Abstract
Bariatric surgery leaks remain a dreaded complication with ominous consequences. Fully covered stents have shown efficacy in the treatment of leaks; however, stent migration remains a major drawback. Ultra-large stents have shown reduced rates of migration and coapt better against the walls, but deep ulcers occur in almost all patients, as well as frequent severe intolerance, bleeding, and perforation. We have developed a large expandable stent with physical characteristics and a particularly flexible mesh design that make it much less traumatic than conventional large stents while maintaining the advantage of being less prone to migration. In this patient with a post-sleeve gastrectomy leak, we provide a proof of concept that the Gastroseal stent is effective and nontraumatic despite its very large size.
Introduction
Staple-line leaks remain a catastrophic complication of bariatric surgery occurring in 1–2% of sleeve gastrectomies; this complication is even more common in revisional procedures.1,2 Endoscopic stenting has proved to be an effective minimally invasive technique for the management of such leaks, although frequent stent migration remains a major drawback.3 Current stents are not adapted to the specific anatomy of bariatric surgery leaks, which typically involve tight lumens and acute angulations. The use of large stents to reduce the risk of migration has been attempted with some success, but large stents are associated with severe intolerance, esophageal strictures, frequent deep ulcers, perforations, and bleeding.4,5 The injury appears to be caused in almost all cases by the distal stent edges. We have developed a stent specifically designed for post-bariatric surgery leaks with significant flexibility and an atraumatic design to avoid the common complications while maintaining a low migration rate.
Case Report
A 32-year-old woman with a body mass index (BMI) of 46 kg/m2 underwent a sleeve gastrectomy for morbid obesity. After an uneventful recovery, she was discharged after 2 days. One week later she presented with fever, epigastric pain, leukocyte count 22,545/µL, and a C-reactive protein 253 mg/dL. Imaging studies including ultrasonography and computed tomography (CT) with oral contrast revealed significant leakage from the gastric sleeve and a left subphrenic collection surrounding the spleen. Pus was collected and drains were inserted laparoscopically. The patient was kept on total parentral nutrition for 3 weeks; upon re-introduction of oral feeding, persistent leakage occurred with increased drain output and a left subphrenic collection. The collection was aspirated under ultrasonographic guidance, revealing frank pus. Endoscopy revealed an 8-mm leak orifice at the gastroesophageal junction oozing some pus. Contrast injection confirmed leakage through this orifice into the left subphrenic space. Due to the presence of infection, friable tissue, and a difficult tangential position, it was decided not to attempt applying an over-the-scope clip. A novel, fully covered, expandable metallic stent was inserted with the upper edge lying in the esophagus and the lower edge lying in the duodenum (Gastroseal™, M.I.Tech, Seoul, South Korea) (Figure 1).
Figure 1.
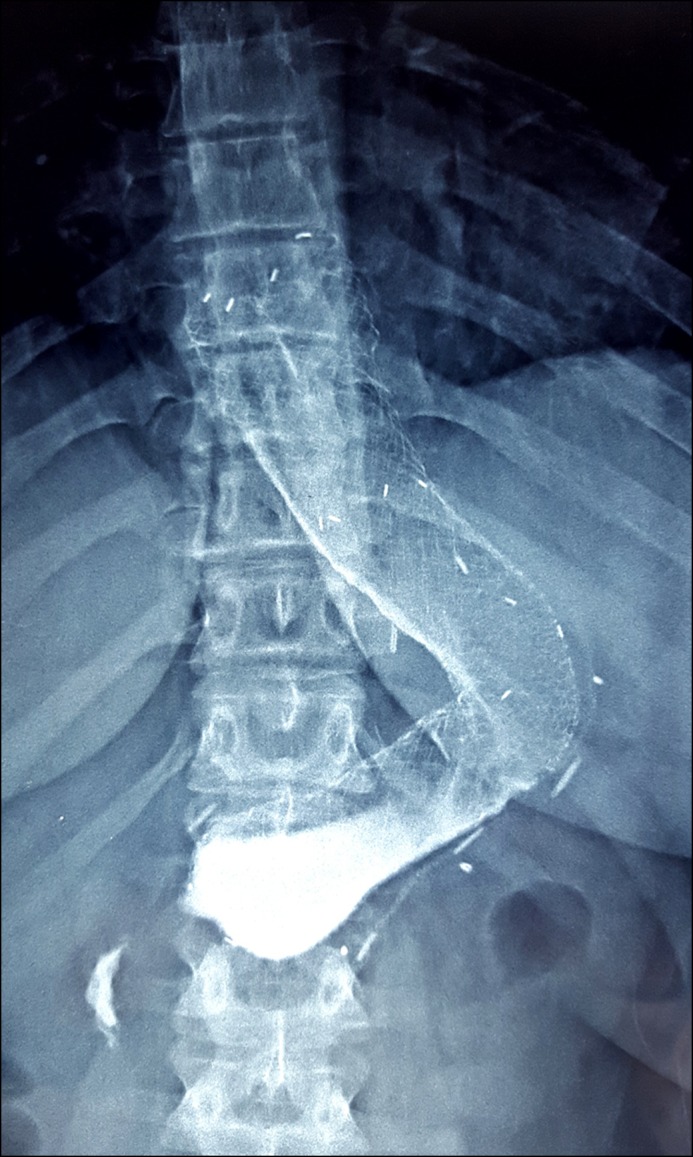
The Gastroseal stent inside gastric sleeve.
The main features of this stent are described here. First, a distal rolled-in and curved edge provides for gentle contact against the duodenal wall. Second, the upper edge is curved inward slightly to reduce the traumatic effect of the upper edge on the esophageal wall; this is intended to reduce the risk of esophageal ulceration and stricture formation. Third, the nitinol mesh design is of the conventional braided type on the top and bottom segments only (5 cm each), but the middle segment is composed of knitted nitinol mesh with a negligible axial force; this is intended to provide high conformability to the angulated lumen, which should yield improved patient tolerance. Fourth, the knitted mesh is longitudinally compressible; this, together with the negligible axial force, significantly diminishes the pressure applied by the distal edge on the duodenal/antral wall. Fifth, the stent’s length (24 cm) ensures complete coverage of the leak area and prevents the reflux of luminal contents from reaching the leak. Finally, a large diameter (shaft 28 mm; edges 36 mm) ensures a complete seal and reduces the risk of migration (Figure 2).
Figure 2.
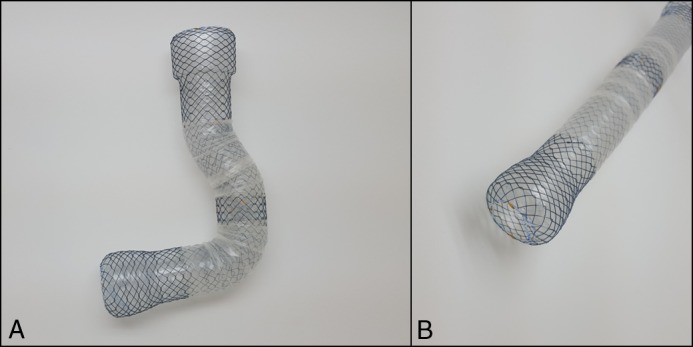
(A) The knitted mesh allows complete flexibility and conformity with a gastric sleeve anatomy. The upper edge is curved inward slightly and the lower edge is completely round to reduce trauma to the esophagus and duodenal bulb, respectively. (B) The distal edge of the Gastroseal stent is rounded to reduce trauma to the duodenal bulb or antrum.
Oral fluid diet was resumed 48 hours after the procedure, and the patient reported only minimal pain and nausea. The patient was discharged 2 days later on a semi-solid diet and oral proton-pump inhibitor. Five weeks later, the stent was removed endoscopically. The stent was visualized in place, and the endoscope passed easily through the stent, revealing no evident trauma or ulceration at the distal end as usually is seen with large stents (Video 1). The stent was removed by a forceps revealing complete healing of the previously described fistula (Figure 3). The patient was discharged on the same day, and after a follow-up of 6 months there is no evidence of leak recurrence or stricture formation, and the patient is eating normally.
Figure 3.

Gastroesophageal junction leak (left); healed leak after stent removal (right).
Discussion
The universally reported drawback of fully covered expandable metal stents is the frequent occurrence of migration, with an incidence of up to 67% in some series.3,6 To reduce migration, several techniques have been proposed, including fixation with clips, suturing the stents in place, or using partially covered stents that embed in the esophageal wall.7-9 Clip fixation has proven ineffective, while suturing—although effective—is associated with unreasonable costs.7,8 Partially covered stents have been advocated by several investigators, but their use is associated with some drawbacks including difficult extraction, stricture formation, and small caliber that allows food content to reflux and reach the leak site.9
Over the last few years we have used ultra-large, fully covered stents to treat bariatric surgery leaks.4 Our experience was encouraging with a significantly reduced risk of migration (18%) and a leak healing rate of 82%.4,10 However, we have noted the frequent occurrence of some adverse events, namely deep ulcers at the distal edge and duodenal perforations and bleeding, severe intolerance necessitating premature stent removal, and recurrent esophageal strictures.10 We have developed the Gastroseal™ stent design to deliver the advantages of the large size and avoid the drawbacks of large stents. From our experience with large stents, we noted that the main factor opposing migration is the large distal end being impacted against the antral or duodenal wall. Having a large yet rounded and smooth distal end of the stent maintains this impaction against the wall, thus reducing the possibility of migration in an atraumatic way. In this particular patient, no ulcers were visualized at the distal end after 5 weeks of implantation; in our previous experience ulcers were detected nearly universally when other large stents were used.4,10 The patient also tolerated the large stent very well, and she was able to depend solely on enteral nutrition throughout the stent period with no evident migration. These findings provide a proof-of-concept that the stent design, particularly the distal edge, is significantly nontraumatic.
In conclusion, we present our first experience with a bariatrics-specific stent with antimigration properties and an atraumatic design to reduce the risk of complications. Although the technical development of a rounded nitinol mesh was challenging, we believe it is a major breakthrough in stent design. We also believe the concept could be applied to other gastrointestinal stents to reduce the traumatic effect of stents.
Disclosures
Author contributions: H. Shehab wrote the manuscript and is the article guarantor. H. Mikhail revised the manuscript.
Financial disclosure: H. Shehab is a consultant for M.I.Tech (Seoul, South Korea), who provided the stent used in this case. The funding source had no role in the design, practice or analysis of this report.
Informed consent was obtained for this case report.
References
- 1.Burgos AM, Braghetto I, Csendes A, et al. Gastric leak after laparoscopic-sleeve gastrectomy for obesity. Obes Surg. 2009;19:2–7. [DOI] [PubMed] [Google Scholar]
- 2.Gould JC, Garren MJ, Starling JR. Lessons learned from the first 100 cases in a new minimally invasive bariatric surgery program. Obes Surg. 2004;14:18–25. [DOI] [PubMed] [Google Scholar]
- 3.van Boeckel PG, Sijbring A, Vleggaar FP, Siersema PD. Systematic review: Temporary stent placement for benign rupture or anastomotic leak of the oesophagus. Aliment Pharmacol Ther. 2011;33:292–301.11. [DOI] [PubMed] [Google Scholar]
- 4.Shehab H, Hakky S, Gawdat K. An endoscopic strategy combining mega stents and over-the-scope clips for the management of post-bariatric surgery leaks and fistulas (with video). Obes Surg. 2016;26:1–8. [DOI] [PubMed] [Google Scholar]
- 5.van den Berg MW, Kerbert AC, van Soest EJ, et al. Safety and efficacy of a fully covered large-diameter self-expanding metal stent for the treatment of upper gastrointestinal perforations, anastomotic leaks, and fistula. Dis Esophagus. 2016;29:2–9. [DOI] [PubMed] [Google Scholar]
- 6.Orive-Calzada A, Calderón-García Á, Bernal-Martínez A, et al. Closure of benign leaks, perforations, and fistulas with temporary placement of fully covered metal stents. Surg Laparosc Endosc Percutan Tech. 2014;24:28–36. [DOI] [PubMed] [Google Scholar]
- 7.Bège T, Emungania O, Vitton V, et al. An endoscopic strategy for management of anastomotic complications from bariatric surgery: A prospective study. Gastrointest Endosc. 2011;73:38–44. [DOI] [PubMed] [Google Scholar]
- 8.Sharaiha RZ, Kumta NA, DeFilippis EM, et al. A large multicenter experience with endoscopic suturing for management of gastrointestinal defects and stent anchorage in 122 patients. J Clin Gastroenterol. J Clin Gastroenterol. 2016;50:88–92. [DOI] [PubMed] [Google Scholar]
- 9.Swinnen J, Eisendrath P, Rigaux J, et al. Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc. 2011;73:0–9. [DOI] [PubMed] [Google Scholar]
- 10.Shehab H, Abdallah E, Gawdat K, Elattar I. Large bariatric-specific stents and over-the-scope clips in the management of post-bariatric surgery leaks. Obes Surg. 2018;28:15–24. [DOI] [PubMed] [Google Scholar]


