11.77–12.06) | 8.7 (8.61–8.86) | 3.2 (3.10–3.25) | 3.4 (3.33–3.49) |
| Cancer‡ | ||||
| Yes | 20.8 (20.04–21.66) | 17.1 (16.32–17.82) | 4.2 (3.77–4.57) | 4.8 (4.39–5.24) |
| No | 13.0 (12.83–13.12) | 9.6 (9.48–9.74) | 3.4 (3.37–3.53) | 3.8 (3.76–3.93) |
| Hepatitis viral B or C | ||||
| Yes | 56.9 (55.02–58.73) | 43.0 (41.12–44.83) | 25.8 (24.23–27.50) | 34.5 (32.70–36.25) |
| No | 12.8 (12.62–12.91) | 9.5 (9.39–9.65) | 3.2 (3.11–3.27) | 3.5 (3.41–3.57) |
| Any chronic condition listed above | ||||
| Yes | 20.2 (19.99–20.49) | 15.9 (15.65–16.10) | 5.1 (4.93–5.20) | 6.0 (5.86–6.15) |
| No | 6.9 (6.73–7.03) | 4.4 (4.30–4.54) | 2.0 (1.92–2.09) | 1.9 (1.84–2.00) |
| Number of chronic conditions listed above | ||||
| None (other condition) | 6.9 (6.73–7.03) | 4.4 (4.30–4.54) | 2.0 (1.92–2.09) | 1.9 (1.84–2.00) |
| 1 | 14.3 (14.02–14.68) | 10.8 (10.51–11.10) | 3.7 (3.51–3.87) | 3.8 (3.63–3.99) |
| 2–3 | 21.2 (20.82–21.61) | 16.9 (16.52–17.24) | 5.3 (5.08–5.51) | 5.9 (5.64–6.09) |
| 4–9 | 32.5 (31.85–33.24) | 26.1 (25.43–26.73) | 8.0 (7.56–8.36) | 11.8 (11.33–12.29) |
Any substance included tobacco, alcohol, and drug (cannabis, opioid/heroin, cocaine/amphetamine, and other drugs).
Arthritis: osteoarthritis or rheumatoid arthritis.
Cancer: breast, endometrial, colorectal, lung, or prostate cancer.
CI: confidence interval. Boldfaced: The estimate differed from the estimate without the chronic condition diagnosis (P<0.01.
Figure 1.
Prevalence of substance use disorder diagnoses among adult patients with and without chronic conditions.
For each of the nine chronic conditions, any SUD was significantly more prevalent among those with a condition than those without it: hypertension (21.8% vs. 9.0%), arthritis (21.4% vs. 11.8%), diabetes (22.5% vs. 11.9%), chronic kidney disease (28.0% vs. 11.7%), asthma (24.0% vs. 12.3%), COPD (35.0% vs. 11.2%), ischemic heart disease (28.9% vs. 11.9%), cancer (20.8% vs. 13.0%), and chronic hepatitis viral B/C (56.9% vs. 12.8%). The prevalence of any SUD increased with the number of the identified chronic conditions (none 6.9%, 1 condition 14.3%, 2–3 conditions 21.2%, and 4–9 conditions 32.5%). Likewise, adults with each of the nine chronic conditions had a significantly higher prevalence of the tobacco, alcohol, and any drug use disorder than those without it. A similar pattern was found for specific drug groups (cannabis, opioid/heroin, cocaine/amphetamine, and other drug use disorders). The results for cannabis, opioid/heroin, cocaine/amphetamine, and other drug use disorders are available online only (Supplementary Table S11).
3.3. Adjusted logistic regression analysis of SUDs (Table 3)
Table 3.
Adjusted analysis of tobacco, alcohol, and drug use disorder among adult patients (N=211,880)
| Substance use disorder | Any substance | Tobacco | Alcohol | Any drug |
|---|---|---|---|---|
| Adjusted odds ratio (AOR) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) |
| Age group in years (vs. 18–25) | ||||
| 26–34 | 1.06 (1.02–1.11) | 1.28 (1.21–1.35) | 0.94 (0.86–1.02) | 0.79 (0.73–0.85) |
| 35–49 | 1.35 (1.30–1.41) | 1.66 (1.58–1.74) | 1.44 (1.34–1.55) | 0.81 (0.76–0.87) |
| 50–64 | 1.00 (0.95–1.05) | 1.25 (1.18–1.32) | 1.19 (1.10–1.30) | 0.35 (0.32–0.39) |
| 65+ | 0.48 (0.45–0.51) | 0.49 (0.46–0.53) | 0.63 (0.56–0.71) | 0.25 (0.23–0.28) |
| Sex (vs. male) | ||||
| Female | 0.50 (0.49–0.51) | 0.60 (0.58–0.62) | 0.25 (0.24–0.27) | 0.48 (0.46–0.50) |
| Race/ethnicity (vs. Caucasian/White) | ||||
| African American/Black | 2.04 (1.98–2.10) | 1.98 (1.92–2.05) | 1.87 (1.77–1.97) | 2.44 (2.32–2.57) |
| Hispanic | 0.77 (0.71–0.83) | 0.45 (0.40–0.50) | 1.89 (1.70–2.10) | 0.60 (0.51–0.71) |
| Asian | 0.26 (0.22–0.30) | 0.24 (0.20–0.29) | 0.31 (0.23–0.42) | 0.21 (0.15–0.30) |
| Multiracial | 1.12 (0.99–1.27) | 1.13 (0.98–1.29) | 1.17 (0.94–1.46) | 1.35 (1.09–1.66) |
| Others | 0.62 (0.55–0.69) | 0.53 (0.47–0.61) | 0.80 (0.66–0.98)† | 0.53 (0.42–0.67) |
| Arthritis‡ (yes vs. no) | 1.27 (1.23–1.32) | 1.22 (1.17–1.27) | 1.02 (0.96–1.10) | 1.59 (1.49–1.69) |
| Diabetes (yes vs. no) | 1.12 (1.08–1.17) | 1.13 (1.09–1.19) | 0.88 (0.82–0.95) | 1.06 (0.99–1.13) |
| Asthma (yes vs. no) | 1.25 (1.20–1.31) | 1.28 (1.22–1.34) | 1.10 (1.02–1.19)† | 1.50 (1.41–1.60) |
| Chronic obstructive pulmonary disease (yes vs. no) | 3.00 (2.88–3.13) | 3.55 (3.41–3.71) | 1.77 (1.64–1.90) | 1.80 (1.68–1.92) |
| Ischemic heart disease (yes vs. no) | 1.93 (1.83–2.02) | 2.01 (1.91–2.12) | 1.36 (1.25–1.48) | 1.99 (1.84–2.15) |
| Hepatitis viral B or C (yes vs. no) | 4.83 (4.42–5.27) | 3.44 (3.14–3.76) | 4.94 (4.45–5.49) | 8.12 (7.32–9.01) |
| Cancer§ (yes vs. no) | 1.27 (1.19–1.35) | 1.37 (1.28–1.46) | 0.93 (0.83–1.04) | 0.99 (0.88–1.10) |
| Mood or anxiety disorder (yes vs. no) | 3.30 (3.20–3.40) | 2.50 (2.41–2.58) | 4.03 (3.82–4.25) | 5.98 (5.68–6.30) |
Note. Each adjusted logistic regression included all variables listed in the first column.
P value was between 0.01 and 0.05. Boldfaced: P<0.05.
Arthritis: osteoarthritis or rheumatoid arthritis.
Cancer: breast, endometrial, colorectal, lung, or prostate cancer.
AOR: adjusted odds ratio. CI: confidence interval.
We conducted logistic regression analyses to identify demographic and medical correlates of SUD (tobacco, alcohol, cannabis, opioid/heroin, cocaine/amphetamine, and other drug use disorders, respectively). We explored the correlation of the nine chronic conditions and mood/anxiety disorder, and excluded two variables (hypertension, chronic kidney disease) from logistic regression models due to their high correlation with other conditions (>0.3). Any mood/anxiety disorder was included in each logistic regression model as a control variable. The results for cannabis, opioid/heroin, cocaine/amphetamine, and other drug use disorders are available online only (Supplementary Table S21).
3.3.1. Demographic correlates.
Adults aged ≥65 years had relatively low odds of having SUDs. Compared with adults aged 18–25, those aged 26–64 had greater odds of having tobacco use disorder, those aged 35–64 had greater odds of having alcohol use disorder, those aged 26–49 had greater odds of having cocaine/amphetamine use disorder, while younger adults aged 18–25 had elevated odds of cannabis and opioid/heroin use disorders.
Females had lower odds of all SUD variables than males. Compared with Caucasians/Whites, African American/Black patients had greater odds of SUDs (tobacco, alcohol, any drug, cannabis, cocaine/amphetamines, other drug), except for opioid/heroin use disorder; Hispanics had greater odds of alcohol use disorders but lower odds of other SUDs (tobacco, cannabis, opioids/heroin, other drugs); Asians had lower odds of SUDs (tobacco, alcohol, any drug, other drugs); and multiracial adults had greater odds of drug use disorders (any drug, cannabis, cocaine/amphetamines).
3.3.2. Medical correlates.
Arthritis, diabetes, asthma, COPD, ischemic heart disease, cancer, and hepatitis were associated with greater odds of tobacco use disorder. Asthma, COPD, ischemic heart disease, and hepatitis were associated with greater odds of alcohol use disorder and drug use disorder (any drug, cannabis, cocaine/amphetamine, opioids/heroin, and other drugs). Arthritis was associated with increased odds of any drug, opioid/heroin, and other drug use disorders. Diabetes was associated with increased odds of opioid/heroin and other drug use disorders, but lower odds of alcohol use disorder in the adjusted model.
3.4. Association of SUD with hospitalization by the number of chronic conditions (Table 4)
Table 4.
Hospitalization by substance use disorder diagnoses among adult patients, stratified by the number of chronic conditions
| Prevalence of inpatient hospitalization, % | Number of chronic conditions* | ||||
|---|---|---|---|---|---|
| Overall | None | 1 | 2–3 | 4–9 | |
| N=211,880 | N=109,556 | N=43,279 | N=41,613 | N=17,432 | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Overall | 30.3 (30.07–30.46) | 17.0 (16.79–17.23) | 25.5 (25.08–25.91) | 48.1 (47.62–48.58) | 82.8 (82.27–83.39) |
| Any substance use disorder | |||||
| Yes | 56.8 (56.22–57.38) | 33.0 (31.96–34.08) | 45.1 (43.85–46.32) | 64.2 (63.23–65.23) | 89.7 (88.83–90.42) |
| No | 26.2 (25.98–26.38) | 15.8 (15.61–16.05) | 22.2 (21.79–22.64) | 43.8 (43.22–44.29) | 79.5 (78.81–80.27) |
| Adjusted Odds Ratio (95% CI)† | 3.34 (3.25–3.44) | 3.48 (3.27–3.70) | 2.82 (2.65–2.99) | 2.48 (2.35–2.62) | 2.57 (2.32–2.85) |
| Tobacco use disorder | |||||
| Yes | 56.1 (55.48–56.82) | 30.9 (29.62–32.23) | 42.0(40.55–43.38) | 62.0 (60.84–63.11) | 88.6 (87.67–89.52) |
| No | 27.4 (27.20–27.60) | 16.4 (16.14–16.59) | 23.5 (23.08–23.93) | 45.3 (44.75–45.80) | 80.8 (80.11–81.47) |
| Adjusted Odds Ratio (95% CI)† | 2.94 (2.85–3.04) | 2.88 (2.67–3.11) | 2.25 (2.10–2.40) | 2.12 (2.01–2.24) | 2.13 (1.91–2.37) |
| Alcohol use disorder | |||||
| Yes | 63.9 (62.80–64.99) | 37.5 (35.53–39.58) | 58.1 (55.65–60.48) | 75.6 (73.73–77.32) | 93.8 (92.40–94.95) |
| No | 29.1 (28.85–29.25) | 16.6 (16.37–16.82) | 24.2 (23.84–24.66) | 46.6 (46.07–47.06) | 81.9 (81.29–82.48) |
| Adjusted Odds Ratio (95% CI)† | 4.07 (3.87–4.29) | 4.55 (4.07–5.10) | 4.47 (4.01–4.98) | 3.52 (3.17–3.90) | 3.49 (2.78–4.38) |
| Any drug use disorder | |||||
| Yes | 73.6 (72.62–74.52) | 51.3 (49.12–53.39) | 66.6 (64.27–68.82) | 79.8 (78.18–81.37) | 94.6 (93.54–95.50) |
| No | 28.5 (28.31–28.71) | 16.3 (16.12–16.56) | 23.9 (23.46–24.28) | 46.1 (45.63–46.62) | 81.3 (80.64–81.87) |
| Adjusted Odds Ratio (95% CI)† | 6.13 (5.81–6.46) | 6.99 (6.29–7.76) | 5.67 (5.09–6.33) | 4.83 (4.35–5.37) | 4.59 (3.75–5.61) |
Chronic conditions included hypertension, arthritis (osteoarthritis or rheumatoid), diabetes (type 1 or 2), chronic kidney disease, asthma, chronic obstructive pulmonary disease, ischemic heart disease, cancer (breast, endometrial, colorectal, lung, or prostate), and hepatitis viral B or C.
Each adjusted logistic regression model of inpatient hospitalization in relation to substance use disorder controlled for continuous age, sex, race/ethnicity, and mood or anxiety disorder diagnosis.
CI: confidence interval. Boldfaced: The estimate differed from the estimate without substance use disorder diagnosis (P<0.01) or P<0.01 for adjusted odds ratios.
Finally, we produced the prevalence and association of hospitalization by SUD status stratified by the total number of chronic conditions (four groups of patients: none, 1, 2–3, and 4–9 conditions). The results for cannabis, opioid/heroin, cocaine/amphetamine, and other drug use disorders are available online only (Supplementary Table S32).
For each SUD variable (any SUD, tobacco, alcohol, any drug, cannabis, opioids/heroin, cocaine/amphetamine, and other drugs, respectively), patients with SUD had a significantly higher prevalence of hospitalization than those without SUD, and the prevalence of hospitalization increased by the number of chronic conditions. The prevalence of hospitalization among patients with SUD was highest in the group with 4–9 chronic conditions, followed orderly by the group with 2–3 conditions and the group with one condition. It was lowest in the group without the chronic condition.
Adjusted logistic regression showed a significant association of the SUD status with increased odds of hospitalization for each SUD variable (any SUD, tobacco, alcohol, any drug, cannabis, opioids/heroin, cocaine/amphetamine, and other drugs, respectively) in every group of patients (none, 1, 2–3, and 4–9 chronic conditions). The strength of association with hospitalization was especially elevated for drug use disorders (cannabis, opioids/heroin, cocaine/amphetamine, and other drugs; Supplementary Table S32).
4. Discussion
Chronic diseases are major drivers of excess healthcare expenditures (Gerteis et al., 2014). Individuals with either SUD or multiple chronic conditions were found to overrepresent super-utilizers of hospital care (e.g., more readmissions, longer stays, higher costs; Jiang et al., 2015). Failing to treat comorbid chronic conditions in healthcare transforming efforts for alcohol/drug use disorder care may result in unnecessary use of ineffectively delivered treatments and poor outcomes. Despite the national shift for promoting behavioral health integration to improve alcohol/drug use disorder care, there is limited research on multicomorbidity of alcohol/drug use disorders and chronic diseases. This study adds new findings on comprehensive patterns of comorbid SUD and chronic diseases, especially for the understudied drug use disorders. First, about 1 in 7 adult patients (13.3%) has SUD recorded in their EHR. Second, as many as 1 in 2 patients had ≥1 chronic condition (1 condition 20.4%, 2–3 conditions 19.6%, 4–9 conditions 8.2%). Third, for every chronic condition, SUD (tobacco, alcohol, any drug) was significantly more prevalent among patients with the chronic condition than those without it. Prevalence of each SUD (tobacco, alcohol, any drug, specific drug group) increased substantially among patients with multiple chronic conditions. Fourth, for every SUD, prevalence of hospitalization was significantly higher among patients with SUD than those without it. Prevalence of hospitalization also increased markedly among those with multiple chronic conditions. These findings reveal a striking pattern of multicomorbidity of SUD and chronic diseases and its positive association with hospitalization for tobacco, alcohol, and drug use disorders.
4.1. What this study adds
The salient finding concerns multicomorbidity of SUD (including drug use disorders) and chronic diseases. Among patients with ≥1 chronic condition, 57.7% had multiple conditions. For each of the SUD variables, prevalence of SUD increased consistently with comorbidity. As many as 32.5% of patients with 4–9 chronic conditions had SUD compared with 14.3% of those with 1 condition and 21.2% of those with 2–3 chronic conditions. One chief reason for the healthcare crisis is the high concentration of healthcare expenditures in a small group of people with multicomorbidity or complex health problems (IOM, 2013). As such, approximately 87% of the U.S. healthcare expenditures was used by 25% of the U.S. population (Cohen, 2014). The high-cost patients should be a priority for more research to better inform intervention strategies to meet their complex healthcare need. Due to survey design features, prior and ongoing large studies of alcohol/drug use disorders are infeasible to study the multicomorbidity of SUDs and chronic diseases (e.g., Lipari et al., 2016; Wu et al., 2016). By using routinely collected healthcare data from patients in real-world settings, this study produces new clinical evidence documenting multicomorbidity for alcohol/drug use disorders and chronic diseases. These comprehensive results on a variety of alcohol/drug use disorders and chronic diseases provide a compelling reason for clinicians to assess and treat comorbid alcohol/drug use disorders and chronic diseases.
Hospitalizations are costly and largely preventable if the patient receives timely or effective ambulatory care (Gao et al., 2014; Jiang et al., 2015). Under the Affordable Care Act, hospital readmission is a main target required by U.S. Centers for Medicare and Medicaid Services to establish the Readmissions Reduction Program to reduce readmission and contain costs (CMS, 2018; Kocher and Adashi, 2011). To mitigate severity bias, we conducted the stratified analysis of hospitalization by the number of chronic conditions. Prevalence of hospitalization ranged from 17.0% among patients without chronic condition to 82.8% among patients with 4–9 chronic conditions. For all four groups of chronic condition, the odds of hospitalization were consistently elevated among patients with SUD versus those without SUD across all SUD groups (e.g., odds of hospitalization for ‘any drug use disorder’ ranging from 4.59–6.99). Our findings demonstrate that SUD, especially drug use disorders, is robustly associated with increased odds of hospitalization.
The comparison of the SUD prevalence from this study of EHR data with the national survey data is complicated by vast differences in the design and target population. In the adult sample of the 2016 National Survey on Drug Use and Health, nicotine dependence (past-month measure, 11.7%) was more prevalent than alcohol (past-year, 6.0%) and drug use disorders (past-year, 2.7%; Center for Behavioral Health Statistics and Quality, 2017). We also found tobacco use disorder to be more prevalent than alcohol and drug use disorders. However, the prevalence of SUDs in this study was based on treatment-seeking patients’ routine healthcare data that were influenced by treatment-seeking behaviors, severity of medical problems, and medical practice. Due to a lack of systematic assessments for alcohol/drug use disorders in general medical settings, alcohol/drug use disorders tend to be underdiagnosed (Saitz and Daaleman, 2017; Wakeman et al., 2016).
Addiction has a long history of being recognized as a chronic, relapsing disease (Leshner, 1997). Team-based chronic care approaches have been advocated to improve health care and outcomes for SUDs (McLellan et al., 2014). However, providers in general medical settings generally have inadequate support or training to provide alcohol/drug use disorder treatment, or are uncomfortable or unwilling to do so (CASA Columbia, 2000; Loheswaran et al., 2015; Wakeman et al., 2016). We found that at least one-fifth of patients with ≥1 chronic condition had at least one SUD recorded in their EHR data, and SUD (tobacco, alcohol, and drug use disorders) was particularly prevalent among those with hepatitis, COPD, ischemic heart disease, or chronic kidney disease. Our data also suggested that patients with tobacco or alcohol use disorder were older, while those with drug use disorder tended to be younger. Males and African American/Black patients (versus Caucasians/Whites) had elevated odds of tobacco, alcohol, and any drug use disorder. The results call for developing infrastructure support and training for primary care providers to assess and treat comorbid alcohol/drug use disorders and chronic conditions, especially among males, African American/Black patients, and adults with multiple chronic diseases (Berry et al., 2018; Hayes et al., 2016).
Finally, we found a high prevalence of tobacco use disorder (43.0%) among patients with hepatitis, which may be related to a high prevalence of co-occurring tobacco use and illicit drug use among people who misuse substances (Marshall et al., 2011). We explored the data and found that 19.3% of patients with tobacco use disorder also had drug use disorder compared with 2.2% patients without tobacco use disorder. The co-existing tobacco use and chronic hepatitis may positively interact and increase the risk of developing liver cancer and premature death (Abdel‐Rahman et al., 2017; Chuang et al., 2010; Pang et al., 2015). Thus, tobacco cessation interventions should also assess and treat comorbid drug use disorders and drug use related hepatitis (Marshall et al., 2011).
4.2. Limitations
This study has some limitations. The results are based on associations that preclude any causal inference. The finding on multicomorbidity and hospitalization may reflect a clustering pattern of risk factors among some patients as well as the issue of “opportunity to be diagnosed” given the presence of one or more chronic disease. For example, substance use, high body mass index, high fasting plasma glucose, high systolic blood pressure, and impaired kidney function are all leading risk factors for mortality that are linked with chronic diseases (Brick, 2012; U.S. Burden of Disease Collaborators, 2018). The treatment-seeking behaviors for a chronic disease would increase the likelihood for being screened for comorbid problems and related diagnoses. In addition, diagnoses based on clinical care data from EHRs are subject to biases and misclassification, and the recency of diagnosis cannot be ascertained precisely (Wu et al., 2013a, 2013b). Compared with SUD diagnoses relying on self-report symptoms, diagnostic errors may be lower for non-SUD chronic conditions that have objective or biological measures to ascertain the conditions or monitor treatment progress.
Due to a variety of reasons (e.g., stigma, lacking routine assessments for SUDs, lacking provider training or treatment resources, competing medical interests, limited time, provider specialty), alcohol and drug use disorders are likely to be under-detected or under-diagnosed in general medical settings (Milhorn, 2017; Muhrer, 2010). These results are from a large academic health system in North Carolina, which limit its generalizability to other settings and regions. All results should be considered conservatively within the clinical context and study limitations. Nonetheless, this study adds new findings on the comorbidity of drug use disorders and chronic conditions as well as its association with hospitalization. The general patterns in the prevalence of SUDs and chronic conditions are consistent with prior studies (Gerteisetal.,2014; Ward and Schiller, 2013; Wu et al., 2015). The associations between SUDs and hospitalization by chronic condition status are in line with other studies of hospitalizations (Berry et al., 2018; Jiang et al., 2015).
4.3. Conclusions
Existing and ongoing large-scale surveys of alcohol/drug use disorders are inadequate for studying top-spending individuals with complex healthcare needs. It is necessary to use the EHR data to identify and characterize patients with multicomorbidity in healthcare settings. While results are constrained by data from one large health system, this study is among the first efforts to comprehensively investigate multicomorbidity of alcohol/drug use disorders and chronic diseases and its association with hospitalization. It adds clinical evidence by showing the presence of SUD (including drug use disorders) as a robust predictor for hospitalization that is independent of the number of comorbid chronic conditions. The findings underscore the clinical importance of and need for treating alcohol/drug use disorders like other chronic conditions with proactive, chronic-care model approaches to enhance treatment engagement, adherence to regimen, self-management skills, and the continuity of care (McLellan et al., 2014). Finally, the high prevalence of hospitalization among a subgroup of patients characterized by having both SUD and multiple chronic conditions calls for research to develop healthcare models for high-risk, complex patients that also treat SUDs (Blumenthal and Abrams, 2016; Powers et al., 2015).
Supplementary Material
Highlights.
Comorbidities of substance use disorders (SUDs) and chronic diseases were examined
In the sample (N=211,880), 48.3% had at least 1 of 9 chronic conditions examined
The prevalence of any SUD (13.3%) increased with the number of comorbidities
Hospitalization was more prevalent among patients with SUD than those without it
Regardless of comorbidity, SUD was associated with elevated odds of hospitalization
Acknowledgments
The authors thanked NIDA CTN’s Publications Committee members and reviewers for their review and comments to help improve the manuscript.
Role of the Funding Source
This study was made possible by research support from the U.S. National Institutes of Health (UG1DA040317, R01MD007658). The sponsoring agency had no further role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the views of NIDA or the National Institutes of Health. NIDA’s staff (Udi E. Ghitza) participation in this publication arises from his role as a project scientist on a cooperative agreement (NIDA CTN-0057), but Dr. Ghitza has not had and will not have any programmatic involvement with the non-cooperative agreement grants/contracts cited.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosures
Conflict of Interest
Li-Tzy Wu has received research funding from Patient-Centered Outcomes Research Institute (PCORI) and Alkermes Inc. The other authors have no conflicts of interest to disclose.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
References
- Abdel‐Rahman O, Helbling D, Schöb O, Eltobgy M, Mohamed H, Schmidt J, Giryes A, Mehrabi A, Iype S, John H, Tekbas A, Zidan A, Oweira H, 2017. Cigarette smoking as a risk factor for the development of and mortality from hepatocellular carcinoma: An updated systematic review of 81 epidemiological studies. J. Evid. Based Med 10, 245–254. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality (AHRQ), 2016. HCUP Clinical Classification Software (CCS) for ICD-9-CM (January 1980 through September 2015) AHRQ, Rockville, MD: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. (accessed February 12 2017). [Google Scholar]
- Berry JG, Gay JC, Maddox KJ, Coleman EA, Bucholz EM, O’Neill MR, Blaine K, Hall M, 2018. Age trends in 30 day hospital readmissions: US national retrospective analysis. BMJ 360, k497 10.1136/bmj.k497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, Whittington J, 2008. The triple aim: are, health, and cost. Health Aff 27, 759–769. [DOI] [PubMed] [Google Scholar]
- Blumenthal D, Abrams MK, 2016. Tailoring complex care management for high-need, high-cost patients. JAMA 316, 1657–1658. [DOI] [PubMed] [Google Scholar]
- Brick J (Ed), 2012. Handbook of the Medical Consequences of Alcohol and Drug Abuse, second ed. The Haworth Press, Taylor and Francis Group, New York. [Google Scholar]
- CASA Columbia, 2000. Missed opportunity: National Survey of Primary Care Physicians and Patients on Substance buse. The National Center on Substance Abuse at Columbia University, New York: https://www.centeronaddiction.org/addiction-research/reports/national-survey-primary-care-physicians-patients-substance-abuse. (accessed February 28, 2018). [Google Scholar]
- Center for Behavioral Health Statistics and Quality (CBHSQ), 2017. 2016 National Survey on Drug Use and Health: Detailed Tables Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf. (accessed August 12, 2018). [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2018. U.S. drug overdose deaths continue to rise; increase fueled by synthetic opioids https://www.cdc.gov/media/releases/2018/p0329-drug-overdose-deaths.html. (accessed August 12, 2018).
- Centers for Medicare and Medicaid Services (CMS), 2014. ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code Titles https://www.cms.gov/medicare/coding/ICD9providerdiagnosticcodes/codes.html. (accessed July 4, 2017).
- Centers for Medicare and Medicaid Services (CMS), 2017. Chronic Conditions https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CC_Main.html. (accessed Januray 12, 2018).
- Centers for Medicare and Medicaid Services (CMS), 2018. Readmissions Reduction Program (HRRP) https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. (accessed April 1, 2018).
- Chuang SC, Lee YC, Hashibe M, Dai M, Zheng T, Boffetta P, 2010. Interaction between cigarette smoking and hepatitis B and C virus infection on the risk of liver cancer: A meta-analysis. Cancer Epidemiol. Biomarkers Prev 19, 1261–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, 2014. Differentials in the concentration of health expenditures across population subgroups in the U.S., 2012. Statistical Brief #448 Agency for Healthcare Research and Quality, Rockville, MD: http://meps.ahrq.gov/mepsweb/data_files/publications/st448/stat448.shtml. (accessed February 10, 2018). [PubMed] [Google Scholar]
- Danford CP, Horvath MM, Hammond WE, Ferranti JM, 2013. Does access modality matter? Evaluation of validity in reusing clinical care data. AMIA Annu. Symp. Proc 2013, 278–283. [PMC free article] [PubMed] [Google Scholar]
- Ducat L, Philipson LH, Anderson BJ, 2014. The mental health comorbidities of diabetes. JAMA 312, 691–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J, Moran E, Li YF, Almenoff PL, 2014. Predicting potentially avoidable hospitalizations. Med. Care 52, 164–171. [DOI] [PubMed] [Google Scholar]
- Gerteis J, Izrael D, Deitz D, LeRoy L, Ricciardi R, Miller T, Basu J, 2014. Multiple chronic conditions chartbook. AHRQ Publications No, Q14–0038 Agency for Healthcare Research and Quality, Rockville, MD: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf. (accessed January 5, 2018). [Google Scholar]
- Ghitza UE, Wu LT, Tai B, 2013. Integrating substance abuse care with community diabetes care: Implications for research and clinical practice. Subst. Abuse Rehabil 4, 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SL, McCarthy D, Radley D, 2016. The impact of a behavioral health condition on high-need adults To the Point, The Commonwealth Fund; http://www.commonwealthfund.org/publications/blog/2016/nov/behavioral-health-high-need-adults. (accessed February 10, 2018). [Google Scholar]
- Hedegaard H, Warner M, Miniño AM, 2017. Drug overdose deaths in the United States, 1999–2016. NCHS data brief, no 294 National Center for Health Statistics, Hyattsville, MD: https://www.cdc.gov/nchs/data/databriefs/db294.pdf. (accessed March 2, 2018). [Google Scholar]
- Heron M, 2016. Deaths: Leading causes for 2013. Natl. Vital Stat. Rep 65, 1–95. [PubMed] [Google Scholar]
- Hoge MA, Morris JA, Laraia M, Pomerantz A, Farley T, 2014. Core competencies for integrated behavioral health and primary care SAMHSA - HRSA Center for Integrated Health Solutions, Washington, DC: https://www.integration.samhsa.gov/workforce/Integration_Competencies_Final.pdf. (accessed February 10, 2018). [Google Scholar]
- Horvath MM, Rusincovitch SA, Brinson S, Shang HC, Evans S, Ferranti JM, 2014. Modular design, application architecture, and usage of a self-service model for enterprise data delivery: The Duke Enterprise Data Unified Content Explorer (DEDUCE). J. Biomed. Inform 52, 231–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (IOM), 2013. Best care at lower cost: The path to continuously learning health care in America The National Academies Press, Washington, DC. [PubMed] [Google Scholar]
- Jiang HJ, Weiss AJ, Barrett ML, Sheng M, 2015. Characteristics of hospital stays for super-utilizers by payer, 2012. HCUP Statistical Brief #190 Agency for Healthcare Research and Quality, Rockville, MD: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb190-Hospital-Stays-Super-Utilizers-Payer-2012.pdf. (accessed February 8,2018). [PubMed] [Google Scholar]
- Kocher RP, Adashi EY, 2011. Hospital readmissions and the Affordable Care Act: aying for coordinated quality care. JAMA 306, 1794–1795. [DOI] [PubMed] [Google Scholar]
- Laderman M, 2015. Behavioral health integration: A key component of the Triple Aim. Popul. Health Manag 18, 320–322. [DOI] [PubMed] [Google Scholar]
- Leshner AI, 1997. Addiction is a brain disease, and it matters. Science 278, 45–47. [DOI] [PubMed] [Google Scholar]
- Levey SMB, Miller BF, deGruy FV, 2012. Behavioral health integration: n essential element of population-based healthcare redesign. Transl. Behav. Med 2, 364–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipari RN, Park-Lee E, Van Horn S, 2016. America’s need for and receipt of substance use treatment in 2015. The CBHSQ Report Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/report_2716/ShortReport-2716.html. (accessed February 1, 2018). [PubMed] [Google Scholar]
- Loheswaran G, Soklaridis S, Selby P, Le Foll B, 2015. Screening and treatment for alcohol, tobacco and opioid use disorders: a survey of family physicians across Ontario. PloS One 10, e0124402 10.1371/journal.pone.0124402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall MM, Kirk GD, Caporaso NE, McCormack MC, Merlo CA, Hague JC, Mehta SH, Engels EA, 2011. Tobacco use and nicotine dependence among HIV-infected and uninfected injection drug users. Addict. Behav 36, 61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Starrels JL, Tai B, Gordon AJ, Brown R, Ghitza U, Gourevitch M, Stein J, Oros M, Horton T, Lindblad R, McNeely J, 2014. Can substance use disorders be managed using the chronic care model? Review and recommendations from a NIDA consensus group. Public Health Rev 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milhorn HT, 2017. Substance Use Disorders: A Guide for the Primary Care Provider Springer, Switzerland. [Google Scholar]
- Military Health System (MHS), 2015. Surveillance Case Definitions https://www.health.mil/Military-Health-Topics/Health-Readiness/Armed-Forces-Health-Surveillance-Branch/Epidemiology-and-Analysis/Surveillance-Case-Definitions. (accessed February 12 2017).
- Muhrer JC, 2010. Detecting and dealing with substance abuse disorders in primary care. J. Nurse Pract 6, 597–605. [Google Scholar]
- Pang Q, Qu K, Zhang J, Xu X, Liu S, Song S, Wang R, Zhang L, Wang Z, Liu C, 2015. Cigarette smoking increases the risk of mortality from liver cancer: a clinical‐based cohort and meta‐analysis. J. Gastroentero. Hepatol 30, 1450–1460. [DOI] [PubMed] [Google Scholar]
- Powers BW,Chaguturu SK,Ferris TG, 2015. Optimizing high-risk care management. JAMA 313, 795–796. [DOI] [PubMed] [Google Scholar]
- Saitz R, Daaleman TP, 2017. Now is the time to address substance use disorders in primary care. Ann. Fam. Med 15, 306–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth R, Scholl L, Rudd RA, Bacon S, 2018. Overdose deaths involving opioids, cocaine, and psychostimulants — United States, 2015–2016. MMWR Morb. Mortal. Wkly. Rep 67, 349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp, 2017. Stata Statistical Software: Release 15 StataCorp LP, College Station, TX. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA), 2017. Behavioral Health Barometer: United States, Volume 4: Indicators as measured through the 2015 National Survey on Drug Use and Health and National Survey of Substance Abuse Treatment Services. HHS Publication No. SMA–17–BaroUS–16 Substance Abuse and Mental Health Services Administration, Rockville, MD: http://www.icctc.org/National_BHBarometer_Volume_4.pdf. (accessed March 10, 2018). [PubMed] [Google Scholar]
- Thorpe K, Jain S, Joski P, 2017. Prevalence and spending associated with patients who have a behavioral health disorder and other conditions. Health Aff 36, 124–132. [DOI] [PubMed] [Google Scholar]
- U.S. Burden of Disease Collaborators, 2018. The state of US health, 1990–2016: Burden of diseases, injuries, and risk factors among US states. JAMA 319,1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau., 2018. QuickFacts United States; Durham County, North Carolina: https://www.census.gov/quickfacts/fact/table/US,durhamcountynorthcarolina/PST045217. (accessed May 3, 2018). [Google Scholar]
- Vivolo-Kantor AM, Seth P, Gladden RM, Mattson CL, Baldwin GT, Kite-Powell A, Coletta MA, 2018. Vital Signs: Trends in emergency department visits for suspected opioid overdoses — United States, July 2016–September 2017. MMWR Morb. Mortal. Wkly. Rep 67, 279–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE, Pham-Kanter G, Donelan K, 2016. Attitudes, practices, and preparedness to care for patients with substance use disorder: Results from a survey of general internists. Subst. Abuse 37, 635–641. [DOI] [PubMed] [Google Scholar]
- Ward BW, Schiller JS, 2013. Prevalence of multiple chronic conditions among US Adults: Estimates from the National Health Interview Survey, 2010. Prev. Chronic Dis 10, 120203 10.5888/pcd10.120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Swartz MS, Wu Z, Mannelli P, Yang C, Blazer DG, 2012. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann. Emerg. Med 60, 172–180 e175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG, Gersing KR, Burchett B, Swartz MS, Mannelli P, NIDA AAPI Workgroup, 2013a. Comorbid substance use disorders with other Axis I and II mental disorders among treatment-seeking Asian Americans, Native Hawaiians/Pacific Islanders, and mixed-race people. J. Psychiatr. Res 47, 1940–1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Gersing KR, Swartz MS, Burchett B, Li TK, Blazer DG, 2013b. Using electronic health records data to assess comorbidities of substance use and psychiatric diagnoses and treatment settings among adults. J. Psychiatr. Res 47, 555–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Ghitza UE, Batch BC, Pencina MJ, Rojas LF, Goldstein BA, Schibler T, Dunham AA, Rusincovitch S, Brady KT, 2015. Substance use and mental diagnoses among adults with and without type 2 diabetes: Results from electronic health records data. Drug Alcohol Depend 156, 162–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Zhu H, Swartz MS, 2016. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend 169, 117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Ghitza UE, Zhu H, Spratt S, Swartz M, Mannelli P, 2018. Substance use disorders and medical comorbidities among high-need, high-risk patients with diabetes. Drug Alcohol Depend 186, 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.