Abstract
Introduction:
Use of electronic nicotine delivery systems (ENDS) has increased markedly. We examined how current ENDS users differ in perceptions of tobacco and ENDS-related health risks as a function of cigarette smoking status.
Methods:
We classified 1329 current ENDS users completing a national online survey based on cigarette smoker status, and employed linear and logistic regression to assess group differences in perceptions of tobacco-related health risks.
Results:
The sample consisted of 38% Current Cigarette Smokers, 40% Former Cigarette Smokers, and 22% Non-Smokers. Our targeted recruitment strategy yielded a balance of key descriptive variables across participants. Significant differences were observed in race, employment and marital status across cigarette smoking status, but not in gender, education, income, or sexual orientation. Participants reported considerable perceived knowledge about health risks associated with tobacco use, but less regarding ENDS use. Current Smokers rated ENDS use as riskier than Non-Smokers, and considered cigarette use less risky for both users and bystanders. Current Smokers were more likely to perceive cardiovascular diseases, diabetes and cancer as the health risks associated with ENDS use. Former Smokers were more likely to perceive such risks with traditional tobacco use. Further, regardless of smoking status, perceived knowledge about the health risks of tobacco or ENDS use was positively associated with perceived likelihood of high risks of cardiovascular diseases and cancer.
Conclusions:
Among current ENDS users, there were significant differences in perceived health risks based on cigarette smoking history. Improved health messaging can be achieved when cigarette smoking status is taken into account.
Keywords: Electronic Nicotine Delivery Systems (ENDS), Vaping, Cigarette Smoking, Dual Users, Tobacco
1. Introduction
Tobacco use remains the number-one preventable cause of disease, disability, and death in the United States (Brandon et al., 2015; Crowley & Health Public Policy Committee of the American College of Physicians, 2015; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health, 2014). Estimates suggested that 20.1% of U.S. adults used (every day or some days) any tobacco product in 2015, 17.6% used any combustible tobacco product, and 3.9% used ≤2 tobacco products (Phillips etal., 2017). Electronic nicotine delivery systems (ENDS), including electronic cigarettes, are devices capable of delivering nicotine in an aerosolized form. Since their introduction to the U.S. market in 2007, use of ENDS has increased significantly, particularly among current and former cigarette smokers (King, Patel, Nguyen, & Dube, 2015; Regan, Promoff, Dube, & Arrazola, 2013; Richardson, Pearson, Xiao, Stalgaitis, & Vallone, 2014). Recent studies have found that the majority of U.S. adults are aware of ENDS products (Glasser etal., 2017). Overall, 15.4% of U.S. adults had ever used ENDS and 3.2% were current users in 2016 (National Center for Health Statistics., 2016; Schoenbom & Gindi, 2015). Among these adult current ENDS users, 58.8% were also current cigarette smokers (i.e., dual users), 29.8% were former cigarette smokers, and 11.4% had never been cigarette smokers (CDC, 2017).
Despite continued public education campaigns about the health risks of cigarette smoking, people tend to underestimate these risks (Krosnick etal., 2017). ENDS have changed the tobacco landscape dramatically, and the debate about their relative benefits and harms is ongoing. The promotion of ENDS as products with lower health risks might appeal to individuals who otherwise would not use tobacco products and to smokers who want to quit use of combustible tobacco products entirely. However, despite the unclear nature of health risks and consequences associated with ENDS, usage is increasingly widespread. Furthermore, although it has been suggested that ENDS are less harmful in the short-term (National Academies of Sciences, Engineering, and Medicine, 2018), relatively little is known about patterns of use, as well as perceptions of the potential health risks or benefits of ENDS, alone or in combination with combustible cigarette smoking (Bhatnagar et al., 2014). Given that limited data are available about the long-term health effects of ENDS, ENDS users may underestimate the health risks, and in turn, overestimate health benefits. Though ENDS are widely promoted as smoking cessation aids, they may actually make it harder for cigarette smokers to quit (Al-Delaimy, Myers, Leas, Strong, & Hofstetter, 2015). Many smokers become “dual” or “poly” users (Kasza et al., 2017), for whom health risks could be compounded (Alzahrani, Pena, Temesgen, & Glantz, 2018). A recent study indicated that daily dual users were estimated to have a nearly five-fold risk for heart attack compared to those who have never used either product (Alzahrani et al., 2018). As many individuals base their decisions to smoke on how they believe the act of smoking changes the risk of contracting specific diseases (Krosnick, Chang, Sherman, Chassin, & Presson, 2006), we hypothesized that perceived health risks of ENDS would be moderated by cigarette smoking status such that use of combustible cigarettes would be associated with (1) lower perceived risk for cigarettes and (2) comparatively higher perceived risk of ENDS and symptoms associated with their use. Former and Never Smokers were hypothesized to show the reverse pattern. Thus the primary objective of this study was to examine the perceived health risks and symptoms associated with cigarette and ENDS use among current ENDS users as a function of cigarette smoking status.
2. Methods
2.1. Study sample
The study sample included 1329 current ENDS users from an adult national online survey of 2561 participants conducted in 2016 that was designed to examine vaping practices and attitudes. Recruitment for the national survey was conducted by a marketing research vendor, Research Now and Survey Sampling International (SSI), from June 24 to August 11, 2016, through their online panels and other panels via affiliated partners. Participants aged 18 or older were recruited via emails sent from the online panels to approximately 13,000 individuals, with the goal of achieving a 20% response rate. Tailored campaigns were conducted to recruit hard-to-reach population segments to ensure their participation. Panelists earn points based on the number of surveys in which they participate and may redeem the points for prizes, with a limit on the number of surveys they may take to avoid over-surveying particular respondents. There were three targeted current ENDS user groups: current cigarette smokers, former cigarette smokers, and non-cigarette smokers. The study was approved by the Institutional Review Board of the University of Mississippi Medical Center.
After online consent was obtained, participants responded to questions about their knowledge, perceptions, and behavior regarding tobacco products including ENDS, as well as socio-demographic information. No identifiable information was collected to maintain the anonymity of respondents. Because recruitment efforts included oversampling of key subgroups (i.e., African Americans, Hispanics/Latinos, and persons of low socioeconomic status), the final sample was not intended to be representative of the general population.
2.2. Measures
2.2.1. ENDS use and cigarette smoking status
All participants (N=2561) were asked “How recently have you used an e-cigarette or another device to vape? ” and “How long have you used a vaping device? ” Consistent with the Population Assessment of Tobacco and Health Study (Hyland et al., 2017) classification, participants were considered “current ENDS users” if they used an ENDS device within the past 30 days and had used for more than 3 months.
The participants were also asked about their cigarette smoking status (i.e., combustible cigarettes) with the following two questions: “Have you ever smoked cigarettes?” with response options about whether they have smoked at least 100 cigarettes in their lifetime, and “How recently have you smoked a cigarette?” Based on their responses to these questions, participants were classified as Current Cigarette Smokers, Former Cigarette Smokers, or Cigarette Non-Smokers. Current Smokers were participants who smoked combustible cigarettes in the past 30 days and smoked 100 cigarettes or more in their lifetime. Former Smokers were participants who had smoked 100 cigarettes or more in their lifetime but who had not smoked in the past 30 days. Non-Smokers were participants who never smoked or smoked fewer than 100 cigarettes in their lifetime and had not smoked in the past 30 days. Note that participants identified as Current Smokers were dual users (i.e., using both ENDS and cigarettes).
2.2.2. Participant characteristics
Participants provided their age, gender, race (White/Caucasian, Black/African American, Other), ethnicity (Hispanic or not), marital status (single, married, divorced/separated, widowed), and sexual orientation (heterosexual, lesbian/gay, bisexual, transgender, other). Proxies for socioeconomic status included education, income, and employment status. Education levels were categorized as less than high school diploma, GED, high school diploma, some college, or college degree or higher. Income levels were based on total annual household income and defined as less than $20,000, $20,000-$49,999, $50,000-$64,999, $65,000-$89,999, and $90,000 and above. Employment was classified as employed vs. not employed, with either a full- or part-time job.
2.2.3. Knowledge and perceptions about tobacco and ENDS use
Knowledge and perceived health risks regarding tobacco and ENDS use were measured by the seven questions listed in Table 1. Questions 1 and 2 addressed knowledge of the health risks associated with tobacco use and ENDS use (using 0 – 10 rating scales); Questions 3 and 4 concerned perceived health risks for each type of tobacco product (i.e., ENDS products, cigarettes, cigars, smokeless tobacco; using 0 – 4 rating scales); and Questions 5 and 6 assessed perceived individual risks associated with tobacco use and ENDS use for specific diseases, including heart disease, stroke, diabetes, high blood pressure (BP), cancer, peripheral vascular disease (PVD), etc. (Yes/No response). Question 7 addressed symptoms believed to be caused by ENDS, including dry mouth, itching/burning skin, cough, nausea, bad breath, etc. (Yes/No response).
Table 1.
Perceived knowledge and health risk questions about tobacco and ENDS use
| Item # | Question | Scale |
|---|---|---|
| 1 | How knowledgeable are you about the health risks associated with tobacco use? | 0 to 10a |
| 2 | How knowledgeable are you about the health risks associated with e-cigarettes or other vaping devices? | 0 to 10a |
| 3 | To what extent do you believe these tobacco products create health risks for their users? (separately for ENDS, cigarettes, cigars, smokeless tobacco) | 1 to 4b |
| 4 | To what extent do you believe these tobacco products create health risks for bystanders (people who are nearby but who aren't using the products)? (separately for ENDS, cigarettes, cigars, smokeless tobacco) | 1 to 4b |
| 5 | Which of the following health risks do you believe are associated with tobacco use (select all that apply)? for each health risk: heart disease, Parkinson's disease, stroke, diabetes, pancreatitis, Crohn's disease, high blood pressure, cancer, obesity, arthritis, stomach ulcers, peripheral vascular disease, high cholesterol, and other | Yes/No |
| 6 | Which of the following health risks do you believe will likely be found to be caused by vaping (select all that apply)? for each health risk: heart disease, Parkinson's disease, stroke, diabetes, pancreatitis, Crohn's disease, high blood pressure, cancer, obesity, arthritis, stomach ulcers, peripheral vascular disease, high cholesterol, and other | Yes/No |
| 7 | Have you experienced any symptoms that you believe may be caused by vaping (select all that apply)? for each symptom: dry mouth, itching/burning of the skin, rash, cough, nausea, high blood pressure, bad breath, irritability, headaches, irregular heartbeat, leg cramps, heartburn, loss of taste/smell, and other | Yes/No |
0=not at all, l=very low, and 10=very high
l=no health risks, 2=minimal health risks, 3=moderate health risks, 4=severe health risks
2.3. Statistical analysis
Descriptive statistics were expressed as mean ± standard deviation for continuous measures and as frequency (%) for categorical measures. Differences in demographic characteristics, socioeconomic status (SES), and perceptions of health risks associated with tobacco and ENDS use by cigarette smoking status were evaluated using Chi-square tests and ANOVA as appropriate. The relationships between cigarette smoking status and perceived health risks were further evaluated using linear regression for Questions 1 and 2, multinomial logistic regression for the ordinal responses to Questions 3 and 4, and logistic regression for the binary responses regarding cancer, heart disease, stroke, high BP and PVD risks in Questions 5 and 6. Regression analyses were adjusted for demographics and SES measures, including age, gender, race, education, income, employment status, and sexual orientation. All statistical analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
3. Results
3.1. Sample characteristics
Approximately 38% were Current Smokers, 40% were Former Smokers, and 22% were Non-Smokers. Descriptive statistics by cigarette smoking status are summarized in Table 2. Our targeted recruitment strategy yielded a balance of sufficient participants across key demographic variables except sexual orientation. Differences were noted across smoking status for age, race, ethnicity, employment status, and marital status, but not gender, education, income, or sexual orientation (Table 1). Younger adults (below age 35) accounted for the majority of Current Smokers (57%) and Non-Smokers (74.5%) but fewer Former Smokers (39.8%). Approximately 26%, 43% and 18% of Current, Former and Non-Smokers respectively were Caucasians, while 29%, 24% and 29% were African-Americans. As for ethnicity, Hispanics comprised the majorities for Current (58.6%) and Non-Smokers (63.1%), while only 44.4% for Former Smokers. Current Smokers were more likely to be employed than Former Smokers or Non-Smokers, and Non-Smokers were more likely to be single.
Table 2.
Descriptive characteristics of current ENDS users by cigarette smoking status
| All (N=1329) | Current Smokers (N=507) | Former Smokers (N=532) | Non-Smokers (N=290) | P-value | |
|---|---|---|---|---|---|
| Age | |||||
| 18–24 | 200 (15.1) | 69 (13.6) | 42(7.9) | 89 (30.7) | <0.0001 |
| 25–34 | 517 (38.9) | 220 (43.4) | 170 (32) | 127 (43.8) | |
| 35–44 | 321 (24.2) | 133 (26.2) | 144 (27.1) | 44 (15.2) | |
| 45–64 | 291 (21.9) | 85 (16.8) | 176 (33.1) | 30(10.3) | |
| Female | 656 (49.4) | 260 (51.3) | 248 (46.6) | 148 (51.0) | 0.262 |
| Race | |||||
| Black/African-American | 361 (27.2) | 149 (29.4) | 127 (23.9) | 85 (29.3) | <0.0001 |
| White/Caucasian | 414 (31.2) | 133 (26.2) | 229 (43.1) | 52 (17.9) | |
| Asian American | 37 (2.8) | 20 (3.9) | 6 (1.1) | 11 (3.8) | |
| Native Hawaiian/Pacific Islander | 24(1.8) | 11 (2.2) | 8 (1.5) | 5 (1.7) | |
| American Indian/Alaskan Native | 36 (2.7) | 13 (2.6) | 12 (2.3) | 11 (3.8) | |
| > 1 race | 126 (9.5) | 47 (9.3) | 46 (8.7) | 33 (11.4) | |
| Other | 331 (24.9) | 134 (26.4) | 104 (19.6) | 93 (32.1) | |
| Hispanic | 716 (53.9) | 297 (58.6) | 236 (44.4) | 183 (63.1) | <0.0001 |
| Education | |||||
| <HS | 48 (3.6) | 19 (3.8) | 17 (3.2) | 12 (4.1) | 0.803 |
| GED | 56 (4.2) | 24 (4.7) | 21 (4) | 11 (3.8) | |
| HS with Diploma | 201 (15.1) | 67 (13.2) | 85 (16) | 49 (16.9) | |
| Some College | 548 (41.2) | 204 (40.2) | 225 (42.3) | 119 (41.0) | |
| College degree or more | 476 (35.8) | 193 (38.1) | 184 (34.6) | 99 (34.1) | |
| Income | |||||
| <$20K | 150 (11.3) | 52 (10.3) | 61 (11.5) | 37 (12.8) | 0.655 |
| $20K to $49,999 | 386 (29.0) | 148 (29.2) | 149 (28.0) | 89 (30.7) | |
| $50K to $64,999 | 252 (19.0) | 105 (20.7) | 98 (18.4) | 49 (16.9) | |
| $65K to $89,999 | 257 (19.3) | 91 (18.0) | 104 (19.6) | 62 (21.4) | |
| $90K & Up | 284 (21.4) | 111 (21.9) | 120 (22.6) | 53 (18.3) | |
| Employment Status | |||||
| Employed | 1033 (77.7) | 427 (84.2) | 392 (73.7) | 214 (73.8) | <0.0001 |
| Homemaker/Unemployed/Retired/Disabled | 248 (18.7) | 64 (12.6) | 131 (24.6) | 53 (18.3) | |
| Student | 48 (3.6) | 16 (3.2) | 9 (1.7) | 23 (7.9) | |
| Marital Status | |||||
| Single, never married | 660 (49.7) | 259 (51.1) | 213 (40.0) | 188 (64.8) | <0.0001 |
| Married | 529 (39.8) | 197 (38.9) | 247 (46.4) | 85 (29.3) | |
| Divorced/Separated/Widowed | 140 (10.5) | 51 (10.1) | 72 (13.5) | 17 (5.9) | |
| Sexual Orientation | |||||
| Heterosexual | 1106 (83.2) | 420 (82.8) | 452 (85.0) | 234 (80.7) | 0.496 |
| Lesbian/Gay | 66 (5.0) | 22 (4.3) | 27 (5.1) | 17 (5.9) | |
| Bisexual | 118 (8.9) | 52 (10.3) | 38 (7.1) | 28 (9.7) | |
| T ransgender/Questioning/Other | 39 (2.9) | 13 (2.6) | 15 (2.8) | 11 (3.8) |
Data are expressed as n (%).
3.2. Perceived health risks and symptoms
Participants rated their knowledge about health risks associated with tobacco use significantly higher relative to ENDS (8.60 ± 1.88 for tobacco vs. 6.06 ± 3.12 for ENDS, p<0.001 by Wilcoxon signed rank test). Perceived knowledge about health risks associated with tobacco use and ENDS use differed only slightly based on cigarette smoking status (Table 3). Nevertheless, the two knowledge measures were positively correlated overall (Pearson correlation r=0.28, p<0.001), particularly for Non-Smokers (r=0.45, p<0.001).
Table 3.
Ratings of knowledge and perceived health risks for tobacco products by cigarette smoking status
| Questions | All | Current Smokers |
Former Smokers |
Non- Smokers |
|---|---|---|---|---|
| Question 1. How knowledgeable are you about the health risks associated with tobacco use?* | ||||
| 8.60 ± 1.88 | 8.64 ± 1.74 | 8.77 ± 1.71 | 8.20 ± 2.31 | |
| Question 2. How knowledgeable are you about the health risks associated with e-cigarettes or other vaping devices? | ||||
| 6.06 ± 3.12 | 6.12 ± 3.10 | 6.06 ± 3.11 | 5.97 ± 3.18 | |
| Question 3. To what extent do you believe these tobacco products create health risks for their users? | ||||
| ENDS* | 2.43 ± 0.87 | 2.62 ± 0.87 | 2.31 ± 0.84 | 2.32 ± 0.86 |
| Cigarettes* | 3.80 ± 0.55 | 3.74 ± 0.61 | 3.85 ± 0.47 | 3.83 ± 0.55 |
| Cigars* | 3.61 ± 0.65 | 3.59 ± 0.66 | 3.67 ± 0.61 | 3.54 ± 0.71 |
| Smokeless tobacco* | 3.41 ± 0.78 | 3.37 ± 0.78 | 3.51 ± 0.72 | 3.29 ± 0.85 |
| Question 4. To what extent do you believe these tobacco products create health risks for bystanders (people who are nearby but who aren’t using the products)? | ||||
| ENDS* | 2.11 ± 1.03 | 2.36 ± 1.05 | 1.87 ± 0.95 | 2.07 ± 1.03 |
| Cigarettes* | 3.54 ± 0.73 | 3.47 ± 0.79 | 3.53 ± 0.72 | 3.68 ± 0.65 |
| Cigars* | 3–43 ± 0.76 | 3.38 ± 0.78 | 3.46 ± 0.73 | 3.48 ± 0.76 |
| Smokeless tobacco * | 2.49 ± 1.19 | 2.61 ± 1.15 | 2.29 ± 1.20 | 2.67 ± 1.16 |
Data are expressed as mean ± STD.
Questions 1 and 2 used a scale of 0 to 10, with 0=not at all, l=very low, and 10=very high.
Questions 3 and 4 were rated for each type of tobacco products using a scale of 1-4, with 1=no health risks, 2=minimal health risks, 3=moderate health risks, 4=severe health risks.
A significant risk difference between Current Smokers, Former Smokers and Non-Smokers from ANOVA (p<0.05).
Participants believed that ENDS posed the lowest health risks in general for users as well as for bystanders/others compared with traditional tobacco products (i.e., combustible cigarettes, cigars, and smokeless) (Table 3). Interestingly, when compared with ratings by Former and Non-Smokers, Current Smokers rated ENDS as higher risk and cigarettes as lower risk for both users and bystanders. The multinomial logistic regression for the perceived health risk scores as ordinal responses confirmed these findings (Table 4). Indeed, compared to Non-Smokers, Current Smokers were more likely to believe that ENDS use is associated with greater health risks for users (Odds Ratio [OR]=1.79, 95% Confidence Interval [CI]: 1.35 to 2.39, p<0.0001) and bystanders (OR=1.62, 95% CI: 1.22 to 2.14, p=0.0008), but Former Smokers did not hold these beliefs. In contrast, compared to Non-Smokers, Current Smokers were less likely to rate cigarettes as having greater health risks for users (OR=0.54, 95% CI: 0.34 to 0.85, p=0.0082) and bystanders (OR=0.54, 95% CI: 0.39 to 0.75, p=0.0003), while Former Smokers held such beliefs for bystanders (OR=0.63, 95% CI: 0.45 to 0.89, p=0.009) but not for users (OR=0.91, 95% CI: 0.56 to 1.49, p=0.72). For cigars, the only significant difference was that Current Smokers rated cigars as less risky for bystanders than Non-Smokers. Further, Former Smokers rated smokeless tobacco as riskier for users (OR=1.52, 95% CI: 1.12 to 2.06, p=0.008) and less risky for bystanders (OR=0.56, 95% CI: 0.42 to 0.75, p<0.0001). There was no difference in the perceived risks for users and bystanders between Current Smokers and Non-Smokers.
Table 4.
Multinomial logistic regression of perceived health risks associated with tobacco products by cigarette smoking status * (reference: Non-Smokers)
| Question 3: To what extent do you believe these tobacco products create health risks for their users? | ||||
|---|---|---|---|---|
| Current Smokers | Former Smokers | |||
| Tobacco Products | OR (95% CI) | p-value | OR (95% CI) | p-value |
| ENDS | 1.79(1.35, 2.39) | <0.0001 | 0.86(0.64, 1.16) | 0.3163 |
| Cigarettes | 0.54 (0.34, 0.85) | 0.0082 | 0.91 (0.56, 1.49) | 0.7158 |
| Cigars | 1.05 (0.76, 1.44) | 0.7793 | 1.27 (0.91, 1.76) | 0.1647 |
| Smokeless Tobacco | 1.13 (0.84, 1.52) | 0.4078 | 1.52(1.12, 2.06) | 0.0079 |
| Question 4: To what extent do you believe these tobacco products create health risks for bystanders (people who are nearby but who aren ’ using the products)? | ||||
|---|---|---|---|---|
| Current Smokers | Former Smokers | |||
| Tobacco Products | OR (95% CI) | p-value | OR (95% CI) | p-value |
| ENDS | 1.62(1.22, 2.14) | 0.0008 | 0.72 (0.54, 0.97) | 0.0285 |
| Cigarettes | 0.54 (0.39, 0.75) | 0.0003 | 0.63 (0.45, 0.89) | 0.0090 |
| Cigars | 0.74 (0.55, 1.00) | 0.0493 | 0.91 (0.67, 1.24) | 0.5508 |
| Smokeless Tobacco | 0.85 (0.65, 1.12) | 0.2496 | 0.56 (0.42, 0.75) | <0.0001 |
Questions 3 and 4 were rated for each type of tobacco product using a scale of 1-4, with 1=no health risks, 2=minimal health risks, 3=moderate health risks, 4=severe health risks.
The association of cigarette smoking with perceived health risk was analyzed in multinomial logistic regression for perceived health risk ordinal response, adjusting for age, gender, race, education, income, employment status, and sexual orientation. The analysis was performed separately for the health risk associated with each tobacco product in Questions 3 and 4.
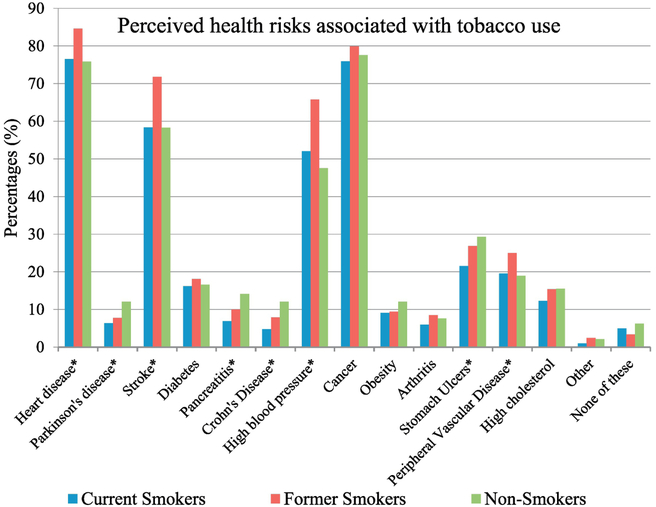
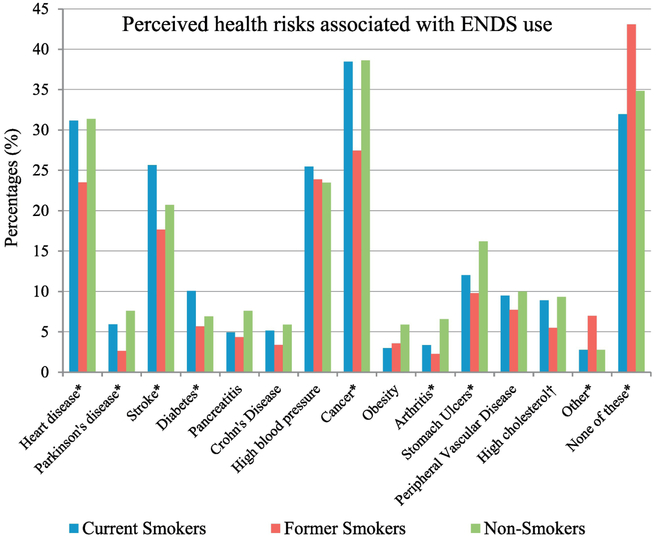
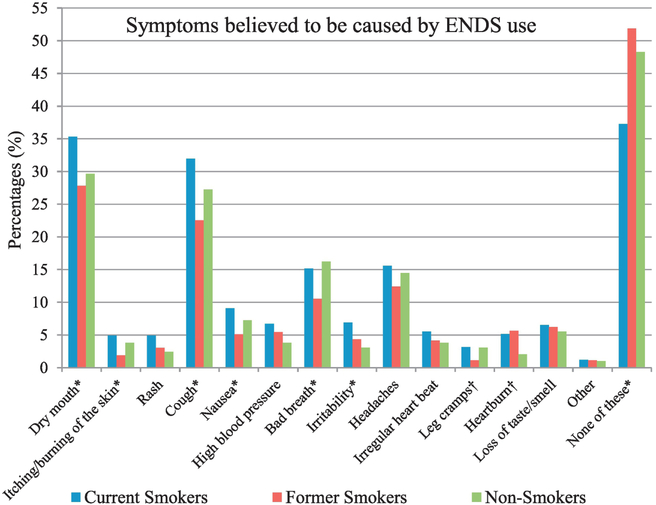
Concerning specific health risks and diseases associated with tobacco and ENDS use, Former Smokers were significantly more likely than Current Smokers or Non-Smokers to perceive heart disease, stroke, high blood pressure, and cancer as the health risks associated with traditional tobacco use (Figure 1). In contrast, compared to Former Smokers, Current Smokers were more likely to associate heart disease, stroke, diabetes, and cancer with ENDS use (Figure 2). Compared to Current Smokers or Former Smokers, Non-Smokers more often associated Parkinson’s disease, pancreatitis, Crohn’s disease, and stomach ulcers with tobacco use (Figure 1) and heart disease, Parkinson’s disease, cancer, arthritis, and stomach ulcers with ENDS use (Figure 2). After adjusting for participants’ demographics and SES characteristics, the only significant differences in risk perceptions of tobacco use and ENDS use between smoking status were found in Former Smokers. Particularly, compared to Non-Smokers, Former Smokers perceived there is a greater risk of high BP associated with tobacco use (OR=1.62, 95% CI: 1.18 to 2.23, p=0.0031), and lower risks of cancer (OR=0.59, 95% CI: 0.43 to 0.82, p=0.0018) and heart disease (OR=0.66, 95% CI: 0.47 to 0.93, p=0.018) associated with ENDS use. Further, regardless of smoking status, the higher the participants rated their knowledge about the health risks of tobacco use (Question 1), the more likely they were to perceive higher risks (13% to 26% higher) for cancer, heart disease, stroke, high BP and PVD associated with tobacco use (Table 5). In contrast, perceived knowledge about the health risks of ENDS use (Question 2) was significantly associated with the perceived risks for heart disease and stroke with ENDS use, but not for cancer, high BP or PVD. Regarding symptoms believed to be caused by ENDS use, Current Smokers were significantly more likely to report dry mouth, itching/burning skin, cough, and nausea than Former Smokers or Non-Smokers (Figure 3).
Figure 1.
Perceived Health Risk associated with Tobacco Use for Question 5: “Which of the following health risks do you believe are associated with tobacco use (select all that apply)?” The risk difference between Current Smokers, Former Smokers and Non-Smokers was evaluated using Chi-square test, with * for a significant difference (p<0.05) and † for a marginally significant difference (0.05 ≤ p < 0.1).
Figure 2.
Perceived Health Risk associated with ENDS Use for Question 6: “Which of the following health risks do you believe will likely be found to be caused by vaping (select all that apply)?” The risk difference between Current Smokers, Former Smokers and Non-Smokers was evaluated using Chi-square test, with * for a significant difference (p<0.05) and † for a marginally significant difference (0.05 ≤ p < 0.1).
Table 5.
Association of knowledge about the health risks with perceived health risks associated with tobacco use and ENDS use
| Perceived risk with Tobacco use | Knowledge about health risk on tobacco use | Perceived risk with ENDS use | Knowledge about health risk on ENDS use | ||
|---|---|---|---|---|---|
| Risk | OR (95 %CI)* | p-value | Risk | OR (95 % CI)† | p-value |
| Cancer | 1.23 (1.15, 1.31) | <.0001 | Cancer | 1.02(0.99, 1.06) | 0.2318 |
| Heart Disease | 1.20(1.12, 1.28) | <.0001 | Heart Disease | 1.06(1.02, 1.10) | 0.0053 |
| Stroke | 1.23 (1.15, 1.31) | <.0001 | Stroke | 1.06(1.01, 1.11) | 0.0116 |
| High BP | 1.13 (1.06, 1.20) | 0.0001 | High BP | 1.04(0.99, 1.08) | 0.0892 |
| PVD | 1.26(1.15, 1.38) | <.0001 | PVD | 1.01 (0.95, 1.08) | 0.7511 |
Odds ratio of the perceived risks in cancer, heart disease, stroke, high BP, and PVD with tobacco use for one point increment in knowledge scale about health risk on tobacco use (Question 1).
Odds ratio of the perceived risks in cancer, heart disease, stroke, high BP, and PVD with ENDS use for one point increment in knowledge scale about health risk on ENDS use (Question 2).
Figure 3.
Symptoms believed to be caused by ENDS use for Question 7: “Have you experienced any symptoms that you believe may be caused by vaping (select all that apply)?” The difference in symptoms between Current Smokers, Former Smokers and Non-Smokers was evaluated using Chi-square test, with * for a significant difference (p<0.05) and † for a marginally significant difference (0.05 ≤ p < 0.1).
4. Discussion
This study characterized 1329 current ENDS users with regard to descriptive variables and perceived health risks associated with tobacco products, including ENDS, as influenced by cigarette smoking status. Significant differences were found across smoking status with age, race/ethnicity, employment, and marital status, but no differences were seen with education, income, or sexual orientation. Current Smokers were more likely to be employed; Non-Smokers skewed younger, Hispanic/Latino and single, whereas Former Smokers skewed older, Caucasian, and married. The participants overall regarded themselves as very knowledgeable about the health risks associated with traditional tobacco product use, but relatively less knowledgeable regarding health risks associated with ENDS use. One possible explanation for this perceived difference in knowledge is the limited research and mixed messages about the health effects of ENDS use currently available, thus highlighting the need for future research. Overall, our findings indicate that current ENDS users significantly differed in their perceived health risks as a function of their cigarette smoking status. Although participants generally believed there were relatively lower risks with ENDS use, Current Smokers rated ENDS use as higher risk than Non-Smokers for both users and bystanders, whereas Former Smokers rated ENDS use as less risky for bystanders. The relatively lower perceived risks of cigarettes by Current Smokers may be a fear-reducing tactic (since they are continuing to smoke), and the rationale for their higher perceived risks of ENDS may reflect a genuine concern regarding potential risks of these devices or a justification to continue use of combustible cigarettes rather than switching solely to ENDS.
It is also noteworthy that Former Smokers perceived ENDS use as relatively lower risk for cardiovascular diseases and cancer, and believed ENDS and smokeless tobacco are significantly less risky for bystanders. Though this study did not evaluate whether ENDS were specifically used as a cessation aid, ENDS appeared to provide an alternative tobacco experience to those who wish to quit cigarette smoking. Previous research has indicated that using ENDS as smoking cessation aids is often linked to extrinsic reasons, such as reducing bad smells and untidiness related to cigarette smoking (Pokhrel & Herzog, 2015). Former Smokers may have been more attuned to the potential relative benefits of ENDS or smokeless tobacco to avoid undesirable consequences of cigarette smoking (e.g., smell, ash, litter), and thus believed that ENDS or smokeless tobacco would not be harmful to bystanders. Our results are consistent with those from a study conducted in Barcelona, in which ENDS were also perceived to pose relatively lower risks to bystanders (Martinez-Sanchez et al., 2015).
For our sample of current ENDS users, health risk knowledge and perceived risks for cancer, heart disease, stroke, high blood pressure and PVD were substantially correlated with perceptions of the risks of tobacco use, but comparatively less so with perceptions of the risks of ENDS use. The long-term risks of tobacco use for cancer and cardiovascular disease are well established, consistent with ratings provided by our participants. One exception is that the perception of the risk of PVD was unrealistically low (<30% in all groups). As expected, the relationship between knowledge and risks associated with ENDS use is weaker, as available information regarding risks and benefits is quite limited and thus more confusing at this time.
Although ENDS products have become widely available and have been marketed in recent years as alternatives to cigarette smoking there are many unanswered questions regarding ENDS use, specifically centered around the impact on individual and public health. A recent report found that the short-term effects of ENDS are less harmful than cigarettes, but they are not risk-free, and their long-term effects remain unclear (National Academies of Sciences, Engineering and Medicine, 2018). In addition to actual health risks, population benefit or harm will depend to a great extent on the public’s perception of product risk and patterns of use. It is certainly conceivable that if users of traditional tobacco products begin using ENDS to support quitting cigarettes, but are unsuccessful, the resultant dual use may increase individual health risks. Indeed, the compounded effects of cigarette smoking were reported in a recent study with daily dual users estimated to have a five-fold increased risk for heart attack (Alzahrani et al., 2018). It is a promising start that the FDA deeming rule requires e-cigarette packaging and advertising to begin carrying a nicotine addiction warning, but additional warnings might be needed for dual users. Further research should be conducted on the nature and impact of dual use (e.g., ENDS and cigarettes) examining behavior longitudinally, as well as perceived personal health effects among dual users. ENDS are increasing in use, particularly among current smokers, and since nicotine exposure can vary greatly by product type and user behavior (Glasser et al., 2017), the health risks and perceptions of health risks about tobacco products can vary considerably across different user groups. Thus, future research should explore such heterogeneity, which will be useful in developing tailored communication strategies about health effects to vulnerable populations including dual users. Overall, research is needed to better understand (1) the health effects associated with long-term use of ENDS products and (2) how to communicate the relative risks of tobacco products as well as their potential impact on consumer product perceptions and use intentions, including both tobacco users and non-users. It is important to note that dual users in our study were cigarette smokers who did not seek cessation treatment, differing from those in other studies that examined dual use in smoking cessation applications (Farsalinos, Romagna, & Voudris, 2015; Nayak, Pechacek, Weaver, & Eriksen, 2016; Vickerman, Beebe, Schauer, Magnusson, & King, 2017). Thus, the perceived health risks of the dual users in our study may differ from the perceptions of treatment seekers.
To our knowledge, this study is one of the larger evaluations of ENDS use in relation to cigarette smoking status. Nevertheless, there are limitations to consider. First, recruitment procedures may have excluded individuals who do not use the Internet; these individuals may differ in important ways from our sample. Second, the survey was cross-sectional, and thus potential changes in perception of health risks over time were not captured. In addition, because of the sampling strategy employed in this study, our findings need to be interpreted with caution as they may not apply to the general population. Nevertheless, a major strength of this work is the characterization of health risk perceptions by cigarette smoking status. This characterization enables a better understanding of motivations and perceptions related to ENDS use.
As awareness of newer tobacco products has increased, more adult cigarette smokers have tried ENDS (McMillen, Gottlieb, Shaefer, Winickoff, & Klein, 2015; Zhu, Zhuang Wong Cummins, & Tedeschi, 2017). Although ENDS use was perceived as less harmful than combustible cigarette smoking more research about the long-term health risks of ENDS use, particularly in combination with adverse risks from other tobacco product use, is needed. Our findings suggest that communication strategies tailored to ENDS users with specific health risk information is warranted. Moreover, communication messages for ENDS users need to take cigarette smoking status into consideration. In order to develop tailored messaging and improved communication strategies for ENDS users, hopefully research findings such as these could be instrumental in informing FDA’s communication campaigns to educate the public about possible health risks of ENDS use, specifically for dual and poly users.
Highlights.
Participants rated higher perceived knowledge about the health risks of tobacco use than ENDS use
Perceived health risk knowledge about tobacco and ENDS use were highly correlated
Current smokers rated health risks of ENDS higher than Former and Non-Smokers
Current Smokers rated health risks of tobacco lower than Former and Non-Smokers
Tobacco and ENDS knowledge were both associated with perceived CV risks
Acknowledgments
Role of Funding Sources
This research was supported by the National Heart, Lung and Blood Institute of the National Institutes of Health and FDA Center for Tobacco Products under Award Number P50HL120163. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Footnotes
Declarations of interest
None
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Al-Delaimy WK, Myers MG, Leas EC, Strong DR, & Hofstetter CR (2015). E-cigarette use in the past and quitting behavior in the future: A population-based study. American Journal of Public Health, 105(6), 1213–1219. doi: 10.2105/AJPH.2014.302482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzahrani T, Pena I, Temesgen N, & Glantz SA (2018). Association between electronic cigarette use and myocardial infarction. American Journal of Preventive Medicine, doi:S0749-3797(18)31871-3 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, … American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. (2014). Electronic cigarettes: A policy statement from the American Heart Association. Circulation, 130(16), 1418–1436. doi: 10.1161/CIR.0000000000000107 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon TH, Goniewicz ML, Hanna NH, Hatsukami DK, Herbst RS, Hobin JA, … Warren GW (2015). Electronic nicotine delivery systems: A policy statement from the American Association for Cancer Research and the American Society of Clinical Oncology. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research, 21(3), 514–525. doi: 10.1158/1078-0432.CCR-14-2544 [doi] [DOI] [PubMed] [Google Scholar]
- CDC. (2017). QuickStats: Percentage of adults who ever used an e-cigarette and percentage who currently use e-cigarettes, by age group - national health interview survey, United States, 2016. MMWR Morbidity and Mortality Weekly Report, 66(33), 892. doi: 10.15585/mmwr.mm6633a6 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley RA, & Health Public Policy Committee of the American College of Physicians. (2015). Electronic nicotine delivery systems: Executive summary of a policy position paper from the American College of Physicians. Annals of Internal Medicine, 162(8), 583–584. doi: 10.7326/M14-2481 [doi] [DOI] [PubMed] [Google Scholar]
- Farsalinos KE, Romagna G, & Voudris V (2015). Factors associated with dual use of tobacco and electronic cigarettes: A case control study. The International Journal on Drug Policy, 26(6), 595–600. doi: 10.1016/j.drugpo.2015.01.006 [doi] [DOI] [PubMed] [Google Scholar]
- Glasser AM, Collins L, Pearson JL, Abudayyeh H, Niaura RS, Abrams DB, & Villanti AC (2017). Overview of electronic nicotine delivery systems: A systematic review. American Journal of Preventive Medicine, 52(2), e33–e66. doi:S0749-3797(16)30573-6 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, … Compton WM (2017). Design and methods of the population assessment of tobacco and health (PATH) study. Tobacco Control, 26(4), 371–378. doi: 10.1136/tobaccocontrol-2016-052934 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, … Hyland AJ (2017). Tobacco-product use by adults and youths in the United States in 2013 and 2014. The New England Journal of Medicine, 376(4), 342–353. doi: 10.1056/NEJMsa1607538 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- King BA, Patel R, Nguyen KH, & Dube SR (2015). Trends in awareness and use of electronic cigarettes among US adults, 2010-2013. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 17(2), 219–227. doi: 10.1093/ntr/ntu191 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krosnick JA, Malhotra N, Mo CH, Bruera EF, Chang L, Pasek J, & Thomas RK (2017). Perceptions of health risks of cigarette smoking: A new measure reveals widespread misunderstanding. PloS One, 12(8), e0182063. doi: 10.1371/journal.pone.0182063 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krosnick JA, Chang L, Sherman SJ, Chassin L, & Presson C (2006). The effects of beliefs about the health consequences of cigarette smoking on smoking onset. Journal of Communication, 56, S18–S37. [Google Scholar]
- Martinez-Sanchez JM, Fu M, Martin-Sanchez JC, Ballbe M, Salto E, & Fernandez E (2015). Perception of electronic cigarettes in the general population: Does their usefulness outweigh their risks? BMJ Open, 5(11), e009218-2015-009218. doi: 10.1136/bmjopen-2015-009218 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen RC, Gottlieb MA, Shaefer RM, Winickoff JP, & Klein JD (2015). Trends in electronic cigarette use among U.S. adults: Use is increasing in both smokers and nonsmokers. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 17(10), 1195–1202. doi: 10.1093/ntr/ntu213 [doi] [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2018). Public health consequences of e-cigarettes. Retrieved from 10.17226/24952. [DOI]
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. (2014). doi:NBK179276 [bookaccession] [Google Scholar]
- National Center for Health Statistics. (2016). Health, United States, 2015: With special feature on racial and ethnic health disparities. Hyattsville, MD. [PubMed] [Google Scholar]
- Nayak P, Pechacek TF, Weaver SR, & Eriksen MP (2016). Electronic nicotine delivery system dual use and intention to quit smoking: Will the socioeconomic gap in smoking get greater? Addictive Behaviors, 61, 112–116. doi: 10.1016/j.addbeh.2016.05.020 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips E, Wang TW, Husten CG, Corey CG, Apelberg BJ, Jamal A, … King BA (2017). Tobacco product use among adults - United States, 2015. MMWR Morbidity and Mortality Weekly Report, 66(44), 1209–1215. doi: 10.15585/mmwr.mm6644a2 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P, & Herzog TA (2015). Reasons for quitting cigarette smoking and electronic cigarette use for cessation help. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 29(1), 114–121. doi: 10.1037/adb0000025 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regan AK, Promoff G, Dube SR, & Arrazola R (2013). Electronic nicotine delivery systems: Adult use and awareness of the 'e-cigarette' in the USA. Tobacco Control, 22(1), 19–23. doi: 10.1136/tobaccocontrol-2011-050044 [doi] [DOI] [PubMed] [Google Scholar]
- Richardson A, Pearson J, Xiao H, Stalgaitis C,& Vallone D (2014). Prevalence, harm perceptions, and reasons for using noncombustible tobacco products among current and former smokers. American Journal of Public Health, 104 (8), 1437–1444. doi: 10.2105/AJPH.2013.301804 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenbom CA, & Gindi RM (2015). Electronic cigarette use among adults: United States, 2014. NCHS Data Brief, (217)(217), 1–8. [PubMed] [Google Scholar]
- Vickerman KA, Beebe LA, Schauer GL, Magnusson B, & King BA (2017). Electronic nicotine delivery system (ENDS) use during smoking cessation: A qualitative study of 40 Oklahoma quitline callers. BMJ Open, 7(4), e013079-2016-013079. doi: 10.1136/bmjopen-2016-013079 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu SH, Zhuang YL, Wong S, Cummins SE, & Tedeschi GJ (2017). E-cigarette use and associated changes in population smoking cessation: Evidence from US current population surveys. BMJ (Clinical Research Ed.), 358, j3262. doi: 10.1136/bmj.j3262 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]