Abstract
Objective:
The authors sought to clarify the etiology of the association between pregnancy and Alcohol Use Disorder (AUD).
Method:
The authors utilized longitudinal, population-wide Swedish medical, pharmacy, and criminal registries to evaluate whether rates of AUD are lower during pregnancy. They compared pregnant women born 1975–1992 (N=322,029) to matched population controls, to female relatives discordant for pregnancy, and to within-individual pre- and post-pregnancy periods. They further compared AUD rates between pregnant women and their partners.
Results:
Pregnancy was inversely associated with AUD across all analyses (odds ratio=0.17– 0.32). In co-relative analyses, the strength of the association increased among more closely related individuals. Within individuals, AUD rates were substantially decreased during pregnancy relative to the pre-pregnancy period (odds ratio=0.25–0.26), and remained reduced during post-partum periods (odds ratio=0.23–0.31). Results were similar for second pregnancies (odds ratio=0.23). The partners of pregnant women also exhibited reductions in AUD (odds ratio=0.45). Among women who became pregnant at earlier ages and those with a history of criminal behavior, the pregnancy-AUD association was especially pronounced (interaction p<0.01), but no moderation was observed for a personal or maternal parental AUD history.
Conclusions:
Findings suggest that pregnancy plays a critical, and likely causal, motivational role in reducing AUD risk among women and, to a lesser extent, their partners. These results extend the understanding of the relationship between pregnancy and alcohol use, demonstrating that even severe outcomes such as AUD are subject to the protective effects of pregnancy.
Keywords: alcohol use disorder, co-relative design, post-partum, pregnancy
Introduction
Alcohol consumption during pregnancy increases risk for miscarriage, stillbirth, and a variety of physical and neurodevelopmental effects collectively known as fetal alcohol spectrum disorders (1), and the World Health Organization notes that “there is no safe level of alcohol use during pregnancy” (2). The World Health Organization and National Institute on Alcohol Abuse and Alcoholism have developed guidance for prevention or reduction of alcohol consumption during pregnancy to reduce alcohol-related harms due to prenatal exposure. However, while discouraged by much of the medical community and socially stigmatized in some environments, alcohol use during pregnancy persists.
In the US, nearly 10% of pregnant women aged 15–44 reported alcohol use, with over 2% reporting binge drinking; alcohol use is more common earlier in the pregnancy, and less common than among non-pregnant women (3). Attitudes toward alcohol consumption during pregnancy vary widely across Europe: 28.5% of UK women reported drinking during pregnancy, while Swedish women more closely resembled American women, with 7.2% continuing to drink (4). Some evidence suggests that drinking during pregnancy is underreported (5).
Though a non-trivial proportion of pregnant women continue to drink, the majority abstain, suggesting that pregnancy serves as a strong incentive. During the US Great Recession of 2008–2009, when binge drinking prevalence increased overall in the US, pregnancy was one of the strongest predictors of decreased likelihood of bingeing (6). Even as past 30-day alcohol consumption and binge drinking have increased among non-pregnant US women, the same behaviors have decreased among pregnant women (7). As noted in the context of prenatal illicit substance use (8), women who misuse substances may be more likely to have an unplanned pregnancy (9, 10), which would result in a positive association between pregnancy and alcohol misuse. However, the drive to protect one’s offspring from the adverse effects of alcohol is likely a counteracting factor, resulting in a negative association between pregnancy and alcohol misuse.
Drinking during pregnancy is associated with a variety of maternal characteristics. Swedish women with lower educational attainment, and those who lived in smaller cities, were more likely to abstain during pregnancy (4, 11). Those who smoked (4) or exhibited heavier or more frequent drinking prior to pregnancy (11–13) reduced their drinking during pregnancy to a lesser degree than non-smokers or light drinkers, respectively. Cognitive factors are also relevant: Women who report drinking to enhance social interactions prior to pregnancy, and those who perceived that small amounts of alcohol were not problematic, were less likely to abstain (13). In contrast, women who received a pamphlet detailing the negative effects of alcohol during pregnancy were more likely to reduce their drinking than those who received standard care (14).
Importantly, alcohol consumption is distinct from, though correlated with, alcohol use disorder (AUD): Light or moderate, but non-dependent, drinkers may abstain during pregnancy without undue effort. In contrast, problem drinking frequently involves motivational and volitional components, potentially due to neurobiological adaptations that reduce cognitive control over substance use (15, 16). Indeed, the diagnostic criteria for AUD include an inability to stop or reduce drinking despite one’s intentions, and drinking for longer or in greater quantities than intended (17). Thus, pregnancy may not be a sufficient incentive for women with AUD to cease drinking. However, contingency management for AUD – though less common than for other substance use disorders (18) – has demonstrated some success at increasing alcohol abstinence rates relative to standard care (19–21), suggesting that volitional capacity can be improved by extrinsic factors. Pregnancy is a qualitatively different motivator than the monetary incentives typically used in such programs: Rather than implicitly relying on immediate positive outcomes of monetary value to oneself, pregnancy-based motivation would rely on avoidance of distal negative outcomes for one’s offspring. This difference may mitigate the effectiveness of the “reward” (22), and may be particularly relevant to AUD given its association with impulsivity and delay discounting (23–26).
Where pregnancy and alcohol misuse are negatively associated, it remains unclear whether this is due to a causal process or to other factors contributing to the coincidence of pregnancy and decreased alcohol misuse. In the current study, we investigate the potential causal association between pregnancy and AUD using Swedish national registries. Though observational data preclude definitive conclusions about causality, we apply a range of analytic methods, in a statistically powerful sample, to clarify the nature of this association. First, we examine rates of AUD in pregnant women relative to matched population-based controls. Second, given the prominent genetic influences on risk for AUD (27), we employ co-relative designs that enable us to control for a degree of genetic liability while examining AUD rates in female relative pairs wherein one member is pregnant and the other is not (i.e., discordant pairs). Third, we capitalize on the longitudinal nature of the registries to apply within-individual designs, comparing rates of AUD registrations during pregnancy to non-pregnant time frames. Finally, we compare rates of AUD in spouses before and during the pregnancy. We thereby extend prior studies focused on alcohol consumption to address whether pregnancy may play a direct role in reduced incidence of AUD.
Methods
Identification of Alcohol Use Disorder.
We utilized several different Swedish population- based registers with national coverage, linking them using each person’s unique identification number. To preserve confidentiality, this was replaced by a serial number. We secured ethical approval for this study from the Regional Ethical Review Board of Lund University (No. 2008/409). AUD was defined by: 1) ICD codes for main and secondary diagnoses (see Supplementary Material for ICD codes) from Swedish medical registers; or 2) registrations of individuals in the Swedish Crime Register. Each individual could have several registrations in the criminal and/or in the medical registers. To avoid double-counting registrations, within each type of register (Criminal and Medical), we allowed for a 90-day period after each registration in which a new registration was not counted.
Sample.
To study the association between pregnancy and AUD, we selected all females born in Sweden 1975–1992 who had at least one child registered in the Swedish multigenerational register where the mother was likely first aware of being pregnant between the ages of 18 and 35. As in a prior study (8), we estimated women were aware of being pregnant 242 days before birth.
Statistical Analyses.
We matched each mother to 5 non-related control women with the same year and month of birth. Furthermore, the control individual had to be alive and registered in Sweden at the time of the case’s pregnancy and not themselves registered as being a mother or having a child within 9 months after the date of birth of the case’s child. For all control individuals we studied AUD during the same period as the case individual (Ncases=322,029 and Ncontrols=1,610,145). We next replicated the matching approach but instead of using non-related random individuals as controls, we matched on female cousins and full-siblings. We allowed for up to three years’ age difference between the case and the relative control. We matched 120,938 control cousins to 104,550 cases and 41,567 control siblings to 40,045 cases. By matching on cousins and siblings, we account for unmeasured genetic and environmental factors shared among cousins and siblings. Finally, we studied AUD using a within-individual model comparing a 242-day period prior to the pregnancy to the pregnancy period.
We used conditional logistic regression, with a separate stratum for each case and their control(s), in which we compare AUD in the case (i.e., AUD during pregnancy) with AUD in the controls (i.e., AUD during a non-pregnant period). Model 1 was only a crude model, whereas in model 2 we adjusted for average parental educational [(1) <=9 years, (2) 10–11 years, (3) 12 years or more] and school achievement of the individual (see (28) for how school achievement was defined). Odds ratios between 0 and 1 would indicate reduced risk for AUD during pregnancy (i.e., a protective effect of pregnancy), while odds ratios >1 would indicate increased risk.
We then combined the population, full-sibling, and cousin datasets, and performed two co-relative analyses. The first allowed all coefficients for each sample to be independent. In the second we modeled the genetic resemblance assuming that it equaled: 0 for the population, +0.125 for cousins and +0.5 for full-siblings. We compared this model with the previous model. Using Akaike’s Information Criterion, a model fit statistic that balances goodness of fit and parsimony. If the second model fitted the data well, we obtained improved estimation of the AUD-pregnancy association among all types of relatives. In this model we are also able to extrapolate an OR for monozygotic twins (there were 0 monozygotic twins registered for AUD while pregnant).
In additional analyses, we investigated if the association between pregnancy and AUD was moderated by the following variables; the average educational status across the individual’s parents; school achievement of the individual; lifetime registration of AUD in the mother’s parent (dichotomized into yes/no); AUD registration in the individual prior to pregnancy; criminal registration in the individual prior to pregnancy (for a definition of Criminal registration see Kendler, Larsson Lonn (29)); drug abuse registration in the individual prior to pregnancy (for a definition of drug abuse see Kendler, Ohlsson (8)); psychiatric registration in the individual prior to pregnancy; age at pregnancy (dichotomized into <=25 years and >25 years); marital status (dichotomized into married/not married; in the analyses of married people, individuals that got married during the control or hazard period were excluded); AUD registration in the father to the child prior to pregnancy; AUD registration in the father to the child during pregnancy. These moderation analyses were performed only on the within-individual sample using an interaction term (using the logit link) between the covariate of interest and mother’s AUD status. In the within-individual sample, we also tested if the decrease in AUD rates between control and pregnancy periods was the same for mothers and fathers. This was done by including an interaction term between a dummy variable indicating mother/father, and AUD status in mother and father.
Finally, we examined, using within-individual analyses only, the rates of AUD in post- partum periods. Our control was the 242-day period prior to pregnancy and we examined three 242-day post-partum risk periods: 0–242, 243–484 and 485–726 days after childbirth. We eliminated from these analyses mothers where the child died during the risk period. We included mothers no longer cohabiting with their child (n=1,088, 3,604, and 4,898 during these three periods) because these mothers had substantial elevations in AUD rates, suggesting that in some cases the child had been removed due to their problematic behavior. Excluding them would bias downward the post-partum AUD rates.
In all these models the within-individual and within-family clustering were taken into consideration. In models that included information on fathers, the father had to cohabit with the mother at the end of the year the child was born. All statistical analyses were performed using SAS 9.3.
Results
Association between pregnancy and AUD registration.
Rates of AUD among pregnant women were considerably lower than among matched controls (odds ratio=0.32 [95% confidence interval=0.27–0.37]; Table 1). This association became stronger (that is, the OR was closer to 0) after controlling for mean parental education and school achievement. These findings corresponded quite closely to the negative association between pregnancy and AUD among cousins discordant for pregnancy (odds ratio=0.31 [0.23–0.42]); similarly, accounting for potential confounders strengthened the observed association. When comparing AUD rates within pregnant women and their discordant biological full sisters, the negative association was even more pronounced (odds ratio=0.22 [0.13–0.36]).
Table 1.
The Observed Association of First Pregnancy with Registration for AUD in the General Population, in Cousin and Sibling Pairs Discordant for Pregnancy and Within-Individuals
| N | Frequency of AUD Registration |
Odds Ratio (95% Confidence Intervals) |
Cohen’s d# (95% Confidence Intervals) |
|||
|---|---|---|---|---|---|---|
| Pregnancy | Control | Model 1* | Model 2** | Model 1* | ||
| Population | 322,029 | 0.05% (N=155) |
0.15% (N=2,452) |
0.32 (0.27; 0.37) |
0.26 (0.22; 0.31) |
0.63 (0.55; 0.72) |
| Cousins | 112,457 | 0.05% (N = 55) |
0.15% (N= 199) |
0.31 (0.23; 0.42) |
0.21 (0.15; 0.30) |
0.65 (0.48; 0.81) |
| Siblings | 40,005 | 0.04% (N = 17) |
0.20% (N = 82) |
0.22 (0.13; 0.36) |
0.83 (0.56; 1.12) |
|
| Within Individual1 | 332,436 | 0.05% (N = 165) |
0.17% (N=559) |
0.25 (0.21; 0.30) |
0.76 (0.66; 0.86) |
|
| Within Individual (2)2 | 332,436 | 0.05% (N = 165) |
0.17% (N=553) |
0.26 (0.21; 0.31) |
0.74 (0.65; 0.86) |
|
| Within Individual (3)3 | 332,436 | 0.05% (N = 165) |
0.18% (N=587) |
0.25 (0.21; 0.30) |
0.76 (0.66; 0.86) |
|
| Within Individual (2nd
pregnancy)1 |
197,383 | 0.02% (N = 40) |
0.07 (N =130) |
0.23 (0.15; 0.35) |
0.81 (0.58; 1.05) |
|
Unadjusted
Adjusted for Mean Parental Education and School Achievement
Control period is the 242 days prior to the start of pregnancy
Control period ends 6 months prior to start of pregnancy
Control period ends 12 months prior to start of pregnancy
We used unadjusted results from the discordant cousin and sibling analyses to fit a co- relative model, extending to estimated odds ratios for discordant monozygotic twins. As shown in Table 2, the estimated odds ratios decline monotonically, from 0.32 to 0.17, as a function of relatedness. These findings are illustrated in the Figure. The fit of the predicted model is superior to that of the observed model as indicated by a lower Akaike’s Information Criterion (Table 2).
Table 2.
The Association between Pregnancy and AUD assessed by an Odds Ratios in the General Population and in Cousins, Siblings and Monozygotic Twins Discordant for Pregnancy as Estimated from our Co-Relative Model
| Sample | Estimated Odds Ratios |
|---|---|
| Population | 0.32 (0.28–0.37) |
| Discordant Cousins | 0.30 (0.26–0.34) |
| Discordant Siblings | 0.24 (0.16–0.35) |
| Discordant Monozygotic Twins | 0.17 (0.08–0.38) |
| Akaike’s Information Criterion (Observed) | 1431449.1 |
| Akaike’s Information Criterion (Predicted) | 1431448.0 |
Figure.
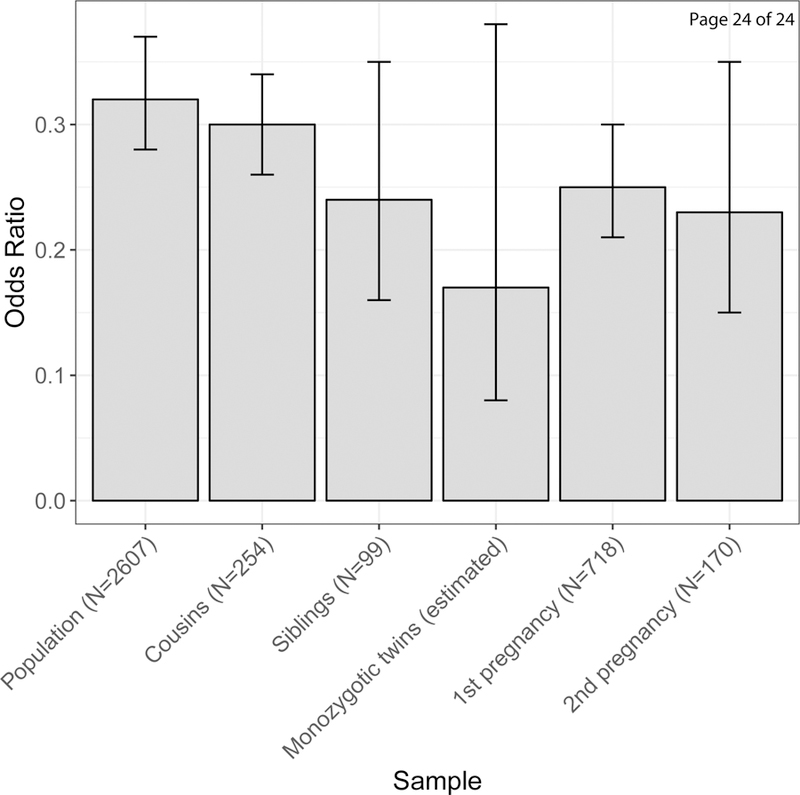
The Association between Pregnancy and Risk for Alcohol Use Disorder – as assessed by an Odds Ratio (± 95% Confidence Intervals) – in the general population, cousins, siblings and monozygotic twins discordant for pregnancy, and within-individuals (comparing matched periods before and during pregnancy) for a first and second pregnancy. The odds ratios are all from the predicted model and are estimated from models without covariates. Sample sizes are based on individuals with alcohol use disorder registrations within each group (see Table 1); for cousins and siblings, these are from discordant pairs.
We conducted a series of within-individual analyses, first using periods prior to pregnancy as our control. Regardless of the control time frame – the 242 days prior to the estimated beginning of the pregnancy, six months prior to start of pregnancy, or 12 months prior to start of pregnancy – the risk of AUD was consistently and substantially reduced during pregnancy (Table 1; odds ratios=0.25–0.26). We next tested whether rates of AUD were similar in the first and second half of a pregnancy, and found no significant difference (odds ratio=1.08 [0.78–1.49). We also examined whether the negative association was observed during a second pregnancy, with comparable results (Table 1; odds ratio=0.23 [0.15–0.35]). Finally, we examined the persistence of the observed negative association during a range of post-partum periods (Table 3). We found a gradual decrease in the protective effect of pregnancy across time, with the prevalence of AUD in the immediate post-partum period (0–242 days after childbirth) only half that in the 3rd period (485–726 days after childbirth). Even so, the confidence intervals for the odds ratios in the 3rd period remained far below one.
Table 3.
Within-Individual Analyses of Rates of Alcohol Use Disorder in the Pre-Pregnancy and Post- Partum Periods
| Risk Period | N | Prevalence of Alcohol Use Disorder during the Control or Risk Period |
Odds Ratio (95% Confidence Interval) |
|
|---|---|---|---|---|
| Control Period |
Risk Period |
|||
| 0–242 days after childbirth | 294,623 | 0.17% | 0.03% | 0.17 (0.13–0.21) |
| 243–484 days after childbirth | 273, 157 | 0.17% | 0.04% | 0.23 (0.19–0.29) |
| 485–726 days after childbirth | 250,855 | 0.17% | 0.06% | 0.31 (0.25–0.38) |
All control periods - 242 days prior to birth
Comparison to fathers.
We tested whether a similar association was observed among biological fathers, using the 287,292 cases where the father and mother were cohabitating at the end of the child’s year of birth. When examined together, the reduction in risk for an AUD registration from the control to the pregnancy period was more pronounced for the mother (odds ratio=0.18 [0.14–0.23) than for the father (odds ratio=0.45 [0.41–0.49]). This difference was also reflected in a model that treats mothers and fathers as independent: The reduction in risk in the control versus pregnancy period was stronger in the mother relative to the father (odds ratio=0.56 [0.47–0.68]).
Potentially moderating factors.
We considered a range of sociodemographic and psychopathological factors that may moderate the negative association between pregnancy and AUD (Table 4). We observed evidence of moderation (p<0.05) for only two factors: a criminal registration in the mother prior to pregnancy, and age at pregnancy (<25 or 25+). Specifically, the negative association between pregnancy and AUD was stronger among mothers with a criminal history relative to their counterparts without a criminal history; similarly, the negative association was more pronounced among younger mothers.
Table 4.
Potential Moderators of the Effect of Pregnancy of Risk for Alcohol Use Disorder
| Absent or Present |
Sample Sizes |
Rates of Alcohol Use Disorder |
Difference | Interaction p value |
Odds Ratio (95% Confidence intervals) |
||
|---|---|---|---|---|---|---|---|
| Pregnancy | Control | ||||||
| General Potential Moderators | |||||||
| Parental Education* | Low | 103,673 | 0.06% | 0.21% | 0.15% | 0.3085 | 0.27 (0.22; 0.34) |
| Mid | 173,238 | 0.05% | 0.17% | 0.39% | 0.23 (0.18; 0.29) | ||
| High | 18,163 | 0.03% | 0.09% | 0.06% | 0.19 (0.12; 0.32) | ||
| Alcohol Use Disorder in Parents of Mother |
No | 293,892 | 0.04% | 0.14% | 0.10% | 0.3293 | 0.24 (0.20; 0.29) |
| Yes | 38,544 | 0.13% | 0.40% | 0.27% | 0.28 (0.21; 0.37) | ||
| School Achievement (SD units)*** |
−2.5 – −1.5 | 20,803 | 0.13% | 0.49% | 0.36% | 0.9201 | 0.22 (0.18; 0.28) |
| −1.5 – −0.5 | 79,205 | 0.07% | 0.24% | 0.17% | 0.22 (0.19; 0.27) | ||
| −0.5 – 0.5 | 120,717 | 0.02% | 0.10% | 0.08% | 0.23 (0.18; 0.29) | ||
| 0.5 – 1.5 | 82,913 | 0.01% | 0.04% | 0.03% | 0.23 (0.16; 0.33) | ||
| 1.5 – 2.5 | 13,542 | 0.00% | 0.00% | 0.00% | 0.23 (0.14; 0.38) | ||
| Prior Alcohol Use Disorder (in Mother) |
No | 327,020 | 0.03% | 0.12% | 0.09% | 0.1492 | 0.23 (0.19; 0.28) |
| Yes | 5,416 | 1.14% | 2.82% | 1.68% | 0.30 (0.23; 0.40) | ||
| Prior Crime (in Mother) | No | 309,765 | 0.03% | 0.13% | 0.10% | 0.0086 | 0.22 (0.18; 0.26) |
| Yes | 22,671 | 0.29% | 0.73% | 0.44% | 0.33 (0.26; 0.43) | ||
| Prior Drug Abuse (in Mother) |
No | 325,836 | 0.03% | 0.12% | 0.09% | 0.1854 | 0.23 (0.19; 0.28) |
| Yes | 6,600 | 0.94% | 2.56% | 1.62% | 0.29 (0.22; 0.38) | ||
| Prior Psychiatric Diagnosis (in Mother) |
No | 328,769 | 0.05% | 0.16% | 0.09% | 0.5862 | 0.25 (0.21; 0.30) |
| Yes | 3,667 | 0.25% | 0.79% | 0.54% | 0.20 (0.09; 0.45) | ||
| Age at Pregnancy | −25 | 135,187 | 0.07% | 0.30% | 0.23% | 0.0009 | 0.21 (0.17; 0.26) |
| 25+ | 197,249 | 0.04% | 0.08% | 0.04% | 0.36 (0.28; 0.47) | ||
| Married** | No | 255,623 | 0.06% | 0.20% | 0.14% | 0.6781 | 0.25 (0.22 0.30) |
| Yes | 38,949 | 0.02% | 0.08% | 0.06% | 0.31 (0.13; 0.75) | ||
| Features of Cohabiting Biological Fathers Alcohol Use Disorder as Potential Moderators | |||||||
| Prior Alcohol Use Disorder in Father |
No | 274,26 6 |
0.02% | 0.09% | 0.07% | 0.2215 | 0.16 (0.12; 0.22) |
| Yes | 13,026 | 0.12% | 0.48% | 0.36% | 0.23 (0.14; 0.38) | ||
| Alcohol Use Disorder during Pregnancy in Fathers |
No | 286,88 6 |
0.02% | 0.11% | 0.09% | 0.8024 | 0.18 (0.14; 0.23) |
| Yes | 406 | 0.74% | 1.98% | 1.24% | 0.15 (0.05; 0.49) | ||
Parental education was used as a continuous term in the models, hence only one interaction term. The odds ratios in the far right column are an illustration of the odds ratios at different levels of parental education.
In the analyses of married people individuals that got married in the control or hazard period were excluded (for these individuals we could not separate if the effect is due to marriage or pregnancy)
School achievement was used as a continuous term in the models, hence only one interaction term. The odds ratios in the far right column are an illustration of the odds ratios at different levels of school achievement (−2, −1, 0, 1, 2).
Discussion
We used national registry data to examine the potential causal relationship between pregnancy and reduced risk for alcohol use disorder among Swedish women. We considered a variety of contextual perspectives: matching to population controls, comparison to female relatives discordant for pregnancy, within-individual control periods, and comparisons between mothers and fathers. We consistently observed markedly lower rates of AUD registrations during pregnancy, with the reduction in risk among mothers ranging from ~70–80% across analyses. Findings are suggestive of “inverse confounding” such that adjustment for potential sociodemographic or genetic confounders strengthened the observed association. These results are consistent with prior reports that women reduce their alcohol consumption during pregnancy (6, 30, 31). Importantly, we extend those findings to demonstrate that the observed association applies to a clinically relevant outcome, indicating that even among women at elevated genetic risk for or with a personal history of AUD, pregnancy can be a critical motivating factor for modifying alcohol misuse.
We first compared pregnant women to matched controls, and accounting for covariates, found that the odds of an AUD registration were reduced by 74% among pregnant women. When controlling for confounding factors by applying a co-relative design, pregnancy was even more strongly protective against risk for AUD, with the odds of AUD reduced by 83% in the pregnant member of a discordant monozygotic twin pair. While the unique nature of pregnancy precludes comparison to other circumstances in which changes to drinking are expected (e.g., contingency management programs), these reductions are objectively substantial. Importantly, previous studies have demonstrated that clear communication from clinicians, such as provision of a pamphlet or interpersonal discussions about the risks of prenatal alcohol use, may further reduce alcohol misuse beyond the effects of pregnancy alone (13, 14). Pregnancy may therefore present an important window of opportunity for intervention (32).
Longitudinal data and the temporally discrete nature of pregnancy enabled us to use women as their own controls, comparing AUD rates during pregnancy to periods preceding and succeeding pregnancy. This approach is not subject to potential confounders that may complicate observed associations between pregnancy and AUD. Given that many pregnancies are planned and women may modify their alcohol use in anticipation, we used a range of time frames as the reference; the quite stable results suggest that even if pregnancy is planned between 6 and 12 months in advance, the actual pregnancy still represents a period of substantial reduction in AUD risk. This relationship was borne out in the post-partum periods as well: In the period immediately succeeding pregnancy, the odds of AUD were identical to that predicted among discordant monozygotic twins. With the next two successive periods, odds increased but remained substantially lower than 1. Thus, the protective effect potentially conferred by pregnancy persists over time with only minor decreases in strength; additional analyses could clarify the extent to which risk stabilizes. Prior work indicates that parenthood itself is inversely associated with AUD risk (33, 34), thus long-term decreases in risk relative to pre-pregnancy are likely.
We evaluated potential moderation of the pregnancy-AUD association by a variety of factors. We found that AUD risk decreased during pregnancy more sharply among women with a history of criminal behavior. Similarly, women who became pregnant prior to age 25 exhibited a more pronounced reduction in AUD risk than those who became pregnant at a later age. These findings suggest that pregnancy may be an especially powerful motivator for healthful behavior among women who are otherwise at higher risk for AUD. Interestingly, we observed no interaction between pregnancy and personal history of AUD. Parental history of AUD, an indicator of genetic and environmental AUD risk, also did not moderate the pregnancy-AUD association. In conjunction with our co-relative analyses, this suggests that while genetic factors may inversely confound the observed association, the protective effect of pregnancy is robust even to the pronounced genetic component of AUD liability. Indeed, the paucity of moderating factors underscores the consistency of pregnancy’s motivational capacity.
Pregnancy is also associated with reduction in partner AUD, though to a lesser extent than among mothers. Again, this suggests that factors other than fetal alcohol exposure contribute to the observed association; a previous study found that changing social contexts and concern for the mother motivated decreased alcohol consumption among the partners of pregnant women (35). The discrepancy in risk reduction across mothers and fathers may be attributable to concerns about alcohol’s direct effect on the fetus: Brief interventions that educate pregnant women about alcohol’s teratogenic effects have been shown to decrease consumption (14, 36). Notably, partner AUD, prior to or during the pregnancy, did not moderate mothers’ AUD risk. A Dutch study of pregnant women found that women drank less if their partner more strongly disapproved of drinking during pregnancy and/or drank less themselves during the pregnancy (37). Taking these findings together, it is possible that health-promoting partner behavior may discourage adverse outcomes in the mother, while the inverse may not be true: Pregnant woman are unlikely to be differentially impacted by “risky” partner behavior.
We note a number of limitations to the current study. Our analyses were conducted on native-born Swedes, and might not generalize to other populations; while we have no reason to believe that Swedish women are substantially different from women in other industrialized countries, the social resources available to pregnant Swedish women may facilitate decreases in alcohol misuse. We selected a birth cohort to maximize data availability during the time frame relevant to childbirth; this may come at the expense of detecting long-term changes in rates of AUD, or specifically changes in the AUD-pregnancy association. Our use of registry data may be more likely to capture more severe cases of AUD and therefore be subject to false negatives; however, false negatives are a pitfall of nearly any study design, and registry records are less subject to recall or reporting bias than self-reports. The reliance on registry records also precludes examination of intra/inter-personal factors such as personality, motives for changes in alcohol use/misuse, quality of the relationship with one’s partner, etc.
In summary, these findings suggest that pregnancy plays a pivotal motivational role in the reduction of AUD. Our results are consistent with a causal role for pregnancy in AUD risk reduction, though this should not be considered definitive due to the observational nature of the data. Negative associations were strong and consistent across all analyses, and were overall robust to moderation by an array of factors that are otherwise reliable predictors of AUD risk. Both parents benefit from the reduction in AUD risk during the pregnancy, with the association more pronounced for mothers, among whom it persists, with modest attenuation, into the post- partum period. In conjunction with evidence from AUD treatment programs that include cash or prize rewards for abstinence, this putative protective role of pregnancy suggests that qualitatively different factors have the potential to motivate reduction in alcohol misuse, which may broaden the possibilities for intervention in AUD treatment. These findings further suggest that the reduction in volition often associated with substance use disorders may be superseded by especially salient circumstances.
Supplementary Material
Acknowledgments:
These analyses were supported by National Institutes of Health grant R01AA023534 and grants from the Swedish Research Council (K2012–70X-15428–08-3), the Swedish Research Council for Health, Working Life and Welfare (In Swedish: Forte; Reg.nr: 2013–1836), the Swedish Research Council (2012–2378; 2014–10134) and FORTE (2014–0804) as well as ALF funding from Region Skåne awarded. The authors also wish to thank The Swedish Twin Registry at the Karolinska Institute, which provided the twin data for this study.
Footnotes
Disclosures: The authors have no competing interests to report.
References
- 1.Sokol RJ, Delaney-Black V, Nordstrom B. Fetal alcohol spectrum disorder. JAMA 2003;290:2996–2999. [DOI] [PubMed] [Google Scholar]
- 2.Schölin L: Prevention of harm caused by alcohol exposure in pregnancy. Rapid review and case studies from Member States Copenhagen, Denmark, World Health Organization; 2016. [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration: Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings Rockville, MD, Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 4.Mardby AC, Lupattelli A, Hensing G, Nordeng H. Consumption of alcohol during pregnancy- A multinational European study. Women Birth 2017;30:e207–e213. [DOI] [PubMed] [Google Scholar]
- 5.Alvik A, Haldorsen T, Groholt B, Lindemann R. Alcohol consumption before and during pregnancy comparing concurrent and retrospective reports. Alcohol Clin Exp Res 2006;30:510– 515. [DOI] [PubMed] [Google Scholar]
- 6.Bor J, Basu S, Coutts A, McKee M, Stuckler D. Alcohol use during the great recession of 2008–2009. Alcohol Alcohol 2013;48:343–348. [DOI] [PubMed] [Google Scholar]
- 7.Slater ME, Haughwout SP, Castle I-JP: Trends in Substance Use Among Reproductive-Age Females in the United States, 2002–2013 Arlington, VA, U.S. Department of Health and Human Services; 2015. [Google Scholar]
- 8.Kendler KS, Ohlsson H, Svikis DS, Sundquist K, Sundquist J. The Protective Effect of Pregnancy on Risk for Drug Abuse: A Population, Co-Relative, Co-Spouse, and Within- Individual Analysis. Am J Psychiatry 2017;174:954–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirby D: Looking for Reasons Why: The Antecedents of Adolescent Sexual Risk-Taking, Pregnancy, and Child-Bearing Washington, DC, National Campaign to Prevent Teen Pregnancy; 1999. [Google Scholar]
- 10.Salas-Wright CP, Vaughn MG, Ugalde J, Todic J. Substance use and teen pregnancy in the United States: evidence from the NSDUH 2002–2012. Addict Behav 2015;45:218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skagerström J, Alehagen S, Häggström-Nordin E, Årestedt K, Nilsen P. Prevalence of alcohol use before and during pregnancy and predictors of drinking during pregnancy: a cross sectional study in Sweden BMC Public Health; 2013;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Comasco E, Hallberg G, Helander A, Oreland L, Sundelin-Wahlsten V. Alcohol consumption among pregnant women in a Swedish sample and its effects on the newborn outcomes. Alcohol Clin Exp Res 2012;36:1779–1786. [DOI] [PubMed] [Google Scholar]
- 13.Nilsen P, Skagerstrom J, Rahmqvist M, Hultgren E, Blomberg M. Alcohol prevention in Swedish antenatal care: effectiveness and perceptions of the Risk Drinking project counseling model. Acta Obstet Gynecol Scand 2012;91:736–743. [DOI] [PubMed] [Google Scholar]
- 14.Bortes C, Geidne S, Eriksson C. Preventing Alcohol Consumption during Pregnancy: A Randomized Controlled Trial. Health (N Y) 2015;07:289–299. [Google Scholar]
- 15.Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry 2005;162:1403–1413. [DOI] [PubMed] [Google Scholar]
- 16.Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology 2010;35:217–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Psychiatric Association: Diagnostic and statistical manual of mental disorders: DSM-5 Washington, D.C., American Psychiatric Association; 2013. [Google Scholar]
- 18.Higgens S, Sigmon S, Heil S: Contingency management in the treatment of substance use disorders: trends in the literature. in Lowinson and Ruiz’s substance abuse : a comprehensive textbook Edited by Ruiz P, Strain EC, Lowinson JH. 5th ed. Philadelphia, Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011. pp. xxiii, 1074 p. [Google Scholar]
- 19.McDonell MG, Leickly E, McPherson S, Skalisky J, Srebnik D, Angelo F, Vilardaga R, Nepom JR, Roll JM, Ries RK. A Randomized Controlled Trial of Ethyl Glucuronide-Based Contingency Management for Outpatients With Co-Occurring Alcohol Use Disorders and Serious Mental Illness. Am J Psychiatry 2017:appiajp201616050627. [DOI] [PMC free article] [PubMed]
- 20.Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes, and they will come: contingency management for treatment of alcohol dependence. J Consult Clin Psychol 2000;68:250–257. [DOI] [PubMed] [Google Scholar]
- 21.Barnett NP, Celio MA, Tidey JW, Murphy JG, Colby SM, Swift RM. A preliminary randomized controlled trial of contingency management for alcohol use reduction using a transdermal alcohol sensor. Addiction 2017;112:1025–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DePhilippis D, Petry NM, Bonn-Miller MO, Rosenbach SB, McKay JR. The national implementation of Contingency Management (CM) in the Department of Veterans Affairs: Attendance at CM sessions and substance use outcomes. Drug Alcohol Depend 2018;185:367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bailey AJ, Gerst K, Finn PR. Delay discounting of losses and rewards in alcohol use disorder: The effect of working memory load. Psychol Addict Behav 2018;32:197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mole TB, Irvine MA, Worbe Y, Collins P, Mitchell SP, Bolton S, Harrison NA, Robbins TW, Voon V. Impulsivity in disorders of food and drug misuse. Psychol Med 2015;45:771–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mitchell SH. The genetic basis of delay discounting and its genetic relationship to alcohol dependence. Behav Processes 2011;87:10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Businelle MS, McVay MA, Kendzor D, Copeland A. A comparison of delay discounting among smokers, substance abusers, and non-dependent controls. Drug Alcohol Depend 2010;112:247–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta- analysis of twin and adoption studies. Psychol Med 2015;45:1061–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kendler KS, Ohlsson H, Sundquist J, Sundquist K. School Achievement, IQ, and Risk of Alcohol Use Disorder: A Prospective, Co-Relative Analysis in a Swedish National Cohort. J Stud Alcohol Drugs 2017;78:186–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kendler KS, Larsson Lonn S, Morris NA, Sundquist J, Langstrom N, Sundquist K. A Swedish national adoption study of criminality. Psychol Med 2014;44:1913–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeVido J, Bogunovic O, Weiss RD. Alcohol use disorders in pregnancy. Harv Rev Psychiatry 2015;23:112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kitsantas P, Gaffney KF, Wu H, Kastello JC. Determinants of alcohol cessation, reduction and no reduction during pregnancy. Arch Gynecol Obstet 2014;289:771–779. [DOI] [PubMed] [Google Scholar]
- 32.Svikis DS, Reid-Quiñones K. Screening and prevention of alcohol and drug use disorders in women. Obstet Gynecol Clin North Am 2003;30:447–468. [DOI] [PubMed] [Google Scholar]
- 33.Chilcoat HD, Breslau N. Alcohol disorders in young adulthood: effects of transitions into adult roles. J Health Soc Behav 1996;37:339–349. [PubMed] [Google Scholar]
- 34.Fergusson DM, Boden JM, John Horwood L. Transition to parenthood and substance use disorders: findings from a 30-year longitudinal study. Drug Alcohol Depend 2012;125:295–300. [DOI] [PubMed] [Google Scholar]
- 35.Hogberg H, Skagerstrom J, Spak F, Nilsen P, Larsson M. Alcohol consumption among partners of pregnant women in Sweden: a cross sectional study. BMC Public Health 2016;16:694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Connor MJ, Whaley SE. Brief intervention for alcohol use by pregnant women. Am J Public Health 2007;97:252–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Wulp NY, Hoving C, de Vries H. Partner’s influences and other correlates of prenatal alcohol use. Matern Child Health J 2015;19:908–916. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


