Abstract
Background Radiocarpal or midcarpal arthritis can occur simultaneously with arthritis of the distal radioulnar joint (DRUJ), leading to functional impairment of the wrist. Treatment often involves wrist arthroplasty or arthrodesis, either with simultaneous or secondary procedures, addressing the DRUJ. Successful treatment of solitary DRUJ arthritis with DRUJ replacement has been reported. However, outcomes in patients with multiple prior wrist surgeries are lacking. Surgery in these wrists is challenging because surgical scarring and advanced bone deformities make implant positioning more difficult. Therefore, the aim of this study was to evaluate the outcomes in patients that underwent total wrist arthrodesis and DRUJ replacement after multiple prior wrist surgeries.
Methods We prospectively enrolled patients that underwent total wrist arthrodesis and replacement of the DRUJ, either simultaneously or during separate procedures from 1999 to 2012. We included 14 patients with a median age of 43 years (interquartile range [IQR]: 35–47). As objective outcomes range of motion, weight-bearing ability, grip strength, was measured. For the subjective outcomes, we used an analogue pain score and the disabilities of the arm shoulder and hand (DASH) scores.
Results At a median follow-up of 5.6 years (IQR: 3.2–7.1). The average DRUJ range of motion and weight lifting ability significantly improved. As for the subjective evaluations, postoperative pain scores improved significantly, as did the DASH scores. Four of the patients had a postoperative complication, including infection and heterotopic ossification, of which two required reoperations. Additionally, 5 patients developed pisotriquetral arthritis requiring, pisiform excision, triquetrum excision, or the combination of both.
Conclusion Distal radioulnar joint replacement with a semiconstrained prosthesis was an effective method to restore the function of the wrist and forearm. As the surgical anatomy and soft tissue envelope were compromised in these patients, additional surgical exposure is necessary, adding to the complexity in these patients. No radiographic loosening
Level of Evidence This is a therapeutic level IV study.
Keywords: distal radioulnar joint arthritis, distal radioulnar joint replacement, midcarpal arthritis, radiocarpal arthritis, wrist arthrodesis
The distal radioulnar joint (DRUJ) semiconstrained prosthesis (Aptis Medical, Glenview, KY) has been shown to be an effective reconstructive option for several acute and chronic problems. These include arthritis either isolated or in conjunction with prior trauma or inflammation, instability, or failed prior reconstructive procedures. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17
Placement of the radial component of the implant at or near the original sigmoid notch will optimize its overall function and limit/undo stresses on both components of the implant. In the face of prior wrist surgeries, this may prove technically more difficult. Distorted anatomy of the distal radius, prior surgical incisions, or the presence of a prior implant will add to the surgical complexity.
The aim of this study was to determine the outcomes of a cohort of patients, who underwent distal radioulnar joint arthroplasty in the face of prior wrist surgery.
Materials and Methods
Study Population
After ethics committee approval, we prospectively enrolled patients that underwent distal radioulnar joint prosthesis replacement from 1998 to 2010. We excluded patients that underwent DRUJ replacement without previous wrist surgery. All patients underwent DRUJ arthroplasty, using the Aptis DRUJ prosthesis ( Fig. 1 ; Aptis Medical). We included 14 patients, 7 males and 7 females, with an average age of 44.4 ± 8.5 years ( Table 1 ). Nine patients were manual laborers (military, construction, mechanic, nurse, truck driver, distribution, butcher, mail man) and five patients did not work prior to their DRUJ arthroplasty. The indication for surgery was ulnar sided pain in all patients and five patients also had ulnar stump impingement. The dominant wrist was affected in 10 of 14 patients.
Fig. 1.

Semiconstrained Distal Radioulnar Joint prosthesis composed of the ulnar stem, radial plate, hemi-socket, and polyethylene ball. (Aptis Medical, Glenview, KY)
Table 1. Patient demographics ( n = 14) .
| Age, mean (SD), years | 44.4 (8.5) |
| Male, n (%) | 7 (50) |
| Dominant hand affected, n (%) | 10 (71) |
| Diagnosis, n (%) | |
| Posttraumatic osteoarthritis | 10 (71) |
| Rheumatoid arthritis | 4 (29) |
| Prior DRUJ surgery, n (%) | |
| Distal ulnar resection | 9 (64) |
| Sauvé-Kapandje procedure | 2 (14) |
| Ligamentous DRUJ stabilization | 3 (21) |
| Prior wrist surgery, n (%) | |
| Total wrist arthrodesis | 10 (71) |
| Radioscapholunate arthrodesis | 3 (21) |
| Wrist replacement | 3 (21) |
| Manual laborer, n (%) | 9 (64) |
Abbreviations: SD, standard deviation, DRUJ, distal radioulnar joint.
Prior to DRUJ replacement, five patients had a Darrach, four patients had ulnar head resection with unipolar prosthesis replacement, Sauvé-Kapandji procedure had been performed in two patients of these three patients had previous ligamentous DRUJ stabilization ( Figs. 2 and 3 ). Three patients had unaddressed severe DRUJ osteoarthritis. Previously 10 patients had total wrist arthrodesis, three patients had a radioscapholunate arthrodesis, and three had a wrist arthroplasty. A median of two prior wrist procedures had been performed in the patients.
Fig. 2.
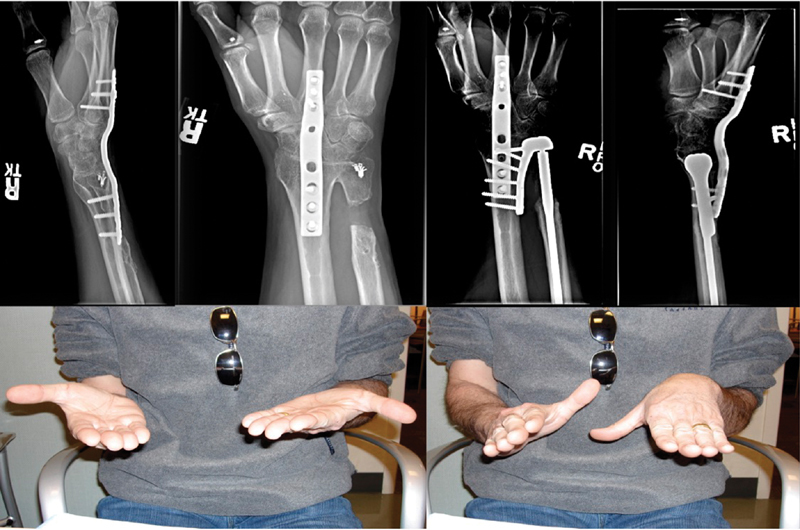
Patient with severe clinical instability of the ulna. Showing preoperative and postoperative radiographs (top) at 6 years of follow-up. Range of motion postoperatively at 6 years of follow-up (below).
Fig. 3.
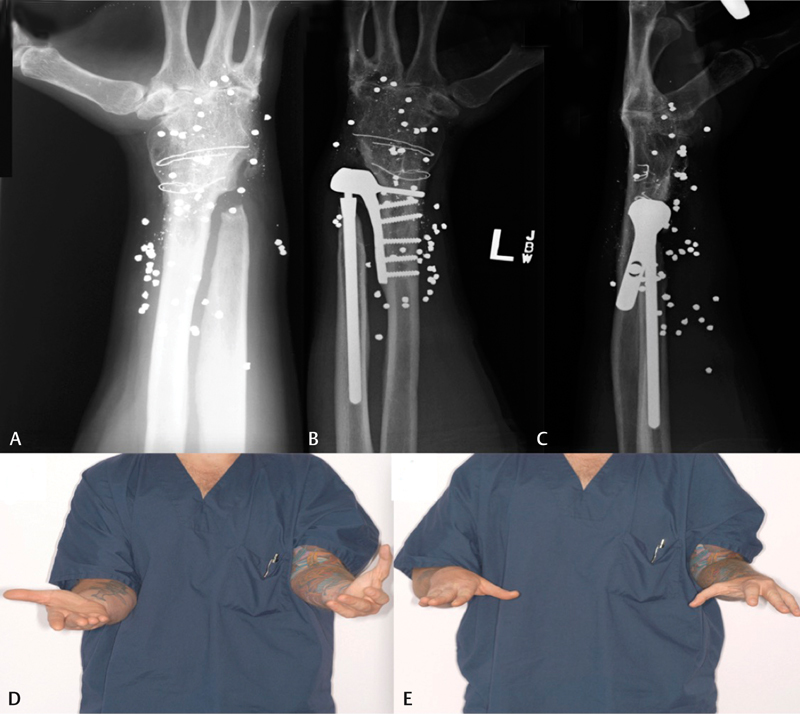
( A ) Wrist radiograph of a patient with prior total wrist arthrodesis presenting with DRUJ instability and severe radius distortion. ( B ) Postoperative antero-posterior wrist radiograph. ( C ) Postoperative lateral wrist radiograph at 9 years of follow-up. ( D , E ) Forearm range of motion at 9 years follow-up.
Surgical Technique
The semiconstrained DRUJ prosthesis is composed of an ulnar stem, a radius plate, a polyethylene ball, and a socket covering, connecting the ulnar stem and the radial plate. 2 The function of the prosthesis matches the function of the distal ulna and radius, by allowing longitudinal migration of the radius throughout pronation and supination, along with the axial rotation of the stem inside the polyethylene ball. This prosthesis also allows the ulna to carry the distal radius against gravitational load. 1 The standard technique for implant placement has been previously described in detail. 18 While each case was different due to the complexity of the initial problem and subsequent surgical procedures, often with a scarred soft tissue envelope, several points should be emphasized. Sufficient soft tissue must be mobilized to have a full view of the lateral column of the distal radius. In the setting of a poorly defined sigmoid notch, the radial component should be placed as distal as possible to still be able to sit easily along the radial column.
Two patients had simultaneous DRUJ arthroplasty and total wrist arthrodesis, which was performed through an incision as for standard wrist fusion extended along the ulnar border of the forearm. The wrist arthrodesis was done first to provide stable orientation of the sigmoid notch. In patients with a prior DRUJ fusion, the ulna was resected at the level of DRUJ using an oscillating saw.
Postoperatively, the patients were placed in a short arm splint for protection of the wrist arthrodesis, allowing immediate pronation and supination. Patients were not immobilized if no arthrodesis was performed. Lifting heavy weights (> 5 kg) was permitted after 4 weeks or until the wrist arthrodesis was healed. In patients, where a wrist arthrodesis had been performed previously, there were no postoperative limitations with regards to mobilization.
Evaluation
We evaluated objective and subjective outcomes during pre- and postoperative clinical visits by the treating surgeon. The preoperative DASH (Disabilities of the Arm, Shoulder and Hand) was available in 10 patients. Pronation and supination of the wrist was measured using a goniometer with the elbow in 90 degrees of flexion. Grip strength was measured using the Jamar Hydraulic Hand Dynamometer (Asimov Engineering Company, LA) in position 2 (4 cm). With the patient in standing position, weight-bearing ability was evaluated by lifting different weights of 2.3, 4.5, 6.8, and 9.1 kg from the elbow in full extension to 90 degrees of flexion (with the forearm in the neutral plane). All measurements were performed three times and the average score was recorded.
We measured pre and postoperative pain scores using an analogue pain scale (0–10 scale) and DASH questionnaire scores. 19 The pain score was recorded when weight bearing in neutral position.
Statistical Analysis
We evaluated the differences between pre- and postoperative range of motion (ROM), weight lifting ability, grip strength, DASH scores, and pain scores using a paired t -test. A level of significance was set at p < 0.05.
Results
Objective and Subjective Outcomes
All postoperative values were recorded at a median final follow-up of 5.6 years (interquartile range [IQR]: 3.2–7.1). The preoperative pronation was 45.6 ± 23.8 degrees and improved to 76.1 ± 17.8 degrees postoperatively ( p < 0.01) ( Table 2 ). The average preoperative supination was 42.3 ± 32.2 degrees and improved to 76.1 ± 15.6 degrees ( p = 0.02) postoperatively. Ten of the 14 patients had full range of forearm rotation, while the other four patients had improvement in motion compared with their preoperative ROM. Weight lifting ability improved significantly from 2.5 ± 1.7 kg preoperatively to 8.5 ± 4.6 kg postoperatively ( p < 0.01). There was no significant increase ( p = 0.08) in grip strength, 16.9 ± 10.8 kg preoperatively versus 26.2 ± 13.1 kg postoperatively.
Table 2. Bivariate analysis objective and subjective outcomes.
| Objective measurements | Preoperative | Postoperative | p -Value |
|---|---|---|---|
| Pronation, mean (SD) degree | 45.6 (23.8) | 76.1 (17.8) | < 0.01 a |
| Supination, mean (SD) degree | 42.3 (32.2) | 76.1 (15.6) | 0.02 a |
| Weight-lifting ability, mean (SD) kg | 2.5 (1.7) | 8.5 (4.6) | < 0.01 a |
| Grip strength, mean (SD) kg | 16.9 (10.8) | 26.2 (13.1) | 0.08 a |
| Subjective measurements | |||
| Pain score, mean (SD) | 6.57 ± 2.00 | 1.29 ± 2.16 | < 0.01 a |
| DASH score, mean (SD) | 77.10 ± 9.62 | 29.94 ± 24.11 | < 0.01 a |
Abbreviations: DASH, disabilities of the arm, shoulder, and hand; SD, standard deviation.
Using paired t -test.
The mean DASH score improved significantly from 77.1 ± 9.6 preoperative to 29.9 ± 24.1 postoperatively ( p < 0.01). The pain score improved significantly from 6.6 ± 2.0 compared with 1.3 ± 2.2 postoperatively ( p < 0.01). Of the nine manual laborers, six returned to work fully, two returned to work partially, and one patient did not return to work. There was no postoperative radiologic loosening of the prosthesis in any patient.
Pain and Complications
Additional surgical procedures were required in seven patients, of which two were directly implant related ( Table 3 ). One patient required implant removal and insertion of antibiotic cement bands to treat a deep infection. After the infection was cleared, the DRUJ implant was reinserted. One patient required excision of heterotopic ossification around the ulna. The chief non–implant-related complaint was new-onset ulnar sided wrist pain which occurred in five patients 6 to 14 months postoperatively. Three of these patients underwent pisiform excision, one patient underwent excision of the triquetrum, and one patient underwent excision of the pisiform and triquetrum. These complaints were diagnosed by direct palpation over the pisiform. This differed from the preoperative complaints as the preoperative pisotriquetral grind test was negative. After this procedure patients were symptom free. Superficial infections occurred in two patients who were treated successfully with antibiotics without surgical intervention. Two patients subsequently underwent total wrist arthrodesis within 3 years of DRUJ arthroplasty due to ongoing radiocarpal pain, posttraumatic osteoarthritis, or rheumatoid arthritis.
Table 3. Postoperative complications, complaints, and reoperations.
| Postoperative complications ( n = 4) | |
|---|---|
| Infection, n (%) | |
| Superficial | 2 (40) |
| Deep | 1 (20) |
| Heterotopic ossification, n (%) | 1 (20) |
| Postoperative complaints ( n = 5) | |
| Ulnar sided wrist pain, n (%) | 5 (100) |
| Reoperations ( n = 7) | |
| Pisiform excision, n (%) | 3 (43) |
| Triqeutrum excision, n (%) | 1 (14) |
| Pisiform and triquetrum excision, n (%) | 1 (14) |
| Implant reinsertion, n (%) | 1 (14) |
| Heterotopic ossification excision, n (%) | 1 (14) |
Discussion
Partial or total wrist arthrodesis is not without its associated complications including nonunion, infection, wound complications, nerve complications, and problems involving the distal radioulnar joint. 20 Zachary et al reported that 3% of their patients who have had total wrist arthrodesis needed distal ulna resection because of DRUJ pain or ulnar abutment within one year postoperatively. 21 Many authors have also reported this adjacent joint arthritis phenomenon in varying rates. 22 23 24 A factor influencing this could be the use of the second metacarpal in fixation of the arthrodesis, deviating the wrist ulnarly causing ulnocarpal abutment. 20 Until recently, one of the few available options for ulnocarpal abutment syndrome after a total arthrodesis of the wrist was excision of the distal ulna or the affected carpal bone. 20 21 However, loss of the DRUJ can be painful and debilitating due to impingement of the ulna on the distal radius, especially during lifting heavy weights. 25 26 Preservation of the DRUJ joint is important for the lifting capacity of the wrist, during which the gravitational load runs from the wrist or hand to the ulnar head. 27 In a biomechanical study by Shaaban et al, this was confirmed. 28 Salvage procedures of the DRUJ such as Darrach or Sauvé Kapandji procedure can result in impingement of the stump of the distal ulna on the distal radius causing pain, especially in active patients. 29 30 Nonetheless, Darrach and Sauvé Kapandji treatments remain good and effective to treat DRUJ arthritis.
The semiconstrained DRUJ prosthesis was designed to restore function lost after failed salvage procedures and has been inserted in over 3,600 patients. Long-term studies show it to be a reliable, reproducible alternative to other DRUJ procedures. 1 This device offers a pain free, stable joint, especially in an active patient having simultaneous arthritis in the carpus and the DRUJ. In this series, we support these findings in patients with multiple prior wrist surgeries, as we showed improved range-of-motion and lifting strength, and subjectively decreased pain after arthrodesis with DRUJ replacement. That grip strength did not improve can be explained by the fact that patients had advanced osteoarthritis of the wrist. The number of reoperations is not surprising given the scared soft tissue envelope, numerous prior surgeries, and distorted bony anatomy. Additionally, the DRUJ arthroplasty may have changed the force-axis of the flexor carpi ulnaris, for which the pisiform acts as a fulcrum, changing the pistotriquetral joint biomechanics causing pisotriquetral arthritis. 31 32
The technical difficulties of the placement of the DRUJ implant are increased in the setting of prior surgical procedures involving the radiocarpal joint. These include the presence of prior incisions limiting the ability to create an extensile approach for the DRUJ implant. The need to remove a fusion plate on the dorsum of the radius further creates additional risk of wound healing. The several instances of wound problems and local infection in this series may reflect this risk. Distortion of the radius will make placement of the radial component considerably more difficult. Lastly, prior surgical procedures in the distal radioulnar joint may lead to a contracted and noncompliant interosseous space, adding to the complexity of a more accurate placement of the radial component. From our experience, we suggest sufficient soft tissue mobilization and distal placement of the radial component when implantation of a semiconstrained DRUJ prosthesis in the scarred wrist.
We need to interpret these results in respect to its strengths and limitations. First, only 10 of the 14 patients had preoperative DASH scores. Second, the diagnosis in this population was inhomogeneous. Finally, we only present a small cohort limiting the statistical analysis. The value of this study is that it shows midterm outcomes of patients that underwent DRUJ replacement, showing that it is a viable option.
In conclusion, using the semiconstrained DRUJ prosthesis as an addition to wrist arthrodesis will improve forearm function in patients with carpal and DRUJ arthritis in the setting of multiple previous wrist surgeries. We have shown that DRUJ replacement improves objective and subjective outcomes in these patients. However, it is important to be aware of the increased complexity of DRUJ replacement in this population and that there is a high reoperation rate.
Conflict of Interest Author L.R.S. is part owner of Aptis Medical LLC, manufacturer of the Aptis total DRUJ replacement prosthesis. Authors S.C., J.L., and J.B.J. have no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) or financial remunerations that might pose a conflict of interest in connection with the submitted article.
Authors' Contributions
Study design: S.H.C., J.B.J., L.R.S. Data assembly: S.H.C., J.L. Data analysis: S.H.C., J.L. Initial draft: S.H.C., J.L., J.B.J., L.R.S. Final approval of manuscript: S.H.C., J.L., J.B.J., L.R.S.
Note
This work was performed at the Christine M. Kleinert Institute for Hand and Microsurgery, University of Louisville School of Medicine, Louisville, Kentucky in collaboration with Hand and Upper Extremity Service, Department of Orthopedic Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts.
References
- 1.Laurentin-Pérez L A, Goodwin A N, Babb B A, Scheker L R. A study of functional outcomes following implantation of a total distal radioulnar joint prosthesis. J Hand Surg Eur Vol. 2008;33(01):18–28. doi: 10.1177/1753193408087118. [DOI] [PubMed] [Google Scholar]
- 2.Scheker L R, Babb B A, Killion P E. Distal ulnar prosthetic replacement. Orthop Clin North Am. 2001;32(02):365–376. doi: 10.1016/s0030-5898(05)70256-x. [DOI] [PubMed] [Google Scholar]
- 3.Coffey M J, Scheker L R, Thirkannad S M. Total distal radioulnar joint arthroplasty in adults with symptomatic Madelung's deformity. Hand (NY) 2009;4(04):427–431. doi: 10.1007/s11552-009-9182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zimmerman R M, Jupiter J B. Outcomes of a self-constrained distal radioulnar joint arthroplasty: a case series of six patients. Hand (NY) 2011;6(04):460–465. doi: 10.1007/s11552-011-9365-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Espinosa-Gutiérrez A, Romo-Rodríguez R. [Semiconstrained bipolar implant arthroplasty of the distal radioulnar joint. Case report] Cir Cir. 2013;81(01):55–59. [PubMed] [Google Scholar]
- 6.Degreef I, De Smet L. The Scheker distal radioulnar joint arthroplasty to unravel a virtually unsolvable problem. Acta Orthop Belg. 2013;79(02):141–145. [PubMed] [Google Scholar]
- 7.Axelsson P, Sollerman C. Constrained implant arthroplasty as a secondary procedure at the distal radioulnar joint: early outcomes. J Hand Surg Am. 2013;38(06):1111–1118. doi: 10.1016/j.jhsa.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 8.Savvidou C, Murphy E, Mailhot E, Jacob S, Scheker L R. Semiconstrained distal radioulnar joint prosthesis. J Wrist Surg. 2013;2(01):41–48. doi: 10.1055/s-0032-1333466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bizimungu R S, Dodds S D. Objective outcomes following semi-constrained total distal radioulnar joint arthroplasty. J Wrist Surg. 2013;2(04):319–323. doi: 10.1055/s-0033-1358544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kakar S, Fox T, Wagner E, Berger R. Linked distal radioulnar joint arthroplasty: an analysis of the APTIS prosthesis. J Hand Surg Eur Vol. 2014;39(07):739–744. doi: 10.1177/1753193414523189. [DOI] [PubMed] [Google Scholar]
- 11.Galvis E J, Pessa J, Scheker L R. Total joint arthroplasty of the distal radioulnar joint for rheumatoid arthritis. J Hand Surg Am. 2014;39(09):1699–1704. doi: 10.1016/j.jhsa.2014.03.043. [DOI] [PubMed] [Google Scholar]
- 12.Kachooei A R, Chase S M, Jupiter J B. Outcome Assessment after Aptis Distal Radioulnar Joint (DRUJ) Implant Arthroplasty. Arch Bone Jt Surg. 2014;2(03):180–184. [PMC free article] [PubMed] [Google Scholar]
- 13.Martínez Villén G, García Martínez B, Aso Vizán A. Total distal radioulnar joint prosthesis as salvage surgery in multioperated patients. Chir Main. 2014;33(06):390–395. doi: 10.1016/j.main.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Sander A L, Ebert F, Marzi I, Frank J. Ergebnisse nach Implantation der Aptis-Prothese zum Ersatz des distalen Radioulnargelenks. Handchir Mikrochir plast Chir. 2015;47(05):306–311. doi: 10.1055/s-0035-1550035. [DOI] [PubMed] [Google Scholar]
- 15.Rampazzo A, Gharb B B, Brock G, Scheker L R. Functional outcomes of the aptis-scheker distal radioulnar joint replacement in patients under 40 years old. J Hand Surg Am. 2015;40(07):1397–1403. doi: 10.1016/j.jhsa.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 16.Giwa L, Spacey K, Packer G. Management of a complex, multioperated intra-articular distal radius fracture. J Wrist Surg. 2015;4(03):179–182. doi: 10.1055/s-0035-1558832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Imbriglia J E, Matthews D. Treatment of chronic post-traumatic dorsal subluxation of the distal ulna by hemiresection-interposition arthroplasty. J Hand Surg Am. 1993;18(05):899–907. doi: 10.1016/0363-5023(93)90064-A. [DOI] [PubMed] [Google Scholar]
- 18.Scheker L R. Implant arthroplasty for the distal radioulnar joint. J Hand Surg Am. 2008;33(09):1639–1644. doi: 10.1016/j.jhsa.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 19.Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4(01):11. doi: 10.1186/1471-2474-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wysocki R W, Cohen M S. Complications of limited and total wrist arthrodesis. Hand Clin. 2010;26(02):221–228. doi: 10.1016/j.hcl.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Zachary S V, Stern P J. Complications following AO/ASIF wrist arthrodesis. J Hand Surg Am. 1995;20(02):339–344. doi: 10.1016/S0363-5023(05)80037-1. [DOI] [PubMed] [Google Scholar]
- 22.Kleinman W B. Long-term study of chronic scapho-lunate instability treated by scapho-trapezio-trapezoid arthrodesis. J Hand Surg Am. 1989;14(03):429–445. doi: 10.1016/s0363-5023(89)80002-4. [DOI] [PubMed] [Google Scholar]
- 23.Minami A, Kato H, Suenaga N, Iwasaki N. Scaphotrapeziotrapezoid fusion: long-term follow-up study. J Orthop Sci. 2003;8(03):319–322. doi: 10.1007/s10776-003-0641-z. [DOI] [PubMed] [Google Scholar]
- 24.Watson H K, Wollstein R, Joseph E, Manzo R, Weinzweig J, Ashmead D., IV Scaphotrapeziotrapezoid arthrodesis: a follow-up study. J Hand Surg Am. 2003;28(03):397–404. doi: 10.1053/jhsu.2003.50072. [DOI] [PubMed] [Google Scholar]
- 25.Bell M J, Hill R J, McMurtry R Y. Ulnar impingement syndrome. J Bone Joint Surg Br. 1985;67(01):126–129. doi: 10.1302/0301-620X.67B1.3968131. [DOI] [PubMed] [Google Scholar]
- 26.Lees V C, Scheker L R. The radiological demonstration of dynamic ulnar impingement. J Hand Surg: Br Eur Volume. 1997;22(04):448–450. [Google Scholar]
- 27.Markolf K L, Lamey D, Yang S, Meals R, Hotchkiss R. Radioulnar load-sharing in the forearm. A study in cadavera. J Bone Joint Surg Am. 1998;80(06):879–888. doi: 10.2106/00004623-199806000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Shaaban H, Giakas G, Bolton M et al. The load-bearing characteristics of the forearm: pattern of axial and bending force transmitted through ulna and radius. J Hand Surg [Br] 2006;31(03):274–279. doi: 10.1016/j.jhsb.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 29.Papatheodorou L K, Rubright J H, Kokkalis Z T, Sotereanos D G. Resection interposition arthroplasty for failed distal ulna resections. J Wrist Surg. 2013;2(01):13–18. doi: 10.1055/s-0032-1333062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watson H K, Brown R E.Ulnar impingement syndrome after Darrach procedure: treatment by advancement lengthening osteotomy of the ulna J Hand Surg Am 198914(2 Pt 1):302–306. [DOI] [PubMed] [Google Scholar]
- 31.Beckers A, Koebke J. Mechanical strain at the pisotriquetral joint. Clin Anat. 1998;11(05):320–326. doi: 10.1002/(SICI)1098-2353(1998)11:5<320::AID-CA5>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 32.Pevny T, Rayan G M, Egle D. Ligamentous and tendinous support of the pisiform, anatomic and biomechanical study. J Hand Surg Am. 1995;20(02):299–304. doi: 10.1016/S0363-5023(05)80030-9. [DOI] [PubMed] [Google Scholar]


