Abstract
Latent myofascial trigger points (MTrP) have been linked to several impairments of muscle function. The present study was conducted in order to examine whether a single bout of self-myofascial release using a foam roller is effective in reducing MTrP sensitivity. Fifty healthy, pain-free subjects (26.8±6 years, 21 men) with latent MTrP in the lateral gastrocnemius muscle were included in the randomized, controlled trial. One week after a familiarization session, they were randomly allocated to three groups: (1) static compression of the most sensitive MTrP using a foam roll, (2) slow dynamic foam rolling of the lateral calf and (3) placebo laser acupuncture of the most sensitive MTrP. Treatment duration in each group was 90 seconds. The pressure pain threshold (PPT) of the most sensitive MTrP was assessed using a handheld algometer prior to and after the intervention. A repeated measures analysis of variance (3x2) did not reveal significant between-group interactions (p>.05) but showed a significant time effect (F=7.715, p<.05). While placebo and dynamic self-myofascial release did not change MTrP sensitivity (p>.05), static compression of MTrP increased the PPT (2.6±0.8 to 3.0±1.1, d=.35; p<.05). Static self_myofascial release using a foam roller might represent an alternative to reduce pressure pain of latent MTrP. Additional research should aim to extend these findings to patients and athletes with myofascial pain syndromes.
Keywords: Foam rolling, Myofascial pain, Self-massage, Fascia
INTRODUCTION
Myofascial trigger points (MTrP), hyperirritable spots located within taut bands of skeletal muscle fibres, have been suggested to represent an important contributor to musculoskeletal pain [1]. According to recent data, active MTrP are prevalent in several chronic disorders such as unilateral shoulder pain of elite swimmers [2]. In addition to active MTrP, also a latent form has been described. While not necessarily leading to pain (in contrast to active trigger points), latent MTrP are linked to accelerated muscle fatigability [3], increased risk of muscle cramps [4], and altered muscular activation patterns [5-7]. In addition to these impairments of muscle function, which potentially hamper sports performance, sustained mechanical nociceptive stimulation of latent MTrP might cause widespread central sensitization or a transformation of latent into active MTrP [8,9]. Against this background, the elimination of latent MTrP seems advisable in order to optimize muscle function and prevent the development of chronic pain syndromes.
A multitude of therapies have been proposed to eliminate MTrP [10,11]. Manual therapeutic approaches such as ischaemic compression or myofascial release represent the modalities applied most often [10,12]. Throughout the past years, self-massage with rigid foam rollers and other small handheld tools (self-myofascial release, SMR) has evolved. It claims to mimic the effects of manual therapy and massage and can be performed in a home-based setting. While it is unclear as to whether SMR primarily affects the muscle or the connective tissue (i.e., the deep fascia), a variety of treatment effects have been described: Besides increasing range of motion [13-15], and accelerating regeneration after sports activities [16-18], it is suggested to reduce trigger point pain. However, the latter assumption has not been investigated so far [19]. The present study, therefore, aimed to examine a) whether self-myofascial release using a foam roll is effective in reducing latent MTrP sensitivity and b) which technique, static or dynamic application, is superior in this context.
MATERIALS AND METHODS
Experimental approach to the problem
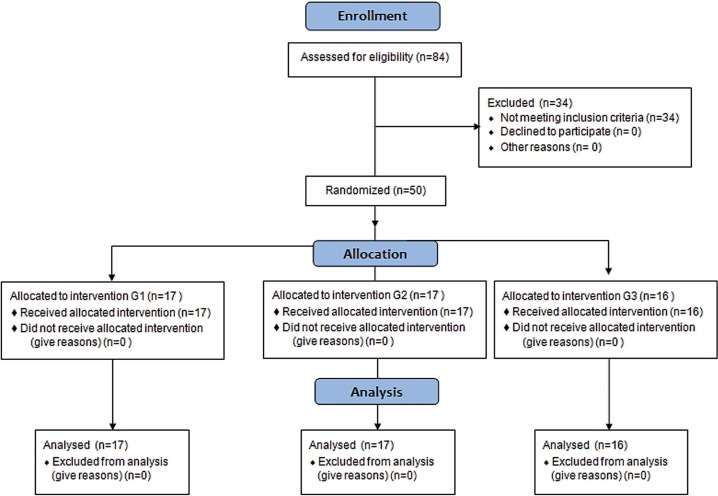
A single-blind, randomized, placebo-controlled, parallel group study (Fig. 1) was conducted comparing a) static compression of a latent MTrP with a foam roller, b) dynamic foam rolling over a latent MTrP, and c) placebo laser acupuncture of a muscle afflicted with a latent MTrP. It was hypothesized that condition a) would be superior to the other interventions with regard to the reduction of pressure pain sensitivity, assessed by means of algometry.
FIG. 1.
CONSORT study flow chart.
Subjects
Healthy, pain-free individuals aged 18 to 40 years with latent myofascial trigger points in the lateral gastrocnemius muscle were included in the present study. Recruitment was conducted through poster advertising and by word of mouth. Exclusion criteria were as follows: (1) severe cardiovascular, pulmonary, neurological, psychiatric or inflammatory rheumatic diseases, (2) specific orthopaedic diseases, e.g. radicular symptoms, myofascial pain syndrome (characterized by presence of active trigger points) or other chronic pain syndromes, (3) analgesic intake in past 48 hours, and (4) history of surgery in the lower extremity.
Procedures
Trigger point detection
All participants were screened for latent MTrP in the lateral gastrocnemius muscle. Aiming to reduce location-specific variance, the search, performed by a trained investigator, was restricted to the area of TrP2 according to Travell and Simons [20], which is located near the muscle belly. The gastrocnemius muscle was chosen because a) it has been shown to exhibit the highest prevalence of latent MTrP in healthy subjects [21], and b) foam rolling is most feasible and easy to standardize at the lower extremity.
Trigger point detection was based on the following criteria: (1) palpable taut band, (2) presence of a painful nodule within this taut band, (3) referred pain on palpation of the nodule. Only MTrP with a pressure pain threshold (PPT) of less than 5 kg/cm² were considered [22]. To ensure identical pre- and post-treatment measurements of MTrP sensitivity, each diagnosed MTrP was marked with a skin marker. The presence of myofascial pain syndrome/active MTrP was excluded by means of screening for the criterion of pain recognition, which is described as the decisive sign of the condition [23].
Randomization
The included participants were randomly allocated to three groups (Fig. 2): static compression of the most sensitive latent MTrP using a foam roller (G1), slow dynamic self-massage of the lateral calf using a foam roller (G2), and placebo laser acupuncture of the most sensitive latent MTrP (G3). Randomization was performed by an independent investigator using BiAs 10.04 (Goethe University, Frank-furt, Germany).
FIG. 2.
Applied interventions: static compression of the MTrP (1), dynamic rolling (2) and placebo laser acupuncture (3).
Interventions
The study comprised two sessions. Session one served as a familiarization session. All subjects were instructed how to handle the foam roll (Blackroll AG, Bottighofen, Switzerland) which was used for the self-myofascial release treatments. Two different techniques were demonstrated: static compression of a painful spot of the muscle and continuous rolling between insertion and origin (Fig. 2). Special focus was placed on relaxing the treated body region. More-over, strategies and positions aiming to increase or decrease the pressure exerted on the tissue were shown. The participants learned to use these strategies in order to achieve a targeted pressure intensity of 6 to 7 on a 10 cm numerical rating scale (NRS) with 0 representing no discomfort and 10 indicating maximum discomfort [24]. The second session was carried out after a wash-out period of one week and consisted of the three-armed intervention. Each of the randomly allocated treatments had a duration of 90 seconds (Fig. 2).
In G1, subjects were instructed to compress the most sensitive trigger point by means of the foam roll without further movement at a targeted subjective discomfort of 6 to 7 on the NRS (as demon-strated in the familiarization session). The G2 group used the device slowly rolling between insertion and origin of the lateral gastrocnemius. A metronome was used to guarantee a standardized movement velocity of five strokes back and forth per minute. By analogy with the static compression group, the targeted discomfort was 6 to 7 on the NRS.
Placebo laser acupuncture (G3) was applied in the prone position using the Laserneedle System (Laserneedle Systems GmbH, Glienicke/Nordbahn, Germany). It contains optical fibres having an ending that resembles a needle. For the treatment, three fibres were fixed by adhesive tape on the skin surrounding the most sensitive MTrP. To ensure blinding, subjects were not informed that the laser source remained switched off during the treatment [25]. Only the laser device was activated to provide visual and acoustic signals. Laser acupuncture has been shown to be both an effective treatment in neck pain [26] and a credible placebo option [25].
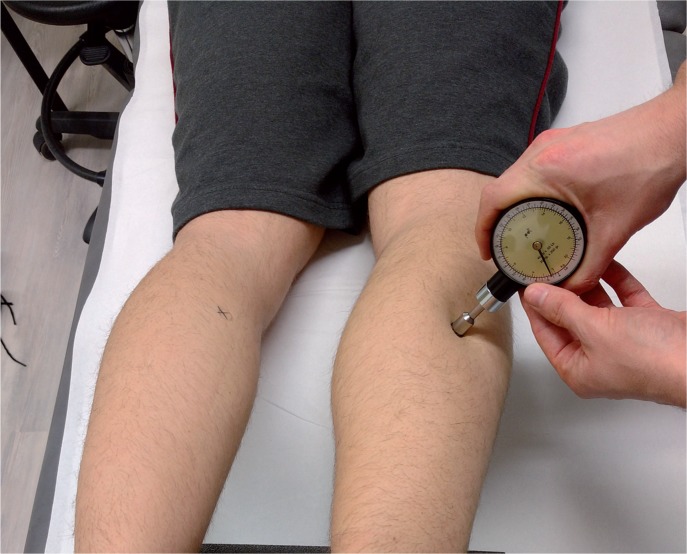
Measurements
Prior to and immediately after intervention, the pressure pain threshold (PPT) of the most sensitive MTrP was measured with a handheld mechanical pressure algometer (diameter 1 cm²; PDT, New York, USA). A trained investigator applied increasing pressure to the MTrP at a rate of approximately 1 kg/cm²/s until the subject reported a painful sensation (Fig. 3). The corresponding force value (kg/cm²) was recorded. The lower the score (and thus PPT), the higher is the tenderness of the tissue in the tested area. The primary MTrP was measured three times with 10-second time intervals. The mean of the two last measurements was employed for further analysis [27]. Sufficient repeated-measures reliability of the device has been demonstrated by Nussbaum and Downes [27].
FIG. 3.
Measurement of the pressure pain threshold at the primary MTrP.
Statistical analyses
From the raw data, mean values and standard deviations were calculated. After testing for variance homogeneity and normal distribution of residuals, a repeated-measures ANOVA (3x2) was used to detect differences between treatments and time. Subsequently, post hoc t tests for dependent (in the case of time effects) or independent samples (in the case of group interactions) were computed. For systematic differences, effect sizes (Cohen’s d, [28]) were calculated and interpreted as small (d=0.2), medium (d=0.5) or large (d=0.8). For all analyses, p values <.05 were considered to be significant. Statistical calculations were performed with SPSS 22 (IBM., Armonk, NY, USA).
Ethics
The study adhered to the CONSORT guidelines [29]. It was conducted in accordance with the Declaration of Helsinki and approval of the local ethics committee was obtained. Each included subject signed informed consent. The trial was registered at clinicaltrials.gov (NCT02609412).
RESULTS
A total of 84 healthy, pain-free subjects were screened for eligibility. Fifty (26.8±6 years, 21 men) of them exhibited latent, but no active MTrP and were included in the trial. After treatment allocation, there were no systematic between-group discrepancies concerning basic anthropometric data and baseline values of MTrP sensitivity (Table 1).
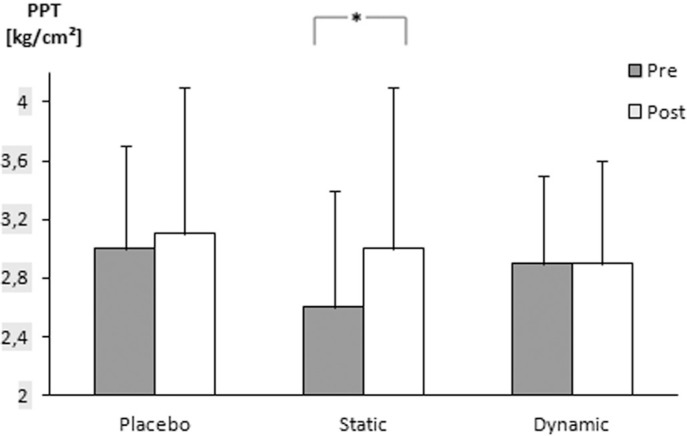
The repeated measures analysis of variance revealed no group interaction (p>.05), but a time effect was observed (F=7.715, p<.05). According to post hoc testing for dependent samples, static compression increased PPT (2.6±0.8 to 3.0±1.1; p<.05, d=.35, Fig. 4). In contrast, dynamic self-myofascial release (2.9±.6 to 2.9±0.7; p>.05) and placebo laser (2.9±0.8 to 3.1±1.0; p>.05) did not change MTrP sensitivity from before to after treatment (p>.05).
FIG. 4.
Mean pre- and post-treatment values of pressure pain (PPT) in the three groups (means and standard deviations are displayed; asterisks indicate significant differences).
DISCUSSION
The present study demonstrated for the first time that a single bout of static self-myofascial release is effective in reducing MTrP sensitivity in the lateral gastrocnemius muscle. The mechanism inducing the pain relief may be analogous to manual ischaemic compression. Previous research found that the sustained pressure applied in related techniques leads to reactive hyperaemia [30], which, in turn, causes a release of muscle fibre tension. Furthermore, increased blood flow accelerates removal of biochemicals such as bradykinin, CGRP, IL-6, IL-8 or TNF-α, which have been shown to be accumulated in myofascial trigger points [31]. Another hypothesis potentially explaining the analgesic treatment effect relates to neurological rather than biochemical mechanisms. It has been suggested that tactile stimulation of a painful area leads to a pre-synaptic inhibition of slow, pain-transmitting nerve fibres [32].
In contrast to static application, which appears to slightly decrease MTrP pain, we found no change of MTrP sensitivity in dynamic foam rolling. As the participants self-massaged the whole lateral gastrocnemius muscle, it might be assumed that this approach does not provide sufficient direct compression of the MTrP. Hence, if athletes intend to treat myofascial pain conditions or aim to reduce MTrP-related impairments of muscle function, static compression with a foam roller may be the only potentially effective treatment modality.
Several other trials have examined manual ischaemic compression (IC) of latent myofascial trigger points. However, most of them focused on the neck region. Aguilera et al. [33] found both ultrasound and IC to be effective in reducing pressure pain. Similarly, Fernández-de-las-Peñas and colleagues [34] showed that transverse friction massage and IC decrease MTrP sensitivity with no differences between the treatments. In a four-armed study, Sarrafzadeh et al. [35] compared IC, phonophoresis and ultrasound to a control group. While all therapies were more effective than the control condition, only the first two treatments were superior to ultrasound application.
Only Grieve et al. [36] examined IC at the lower extremity, which is highly relevant for athletes. After manually treating the soleus muscle, they observed an increased ankle range of motion, but they did not measure pressure pain. The results of the present study are generally in line with the previous research demonstrating the efficacy of ischaemic compression in decreasing latent MTrP sensitivity or enhancing muscle function. However, our study is the first to use a foam roller for treating myofascial trigger points. Thus, no direct comparison can be made with respect to efficacy.
While static MTrP compression induced a decrease in pressure pain, it was not superior to placebo laser acupuncture. Additional studies with a larger sample size might have the required power to detect a between-group difference. Nonetheless, we consider the present study’s findings to have clinical relevance. Only a few non-invasive therapies for MTrP have been proven to be effective [10,12]. In view of this, two arguments support the use of a foam roller to treat MTrP. Firstly, the acute pain relief of 15% and the small to moderate effect size are notable as the duration of the single treatment was only 90 seconds. Secondly, the foam roller can easily be used by the athlete himself and in the absence of a physical therapist or physician, which fosters his independence and possibly reduces health care costs associated with other treatments.
Some methodological issues have to be discussed. Previous trials examining self-myofascial release used an apparatus to guarantee constant pressure and uniformity in rolling velocity [14,15] without or with little active involvement of the subjects. In contrast, our subjects were instructed to perform the treatment themselves as it is done in practice. To standardize rolling speed we used a metronome and the degree of pressure was dependent on the subjective level of discomfort, which was set to 6-7 on a numerical rating scale. It is likely that the implementation of a custom-made device facilitates more precise application of speed and pressure. However, we assume that our approach still guaranteed a high degree of standardization. Furthermore, as the present study aimed to produce data mimicking the results of realistic therapeutic/sports-related settings, the chosen protocol seems more appropriate. Regarding the trial design, we only examined the intervention effects immediately after treatment. It is possible that the soft tissue adapts after a latency period, which cannot be covered without further measurements. Future studies might hence include a longer time frame. Finally, in our trial, we focussed on the pressure pain threshold only, which is a limitation. It would be interesting to examine additional outcome parameters in future studies. The assessment of subjective motion-related pain (e.g. visual analogue scale), viscoelastic tissue properties (stiffness and elasticity), or imaging characteristics (ultrasound, elastography) could provide valuable information helping to explain the treatment effects.
Practical implications
The treatment of latent myofascial trigger points using a foam roller represents an intriguing option to resolve impairments of muscle function arising from MTrP. In contrast to dynamic rolling, only static compression might be effective and should be preferred by athletes. A key benefit of self-myofascial release consists in the fact that treatments can be performed by a player himself and according to his individual needs. Furthermore, although the observed effects have yet to be confirmed in trials with larger sample sizes (in particular against a placebo control), the comparably short treatment duration allows the technique to be applied during game breaks (e.g. half time) and warm-up. Future research with larger sample sizes should examine dose-response relationships (e.g., whether longer or repeated treatments are more effective than a single bout) and the intervention’s efficacy in other body regions as well as in active MTrP.
CONCLUSIONS
The use of a foam roller, applying static compression to latent MTrP, might help sportsmen to resolve impairments of muscle function and optimize performance. In view of our findings, the potential role of static self-myofascial release in the treatment of sports-related pain syndromes (e.g. runner’s knee) should be further elucidated.
Acknowledgements
The authors would like to thank Florian Völker for his assistance in data collection.
REFERENCES
- 1.Lavelle ED, Lavelle W, Smith HS. Myofascial Trigger Points. Anesthesiol Clinics. 2007;25:841–851. doi: 10.1016/j.anclin.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Hidalgo-Lozano A, Fernández-de-las-Peñas C, Calderón-Soto C, Domingo-Camara A, Madeleine P, Arroyo-Morales M. Elite swimmers with and without unilateral shoulder paIn: mechanical hyperalgesia and active/latent muscle trigger points in neck-shoulder muscles. Scand J Med Sci Sports. 2013;23:66–73. doi: 10.1111/j.1600-0838.2011.01331.x. [DOI] [PubMed] [Google Scholar]
- 3.Ge H, Arendt-Nielsen L, Madeleine P. Accelerated muscle fatigability of latent myofascial trigger points in humans. Pain Med. 2012;13:957–964. doi: 10.1111/j.1526-4637.2012.01416.x. [DOI] [PubMed] [Google Scholar]
- 4.Ge H, Zhang Y, Boudreau S, Yue S, Arendt-Nielsen L. Induction of muscle cramps by nociceptive stimulation of latent myofascial trigger points. Exp Brain Res. 2008;187:623–629. doi: 10.1007/s00221-008-1331-y. [DOI] [PubMed] [Google Scholar]
- 5.Ibarra JM, Ge H, Wang C, Martínez Vizcaíno V, Graven-Nielsen T, Arendt-Nielsen L. Latent Myofascial Trigger Points are Associated With an Increased Antagonistic Muscle Activity During Agonist Muscle Contraction. J Pain. 2011;12:1282–1288. doi: 10.1016/j.jpain.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Ge H, Monterde S, Graven-Nielsen T, Arendt-Nielsen L. Latent Myofascial Trigger Points Are Associated With an Increased Intramuscular Electromyographic Activity During Synergistic Muscle Activation. J Pain. 2014;15:181–187. doi: 10.1016/j.jpain.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Lucas KR, Polus BI, Rich PA. Latent myofascial trigger points: their effects on muscle activation and movement efficiency. J Bodyw Mov Ther. 2004;8:160–166. [Google Scholar]
- 8.Xu Y, Ge H, Arendt-Nielsen L. Sustained Nociceptive Mechanical Stimulation of Latent Myofascial Trigger Point Induces Central Sensitization in Healthy Subjects. J Pain. 2010;11:1348–1355. doi: 10.1016/j.jpain.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Ge H, Arendt-Nielsen L. Latent Myofascial Trigger Points. Curr Pain Headache Rep. 2011;15:386–392. doi: 10.1007/s11916-011-0210-6. [DOI] [PubMed] [Google Scholar]
- 10.las Peñas CF de, Sohrbeck Campo M, Fernández Carnero J, Miangolarra Page JC. Manual therapies in myofascial trigger point treatment: a systematic review. J Bodyw Mov Ther. 2005;9:27–34. [Google Scholar]
- 11.Tough EA, White AR, Cummings TM, Richards SH, Campbell JL. Acupuncture and dry needling in the management of myofascial trigger point paIn: A systematic review and meta-analysis of randomised controlled trials. Eur J Pain. 2009;13:3–10. doi: 10.1016/j.ejpain.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Rickards LD. The effectiveness of non-invasive treatments for active myofascial trigger point paIn: A systematic review of the literature. Int J Osteop Med. 2006;9:120–136. [Google Scholar]
- 13.MacDonald GZ, Penney MD, Mullaley ME, et al. An Acute Bout of Self-Myofascial Release Increases Range of Motion Without a Subsequent Decrease in Muscle Activation or Force. J Strength Cond Res. 2013;27:812–821. doi: 10.1519/JSC.0b013e31825c2bc1. [DOI] [PubMed] [Google Scholar]
- 14.Sullivan KM, Silvey DBJ, Button DC, Behm DG. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther. 2013;8:228–236. [PMC free article] [PubMed] [Google Scholar]
- 15.Bradbury-Squires DJ, Noftall JC, Sullivan KM, Behm DG, Power KE, Button DC. Roller-Massager Application to the Quadriceps and Knee-Joint Range of Motion and Neuromuscular Efficiency During a Lunge. J Athl Train. 2015;50:133–140. doi: 10.4085/1062-6050-49.5.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Healey KC, Hatfield DL, Blanpied P, Dorfman LR, Riebe D. The Effects of Myofascial Release With Foam Rolling on Performance. J Strength Cond Res. 2014;28:61–68. doi: 10.1519/JSC.0b013e3182956569. [DOI] [PubMed] [Google Scholar]
- 17.MacDonald GZ, Button DC, Drinkwater EJ, Behm DG. Foam Rolling as a Recovery Tool after an Intense Bout of Physical Activity. Med Sci Sports Exerc. 2014;46:131–142. doi: 10.1249/MSS.0b013e3182a123db. [DOI] [PubMed] [Google Scholar]
- 18.Pearcey GEP, Bradbury-Squires DJ, Kawamoto J, Drinkwater EJ, Behm DG, Button DC. Foam Rolling for Delayed-Onset Muscle Soreness and Recovery of Dynamic Performance Measures. J Athl Train. 2015;50:5–13. doi: 10.4085/1062-6050-50.1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalichman L, Ben David C. Effect of self-myofascial release on myofascial pain, muscle flexibility, and strength: A narrative review. J Bodyw Mov Ther. 2016 doi: 10.1016/j.jbmt.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Travell JG, Simons LS. Myofascial pain and dysfunction: The trigger point manual. Williams & Wilkins; 1999. [Google Scholar]
- 21.Zuil-Escobar JC, Martínez-Cepa CB, Martín-Urrialde JA, Gómez-Conesa A. The Prevalence of Latent Trigger Points in Lower Limb Muscles in Asymptomatic Subjects. 2016. [DOI] [PubMed]
- 22.Sciotti VM, Mittak VL, DiMarco L, et al. Clinical precision of myofascial trigger point location in the trapezius muscle. Pain. 2001;93:259–266. doi: 10.1016/S0304-3959(01)00325-6. [DOI] [PubMed] [Google Scholar]
- 23.Shah JP, Thaker N, Heimur J, Aredo JV, Skdhar S, Gerber LH. Myofascial trigger points then and now: a historical and scientific perspective. PM&R. 2015;7:746–761. doi: 10.1016/j.pmrj.2015.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fryer G, Hodgson L. The effect of manual pressure release on myofascial trigger points in the upper trapezius muscle. J Bodyw Mov Ther. 2005;9:248–255. [Google Scholar]
- 25.Irnich D, Behrens N, Molzen H, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ. 2001;322:1574–1578. doi: 10.1136/bmj.322.7302.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chow RT, Johnson MI, Lopes-Martins RAB, Bjordal JM. Efficacy of low-level laser therapy in the management of neck paIn: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet. 2009;374:1897–1908. doi: 10.1016/S0140-6736(09)61522-1. [DOI] [PubMed] [Google Scholar]
- 27.Nussbaum EL, Downes L. Reliability of clinical pressure-pain algometric measurements obtained on consecutive days. Phys Ther. 1998;78:160–169. doi: 10.1093/ptj/78.2.160. [DOI] [PubMed] [Google Scholar]
- 28.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 29.Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moraska AF, Hickner RC, Kohrt WM, Brewer A. Changes in Blood Flow and Cellular Metabolism at a Myofascial Trigger Point With Trigger Point Release (Ischemic Compression): A Proof-of-Principle Pilot Study. Arch Phys Med Rehabil. 2013;94:196–200. doi: 10.1016/j.apmr.2012.08.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shah JP, Danoff JV, Desai MJ, et al. Biochemicals Associated With Pain and Inflammation are Elevated in Sites Near to and Remote From Active Myofascial Trigger Points. Arch Phys Med Rehabil. 2008;89:16–23. doi: 10.1016/j.apmr.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 32.Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35:235–256. doi: 10.2165/00007256-200535030-00004. [DOI] [PubMed] [Google Scholar]
- 33.Aguilera FJM, Martín DP, Masanet RA, Botella AC, Soler LB, Morell FB. Immediate Effect of Ultrasound and Ischemic Compression Techniques for the Treatment of Trapezius Latent Myofascial Trigger Points in Healthy Subjects: A Randomized Controlled Study. J Manipul Physiol Therapeutics. 2009;32:515–520. doi: 10.1016/j.jmpt.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 34.Fernández-de-las-Peñas C, Alonso-Blanco C, Fernández-Carnero J, Carlos Miangolarra-Page J. The immediate effect of ischemic compression technique and transverse friction massage on tenderness of active and latent myofascial trigger points: a pilot study. J Bodyw Mov Ther. 2006;10:3–9. [Google Scholar]
- 35.Sarrafzadeh J, Ahmadi A, Yassin M. The Effects of Pressure Release, Phonophoresis of Hydrocortisone, and Ultrasound on Upper Trapezius Latent Myofascial Trigger Point. Arch Phys Med Rehabil. 2012;93:72–77. doi: 10.1016/j.apmr.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Grieve R, Clark J, Pearson E, Bullock S, Boyer C, Jarrett A. The immediate effect of soleus trigger point pressure release on restricted ankle joint dorsiflexion: A pilot randomised controlled trial. J Bodyw Mov Ther. 2011;15:42–49. doi: 10.1016/j.jbmt.2010.02.005. [DOI] [PubMed] [Google Scholar]