Abstract
Objectives.
African American men who have sex with men and women (MSMW) are among the populations at highest need for HIV prevention programs in the United States. We tested a theory-based, community participatory behavioral intervention aiming to reduce sexual risk for HIV transmission in this population.
Methods.
A randomized clinical trial involving 396 African American MSMW who were assigned to a 4-session intervention involving HIV testing and counseling (n=199) or to a HIV testing and counseling only (n=197) control. In the 4-session intervention program, counselors provided education on HIV and STI risk, condom use, HIV testing, interpersonal sexual dynamics with both male and female partners, and motivational “triggers” of condomless sex. Participants completed baseline, 6-month, and 9-month assessments, and changes in HIV behavioral risk indicators were examined by condition and time.
Results.
There were no statistically significant differences in sexual risk between the intervention condition and the control condition. Regardless of condition, participants reported significant reductions in mean number of condomless sex events with female casual partners from baseline (6.04) to 6-months (2.58) and 9-months (1.47), and with male casual partners from baseline (2.61) to 6-months (1.18) and 9-months (0.60). Condition-by-time interaction effects and condition main effects were non-significant.
Conclusions.
Although there were no significant differences by condition, findings support the effects of brief behavioral counseling and HIV testing on reducing condomless sex with casual female and male partners among African American MSMW. Future research should examine further the potential for brief behavioral counseling to promote biomedical HIV prevention and to reduce co-morbid health issues such as substance use among African American MSMW.
Keywords: HIV Prevention Intervention, Bisexual, Non-Gay Identified Men, HIV Testing, Sexual Risk
Introduction
African Americans represent almost half of individuals who test positive for HIV in the United States (Centers for Disease Control, 2018). In 2016, 17,528 African Americans were newly diagnosed with HIV/AIDS, more than half of these cases (58%) were among gay or bisexual men (Centers for Disease Control and Prevention, 2018). If current incidence rates continue, 1 in 2 African American gay and bisexual men will be diagnosed with HIV in their lifetime (Centers for Disease Control and Prevention, 2016). A growing number of behavioral HIV prevention interventions targeting African American men who have sex with men (MSM) have been effective in reducing condomless sex (Maulsby, et al., 2013). In addition to providing education and behaviors skills about condom use, effective interventions with African American MSM have addressed motivational and social factors associated with sexual risk behaviors. For example, one effective HIV prevention program for African American MSM, entitled Many Men, Many Voices (3MV), is endorsed by the Centers for Disease Control and Prevention (CDC) and involves small-group activities facilitated by trained peer educators to facilitate HIV awareness and group discussions of homosexual/gay identity and cultural, religious, and social norms related to sexual behavior and risk reduction (Wilton, et al., 2009). Another CDC-endorsed intervention, entitled D-up, or Defend Yourself, (Jones, et al., 2008) uses peer leaders and social networks of gay-identified African American men to change social norms and promote condom use within these networks.
A growing body of research brings attention to African American MSM who also have sex with women but who do not identify as gay/homosexual or bisexual. Research with these men has reported high levels of condomless sex with both female and male partners, including condomless sex while under the influence of alcohol and other substances, high levels of exchange sex, as well as suboptimal levels of HIV knowledge and testing behaviors (Dyer et al., 2013; Lauby, et al. 2008). Researchers have also noted the presence of gender role conflict and hypermasculinity among African American men who have sex with men and women (MSMW), which have been associated with psychological distress, internalized homophobia, increased numbers of male and female partners, and unprotected vaginal or anal intercourse (LaPollo, Bond, & Lauby, 2014; Bingham, Harawa, & Williams, 2013). Studies that have compared MSMW to MSM only (MSMO) have found that MSMW were more likely to be African American than White, to have higher rates of depression, to engage in polydrug use, to have more dense social and sexual networks, and to have higher viral loads than MSMO (Latkin et al., 2011; Singh, Hu, Wheeler, & Hall, 2014; Friedman et al., 2014a). In a systematic review that compared HIV prevalence for MSMW to MSMO and MSW only, researchers estimated that approximately 1.0% of US males are MSMW, and approximately 121,800 of these bisexually active men are living with HIV (Friedman et al., 2014b). They also reported that MSMW were less than half as likely to be HIV positive than MSMO, yet were five times more likely to be HIV positive than MSW only (Friedman et al., 2014b).
African American MSMW may challenge targeted HIV prevention approaches with MSM that focus explicitly on sexual orientation categories and identities. In particular, African American MSMW who do not identify themselves as homosexual/gay or as bisexual are unlikely to associate with social networks of other openly homosexual/gay or bisexual men, and thus are unlikely to participate in programs that prioritize gay identity and gay community affiliation as foundations for HIV prevention (Malebranche, 2008). Previous research has indicated that these men prioritize secrecy about their same sex behaviors and prefer not to disclose their sexuality in group settings (Operario, Smith, & Kegeles, 2008). Studies have also suggested that some African American MSMW view their same-sex behaviors within compartmentalized episodes (i.e., discrete behaviors that are disconnected from identity) or as consequences of social/environmental “triggers” (e.g., occurring while under the influence, or during moments of extreme stress or sexual arousal) rather than as markers of sexual identity, orientation, or preference (Malebranche, Arriola, Jenkins, Dauria, & Patel, 2010).
Intervention researchers have begun to apply behavioral risk reduction strategies that have been found to be successful with African American MSM to HIV prevention programs specifically tailored to African American MSMW. For example, the MAALES intervention uses a small group format to promote HIV risk reduction for African American MSMW. This intervention was efficacious in reducing unprotected sex acts for female partners but was not significantly associated with reductions in unprotected sex acts for male partners (Harawa et al, 2013). More recently, a six session, individual-level intervention, known as Project RISE, used an ecosystems approach to HIV prevention for African American MSMW, and was found to be efficacious in reducing number of female partners, as well as numbers of condomless sex events with female partners, and with all partners at follow up (Lauby et al., 2018). Given the complexity of the sexual lives of African American MSMW, their dense social and sexual networks, and continued risk for HIV, culturally sensitive prevention programs that meet the unique needs of this population continue to be needed.
We developed a behavioral HIV prevention program for African American MSMW who do not identify as gay/homosexual or bisexual, entitled the Bruthas Project (or Bruthas), to be delivered in conjunction with HIV testing and counseling. Guided by principles of community-based participatory research, we developed a team of university-based researchers and community-based HIV prevention providers who worked in partnership to identify the research agenda and priorities. We used qualitative methodologies to identify social and cultural factors that contribute to HIV risk behaviors in this population, and based on these findings designed a culturally sensitive intervention to target modifiable risk factors (described in Methods). We also identified program implementation factors to enhance participation and engagement of African American MSMW in the program. Bruthas was based on the Information-Motivation-Behavior (IMB) model of health behavior change (Fisher & Fisher, 1996), and involved a series of four individual counseling sessions with a trained peer educator who was either from the target population or familiar with same sex sexuality. Sessions addressed principles of HIV and STI transmission risk, HIV testing behaviors, contextual and relationship factors related to sex with both female and male partners, and motivational or situational “triggers” of condomless sex such as loneliness, anxiety, or drug use. Bruthas was designed to be implemented in conjunction with culturally sensitive HIV testing and counseling services provided in community-based settings, and consists of four supplemental one-on-one counseling sessions for men to discuss their HIV-related risk behaviors. These tailored individual counseling sessions were explicitly designed for African American MSMW who have knowledge of their current HIV status by either having just tested or by being previously diagnosed with HIV. Full details about Bruthas are provided elsewhere (Arnold et al., 2015).
We conducted a randomized controlled trial to evaluate effects of the Bruthas Project on HIV risk behavior among African American MSMW who do not identify as gay/homosexual or bisexual. We hypothesized that individuals who participate in the culturally appropriate four-session Bruthas intervention would report reduced condomless sex with male and female (cisgender and transgender) partners compared with those who received a single session, featuring only the culturally appropriate HIV testing and counseling. The trial was registered at Clinicaltrials.gov (NCT01270230).
Methods
Participants
Eligibility criteria included being at least 18 years old, identifying as cis-gender male, living in the San Francisco Bay Area, having had sex (anal, vaginal or oral) with at least one male and one female in the past 12 months, and not currently enrolled in another HIV prevention intervention program. Individuals who identified as HIV-negative, status unknown, and positive were eligible. Prior to data collection, when the study design was originated we estimated that a minimum of n=170 individuals per group would be needed for analysis under the assumptions of power (1-β)=0.80, α=0.05, three observational assessments per individual, and a Cohen h statistic effect size range from 0.2 to 0.3. Recruitment occurred from February 2011 to May 2014. With input from a community advisory board, we identified community and commercial venues (e.g., parks, nightclubs, bars), street locations, and non-profit and health service agencies where members of the target population gather. Using mobile units, our team was able to recruit from outside nightclubs, parks, and street locations. We also disseminated informational fliers about the research study containing contact information for the project office. Potential participants were informally screened on the street and then invited inside our private mobile clinics or to the project office for the formal computer-based screening and study intake. We formally screened 565 men of whom 396 met eligibility criteria and enrolled in the study. Everyone who screened as eligible was enrolled. Informed consent was obtained from all participants enrolled in the study.
Procedures
After providing informed consent, participants completed a baseline survey (see Measures) using audio computer-assisted self-interviewing (ACASI) and provided personal contact information. Participants were then randomized to the intervention condition (n=199) or control condition (n=197) by a research assistant using a pre-determined randomization pattern produced by a computer algorithm. A separate randomization pattern was executed for each of 4 groups defined through simultaneous stratification of potential participants by HIV status (HIV-negative/HIV-unknown vs. HIV-positive) and baseline sexual risk behavior (condomless anal intercourse with a male partner in the past 3 months vs. no condomless anal intercourse in the past 3 months). Each group randomization pattern changed with every 10 participants enrolled in that group. This was done to ensure that balance was maintained within each of the four groups between intervention and control conditions throughout the lengthy recruitment process. Neither the participants nor the research assistants knew condition assignments in advance.
Participants who self-reported being HIV-negative or status-unknown in the baseline survey then completed rapid HIV testing and counseling with trained project staff, who were African American men themselves. One participant tested positive for HIV during this process and was immediately referred to confirmatory testing and care, but remained enrolled in the study in accordance with the study protocol. Participants randomly assigned to the intervention group received schedules for subsequent counseling sessions, and all participants received schedules for 6- and 9- month follow-up assessments. We made phone calls to all participants after 3-months to update their contact information and to remind them of the time and location of follow-up assessments. Participants received $35 for each survey assessment and counseling session completed. The Committee on Human Research, the Institutional Review Board at the University of California San Francisco (UCSF), approved the study protocol.
Intervention.
The intervention followed theoretical principles of the IMB model of health behavior change, (Fisher and Fisher, 1996) and was designed to supplement the intake session which included HIV testing and behavioral counseling for negative and status unknown participants. African American male counselors were trained to provide culturally sensitive and non-judgmental educational information, motivational messages, and behavioral skills lessons and reinforcement. Four bi-weekly sessions, delivered over approximately 3 months, were provided to supplement a culturally tailored HIV testing and counseling session at intake. The intake session included rapid HIV testing and counseling, which featured discussion of general HIV and STI risk factors, condom use, and recognizing personal risk. This content was tailored from standardized testing and counseling to be specific to men who have sex with both men and women, and to emphasize a non-judgemental approach to complex sexual partnerships and interactions. The first supplemental intervention session was scheduled two weeks after participants completed the baseline assessment and testing, and covered information about the local epidemic; a personal risk assessment, which included a discussion of relationships and sexual communication; a condom demonstration; and the importance of regular testing. The second session, delivered two weeks later, addressed sexual risk behaviors and routes for HIV transmission with female partners, as well as relationship dynamics with main female sex partners and casual female sex partners. The third session addressed sexual risk behavior and routes for HIV transmission with male partners, as well as relationship dynamics with main male sex partners and casual male sex partners. The fourth session addressed situational contexts and motivational “triggers” for condomless sex with female and male partners (both main and casual), and concluded with a specific individualized plan for reducing HIV-related risk behavior according to gender and type of partner. Counselors were trained in principles of motivational counseling (e.g., using affirming and non-judgmental language and reinforcement) and were instructed to not make assumptions about participants’ sexual identity or orientation in all sessions. Sessions 2-4 included interactive role play scenarios in which participants described their responses to realistic sexual episodes with female and male partners. Based on these activities, counselors provided supportive feedback and reinforcement about engaging in lower risk behaviors. As “homework” assignments between sessions 2-4, participants were asked to practice behavioral risk reduction skills with their partners.
Control.
In the control condition, participants completed only culturally tailored HIV testing and counseling, which featured a general discussion HIV and STI risk factors, condom use, and discussion about knowing one’s HIV status and recognizing personal risk. This counseling was based on standardized HIV testing and counseling, but was tailored to African American men who have sex with both men and women in that it included non-judgmental and open discussion of sexual activities with both men and women. Control participants had no further contact with the intervention counselor after the session. All participants who reported negative or unknown sero-status were HIV tested as part of the intake session using rapid tests and provided their results.
Measures
Demographics.
We asked about age, educational attainment, employment status, income level in the past month, history of incarceration (lifetime and past 3 months), and homelessness in the past year.
HIV Status.
HIV status was self-reported in each survey assessment. In addition, at enrollment we provided HIV testing to participants who reported unknown or HIV-negative serostatus. Consequently, by the completion of the Baseline phase of the study we no longer had any status unknown participants.
Sexual Behavior.
We asked participants to enumerate their female, male, and transgender female sexual partners in the last 3 months. Participants were asked to differentiate sexual partners by main partner and casual partner status. For each sexual partner status, we asked participants to report frequency of vaginal and/or anal intercourse (i.e., number of times) in the last 3 months, and frequency of intercourse using condoms and not using condoms in the past 3 months.
Data Analysis
All statistical analyses were performed using algorithms in Stata Version 14 which employ maximum likelihood estimation of parameters in mixed effects models. For each outcome the initial analysis model included fixed effects for Condition (Control vs. Intervention) and Time (Baseline vs. 6-month follow-up vs. 9-month follow-up) plus the Condition by Time interaction, and allowed for random intercepts and random slopes for Time to accommodate inter-individual variation in Baseline scores and score trajectories. The covariance matrix for the random effects was specified to be unstructured. Given that the outcomes are counts, we first attempted mixed effects negative binomial regression, but none of those models would converge. Observation of the data suggested over-specification of the models due to lack of variation in individual slopes, but non-convergence precluded direct quantitative assessment of that assertion. Instead, we log transformed the outcomes and employed mixed effects linear regression models. Graphical investigation of residuals revealed normal-like distributions and no evidence of non-constant error variance. In addition, the results were calculated with robust variance estimates to further guard against errors due to model misspecification or any remaining assumption violations. For any outcome where the Condition by Time interaction was determined to be statistically nonsignificant (p > 0.05), the mixed effects liner regression analysis was repeated with the interaction effect deleted. A sensitivity analysis was undertaken in the form of mixed effects negative binomial regression with random intercepts, but not random slopes. These models converged easily and yielded identical conclusions about which effects were statistically significant. This lends added confidence in our results.
Results
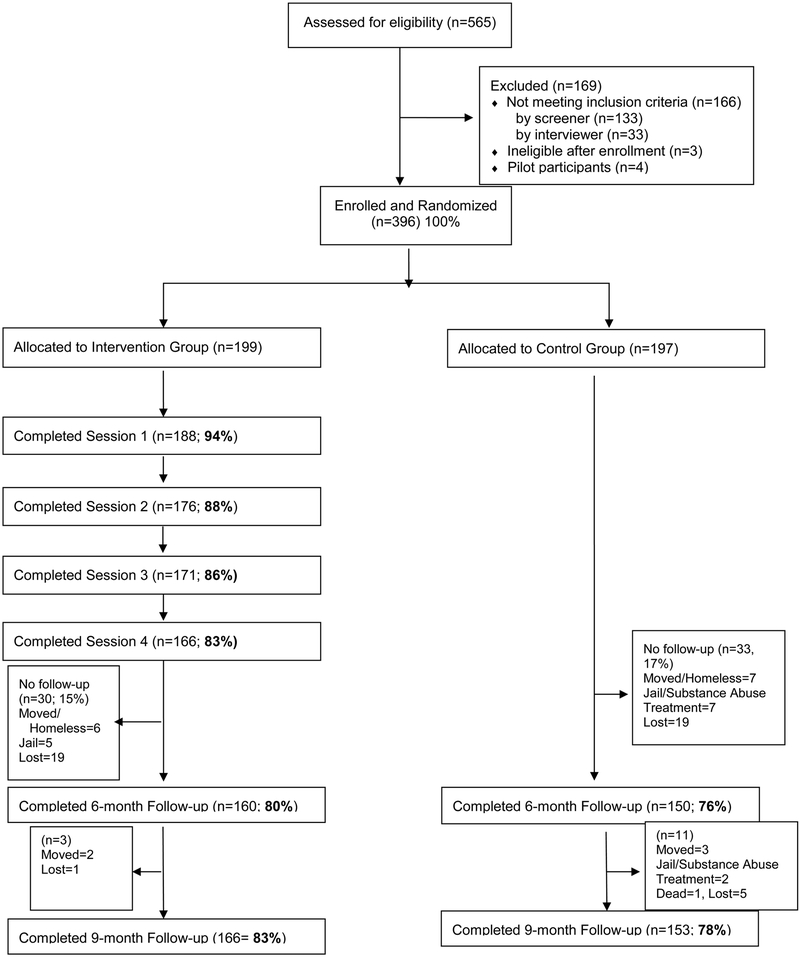
Figure 1 provides information about screening, enrollment, and retention of participants, and Table 1 provides descriptive information about the cohort. Over the course of the trial, we retained 80% of participants in the intervention arm and 76% of participants in the control arm at 6 months follow up (χ2=1.06, df=1, p=.304), and 83% of participants in the intervention arm and 78% of participants in the control arm at 9 months follow up (χ2=2.09, df=1, p=.148), the trial’s conclusion. Thus, there were no significant differences in attrition between the intervention and control conditions. Reasons for attrition included moving, incarceration, and entry into residential substance use treatment facilities. Our sample was relatively older, and characterized by low socioeconomic status (see Table 1). The average participant age was 45.9 years (SD=9.64). The majority (72.8%) were unemployed, and 86.6% earned less than $1,000 income during the previous month. Overall, 27.0% did not complete high school, 43.7% had a high school diploma or GED, 21.5% had some college, and 7.8% had a college degree. Additionally, 51.4% were homeless at some time during the past year, 92.4% had ever been incarcerated (15.2% were incarcerated during the past 3 months), and 16.7% were HIV-positive at baseline. There were no differences between intervention and control groups on these characteristics.
Figure 1:
Bruthas Project Participant Flow Chart
Table 1.
Baseline: Demographic Characteristics of Bruthas Cohort
| Variable | Category | Total (N=396) |
Control (n=197) |
Intervention (n=199) |
Control vs. Intervention |
||
|---|---|---|---|---|---|---|---|
| % | % | % | χ2 | df | p-value | ||
| Age1 | 5.71 | 3 | 0.13 | ||||
| 19-34 | 13.6 | 15.2 | 12.1 | ||||
| 35-44 | 22.7 | 26.4 | 19.1 | ||||
| 45-54 | 46.7 | 41.1 | 52.3 | ||||
| 55 or older | 16.9 | 17.3 | 16.6 | ||||
| Education | 3.60 | 3 | 0.31 | ||||
| < HS diploma | 27.0 | 29.4 | 24.6 | ||||
| HS diploma/GED | 43.7 | 41.1 | 46.2 | ||||
| Some college | 21.5 | 19.8 | 23.1 | ||||
| College degree | 7.8 | 9.6 | 6.0 | ||||
| Employment | 2.37 | 3 | 0.50 | ||||
| Employed full-time | 5.3 | 6.1 | 4.5 | ||||
| Employed part-time | 9.1 | 10.2 | 8.1 | ||||
| Employed sometimes | 12.7 | 14.3 | 11.1 | ||||
| Unemployed | 72.8 | 69.4 | 76.3 | ||||
| Income (last month) | 3.39 | 3 | 0.34 | ||||
| $0 - $249 | 33.3 | 33.0 | 33.7 | ||||
| $250 - $499 | 19.4 | 17.3 | 21.6 | ||||
| $500 - $999 | 33.8 | 33.5 | 34.2 | ||||
| $1,000 or more | 13.4 | 16.2 | 10.6 | ||||
| Homeless (past year) | 1.11 | 1 | 0.29 | ||||
| Yes | 51.4 | 48.7 | 54.0 | ||||
| No | 48.6 | 51.3 | 46.0 | ||||
| Prison/Jail | 2.98 | 2 | 0.23 | ||||
| Never | 7.6 | 6.1 | 9.1 | ||||
| > 3 months ago | 77.2 | 76.0 | 78.3 | ||||
| In past 3 months | 15.2 | 17.9 | 12.6 | ||||
| Serostatus2 | 0.24 | 1 | 0.62 | ||||
| HIV-negative | 83.3 | 84.3 | 82.4 | ||||
| HIV-positive | 16.7 | 15.7 | 17.6 | ||||
(Mean, SD): Control (45.39, 9.93), Intervention (46.41, 9.33), Total (45.90, 9.64)
After testing of men who self-reported as non-positive at Baseline
Table 2 presents descriptive information about sexual behavior during the past 3 months assessed at baseline. Overall, among the 71.1% of participants who reported sex with a male during the past 3 months, the mean number of male partners during that period was 3.51 (SD=6.03); among the 87.4% who reported having sex with a female during the past 3 months the mean number of female partners was 3.59 (SD=3.93); and among the 23.4% who reporting having sex with a transgender female partner during the past 3 months the mean number of transgender female partners was 1.88 (SD=1.80). There were no differences between intervention and control groups on these baseline sexual behaviors as indicated by the chi-square and t-test results. Given the limited number of participants engaging in sex with transgender female partners, we decided not to pursue further analysis of sexual behavior with those partners as a separate category.
Table 2.
Baseline: Sexual Behavior in the Past 3 Months
| Behavior | Statistic | Total (N=396) |
Control (n=197) |
Intervention (n=199) |
Control vs.Intervention | |||
|---|---|---|---|---|---|---|---|---|
| χ2 | t | df | p-value | |||||
| Sex with a man | % | 71.1 | 71.1 | 71.2 | 0.001 | 1 | 0.97 | |
| Male sex partners | Mean (SD) | 3.51 (6.03) | 3.33 (5.06) | 3.68 (6.87) | −0.49 | 279 | 0.63 | |
| Sex with a woman | % | 87.4 | 87.3 | 87.4 | 0.001 | 1 | 0.97 | |
| Female sex partners | Mean (SD) | 3.59 (3.93) | 3.67 (3.25) | 3.52 (4.51) | 0.36 | 344 | 0.72 | |
| Sex with a man and sex with a woman | % | 63.5 | 62.4 | 64.6 | 0.21 | 1 | 0.65 | |
| Male sex partners | Mean (SD) | 3.56 (6.28) | 3.33 (5.30) | 3.77 (7.11) | −0.55 | 249 | 0.58 | |
| Female sex partners | Mean (SD) | 3.87 (4.25) | 4.03 (3.36) | 3.71 (4.97) | 0.60 | 249 | 0.55 | |
| Sex with a transwoman | % | 23.4 | 21.0 | 25.8 | 1.23 | 1 | 0.27 | |
| Transwoman sex partners | Mean (SD) | 1.88 (1.80) | 1.85 (1.68) | 1.90 (1.91) | −0.13 | 90 | 0.90 | |
Note: Calculation of mean number of partners is restricted to the subsample of participants who engaged in sex with that partner gender.
Table 3 presents the mean number of condomless sex events with female and male partners by partner type (any partner, main partner, casual partner) by condition at baseline, 6-, and 9-month assessment. We found no significant condition by time interaction effects on condomless sex events with female partners, male partners or all (including transgender female) partners combined. This was true regardless of partner type (all such partners, primary partners only, or casual partners only). Consequently, the data were re-analyzed with the interaction term deleted. Table 4 presents the comparisons by condition and by time (6-months vs. baseline, 9-months vs. baseline, 9-months vs. 6-months) for condomless sex events. We found significant reductions in condomless sex events with casual female partners from baseline to 6-months (b=−0.589, SE=0.070, p<.001) and from baseline to 9-months (b=−0.733, SE=0.068, p<.001), as well as a significant reduction from 6-months to 9-months (b=−0.145, SE=0.057, p=.01). No significant changes over time in sexual risk behavior were observed with main female partners. Similarly, we found significant reductions in condomless sex events with casual male partners from baseline to 6-months (b=−0.380, SE=0.054, p<.001) and from baseline to 9-months (b=−0.383, SE=0.049, p<.001), but no significant reductions from 6 months to 9 months. Again, no significant change over time was observed with main male partners. No effects for condition (intervention vs. control) were found on any sexual behavior outcome.
Table 3.
Mean Number of Condomless Intercourse Events by Condition and Time
| Partner Type | Condition | Baseline | Time 6-months |
9-months | Total |
|---|---|---|---|---|---|
| (N=396) | (n=310) | (n=319) | |||
| Any Female | Control (n=197) | 11.27 | 7.09 | 7.46 | 8.84 |
| Intervention (n=199) | 10.66 | 8.52 | 6.79 | 8.78 | |
| Total | 10.96 | 7.82 | 7.11 | ||
| Female Main | Control (n=197) | 4.48 | 4.78 | 5.74 | 4.95 |
| Intervention (n=199) | 5.31 | 5.82 | 5.54 | 5.54 | |
| Total | 4.89 | 5.31 | 5.63 | ||
| Female Casual | Control (n=197) | 6.70 | 2.36 | 1.71 | 3.87 |
| Intervention (n=199) | 5.38 | 2.79 | 1.25 | 3.28 | |
| Total | 6.04 | 2.58 | 1.47 | ||
| Any Male | Control (n=197) | 2.61 | 1.32 | 0.92 | 1.70 |
| Intervention (n=199) | 4.07 | 2.62 | 1.45 | 2.79 | |
| Total | 3.34 | 1.99 | 1.20 | ||
| Male Main | Control (n=197) | 0.23 | 0.63 | 0.19 | 0.34 |
| Intervention (n=199) | 1.24 | 1.00 | 0.93 | 1.07 | |
| Total | 0.73 | 0.82 | 0.57 | ||
| Male Casual | Control (n=197) | 2.37 | 0.69 | 0.73 | 1.37 |
| Intervention (n=199) | 2.85 | 1.64 | 0.48 | 1.73 | |
| Total | 2.61 | 1.18 | 0.60 | ||
| Any Partner* | Control (n=197) | 14.73 | 8.58 | 8.66 | 11.00 |
| Intervention (n=199) | 17.02 | 11.54 | 8.77 | 12.74 | |
| Total | 15.88 | 10.09 | 8.72 | ||
| Any Main* | Control (n=197) | 4.78 | 5.48 | 5.93 | 5.34 |
| Intervention (n=199) | 7.81 | 7.00 | 6.87 | 7.27 | |
| Total | 6.29 | 6.26 | 6.41 | ||
| Any Casual* | Control (n=197) | 9.77 | 3.16 | 2.70 | 5.62 |
| Intervention (n=199) | 9.22 | 4.78 | 1.92 | 5.56 | |
| Total | 9.50 | 3.99 | 2.30 |
Includes men, women, and transwomen
Table 4.
Condition and Time Effects on Condomless Intercourse Events
| Partner Type | Effect | Comparison | Coefficient | Robust SE | p-value |
|---|---|---|---|---|---|
| Any Female | Condition | Intervention vs. Control | −0.063 | 0.112 | 0.575 |
| Time | 6-months vs. Baseline | −0.493 | 0.080 | <0.001 | |
| 9-months vs. Baseline | −0.571 | 0.080 | <0.001 | ||
| 9-months vs. 6-months | −0.077 | 0.077 | 0.314 | ||
| Female Main | Condition | Intervention vs. Control | 0.050 | 0.096 | 0.605 |
| Time | 6-months vs. Baseline | 0.008 | 0.077 | 0.917 | |
| 9-months vs. Baseline | 0.049 | 0.080 | 0.542 | ||
| 9-months vs. 6-months | 0.041 | 0.075 | 0.584 | ||
| Female Casual | Condition | Intervention vs. Control | −0.064 | 0.075 | 0.393 |
| Time | 6-months vs. Baseline | −0.589 | 0.070 | <0.001 | |
| 9-months vs. Baseline | −0.733 | 0.068 | <0.001 | ||
| 9-months vs. 6-months | −0.145 | 0.057 | 0.012 | ||
| Any Male | Condition | Intervention vs. Control | 0.024 | 0.066 | 0.713 |
| Time | 6-months vs. Baseline | −0.391 | 0.058 | <0.001 | |
| 9-months vs. Baseline | −0.379 | 0.053 | <0.001 | ||
| 9-months vs. 6-months | 0.012 | 0.040 | 0.757 | ||
| Male Main | Condition | Intervention vs. Control | 0.057 | 0.036 | 0.113 |
| Time | 6-months vs. Baseline | −0.027 | 0.034 | 0.430 | |
| 9-months vs. Baseline | −0.026 | 0.030 | 0.385 | ||
| 9-months vs. 6-months | <0.001 | 0.029 | 0.990 | ||
| Male Casual | Condition | Intervention vs. Control | −0.003 | 0.052 | 0.959 |
| Time | 6-months vs. Baseline | −0.380 | 0.054 | <0.001 | |
| 9-months vs. Baseline | −0.383 | 0.049 | <0.001 | ||
| 9-months vs. 6-months | −0.002 | 0.040 | 0.953 | ||
| Any Partner* | Condition | Intervention vs. Control | 0.013 | 0.115 | 0.912 |
| Time | 6-months vs. Baseline | −0.675 | 0.085 | <0.001 | |
| 9-months vs. Baseline | −0.717 | 0.085 | <0.001 | ||
| 9-months vs. 6-months | −0.042 | 0.082 | 0.608 | ||
| Any Main* | Condition | Intervention vs. Control | 0.139 | 0.102 | 0.172 |
| Time | 6-months vs. Baseline | −0.023 | 0.084 | 0.786 | |
| 9-months vs. Baseline | 0.030 | 0.085 | 0.725 | ||
| 9-months vs. 6-months | 0.053 | 0.080 | 0.509 | ||
| Any Casual* | Condition | Intervention vs. Control | −0.048 | 0.088 | 0.585 |
| Time | 6-months vs. Baseline | −0.744 | 0.078 | <0.001 | |
| 9-months vs. Baseline | −0.893 | 0.075 | <0.001 | ||
| 9-months vs. 6-months | −0.149 | 0.066 | 0.024 |
Note: Data are from mixed effects linear regression models regressing each log-transformed outcome on fixed effects for Condition and Time while allowing for random intercepts and random slopes for Time assuming an unstructured covariance matrix. Robust variance estimates were computed.
Includes men, women, and transwomen
Discussion
The Bruthas Project used a community-based participatory research (CBPR) approach to design and implement a culturally sensitive HIV prevention outreach and counseling program to reach African American MSMW who do not identify as gay/homosexual or bisexual (Minkler, 2005). Building on a longstanding partnership between university-based researchers and community-based HIV prevention providers, the study team also relied on a Community Advisory Board that was primarily made up of members of the target population as well as service providers. CBPR therefore informed the content of the intervention as well as the way the trial was fielded in conjunction with culturally sensitive HIV testing and counseling (Cornwell et al., 2016). The supplemental 4-session Bruthas program was designed to build on HIV testing and counseling and by offering culturally tailored counseling about HIV/STI transmission, condom use, relationships and sexual communication, and assessing personal risk in the first counseling session, followed by additional sessions to motivate participants to consider interpersonal dynamics with female and male partners and situational triggers of condomless sex (Arnold et al., 2015; Operario, Smith, Arnold, & Kegeles, 2010). Regardless of condition, all participants reported significant reductions in condomless sex with casual male and female partners, and effects were sustained over 9 months of observation. We did not find differences in primary outcomes between participants in the supplemental 4-session program compared with those who received the culturally tailored counseling and testing intake session alone.
Findings suggest that even a culturally tailored HIV testing and counseling session for those reporting unknown or negative status delivered by trained peer educators, as participants in our control condition received, can contribute to reductions in HIV risk behavior with African American MSMW. Although HIV testing and counseling has been associated with reduced sexual risk behavior in prior studies (Maulsby et al., 2013), we had not anticipated the significant impact it would have on this population. This effect can be interpreted in light of the unmet HIV prevention needs of this population. The Bruthas Project was the first known HIV prevention effort delivered in the target geographic area that focused on the specific needs of African American MSMW, and our study reached a socially and economically marginalized cohort of men who had not previously accessed HIV-related services. Indeed, our formative work demonstrated that this population avoided HIV prevention services because they were provided by gay-identified agencies. Strong behavioral risk reductions observed in the control condition may be due in part to the high need for prevention services coupled with the historical absence of culturally sensitive programs, including HIV testing and counseling programs, for this population, thereby rendering a single counseling and testing session highly potent. Use of non-judgmental motivational counseling delivered by trained and culturally sensitive African American male counselors may have potentiated the effects of the single-session condition. Indeed, previous research has found that single-session or other brief interventions can be effective in reducing health risk behaviors, for example in the use of motivational interviewing techniques for reducing alcohol and substance use (Carrico, Zepf, Meanley, Batchelder, & Stall, 2016).
Contrary to our expectations, the supplemental 4-session intervention did not contribute to greater reductions in condomless sex compared to the culturally tailored testing and counseling-based control. This might be due in part to floor effects. In both intervention and control groups, the number of condomless sex events in the past 3 months with casual female partners reduced from 6 events at baseline to 1.5 events at 9-month follow-up; with casual male partners, the number of condomless sex events reduced from 2.6 events at baseline to less than 1 event at 9-month follow-up. Reductions in behavioral risk events beyond these low levels may be difficult to achieve.
There are several limitations to this study. Because the study design involved a highly active control group, a choice we made within the framework of using CBPR to field the randomized controlled trial, we are unable to compare behavior changes in the single-session counseling and testing control or supplemental 4-session Bruthas intervention conditions compared with a non-active control (e.g., no-treatment or delayed control or alternative control in which intervention style/content was irrelevant to the primary outcome). This allowed us to conduct the study in an ethical manner that was responsive to the needs of the community, but may have undermined our ability to detect differences due to the 4 session intervention alone. We did not include biological assessments of HIV or STI at 6- or 9-month follow-up, and findings rely on self-report. Assessments did not include measures that might have better captured secondary outcomes related to the supplemental 4-session intervention content such as relationship dynamics and communication, as well as awareness of situational triggers of condomless sex. Mediators of the intervention effect on primary outcomes have not yet been examined, and future analyses are pending. Finally, it is unclear why effects were obtained only with casual partners and not with main partners, although previous research has documented challenges in changing sexual behaviors within the context of a committed primary partnership, indicating the need for couple-based interventions with this population (Burton, Darbes, & Operario, 2010; Hoff, Beougher, Chakravarty, Darbes, & Neilands, 2010).
Conclusion
In conclusion, this evaluation of the Bruthas Project provides evidence to suggest the importance of motivational counseling delivered in a culturally competent and non-judgmental manner on reducing HIV risk with African American MSMW. Principles of the Bruthas Project can be applied to other relevant domains within HIV intervention research - for example, in the development of counseling programs to promote linkage to and engagement in care and medication adherence among African American MSM or MSMW living with HIV, or in programs to promote pre-exposure prophylaxis among African American MSMW, or further prevention efforts addressing co-morbidities of HIV risk, substance use and mental health among African American MSMW. Given the effects in the single-session counseling condition, brief interventions may be especially worth considering.
Finally, the design, implementation, and evaluation of the Bruthas Project intervention benefitted from following principles of CBPR, (Minkler, 2005) in which university-based researchers collaborated in non-hierarchical partnership with community-based service providers. Given the highly stigmatized experiences and hard-to-reach nature of the population, efforts to reduce HIV risk or promote HIV care or medication adherence with African American MSMW should consider efforts to maximize community buy-in and participation at all stages of program design and delivery.
Acknowledgments
EA conceived the study, oversaw data collection and analyses, and drafted and revised the paper. SK helped design the intervention, helped supervise the trial, and revised the paper, LP and TN supervised quantitative data collection, conducted analyses, and drafted and revised the paper, JW and WS collected the data, and revised the paper. MB provided the intervention, and revised the draft paper, SC, GL, and CDS helped supervise the trial, and revised the draft paper. DO helped design the study, helped supervise the trial, and drafted and revised the paper. All authors read and approved the final manuscript. We would like to thank our study participants, and Raysean Ford, Michael Arnold, Elizabeth Bartmess, and Stuart Gaffney for their contributions to this study.
Funding. Funding was received from the National Institutes of Health to conduct this study, NIH/NIMH R01 MH090899 (PI: Arnold); NIH/NCRR CTSI UTLITR00004. The funders had no role in the design, execution or decision to publish this research.
Footnotes
Disclosure of potential conflicts of interest. The authors declare that they have no conflicts of interest.
Ethical approval. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was reviewed and approved by the University of California San Francisco Committee on Human Research.
Informed consent. Written informed consent was obtained from all individual participants included in the study.
References
- Arnold EA, Operario D, Cornwell S, Benjamin M, Smith CD, Lockett G, et al. (2015). The Development of a Counseling-Based HIV Prevention Intervention for African American Men Who Have Sex With Men and Women: The Bruthas Project. AIDS education and prevention 27(6), 505–521. doi: 10.1521/aeap.2015.27.6.505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham T, Harawa N, & Williams J (2013) Gender role conflict among African America men who have sex with men and women: Associations with mental health and sexual risk and disclosure behaviors. Am J Public Health 103: 127–133. doi: 10.2105/AJPH.2012.300855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton J, Darbes LA, & Operario D (2010). Couples-focused behavioral interventions for prevention of HIV: systematic review of the state of evidence. AIDS and Behavior, 14(1), 1–10. doi: 10.1007/s10461-008-9471-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico AW, Zepf R, Meanley S, Batchelder A, & Stall R (2016). Critical Review: When the Party is Over: A Systematic Review of Behavioral Interventions for Substance-Using Men Who Have Sex with Men. Journal of Acquired Immune Deficiency Syndromes, 73(3), 299–306. doi: 10.1097/QAI.0000000000001102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). HIV and African Americans: HIV Diagnoses in 2016: CDC HIV/AIDS Fact Sheet. [Google Scholar]
- Centers for Disease Control and Prevention. (2016). HIV Among African American Gay and Bisexual Men. Atlanta: HIV/AIDS Surveilance Unit. [Google Scholar]
- Cornwell S, Operario D, Benjamin M, Stewart WR, Weeks J, Lockett G, Kegeles SM, Arnold EA (2016). Using Community-based Participatory Research (CBPR) to carry out a randomized controlled trial of a home grown HIV prevention intervention in an urban setting. Society for Prevention Research Annual Meeting, San Francisco, [Google Scholar]
- Dyer TP, Regan R, Wilton L, Harawa N, Ou SS, Wang L, Shoptaw S (2013). Differences in substance use, psychosocial characteristics and HIV-related risk behavior between black men who have sex with men only (BMSMO) and black men who have sex with men and women (BMSMW) in six US cities. J of Urban Health 90(60): 1181–1193. doi: 10.1007/s11524-013-9811-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, & Fisher WA (1996). The information-motivation-behavioral skills model of AIDS risk behavior and change: Empirical support and application In Oskamp S & C Thompson S (Eds.), Understanding and Preventing HIV Risk Behavior (pp. 100–127). Thousand Oaks, CA: Sage. [Google Scholar]
- Friedman MR, Stall R, Silvestre AJ, Mustanski B, Shoptaw S, Surkan P, Rinaldo CR, & Plankey MW (2014a). Stuck in the middle: Longitudinal HIV-related health disparities among men who have sex with men and women. J Acquir Immune Defic Syndr. 66(2): 213–220. doi: 10.1097/QAI.0000000000000143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MR, Wei C, Klem ML, Silvestre AJ, Markovic N, et al. (2014b). HIV Infection and Sexual Risk among Men Who Have Sex with Men and Women (MSMW): A Systematic Review and Meta-Analysis. PLoS ONE 9(1): e87139. doi: 10.1371/journal.pone.0087139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harawa NT, Williams JK, McCuller WJ, Ramamurthi HC, Lee M, Shapiro MF, Norris KC, & Cunningham WE (2013). Efficacy of a culturally congruent HIV-risk reduction intervention for behaviorally bisexual black men: Results of a Randomized Trial. AIDS, 27(12), 1979–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff CC, Beougher SC, Chakravarty D, Darbes LA, & Neilands TB (2010). Relationship characteristics and motivations behind agreements among gay male couples: differences by agreement type and couple serostatus.. AIDS Care, 22(7), 827–835. doi: 10.1080/09540120903443384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones KT, Gray P, Whiteside YO, Wang T, Bost D, Dunbar E, et al. (2008). Evaluation of an HIV prevention intervention adapted for Black men who have sex with men. Am J Public Health, 98(6), 1043–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaPollo AB, Bond L, & Lauby JL (2014). Hypermasclinity and sexual risk among black and white men who have sex with men and women. American J of Men's Health, 8(5): 362–372. doi: 10.1177/1557988313512861 [DOI] [PubMed] [Google Scholar]
- Latkin C Yang C, Tobin K, Penniman T, Patterson J, & Spikes P (2011). Differences in the social networks of African American men who have sex with men only and those who have sex with men and women. Am J Public Health. 2011;101:e18–e23. doi: 10.2105/AJPH.2011.300281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauby JL, Millett GA, LaPollo AB, Bond L, Murrill CS, & Marks G (2008). Sexual risk behaviors of HIV-positive, HIV-negative, and serostatus-unknown Black men who have sex with men and women. Arch Sex Behav, 37(5), 708–719. [DOI] [PubMed] [Google Scholar]
- Lauby JL, Milnamow M, Joseph HA, Hitchcock S, Carson L, Pan Y, Mendoza M, Millett G (2018). Evaluation of Project Rise, an HIV prevention intervention for black bisexual men using an ecosystems approach. AIDS and Behav 22(1): 164–177. doi: 10.1007/s10461-017-1892-5 [DOI] [PubMed] [Google Scholar]
- Malebranche DJ (2008). Bisexually active Black men in the United States and HIV: Acknowledging more than the "Down Low". Arch Sex Behav, 37(5), 810–816. doi: 10.1007/s10508-008-9364-7 [DOI] [PubMed] [Google Scholar]
- Malebranche DJ, Arriola KJ, Jenkins TR, Dauria E, & Patel SN (2010). Exploring the "bisexual bridge": a qualitative study of risk behavior and disclosure of same-sex behavior among black bisexual men. Am J Public Health, 100(1), 159–164. doi: 10.2105/AJPH.2008.158725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulsby C, Millett G, Lindsey K, Kelly R, Johnson D, Holtgrave D (2013). A systematic review of HIV interventions for black men who have sex with men. BMC Public Health 13: 625. doi: 1186/1471-2458-13-625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M (2005). Community-based research partnerships: challenges and opportunities. J of urban health 82(2 Suppl 2), ii3–12. doi: 10.1093/jurban/jti034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Smith CD, Arnold E, & Kegeles S (2010). The Bruthas Project: evaluation of a community-based HIV prevention intervention for African American men who have sex with men and women. AIDS Educ Prev, 22(1), 37–48. doi: 10.1521/aeap.2010.22.1.37 [DOI] [PubMed] [Google Scholar]
- Operario D, Smith CD, & Kegeles S (2008). Social and psychological context for HIV risk in non-gay-identified African American men who have sex with men. AIDS Educ Prev, 20(4), 347–359. [DOI] [PubMed] [Google Scholar]
- Singh S, Hu X, Wheeler W, Hall IH (2014). HIV diagnoses among men who have sex with men and women-United States and 6 dependent areas, 2008-2011. Am J Public Health, 104(9): 1700–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilton L, Herbst JH, Coury-Doniger P, Painter TM, English G, Alvarez ME, et al. (2009). Efficacy of an HIV/STI prevention intervention for black men who have sex with men: findings from the Many Men, Many Voices (3MV) project. AIDS Behav, 13(3), 532–544. [DOI] [PubMed] [Google Scholar]