Abstract
Autophagy is a catabolic process by which eukaryotic cells eliminate cytosolic materials through vacuole-mediated sequestration and subsequent delivery to lysosomes for degradation, thus maintaining cellular homeostasis and the integrity of organelles. Autophagy has emerged as playing a critical role in the regulation of liver physiology and the balancing of liver metabolism. Conversely, numerous recent studies have indicated that autophagy may disease-dependently participate in the pathogenesis of liver diseases, such as liver hepatitis, steatosis, fibrosis, cirrhosis, and hepatocellular carcinoma. This review summarizes the current knowledge on the functions of autophagy in hepatic metabolism and the contribution of autophagy to the pathophysiology of liver-related diseases. Moreover, the impacts of autophagy modulation on the amelioration of the development and progression of liver diseases are also discussed.
Keywords: autophagy, selective autophagy, liver, liver disease, hepatitis, steatosis, fibrosis, cirrhosis, hepatocellular carcinoma
1. Introduction
Autophagy is an evolutionarily conserved process that catabolizes intracellular components through lysosomes to recycle nutrients for supplying energy and regenerating organelles [1,2]. Several types of stress and damage stimuli, such as the deprivation of nutrients, the damage of organelles, the unfolding and aggregation of proteins, and tissue injury have been shown to induce autophagy [3,4]. Interference with the precise and appropriate process of autophagy may contribute to the pathogeneses of various human diseases, such as liver-associated diseases, neurodegenerative diseases, cancer, and infectious diseases [5,6]. In the past few decades, the homeostatic role of autophagy has emerged in the regulation of liver physiology through promoting the degradations of macromolecules and organelles to support the balance of energy as well as the metabolism and regeneration of organelles [7,8,9]. Additionally, autophagy has been indicated as a disease-associated factor that is modulated in the liver cells of people with liver-related diseases, and it contributes to the development and progression of various liver diseases, including hepatitis, steatosis, fibrosis, cirrhosis, and hepatocellular carcinoma [7,10,11,12]. Autophagy protects liver cells against injury and cell death by eliminating the damaged organelles and proteins that are introduced in those with liver-associated diseases. Conversely, autophagy could also act as an alternative pathway that promotes the development and progression of liver diseases. Most importantly, the modulation of autophagy has been extensively proved to alter the occurrence and outcome of liver-related diseases, implying that it represents a novel therapeutic target for the design of new and effective therapies to prevent and treat liver diseases. In this paper, we summarize the current knowledge on the functional role of autophagy in liver physiology and address how autophagy is regulated by liver-associated diseases to become involved in the prevention or promotion of disease occurrence and pathogenesis.
2. Overview of Autophagy
The term autophagy is derived from the Greek words for auto (“self”) and phagy (“eating”). The concept of autophagy was initially devised from the observation of vesicle-like dense bodies that encompass cytoplasmic organelles, such as mitochondria and endoplasmic reticulum (ER), in differentiated kidney tissue in mice and glucagon-perfused rat hepatocytes viewed using transmission electron microscopy (TEM) [13,14,15,16]. These double-membraned dense bodies were shown to be associated with the lysosome-mediated degradative process [13,14,15,16]. Subsequently, this process was termed “autophagy” by de Duve, the 1974 Nobel Laureate in Physiology or Medicine, at the Ciba Symposium on Lysosome in 1963 [17,18]. In the late 1960s, several studies, through morphological and biochemical characterization, revealed that glucagon induces the formation of autophagic vacuoles, which are influenced by lysosomes and lysosomal enzymes [19,20]. Despite the effects of glucagon, the deprivation of amino acids and growth factors was indicated to trigger autophagy [21,22,23,24]. From the 1970s to the 1990s, numerous studies demonstrated that the induction of autophagy enhanced the degradation of long-lived proteins, leading to a decrease in amino acid levels [24,25,26]. Additionally, the molecular signaling underlying autophagy initiation and the autophagy inhibitors generated from these findings, such as 3-methyladenine (3-MA) and okadaic acid, have been identified and characterized [24,27,28,29,30,31,32,33]. The membrane source of support for a phagophore for the emergence of autophagic vacuoles was first described in the late 1980s [34] and was further characterized in the 1990s [35,36,37,38,39,40,41]. The comprehensive isolation and molecular cloning of autophagy-related genes (ATGs) were initiated by Ohsumi, who was the 2016 Nobel Laureate in Physiology or Medicine for work on the genetic screening of temperature-sensitive, autophagy-defective mutants in Saccharomyces cerevisiae [42,43,44]. Ohsumi identified 15 autophagy-defective mutants that can be respectively complemented by the corresponding ATGs, which function in the entire process of yeast autophagy and degradation [43]. Analogous to yeast, the functional ATGs involved in autophagy in humans and other eukaryotes were also identified and characterized [45,46,47,48,49]. To date, approximately 40 ATGs have been identified [49,50,51], most of which have been evolutionarily conserved among almost all eukaryotes. Furthermore, the nomenclature for ATGs across different species of eukaryotes has been unified [45,46,47,48,49].
2.1. Three Modes of Autophagy
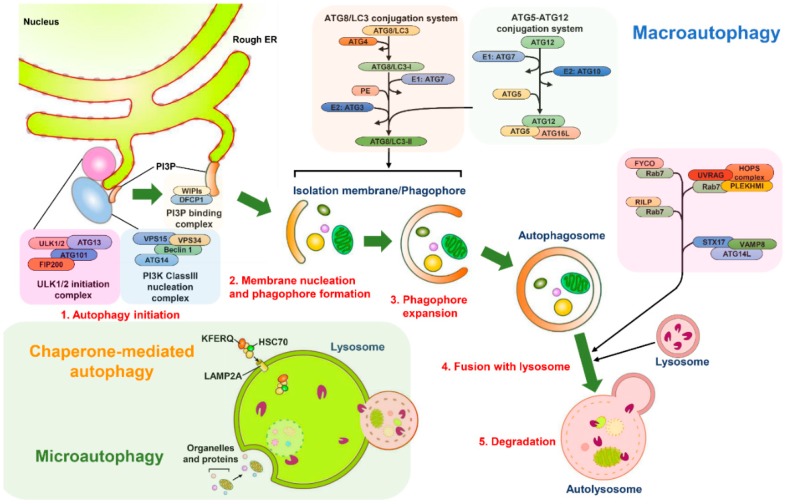
Three types of autophagy have been defined according to the mechanism used for the delivery of the intracellular components to lysosomes for degradation: microautophagy, chaperone-mediated autophagy (CMA), and macroautophagy (Figure 1) [1,2]. Microautophagy was defined in mammalian cells through TEM observation of a lysosomal membrane rearranged to have a protrusion and arm-like structure to wrap the cytoplasmic portion into the lumen of the lysosome for decomposition (Figure 1) [17,52,53]. Microautophagy not only randomly engulfs the intracellular materials to instigate degradation (so-called nonselective microautophagy) but also selectively eliminates specific organelles (defined as selective microautophagy) in yeast cells [54,55]. Although core ATG proteins and the endosomal sorting complexes required for transport (ESCRT) machinery are required for microautophagy [56,57,58,59,60], information about how microautophagy is precisely induced and the detailed molecular mechanisms underlying the process of microautophagy remain limited. Similarly, the functional role of microautophagy in human health and diseases is also largely unknown and requires further investigations. CMA is characterized by a selective elimination process in which the degradative substrates that contain the pentapeptide “Lys-Phe-Glu-Arg-Gln” (KFERQ) motifs are specifically recognized by a cytosolic chaperone, namely, the heat-shock cognate protein of 70 kDa (HSC70); these motifs are transported into the lysosomal lumen through the lysosomal membrane protein 2A (LAMP2A)-mediated docking process (Figure 1) [61,62]. Multiple types of stress have been shown to induce CMA, such as nutrient starvation, DNA damage, hypoxia, oxidative stress, and metabolic imbalance [63,64,65,66,67,68]. Crucially, CMA plays a role in the replenishment of amino acids and ATP in cells that have undergone prolonged starvation [64,69], the regulation of lipid metabolism [70,71], the reprogramming of gene transcription [72,73,74], the activation of immune responses [75,76], the control of cell cycle progression [68,77], and the control of ageing [78,79]. Accordingly, the malfunctioning of CMA has emerged as a contributor to numerous human diseases, such as tumorigenesis [80,81,82,83], neurodegenerative disorders [84,85,86,87,88,89], liver diseases [90,91], and lysosomal storage disorders [92]. In macroautophagy (hereafter referred to as autophagy), the membrane rearrangement process leads to the formation of an autophagosome, a double-membranous vacuole that sequestrates the cytoplasmic components and delivers them to lysosomes for degradation (Figure 1) [2,93]. Several types of stress, such as the starvation of nutrients, damage of organelles, aggregation of proteins, and invasion of pathogens, have been shown to induce autophagy [3,4]. In the past decade, autophagy has emerged as a “double-edged sword” in the pathogenesis of a variety of human diseases, including neurodegenerative diseases [94,95,96,97], cancer [98,99], cardiovascular diseases [100,101,102], ageing [94,99,100,101,102,103,104], infectious diseases [105,106], and metabolic disorders [98,107,108,109,110]. Therefore, targeting autophagy could be a feasible strategy for treating human diseases.
Figure 1.
Schematic diagram of the autophagy pathway. There are three main types of autophagy: microautophagy, chaperone-mediated autophagy (CMA), and macroautophagy. The process of microautophagy undergoes an invagination and scission process of the lysosomal membrane that sequestrate the cytosolic portions into the lysosomal lumen for degradation. In CMA, the heat-shock cognate protein of 70 kDa (HSC70) recognizes the substrates that contain the pentapeptide “Lys-Phe-Glu-Arg-Gln” (KFERQ) motifs and deliver them to lysosomes through interacting with lysosomal membrane protein 2A (LAMP2A). Macroautophagy is a stepwise vacuole biogenesis process that initiates with the nucleation of the membrane to form a phagophore, the expansion of a phagophore to the closure of autophagosomes, and the fusion of autophagosomes with lysosomes to mature autolysosomes. Finally, the engulfed intracellular components are eliminated within the autolysosomes. When the cells are deprived of nutrients, the inhibition of the mammalian target of rapamycin (mTOR) complex induces the translocation of the unc-51 like-kinase (ULK1/2) complex (ULK1/2, autophagy-related gene (ATG) 13, RB1-inducible coiled-coil 1 (RB1CC1, also known as FIP200), and ATG101) to the membrane nucleation site. The translocated ULK1/2 complex in turn recruits and activates the class III phosphatidylinositol-3-OH kinase (class III-PI(3)K complex, including Vps34/PI(3)KC3, Vps15, Beclin 1, and ATG14) to produce phosphatidylinositol-3-phosphate (PtdIns(3)P). Subsequently, PtdIns(3)P recruits the double-FYVE-containing protein 1 (DFCP1) and WD-repeat domain PtdIns(3)P-interacting (WIPI) family proteins to promote the formation of the isolation membrane (IM)/phagophore. Two ubiquitin-like (UBL) conjugation systems underlie the expansion and elongation of the phagophore to form mature autophagosomes. The ubiquitin conjugation enzyme 1 (E1) ATG7 activates ATG12 through a thioester bonding with ATG12, and then ATG12 is transferred to ATG10 enzyme 2 (E2). ATG12 is finally conjugated to ATG5, forming an ATG5-ATG12 complex, which in turn interacts with ATG16L to form an ATG12-ATG5-ATG16L complex. To successfully conjugate phosphatidylethanolamine (PE) to ATG8/LC3 family proteins, the ATG8/LC3 family proteins are cleaved by the cysteine protease ATG4 to expose the C-terminal glycine residues, generating the ATG8/LC3-I. Then, ATG8/LC3-I is covalently linked to PE to form the lipidated form of LC3 (ATG8/LC3-II) via an enzyme cascade of ATG7 E1 and ATG3 E2. The fusion of autophagosomes and lysosomes relies on the interactions between the small GTPase Ras-related protein 7 (Rab7) and cytoskeleton-associated factors, the FYVE and coiled-coil domain-containing 1 (FYCO1) and Rab-interacting lysosomal protein (RILP). Additionally, UV radiation resistance-associated (UVRAG), the homotypic fusion and protein sorting (HOPS) complex, pleckstrin homology domain-containing protein family member 1 (PLEKHM1), and protein complex containing syntaxin 17 (STX17), vesicle-associated protein 8 (VAMP8), and synaptosome-associated protein 29 (SNAP29) are involved in the maturation process of autolysosomes.
2.2. Stepwise Process of Vacuole Biogenesis for Autophagy
Autophagy undergoes a stepwise process for vacuole biogenesis that involves the initial nucleation and elongation of the isolation membrane (IM)/phagophore, the closure of autophagosomes, and the fusion of autophagosomes with lysosomes to form autolysosomes (Figure 1) [111,112,113]. Numerous organelles [112,113,114], including the ER [115,116], Golgi apparatus [117], mitochondria [118], recycling endosome [119,120], plasma membrane [121], and mitochondria-associated ER membrane (MAM) [122] support the membrane source for the emergence of the IM/phagophore. At the initial stage, the IM/phagophore that originates from a particular membrane structure, which is often derived from the ER, expands to form a double-membraned and enclosed autophagosome (Figure 1) [114,123,124,125]. Subsequently, mature autophagosomes fuse with the lysosome to generate autolysosomes in which the interior materials are degraded by lysosomal proteases (Figure 1) [124,126,127,128].
Most ATGs (also known as core ATGs) and the signaling molecules and vesicle-trafficking factors involved in other cellular pathways are coordinately required for the completion of the entire autophagic process (Figure 1) [93,129,130]. The starvation of nutrients in cells leads to the suppression of the mammalian target of rapamycin (mTOR), a serine/threonine protein kinase required for controlling cell growth [131,132]. The repression of mTOR results in the translocation of the unc-51 like-kinase (ULK) complex (contains ULK1/2, ATG13, RB1-inducible coiled-coil 1 (RB1CC1, also known as FIP200) and ATG101( from the cytosol to a certain domain reconstituted from the ER (Figure 1) [133,134]. This translocation of the ULK complex in turn recruits the class III phosphatidylinositol-3-OH kinase (PI(3)K) complex (class III-PI(3)K, including Vps34/PI(3)KC3, Vps15, Beclin 1, and ATG14) to the ER membrane-derived domain (Figure 1) [130,135,136] and enhances the activity of the PI(3)K complex through the phosphorylation of Vps34/PI(3)KC3 [137]. PI(3)K in turn produces phosphatidylinositol-3-phosphate (PtdIns(3)P), leading to the recruitment of double-FYVE-containing protein 1 (DFCP1) and WD-repeat domain PtdIns(3)P-interacting (WIPI, the mammalian orthologue of ATG18) family proteins to promote the organization of an ER-associated omegasome structure (also termed IM/phagophore) (Figure 1) [130,135,136,138,139]. Moreover, two multi-spanning membrane proteins, namely ATG9a and vacuole membrane protein 1 (VMP1), are critical to the initial biogenesis of autophagosomes. The ATG9a-enriched vesicles that are trafficked from the trans-Golgi network (TGN) to the ER deliver the lipid bilayers required for autophagosome formation [140,141,142]. ER-associated VMP1 interacts with Beclin 1 of the PI(3)K complex, thereby facilitating the generation of PtdIns(3)P required for the assembly of IM/phagophore [143,144,145]. The subsequent expansion and enclosure of the IM/phagophore into a mature autophagosome requires two ubiquitin-like (UBL) conjugation systems (Figure 1) [146,147,148,149]. The ATG5-ATG12 conjugate is formed by the ATG7 (E1) and ATG10 (E2) enzymatic cascade (Figure 1). This conjugate then forms a trimeric complex with ATG16L (an ATG12-ATG5-ATG16L complex) [146,147,150,151,152]. The other conjugation is that of the phosphatidylethanolamine (PE)-conjugated ATG8 family proteins (including the microtubule-associated protein 1 light chain 3 (LC3) and gamma-aminobutyric acid receptor-associated protein (GABARAP) subfamilies). After protein translation, the C-terminal region of ATG8/LC3 family proteins are immediately processed by ATG4 family proteases to form ATG8/LC3-I. Then, ATG7 enzyme 1 (E1) and ATG3 enzyme 2 (E2) confer the conjugation of the ATG8/LC3-I to generate PE-ATG8/LC3, sometimes called ATG8-LC3-II (also known as lipidated ATG8-LC3) (Figure 1) [153,154,155]. PE-ATG8/LC3 participates in the elongation of the autophagosomal membrane [156] and the tethering and membrane fusion of autophagic vacuoles [149]. Notably, ATG5-ATG12 may act as an E3-like enzyme to promote the lipidation of ATG8/LC3 [157,158], thereby promoting the formation of autophagosomes. Additionally, the sphingolipid microdomains, so-called lipid rafts, were indicated to play roles in the morphogenesis of autophagic vacuoles [159]. The fluorescence resonance energy transfer (FRET) and co-immunoprecipitation (co-IP) studies showed that ganglioside GD3, a paradigmatic raft constituent, interacts with PI3P and LC3-II on the immature autophagosomal membrane [159]. Also, the interactions between GD3 and WIPI/ATG18 family proteins as well as autophagy and Beclin 1 regulator 1 (AMBRA1) were shown in MAM raft-like microdomains [160]. Downregulation of GD3 level by gene knockdown of ST8SIA1/GD3 synthase and alteration of sphingolipid metabolism by fumonisin B1 was demonstrated to inhibit autophagic process [159] and interfere with the interaction of AMBRA1 with calnexin at MAM [160], implying that MAM-associated lipid rafts function in the biogenesis of autophagosomes.
The mature autophagosome fuses with a lysosome, forming an autolysosome in which acidic proteases degrade the sequestrated materials to recycle their nutrients. The autophagosome–lysosome fusion process relies on the multilayered actions of protein–protein interactions, microtubule-mediated transport, and membrane fusion events [123,125,126,128]. The actions of the microtubule ensures the precise transport of the autophagosome to the lysosome for fusion [128,161,162]. The small GTPase Ras-related protein 7 (Rab7) located on the autophagosomal membrane interacts with FYVE and coiled-coil domain-containing 1 (FYCO1) and Rab-interacting lysosomal protein (RILP), two effectors that are respectively linked to kinesin and dynactin in microtubules [163,164,165,166,167], enabling the movements of the autophagosomes on microtubules (Figure 1). Apart from microtubules, the histone deacetylase 6 (HDAC6)-induced remodeling of F-actin and the formation of the F-actin network also promote autophagosome–lysosome fusion in the quality control autophagy-mediated removal of aggregated proteins rather than starvation-induced autophagy [168]. In addition to bridging the transport of autophagosomes on microtubules, Rab7 located on late endosomes and lysosomes stimulates autophagosome–lysosome fusion through recruiting several effectors of this action, including the pleckstrin homology domain-containing protein family member 1 (PLEKHM1) and the homotypic fusion and protein sorting (HOPS) complex (Figure 1) [153,154]. PLEKHM1 contains an LC3-interacting motif that can bind to ATG8 family proteins located on the autophagosomal membrane and concomitantly interacts with Rab7 as well as the HOPS complex, thereby facilitating the fusion of autophagosomes and lysosomes (Figure 1) [169]. Additionally, the PI(3)K complex-associated UV radiation resistance-associated gene (UVRAG) binds to the HOPS complex via Vps16 to induce Rab7 GTPas activity and trigger autophagosome–lysosome fusion [136,170,171]. Notably, the binding of Rubicon to the PI(3)K protein complex reciprocally interferes with the fusion of autophagosomes and lysosomes [136]. Another protein complex, containing ATG14L, syntaxin 17 (STX17), synaptosome-associated protein 29 (SNAP29), and vesicle-associated membrane protein 8 (VAMP8), also stimulates autophagosome–lysosome fusion, presumably through the membrane tethering and fusion process (Figure 1) [172,173]. Recently, ATG8 family proteins were shown to be mainly active during autophagosome–lysosome fusion rather than autophagosome biogenesis at the initial stage of autophagy by recruiting PLEKHM1 in PTEN-induced putative kinase 1 (PINK1)/Parkinson’s disease protein (Parkin)-mediated autophagic clearance of mitochondria (so called mitophagy) and starvation autophagy [174]. In addition to acting at the biogenesis of autophagosomes [159], lipid rafts have emerged as a regulator of autolysosome maturation [159,160]. The interaction between GD3 and lysosome-associated membrane protein-1 (LAMP1) in the autolysosomal membrane as demonstrated by FRET, co-IP, and TEM assays indicated that GD3-enriched lipid rafts could induce membrane remodeling to promote the morphogenesis of autolysosomes and increase autophagic flux [160].
After degradation within autolysosomes, the nutrient-fed-reactivation of mTOR suppresses autophagy initiation and concomitantly initiates autophagic lysosome reformation (ALR), thereby terminating autophagy [175]. Related studies have implied that spinster (spin), a lysosomal efflux permease, is required for ALR formation [176]. Recently, the Cullin 3-Kelch-like protein 20 (KLHL20) ubiquitin ligase was also shown to participate in autophagy termination by promoting the turnover of the ULK1 and Vps34 complexes [177]. Nevertheless, the detailed molecular mechanism underlying the biogenesis of autophagic vacuoles within the entire autophagy process is not comprehensively understood and further investigations are required.
2.3. Selective Autophagy and Cargo Recognition
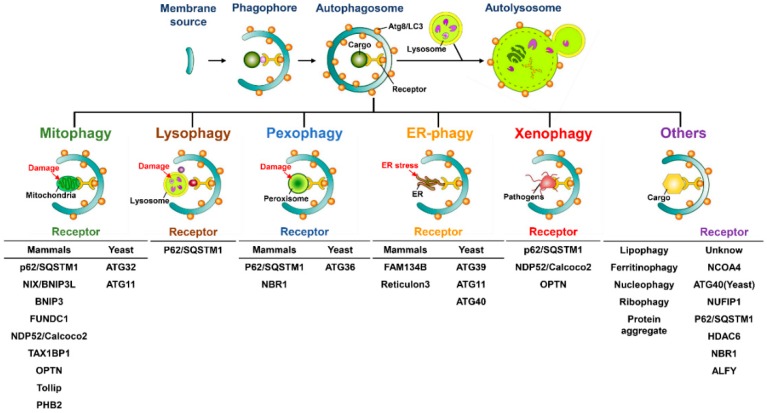
Autophagy has been considered to be a bulky and nonselective degradative process; however, a growing body of literature has indicated that autophagy may selectively sequestrate specific cargos, including organelles and proteins, to induce degradation. This is termed “selective autophagy” [178,179,180]. The concept of selective autophagy was first described in 1973, in a study that showed that a diabetogenic dose of alloxan or streptozotocin induces selective autophagy to degrade β-granules in intermediate cells in the pancreas of rats [181]. At the initial stage of selective autophagy, the specific cargo receptors recognize the degradative cargos that are tagged through polyubiquitination or additional adaptor proteins and then deliver them into the autophagosome through the interaction of cargo receptors with ATG8 family proteins located on the autophagosomal membrane [182,183,184,185]. Numerous cargo receptors of selective autophagy have been identified and characterized, including the neighbor of BRCA1 (NBR1), calcium-binding and coiled-coil domain-containing protein 2 (Calcoco2, also known as NDP52), p62/sequestosome 1 (SQSTM1), and optineurin (OPTN), all of which contain LC3-interacting regions (LIRs) to bind ATG8 family proteins, thus engulfing the cargos into autophagosomes (Figure 2) [184,185,186]. In addition to eliminating degradative substrates through LIR-containing cargo receptors, the potential ATG8-interacting motifs (AIMs) and GABARAP-interacting motifs (GIMs) have been recently found to regulate selective autophagy within ATGs and other cellular proteins [187,188,189,190]. For example, the Saccharomyces cerevisiae ATG19 was shown to directly interact with ATG5 through AIMs, and that interaction recruits the ATG5-ATG12-ATG16L trimeric complex, thus enhancing the lipidation of ATG8/LC3 to promote the local biogenesis of autophagosomes to sequestrate the cargos [191].
Figure 2.
Different modes of selective autophagy. Degradation of selective autophagy involves the specific interactions between the ATG8/LC3-interacting regions (LIRs) within cargo receptors and ATG8/LC3 located onto autophagosomal membrane. The ubiquitination of degradative cargos or associated ligand proteins is often required for recognition by cargo receptors. Selective autophagy has been shown to eliminate different kinds of organelles and proteins, including damaged mitochondria (mitophagy), injured lysosomes (lysophagy), damaged peroxisomes (pexophagy), stressed ER (ER-phagy), and infectious pathogens (xenophagy), through specific cargo receptors in yeast and mammalian cells as indicated. Also, lipid droplets (LDs) ferritin, nuclei, ribosomes, and protein aggregates are also degraded by selective autophagy via the identified cargo receptors and other unknown adaptor proteins.
Regarding the maintenance of the organelle integrity in eukaryotic cells, selective autophagy plays a homeostatic role in the selective elimination of damaged organelles, termed organellophagy [178,180,192], which provides the recycled nutrients for the regeneration of mitochondria, peroxisomes, the ER, lipid droplets (LDs), ribosomes, lysosomes, and nuclei (Figure 2). Numerous stimuli, such as hypoxia [193,194], the accumulation of reactive oxygen species (ROS) [195,196,197], and mitochondrial depolarization [198,199,200], can result in the fission, depolarization, and damage of mitochondria. Mitochondrial damage triggers selective autophagy to degrade the harmful mitochondria in a process known as mitophagy [201,202]. Mitophagy is often initiated without adequate cleavage of PINK1 by presenilin-associated rhomboid-like protein (PARL) within the inner mitochondrial membrane of damaged mitochondria, thus suppressing the degradation of PINK1 [203,204]. This outcome in turn leads to the accumulation of PINK1 on the outer mitochondrial membrane, thereby phosphorylating ubiquitin at serine 65 and then recruiting the ubiquitin enzyme 3 (E3) ligase Parkin [198,199,200,205,206,207]. Subsequently, Parkin ubiquitinates the mitochondrial proteins onto the outer mitochondrial membrane [198,199,200,205,208], thus recruiting specific cargo receptors, such as Calcoco2/NDP52 and OPTN, for the removal of mitochondria through autophagy (Figure 2) [202,209]. The translocation of these cargo receptors also induces the local concentration of phagophore-organization effectors, including DFCP1 and WIPI/ATG18 family proteins, for autophagosome maturation proximal to the damaged mitochondria [209]. Additionally, TANK binding kinase 1 (TBK1) participates in the cargo recognition process of mitophagy by phosphorylating p62/SQSTM1 at serine residue 403 and OPTN at serine residues 177, 473, and 513 [210,211,212]. Despite the PINK1/Parkin-induced ubiquitination of damaged mitochondria, several outer mitochondrial membrane proteins, including FUN14 domain-containing 1 (FUNDC1), BCL2/adenovirus E1B 19 kDa protein-interacting protein 3 (BNIP3), BCL2/adenovirus E1B 19 kDa protein-interacting protein 3-like (BNIP3L), and yeast ATG32, also activate mitophagy in a ubiquitin-independent manner (Figure 2) [213,214,215,216,217]. Recently, numerous studies have identified novel cargo receptors for mitophagy, such as prohibitin 2 (PHB2) and Toll-interacting protein (Tollip) (Figure 2) [218,219]. In contrast, the deubiquitination (DUB) of mitochondrial proteins onto the outer membrane of mitochondria by DUB enzymes USP30 and USP35 antagonizes mitophagy [220,221].
Selective autophagy promotes the turnover of other intracellular organelles. The specific cargo receptors that confer the elimination of these organelles are also identified and characterized. To degrade oxidized and damaged peroxisomes through pexophagy, yeast ATG36 and mammalian NBR1 and p62/SQSTM1 are required to target the degradative peroxisomes to autophagosomes (Figure 2) [222,223,224,225]. Numerous kinases, such as yeast Hrr25 and mammalian ataxia-telangiectasia-mutated (ATM), induce the phosphorylation of these two cargo receptors, thus promoting the delivery of peroxisomes to the autophagosomal membrane [226,227]. The polyubiquitination of several peroxisomal (PEX) membrane proteins, such as PEX5 and the 70-kDa PEX membrane protein (PMP70), facilitates the recognition of damaged peroxisomes by cargo receptors [227,228].
The targeting of a stressed ER to degradation through ER-phagy involves the biological activities of ATG39, ATG11, and ATG40 [229] in yeast cells; the family with sequence similarity 134, member B (FAM134B) (Figure 2); and reticulon family proteins in mammals [230,231]. ATG39 and ATG11 also participate in the selective degradation of yeast nuclei, termed nucleophagy (Figure 2) [229]. The clearance of protein aggregates by selective autophagy is achieved through the p62/SQSTM1- and HDAC6-mediated recognition of Lys63 (K63)-linked poly-ubiquitination of aggregated proteins [168,232,233,234]. Moreover, NBR1 and autophagy-linked FYVE (ALFY) could cooperate with p62/SQSTM1 to degrade protein aggregates through selective autophagy (Figure 2) [235,236,237,238]. The injured lysosomes have recently been reported to be removed by lysophagy, which begins with the recruitment of galectin-3 and LC3 onto lysosomal membranes, which are subsequently recognized by p62/SQSTM1 and delivered to the autophagosome for degradation (Figure 2) [239,240]. Similarly, selective autophagy has emerged as playing a pivotal role in the clearance of ribosomes, termed ribophagy (Figure 2) [241,242], and in the catabolism of LDs for maintaining metabolic homeostasis (Figure 2) [243,244].
In addition to organellophagy, the cargo receptors of selective autophagy can eliminate specific proteins and invading pathogens. The nuclear receptor coactivator 4 (NCOA4) has been recently shown to interact with ATG8 family proteins and to target ferritin heavy and light chains for autophagic degradation, thus modulating the intracellular level of iron (Figure 2) [245,246]. The turnover of ferritin through selective autophagy, termed ferritinophagy, has been implicated in the regulation of erythropoiesis and DNA replication in blood cells [247,248]. The elimination of infectious pathogens by xenophagy represents the host’s first-line defense in restricting microbial infections [249,250,251]. Pexophagy involves the engulfment of invading pathogens by p62/SQSTM1-, Calcoco2/NDP52-, and OPTN-mediated recognition processes and delivery to the autophagosome for degradation (Figure 2) [106,252,253]. The phosphorylations of p62/SQSTM1 (at serine residues 349 and 403) and OPTN (at serine 177) promote the clearance of infecting pathogens through pexophagy [253,254,255,256]. Taken together, selective autophagy not only maintains cellular homeostasis by removing damaged organelles but also acts as a host defensive mechanism to counteract pathogen infection.
2.4. Autophagy as an Alternative Cell-Death Pathway
Autophagy (“self-eating”) has been considered a stress-responsive, survival mechanism to protect cells against apoptosis (“self-killing”, type I cell death) [257,258,259]. Autophagy is often activated by the inhibition of apoptosis. For instance, simultaneous gene knockout of BAX and BAK, two BCL2 family proteins involved in cell apoptosis in mice was shown to activate autophagy to counteract etoposide (an inhibitor of topoisomerase-2)-induced cell death [260]. Reciprocally, apoptosis can be activated by inhibiting autophagy. Interference with autophagy by gene silencing and pharmacological inhibitors in nutrient-starved cells was shown to trigger cell apoptosis [261]. The specific gene knockout of ATG5 in neuron cells and T cells in mice was demonstrated to increase apoptotic cell death [262,263]. However, autophagy confers an alternative route to promote cell death, known as type II cell death under some specific cellular conditions [264,265]. For instance, human immunodeficiency virus (HIV) infection leads to autophagy activation to trigger apoptotic cell death of CD4/CXCR4-expressing T cells [266]. The inhibition of HIV Env-induced autophagy by gene knockdown and pharmacological inhibitors was demonstrated to interfere with cell apoptotic death [266]. In spite of apoptosis, autophagy was also indicated to promote necrotic cell death [267]. Autophagy was demonstrated to be activated by caspase inhibition to promote cell death through the accumulation of ROS and degradation of catalases [267]. This caspase inhibition-induced cell death could be reversed by interference with autophagy by siRNAs against ATGs and autophagy inhibitors [267]. Notably, the enhancement of cellular autophagy by the Tat-Beclin1 peptide was specifically demonstrated to trigger the “autosis” cell death pathway, which is mediated by the Na+, K+-ATPase pump and is characterized by the convolution of nuceli at the early-stage and focal swelling of the perinuclear space at the late-stage [268,269]. Besides the autophagy-inducing Tat-Beclin1 peptide, starvation and in vivo cerebral hypoxia-ischemia were also shown to induce autotic cell death [268,269]. These studies together indicate that autophagy not only adapts to stresses to avoid cell death but also induces diverse types of cell death pathways to kill cells when cells no longer circumvent certain stimuli.
3. Regulation and Functional Roles of Autophagy in Liver Physiology
3.1. The Leading Discovery of Autophagy in Liver Tissue
Hepatocytes in liver tissue were initially revealed to contain autophagic vacuoles. In the early 1960s, Ashford et al. first demonstrated that glucagon perfusion in rats can induce the formation of polymorphic dense bodies in liver cells (Table 1) [14]. These dense bodies were shown to sequestrate the fragmented and morphologically abnormal mitochondria, which were associated with autolysis triggered by the glucagon-related protein catabolic process (Table 1) [14]. Similarly, the treatment of rat livers with the detergent Triton also led to the formation of dense bodies (known as cytolysomes) that exhibit two patterns: one consists of double-membraned vacuoles containing mitochondria and ER membrane fragments and the other consists of single-membrane vesicles in which the engulfed materials are degraded (Table 1) [15]. Soon thereafter, glucagon was revealed to be as an activator of autophagy in liver cells (Table 1) [19,20,270], which were standardized for monitoring autophagy. De Duve and Deter first observed that glucagon administration triggers an increase in lysosomal size, which could be related to the formation of autophagic vacuoles in the rat livers (Table 1) [19]. After the biochemical fractionation of lysosomes, their study further revealed that glucagon induction upregulates acidic phosphatase as well as cathepsin D in lysosomes and also increases the fragility of lysosomes in Rat liver (Table 1) [19]. In a subsequent study that combined biochemical fractionation and TEM, Deter and colleagues revealed by a morphological quantification that glucagon-induced autophagic vacuoles represent a substantial portion of lysosomes in liver homogenates (Table 1) [20]. Their study implied that hepatic lysosomes are involved in the biogenesis of autophagic vacuoles and thus provide the main source of acidic proteases for the degradation of sequestrated interior materials (Table 1) [20]. Moreover, two types of glucagon-triggered autophagic vacuoles in the liver were further specified: type I vacuoles are predominantly double-membraned vacuoles that contain the ER, ribosomes, and ground cytoplasm and type II vacuoles are larger than type I vacuoles and are composed of a single limiting membrane, in which the sequestrated ER and cytoplasm are broken down (Table 1) [270]. Taken together, these studies not only indicate that hepatic autophagy may present a novel degradative process that eliminates the intracellular components in the liver but also provide evidence that lysosomes participate in autophagy to support proteolytic enzymes.
Table 1.
Summary of autophagy in liver physiology.
| Experimental Model | Characteristics of Autophagy | Function of Autophagy | References |
|---|---|---|---|
| Rat liver (Perfusion of glucagon) |
Electron micrograph of polymorphic dense bodies | Sequestration of deformed mitochondria that is associated with glucagon-related catabolic process | [14] |
| Rat liver (Intravenous injection of Triton WR-1339) |
Electron micrograph of polymorphic dense bodies that includes single- and double-membraned vesicles (termed cytolysomes) | Degradation and degeneration of mitochondria in Triton-treated hepatic cells | [15] |
| Rat liver (Intravenous injection of glucagon) |
Biochemical fractionation of lysosomes and autophagic vacuoles | Association with lysosomes and enrichment of lysosomal acidic enzymes within autophagic vacuoles for protein degradation in the glucagon-stimulated liver cells | [19] |
| Rat liver (Intravenous injection of glucagon) |
|
|
[20] |
| Rat liver (Intravenous injection of glucagon) |
|
|
[270] |
| Rat liver (Intraperitoneal injection of dimethylnitrosamine (DMNA)) |
|
|
[272] |
| Rat liver (Long-term starvation) |
Electron micrograph of autophagic vacuoles that engulf organelles |
|
[273,274,275] |
| Rat liver (Intraperitoneal injection of glucagon and cycloheximide) |
Electron micrograph of autophagic vacuoles | The correlation of autophagic vacuoles formation with the rate of protein synthesis and the level of energy | [276,277,278] |
| Mouse liver (Intravenous injection of lysine acetylsalicylate |
Electron micrograph of single- and multiple-membranous autophagic vacuoles | The engulfment of intracellular components within autophagic vacuoles that may protect the lysine acetylsalicylate-treated liver cells against injury | [279] |
| Rat liver (Hypothermia) |
Electron micrograph of autophagic vacuoles that sequestrate enlarged mitochondria and disorganized endoplasmic reticulum (ER) | The elimination of intracellular organelles by hypothermia-induced autophagic vacuoles in hepatocytes | [280] |
| Rat liver (Intraperitoneal injection of vinblastine) |
Electron micrograph of autophagic vacuoles that engulf organelles | Degradation of intracellular organelles within autophagic vacuoles | [281] |
| Rat liver (Perfusion of amino acids-deprived medium) |
Electron micrograph of autophagic vacuoles that engulf organelles | Maintenance of intracellular amino acids in hepatocytes and recycling of nutrients | [21] |
| Rat liver (Perfusion of amino acids-deprived medium) |
Electron micrograph of autophagic vacuoles that engulf organelles | Decreased the intracellular amounts of glucogenic amino acids by autophagy | [25] |
|
|
Degradation of intracellular organelles and endogenous proteins, which is inhibited by methylated adenosine derivatives and refeeding | [24,30,282] |
| Rat liver |
|
Degradation of intracellular organelles and endogenous proteins, which is inhibited by insulin, 3-methyladenine (3-MA), vinblastine, and amino acids | [22,23,287,288,289,290,291,292,293,294] |
| Newborn rat hepatocytes | Electron micrograph of autophagic vacuoles that is closely related to the degradation of fetal-type glycogen | Degradation of fetal-type glycogen in the neonatal period | [295] |
|
Autophagic degradation of RNA and proteins in liver, which is inhibited by chloroquine and amino acids | [296] | |
| Rat liver | Electron micrograph and biochemical fractionation of lysosomes and autophagic vacuoles | Degradation of proteasomes by lysosomes and autophagic vacuoles | [297] |
| Rat liver | Restriction of ischemic liver injury by inhibition of autophagy | [298] | |
|
Enhancement of cell survival of carcinogen-treated hepatocytes by reduced autophagy | [299] | |
| Primary rat hepatocytes | Electron micrograph of autophagic vacuoles | Increased the intracellular iron pool by autophagic turnover of ferritin and iron-containing proteins | [300] |
| Liver specimens of patients | Electron micrograph of autophagic vacuoles | Promotion of cell death in anorexia nervosa livers of patients by starvation-induced autophagy | [301] |
| Rat hepatoma H4IIE cells | Support of amino acids from autophagic proteolysis of endogenous proteins to the regulation of translational effectors | [302] | |
| Wild type and liver-specific knockout of ATG7 mice |
|
Maintenance of blood glucose and amino acids levels by hepatic autophagy | [303] |
| Primary human and mouse hepatic stellate cells |
|
Involvement of enhanced autophagic flux in the activation of hepatic stellate cells | [304] |
| Rat liver | Degradation of cathepsin family enzymes (B, H, and L) | Reduced lysosomal proteolysis by suppression of autophagy in regenerating liver | [305] |
| Rat liver |
|
Involvement of autophagy in the degeneration of hepatocytes of liver grafts | [306] |
| Wild type and liver-specific Tet-off-LAMP2A transgenic mice | Electron micrograph of CMA-mediated autophagic process | The maintenance of liver function and protection against liver damage by hepatic CMA | [79] |
| Mouse hepatocytes (In vivo and in vitro ischemia and reperfusion) |
|
Amelioration of liver damage and restoration of mitochondrial function in liver after ischemia and reperfusion | [307] |
|
|
Elimination of components of MDBs by rapamycin-induced autophagy | [308,309] |
|
|
|
[243,244,310,311] |
|
|
|
[312,313,314,315,316,317,318] |
|
|
|
[319,320,321,322,323] |
|
|
|
[321,324] |
3.2. The Role of Autophagy in Balancing Metabolism and Sensing Stresses in the Liver
The regulation of autophagy in liver physiology and the modulation of autophagy by liver injury were discovered in the early 1970s [271,272,273,274]. The study by Pfeifer first revealed the role of autophagy in the decomposition of glycogen in liver atrophy [273]. Long-term starvation has been shown to induce hepatic autophagy, correlating with cell atrophy in rat livers (Table 1) [274,275]. These studies suggested that hepatic autophagy may detect malnutrition in the liver as well as liver damage, instantly supporting the refueling of nutrients through degradation. Accordingly, the formation of autophagic vacuoles was shown to be energy-dependent and correlated with the rate of protein synthesis (Table 1) [276,277], alteration of metabolites (Table 1) [278,279,280], and interference with cytoskeleton organization (Table 1) [281]. In the late 1970s, stress and amino acid deprivation were demonstrated to trigger autophagy in hepatic cells (Table 1) [21,25,280]. This autophagic proteolytic effect induced by the deprivation of nutrients in hepatocytes can be inhibited by the refeeding of nutrients and autophagy inhibitors (Table 1) [24,30,282], indicating that the status of nutrient supplies plays a detrimental role in autophagy activation in the liver. These studies collectively imply that autophagy acts as a regulator that senses changes in the metabolism and alterations of energy in the liver.
The induction of hepatocellular necrosis by dimethylnitrosamine (DMNA) can increase the number and size of autophagic vacuoles in the period beyond the onset of cell necrosis (Table 1) [271,272], suggesting that autophagy might be activated to counteract cell death in the liver. At the same time, numerous studies have shown that the smooth membrane of the ER can contribute to the membranous structure that supports autophagosome biogenesis in liver cells [283,284,285,286,287], leading to a new paradigm for understanding the membrane resource for developing autophagosomal membranes. Collectively, these studies indicate that hepatic autophagy could be activated by numerous stimuli, such as nutrient starvation, metabolism imbalance, and liver injury, to promote the maintenance of metabolic homeostasis.
3.3. Turnover of Macromolecules through Autophagy in the Liver
In the late 1970s, autophagy was first shown to degrade glycogen and to participate in the selective elimination of organelles in the liver (Table 1) [23]. In line with this study, biochemical and morphological studies have, together, demonstrated that hepatic autophagy plays a major role in protein degradation and the degeneration of organelles through the formation of autolysosomes (Table 1) [23,25,287,288,289,290,291,292,293,294]. The functional roles of autophagic degradation in the liver were implicated in the turnover track of intracellular macromolecules, such as the degradation of fetal-type glycogen in the neonatal period (Table 1) [295], the destruction of damaged organelles by virus infection (Table 1) [325], the selective degradation of RNA and proteins through the deprivation of amino acids (Table 1) [296], and the elimination of the ubiquitin–proteasomal pathway through long-term starvation (Table 1) [297]. Additionally, hepatic autophagy is involved in multiple cell surveillance mechanisms, including the regulation of ischemic liver injury (Table 1) [298], the growth suppression of carcinogen-treated hepatocytes (Table 1) [299], the modulation of the iron pool and sensitivity to oxidative stress (Table 1) [300], and the regulation of cell death in the damaged livers of patients with anorexia nervosa (Table 1) [301]. Conversely, autophagy plays critical roles in the integration of metabolic pathways by regulating the supply of amino acids for effective translation in hepatoma cells (Table 1) [302], the balancing of blood glucose and amino acid levels (Table 1) [303], and the activation of hepatic stellate cells (Table 1) [304]. Moreover, autophagy participates in the regulation of lysosomal proteolysis in liver regeneration (Table 1) [305], the degeneration of transplanted livers in rats (Table 1) [306], the maintenance of hepatic function in the aged liver (Table 1) [79], and the suppression of age-dependent ischemia in injured livers (Table 1) [307]. Taken together, these results indicate that autophagy acts as a protector in physiologically balancing liver metabolism and maintaining liver function and growth.
3.4. Selective Degradation of Organelles through Autophagy in the Liver
In the past few decades, numerous studies have indicated that autophagy participates in the catabolism of intracellular compartments in the liver, including Mallory–Denk bodies (MDBs) [308,309,326], LDs [70,71,243,244,310,311,327,328], peroxisomes [312,313,314,315,316,317,318,329,330], mitochondria [320,321,322,323], and the ER [324,331] (Table 1). A biochemical fractionation study indicated that a considerable portion of several types of organelles was sequestrated within autophagic vacuoles in rat hepatocytes (Table 1) [332,333], implying the functional roles of autophagy in the elimination of intracellular organelles in the liver. MDBs are cytosolic hyaline inclusions that were discovered in the hepatocytes of patients with alcoholic hepatitis in 1911 by Mallory [334] and further characterized in mouse livers by Denk in the late 1970s [335,336]. Several intracellular components are enclosed in MDBs, including keratins, chaperones, protein degradation machinery that contains ubiquitin and p62/SQSTM1, and phosphoproteins [337]. MDBs have been observed in various liver diseases, such as alcoholic steatohepatitis, nonalcoholic steatohepatitis (NASH), nonalcoholic fatty liver disease (NAFLD), and hepatocellular carcinoma (HCC) [337,338,339]. Harada et al. first demonstrated that rapamycin-induced autophagy may mediate the turnover of bortezomib-induced MDBs in in vitro cell cultures and in vivo mouse models [308,309], supporting autophagy′s role in the clearance of cytoplasmic inclusions.
LDs are the primary organelles that store neutral lipids, including cholesterol ester and triglycerides (TG), and serve as a reservoir for energy, particularly for the liver [340,341,342]. The aberrant accumulation of lipids in LDs has been evinced in numerous metabolic disorders in the liver, such as hepatic steatosis, NASH, and NAFLD, leading to global health burdens in modern society (Table 1) [328,340,342,343]. The role of autophagy in LD dynamics was originally defined in the analysis by Fujimoto et al. of apolipoprotein B (ApoB) degradation (Table 1) [311]. By combining biochemical fractionation and microscope-based approaches, the authors posited that autophagy may promote the degradation of ApoB, which specifically occurs around the surface of LDs in hepatocytes (Table 1) [311]. Subsequently, Singh et al. showed that interference with autophagy by the knockdown of the ATG5 gene expression increased TG accumulation and inhibited the β-oxidation of free fatty acids (FFAs) and degradation of TG in hepatocytes (Table 1) [244]. Their TEM-based ultrastructural study further indicated that LDs are delivered into autophagic vacuoles for degradation, which is enhanced by nutrient starvation (Table 1) [244]. Their study first uncovered the role of autophagy in the catabolism of LDs, (e.g., “lipophagy”). Another study further confirmed that starvation upregulated lysosomal lipase activity in the autophagic fraction of the liver to promote lipid degradation (Table 1) [310]. In contrast, ATG7 deficiency in mouse hepatocytes was shown to impede the formation of LDs (Table 1) [243]. The specific localization of lipidated-LC3 onto the surface of LDs in starved mouse hepatocytes suggested that the ATG8/LC3-lipidation process might be involved in the biogenesis of hepatic LDs (Table 1) [243]. In line with this study, another report demonstrated that mammalian ATG2 plays a crucial role in the morphogenesis and dynamics of LDs (Table 1) [344]. In addition, autophagy was shown to inhibit ethanol-induced steatosis in mouse livers and to protect liver cells from ethanol-triggered hepatotoxicity (Table 1) [345]. In addition to macroautophagy, CMA was recently indicated to promote the degradation of LD-associated proteins perilipin 2 (PLIN2) and perilipin 3 (PLIN3) to control LDs biogenesis [70]. Moreover, the 5′-AMP-activated protein kinase (AMPK)-induced phosphorylation of PLIN2 was shown to promote its interaction with HSC70, a chaperone of CMA, and thus facilitate the degradation of PLIN2, thereby recruiting lysosomes and cytosolic lipases to catabolize LDs [71]. More importantly, this specific form of LD degradation through autophagy, the so-called lipophagy, was reported to participate in thyroid hormone-induced LD catabolism (Table 1) [346,347].
The sequestration of peroxisomes within autophagic vacuoles was initially observed in a study showing that antilipolytic agent-treated rat livers that contained enhanced autophagic vacuoles engulfed peroxisomes and downregulated the activities of peroxisomal enzymes (Table 1) [312,315], suggesting that autophagy participates in peroxisome degradation. Analogously, autophagic vacuoles have also been reported to sequestrate peroxisomes in the hepatocytes of patients with chronic hepatitis B virus (HBV) who received transplantation and immunosuppressive therapy (Table 1) [329]. Subsequently, amino acid deprivation-induced autophagy was suggested to selectively degrade peroxisomes in hepatocytes isolated from clofibrate-treated rats, and this degradation was completely inhibited by the administration of 3-MA (Table 1) [316]. Furthermore, several other studies have demonstrated that autophagy is involved in the elimination of excess peroxisomes, thus prohibiting the uncontrolled proliferation of peroxisomes in the liver [36,38,313,314,317,330]. Moreover, the selective degradation of peroxisome autophagy, termed “pexophagy”, may regulate peroxisome proliferator-activated receptor α (PPARα) target genes and the β-oxidation of FFAs to prevent hepatic steatosis and tumorigenesis in the liver (Table 1) [348] and acute liver failure induced by inflammation (Table 1) [349].
Mitochondria and the ER are the intracellular organelles that were originally detected in autophagic vacuoles in the late 1950s and early 1960s [13,14,15,16]. The concepts underpinning the degradation of mitochondria through autophagy was derived from the observation that the rate of mitochondria removal was selectively and positively correlated with the formation of autophagic vacuoles in rat livers [23,287]. Subsequently, studies have shown that autophagic vacuoles contain the mitochondrial enzymes of the liver [37,38,350,351,352], further indicating that hepatic autophagy selectively eliminates mitochondria. The autophagic degradation of mitochondria in hepatocytes was further demonstrated to introduce mitochondrial injury, thus promoting the pathogenesis of alpha (1)-antitrypsin (α1-AT) deficiency-induced liver injury that was highly associated with chronic liver diseases (Table 1) [353,354,355]. Komatsu et al. first demonstrated that the genetic knockout of ATG7 in mice interfered with autophagosome biogenesis in livers in which deformed mitochondria had accumulated (Table 1) [356], suggesting that hepatic autophagy plays a major role in mitochondria degradation. The targeting of mitochondria to autophagic degradation was enhanced in the livers of aged mice (Table 1) [321]. Moreover, the impairment of hepatic autophagy was involved in mitochondrial dysfunction in ischemia/reperfusion (I/R)-triggered mouse liver injuries (Table 1) [357]. By contrast, the autophagy-mediated degradation of mitochondria was related to acute liver cell damage in patients with anorexia nervosa (Table 1) [301]. The selective degradation of autophagy, termed “mitophagy”, was demonstrated to underlie mitochondrial remodeling in rat hepatocytes [323]. Mitophagy reduces ethanol-induced toxicity in mouse livers (Table 1) [345], regulates interferon (IFN)-mediated antiviral responses (Table 1) [358], protects liver cells against acetaminophen-induced hepatotoxicity (Table 1) [359], rescues liver function in efavirenz-induced mitochondrial dysfunction (Table 1) [360], suppresses the development of HCC (Table 1) [361], and prevents liver damage in patients with NAFLD (Table 1) [362,363]. Overall, autophagy not only plays a crucial role in the balance of diverse metabolic pathways but also promotes the elimination of damaged organelles and protects liver cells from injury, thereby maintaining cellular homeostasis.
4. Autophagy: A Friend or Foe in Liver Diseases?
4.1. Liver Injury
The correlation of autophagy and liver injury was first described in studies showing that DMNA-induced liver damage activates the formation of autophagic vacuoles (Table 2) [272]. Subsequently, the formation of autophagic vacuoles was detected in the injured liver cells of mice treated with lysine acetylsalicylate (Table 2) [279], in the livers of mice exposed to acute stressors (Table 2) [364], and in the injured hepatocytes of rats infected with lethal Escherichia coli (Table 2) [365]. Numerous physiological and pathological stimuli in the Rat liver were implicated in the elevated autophagy-mediated protein degradation (Table 2) [366]. Alpha (1)-antitrypsin deficiency has been considered as a major cause of liver injury in patients with chronic hepatitis and HCC (Table 2) [367,368,369]. Autophagy has been extensively demonstrated to be activated in the injured liver of α1-AT-deficient mice and may participate in the disposal of mutant α1-ATZ aggregated proteins (Table 2) [353,354,370]. The role of autophagy in the clearance of α1-ATZ mutated proteins was further proven by genetic studies showing that the gene knockout of ATG5 in mice leads to an increased abundance of insoluble α1-ATZ [371] and that the deficiency of ATG6 and ATG14 inhibits α1-ATZ degradation in yeast cells (Table 2) [372]. Conversely, the induction of autophagy by rapamycin may reduce intrahepatic α1-ATZ aggregation and related liver injury in mice (Table 2) [373]. These studies collectively indicate that autophagic degradation plays a pivotal role in the elimination of α1-ATZ aggregates in the cytoplasm to prevent these aggregated proteins from impairing the ubiquitin–proteasomal pathway and to protect liver cells from organelle damage and cell death (Table 2) [355,374,375,376].
Table 2.
Summary of autophagy in liver injury.
| Experimental Model | Characteristics of Autophagy | Function of Autophagy | References |
|---|---|---|---|
| Rat liver (Intraperitoneal injection of DMNA) |
|
|
[272] |
| Mouse liver (Intravenous injection of lysine acetylsalicylate |
Electron micrograph of single- and multiple-membranous autophagic vacuoles | The engulfment of intracellular components within autophagic vacuoles that may protect the lysine acetylsalicylate-treated liver cells against injury | [279] |
| Rat liver (Stressors: fasting, cortisol injection, reserpine injection, restraint, spinal cord transection, etc.) |
Electron micrograph of single- and multiple-membranous autophagic vacuoles | Protection of liver cells against multiple stress responses | [364] |
| Rat liver (Lethal Escherichia coli) |
Electron micrograph of autophagic vacuoles | Association of hepatic autophagy in Escherichia coli-induced liver injury | [365] |
| Rat hepatocytes (Calcium ionophore, microtubule active agents, and hepatotoxins) |
Detection of autophagic degradation of endogenous proteins | Decreased autophagic degradation by liver injury | [366] |
|
|
|
[353,354,355,371,372,373] |
|
|
|
[356,377,378,379,380,381] |
| Liver specimens of liver-related diseases patients |
|
Association of increased autophagy with the chemotherapy-injured liver after ischemic preconditioning | [382,383] |
| Mouse hepatocytes (In vivo and in vitro ischemia and reperfusion) |
|
Amelioration of liver damage and restoration of mitochondrial function in liver after ischemia and reperfusion | [307] |
|
|
|
[345,384] |
| Primary mouse hepatocytes (LPS; Cecal ligation and performation) |
|
|
[385] |
|
|
Protection of fatty acids-induced lipotoxicity and liver injury by autophagy | [386] |
| Chang liver cells (PEI treatment) |
|
Enhancement of the PEI-induced cytotoxicity in liver cells by autophagy | [387] |
| Wild type and liver-specific knockout of ATG7 mice (APAP treatment) |
|
|
[388] |
| Rat liver (Cold ischemia/warm reperfusion; liver transplantation) |
|
|
[389] |
| Liver specimens of patients | Electron micrograph of autophagic vacuoles | Promotion of cell death in anorexia nervosa livers of patients by starvation-induced autophagy | [301] |
|
Immunofluorescence analysis of GFP-LC3-labeled punctate structure |
|
[390] |
|
|
|
[391] |
| Isolated hepatocytes from wild type and caspase 1−/− mice |
|
|
[392] |
| Isolated mouse hepatocytes and Kupffer cells | Detection of lipidation of ATG8/LC3 |
|
[393] |
| Mouse liver | Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[394] |
| Isolated mouse hepatic stellate cells | Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[395] |
| Rat liver (Ischemia/reperfusion) |
Detections of lipidation of ATG8/LC3 |
|
[396] |
| Mouse liver (LPS/D-galactosamine (GalN)) |
Detections of lipidation of ATG8/LC3 | Induced ER stress and autophagy at the early stage of LPS/GalN-induced liver injury | [397] |
| Mouse liver (Ischemia/reperfusion; fasting) |
Detections of lipidation of ATG8/LC3 |
|
[398] |
| Wild type and liver-specific knockout of ATG7 mice | Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[399] |
| Mouse liver (Ischemia/reperfusion; fasting) |
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[349] |
| Wild type and NRBF2 knockout mice |
|
|
[400] |
| Mouse liver (Cecal ligation and puncture) |
Immunofluorescence analysis of ATG8/LC3 |
|
[401,402,403] |
| Wild type and liver specific HIF-1β knockout mice |
|
|
[404] |
| Mouse liver (Ischemia/reperfusion) |
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[405] |
| Mouse liver (Ischemia/reperfusion) |
|
|
[406] |
| Mouse liver (Ischemia/reperfusion) |
|
|
[407] |
| Mouse liver (LPS/D-GalN) |
|
|
[408] |
| Wild type and Cd38−/− mice (LPS/D-GalN) |
|
|
[409] |
| Wild type and liver specific KLF6 knockout mice |
|
|
[410] |
Evidence for the physiological significance of autophagy in the clearance of the cytoplasmic inclusion body was uncovered by the study of Komatsu et al. on ATG gene knockout in mice experiments (Table 2) [356,377]. The genetic deletion of ATG7 in mice resulted in the accumulations of ubiquitin- and p62/SQSTM1-containing protein aggregates and abnormal mitochondria in liver cells and caused liver injury (Table 2) [356], implying that autophagy protects liver cells from damage by promoting the clearance of aggregate-prone proteins. In addition, the gene knockout of p62/SQSTM1 in mice livers represses the accumulation of aggregated proteins in such livers and attenuates liver injury, indicating that autophagy prohibits damage of the liver through the p62/SQSTM1-mediated disposal of cytoplasmic inclusion proteins (Table 2) [377]. Moreover, the accumulated p62/SQSTM1 through autophagy deficiency was shown to interact with Kelch-like ECH-associated protein 1 (Keap1) and interfere with the Cullin3-Kepa1 ubiquitin E3 ligase-mediated proteasomal degradation of nuclear factor erythroid 2-related factor 2 (Nrf2), thereby stabilizing and translocating Nrf2 into the nucleus to transcriptionally activate antioxidant genes expressions (Table 2) [378]. Liver dysfunction in autophagy-deficient mice was further exacerbated by an additional knockout of Keap1 (Table 2) [378]. The upregulation of the p62/SQSTM1-containing aggregate and induction of Nrf2-targeted genes were detected in a major group of HCC cell lines (Table 2) [379]. The induction of liver injury through autophagy deficiency may be associated with the upregulation of oxidation stress, as demonstrated by the high levels of oxidative stress-inducible proteins detected in mouse livers lacking the ATG7 gene expression (Table 2) [380]. Moreover, a reduction of oxidative damage by hepatic autophagy represses ischemic liver injury (Table 2) [381]. These aforementioned studies indicate that autophagic degradation in the liver eliminates aggregate-prone proteins to prevent liver injury. Furthermore, the deregulation of autophagy may induce liver damage and progressive liver diseases.
However, autophagy was shown to be activated in chemotherapy-injured livers to limit the necrotic cell death of hepatocytes (Table 2) [382,383]. Moreover, it was implicated in the repression of age-dependent ischemia and reperfusion-induced liver injury in mice (Table 2) [307]. Autophagy was also suggested to reduce acute ethanol-induced hepatotoxicity in mouse livers by promoting damage to mitochondria through mitophagy (Table 2) [345,384]. Sepsis and lipopolysaccharide (LPS)-induced autophagy via heme oxygenase-1 (HO-1) signaling also protects hepatocytes from death (Table 2) [385]. Moreover, autophagy is also involved in the inhibition of lipotoxicity in the hepatocytes of injured livers (Table 2) [386], in the enhancement of cytotoxicity in polyethyleneimine (PEI)-triggered liver damage (Table 2) [387], and in the protection of livers against acetaminophen (APAP)-induced hepatotoxicity (Table 2) [359,388]. These results collectively suggest a protective role of autophagy in the suppression of liver injury caused by various stimuli. By contrast, other studies have shown the opposite effect of autophagy in liver dysfunction, such as its contribution to cell death during liver graft dysfunction (Table 2) [389] and its involvement in liver cell death in patients with anorexia nervosa (Table 2) [268,301].
Numerous signaling pathways have been shown to activate autophagy during liver injury, such as insulin-like growth factor-1 (IGF-1) signaling [390]; gene transfer of transcription factor EB (TFEB) activity [391]; caspase 1 activation [392]; activation of NACHT, LRR, and PYD domains-containing protein 3 (NLRP3) inflammasome [393]; suppression of protein kinase C (PKC) downstream signaling [394]; and ER stress [395,396,397] (Table 2). However, the NAD-dependent deacetylase sirtuin-1 (Sirt1)-dependent downregulation of circulating high mobility group protein B1 (HMGB1) [398,399], activation of PPARα [349], nuclear receptor binding factor 2 (NRBF2)-mediated activation of the PI(3)K complex [400], AMPK activation [401,402,403], hypoxia-inducing factor-1α (HIF-1α) [404], retinoic acid receptor α (RARα) [405], HO-1 signaling [406,407], suppression of c-jun-N-terminal kinase (JNK) [408], nicotinic acid adenine dinucleotide phosphate (NAADP)-mediated calcium signaling [409], and Krüppel-like factor 6 (KLF6)-mediated transcription [410] were shown to participate in the autophagy-mediated protection against liver injury (Table 2). Nevertheless, these studies collectively indicate that autophagy plays a critical role in protecting liver cells against different types of liver injury. Furthermore, they demonstrate that autophagy represents a potential target for the development of new therapeutic agents for treating liver diseases.
4.2. Steatosis and Fatty Liver Diseases
Autophagy promotes LD catabolism (Table 3) [70,71,244,310,311,346,347], and the components of the autophagic machinery were shown to participate in the biogenesis of LDs (Table 3) [243,344]. These studies, thus, imply that hepatic autophagy has a homeostatic role in the regulation of lipid metabolism to prevent liver steatosis. Moreover, it is also a therapeutic target for developing novel therapies for curing fatty liver diseases [11,12,328,411]. An earlier report showed that interference with autophagic degradation in the fatty livers of rats was correlated with tissue necrosis and the limitation of mitochondrial injury (Table 3) [412]. Ding et al. provided the first evidence that the repression of autophagy in the liver by pharmacological inhibitors and RNA interference resulted in the accumulation of LDs and induced apoptosis of hepatocytes of mice (Table 3) [345], suggesting that autophagy attenuates the formation of alcoholic fatty liver. In line with this finding, another study demonstrated that the cytochrome P450 2E1 (CYP2E1) mediated the upregulation of oxidative stress-suppressed autophagy, thus leading to lipid accumulation in cultured liver cells (Table 3) [413]. The inhibition of autophagy by a thymidine analog was shown to lead to lipid accumulation, increased ROS, and hepatic dysfunction (Table 3) [414]. Autophagy was also demonstrated to be activated by exendin-4 to combat dysfunctional ER stress and lipid accumulation in unsaturated fatty acid-induced NAFLD mice (Table 3) [386,415], indicating that autophagy prevents steatosis under NAFLD conditions. The ablation of starvation-induced autophagy by the liver-specific deletion of Vps34, the kinase of the PI(3)K complex in mice, led to the development of hepatic steatosis and hepatomegaly (Table 3) [416]. Additionally, the tumor suppressing p73-mediated transcription of ATG5 promotes autophagy activation to regulate lipid metabolism in hepatocytes (Table 3) [417]. The deletion of the acyl-CoA-dependent lysocardiolipin acyltransferase (ALCAT1), an enzyme required for mitochondrial bioenergetics, was proved to promote autophagosome formation and to prevent NAFLD and related metabolic disorders in mice (Table 3) [418]. Transcriptional factor 3 (TFE3) induced lipophagy to alleviate hepatic steatosis (Table 3) [419]. The sterol regulatory element-binding proteins (SREBPs)-patatin-like phospholipase domain-containing enzyme 8 (PNPLA8) axis was demonstrated to activate autophagy to decrease hepatic steatosis in mice with NAFLD (Table 3) [420]. Interference with the ApoB synthesis has been indicated to induce ER stress to trigger autophagy, thus preventing hepatic steatosis in mice (Table 3) [421]. Rubicon was shown to repress the entire autophagic process to induce lipid accumulation and to trigger cell apoptosis in mice with NAFLD (Table 3) [422]. Saturated fatty acids-induced sirtuin 3 (SIRT3) impaired autophagy to contribute to lipotoxicity in hepatocytes (Table 3) [423]. Recently, the suppression of transcription factor EB (TFEB)-mediated lysosome biogenesis and autophagy was demonstrated to promote chronic ethanol uptake-induced hepatic steatosis and liver injury (Table 3) [424].
Table 3.
Summary of autophagy in steatosis and fatty liver diseases.
| Experimental Model | Characteristics of Autophagy | Function of Autophagy | References |
|---|---|---|---|
|
|
|
[243,244,310,311] |
|
|
|
[346,347] |
| Rat liver (Carbohydrate-rich diet; hypothermic reconditioning) |
Detection of the lipidation of ATG8/LC3 |
|
[412] |
|
|
|
[345,384] |
| Human hepatoma cell line, HepG2 E47 cells |
|
|
[413] |
|
|
|
[414] |
| Primary human hepatocytes |
|
|
[415] |
|
|
|
[386] |
| Wild type and liver-specific knockout of Vps34/PI(3)KC3 mice |
|
|
[416] |
|
|
|
[417] |
| Wild type and ALCAT1 knockout mice |
|
|
[418] |
| Human hepatocyte, L02 cells |
|
|
[419] |
| Mouse liver | Detection of the lipidation of ATG8/LC3 |
|
[420] |
| Wild type and apobec-1 knockout mice |
|
|
[421] |
|
|
|
[422] |
| Wild type and SIRT3 knockout mice |
|
|
[423] |
|
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[424] |
|
|
|
[425] |
| Wild type and G6Pase−/− mice |
|
|
[427] |
| Mouse liver |
|
|
[429] |
|
Detection of the lipidation of ATG8/LC3 |
|
[428] |
| Human hepatoma, Huh7 cells |
|
|
[430] |
| Wild type and Parkin knockout mice |
|
|
[431] |
| Wild type and Drp, Parkin, p62/SQSTM1, Nrf2, and Opa1-knockout mice |
|
[362] | |
| Wild type and liver-specific knockout of ATG7 mice | Detection of the lipidation of ATG8/LC3 |
|
[433] |
| Wild type and liver-specific knockout of FIP200/RB1CC1 mice |
|
|
[432] |
|
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[434] |
| Human hepatoma, HepG2 cells |
|
|
[363] |
| Wild type and ob/ob mice |
|
|
[435] |
|
|
|
[436] |
| Liver specimens of NAFLD patients | Electron micrograph of autophagic vacuoles |
|
[437] |
The enhancement of autophagy using pharmacological approaches has been shown to alleviate liver steatosis and injury in alcoholic and nonalcoholic fatty livers in mice (Table 3) [425,426]. The gluscose-6-phosphatase (G6Pase) deficiency-induced von Gieke’s disease (GSDIa), a common glycogen storage disorder, has been shown to impair autophagy, leading to hepatic steatosis in those with NAFLD (Table 3) [427]. Furthermore, the pharmacological elevation of autophagy indicated that it could reverse lipid accumulation and liver damage (Table 3) [427]. Trehalose, a naturally occurring disaccharide, was shown to inhibit solute carrier 2A to activate autophagy, thus preventing hepatic steatosis (Table 3) [428]. The activation of autophagy by rapamycin was shown to attenuate ethanol-LPS-induced hepatic steatosis and injury (Table 3) [429]. Taken together, these studies evince that the induction of autophagy through pharmacological approaches represents a feasible therapeutic approach for treating fatty liver diseases. In spite of ethanol- and NAFLD-induced hepatic steatosis, autophagy is known to protect hepatocytes from hepatitis C virus (HCV)-induced liver steatosis in patients with chronic HCV (Table 3) [430]. In addition to autophagy, the specific deletion of CMA in mice leads to hepatic glycogen and induced liver steatosis, implying the role of age-dependent CMA in balancing liver metabolism by promoting lipid catabolism [69]. Parkin-mediated mitophagy was reported to protect against alcohol-induced mitochondrial dysfunction, hepatic steatosis, and liver injury in mice (Table 3) [431]. However, a recent study demonstrated that the p62/SQSTM1-mediated recruitment of Cullin-Kepa1-Rbx ubiquitin E3 ligase ubiquitinates mitochondria and induces mitophagy to alleviate liver injury in mice with NAFLD (Table 3) [362]. The liver-specific deletion of FIP200/RB1CC1 was reported to suppress lipid accumulation, to decrease lipogenic gene expression, and to exacerbate LPS and endotoxin-induced liver injury in an NAFLD mouse model (Table 3) [432].
In contrast to the role of autophagy in attenuating liver steatosis and injury, a series of studies has shown that autophagy also promotes the pathogenesis of steatohepatitis diseases. Autophagy in Kupffer cells was shown to be suppressed by hepatic steatosis, and that enhances an inflammatory response to endotoxins (Table 3) [433]. Additionally, chronic alcohol intake was reported to suppress hepatic autophagy and to promote liver steatosis as well as inflammation, which can be reversed by mitochondrial aldehyde dehydrogenase (ALDH2), a detoxification enzyme of ethanol metabolite acetaldehyde (Table 3) [434]. However, in a recent study, mitophagy and ER-phagy independently participated in the progression of NAFLD (Table 3) [363]. In addition, obesity-induced hepatic steatosis inhibited autophagic proteolysis by interfering with the fusion of autophagosomes with lysosomes (Table 3) [435]. Moreover, hepatic steatosis in the livers of patients with NAFLD and in a murine model of NAFLD were shown to impair autophagic flux, which is associated with elevated ER stress and cell apoptosis (Table 3) [436]. Another study reported that the suppressed expressions of cathepsin family enzymes increased p62/SQSTM1 level in patients with NAFLD with autophagic dysfunction and hepatic inflammasome (Table 3) [437]. These results suggest that hepatic steatosis could interfere with the autophagic process to promote disease progression in patients with fatty liver diseases.
4.3. Liver Cancer
The relevance of autophagy in the tumorigenesis of liver cancer was first suggested in an ultrastructural microscopy study published in the late 1970s [438]. By using TEM to investigate changes in the subcellular organelles of liver tissues in the different disease progression stages of patients with liver cancer, Hruban’s study revealed that an increased formation of autophagic vacuoles was associated with early-stage carcinogenesis (Table 4) [438]. Subsequently, another study demonstrated that the induction of carcinogenesis in rat hepatocytes mitigated amino acid deprivation-induced autophagic responsiveness and concomitantly allowed carcinogen-treated cells to survive for a longer period, suggesting that autophagy impaired by carcinogens might benefit the cell growth of carcinogen-altered hepatocytes to promote tumorigenesis (Table 4) [439]. Also, autophagic degradation of cytoplasmic constituents was shown to be negatively regulated by the growth of rat hepatoma cells (Table 4) [440,441,442], implying that downregulated autophagy may selectively promote cell growth from normal cells to transformed cancer cells (Table 4) [443].
Table 4.
Summary of autophagy in liver cancer.
| Experimental Model | Characteristics of Autophagy | Function of Autophagy | References |
|---|---|---|---|
| Rat liver (Hepatectomy; DEN; amino acid deprivation) |
Degradation of endogenous proteins |
|
[439] |
| Rat liver |
|
|
[440,441,442,443] |
|
|
|
[444,445] |
| Huma hepatoma, HepG2 cells |
|
|
[446] |
| Human hepatoma, SMMC7721 cells |
|
|
[447] |
|
Electron micrograph of autophagic vacuoles that contain mitochondria |
|
[539] |
| Rat liver (DEN; CQ) |
|
|
[448] |
| Wild type and liver-specific knockout of ATG5 mice |
|
|
[449] |
|
|
|
[450] |
|
|
|
[451] |
| Wild type and liver-specific knockout of ATG7 mice |
|
|
[452] |
| Liver specimens of HCC patients |
|
|
[453] |
| Human hepatoma, HepG2 cells |
|
|
[454] |
|
|
|
[455,456,457] |
|
|
Inhibited cell growth and induced cell death of HCC cells by chemotherapy- and photodynamic therapy-induced autophagy | [383,458,459,460,461,462,463,464,465,466,467] |
|
|
|
[468,469,470,471,472,473,474,475] |
|
|
|
[476,477,478,479,480,481,482,483,484,485] |
|
|
Enhanced anti-tumor drugs and natural compounds-induced cell death in HCC cells by autophagy inhibition | [486,487,488,489,490,491,492,493,494] |
|
|
|
[495] |
|
|
|
[496] |
| Human hepatoma cells |
|
|
[497] |
|
|
|
[498] |
|
|
|
[495,496,497,498,499,500,501,502,503,504,505,506,507] |
|
|
|
[508] |
| Human hepatoma cells |
|
|
[510] |
|
|
|
[356,377,378,379,380,381] |
|
Electron micrograph of autophagic vacuoles |
|
[511] |
|
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[512] |
|
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[513,514] |
| Wild type, liver-specific knockout of ATG7, Nrf2 knockout, YAP knockout, ATG7/Nrf2 double knockout, ATG7/YAP double knockout mice |
|
|
[515] |
|
|
|
[516] |
|
|
|
[517] |
|
|
|
[518] |
|
|
|
[519] |
| Human hepatoma cells | Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[520] |
| Human cholangiocellular carcinoma cell lines |
|
Participation in Vitamin K2-mediated growth inhibition by autophagy | [521] |
|
|
|
[523,524,525,530] |
| 1. The KrasG12D mutation and p53 deletion-induced intrahepatic cholangiocellular carcinoma (IHCC) |
|
Requirement of induced autophagy for cell growth in IHCC | [526,527] |
|
Immunofluorescence analysis of GFP-LC3 | Participation in decitabine-induced growth suppression by autophagy | [522] |
|
|
Participation in multi-drug resistance of chemotherapy by autophagy | [532] |
| Human cholangiocarcinoma cell lines |
|
Participation in cell survival signaling of ABC294640-treated human cholangiocarcinoma cells | [533] |
|
Detection of lipidation of ATG8/LC3 and p62/SQSTM1 |
|
[534,540] |
| Human cholangiocarcinoma cell line | Detection of lipidation of ATG8/LC3 and p62/SQSTM1 |
|
[528,529] |
| Human cholangiocarcinoma cell line |
|
|
[535,536] |
| Human cholangiocarcinoma cell line |
|
|
[537,538] |
Moreover, the deregulation of autophagy was reported to be synergistically associated with altered apoptotic activity, tumor malignancy, and poor prognosis in HCC (Table 4) [444,445]. The activation of autophagy by the knockdown of HIF-2α was demonstrated to attenuate cell apoptosis to promote the cell survival of hepatocellular tumor spheroids (Table 4) [446]. The dysregulation of autophagy through the downregulation of the Beclin 1 expression was reported to be involved in HAb18G/CD147, a transmembrane glycoprotein-induced biomarker of tumorigenesis in human hepatoma cells (Table 4) [447]. Notably, autophagy was shown to suppress hepatocarcinogenesis at the dysplastic stage but promoted tumor growth in the tumor-forming stage (Table 4) [448]. However, in one study, autophagy was reported to maintain mitochondrial integrity and to protect cells against oxidative stress in the early stages of tumor development to prevent hepatocarcinogenesis but was reported to downregulate tumor suppressors to promote the development of HCC (Table 4) [449]. Autophagy was activated by the long noncoding RNAs (lncRNAs)/has-miR-30b-5p axis to promote hepatocarcinogenesis (Table 4) [450]. Autophagy was also reported to be involved in the promotion of HCC cell invasion by regulating the epithelial–mesenchymal transition (EMT) (Table 4) [451,452]. Furthermore, it supports intracellular ATP in the cell proliferation of liver cancer cells through activating mitochondrial β-oxidation (Table 4) [453,454].
The induction of autophagy by concanavalin A (ConA) was demonstrated to inhibit tumor nodule formation in mouse livers and to prolong survival (Table 4) [455,456,457], indicating that the modulation of autophagy is a potential target for designing anticancer therapies for liver cancer. Similarly, the induction of autophagy by different chemotherapy drugs, naturally isolated compounds, and photodynamic therapy has been suggested to inhibit hepatoma cell growth and induce cell death (Table 4) [383,458,459,460,461,462,463,464,465,466,467]. Furthermore, the activation of autophagy was reported to mediate the transforming growth factor-β (TGF-β)-induced growth inhibition and cellular apoptosis of HCC [468], the microtubule-associated protein 1S (MAP1S)-mediated suppression of hepatocarcinogenesis [469], the HDAC6-associated induction of liver cancer cell death [470], the inactivated HDAC1-induced cell death of liver cancer cells [471], the oroxylin A-triggered HCC cell death [472], the MLN4924-induced repression of liver cancer cell growth [473], and the repressed regulator of cullins 1 (ROC1)-mediated inhibition of liver cancer cell growth [474] (Table 4). In addition, autophagy was demonstrated to be induced by Hedgehog inhibition to reduce the liver cancer cell growth induced by several stimuli (Table 4) [475].
Numerous studies have also suggested that autophagy facilitates cell death in human HCC cells treated with a group of anticancer molecules (Table 4) [476,477,478,479,480,481,482,483,484,485]. By contrast, interference with hepatic autophagy can enhance antitumor drug- and biologically active compound-triggered deaths of HCC cells (Table 4) [486,487,488,489,490,491,492,493,494], suggesting that the inhibition of autophagy could be combined with chemotherapy drugs to instigate the death of liver cancer cells. Furthermore, the inhibition of autophagy reportedly represses the development of hepatoblastoma and HCC [495,496], reduces the viability of HCC under hypoxia [497], and induces cell apoptosis in HCC cells by a proteasome inhibitor [498] (Table 4). Autophagy may also contribute to the chemoresistance of HCC (Table 4) [499,500,501,502,503,504,505,506,507]. The suppression of autophagy was found to enhance the susceptibility of liver cancer cells toward sorafenib-induced cell death (Table 4) [508]. Moreover, autophagy was activated by sorafenib and premexetred-combined chemotherapy to enhance the killing of liver cancer cells though also inducing intrinsic cell apoptosis [509]. By contrast, autophagy was reciprocally shown to suppress the chemotherapy-induced apoptosis of HCC cells (Table 4) [510]. Nevertheless, these studies collectively highlight that the modulation of autophagy can be feasibly adapted to form a new therapeutic strategy to cure liver cancers.
The suppressive role of autophagy in the tumorigenesis of liver cancer in in vivo animal models was demonstrated by the studies of Komatsu et al. and Mizushima et al. (Table 4) [379,511]. Komatsu et al. revealed that the liver-specific knockout of ATG7 in mice leads to the development of multiple tumors in the liver, which is accompanied by the accumulation of p62/SQSTM1-induced Nrf2 and downstream transcriptional activation of antioxidant genes (Table 4) [379]. The upregulated p62/SQSTM1-induced Nrf2 activation through Keap1 degradation by autophagy deficiency was analogously detected in the liver tissues of human hepatocellular carcinoma (Table 4) [379]. Similarly, the mosaic deletion of ATG5 in mice was shown to cause multiple liver tumors in which ubiquitin and p62/SQSTM1 were accumulated. Furthermore, oxidative stress and genomic damage responses were elevated (Table 4) [511]. The progression of liver cancer in mice with partial ATG5 deletions was suppressed by the simultaneous knockout of p62/SQSTM1 (Table 4) [511]. Taken together, these results indicate that autophagy is required for the repression of tumorigenesis in liver cancers. A recent study further demonstrated that in the tumor regions of liver tissues in HCV-positive patients with HCC, a high phosphorylation level of p62/SQSTM1 at serine 349 promotes glucoronate pathways and glutathione synthesis through Nrf2-downstream transcription (Table 4) [255,512]. This phospho-p62/SQSTM1-Nrf2 axis-dependent metabolic reprogramming is involved in the survival and chemoresistance of HCC cells and is, thus, a therapeutic target for designing anticancer drugs with improved efficacy (Table 4) [512]. Analogously, p62/SQSTM1 was also induced by diethylnitrosamine (DEN) to enhance carcinogenic activity through Nrf2-induced antioxidant responses and mTORC1 signaling (Table 4) [513]. The accumulated p62/SQSTM1-positive aggregate in the liver tissues contributed to disease progression in NASH and HCC and was correlated with the recurrence of HCC after curative ablation (Table 4) [513]. These results indicate that p62/SQSTM1 could serve as a prognostic biomarker for HCC recurrence after curative ablation (Table 4) [513,514]. Recently, the hepatocyte-specific ablation of ATG7 in mice was shown to promote liver size, fibrosis, the expansion of progenitor cells, and hepatocarcinogenesis, as accompanied by the accumulation of the yes-associated protein (YAP), an effector of the Hippo signaling pathway (Table 4) [515], suggesting that autophagy acts to prevent the progression of liver-related diseases by targeting YAP to induce degradation.
Recently, mitochondrial fission was found to be frequently upregulated in the liver tissues of patient with HCC and related to poor prognosis (Table 4) [516]. Elevated mitochondrial fission activates autophagy to promote the survival of HCC cells through increased ROS production in in vitro and in vivo models (Table 4) [516]. The autophagic degradation of HIF-1α was reported to be repressed by α-2 adrenergic receptors (ADRB2) signaling and to promote the survival, disease progression, and sorafenib resistance in patients with HCC (Table 4) [517]. The nutrition deprivation-mediated activation of ketone catabolism and ketolysis in HCC cells was shown to suppress AMPK to inhibit the excess activation of autophagy, thereby promoting tumor growth (Table 4) [518]. Conversely, the p300/CBP-associated factor (PCAF) was reported to promote autophagy to inhibit the growth of HCC cells (Table 4) [519]. Moreover, mitophagy was recently shown to remove p53 to maintain hepatic cancer stem cells (CSCs), thus eliciting hepatocarcinogenesis (Table 4) [520]. These studies strengthen the scenario that autophagy is involved in multiple biological pathways and contributes to the tumorigenesis of HCC.
In addition to HCC, autophagy was indicated to function in the development of cholangiocarcinoma. Autophagy was first shown to be activated to participate in vitamin K2 (a well-known antitumor agent for treating malignant leukemia and HCC)-induced cell growth inhibition in cholangiocellular carcinoma cell lines (Table 4) [521]. In addition to vitamin K2, autophagy was reported to be induced in cholangiocellular carcinoma cell lines and mouse xenografts treated with decitabine, an inhibitor of DNA methyltransferase that was shown to suppress tumor development of various cancer types (Table 4) [522]. Activated autophagy was detected in tumor cells from a xenograft tumor model in nude mice and in specimens from clinical cholangiocellular patients (Table 4) [523]. Interference with autophagy was demonstrated to induce cell apoptosis in cholangiocellular cell lines, to suppress cholangiocellular tumor development in a mice xenograft model, and to enhance chemotherapy sensitivity of cisplatin-treated cholangiocellular cells [523]. Moreover, a lower Beclin 1 expression was shown to be associated with lymph node metastasis and poor survival rates of intrahepatic cholangiocellular carcinoma (IHCC) patients (Table 4) [524,525]. Analogously, autophagy was also activated in KrasG12D mutations and p53 deletions (Kras/p53)-induced IHCC in mice (Table 4) [526,527]. The blockade of autophagy by CQ inhibited the tumor cell growth in Kras/p53 IHCC (Table 4) [526,527]. Similarly, CQ was shown to increase the chemosensitivity of cisplatin-treated human cholangiocarcinoma (CCA) cells (Table 4) [528] and to enhance cell apoptosis of human CCA cells through ER stress (Table 4) [529]. In addition, the expressions of HIF-1α, BNIP3, and PI(3)KC3 were positively correlated with lymph node metastasis and poor survival rate in cholangiocellular carcinoma patients [530]. The expressions of LC3B, Beclin 1, and p62/SQSTM1 was shown to be increased at the early stage of multistep cholangiocarcinogenesis in hepatolithiasis [531]. Autophagy was also induced by 5-fluorouracil (5-FU)-treated CCA cells (Table 4) [532]. The 5-FU-activated autophagy was inhibited by capsaicin (the major pungent ingredient found in hot red chili peppers that was shown to repress cell growth of malignant tumors) (Table 4) [532], suggesting that autophagy may participate in the multidrug resistance of chemotherapy in CCA. Treatments with the sphingosine kinase 2 inhibitor, ABC294640, in CCA cells was shown to induce autophagy, and the inhibition of autophagy by CQ and BAF-A1 potentiated ABC294640-induced cell cytotoxicity and apoptosis (Table 4) [533]. The suppressed autophagic flux was indicated to contribute to oblongifolin C (a natural, small molecule that induces cell apoptosis in cervical cancer)-induced cell apoptosis of human CCA cells (Table 4) [534] and to salinomycin-inhibited tumor cell growth in CCA mouse xenograft model (Table 4). Additionally, p53 was demonstrated to activate autophagy in CCA cells, and the repression of p53 was reported to enhance the chemosensitivity in nutrient-deprived CCA cells through downregulating autophagy (Table 4) [535]. In line with this study, compound C (a pharmacological inhibitor of AMPK) treatment in human CCA cells was shown to induce p53-dependent autophagy to protect cells from apoptosis (Table 4) [536]. On the contrary, autophagy was indicated to participate in microRNA (miR)-124-induced cell death in human CCA cells (Table 4) [537] and in dihydroartemisinin-triggered cell death of human CCA cells through the death-associated protein kinase (DAPK)–Beclin 1 pathway (Table 4) [538]. Collectively, these studies indicate that autophagy may participate in the development of IHCC, and the modulation of autophagy by pharmacological inhibitors could serve as a therapeutic option to treat IHCC.
4.4. Viral Hepatitis
In the past decade, hepatic autophagy has been extensively shown to participate in the liver cells infected with hepatitis viruses, including HBV and HCV. In the late 2000s, the HCV-H77 (genotype 1a) infection was first shown to activate the formation of autophagic vacuoles in immortalized human hepatocytes (IHH) (Table 5) [541]. Furthermore, in the replication of a full-length HCV-JFH1 (genotype 2a) viral RNA in human HCC, Huh7 cells were found to induce an incomplete autophagic process that enhanced the accumulation of autolysosomes and interfered with autophagic flux and degradation (Table 5) [542]. HCV-JFH1-induced autophagosome formation was further demonstrated to be required for viral RNA replication (Table 5) [542]. Moreover, ATG5 was shown to interact with the nonstructural (NS) proteins of HCV, NS4B (a viral protein that reconstitutes a membranous web for the replication of viral RNA), and NS5B (a RNA polymerase that replicates viral RNA) to promote HCV viral replication (Table 5) [543]. The HCV-induced autophagosomal membrane was reported to provide a membraned platform that contains HCV NS5A, NS5B, and viral RNA for replication (Table 5) [544,545,546]. These studies imply that HCV activates the autophagic process to organize a membranous structure for replicating viral RNA. However, several contradictory studies have indicated that HCV-induced autophagic vacuoles do not colocalize with viral proteins or viral RNA (Table 5) [547,548,549,550,551], suggesting that the viral-triggered biogenesis of autophagic vacuoles may not be necessary for viral RNA replication.
Table 5.
Summary of autophagy in viral hepatitis.
| Experimental Model | Characteristics of Autophagy | Function of Autophagy | References |
|---|---|---|---|
|
|
Unknown | [541] |
| Human hepatoma, Huh7.5 cells (Transfection of HCV viral RNA) |
|
Promotion on viral RNA replication | [542] |
| Human hepatoma, Huh7 cells (HCV infection) |
|
|
[548] |
| Human hepatoma, Huh7 cells (HCV infection) |
|
|
[549,591] |
|
Colocalization of autophagosomes and lysosomes |
|
[552] |
| Human hepatoma, Huh7 cells (HCV infection) |
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[553] |
| Human hepatoma, Huh7 and Huh7.5.1 cells (HCV infection; transfection of HCV replicon RNA) |
Detection of lipidation of ATG8/LC3 |
|
[544] |
| Human hepatoma, Huh7 cells (HCV infection) |
|
[543] | |
| Human hepatoma, Huh7.5.1 (Transfection of HCV replicon RNA) |
Electron micrograph of autophagic vacuoles |
|
[545] |
| Human hepatoma, Huh7 and Huh7.5.1 cells (HCV infection; transfection of HCV replicon RNA) |
Immunofluorescence analysis of GFP-LC3 |
|
[546] |
| Human hepatoma, Huh7.5.1 cells (HCV infection) |
Immunofluorescence analysis of GFP-LC3 | Promotion on the release of viral particles | [555] |
|
Colocalization of autophagosomes and lysosomes | Promotion on the release of viral particles | [556] |
| Human hepatoma, Huh7 and Huh7.5.1 cells (HCV infection; transfection of HCV replicon RNA) |
Immunofluorescence analysis of GFP-LC3 | Promotion on the release of viral particles | [557] |
| Human hepatoma, Huh7 cells (Transfection of HCV replicon RNA) |
|
Counteracting the viral-induced cell death | [558] |
| Human hepatoma, Huh7.5 cells (HCV infection; transfection of HCV replicon RNA) |
Detection of lipidation of ATG8/LC3 | Unknown | [592] |
| Human hepatoma, Huh7.5 cells (HCV infection) |
Detection of lipidation of ATG8/LC3 | Promotion on viral RNA replication | [593] |
| Human hepatoma, Huh7 cells (Transfection of HCV replicon RNA) |
Detection of lipidation of ATG8/LC3 | Unknown | [559] |
| Human hepatoma, Huh7 cells (HCV infection; transfection of HCV replicon RNA) |
|
Promotion on HNF1α degradation | [571] |
| Human hepatoma, Huh7 and Huh7.5.1 cells (HCV infection; transfection of HCV replicon RNA) |
|
Facilitation on virion release | [561] |
| Human hepatoma, Huh7.5.1 cells (HCV infection; transfection of HCV replicon RNA) |
|
|
[571] |
| Human hepatoma, HepG2 cells (Transfection of HCV replicon RNA) |
|
Promotion on the degradation of replicon RNA | [563,564] |
|
|
Promotion on LDs catabolism | [430] |
| Human hepatoma, Huh7.5.1 cells (HCV infection; transfection of HCV replicon RNA) |
|
|
[565,567] |
| Human hepatoma, Huh7 cells (HCV infection; transfection of HCV viral protein) |
|
Sustained mitochondrial injury | [568] |
| Human hepatoma, Huh7 cells (HCV infection; transfection of HCV replicon RNA) |
|
Unknown | [571] |
| Human hepatoma, Huh7 and Huh7.5.1 cells (HCV infection) |
|
Suppression of innate antiviral immunity | [570] |
| Human hepatoma, Huh7 cells (HCV infection) |
|
|
[572] |
|
|
|
[574,575,576] |
| Human hepatoma cell lines (HBx transfection; transfection of HBV genomic DNA) |
|
|
[577] |
| Human hepatoma, Huh7 cells (SHBs transfection; transfection of HBV genomic DNA) |
|
|
[578] |
| Human hepatoma, Huh7 cells (Transfection of HBV genomic DNA) |
|
|
[579] |
|
|
|
[580] |
| Human hepatoma, HepG2.2.15 cells (Transfection of HBV genomic DNA) |
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[581] |
| Human hepatoma, HepG2.2.15 cells (Transfection of HBV genomic DNA) |
|
|
[582] |
|
|
Reduced starvation-induced cell death by HBx via autophagy activation and inhibition of mitochondrial apoptotic pathway | [583] |
| Human hepatoma, Huh7 and HepG2 cells (Transfection of HBV genomic DNA) |
|
[584] | |
|
|
|
[585] |
| Human hepatoma, HepG2.2.15 cells cells (HBx transfection) |
|
Induced autophagy by HBx through PI(3)K/Akt-mTOR pathway | [586] |
|
|
Induced autophagy by HBx through activating death-associated kinase | [587] |
|
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation | Induced autophagy by HBx through ROS-mediated JNK regulation of Beclin 1/Bcl-2 interaction | [588] |
|
|
Induced autophagy by HBx through interacting with HMGB1 | [589] |
| Human hepatoma, Huh7 cells (HBx transfection) |
|
Inhibited autophagic degradation by HBx through impairing lysosomal maturation | [590] |
The infection by a cell culture-derived HCV-JFH1 virus (HCVcc) into Huh7.5.1 cells, a clone derived from Huh7 cells that is highly permissive to HCV growth, is known to promote the translation of incoming viral RNA, thus establishing a virus infection (Table 5) [548]. Another study showed that a HCVcc-JFH1 infection activates an entire autophagic process throughout the maturation of autolysosomes to support viral RNA replication by suppressing the HCV pathogen associated molecular pattern-mediated innate antiviral responses (Table 5) [548,549]. Similarly, the genetical silencing of ATGs, including Beclin and ATG7, was found to suppress HCV viral infectivity and to upregulate interferon-stimulated gene (ISG) expression in HCV H77-infected IHH cells (Table 5) [552]. Moreover, a recent study revealed that HCV may activate autophagy to degrade the tumor necrosis factor receptor (TNFR)-associated factor 6 (TRAF6) through p62/SQSTM1, thus alleviating innate host immunity (Table 5) [553]. These results together indicate that HCV may induce hepatic autophagy to repress innate antiviral immunity to promote the HCV-infecting life cycle in liver cells (Table 5) [548,549,552,554]. Moreover, the HCV infection was shown to participate in the assembly of infectious particles rather than to affect the replication of intracellular viral RNA (Table 5) [555]. Further studies have demonstrated that autophagy mediates the egress of HCV virion through the CD63-associated exosome pathway (Table 5) [556] and the regulation of apolipoprotein E (ApoE) transport (Table 5) [557]. Additionally, HCV-activated autophagy may depend on different HCV genotypes (Table 5) [558]. The replication of HCV-Con1 (genotype 1b) was reported to impede the fusion of autophagosomes with lysosomes, thus protecting infected liver cells from cell death (Table 5) [558].
Numerous studies have demonstrated that the ER stress-associated unfolded protein response (UPR) is required for HCV-induced autophagy (Table 5) [542,548,549,554], presumably through the DNA damage-inducible transcript 3 protein (DDIT3, also known as CHOP)-mediated transcription of LC3B and ATG5, to activate autophagy (Table 5) [559]. Furthermore, UPR is required for interference with protein kinase B (PKB)-tuberous sclerosis (TSC)-mTOR complex 1 (mTORC1) signaling (Table 5) [560]. STX17, an autophagy regulator implicated in the biogenesis of autophagic vacuoles, may regulate HCV virion egress (Table 5) [561] and promote viral RNA replication (Table 5) [562]. Recently, the alternative splicing of ATG10 was shown to regulate HCV replication through affecting autophagic flux (Table 5) [563,564].
Apart from bulk and nonselective autophagy, HCV was shown to activate autophagy to selectively degrade intracellular organelles, such as LDs and mitochondria (Table 5) [430,565]. The level of lipidated LC3 was inversely correlated with the clinical parameters related to hepatic steatosis in the liver samples of patients with chronic HCV (Table 5) [430]. The HCV-activated autophagic vacuoles were found to engulf LDs in HCV-replicon and HCV-infected cells (Table 5) [430]. In addition, interference with autophagy by pharmacological inhibitors and gene knockdown was demonstrated to significantly enhance the intracellular levels of cholesterol (Table 5) [430], suggesting that the inhibition of autophagic degradation of LDs may result in the occurrence of hepatic steatosis in chronically HCV-infected patients. These results indicate that HCV could induce autophagy to catabolize LDs to protect HCV-infected cells against excess LDs accumulation. Moreover, HCV infection has been shown to trigger the formation of mitophagosomes that degrade mitochondria via the PINK1–Parkin axis in infected cells, thereby promoting HCV viral RNA replication (Table 5) [565,566]. Another study indicated that HCV-induced mitochondrial fission is required for the elimination of mitochondria in infected cells (Table 5) [567]. These studies argue that HCV may activate autophagic degradation to clear the mitochondria with viral-induced damage to attenuate the cell apoptosis of infected liver cells (Table 5) [567]. Oppositely, another study reported that HCV capsids interact with Parkin to impede the translocation of Parkin from the cytoplasm to mitochondria to inhibit mitophagy and to sustain HCV-induced mitochondrial damage and injury in infected liver cells (Table 5) [568]. Recently, HCV viral RNA was shown to induce selective autophagy, possibly promoting the elimination of ubiquitinated protein aggregates (Table 5) [569]. However, CMA was also reported to be activated by HCV and implicated in the degradation of IFN-alpha receptor-1 (IFNAR1), which is stimulated by FFAs (Table 5) [570]. Another study demonstrated that HCV NS5A interacts with HSC70 to promote the degradation of hepatocyte nuclear factor 1α (HNF1α) (Table 5) [571]. Recently, IFN-β-inducible SCOTIN was shown to recruit HCV NS5A into autolysosomes for degradation, restricting the HCV infection (Table 5) [572]. These studies collectively suggest that HCV subverts autophagy to antagonize viral RNA replication and the harmful host responses in infected liver cells.
The induction of autophagy by HBV was first discovered through observing the autophagic degradation of peroxisomes in the liver tissues of patients with chronic HBV who received kidney transplantations and immunosuppressive therapy [329]. Levine et al. showed that the heterozygous deletion of Beclin 1 downregulates autophagy in liver cells, thus promoting HBV-associated premalignant lesions [573]. The HBV infection was further revealed to induce the early-stage formation of autophagic vacuoles in Huh7.5.1 cells through increasing PI(3)K enzyme activity to promote HBV DNA replication (Table 5) [574,575]. The role of autophagy in HBV DNA replication was further confirmed by a study that revealed that the ablation of ATG5 inhibits autophagy to reduce the HBV gene expression in liver cells and in sera (Table 5) [576]. HBV viral proteins, such as HBV x protein (HBx) and HBV small surface protein (SHB), activate autophagy in liver cells through enhancing the Beclin 1 expression and inducing UPR (Table 5) [577,578], thus promoting HBV replication. Recently, HBV was shown to subvert the ATG5-ATG12-ATG16L complex rather than the lipidated ATG8/LC3-mediated autophagosome biogenesis to support the assembly and stability of the HBV nucleocapsid, suggesting that HBV exploits nondegradative autophagy to facilitate HBV propagation (Table 5) [579]. Moreover, HBV can promote autophagy through the miR-192-3p-XIAP axis to benefit HBV replication in vitro and in vivo (Table 5) [580]. In addition to these findings that autophagy promotes HBV growth, Epigallocatechin-3-gallate (EGCG), a major polyphenol in green tea, was demonstrated to inhibit HBV-induced autophagy through increasing lysosomal acidification, thus repressing HBV growth (Table 5) [581]. In spite of genomic DNA replication, HBV-activated autophagy may participate in the secretion of infectious virions in infected cells (Table 5) [582].
HBx-induced autophagy was reported to inhibit mitochondrial apoptosis to promote the survival of HBV genomic DNA-transfected cells (Table 5) [583]. Also, autophagy and ER-associated degradation (ERAD) were shown to promote the degradation of HBV enveloped proteins for the establishment of chronic HBV infection (Table 5) [584]. Additionally, autophagy was negatively correlated with an oncogenic miR-244, which was degraded through the autophagic process in the liver tissues of HBV-associated patients with HCC and HBx-transgenic mice (Table 5) [585]. Reduced ATG5 expression and elevated miR-244 level were significantly correlated with HBV infection and a poor survival rate (Table 5) [585], suggesting that autophagy promotes the degradation of miR-244 to repress HBV-associated tumorigenesis. HBx was shown to activate autophagy through the PI(3)K/Akt-mTOR pathway [586], death-associated protein kinase [587], the JNK2-mediated regulation of Beclin 1/Bcl-2 interaction [588], and the upregulation of HMGB1 [589] (Table 5). By contrast, the transfection of HBV genomic DNA and overexpression of HBx in hepatoma cells interfere with autophagic degradation by impairing the maturation of lysosomes (Table 5) [590]. Additionally, accumulated p62/SQSTM1 and defected cathepsin D were positively related to the liver tissues of people with chronic HBV infection and HBV-associated liver cancer (Table 5) [590], suggesting that HBV’s inhibition of autophagy could result in the development of HCC. Taken together, these results indicate that HBV may modulate autophagy to promote viral growth and may participate in the development of HBV-related liver cancer.
4.5. Fibrosis and Cirrhosis
Autophagy was previously shown to eliminate the mutant α1-ATZ aggregated proteins in liver cells [353,354,370]. The enhancement of autophagy by carbamazepine (CBZ) was reported to reduce the accumulation of α1-ATZ and the inhibited hepatic fibrosis in a α1-AT-deficient mouse model (Table 6) [594] and to reduce the death of hepatic cells in fibrinogen-storage-related diseases (Table 6) [595]. Furthermore, activation of autophagy by gene transfer of the autophagy regulator, TFEB, was demonstrated to enhance the removal of α1-ATZ inclusion bodies and to reverse α1-ATZ-induced liver damage in a α1-AT-deficient mouse model (Table 6) [391]. The induction of MAP1s-mediated autophagy by spermidine was found to prevent liver fibrosis and HCC development in mice (Table 6) [596]. Moreover, in a tetrachloride (CCl4)-induced fibrosis mouse model, human palatine tonsil-derived mesenchymal stem cells (T-MSCs) that differentiated into hepatocyte-like cells were found to ameliorate hepatic fibrosis in an autophagy-dependent manner (Table 6) [597]. Interference with autophagic degradation by chloroquine was reported to improve CCl4-induced liver fibrosis through inhibiting the activation of hepatic stellate cells (Table 6) [598]. The impairment of autophagy by dihydroceramide promoted the disease progression of hepatic steatosis to liver fibrosis (Table 5) [599]. Similarly, impaired autophagy-mediated inhibition of YAP degradation also resulted in liver fibrosis (Table 6) [515]. Autophagy was shown to protect liver sinusoidal endothelial cells (LSECs) from oxidative stress to ameliorate liver fibrosis (Table 6) [600]. These studies collectively indicate that autophagy prevents the development of liver fibrosis.
Table 6.
Summary of autophagy in fibrosis and cirrhosis.
| Experimental Model | Characteristics of Autophagy | Function of Autophagy | References |
|---|---|---|---|
|
|
|
[594] |
| Liver specimens of fibrinogen storage disease | Electron micrograph of autophagic vacuoles | Diminished hepatocellular death in fibrinogen storage diseases by CBZ | [595] |
| Mouse liver (CCl4) |
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation | Prevented liver fibrosis in HCC by activating MAP1S-mediated autophagy | [596] |
| Mouse liver (CCl4) |
Immunofluorescence analysis of LC3 | Amelioration of liver fibrosis by T-MSCs via activating autophagy | [597] |
| Rat liver (CCl4) |
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation | Improved liver fibrosis by chloroquine through inhibiting activation of hepatic stellate cells | [598] |
|
|
|
[599] |
|
|
|
[600] |
|
|
|
[603] |
| Wild type and liver specific knockout of ATG5 mice and Nrf2 knockout mice |
|
|
[404] |
|
Immunofluorescence analysis of LC3 |
|
[605] |
|
|
Reduced CCl4-induced liver fibrosis by DMKG through inhibition of autophagy in hepatic stellate cells in vivo | [607] |
| Mouse liver (CCL4) |
|
Prevented hepatic fibrosis by Quercetin through reducing hepatic stellate cell activation and inhibiting autophagy | [608] |
|
Detection of lipidation of ATG8/LC3 | Amelioration of liver fibrosis by 3-MA through inhibition of autophagy and hepatic stellate cell activation | [609] |
|
|
|
[610] |
|
Detection of lipidation of ATG8/LC3 |
|
[611] |
|
|
|
[613] |
|
Immunofluorescence analysis of LC3 |
|
[614] |
|
|
|
|
|
Detections of lipidation of ATG8/LC3 and p62/SQSTM1 degradation |
|
[616] |
HIF-1α, ROS-JNK1/2-dependent activation, and the X-box binding protein 1 (XBP1) signaling of UPR were required for the autophagy-mediated activation of hepatic stellate cells (Table 6) [601,602,603]. Moreover, autophagy deficiency was reported to induce cell death in hepatocytes, leading to liver inflammation, hepatic fibrosis, and tumorigenesis by substantially activating Nrf2 (Table 6) [604]. Taken together, these studies indicate that autophagic degradation plays a critical role in preventing liver fibrosis. In addition, macrophages derived from mice with an ATG5 deletion was found to secrete high levels of ROS-induced interleukin 1A (IL-1A) and IL-1B, which were correlated with the enhanced accumulation of matrix and fibrogenic cells in CCl4-induced fibrosis livers and upregulated profibrogenic genes expressions in the cocultured hepatic myofibroblasts (Table 6) [605], suggesting that the activation of autophagy in macrophages may repress liver fibrosis. These studies imply that autophagy regulates multiple biological processes to mitigate the occurrence of hepatic fibrosis.
By contrast, one study has shown that autophagy promotes hepatic fibrogenesis by activating hepatic stellate cells in the CCl4 or thioacetamide (TAA)-induced liver fibrosis mouse model (Table 6) [606]. Similarly, dimethyl α-ketoglutarate (DMKG) was reported to inhibit CCl4-induced hepatic fibrosis through reducing autophagy (Table 6) [607]. Furthermore, quercetin attenuated bile duct ligation (BDL) and CCl4-induced liver fibrosis in mice through inhibiting hepatic stellate cell activation and autophagy (Table 6) [608]. Analogously, 3-MA was reported to ameliorate hepatic fibrosis through impairing autophagy initiation in hepatic stellate cells (Table 6) [609]. The genetic deletion of Golgin A2 (GOLAG2), a cis-Golgi protein, reportedly activates autophagy and promotes liver fibrosis in mice (Table 6) [610]. Furthermore, through activating autophagy, β-arrestin 1 (β-arr1) has been implicated in improving the compensatory proliferation of hepatocytes and the growth of hepatic stellate cells with a consequence in liver fibrosis (Table 6) [611]. These studies indicate autophagy’s promoting role in liver fibrosis development.
Unsurprisingly, autophagy was also correlated with cirrhosis in the liver samples of patients with chronic liver disease [612]. The aggregation of p62/SQSTM1 through defective autophagy was found to be increased in the damaged bile ducts of primary biliary cirrhosis (PBC) patients (Table 6) [613]. The elevated expressions of mitochondrial antigens, including pyruvate dehydrogenase complex-E2 component (PDC-E2) and cytochrome c oxidase, subunit I (CCO), was further shown to be associated with the autoimmune pathogenesis of bile duct lesions in patients with PBC (Table 6) [614]. The increased level of LC3B, the colocalization of LC3B with LAMP1, and the elevated expressions of LAMP2 and cathepsin D were detected in the liver samples of patients with cirrhosis (Table 6) [615]. The impairment of autophagy by CQ was reported to be attenuated the CCl4-induced ductular reaction and fibrosis (Table 6) [615]. By contrast, autophagy was reported to contribute to the formation of hepatocyte growth factor (HGF)-directed Axin2+CD90+ CSCs to promote hepatocarcinogenesis in cirrhotic livers (Table 6) [616]. These studies together constitute the notion that autophagy may regulate the occurrence of liver cirrhosis.
5. Conclusions and Future Directions
Autophagy plays a critical role in the maintenance of cellular homeostasis and the elimination of unwanted intracellular materials, such as proteins and organelles, in liver physiology. Autophagy has been extensively shown to be regulated in liver cells in multiple liver diseases. The activation of autophagy has mostly been conceptualized as a protector of liver cells against injury. Furthermore, it has been suggested to prevent the development of liver-associated diseases through the autophagic degradation of aggregate-prone proteins and damaged organelles. In accordance with the protective roles of autophagy, the enhancement of autophagy in liver cells is considered a treatment strategy for ameliorating the development of liver diseases. By contrast, autophagy has also been implicated in promoting liver damage-induced cell death and the development of liver-related diseases, suggesting that interference with autophagy may represent a novel route to mitigate the progression of liver diseases. Hence, the physiological significance of autophagy in liver diseases is still debated and is largely hampered by discrepancies between studies. Our current understanding of hepatic autophagy in liver diseases seems to be context-dependent and disease stage-dependent. Nevertheless, further investigations are required to comprehensively dissect the detailed role of autophagy in the induction and progression of liver-related diseases. Moreover, an improved understanding of the clinical relevance of autophagy in the different stages of liver disease progression is required. Furthermore, the innovative and integrative system-based biology approach should be employed to identify distinct aspects of autophagy that can be targeted and used for the development of a feasible treatment strategy to effectively cure liver diseases in clinical settings.
Acknowledgments
The author apologizes to the colleagues whose work could not be cited due to space limitations. The author thanks Bert Tan for suggestions on the manuscript preparation.
Author Contributions
Conceptualization, original draft preparation, review, and editing: P.-Y.K.
Funding
This study was supported by research grants from the National Health Research Institute (NHRI-EX103-10322SC, NHRI-EX104-10322SC, NHRI-EX105-10322SC, and NHRI-EX106-10322SC), Miaoli; the Ministry of Science and Technology (MOST 102-2320-B-182-037-MY3 and MOST 105-2628-B-182-001-MY3), Taipei; and Chang Gung Memorial Hospital (CMRPD1C0211, CMRPD1D0021, CMRPD1D0022, CMRPD1D0023, CMRPD1G0281, CRRPD1F0031, CMRPG3F0571, and CMRPD1H0681), Taoyuan, Taiwan.
Conflicts of Interest
The author has no conflicts of interest to declare.
References
- 1.Mizushima N. A brief history of autophagy from cell biology to physiology and disease. Nat. Cell Biol. 2018;20:521–527. doi: 10.1038/s41556-018-0092-5. [DOI] [PubMed] [Google Scholar]
- 2.Galluzzi L., Baehrecke E.H., Ballabio A., Boya P., Bravo-San Pedro J.M., Cecconi F., Choi A.M., Chu C.T., Codogno P., Colombo M.I., et al. Molecular definitions of autophagy and related processes. EMBO J. 2017;36:1811–1836. doi: 10.15252/embj.201796697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Z., Klionsky D.J. Eaten alive: A history of macroautophagy. Nat. Cell Biol. 2010;12:814–822. doi: 10.1038/ncb0910-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kroemer G., Marino G., Levine B. Autophagy and the integrated stress response. Mol. Cell. 2010;40:280–293. doi: 10.1016/j.molcel.2010.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levine B., Packer M., Codogno P. Development of autophagy inducers in clinical medicine. J. Clin. Investig. 2015;125:14–24. doi: 10.1172/JCI73938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi A.M., Ryter S.W., Levine B. Autophagy in human health and disease. N. Engl. J. Med. 2013;368:651–662. doi: 10.1056/NEJMra1205406. [DOI] [PubMed] [Google Scholar]
- 7.Ueno T., Komatsu M. Autophagy in the liver: Functions in health and disease. Nat. Rev. Gastroenterol. Hepatol. 2017;14:170–184. doi: 10.1038/nrgastro.2016.185. [DOI] [PubMed] [Google Scholar]
- 8.Yin X.M., Ding W.X., Gao W. Autophagy in the liver. Hepatology. 2008;47:1773–1785. doi: 10.1002/hep.22146. [DOI] [PubMed] [Google Scholar]
- 9.Khambu B., Yan S., Huda N., Liu G., Yin X.M. Homeostatic Role of Autophagy in Hepatocytes. Semin. Liver Dis. 2018;38:308–319. doi: 10.1055/s-0038-1669939. [DOI] [PubMed] [Google Scholar]
- 10.Wang K. Autophagy and apoptosis in liver injury. Cell Cycle. 2015;14:1631–1642. doi: 10.1080/15384101.2015.1038685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Czaja M.J. Functions of autophagy in hepatic and pancreatic physiology and disease. Gastroenterology. 2011;140:1895–1908. doi: 10.1053/j.gastro.2011.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rautou P.E., Mansouri A., Lebrec D., Durand F., Valla D., Moreau R. Autophagy in liver diseases. J. Hepatol. 2010;53:1123–1134. doi: 10.1016/j.jhep.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Clark S.L., Jr. Cellular differentiation in the kidneys of newborn mice studies with the electron microscope. J. Biophys. Biochem. Cytol. 1957;3:349–362. doi: 10.1083/jcb.3.3.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ashford T.P., Porter K.R. Cytoplasmic components in hepatic cell lysosomes. J. Cell Biol. 1962;12:198–202. doi: 10.1083/jcb.12.1.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Novikoff A.B., Essner E. Cytolysomes and mitochondrial degeneration. J. Cell Biol. 1962;15:140–146. doi: 10.1083/jcb.15.1.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Novikoff A.B. The proximal tubule cell in experimental hydronephrosis. J. Biophys. Biochem. Cytol. 1959;6:136–138. doi: 10.1083/jcb.6.1.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Duve C., Wattiaux R. Functions of lysosomes. Annu. Rev. Physiol. 1966;28:435–492. doi: 10.1146/annurev.ph.28.030166.002251. [DOI] [PubMed] [Google Scholar]
- 18.Klionsky D.J. Autophagy revisited: A conversation with Christian de Duve. Autophagy. 2008;4:740–743. doi: 10.4161/auto.6398. [DOI] [PubMed] [Google Scholar]
- 19.Deter R.L., De Duve C. Influence of glucagon, an inducer of cellular autophagy, on some physical properties of Rat liver lysosomes. J. Cell Biol. 1967;33:437–449. doi: 10.1083/jcb.33.2.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deter R.L., Baudhuin P., De Duve C. Participation of lysosomes in cellular autophagy induced in Rat liver by glucagon. J. Cell Biol. 1967;35:C11–C16. doi: 10.1083/jcb.35.2.C11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mortimore G.E., Schworer C.M. Induction of autophagy by amino-acid deprivation in perfused rat liver. Nature. 1977;270:174–176. doi: 10.1038/270174a0. [DOI] [PubMed] [Google Scholar]
- 22.Pfeifer U. Inhibition by insulin of the physiological autophagic breakdown of cell organelles. Acta Biol. Med. Ger. 1977;36:1691–1694. [PubMed] [Google Scholar]
- 23.Pfeifer U. Inhibition by insulin of the formation of autophagic vacuoles in rat liver. A morphometric approach to the kinetics of intracellular degradation by autophagy. J. Cell Biol. 1978;78:152–167. doi: 10.1083/jcb.78.1.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kovacs A.L., Molnar K., Seglen P.O. Inhibition of autophagic sequestration and endogenous protein degradation in isolated rat hepatocytes by methylated adenosine derivatives. FEBS Lett. 1981;134:194–196. doi: 10.1016/0014-5793(81)80600-X. [DOI] [PubMed] [Google Scholar]
- 25.Schworer C.M., Mortimore G.E. Glucagon-induced autophagy and proteolysis in rat liver: Mediation by selective deprivation of intracellular amino acids. Proc. Natl. Acad. Sci. USA. 1979;76:3169–3173. doi: 10.1073/pnas.76.7.3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schworer C.M., Shiffer K.A., Mortimore G.E. Quantitative relationship between autophagy and proteolysis during graded amino acid deprivation in perfused rat liver. J. Biol. Chem. 1981;256:7652–7658. [PubMed] [Google Scholar]
- 27.Blankson H., Holen I., Seglen P.O. Disruption of the cytokeratin cytoskeleton and inhibition of hepatocytic autophagy by okadaic acid. Exp. Cell Res. 1995;218:522–530. doi: 10.1006/excr.1995.1187. [DOI] [PubMed] [Google Scholar]
- 28.Holen I., Gordon P.B., Seglen P.O. Protein kinase-dependent effects of okadaic acid on hepatocytic autophagy and cytoskeletal integrity. Pt 3Biochem. J. 1992;284:633–636. doi: 10.1042/bj2840633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holen I., Stromhaug P.E., Gordon P.B., Fengsrud M., Berg T.O., Seglen P.O. Inhibition of autophagy and multiple steps in asialoglycoprotein endocytosis by inhibitors of tyrosine protein kinases (tyrphostins) J. Biol. Chem. 1995;270:12823–12831. doi: 10.1074/jbc.270.21.12823. [DOI] [PubMed] [Google Scholar]
- 30.Seglen P.O., Gordon P.B. 3-Methyladenine: Specific inhibitor of autophagic/lysosomal protein degradation in isolated rat hepatocytes. Proc. Natl. Acad. Sci. USA. 1982;79:1889–1892. doi: 10.1073/pnas.79.6.1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kovacs A.L., Seglen P.O. Inhibition of hepatocytic protein degradation by methylaminopurines and inhibitors of protein synthesis. Biochim. Biophys. Acta. 1981;676:213–220. doi: 10.1016/0304-4165(81)90189-6. [DOI] [PubMed] [Google Scholar]
- 32.Gordon P.B., Kovacs A.L., Seglen P.O. Temperature dependence of protein degradation, autophagic sequestration and mitochondrial sugar uptake in rat hepatocytes. Biochim. Biophys. Acta. 1987;929:128–133. doi: 10.1016/0167-4889(87)90167-4. [DOI] [PubMed] [Google Scholar]
- 33.Plomp P.J., Wolvetang E.J., Groen A.K., Meijer A.J., Gordon P.B., Seglen P.O. Energy dependence of autophagic protein degradation in isolated rat hepatocytes. Eur. J. Biochem. 1987;164:197–203. doi: 10.1111/j.1432-1033.1987.tb11011.x. [DOI] [PubMed] [Google Scholar]
- 34.Gordon P.B., Seglen P.O. Prelysosomal convergence of autophagic and endocytic pathways. Biochem. Biophys. Res. Commun. 1988;151:40–47. doi: 10.1016/0006-291X(88)90556-6. [DOI] [PubMed] [Google Scholar]
- 35.Yamamoto A., Masaki R., Tashiro Y. Characterization of the isolation membranes and the limiting membranes of autophagosomes in rat hepatocytes by lectin cytochemistry. J. Histochem. Cytochem. 1990;38:573–580. doi: 10.1177/38.4.2319125. [DOI] [PubMed] [Google Scholar]
- 36.Yokota S. Formation of autophagosomes during degradation of excess peroxisomes induced by administration of dioctyl phthalate. Eur. J. Cell Biol. 1993;61:67–80. [PubMed] [Google Scholar]
- 37.Yokota S., Himeno M., Roth J., Brada D., Kato K. Formation of autophagosomes during degradation of excess peroxisomes induced by di-(2-ethylhexyl)phthalate treatment. II. Immunocytochemical analysis of early and late autophagosomes. Eur. J. Cell Biol. 1993;62:372–383. [PubMed] [Google Scholar]
- 38.Yokota S., Himeno M., Kato K. Formation of autophagosomes during degradation of excess peroxisomes induced by di-(2-ethylhexyl)-phthalate treatment. III. Fusion of early autophagosomes with lysosomal compartments. Eur. J. Cell Biol. 1995;66:15–24. [PubMed] [Google Scholar]
- 39.Liou W., Geuze H.J., Geelen M.J., Slot J.W. The autophagic and endocytic pathways converge at the nascent autophagic vacuoles. J. Cell Biol. 1997;136:61–70. doi: 10.1083/jcb.136.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fengsrud M., Roos N., Berg T., Liou W., Slot J.W., Seglen P.O. Ultrastructural and immunocytochemical characterization of autophagic vacuoles in isolated hepatocytes: Effects of vinblastine and asparagine on vacuole distributions. Exp. Cell Res. 1995;221:504–519. doi: 10.1006/excr.1995.1402. [DOI] [PubMed] [Google Scholar]
- 41.Furuno K., Ishikawa T., Akasaki K., Lee S., Nishimura Y., Tsuji H., Himeno M., Kato K. Immunocytochemical study of the surrounding envelope of autophagic vacuoles in cultured rat hepatocytes. Exp. Cell Res. 1990;189:261–268. doi: 10.1016/0014-4827(90)90245-6. [DOI] [PubMed] [Google Scholar]
- 42.Takeshige K., Baba M., Tsuboi S., Noda T., Ohsumi Y. Autophagy in yeast demonstrated with proteinase-deficient mutants and conditions for its induction. J. Cell Biol. 1992;119:301–311. doi: 10.1083/jcb.119.2.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsukada M., Ohsumi Y. Isolation and characterization of autophagy-defective mutants of Saccharomyces cerevisiae. FEBS Lett. 1993;333:169–174. doi: 10.1016/0014-5793(93)80398-E. [DOI] [PubMed] [Google Scholar]
- 44.Noda T., Matsuura A., Wada Y., Ohsumi Y. Novel system for monitoring autophagy in the yeast Saccharomyces cerevisiae. Biochem. Biophys. Res. Commun. 1995;210:126–132. doi: 10.1006/bbrc.1995.1636. [DOI] [PubMed] [Google Scholar]
- 45.Harding T.M., Hefner-Gravink A., Thumm M., Klionsky D.J. Genetic and phenotypic overlap between autophagy and the cytoplasm to vacuole protein targeting pathway. J. Biol. Chem. 1996;271:17621–17624. doi: 10.1074/jbc.271.30.17621. [DOI] [PubMed] [Google Scholar]
- 46.Schlumpberger M., Schaeffeler E., Straub M., Bredschneider M., Wolf D.H., Thumm M. AUT1, a gene essential for autophagocytosis in the yeast Saccharomyces cerevisiae. J. Bacteriol. 1997;179:1068–1076. doi: 10.1128/jb.179.4.1068-1076.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Straub M., Bredschneider M., Thumm M. AUT3, a serine/threonine kinase gene, is essential for autophagocytosis in Saccharomyces cerevisiae. J. Bacteriol. 1997;179:3875–3883. doi: 10.1128/jb.179.12.3875-3883.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lang T., Schaeffeler E., Bernreuther D., Bredschneider M., Wolf D.H., Thumm M. Aut2p and Aut7p, two novel microtubule-associated proteins are essential for delivery of autophagic vesicles to the vacuole. EMBO J. 1998;17:3597–3607. doi: 10.1093/emboj/17.13.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klionsky D.J., Cregg J.M., Dunn W.A., Jr., Emr S.D., Sakai Y., Sandoval I.V., Sibirny A., Subramani S., Thumm M., Veenhuis M., et al. A unified nomenclature for yeast autophagy-related genes. Dev. Cell. 2003;5:539–545. doi: 10.1016/S1534-5807(03)00296-X. [DOI] [PubMed] [Google Scholar]
- 50.Klionsky D.J., Codogno P., Cuervo A.M., Deretic V., Elazar Z., Fueyo-Margareto J., Gewirtz D.A., Kroemer G., Levine B., Mizushima N., et al. A comprehensive glossary of autophagy-related molecules and processes. Autophagy. 2010;6:438–448. doi: 10.4161/auto.6.4.12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klionsky D.J., Baehrecke E.H., Brumell J.H., Chu C.T., Codogno P., Cuervo A.M., Debnath J., Deretic V., Elazar Z., Eskelinen E.L., et al. A comprehensive glossary of autophagy-related molecules and processes (2nd edition) Autophagy. 2011;7:1273–1294. doi: 10.4161/auto.7.11.17661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ahlberg J., Marzella L., Glaumann H. Uptake and degradation of proteins by isolated Rat liver lysosomes. Suggestion of a microautophagic pathway of proteolysis. Lab. Investig. 1982;47:523–532. [PubMed] [Google Scholar]
- 53.Sakai M., Araki N., Ogawa K. Lysosomal movements during heterophagy and autophagy: With special reference to nematolysosome and wrapping lysosome. J. Electron Microsc. Tech. 1989;12:101–131. doi: 10.1002/jemt.1060120206. [DOI] [PubMed] [Google Scholar]
- 54.Mijaljica D., Prescott M., Devenish R.J. Microautophagy in mammalian cells: Revisiting a 40-year-old conundrum. Autophagy. 2011;7:673–682. doi: 10.4161/auto.7.7.14733. [DOI] [PubMed] [Google Scholar]
- 55.Oku M., Sakai Y. Three Distinct Types of Microautophagy Based on Membrane Dynamics and Molecular Machineries. Bioessays. 2018;40:e1800008. doi: 10.1002/bies.201800008. [DOI] [PubMed] [Google Scholar]
- 56.Sattler T., Mayer A. Cell-free reconstitution of microautophagic vacuole invagination and vesicle formation. J. Cell Biol. 2000;151:529–538. doi: 10.1083/jcb.151.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Krick R., Muehe Y., Prick T., Bremer S., Schlotterhose P., Eskelinen E.L., Millen J., Goldfarb D.S., Thumm M. Piecemeal microautophagy of the nucleus requires the core macroautophagy genes. Mol. Biol. Cell. 2008;19:4492–4505. doi: 10.1091/mbc.e08-04-0363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang C.W., Miao Y.H., Chang Y.S. A sterol-enriched vacuolar microdomain mediates stationary phase lipophagy in budding yeast. J. Cell Biol. 2014;206:357–366. doi: 10.1083/jcb.201404115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Oku M., Maeda Y., Kagohashi Y., Kondo T., Yamada M., Fujimoto T., Sakai Y. Evidence for ESCRT- and clathrin-dependent microautophagy. J. Cell Biol. 2017;216:3263–3274. doi: 10.1083/jcb.201611029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhu L., Jorgensen J.R., Li M., Chuang Y.S., Emr S.D. ESCRTs function directly on the lysosome membrane to downregulate ubiquitinated lysosomal membrane proteins. eLife. 2017;6 doi: 10.7554/eLife.26403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kaushik S., Cuervo A.M. The coming of age of chaperone-mediated autophagy. Nat. Rev. Mol. Cell Biol. 2018;19:365–381. doi: 10.1038/s41580-018-0001-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tekirdag K., Cuervo A.M. Chaperone-mediated autophagy and endosomal microautophagy: Joint by a chaperone. J. Biol. Chem. 2018;293:5414–5424. doi: 10.1074/jbc.R117.818237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Park C., Suh Y., Cuervo A.M. Regulated degradation of Chk1 by chaperone-mediated autophagy in response to DNA damage. Nat. Commun. 2015;6:6823. doi: 10.1038/ncomms7823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cuervo A.M., Knecht E., Terlecky S.R., Dice J.F. Activation of a selective pathway of lysosomal proteolysis in Rat liver by prolonged starvation. Am. J. Physiol. 1995;269:C1200–C1208. doi: 10.1152/ajpcell.1995.269.5.C1200. [DOI] [PubMed] [Google Scholar]
- 65.Kiffin R., Christian C., Knecht E., Cuervo A.M. Activation of chaperone-mediated autophagy during oxidative stress. Mol. Biol. Cell. 2004;15:4829–4840. doi: 10.1091/mbc.e04-06-0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dohi E., Tanaka S., Seki T., Miyagi T., Hide I., Takahashi T., Matsumoto M., Sakai N. Hypoxic stress activates chaperone-mediated autophagy and modulates neuronal cell survival. Neurochem. Int. 2012;60:431–442. doi: 10.1016/j.neuint.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 67.Finn P.F., Dice J.F. Ketone bodies stimulate chaperone-mediated autophagy. J. Biol. Chem. 2005;280:25864–25870. doi: 10.1074/jbc.M502456200. [DOI] [PubMed] [Google Scholar]
- 68.Ferreira J.V., Fofo H., Bejarano E., Bento C.F., Ramalho J.S., Girao H., Pereira P. STUB1/CHIP is required for HIF1A degradation by chaperone-mediated autophagy. Autophagy. 2013;9:1349–1366. doi: 10.4161/auto.25190. [DOI] [PubMed] [Google Scholar]
- 69.Schneider J.L., Suh Y., Cuervo A.M. Deficient chaperone-mediated autophagy in liver leads to metabolic dysregulation. Cell Metab. 2014;20:417–432. doi: 10.1016/j.cmet.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kaushik S., Cuervo A.M. Degradation of lipid droplet-associated proteins by chaperone-mediated autophagy facilitates lipolysis. Nat. Cell Biol. 2015;17:759–770. doi: 10.1038/ncb3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kaushik S., Cuervo A.M. AMPK-dependent phosphorylation of lipid droplet protein PLIN2 triggers its degradation by CMA. Autophagy. 2016;12:432–438. doi: 10.1080/15548627.2015.1124226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cuervo A.M., Hu W., Lim B., Dice J.F. IkappaB is a substrate for a selective pathway of lysosomal proteolysis. Mol. Biol. Cell. 1998;9:1995–2010. doi: 10.1091/mbc.9.8.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang Q., She H., Gearing M., Colla E., Lee M., Shacka J.J., Mao Z. Regulation of neuronal survival factor MEF2D by chaperone-mediated autophagy. Science. 2009;323:124–127. doi: 10.1126/science.1166088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang L., Sun Y., Fei M., Tan C., Wu J., Zheng J., Tang J., Sun W., Lv Z., Bao J., et al. Disruption of chaperone-mediated autophagy-dependent degradation of MEF2A by oxidative stress-induced lysosome destabilization. Autophagy. 2014;10:1015–1035. doi: 10.4161/auto.28477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Valdor R., Mocholi E., Botbol Y., Guerrero-Ros I., Chandra D., Koga H., Gravekamp C., Cuervo A.M., Macian F. Chaperone-mediated autophagy regulates T cell responses through targeted degradation of negative regulators of T cell activation. Nat. Immunol. 2014;15:1046–1054. doi: 10.1038/ni.3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hu M.M., Yang Q., Xie X.Q., Liao C.Y., Lin H., Liu T.T., Yin L., Shu H.B. Sumoylation Promotes the Stability of the DNA Sensor cGAS and the Adaptor STING to Regulate the Kinetics of Response to DNA Virus. Immunity. 2016;45:555–569. doi: 10.1016/j.immuni.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 77.Hubbi M.E., Gilkes D.M., Hu H., Kshitiz, Ahmed I., Semenza G.L. Cyclin-dependent kinases regulate lysosomal degradation of hypoxia-inducible factor 1alpha to promote cell-cycle progression. Proc. Natl. Acad. Sci. USA. 2014;111:E3325–E3334. doi: 10.1073/pnas.1412840111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cuervo A.M., Dice J.F. Age-related decline in chaperone-mediated autophagy. J. Biol. Chem. 2000;275:31505–31513. doi: 10.1074/jbc.M002102200. [DOI] [PubMed] [Google Scholar]
- 79.Zhang C., Cuervo A.M. Restoration of chaperone-mediated autophagy in aging liver improves cellular maintenance and hepatic function. Nat. Med. 2008;14:959–965. doi: 10.1038/nm.1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lv L., Li D., Zhao D., Lin R., Chu Y., Zhang H., Zha Z., Liu Y., Li Z., Xu Y., et al. Acetylation targets the M2 isoform of pyruvate kinase for degradation through chaperone-mediated autophagy and promotes tumor growth. Mol. Cell. 2011;42:719–730. doi: 10.1016/j.molcel.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Saha T. LAMP2A overexpression in breast tumors promotes cancer cell survival via chaperone-mediated autophagy. Autophagy. 2012;8:1643–1656. doi: 10.4161/auto.21654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chava S., Lee C., Aydin Y., Chandra P.K., Dash A., Chedid M., Thung S.N., Moroz K., Wu T., Nayak N.C., et al. Chaperone-mediated autophagy compensates for impaired macroautophagy in the cirrhotic liver to promote hepatocellular carcinoma. Oncotarget. 2017;8:40019–40036. doi: 10.18632/oncotarget.16685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Xilouri M., Brekk O.R., Landeck N., Pitychoutis P.M., Papasilekas T., Papadopoulou-Daifoti Z., Kirik D., Stefanis L. Boosting chaperone-mediated autophagy in vivo mitigates alpha-synuclein-induced neurodegeneration. Brain. 2013;136:2130–2146. doi: 10.1093/brain/awt131. [DOI] [PubMed] [Google Scholar]
- 84.Wang B., Cai Z., Tao K., Zeng W., Lu F., Yang R., Feng D., Gao G., Yang Q. Essential control of mitochondrial morphology and function by chaperone-mediated autophagy through degradation of PARK7. Autophagy. 2016;12:1215–1228. doi: 10.1080/15548627.2016.1179401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang Y., Martinez-Vicente M., Kruger U., Kaushik S., Wong E., Mandelkow E.M., Cuervo A.M., Mandelkow E. Tau fragmentation, aggregation and clearance: The dual role of lysosomal processing. Hum. Mol. Genet. 2009;18:4153–4170. doi: 10.1093/hmg/ddp367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Park J.S., Kim D.H., Yoon S.Y. Regulation of amyloid precursor protein processing by its KFERQ motif. BMB Rep. 2016;49:337–342. doi: 10.5483/BMBRep.2016.49.6.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang C.C., Bose J.K., Majumder P., Lee K.H., Huang J.T., Huang J.K., Shen C.K. Metabolism and mis-metabolism of the neuropathological signature protein TDP-43. J. Cell Sci. 2014;127:3024–3038. doi: 10.1242/jcs.136150. [DOI] [PubMed] [Google Scholar]
- 88.Bauer P.O., Goswami A., Wong H.K., Okuno M., Kurosawa M., Yamada M., Miyazaki H., Matsumoto G., Kino Y., Nagai Y., et al. Harnessing chaperone-mediated autophagy for the selective degradation of mutant huntingtin protein. Nat. Biotechnol. 2010;28:256–263. doi: 10.1038/nbt.1608. [DOI] [PubMed] [Google Scholar]
- 89.Koga H., Martinez-Vicente M., Arias E., Kaushik S., Sulzer D., Cuervo A.M. Constitutive upregulation of chaperone-mediated autophagy in Huntington’s disease. J. Neurosci. 2011;31:18492–18505. doi: 10.1523/JNEUROSCI.3219-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li Y., Lu L., Luo N., Wang Y.Q., Gao H.M. Inhibition of PI3K/AKt/mTOR signaling pathway protects against d-galactosamine/lipopolysaccharide-induced acute liver failure by chaperone-mediated autophagy in rats. Biomed. Pharmacother. 2017;92:544–553. doi: 10.1016/j.biopha.2017.05.037. [DOI] [PubMed] [Google Scholar]
- 91.Das S., Seth R.K., Kumar A., Kadiiska M.B., Michelotti G., Diehl A.M., Chatterjee S. Purinergic receptor X7 is a key modulator of metabolic oxidative stress-mediated autophagy and inflammation in experimental nonalcoholic steatohepatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2013;305:G950–G963. doi: 10.1152/ajpgi.00235.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Venugopal B., Mesires N.T., Kennedy J.C., Curcio-Morelli C., Laplante J.M., Dice J.F., Slaugenhaupt S.A. Chaperone-mediated autophagy is defective in mucolipidosis type IV. J. Cell Physiol. 2009;219:344–353. doi: 10.1002/jcp.21676. [DOI] [PubMed] [Google Scholar]
- 93.Feng Y., He D., Yao Z., Klionsky D.J. The machinery of macroautophagy. Cell Res. 2014;24:24–41. doi: 10.1038/cr.2013.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Madeo F., Zimmermann A., Maiuri M.C., Kroemer G. Essential role for autophagy in life span extension. J. Clin. Investig. 2015;125:85–93. doi: 10.1172/JCI73946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Menzies F.M., Fleming A., Caricasole A., Bento C.F., Andrews S.P., Ashkenazi A., Fullgrabe J., Jackson A., Jimenez Sanchez M., Karabiyik C., et al. Autophagy and Neurodegeneration: Pathogenic Mechanisms and Therapeutic Opportunities. Neuron. 2017;93:1015–1034. doi: 10.1016/j.neuron.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 96.Harris H., Rubinsztein D.C. Control of autophagy as a therapy for neurodegenerative disease. Nat. Rev. Neurol. 2011;8:108–117. doi: 10.1038/nrneurol.2011.200. [DOI] [PubMed] [Google Scholar]
- 97.Boland B., Yu W.H., Corti O., Mollereau B., Henriques A., Bezard E., Pastores G.M., Rubinsztein D.C., Nixon R.A., Duchen M.R., et al. Promoting the clearance of neurotoxic proteins in neurodegenerative disorders of ageing. Nat. Rev. Drug Discov. 2018;17:660–688. doi: 10.1038/nrd.2018.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Galluzzi L., Pietrocola F., Levine B., Kroemer G. Metabolic control of autophagy. Cell. 2014;159:1263–1276. doi: 10.1016/j.cell.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Doherty J., Baehrecke E.H. Life, death and autophagy. Nat. Cell Biol. 2018;20:1110–1117. doi: 10.1038/s41556-018-0201-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Abdellatif M., Sedej S., Carmona-Gutierrez D., Madeo F., Kroemer G. Autophagy in Cardiovascular Aging. Circ. Res. 2018;123:803–824. doi: 10.1161/CIRCRESAHA.118.312208. [DOI] [PubMed] [Google Scholar]
- 101.Ren J., Sowers J.R., Zhang Y. Metabolic Stress, Autophagy, and Cardiovascular Aging: From Pathophysiology to Therapeutics. Trends Endocrinol. Metab. 2018;29:699–711. doi: 10.1016/j.tem.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Picca A., Mankowski R.T., Burman J.L., Donisi L., Kim J.S., Marzetti E., Leeuwenburgh C. Mitochondrial quality control mechanisms as molecular targets in cardiac ageing. Nat. Rev. Cardiol. 2018;15:543–554. doi: 10.1038/s41569-018-0059-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bagherniya M., Butler A.E., Barreto G.E., Sahebkar A. The effect of fasting or calorie restriction on autophagy induction: A review of the literature. Ageing Res. Rev. 2018;47:183–197. doi: 10.1016/j.arr.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 104.Rubinsztein D.C., Marino G., Kroemer G. Autophagy and aging. Cell. 2011;146:682–695. doi: 10.1016/j.cell.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 105.Deretic V., Levine B. Autophagy balances inflammation in innate immunity. Autophagy. 2018;14:243–251. doi: 10.1080/15548627.2017.1402992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gomes L.C., Dikic I. Autophagy in antimicrobial immunity. Mol. Cell. 2014;54:224–233. doi: 10.1016/j.molcel.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 107.Zhang Y., Sowers J.R., Ren J. Targeting autophagy in obesity: From pathophysiology to management. Nat. Rev. Endocrinol. 2018;14:356–376. doi: 10.1038/s41574-018-0009-1. [DOI] [PubMed] [Google Scholar]
- 108.Kim K.H., Lee M.S. Autophagy—A key player in cellular and body metabolism. Nat. Rev. Endocrinol. 2014;10:322–337. doi: 10.1038/nrendo.2014.35. [DOI] [PubMed] [Google Scholar]
- 109.Kroemer G. Autophagy: A druggable process that is deregulated in aging and human disease. J. Clin. Investig. 2015;125:1–4. doi: 10.1172/JCI78652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Green D.R., Galluzzi L., Kroemer G. Cell biology. Metabolic control of cell death. Science. 2014;345:1250256. doi: 10.1126/science.1250256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Carlsson S.R., Simonsen A. Membrane dynamics in autophagosome biogenesis. J. Cell Sci. 2015;128:193–205. doi: 10.1242/jcs.141036. [DOI] [PubMed] [Google Scholar]
- 112.Lamb C.A., Yoshimori T., Tooze S.A. The autophagosome: Origins unknown, biogenesis complex. Nat. Rev. Mol. Cell Biol. 2013;14:759–774. doi: 10.1038/nrm3696. [DOI] [PubMed] [Google Scholar]
- 113.Shibutani S.T., Yoshimori T. A current perspective of autophagosome biogenesis. Cell Res. 2014;24:58–68. doi: 10.1038/cr.2013.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mercer T.J., Gubas A., Tooze S.A. A molecular perspective of mammalian autophagosome biogenesis. J. Biol. Chem. 2018;293:5386–5395. doi: 10.1074/jbc.R117.810366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hayashi-Nishino M., Fujita N., Noda T., Yamaguchi A., Yoshimori T., Yamamoto A. A subdomain of the endoplasmic reticulum forms a cradle for autophagosome formation. Nat. Cell Biol. 2009;11:1433–1437. doi: 10.1038/ncb1991. [DOI] [PubMed] [Google Scholar]
- 116.Yla-Anttila P., Vihinen H., Jokitalo E., Eskelinen E.L. 3D tomography reveals connections between the phagophore and endoplasmic reticulum. Autophagy. 2009;5:1180–1185. doi: 10.4161/auto.5.8.10274. [DOI] [PubMed] [Google Scholar]
- 117.Yen W.L., Shintani T., Nair U., Cao Y., Richardson B.C., Li Z., Hughson F.M., Baba M., Klionsky D.J. The conserved oligomeric Golgi complex is involved in double-membrane vesicle formation during autophagy. J. Cell Biol. 2010;188:101–114. doi: 10.1083/jcb.200904075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Reggiori F., Shintani T., Nair U., Klionsky D.J. Atg9 cycles between mitochondria and the pre-autophagosomal structure in yeasts. Autophagy. 2005;1:101–109. doi: 10.4161/auto.1.2.1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Puri C., Vicinanza M., Ashkenazi A., Gratian M.J., Zhang Q., Bento C.F., Renna M., Menzies F.M., Rubinsztein D.C. The RAB11A-Positive Compartment Is a Primary Platform for Autophagosome Assembly Mediated by WIPI2 Recognition of PI3P-RAB11A. Dev. Cell. 2018;45:114–131. doi: 10.1016/j.devcel.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Knaevelsrud H., Soreng K., Raiborg C., Haberg K., Rasmuson F., Brech A., Liestol K., Rusten T.E., Stenmark H., Neufeld T.P., et al. Membrane remodeling by the PX-BAR protein SNX18 promotes autophagosome formation. J. Cell Biol. 2013;202:331–349. doi: 10.1083/jcb.201205129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ravikumar B., Moreau K., Jahreiss L., Puri C., Rubinsztein D.C. Plasma membrane contributes to the formation of pre-autophagosomal structures. Nat. Cell Biol. 2010;12:747–757. doi: 10.1038/ncb2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hamasaki M., Furuta N., Matsuda A., Nezu A., Yamamoto A., Fujita N., Oomori H., Noda T., Haraguchi T., Hiraoka Y., et al. Autophagosomes form at ER-mitochondria contact sites. Nature. 2013;495:389–393. doi: 10.1038/nature11910. [DOI] [PubMed] [Google Scholar]
- 123.Reggiori F., Ungermann C. Autophagosome Maturation and Fusion. J. Mol. Biol. 2017;429:486–496. doi: 10.1016/j.jmb.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 124.Zhao Y.G., Zhang H. Formation and maturation of autophagosomes in higher eukaryotes: A social network. Curr. Opin. Cell Biol. 2018;53:29–36. doi: 10.1016/j.ceb.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 125.Yu S., Melia T.J. The coordination of membrane fission and fusion at the end of autophagosome maturation. Curr. Opin. Cell Biol. 2017;47:92–98. doi: 10.1016/j.ceb.2017.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kriegenburg F., Ungermann C., Reggiori F. Coordination of Autophagosome-Lysosome Fusion by Atg8 Family Members. Curr. Biol. 2018;28:R512–R518. doi: 10.1016/j.cub.2018.02.034. [DOI] [PubMed] [Google Scholar]
- 127.Yu L., Chen Y., Tooze S.A. Autophagy pathway: Cellular and molecular mechanisms. Autophagy. 2018;14:207–215. doi: 10.1080/15548627.2017.1378838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nakamura S., Yoshimori T. New insights into autophagosome-lysosome fusion. J. Cell Sci. 2017;130:1209–1216. doi: 10.1242/jcs.196352. [DOI] [PubMed] [Google Scholar]
- 129.Mizushima N., Yoshimori T., Ohsumi Y. The role of Atg proteins in autophagosome formation. Annu. Rev. Cell Dev. Biol. 2011;27:107–132. doi: 10.1146/annurev-cellbio-092910-154005. [DOI] [PubMed] [Google Scholar]
- 130.Itakura E., Mizushima N. Characterization of autophagosome formation site by a hierarchical analysis of mammalian Atg proteins. Autophagy. 2010;6:764–776. doi: 10.4161/auto.6.6.12709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Saxton R.A., Sabatini D.M. mTOR Signaling in Growth, Metabolism, and Disease. Cell. 2017;169:361–371. doi: 10.1016/j.cell.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 132.Wolfson R.L., Sabatini D.M. The Dawn of the Age of Amino Acid Sensors for the mTORC1 Pathway. Cell Metab. 2017;26:301–309. doi: 10.1016/j.cmet.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Jewell J.L., Russell R.C., Guan K.L. Amino acid signalling upstream of mTOR. Nat. Rev. Mol. Cell Biol. 2013;14:133–139. doi: 10.1038/nrm3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mizushima N. The role of the Atg1/ULK1 complex in autophagy regulation. Curr. Opin. Cell Biol. 2010;22:132–139. doi: 10.1016/j.ceb.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 135.Matsunaga K., Morita E., Saitoh T., Akira S., Ktistakis N.T., Izumi T., Noda T., Yoshimori T. Autophagy requires endoplasmic reticulum targeting of the PI3-kinase complex via Atg14L. J. Cell Biol. 2010;190:511–521. doi: 10.1083/jcb.200911141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Matsunaga K., Saitoh T., Tabata K., Omori H., Satoh T., Kurotori N., Maejima I., Shirahama-Noda K., Ichimura T., Isobe T., et al. Two Beclin 1-binding proteins, Atg14L and Rubicon, reciprocally regulate autophagy at different stages. Nat. Cell Biol. 2009;11:385–396. doi: 10.1038/ncb1846. [DOI] [PubMed] [Google Scholar]
- 137.Russell R.C., Tian Y., Yuan H., Park H.W., Chang Y.Y., Kim J., Kim H., Neufeld T.P., Dillin A., Guan K.L. ULK1 induces autophagy by phosphorylating Beclin-1 and activating VPS34 lipid kinase. Nat. Cell Biol. 2013;15:741–750. doi: 10.1038/ncb2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Axe E.L., Walker S.A., Manifava M., Chandra P., Roderick H.L., Habermann A., Griffiths G., Ktistakis N.T. Autophagosome formation from membrane compartments enriched in phosphatidylinositol 3-phosphate and dynamically connected to the endoplasmic reticulum. J. Cell Biol. 2008;182:685–701. doi: 10.1083/jcb.200803137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Polson H.E., de Lartigue J., Rigden D.J., Reedijk M., Urbe S., Clague M.J., Tooze S.A. Mammalian Atg18 (WIPI2) localizes to omegasome-anchored phagophores and positively regulates LC3 lipidation. Autophagy. 2010;6:506–522. doi: 10.4161/auto.6.4.11863. [DOI] [PubMed] [Google Scholar]
- 140.Yamamoto H., Kakuta S., Watanabe T.M., Kitamura A., Sekito T., Kondo-Kakuta C., Ichikawa R., Kinjo M., Ohsumi Y. Atg9 vesicles are an important membrane source during early steps of autophagosome formation. J. Cell Biol. 2012;198:219–233. doi: 10.1083/jcb.201202061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Orsi A., Razi M., Dooley H.C., Robinson D., Weston A.E., Collinson L.M., Tooze S.A. Dynamic and transient interactions of Atg9 with autophagosomes, but not membrane integration, are required for autophagy. Mol. Biol. Cell. 2012;23:1860–1873. doi: 10.1091/mbc.e11-09-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Mari M., Griffith J., Rieter E., Krishnappa L., Klionsky D.J., Reggiori F. An Atg9-containing compartment that functions in the early steps of autophagosome biogenesis. J. Cell Biol. 2010;190:1005–1022. doi: 10.1083/jcb.200912089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Molejon M.I., Ropolo A., Re A.L., Boggio V., Vaccaro M.I. The VMP1-Beclin 1 interaction regulates autophagy induction. Sci. Rep. 2013;3:1055. doi: 10.1038/srep01055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ropolo A., Grasso D., Pardo R., Sacchetti M.L., Archange C., Lo Re A., Seux M., Nowak J., Gonzalez C.D., Iovanna J.L., et al. The pancreatitis-induced vacuole membrane protein 1 triggers autophagy in mammalian cells. J. Biol. Chem. 2007;282:37124–37133. doi: 10.1074/jbc.M706956200. [DOI] [PubMed] [Google Scholar]
- 145.Zhao Y.G., Chen Y., Miao G., Zhao H., Qu W., Li D., Wang Z., Liu N., Li L., Chen S., et al. The ER-Localized Transmembrane Protein EPG-3/VMP1 Regulates SERCA Activity to Control ER-Isolation Membrane Contacts for Autophagosome Formation. Mol. Cell. 2017;67:974–989. doi: 10.1016/j.molcel.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 146.Mizushima N., Sugita H., Yoshimori T., Ohsumi Y. A new protein conjugation system in human. The counterpart of the yeast Apg12p conjugation system essential for autophagy. J. Biol. Chem. 1998;273:33889–33892. doi: 10.1074/jbc.273.51.33889. [DOI] [PubMed] [Google Scholar]
- 147.Mizushima N., Noda T., Yoshimori T., Tanaka Y., Ishii T., George M.D., Klionsky D.J., Ohsumi M., Ohsumi Y. A protein conjugation system essential for autophagy. Nature. 1998;395:395–398. doi: 10.1038/26506. [DOI] [PubMed] [Google Scholar]
- 148.Suzuki K., Kirisako T., Kamada Y., Mizushima N., Noda T., Ohsumi Y. The pre-autophagosomal structure organized by concerted functions of APG genes is essential for autophagosome formation. EMBO J. 2001;20:5971–5981. doi: 10.1093/emboj/20.21.5971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Nakatogawa H., Ichimura Y., Ohsumi Y. Atg8, a ubiquitin-like protein required for autophagosome formation, mediates membrane tethering and hemifusion. Cell. 2007;130:165–178. doi: 10.1016/j.cell.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 150.Fujita N., Itoh T., Omori H., Fukuda M., Noda T., Yoshimori T. The Atg16L complex specifies the site of LC3 lipidation for membrane biogenesis in autophagy. Mol. Biol. Cell. 2008;19:2092–2100. doi: 10.1091/mbc.e07-12-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Mizushima N., Noda T., Ohsumi Y. Apg16p is required for the function of the Apg12p-Apg5p conjugate in the yeast autophagy pathway. EMBO J. 1999;18:3888–3896. doi: 10.1093/emboj/18.14.3888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kuma A., Mizushima N., Ishihara N., Ohsumi Y. Formation of the approximately 350-kDa Apg12-Apg5.Apg16 multimeric complex, mediated by Apg16 oligomerization, is essential for autophagy in yeast. J. Biol. Chem. 2002;277:18619–18625. doi: 10.1074/jbc.M111889200. [DOI] [PubMed] [Google Scholar]
- 153.Kabeya Y., Mizushima N., Ueno T., Yamamoto A., Kirisako T., Noda T., Kominami E., Ohsumi Y., Yoshimori T. LC3, a mammalian homologue of yeast Apg8p, is localized in autophagosome membranes after processing. EMBO J. 2000;19:5720–5728. doi: 10.1093/emboj/19.21.5720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kabeya Y., Mizushima N., Yamamoto A., Oshitani-Okamoto S., Ohsumi Y., Yoshimori T. LC3, GABARAP and GATE16 localize to autophagosomal membrane depending on form-II formation. J. Cell Sci. 2004;117:2805–2812. doi: 10.1242/jcs.01131. [DOI] [PubMed] [Google Scholar]
- 155.Ichimura Y., Kirisako T., Takao T., Satomi Y., Shimonishi Y., Ishihara N., Mizushima N., Tanida I., Kominami E., Ohsumi M., et al. A ubiquitin-like system mediates protein lipidation. Nature. 2000;408:488–492. doi: 10.1038/35044114. [DOI] [PubMed] [Google Scholar]
- 156.Xie Z., Nair U., Klionsky D.J. Atg8 controls phagophore expansion during autophagosome formation. Mol. Biol. Cell. 2008;19:3290–3298. doi: 10.1091/mbc.e07-12-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hanada T., Noda N.N., Satomi Y., Ichimura Y., Fujioka Y., Takao T., Inagaki F., Ohsumi Y. The Atg12-Atg5 conjugate has a novel E3-like activity for protein lipidation in autophagy. J. Biol. Chem. 2007;282:37298–37302. doi: 10.1074/jbc.C700195200. [DOI] [PubMed] [Google Scholar]
- 158.Romanov J., Walczak M., Ibiricu I., Schuchner S., Ogris E., Kraft C., Martens S. Mechanism and functions of membrane binding by the Atg5-Atg12/Atg16 complex during autophagosome formation. EMBO J. 2012;31:4304–4317. doi: 10.1038/emboj.2012.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Matarrese P., Garofalo T., Manganelli V., Gambardella L., Marconi M., Grasso M., Tinari A., Misasi R., Malorni W., Sorice M. Evidence for the involvement of GD3 ganglioside in autophagosome formation and maturation. Autophagy. 2014;10:750–765. doi: 10.4161/auto.27959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Garofalo T., Matarrese P., Manganelli V., Marconi M., Tinari A., Gambardella L., Faggioni A., Misasi R., Sorice M., Malorni W. Evidence for the involvement of lipid rafts localized at the ER-mitochondria associated membranes in autophagosome formation. Autophagy. 2016;12:917–935. doi: 10.1080/15548627.2016.1160971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kimura S., Noda T., Yoshimori T. Dynein-dependent movement of autophagosomes mediates efficient encounters with lysosomes. Cell Struct. Funct. 2008;33:109–122. doi: 10.1247/csf.08005. [DOI] [PubMed] [Google Scholar]
- 162.Cardoso C.M., Groth-Pedersen L., Hoyer-Hansen M., Kirkegaard T., Corcelle E., Andersen J.S., Jaattela M., Nylandsted J. Depletion of kinesin 5B affects lysosomal distribution and stability and induces peri-nuclear accumulation of autophagosomes in cancer cells. PLoS ONE. 2009;4:e4424. doi: 10.1371/journal.pone.0004424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Jager S., Bucci C., Tanida I., Ueno T., Kominami E., Saftig P., Eskelinen E.L. Role for Rab7 in maturation of late autophagic vacuoles. J. Cell Sci. 2004;117:4837–4848. doi: 10.1242/jcs.01370. [DOI] [PubMed] [Google Scholar]
- 164.Gutierrez M.G., Munafo D.B., Beron W., Colombo M.I. Rab7 is required for the normal progression of the autophagic pathway in mammalian cells. J. Cell Sci. 2004;117:2687–2697. doi: 10.1242/jcs.01114. [DOI] [PubMed] [Google Scholar]
- 165.Pankiv S., Johansen T. FYCO1: Linking autophagosomes to microtubule plus end-directing molecular motors. Autophagy. 2010;6:550–552. doi: 10.4161/auto.6.4.11670. [DOI] [PubMed] [Google Scholar]
- 166.Pankiv S., Alemu E.A., Brech A., Bruun J.A., Lamark T., Overvatn A., Bjorkoy G., Johansen T. FYCO1 is a Rab7 effector that binds to LC3 and PI3P to mediate microtubule plus end-directed vesicle transport. J. Cell Biol. 2010;188:253–269. doi: 10.1083/jcb.200907015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Jordens I., Fernandez-Borja M., Marsman M., Dusseljee S., Janssen L., Calafat J., Janssen H., Wubbolts R., Neefjes J. The Rab7 effector protein RILP controls lysosomal transport by inducing the recruitment of dynein-dynactin motors. Curr. Biol. 2001;11:1680–1685. doi: 10.1016/S0960-9822(01)00531-0. [DOI] [PubMed] [Google Scholar]
- 168.Lee J.Y., Koga H., Kawaguchi Y., Tang W., Wong E., Gao Y.S., Pandey U.B., Kaushik S., Tresse E., Lu J., et al. HDAC6 controls autophagosome maturation essential for ubiquitin-selective quality-control autophagy. EMBO J. 2010;29:969–980. doi: 10.1038/emboj.2009.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.McEwan D.G., Popovic D., Gubas A., Terawaki S., Suzuki H., Stadel D., Coxon F.P., Miranda de Stegmann D., Bhogaraju S., Maddi K., et al. PLEKHM1 regulates autophagosome-lysosome fusion through HOPS complex and LC3/GABARAP proteins. Mol. Cell. 2015;57:39–54. doi: 10.1016/j.molcel.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 170.Liang C., Lee J.S., Inn K.S., Gack M.U., Li Q., Roberts E.A., Vergne I., Deretic V., Feng P., Akazawa C., et al. Beclin1-binding UVRAG targets the class C Vps complex to coordinate autophagosome maturation and endocytic trafficking. Nat. Cell Biol. 2008;10:776–787. doi: 10.1038/ncb1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Zhong Y., Wang Q.J., Li X., Yan Y., Backer J.M., Chait B.T., Heintz N., Yue Z. Distinct regulation of autophagic activity by Atg14L and Rubicon associated with Beclin 1-phosphatidylinositol-3-kinase complex. Nat. Cell Biol. 2009;11:468–476. doi: 10.1038/ncb1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Diao J., Li L., Lai Y., Zhong Q. In Vitro Reconstitution of Autophagosome-Lysosome Fusion. Methods Enzymol. 2017;587:365–376. doi: 10.1016/bs.mie.2016.09.065. [DOI] [PubMed] [Google Scholar]
- 173.Diao J., Liu R., Rong Y., Zhao M., Zhang J., Lai Y., Zhou Q., Wilz L.M., Li J., Vivona S., et al. ATG14 promotes membrane tethering and fusion of autophagosomes to endolysosomes. Nature. 2015;520:563–566. doi: 10.1038/nature14147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Nguyen T.N., Padman B.S., Usher J., Oorschot V., Ramm G., Lazarou M. Atg8 family LC3/GABARAP proteins are crucial for autophagosome-lysosome fusion but not autophagosome formation during PINK1/Parkin mitophagy and starvation. J. Cell Biol. 2016;215:857–874. doi: 10.1083/jcb.201607039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yu L., McPhee C.K., Zheng L., Mardones G.A., Rong Y., Peng J., Mi N., Zhao Y., Liu Z., Wan F., et al. Termination of autophagy and reformation of lysosomes regulated by mTOR. Nature. 2010;465:942–946. doi: 10.1038/nature09076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Rong Y., McPhee C.K., Deng S., Huang L., Chen L., Liu M., Tracy K., Baehrecke E.H., Yu L., Lenardo M.J. Spinster is required for autophagic lysosome reformation and mTOR reactivation following starvation. Proc. Natl. Acad. Sci. USA. 2011;108:7826–7831. doi: 10.1073/pnas.1013800108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Liu C.C., Lin Y.C., Chen Y.H., Chen C.M., Pang L.Y., Chen H.A., Wu P.R., Lin M.Y., Jiang S.T., Tsai T.F., et al. Cul3-KLHL20 Ubiquitin Ligase Governs the Turnover of ULK1 and VPS34 Complexes to Control Autophagy Termination. Mol. Cell. 2016;61:84–97. doi: 10.1016/j.molcel.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 178.Gatica D., Lahiri V., Klionsky D.J. Cargo recognition and degradation by selective autophagy. Nat. Cell Biol. 2018;20:233–242. doi: 10.1038/s41556-018-0037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zaffagnini G., Martens S. Mechanisms of Selective Autophagy. J. Mol. Biol. 2016;428:1714–1724. doi: 10.1016/j.jmb.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Anding A.L., Baehrecke E.H. Cleaning House: Selective Autophagy of Organelles. Dev. Cell. 2017;41:10–22. doi: 10.1016/j.devcel.2017.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Melmed R.N., Benitez C.J., Holt S.J. Intermediate cells of the pancreas. 3. Selective autophagy and destruction of beta-granules in intermediate cells of the rat pancreas induced by alloxan and streptozotocin. J. Cell Sci. 1973;13:297–315. doi: 10.1242/jcs.13.1.297. [DOI] [PubMed] [Google Scholar]
- 182.Stolz A., Ernst A., Dikic I. Cargo recognition and trafficking in selective autophagy. Nat. Cell Biol. 2014;16:495–501. doi: 10.1038/ncb2979. [DOI] [PubMed] [Google Scholar]
- 183.Rogov V., Dotsch V., Johansen T., Kirkin V. Interactions between autophagy receptors and ubiquitin-like proteins form the molecular basis for selective autophagy. Mol. Cell. 2014;53:167–178. doi: 10.1016/j.molcel.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 184.Birgisdottir A.B., Lamark T., Johansen T. The LIR motif—Crucial for selective autophagy. J. Cell Sci. 2013;126:3237–3247. doi: 10.1242/jcs.126128. [DOI] [PubMed] [Google Scholar]
- 185.Johansen T., Lamark T. Selective autophagy mediated by autophagic adapter proteins. Autophagy. 2011;7:279–296. doi: 10.4161/auto.7.3.14487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kirkin V., McEwan D.G., Novak I., Dikic I. A role for ubiquitin in selective autophagy. Mol. Cell. 2009;34:259–269. doi: 10.1016/j.molcel.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 187.Rogov V.V., Stolz A., Ravichandran A.C., Rios-Szwed D.O., Suzuki H., Kniss A., Lohr F., Wakatsuki S., Dotsch V., Dikic I., et al. Structural and functional analysis of the GABARAP interaction motif (GIM) EMBO Rep. 2017;18:1382–1396. doi: 10.15252/embr.201643587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Fracchiolla D., Sawa-Makarska J., Martens S. Beyond Atg8 binding: The role of AIM/LIR motifs in autophagy. Autophagy. 2017;13:978–979. doi: 10.1080/15548627.2016.1277311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Schaaf M.B., Keulers T.G., Vooijs M.A., Rouschop K.M. LC3/GABARAP family proteins: Autophagy-(un)related functions. FASEB J. 2016;30:3961–3978. doi: 10.1096/fj.201600698R. [DOI] [PubMed] [Google Scholar]
- 190.Jacomin A.C., Samavedam S., Promponas V., Nezis I.P. iLIR database: A web resource for LIR motif-containing proteins in eukaryotes. Autophagy. 2016;12:1945–1953. doi: 10.1080/15548627.2016.1207016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Fracchiolla D., Sawa-Makarska J., Zens B., Ruiter A., Zaffagnini G., Brezovich A., Romanov J., Runggatscher K., Kraft C., Zagrovic B., et al. Mechanism of cargo-directed Atg8 conjugation during selective autophagy. eLife. 2016;5 doi: 10.7554/eLife.18544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Okamoto K. Organellophagy: Eliminating cellular building blocks via selective autophagy. J. Cell Biol. 2014;205:435–445. doi: 10.1083/jcb.201402054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Bellot G., Garcia-Medina R., Gounon P., Chiche J., Roux D., Pouyssegur J., Mazure N.M. Hypoxia-induced autophagy is mediated through hypoxia-inducible factor induction of BNIP3 and BNIP3L via their BH3 domains. Mol. Cell Biol. 2009;29:2570–2581. doi: 10.1128/MCB.00166-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Zhang H., Bosch-Marce M., Shimoda L.A., Tan Y.S., Baek J.H., Wesley J.B., Gonzalez F.J., Semenza G.L. Mitochondrial autophagy is an HIF-1-dependent adaptive metabolic response to hypoxia. J. Biol. Chem. 2008;283:10892–10903. doi: 10.1074/jbc.M800102200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 195.Frank M., Duvezin-Caubet S., Koob S., Occhipinti A., Jagasia R., Petcherski A., Ruonala M.O., Priault M., Salin B., Reichert A.S. Mitophagy is triggered by mild oxidative stress in a mitochondrial fission dependent manner. Biochim. Biophys. Acta. 2012;1823:2297–2310. doi: 10.1016/j.bbamcr.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 196.Xiao B., Goh J.Y., Xiao L., Xian H., Lim K.L., Liou Y.C. Reactive oxygen species trigger Parkin/PINK1 pathway-dependent mitophagy by inducing mitochondrial recruitment of Parkin. J. Biol. Chem. 2017;292:16697–16708. doi: 10.1074/jbc.M117.787739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Xiao B., Deng X., Lim G.G.Y., Xie S., Zhou Z.D., Lim K.L., Tan E.K. Superoxide drives progression of Parkin/PINK1-dependent mitophagy following translocation of Parkin to mitochondria. Cell Death Dis. 2017;8:e3097. doi: 10.1038/cddis.2017.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Narendra D., Tanaka A., Suen D.F., Youle R.J. Parkin is recruited selectively to impaired mitochondria and promotes their autophagy. J. Cell Biol. 2008;183:795–803. doi: 10.1083/jcb.200809125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Matsuda N., Sato S., Shiba K., Okatsu K., Saisho K., Gautier C.A., Sou Y.S., Saiki S., Kawajiri S., Sato F., et al. PINK1 stabilized by mitochondrial depolarization recruits Parkin to damaged mitochondria and activates latent Parkin for mitophagy. J. Cell Biol. 2010;189:211–221. doi: 10.1083/jcb.200910140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Narendra D.P., Jin S.M., Tanaka A., Suen D.F., Gautier C.A., Shen J., Cookson M.R., Youle R.J. PINK1 is selectively stabilized on impaired mitochondria to activate Parkin. PLoS Biol. 2010;8:e1000298. doi: 10.1371/journal.pbio.1000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ashrafi G., Schwarz T.L. The pathways of mitophagy for quality control and clearance of mitochondria. Cell Death Differ. 2013;20:31–42. doi: 10.1038/cdd.2012.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Pickles S., Vigie P., Youle R.J. Mitophagy and Quality Control Mechanisms in Mitochondrial Maintenance. Curr. Biol. 2018;28:R170–R185. doi: 10.1016/j.cub.2018.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Jin S.M., Lazarou M., Wang C., Kane L.A., Narendra D.P., Youle R.J. Mitochondrial membrane potential regulates PINK1 import and proteolytic destabilization by PARL. J. Cell Biol. 2010;191:933–942. doi: 10.1083/jcb.201008084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Meissner C., Lorenz H., Weihofen A., Selkoe D.J., Lemberg M.K. The mitochondrial intramembrane protease PARL cleaves human Pink1 to regulate Pink1 trafficking. J. Neurochem. 2011;117:856–867. doi: 10.1111/j.1471-4159.2011.07253.x. [DOI] [PubMed] [Google Scholar]
- 205.Vives-Bauza C., Zhou C., Huang Y., Cui M., de Vries R.L., Kim J., May J., Tocilescu M.A., Liu W., Ko H.S., et al. PINK1-dependent recruitment of Parkin to mitochondria in mitophagy. Proc. Natl. Acad. Sci. USA. 2010;107:378–383. doi: 10.1073/pnas.0911187107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Koyano F., Okatsu K., Kosako H., Tamura Y., Go E., Kimura M., Kimura Y., Tsuchiya H., Yoshihara H., Hirokawa T., et al. Ubiquitin is phosphorylated by PINK1 to activate parkin. Nature. 2014;510:162–166. doi: 10.1038/nature13392. [DOI] [PubMed] [Google Scholar]
- 207.Kane L.A., Lazarou M., Fogel A.I., Li Y., Yamano K., Sarraf S.A., Banerjee S., Youle R.J. PINK1 phosphorylates ubiquitin to activate Parkin E3 ubiquitin ligase activity. J. Cell Biol. 2014;205:143–153. doi: 10.1083/jcb.201402104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Yang J.Y., Yang W.Y. Bit-by-bit autophagic removal of parkin-labelled mitochondria. Nat. Commun. 2013;4:2428. doi: 10.1038/ncomms3428. [DOI] [PubMed] [Google Scholar]
- 209.Lazarou M., Sliter D.A., Kane L.A., Sarraf S.A., Wang C., Burman J.L., Sideris D.P., Fogel A.I., Youle R.J. The ubiquitin kinase PINK1 recruits autophagy receptors to induce mitophagy. Nature. 2015;524:309–314. doi: 10.1038/nature14893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Heo J.M., Ordureau A., Paulo J.A., Rinehart J., Harper J.W. The PINK1-PARKIN Mitochondrial Ubiquitylation Pathway Drives a Program of OPTN/NDP52 Recruitment and TBK1 Activation to Promote Mitophagy. Mol. Cell. 2015;60:7–20. doi: 10.1016/j.molcel.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Richter B., Sliter D.A., Herhaus L., Stolz A., Wang C., Beli P., Zaffagnini G., Wild P., Martens S., Wagner S.A., et al. Phosphorylation of OPTN by TBK1 enhances its binding to Ub chains and promotes selective autophagy of damaged mitochondria. Proc. Natl. Acad. Sci. USA. 2016;113:4039–4044. doi: 10.1073/pnas.1523926113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Matsumoto G., Shimogori T., Hattori N., Nukina N. TBK1 controls autophagosomal engulfment of polyubiquitinated mitochondria through p62/SQSTM1 phosphorylation. Hum. Mol. Genet. 2015;24:4429–4442. doi: 10.1093/hmg/ddv179. [DOI] [PubMed] [Google Scholar]
- 213.Ding W.X., Ni H.M., Li M., Liao Y., Chen X., Stolz D.B., Dorn G.W., 2nd, Yin X.M. Nix is critical to two distinct phases of mitophagy, reactive oxygen species-mediated autophagy induction and Parkin-ubiquitin-p62-mediated mitochondrial priming. J. Biol. Chem. 2010;285:27879–27890. doi: 10.1074/jbc.M110.119537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Novak I., Kirkin V., McEwan D.G., Zhang J., Wild P., Rozenknop A., Rogov V., Lohr F., Popovic D., Occhipinti A., et al. Nix is a selective autophagy receptor for mitochondrial clearance. EMBO Rep. 2010;11:45–51. doi: 10.1038/embor.2009.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Quinsay M.N., Thomas R.L., Lee Y., Gustafsson A.B. Bnip3-mediated mitochondrial autophagy is independent of the mitochondrial permeability transition pore. Autophagy. 2010;6:855–862. doi: 10.4161/auto.6.7.13005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Liu L., Feng D., Chen G., Chen M., Zheng Q., Song P., Ma Q., Zhu C., Wang R., Qi W., et al. Mitochondrial outer-membrane protein FUNDC1 mediates hypoxia-induced mitophagy in mammalian cells. Nat. Cell Biol. 2012;14:177–185. doi: 10.1038/ncb2422. [DOI] [PubMed] [Google Scholar]
- 217.Wu W., Tian W., Hu Z., Chen G., Huang L., Li W., Zhang X., Xue P., Zhou C., Liu L., et al. ULK1 translocates to mitochondria and phosphorylates FUNDC1 to regulate mitophagy. EMBO Rep. 2014;15:566–575. doi: 10.1002/embr.201438501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Lu K., Psakhye I., Jentsch S. Autophagic clearance of polyQ proteins mediated by ubiquitin-Atg8 adaptors of the conserved CUET protein family. Cell. 2014;158:549–563. doi: 10.1016/j.cell.2014.05.048. [DOI] [PubMed] [Google Scholar]
- 219.Wei Y., Chiang W.C., Sumpter R., Jr., Mishra P., Levine B. Prohibitin 2 Is an Inner Mitochondrial Membrane Mitophagy Receptor. Cell. 2017;168:224–238. doi: 10.1016/j.cell.2016.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Bingol B., Tea J.S., Phu L., Reichelt M., Bakalarski C.E., Song Q., Foreman O., Kirkpatrick D.S., Sheng M. The mitochondrial deubiquitinase USP30 opposes parkin-mediated mitophagy. Nature. 2014;510:370–375. doi: 10.1038/nature13418. [DOI] [PubMed] [Google Scholar]
- 221.Wang Y., Serricchio M., Jauregui M., Shanbhag R., Stoltz T., Di Paolo C.T., Kim P.K., McQuibban G.A. Deubiquitinating enzymes regulate PARK2-mediated mitophagy. Autophagy. 2015;11:595–606. doi: 10.1080/15548627.2015.1034408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Motley A.M., Nuttall J.M., Hettema E.H. Pex3-anchored Atg36 tags peroxisomes for degradation in Saccharomyces cerevisiae. EMBO J. 2012;31:2852–2868. doi: 10.1038/emboj.2012.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kim P.K., Hailey D.W., Mullen R.T., Lippincott-Schwartz J. Ubiquitin signals autophagic degradation of cytosolic proteins and peroxisomes. Proc. Natl. Acad. Sci. USA. 2008;105:20567–20574. doi: 10.1073/pnas.0810611105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Deosaran E., Larsen K.B., Hua R., Sargent G., Wang Y., Kim S., Lamark T., Jauregui M., Law K., Lippincott-Schwartz J., et al. NBR1 acts as an autophagy receptor for peroxisomes. J. Cell Sci. 2013;126:939–952. doi: 10.1242/jcs.114819. [DOI] [PubMed] [Google Scholar]
- 225.Shibata M., Oikawa K., Yoshimoto K., Kondo M., Mano S., Yamada K., Hayashi M., Sakamoto W., Ohsumi Y., Nishimura M. Highly oxidized peroxisomes are selectively degraded via autophagy in Arabidopsis. Plant. Cell. 2013;25:4967–4983. doi: 10.1105/tpc.113.116947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Tanaka C., Tan L.J., Mochida K., Kirisako H., Koizumi M., Asai E., Sakoh-Nakatogawa M., Ohsumi Y., Nakatogawa H. Hrr25 triggers selective autophagy-related pathways by phosphorylating receptor proteins. J. Cell Biol. 2014;207:91–105. doi: 10.1083/jcb.201402128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Zhang J., Tripathi D.N., Jing J., Alexander A., Kim J., Powell R.T., Dere R., Tait-Mulder J., Lee J.H., Paull T.T., et al. ATM functions at the peroxisome to induce pexophagy in response to ROS. Nat. Cell Biol. 2015;17:1259–1269. doi: 10.1038/ncb3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Sargent G., van Zutphen T., Shatseva T., Zhang L., Di Giovanni V., Bandsma R., Kim P.K. PEX2 is the E3 ubiquitin ligase required for pexophagy during starvation. J. Cell Biol. 2016;214:677–690. doi: 10.1083/jcb.201511034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Mochida K., Oikawa Y., Kimura Y., Kirisako H., Hirano H., Ohsumi Y., Nakatogawa H. Receptor-mediated selective autophagy degrades the endoplasmic reticulum and the nucleus. Nature. 2015;522:359–362. doi: 10.1038/nature14506. [DOI] [PubMed] [Google Scholar]
- 230.Khaminets A., Heinrich T., Mari M., Grumati P., Huebner A.K., Akutsu M., Liebmann L., Stolz A., Nietzsche S., Koch N., et al. Regulation of endoplasmic reticulum turnover by selective autophagy. Nature. 2015;522:354–358. doi: 10.1038/nature14498. [DOI] [PubMed] [Google Scholar]
- 231.Grumati P., Morozzi G., Holper S., Mari M., Harwardt M.I., Yan R., Muller S., Reggiori F., Heilemann M., Dikic I. Full length RTN3 regulates turnover of tubular endoplasmic reticulum via selective autophagy. eLife. 2017;6 doi: 10.7554/eLife.25555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Seibenhener M.L., Babu J.R., Geetha T., Wong H.C., Krishna N.R., Wooten M.W. Sequestosome 1/p62 is a polyubiquitin chain binding protein involved in ubiquitin proteasome degradation. Mol. Cell Biol. 2004;24:8055–8068. doi: 10.1128/MCB.24.18.8055-8068.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Olzmann J.A., Chin L.S. Parkin-mediated K63-linked polyubiquitination: A signal for targeting misfolded proteins to the aggresome-autophagy pathway. Autophagy. 2008;4:85–87. doi: 10.4161/auto.5172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Olzmann J.A., Li L., Chudaev M.V., Chen J., Perez F.A., Palmiter R.D., Chin L.S. Parkin-mediated K63-linked polyubiquitination targets misfolded DJ-1 to aggresomes via binding to HDAC6. J. Cell Biol. 2007;178:1025–1038. doi: 10.1083/jcb.200611128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Kirkin V., Lamark T., Sou Y.S., Bjorkoy G., Nunn J.L., Bruun J.A., Shvets E., McEwan D.G., Clausen T.H., Wild P., et al. A role for NBR1 in autophagosomal degradation of ubiquitinated substrates. Mol. Cell. 2009;33:505–516. doi: 10.1016/j.molcel.2009.01.020. [DOI] [PubMed] [Google Scholar]
- 236.Filimonenko M., Isakson P., Finley K.D., Anderson M., Jeong H., Melia T.J., Bartlett B.J., Myers K.M., Birkeland H.C., Lamark T., et al. The selective macroautophagic degradation of aggregated proteins requires the PI3P-binding protein Alfy. Mol. Cell. 2010;38:265–279. doi: 10.1016/j.molcel.2010.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Clausen T.H., Lamark T., Isakson P., Finley K., Larsen K.B., Brech A., Overvatn A., Stenmark H., Bjorkoy G., Simonsen A., et al. p62/SQSTM1 and ALFY interact to facilitate the formation of p62 bodies/ALIS and their degradation by autophagy. Autophagy. 2010;6:330–344. doi: 10.4161/auto.6.3.11226. [DOI] [PubMed] [Google Scholar]
- 238.Simonsen A., Birkeland H.C., Gillooly D.J., Mizushima N., Kuma A., Yoshimori T., Slagsvold T., Brech A., Stenmark H. Alfy, a novel FYVE-domain-containing protein associated with protein granules and autophagic membranes. J. Cell Sci. 2004;117:4239–4251. doi: 10.1242/jcs.01287. [DOI] [PubMed] [Google Scholar]
- 239.Maejima I., Takahashi A., Omori H., Kimura T., Takabatake Y., Saitoh T., Yamamoto A., Hamasaki M., Noda T., Isaka Y., et al. Autophagy sequesters damaged lysosomes to control lysosomal biogenesis and kidney injury. EMBO J. 2013;32:2336–2347. doi: 10.1038/emboj.2013.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Hung Y.H., Chen L.M., Yang J.Y., Yang W.Y. Spatiotemporally controlled induction of autophagy-mediated lysosome turnover. Nat. Commun. 2013;4:2111. doi: 10.1038/ncomms3111. [DOI] [PubMed] [Google Scholar]
- 241.Wyant G.A., Abu-Remaileh M., Frenkel E.M., Laqtom N.N., Dharamdasani V., Lewis C.A., Chan S.H., Heinze I., Ori A., Sabatini D.M. NUFIP1 is a ribosome receptor for starvation-induced ribophagy. Science. 2018;360:751–758. doi: 10.1126/science.aar2663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.An H., Harper J.W. Systematic analysis of ribophagy in human cells reveals bystander flux during selective autophagy. Nat. Cell Biol. 2018;20:135–143. doi: 10.1038/s41556-017-0007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Shibata M., Yoshimura K., Furuya N., Koike M., Ueno T., Komatsu M., Arai H., Tanaka K., Kominami E., Uchiyama Y. The MAP1-LC3 conjugation system is involved in lipid droplet formation. Biochem. Biophys. Res. Commun. 2009;382:419–423. doi: 10.1016/j.bbrc.2009.03.039. [DOI] [PubMed] [Google Scholar]
- 244.Singh R., Kaushik S., Wang Y., Xiang Y., Novak I., Komatsu M., Tanaka K., Cuervo A.M., Czaja M.J. Autophagy regulates lipid metabolism. Nature. 2009;458:1131–1135. doi: 10.1038/nature07976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Mancias J.D., Wang X., Gygi S.P., Harper J.W., Kimmelman A.C. Quantitative proteomics identifies NCOA4 as the cargo receptor mediating ferritinophagy. Nature. 2014;509:105–109. doi: 10.1038/nature13148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Hou W., Xie Y., Song X., Sun X., Lotze M.T., Zeh H.J., 3rd, Kang R., Tang D. Autophagy promotes ferroptosis by degradation of ferritin. Autophagy. 2016;12:1425–1428. doi: 10.1080/15548627.2016.1187366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Mancias J.D., Pontano Vaites L., Nissim S., Biancur D.E., Kim A.J., Wang X., Liu Y., Goessling W., Kimmelman A.C., Harper J.W. Ferritinophagy via NCOA4 is required for erythropoiesis and is regulated by iron dependent HERC2-mediated proteolysis. eLife. 2015;4 doi: 10.7554/eLife.10308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Bellelli R., Federico G., Matte A., Colecchia D., Iolascon A., Chiariello M., Santoro M., De Franceschi L., Carlomagno F. NCOA4 Deficiency Impairs Systemic Iron Homeostasis. Cell Rep. 2016;14:411–421. doi: 10.1016/j.celrep.2015.12.065. [DOI] [PubMed] [Google Scholar]
- 249.Orvedahl A., MacPherson S., Sumpter R., Jr., Talloczy Z., Zou Z., Levine B. Autophagy protects against Sindbis virus infection of the central nervous system. Cell Host Microbe. 2010;7:115–127. doi: 10.1016/j.chom.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Liu Y., Schiff M., Czymmek K., Talloczy Z., Levine B., Dinesh-Kumar S.P. Autophagy regulates programmed cell death during the plant innate immune response. Cell. 2005;121:567–577. doi: 10.1016/j.cell.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 251.Liang X.H., Kleeman L.K., Jiang H.H., Gordon G., Goldman J.E., Berry G., Herman B., Levine B. Protection against fatal Sindbis virus encephalitis by beclin, a novel Bcl-2-interacting protein. J. Virol. 1998;72:8586–8596. doi: 10.1128/jvi.72.11.8586-8596.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Verlhac P., Gregoire I.P., Azocar O., Petkova D.S., Baguet J., Viret C., Faure M. Autophagy receptor NDP52 regulates pathogen-containing autophagosome maturation. Cell Host Microbe. 2015;17:515–525. doi: 10.1016/j.chom.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 253.Wild P., Farhan H., McEwan D.G., Wagner S., Rogov V.V., Brady N.R., Richter B., Korac J., Waidmann O., Choudhary C., et al. Phosphorylation of the autophagy receptor optineurin restricts Salmonella growth. Science. 2011;333:228–233. doi: 10.1126/science.1205405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Pilli M., Arko-Mensah J., Ponpuak M., Roberts E., Master S., Mandell M.A., Dupont N., Ornatowski W., Jiang S., Bradfute S.B., et al. TBK-1 promotes autophagy-mediated antimicrobial defense by controlling autophagosome maturation. Immunity. 2012;37:223–234. doi: 10.1016/j.immuni.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Ichimura Y., Waguri S., Sou Y.S., Kageyama S., Hasegawa J., Ishimura R., Saito T., Yang Y., Kouno T., Fukutomi T., et al. Phosphorylation of p62 activates the Keap1-Nrf2 pathway during selective autophagy. Mol. Cell. 2013;51:618–631. doi: 10.1016/j.molcel.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 256.Ishimura R., Tanaka K., Komatsu M. Dissection of the role of p62/Sqstm1 in activation of Nrf2 during xenophagy. FEBS Lett. 2014;588:822–828. doi: 10.1016/j.febslet.2014.01.045. [DOI] [PubMed] [Google Scholar]
- 257.Maiuri M.C., Zalckvar E., Kimchi A., Kroemer G. Self-eating and self-killing: Crosstalk between autophagy and apoptosis. Nat. Rev. Mol. Cell Biol. 2007;8:741–752. doi: 10.1038/nrm2239. [DOI] [PubMed] [Google Scholar]
- 258.Eisenberg-Lerner A., Bialik S., Simon H.U., Kimchi A. Life and death partners: Apoptosis, autophagy and the cross-talk between them. Cell Death Differ. 2009;16:966–975. doi: 10.1038/cdd.2009.33. [DOI] [PubMed] [Google Scholar]
- 259.Nikoletopoulou V., Markaki M., Palikaras K., Tavernarakis N. Crosstalk between apoptosis, necrosis and autophagy. Biochim. Biophys. Acta. 2013;1833:3448–3459. doi: 10.1016/j.bbamcr.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 260.Shimizu S., Kanaseki T., Mizushima N., Mizuta T., Arakawa-Kobayashi S., Thompson C.B., Tsujimoto Y. Role of Bcl-2 family proteins in a non-apoptotic programmed cell death dependent on autophagy genes. Nat. Cell Biol. 2004;6:1221–1228. doi: 10.1038/ncb1192. [DOI] [PubMed] [Google Scholar]
- 261.Boya P., Gonzalez-Polo R.A., Casares N., Perfettini J.L., Dessen P., Larochette N., Metivier D., Meley D., Souquere S., Yoshimori T., et al. Inhibition of macroautophagy triggers apoptosis. Mol. Cell Biol. 2005;25:1025–1040. doi: 10.1128/MCB.25.3.1025-1040.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Hara T., Nakamura K., Matsui M., Yamamoto A., Nakahara Y., Suzuki-Migishima R., Yokoyama M., Mishima K., Saito I., Okano H., et al. Suppression of basal autophagy in neural cells causes neurodegenerative disease in mice. Nature. 2006;441:885–889. doi: 10.1038/nature04724. [DOI] [PubMed] [Google Scholar]
- 263.Pua H.H., Dzhagalov I., Chuck M., Mizushima N., He Y.W. A critical role for the autophagy gene Atg5 in T cell survival and proliferation. J. Exp. Med. 2007;204:25–31. doi: 10.1084/jem.20061303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Baehrecke E.H. Autophagy: Dual roles in life and death? Nat. Rev. Mol. Cell Biol. 2005;6:505–510. doi: 10.1038/nrm1666. [DOI] [PubMed] [Google Scholar]
- 265.Levine B., Yuan J. Autophagy in cell death: An innocent convict? J. Clin. Investg. 2005;115:2679–2688. doi: 10.1172/JCI26390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Espert L., Denizot M., Grimaldi M., Robert-Hebmann V., Gay B., Varbanov M., Codogno P., Biard-Piechaczyk M. Autophagy is involved in T cell death after binding of HIV-1 envelope proteins to CXCR4. J. Clin. Investig. 2006;116:2161–2172. doi: 10.1172/JCI26185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Yu L., Wan F., Dutta S., Welsh S., Liu Z., Freundt E., Baehrecke E.H., Lenardo M. Autophagic programmed cell death by selective catalase degradation. Proc. Natl. Acad. Sci. USA. 2006;103:4952–4957. doi: 10.1073/pnas.0511288103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Liu Y., Shoji-Kawata S., Sumpter R.M., Jr., Wei Y., Ginet V., Zhang L., Posner B., Tran K.A., Green D.R., Xavier R.J., et al. Autosis is a Na+, K+-ATPase-regulated form of cell death triggered by autophagy-inducing peptides, starvation, and hypoxia-ischemia. Proc. Natl. Acad. Sci. USA. 2013;110:20364–20371. doi: 10.1073/pnas.1319661110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Liu Y., Levine B. Autosis and autophagic cell death: The dark side of autophagy. Cell Death Differ. 2015;22:367–376. doi: 10.1038/cdd.2014.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Deter R.L. Quantitative characterization of dense body, autophagic vacuole, and acid phosphatase-bearing particle populations during the early phases of glucagon-induced autophagy in rat liver. J. Cell Biol. 1971;48:473–489. doi: 10.1083/jcb.48.3.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Grasso P., Gangolli S.D., Wright M., Hendy R. Liver enlargement and autophagy in rats. J. Pathol. 1972;107:Pxvi. [PubMed] [Google Scholar]
- 272.Hendy R., Grasso P. Autophagy in acute liver damage produced in the rat by dimethylnitrosamine. Chem. Biol. Interact. 1972;5:401–413. doi: 10.1016/0009-2797(72)90077-4. [DOI] [PubMed] [Google Scholar]
- 273.Pfeifer U. Cellular autophagy: Glycogen segregation in early stages of a partial liver atrophy. Virchows Arch. B Cell Pathol. 1970;5:242–253. [PubMed] [Google Scholar]
- 274.Pfeifer U. Cellular autophagy and cell atrophy in the Rat liver during long-term starvation. A quantitative morphological study with regard to diurnal variations. Virchows Arch. B Cell Pathol. 1973;12:195–211. doi: 10.1007/BF02893998. [DOI] [PubMed] [Google Scholar]
- 275.Krustev L.P. Cell autophagy of the liver in starvation and undernutrition. Bibl. Nutr. Dieta. 1976:145–154. doi: 10.1159/000399079. [DOI] [PubMed] [Google Scholar]
- 276.Shelburne J.D., Arstila A.U., Trump B.F. Studies on cellular autophagocytosis. The relationship of autophagocytosis to protein synthesis and to energy metabolism in Rat liver and flounder kidney tubules in vitro. Am. J. Pathol. 1973;73:641–670. [PMC free article] [PubMed] [Google Scholar]
- 277.Rumpelt H.J., Weisbach T. Effect of cycloheximide on glucagon-induced autophagy. Quantitative examinations on hepatocytes in the rat. Am. J. Pathol. 1978;91:49–56. [PMC free article] [PubMed] [Google Scholar]
- 278.Shelburne J.D., Arstila A.U., Trump B.F. Studies on cellular autophagocytosis. Cyclic AMP- and dibutyryl cyclic AMP-stimulated autophagy in rat liver. Am. J. Pathol. 1973;72:521–540. [PMC free article] [PubMed] [Google Scholar]
- 279.Aguas A.P., Soares J.O., Nunes J.F. Autophagy in mouse hepatocytes induced by lysine acetylsalicylate. Experientia. 1978;34:1618–1619. doi: 10.1007/BF02034711. [DOI] [PubMed] [Google Scholar]
- 280.Salas M., Tuchweber B., Kourounakis P., Selye H. Temperature-dependence of stress-induced hepatic autophagy. Experientia. 1977;33:612–614. doi: 10.1007/BF01946531. [DOI] [PubMed] [Google Scholar]
- 281.Arstila A.U., Nuuja I.J., Trump B.F. Studies on cellular autophagocytosis. Vinblastine-induced autophagy in the rat liver. Exp. Cell Res. 1974;87:249–252. doi: 10.1016/0014-4827(74)90477-7. [DOI] [PubMed] [Google Scholar]
- 282.Mortimore G.E., Hutson N.J., Surmacz C.A. Quantitative correlation between proteolysis and macro- and microautophagy in mouse hepatocytes during starvation and refeeding. Proc. Natl. Acad. Sci. USA. 1983;80:2179–2183. doi: 10.1073/pnas.80.8.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Novikoff A.B., Shin W.Y. Endoplasmic reticulum and autophagy in rat hepatocytes. Proc. Natl. Acad. Sci. USA. 1978;75:5039–5042. doi: 10.1073/pnas.75.10.5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Hirsimaki P., Reunanen H. Studies on vinblastine-induced autophagocytosis in mouse liver. II. Origin of membranes and acquisition of acid phosphatase. Histochemistry. 1980;67:139–153. doi: 10.1007/BF00493232. [DOI] [PubMed] [Google Scholar]
- 285.Reunanen H., Hirsimaki P. Studies on vinblastine-induced autophagocytosis in mouse liver. IV. Origin of membranes. Histochemistry. 1983;79:59–67. doi: 10.1007/BF00494342. [DOI] [PubMed] [Google Scholar]
- 286.Reunanen H., Punnonen E.L., Hirsimaki P. Studies on vinblastine-induced autophagocytosis in mouse liver. V. A cytochemical study on the origin of membranes. Histochemistry. 1985;83:513–517. doi: 10.1007/BF00492453. [DOI] [PubMed] [Google Scholar]
- 287.Marzella L., Ahlberg J., Glaumann H. Isolation of autophagic vacuoles from rat liver: Morphological and biochemical characterization. J. Cell Biol. 1982;93:144–154. doi: 10.1083/jcb.93.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Deter R.L. Analog modeling of glucagon-induced autophagy in rat liver. I. Conceptual and mathematical model of telolysosome-autophagosome-autolysosome interaction. Exp. Cell Res. 1975;94:122–126. doi: 10.1016/0014-4827(75)90538-8. [DOI] [PubMed] [Google Scholar]
- 289.Deter R.L. Analog modeling of glucagon-induced autophagy in rat liver. II. Evaluation of iron labeling as a means for identifying telolysosome, autophagosome and autolysosome populations. Exp. Cell Res. 1975;94:127–139. doi: 10.1016/0014-4827(75)90539-X. [DOI] [PubMed] [Google Scholar]
- 290.Hopgood M.F., Clark M.G., Ballard F.J. Protein degradation in hepatocyte monolayers. Effects of glucagon, adenosine 3′:5′-cyclic monophosphate and insulin. Biochem. J. 1980;186:71–79. doi: 10.1042/bj1860071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Marzella L., Sandberg P.O., Glaumann H. Autophagic degradation in Rat liver after vinblastine treatment. Exp. Cell Res. 1980;128:291–301. doi: 10.1016/0014-4827(80)90065-8. [DOI] [PubMed] [Google Scholar]
- 292.Schworer C.M., Cox J.R., Mortimore G.E. Alteration of lysosomal density by sequestered glycogen during deprivation-induced autophagy in rat liver. Biochem. Biophys. Res. Commun. 1979;87:163–170. doi: 10.1016/0006-291X(79)91661-9. [DOI] [PubMed] [Google Scholar]
- 293.Searle J., Lawson T.A., Abbott P.J., Harmon B., Kerr J.F. An electron-microscope study of the mode of cell death induced by cancer-chemotherapeutic agents in populations of proliferating normal and neoplastic cells. J. Pathol. 1975;116:129–138. doi: 10.1002/path.1711160302. [DOI] [PubMed] [Google Scholar]
- 294.Seglen P.O., Gordon P.B., Poli A. Amino acid inhibition of the autophagic/lysosomal pathway of protein degradation in isolated rat hepatocytes. Biochim. Biophys. Acta. 1980;630:103–118. doi: 10.1016/0304-4165(80)90141-5. [DOI] [PubMed] [Google Scholar]
- 295.Iwamasa T., Tsuru T., Hamada T., Takeuchi T. Physicochemical and ultrastructural studies on glycogenosomes in newborn rat hepatocytes. Pathol. Res. Pract. 1980;167:363–373. doi: 10.1016/S0344-0338(80)80065-3. [DOI] [PubMed] [Google Scholar]
- 296.Lardeux B.R., Mortimore G.E. Amino acid and hormonal control of macromolecular turnover in perfused rat liver. Evidence for selective autophagy. J. Biol. Chem. 1987;262:14514–14519. [PubMed] [Google Scholar]
- 297.Cuervo A.M., Palmer A., Rivett A.J., Knecht E. Degradation of proteasomes by lysosomes in rat liver. Eur. J. Biochem. 1995;227:792–800. doi: 10.1111/j.1432-1033.1995.tb20203.x. [DOI] [PubMed] [Google Scholar]
- 298.Schneider P.D., Gorschboth C.M. Limiting ischemic liver injury by interfering with lysosomal autophagy. J. Surg Res. 1983;34:550–554. doi: 10.1016/0022-4804(83)90108-7. [DOI] [PubMed] [Google Scholar]
- 299.Schwarze P.E., Seglen P.O. Reduced autophagic activity, improved protein balance and enhanced in vitro survival of hepatocytes isolated from carcinogen-treated rats. Exp. Cell Res. 1985;157:15–28. doi: 10.1016/0014-4827(85)90148-X. [DOI] [PubMed] [Google Scholar]
- 300.Ollinger K., Roberg K. Nutrient deprivation of cultured rat hepatocytes increases the desferrioxamine-available iron pool and augments the sensitivity to hydrogen peroxide. J. Biol. Chem. 1997;272:23707–23711. doi: 10.1074/jbc.272.38.23707. [DOI] [PubMed] [Google Scholar]
- 301.Rautou P.E., Cazals-Hatem D., Moreau R., Francoz C., Feldmann G., Lebrec D., Ogier-Denis E., Bedossa P., Valla D., Durand F. Acute liver cell damage in patients with anorexia nervosa: A possible role of starvation-induced hepatocyte autophagy. Gastroenterology. 2008;135:840–848. doi: 10.1053/j.gastro.2008.05.055. [DOI] [PubMed] [Google Scholar]
- 302.Shigemitsu K., Tsujishita Y., Hara K., Nanahoshi M., Avruch J., Yonezawa K. Regulation of translational effectors by amino acid and mammalian target of rapamycin signaling pathways. Possible involvement of autophagy in cultured hepatoma cells. J. Biol. Chem. 1999;274:1058–1065. doi: 10.1074/jbc.274.2.1058. [DOI] [PubMed] [Google Scholar]
- 303.Ezaki J., Matsumoto N., Takeda-Ezaki M., Komatsu M., Takahashi K., Hiraoka Y., Taka H., Fujimura T., Takehana K., Yoshida M., et al. Liver autophagy contributes to the maintenance of blood glucose and amino acid levels. Autophagy. 2011;7:727–736. doi: 10.4161/auto.7.7.15371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Thoen L.F., Guimaraes E.L., Dolle L., Mannaerts I., Najimi M., Sokal E., van Grunsven L.A. A role for autophagy during hepatic stellate cell activation. J. Hepatol. 2011;55:1353–1360. doi: 10.1016/j.jhep.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 305.Watanabe K., Ishidoh K., Ueno T., Sato N., Kominami E. Suppression of lysosomal proteolysis at three different steps in regenerating rat liver. J. Biochem. 1998;124:947–956. doi: 10.1093/oxfordjournals.jbchem.a022212. [DOI] [PubMed] [Google Scholar]
- 306.Lu Z., Dono K., Gotoh K., Shibata M., Koike M., Marubashi S., Miyamoto A., Takeda Y., Nagano H., Umeshita K., et al. Participation of autophagy in the degeneration process of rat hepatocytes after transplantation following prolonged cold preservation. Arch. Histol. Cytol. 2005;68:71–80. doi: 10.1679/aohc.68.71. [DOI] [PubMed] [Google Scholar]
- 307.Wang J.H., Ahn I.S., Fischer T.D., Byeon J.I., Dunn W.A., Jr., Behrns K.E., Leeuwenburgh C., Kim J.S. Autophagy suppresses age-dependent ischemia and reperfusion injury in livers of mice. Gastroenterology. 2011;141:2188–2199. doi: 10.1053/j.gastro.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Harada M. Autophagy is involved in the elimination of intracellular inclusions, Mallory-Denk bodies, in hepatocytes. Med. Mol. Morphol. 2010;43:13–18. doi: 10.1007/s00795-009-0476-5. [DOI] [PubMed] [Google Scholar]
- 309.Harada M., Hanada S., Toivola D.M., Ghori N., Omary M.B. Autophagy activation by rapamycin eliminates mouse Mallory-Denk bodies and blocks their proteasome inhibitor-mediated formation. Hepatology. 2008;47:2026–2035. doi: 10.1002/hep.22294. [DOI] [PubMed] [Google Scholar]
- 310.Skop V., Cahova M., Papackova Z., Palenickova E., Dankova H., Baranowski M., Zabielski P., Zdychova J., Zidkova J., Kazdova L. Autophagy-lysosomal pathway is involved in lipid degradation in rat liver. Physiol. Res. 2012;61:287–297. doi: 10.33549/physiolres.932285. [DOI] [PubMed] [Google Scholar]
- 311.Ohsaki Y., Cheng J., Fujita A., Tokumoto T., Fujimoto T. Cytoplasmic lipid droplets are sites of convergence of proteasomal and autophagic degradation of apolipoprotein B. Mol. Biol. Cell. 2006;17:2674–2683. doi: 10.1091/mbc.e05-07-0659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Bergamini E., De Tata V., Cubeddu T.L., Masiello P., Pollera M. Increased degradation in Rat liver induced by antilipolytic agents: A model for studying autophagy and protein degradation in liver? Exp. Mol. Pathol. 1987;46:114–122. doi: 10.1016/0014-4800(87)90035-9. [DOI] [PubMed] [Google Scholar]
- 313.Iwata J., Ezaki J., Komatsu M., Yokota S., Ueno T., Tanida I., Chiba T., Tanaka K., Kominami E. Excess peroxisomes are degraded by autophagic machinery in mammals. J. Biol. Chem. 2006;281:4035–4041. doi: 10.1074/jbc.M512283200. [DOI] [PubMed] [Google Scholar]
- 314.Kondo K., Makita T. Inhibition of peroxisomal degradation by 3-methyladenine (3MA) in primary cultures of rat hepatocytes. Anat. Rec. 1997;247:449–454. doi: 10.1002/(SICI)1097-0185(199704)247:4<449::AID-AR2>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 315.Locci Cubeddu T., Masiello P., Pollera M., Bergamini E. Effects of antilipolytic agents on Rat liver peroxisomes and peroxisomal oxidative activities. Biochim. Biophys. Acta. 1985;839:96–104. doi: 10.1016/0304-4165(85)90186-2. [DOI] [PubMed] [Google Scholar]
- 316.Luiken J.J., van den Berg M., Heikoop J.C., Meijer A.J. Autophagic degradation of peroxisomes in isolated rat hepatocytes. FEBS Lett. 1992;304:93–97. doi: 10.1016/0014-5793(92)80596-9. [DOI] [PubMed] [Google Scholar]
- 317.Nardacci R., Sartori C., Stefanini S. Selective autophagy of clofibrate-induced Rat liver peroxisomes. Cytochemistry and immunocytochemistry on tissue specimens and on fractions obtained by Nycodenz density gradient centrifugation. Cell. Mol. Biol. (Noisy-le-Grand) 2000;46:1277–1290. [PubMed] [Google Scholar]
- 318.Walter K.M., Schonenberger M.J., Trotzmuller M., Horn M., Elsasser H.P., Moser A.B., Lucas M.S., Schwarz T., Gerber P.A., Faust P.L., et al. Hif-2alpha promotes degradation of mammalian peroxisomes by selective autophagy. Cell Metab. 2014;20:882–897. doi: 10.1016/j.cmet.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 319.Donati A., Taddei M., Cavallini G., Bergamini E. Stimulation of macroautophagy can rescue older cells from 8-OHdG mtDNA accumulation: A safe and easy way to meet goals in the SENS agenda. Rejuvenation Res. 2006;9:408–412. doi: 10.1089/rej.2006.9.408. [DOI] [PubMed] [Google Scholar]
- 320.Bilanges B., Alliouachene S., Pearce W., Morelli D., Szabadkai G., Chung Y.L., Chicanne G., Valet C., Hill J.M., Voshol P.J., et al. Vps34 PI 3-kinase inactivation enhances insulin sensitivity through reprogramming of mitochondrial metabolism. Nat. Commun. 2017;8:1804. doi: 10.1038/s41467-017-01969-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Cavallini G., Donati A., Taddei M., Bergamini E. Evidence for selective mitochondrial autophagy and failure in aging. Autophagy. 2007;3:26–27. doi: 10.4161/auto.3268. [DOI] [PubMed] [Google Scholar]
- 322.Kim I., Lemasters J.J. Mitochondrial degradation by autophagy (mitophagy) in GFP-LC3 transgenic hepatocytes during nutrient deprivation. Am. J. Physiol. Cell Physiol. 2011;300:C308–C317. doi: 10.1152/ajpcell.00056.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Rodriguez-Enriquez S., Kai Y., Maldonado E., Currin R.T., Lemasters J.J. Roles of mitophagy and the mitochondrial permeability transition in remodeling of cultured rat hepatocytes. Autophagy. 2009;5:1099–1106. doi: 10.4161/auto.5.8.9825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Yang L., Li P., Fu S., Calay E.S., Hotamisligil G.S. Defective hepatic autophagy in obesity promotes ER stress and causes insulin resistance. Cell Metab. 2010;11:467–478. doi: 10.1016/j.cmet.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Woodfin B.M., Davis L.E. Liver autophagy in the influenza B virus model of Reye’s syndrome in mice. J. Cell Biochem. 1986;31:271–275. doi: 10.1002/jcb.240310404. [DOI] [PubMed] [Google Scholar]
- 326.Strnad P., Zatloukal K., Stumptner C., Kulaksiz H., Denk H. Mallory-Denk-bodies: Lessons from keratin-containing hepatic inclusion bodies. Biochim. Biophys. Acta. 2008;1782:764–774. doi: 10.1016/j.bbadis.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 327.Dong H., Czaja M.J. Regulation of lipid droplets by autophagy. Trends Endocrinol. Metab. 2011;22:234–240. doi: 10.1016/j.tem.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Martinez-Lopez N., Singh R. Autophagy and Lipid Droplets in the Liver. Annu. Rev. Nutr. 2015;35:215–237. doi: 10.1146/annurev-nutr-071813-105336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Reinke P., David H., Uerlings I., Decker T. Pathology of hepatic peroxisomes in chronic hepatitis B and immunosuppression. Exp. Pathol. 1988;34:71–77. doi: 10.1016/S0232-1513(88)80030-6. [DOI] [PubMed] [Google Scholar]
- 330.Yokota S., Dariush Fahimi H. Degradation of excess peroxisomes in mammalian liver cells by autophagy and other mechanisms. Histochem. Cell Biol. 2009;131:455–458. doi: 10.1007/s00418-009-0564-6. [DOI] [PubMed] [Google Scholar]
- 331.Kwanten W.J., Vandewynckel Y.P., Martinet W., De Winter B.Y., Michielsen P.P., Van Hoof V.O., Driessen A., Timmermans J.P., Bedossa P., Van Vlierberghe H., et al. Hepatocellular autophagy modulates the unfolded protein response and fasting-induced steatosis in mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2016;311:G599–G609. doi: 10.1152/ajpgi.00418.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Stromhaug P.E., Berg T.O., Fengsrud M., Seglen P.O. Purification and characterization of autophagosomes from rat hepatocytes. Pt 2Biochem. J. 1998;335:217–224. doi: 10.1042/bj3350217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Seglen P.O., Brinchmann M.F. Purification of autophagosomes from rat hepatocytes. Autophagy. 2010;6:542–547. doi: 10.4161/auto.6.4.11272. [DOI] [PubMed] [Google Scholar]
- 334.Mallory F.B. Chronic Passive Congestion of the Liver. J. Med. Res. 1911;24:453, 455–462. [PMC free article] [PubMed] [Google Scholar]
- 335.Denk H., Gschnait F., Wolff K. Hepatocellar hyalin (Mallory bodies) in long term griseofulvin-treated mice: A new experimental model for the study of hyalin formation. Lab. Investig. 1975;32:773–776. [PubMed] [Google Scholar]
- 336.Denk H., Eckerstorfer R. Colchicine-induced Mallory body formation in the mouse. Lab. Investig. 1977;36:563–565. [PubMed] [Google Scholar]
- 337.Zatloukal K., French S.W., Stumptner C., Strnad P., Harada M., Toivola D.M., Cadrin M., Omary M.B. From Mallory to Mallory-Denk bodies: What, how and why? Exp. Cell Res. 2007;313:2033–2049. doi: 10.1016/j.yexcr.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 338.Rakoski M.O., Brown M.B., Fontana R.J., Bonkovsky H.L., Brunt E.M., Goodman Z.D., Lok A.S., Omary M.B., Group H.-C.T. Mallory-Denk bodies are associated with outcomes and histologic features in patients with chronic hepatitis C. Clin. Gastroenterol. Hepatol. 2011;9:902–909. doi: 10.1016/j.cgh.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Basaranoglu M., Turhan N., Sonsuz A., Basaranoglu G. Mallory-Denk Bodies in chronic hepatitis. World J. Gastroenterol. 2011;17:2172–2177. doi: 10.3748/wjg.v17.i17.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Gluchowski N.L., Becuwe M., Walther T.C., Farese R.V., Jr. Lipid droplets and liver disease: From basic biology to clinical implications. Nat. Rev. Gastroenterol. Hepatol. 2017;14:343–355. doi: 10.1038/nrgastro.2017.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Walther T.C., Chung J., Farese R.V., Jr. Lipid Droplet Biogenesis. Annu. Rev. Cell Dev. Biol. 2017;33:491–510. doi: 10.1146/annurev-cellbio-100616-060608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Walther T.C., Farese R.V., Jr. Lipid droplets and cellular lipid metabolism. Annu. Rev. Biochem. 2012;81:687–714. doi: 10.1146/annurev-biochem-061009-102430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Mashek D.G., Khan S.A., Sathyanarayan A., Ploeger J.M., Franklin M.P. Hepatic lipid droplet biology: Getting to the root of fatty liver. Hepatology. 2015;62:964–967. doi: 10.1002/hep.27839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Velikkakath A.K., Nishimura T., Oita E., Ishihara N., Mizushima N. Mammalian Atg2 proteins are essential for autophagosome formation and important for regulation of size and distribution of lipid droplets. Mol. Biol. Cell. 2012;23:896–909. doi: 10.1091/mbc.e11-09-0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Ding W.X., Li M., Chen X., Ni H.M., Lin C.W., Gao W., Lu B., Stolz D.B., Clemens D.L., Yin X.M. Autophagy reduces acute ethanol-induced hepatotoxicity and steatosis in mice. Gastroenterology. 2010;139:1740–1752. doi: 10.1053/j.gastro.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Sinha R.A., You S.H., Zhou J., Siddique M.M., Bay B.H., Zhu X., Privalsky M.L., Cheng S.Y., Stevens R.D., Summers S.A., et al. Thyroid hormone stimulates hepatic lipid catabolism via activation of autophagy. J. Clin. Investig. 2012;122:2428–2438. doi: 10.1172/JCI60580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Tseng Y.H., Ke P.Y., Liao C.J., Wu S.M., Chi H.C., Tsai C.Y., Chen C.Y., Lin Y.H., Lin K.H. Chromosome 19 open reading frame 80 is upregulated by thyroid hormone and modulates autophagy and lipid metabolism. Autophagy. 2014;10:20–31. doi: 10.4161/auto.26126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Inokuchi-Shimizu S., Park E.J., Roh Y.S., Yang L., Zhang B., Song J., Liang S., Pimienta M., Taniguchi K., Wu X., et al. TAK1-mediated autophagy and fatty acid oxidation prevent hepatosteatosis and tumorigenesis. J. Clin. Investig. 2014;124:3566–3578. doi: 10.1172/JCI74068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Jiao M., Ren F., Zhou L., Zhang X., Zhang L., Wen T., Wei L., Wang X., Shi H., Bai L., et al. Peroxisome proliferator-activated receptor alpha activation attenuates the inflammatory response to protect the liver from acute failure by promoting the autophagy pathway. Cell Death Dis. 2014;5:e1397. doi: 10.1038/cddis.2014.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Vargas J.L., Roche E., Knecht E., Grisolia S. Differences in the half-lives of some mitochondrial Rat liver enzymes may derive partially from hepatocyte heterogeneity. FEBS Lett. 1987;224:182–186. doi: 10.1016/0014-5793(87)80444-1. [DOI] [PubMed] [Google Scholar]
- 351.Jorda A., Perez-Pastor E., Portoles M. Effect of streptozotocin-diabetes on Rat liver mitochondrial adenosine triphosphatase turnover. Biochem. J. 1988;251:621–624. doi: 10.1042/bj2510621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Knecht E., Martinez-Ramon A., Grisolia S. Autophagy of mitochondria in Rat liver assessed by immunogold procedures. J. Histochem. Cytochem. 1988;36:1433–1440. doi: 10.1177/36.11.3171166. [DOI] [PubMed] [Google Scholar]
- 353.Teckman J.H., An J.K., Blomenkamp K., Schmidt B., Perlmutter D. Mitochondrial autophagy and injury in the liver in alpha 1-antitrypsin deficiency. Am. J. Physiol. Gastrointest. Liver Physiol. 2004;286:G851–G862. doi: 10.1152/ajpgi.00175.2003. [DOI] [PubMed] [Google Scholar]
- 354.Teckman J.H., An J.K., Loethen S., Perlmutter D.H. Fasting in alpha1-antitrypsin deficient liver: Constitutive [correction of consultative] activation of autophagy. Am. J. Physiol. Gastrointest. Liver Physiol. 2002;283:G1156–G1165. doi: 10.1152/ajpgi.00041.2002. [DOI] [PubMed] [Google Scholar]
- 355.Perlmutter D.H. Liver injury in alpha1-antitrypsin deficiency: An aggregated protein induces mitochondrial injury. J. Clin. Investig. 2002;110:1579–1583. doi: 10.1172/JCI0216787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Komatsu M., Waguri S., Ueno T., Iwata J., Murata S., Tanida I., Ezaki J., Mizushima N., Ohsumi Y., Uchiyama Y., et al. Impairment of starvation-induced and constitutive autophagy in Atg7-deficient mice. J. Cell Biol. 2005;169:425–434. doi: 10.1083/jcb.200412022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Kim J.S., Nitta T., Mohuczy D., O’Malley K.A., Moldawer L.L., Dunn W.A., Jr., Behrns K.E. Impaired autophagy: A mechanism of mitochondrial dysfunction in anoxic rat hepatocytes. Hepatology. 2008;47:1725–1736. doi: 10.1002/hep.22187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Desai M.M., Gong B., Chan T., Davey R.A., Soong L., Kolokoltsov A.A., Sun J. Differential, type I interferon-mediated autophagic trafficking of hepatitis C virus proteins in mouse liver. Gastroenterology. 2011;141:674–685. doi: 10.1053/j.gastro.2011.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Ni H.M., Bockus A., Boggess N., Jaeschke H., Ding W.X. Activation of autophagy protects against acetaminophen-induced hepatotoxicity. Hepatology. 2012;55:222–232. doi: 10.1002/hep.24690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Apostolova N., Gomez-Sucerquia L.J., Gortat A., Blas-Garcia A., Esplugues J.V. Autophagy as a rescue mechanism in efavirenz-induced mitochondrial dysfunction: A lesson from hepatic cells. Autophagy. 2011;7:1402–1404. doi: 10.4161/auto.7.11.17653. [DOI] [PubMed] [Google Scholar]
- 361.Li W., Li Y., Siraj S., Jin H., Fan Y., Yang X., Huang X., Wang X., Wang J., Liu L., et al. FUNDC1-mediated mitophagy suppresses hepatocarcinogenesis by inhibition of inflammasome activation. Hepatology. 2018 doi: 10.1002/hep.30191. [DOI] [PubMed] [Google Scholar]
- 362.Yamada T., Murata D., Adachi Y., Itoh K., Kameoka S., Igarashi A., Kato T., Araki Y., Huganir R.L., Dawson T.M., et al. Mitochondrial Stasis Reveals p62-Mediated Ubiquitination in Parkin-Independent Mitophagy and Mitigates Nonalcoholic Fatty Liver Disease. Cell Metab. 2018;28:588–604. doi: 10.1016/j.cmet.2018.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Pang L., Liu K., Liu D., Lv F., Zang Y., Xie F., Yin J., Shi Y., Wang Y., Chen D. Differential effects of reticulophagy and mitophagy on nonalcoholic fatty liver disease. Cell Death Dis. 2018;9:90. doi: 10.1038/s41419-017-0136-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Salas M., Tuchweber B., Kourounakis P. Liver ultrastructure during acute stress. Pathol. Res. Pract. 1980;167:217–233. doi: 10.1016/S0344-0338(80)80052-5. [DOI] [PubMed] [Google Scholar]
- 365.Sato T., Tanaka J., Kono Y., Jones R.T., Cowley R.A., Trump B.F. Hepatic cellular injury following lethal Escherichia coli bacteremia in rats. Lab. Investig. 1982;47:304–310. [PubMed] [Google Scholar]
- 366.Yu Q.C., Marzella L. Response of autophagic protein degradation to physiologic and pathologic stimuli in rat hepatocyte monolayer cultures. Lab. Investig. 1988;58:643–652. [PubMed] [Google Scholar]
- 367.Greene C.M., Marciniak S.J., Teckman J., Ferrarotti I., Brantly M.L., Lomas D.A., Stoller J.K., McElvaney N.G. alpha1-Antitrypsin deficiency. Nat. Rev. Dis. Primers. 2016;2:16051. doi: 10.1038/nrdp.2016.51. [DOI] [PubMed] [Google Scholar]
- 368.Lomas D.A., Hurst J.R., Gooptu B. Update on alpha-1 antitrypsin deficiency: New therapies. J. Hepatol. 2016;65:413–424. doi: 10.1016/j.jhep.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 369.Rudnick D.A., Perlmutter D.H. Alpha-1-antitrypsin deficiency: A new paradigm for hepatocellular carcinoma in genetic liver disease. Hepatology. 2005;42:514–521. doi: 10.1002/hep.20815. [DOI] [PubMed] [Google Scholar]
- 370.Teckman J.H., Perlmutter D.H. Retention of mutant alpha(1)-antitrypsin Z in endoplasmic reticulum is associated with an autophagic response. Am. J. Physiol. Gastrointest. Liver Physiol. 2000;279:G961–G974. doi: 10.1152/ajpgi.2000.279.5.G961. [DOI] [PubMed] [Google Scholar]
- 371.Kamimoto T., Shoji S., Hidvegi T., Mizushima N., Umebayashi K., Perlmutter D.H., Yoshimori T. Intracellular inclusions containing mutant alpha1-antitrypsin Z are propagated in the absence of autophagic activity. J. Biol. Chem. 2006;281:4467–4476. doi: 10.1074/jbc.M509409200. [DOI] [PubMed] [Google Scholar]
- 372.Kruse K.B., Brodsky J.L., McCracken A.A. Characterization of an ERAD gene as VPS30/ATG6 reveals two alternative and functionally distinct protein quality control pathways: One for soluble Z variant of human alpha-1 proteinase inhibitor (A1PiZ) and another for aggregates of A1PiZ. Mol. Biol. Cell. 2006;17:203–212. doi: 10.1091/mbc.e04-09-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Kaushal S., Annamali M., Blomenkamp K., Rudnick D., Halloran D., Brunt E.M., Teckman J.H. Rapamycin reduces intrahepatic alpha-1-antitrypsin mutant Z protein polymers and liver injury in a mouse model. Exp. Biol. Med. (Maywood) 2010;235:700–709. doi: 10.1258/ebm.2010.009297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Perlmutter D.H. The role of autophagy in alpha-1-antitrypsin deficiency: A specific cellular response in genetic diseases associated with aggregation-prone proteins. Autophagy. 2006;2:258–263. doi: 10.4161/auto.2882. [DOI] [PubMed] [Google Scholar]
- 375.Perlmutter D.H. Autophagic disposal of the aggregation-prone protein that causes liver inflammation and carcinogenesis in alpha-1-antitrypsin deficiency. Cell Death Differ. 2009;16:39–45. doi: 10.1038/cdd.2008.103. [DOI] [PubMed] [Google Scholar]
- 376.Lindblad D., Blomenkamp K., Teckman J. Alpha-1-antitrypsin mutant Z protein content in individual hepatocytes correlates with cell death in a mouse model. Hepatology. 2007;46:1228–1235. doi: 10.1002/hep.21822. [DOI] [PubMed] [Google Scholar]
- 377.Komatsu M., Waguri S., Koike M., Sou Y.S., Ueno T., Hara T., Mizushima N., Iwata J., Ezaki J., Murata S., et al. Homeostatic levels of p62 control cytoplasmic inclusion body formation in autophagy-deficient mice. Cell. 2007;131:1149–1163. doi: 10.1016/j.cell.2007.10.035. [DOI] [PubMed] [Google Scholar]
- 378.Komatsu M., Kurokawa H., Waguri S., Taguchi K., Kobayashi A., Ichimura Y., Sou Y.S., Ueno I., Sakamoto A., Tong K.I., et al. The selective autophagy substrate p62 activates the stress responsive transcription factor Nrf2 through inactivation of Keap1. Nat. Cell Biol. 2010;12:213–223. doi: 10.1038/ncb2021. [DOI] [PubMed] [Google Scholar]
- 379.Inami Y., Waguri S., Sakamoto A., Kouno T., Nakada K., Hino O., Watanabe S., Ando J., Iwadate M., Yamamoto M., et al. Persistent activation of Nrf2 through p62 in hepatocellular carcinoma cells. J. Cell Biol. 2011;193:275–284. doi: 10.1083/jcb.201102031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Matsumoto N., Ezaki J., Komatsu M., Takahashi K., Mineki R., Taka H., Kikkawa M., Fujimura T., Takeda-Ezaki M., Ueno T., et al. Comprehensive proteomics analysis of autophagy-deficient mouse liver. Biochem. Biophys. Res. Commun. 2008;368:643–649. doi: 10.1016/j.bbrc.2008.01.112. [DOI] [PubMed] [Google Scholar]
- 381.Sun K., Xie X., Liu Y., Han Z., Zhao X., Cai N., Zhang S., Song J., Wei L. Autophagy lessens ischemic liver injury by reducing oxidative damage. Cell Biosci. 2013;3:26. doi: 10.1186/2045-3701-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Esposti D.D., Domart M.C., Sebagh M., Harper F., Pierron G., Brenner C., Lemoine A. Autophagy is induced by ischemic preconditioning in human livers formerly treated by chemotherapy to limit necrosis. Autophagy. 2010;6:172–174. doi: 10.4161/auto.6.1.10699. [DOI] [PubMed] [Google Scholar]
- 383.Domart M.C., Esposti D.D., Sebagh M., Olaya N., Harper F., Pierron G., Franc B., Tanabe K.K., Debuire B., Azoulay D., et al. Concurrent induction of necrosis, apoptosis, and autophagy in ischemic preconditioned human livers formerly treated by chemotherapy. J. Hepatol. 2009;51:881–889. doi: 10.1016/j.jhep.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 384.Ding W.X., Li M., Yin X.M. Selective taste of ethanol-induced autophagy for mitochondria and lipid droplets. Autophagy. 2011;7:248–249. doi: 10.4161/auto.7.2.14347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Carchman E.H., Rao J., Loughran P.A., Rosengart M.R., Zuckerbraun B.S. Heme oxygenase-1-mediated autophagy protects against hepatocyte cell death and hepatic injury from infection/sepsis in mice. Hepatology. 2011;53:2053–2062. doi: 10.1002/hep.24324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Mei S., Ni H.M., Manley S., Bockus A., Kassel K.M., Luyendyk J.P., Copple B.L., Ding W.X. Differential roles of unsaturated and saturated fatty acids on autophagy and apoptosis in hepatocytes. J. Pharmacol. Exp. Ther. 2011;339:487–498. doi: 10.1124/jpet.111.184341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Gao X., Yao L., Song Q., Zhu L., Xia Z., Xia H., Jiang X., Chen J., Chen H. The association of autophagy with polyethylenimine-induced cytotoxicity in nephritic and hepatic cell lines. Biomaterials. 2011;32:8613–8625. doi: 10.1016/j.biomaterials.2011.07.047. [DOI] [PubMed] [Google Scholar]
- 388.Igusa Y., Yamashina S., Izumi K., Inami Y., Fukada H., Komatsu M., Tanaka K., Ikejima K., Watanabe S. Loss of autophagy promotes murine acetaminophen hepatotoxicity. J. Gastroenterol. 2012;47:433–443. doi: 10.1007/s00535-011-0500-0. [DOI] [PubMed] [Google Scholar]
- 389.Gotoh K., Lu Z., Morita M., Shibata M., Koike M., Waguri S., Dono K., Doki Y., Kominami E., Sugioka A., et al. Participation of autophagy in the initiation of graft dysfunction after Rat liver transplantation. Autophagy. 2009;5:351–360. doi: 10.4161/auto.5.3.7650. [DOI] [PubMed] [Google Scholar]
- 390.Xu X., Hueckstaedt L.K., Ren J. Deficiency of insulin-like growth factor 1 attenuates aging-induced changes in hepatic function: Role of autophagy. J. Hepatol. 2013;59:308–317. doi: 10.1016/j.jhep.2013.03.037. [DOI] [PubMed] [Google Scholar]
- 391.Pastore N., Blomenkamp K., Annunziata F., Piccolo P., Mithbaokar P., Maria Sepe R., Vetrini F., Palmer D., Ng P., Polishchuk E., et al. Gene transfer of master autophagy regulator TFEB results in clearance of toxic protein and correction of hepatic disease in alpha-1-anti-trypsin deficiency. EMBO Mol. Med. 2013;5:397–412. doi: 10.1002/emmm.201202046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Sun Q., Gao W., Loughran P., Shapiro R., Fan J., Billiar T.R., Scott M.J. Caspase 1 activation is protective against hepatocyte cell death by up-regulating beclin 1 protein and mitochondrial autophagy in the setting of redox stress. J. Biol. Chem. 2013;288:15947–15958. doi: 10.1074/jbc.M112.426791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Du R.H., Tan J., Yan N., Wang L., Qiao C., Ding J.H., Lu M., Hu G. Kir6.2 knockout aggravates lipopolysaccharide-induced mouse liver injury via enhancing NLRP3 inflammasome activation. J. Gastroenterol. 2014;49:727–736. doi: 10.1007/s00535-013-0823-0. [DOI] [PubMed] [Google Scholar]
- 394.Saberi B., Ybanez M.D., Johnson H.S., Gaarde W.A., Han D., Kaplowitz N. Protein kinase C (PKC) participates in acetaminophen hepatotoxicity through c-jun-N-terminal kinase (JNK)-dependent and -independent signaling pathways. Hepatology. 2014;59:1543–1554. doi: 10.1002/hep.26625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Hernandez-Gea V., Hilscher M., Rozenfeld R., Lim M.P., Nieto N., Werner S., Devi L.A., Friedman S.L. Endoplasmic reticulum stress induces fibrogenic activity in hepatic stellate cells through autophagy. J. Hepatol. 2013;59:98–104. doi: 10.1016/j.jhep.2013.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Liu D., Liu X., Zhou T., Yao W., Zhao J., Zheng Z., Jiang W., Wang F., Aikhionbare F.O., Hill D.L., et al. IRE1-RACK1 axis orchestrates ER stress preconditioning-elicited cytoprotection from ischemia/reperfusion injury in liver. J. Mol. Cell Biol. 2016;8:144–156. doi: 10.1093/jmcb/mjv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Shi T., Song W., Xu R. Autophagy and ER stress in LPS/GalNinduced acute liver injury. Mol. Med. Rep. 2017;16:7001–7005. doi: 10.3892/mmr.2017.7409. [DOI] [PubMed] [Google Scholar]
- 398.Rickenbacher A., Jang J.H., Limani P., Ungethum U., Lehmann K., Oberkofler C.E., Weber A., Graf R., Humar B., Clavien P.A. Fasting protects liver from ischemic injury through Sirt1-mediated downregulation of circulating HMGB1 in mice. J. Hepatol. 2014;61:301–308. doi: 10.1016/j.jhep.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 399.Khambu B., Huda N., Chen X., Antoine D.J., Li Y., Dai G., Kohler U.A., Zong W.X., Waguri S., Werner S., et al. HMGB1 promotes ductular reaction and tumorigenesis in autophagy-deficient livers. J. Clin. Investig. 2018;128:2419–2435. doi: 10.1172/JCI91814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Lu J., He L., Behrends C., Araki M., Araki K., Jun Wang Q., Catanzaro J.M., Friedman S.L., Zong W.X., Fiel M.I., et al. NRBF2 regulates autophagy and prevents liver injury by modulating Atg14L-linked phosphatidylinositol-3 kinase III activity. Nat. Commun. 2014;5:3920. doi: 10.1038/ncomms4920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Escobar D.A., Botero-Quintero A.M., Kautza B.C., Luciano J., Loughran P., Darwiche S., Rosengart M.R., Zuckerbraun B.S., Gomez H. Adenosine monophosphate-activated protein kinase activation protects against sepsis-induced organ injury and inflammation. J. Surg. Res. 2015;194:262–272. doi: 10.1016/j.jss.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Xing W., Yang L., Peng Y., Wang Q., Gao M., Yang M., Xiao X. Ginsenoside Rg3 attenuates sepsis-induced injury and mitochondrial dysfunction in liver via AMPK-mediated autophagy flux. Biosci. Rep. 2017;37 doi: 10.1042/BSR20170934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Li J., Chen B., Zhong L., Gao F., Zhu H., Wang F. AMP-activated protein kinase agonist N6-(3-hydroxyphenyl)adenosine protects against fulminant hepatitis by suppressing inflammation and apoptosis. Cell Death Dis. 2018;9:37. doi: 10.1038/s41419-017-0118-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Ni H.M., Bhakta A., Wang S., Li Z., Manley S., Huang H., Copple B., Ding W.X. Role of hypoxia inducing factor-1beta in alcohol-induced autophagy, steatosis and liver injury in mice. PLoS ONE. 2014;9:e115849. doi: 10.1371/journal.pone.0115849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Zhong C., Pu L.Y., Fang M.M., Gu Z., Rao J.H., Wang X.H. Retinoic acid receptor alpha promotes autophagy to alleviate liver ischemia and reperfusion injury. World J. Gastroenterol. 2015;21:12381–12391. doi: 10.3748/wjg.v21.i43.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Liu A., Guo E., Yang J., Li R., Yang Y., Liu S., Hu J., Jiang X., Dirsch O., Dahmen U., et al. Ischemic preconditioning attenuates ischemia/reperfusion injury in rat steatotic liver: Role of heme oxygenase-1-mediated autophagy. Oncotarget. 2016;7:78372–78386. doi: 10.18632/oncotarget.13281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Xu D., Chen L., Chen X., Wen Y., Yu C., Yao J., Wu H., Wang X., Xia Q., Kong X. The triterpenoid CDDO-imidazolide ameliorates mouse liver ischemia-reperfusion injury through activating the Nrf2/HO-1 pathway enhanced autophagy. Cell Death Dis. 2017;8:e2983. doi: 10.1038/cddis.2017.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Guo E., Li R., Yang J., Zhang J., Li A., Yang Y., Liu S., Liu A., Jiang X. FK866 attenuates acute hepatic failure through c-jun-N-terminal kinase (JNK)-dependent autophagy. Sci. Rep. 2017;7:2206. doi: 10.1038/s41598-017-02318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Rah S.Y., Lee Y.H., Kim U.H. NAADP-mediated Ca(2+) signaling promotes autophagy and protects against LPS-induced liver injury. FASEB J. 2017;31:3126–3137. doi: 10.1096/fj.201601290R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Sydor S., Manka P., Best J., Jafoui S., Sowa J.P., Zoubek M.E., Hernandez-Gea V., Cubero F.J., Kalsch J., Vetter D., et al. Kruppel-like factor 6 is a transcriptional activator of autophagy in acute liver injury. Sci. Rep. 2017;7:8119. doi: 10.1038/s41598-017-08680-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Czaja M.J., Ding W.X., Donohue T.M., Jr., Friedman S.L., Kim J.S., Komatsu M., Lemasters J.J., Lemoine A., Lin J.D., Ou J.H., et al. Functions of autophagy in normal and diseased liver. Autophagy. 2013;9:1131–1158. doi: 10.4161/auto.25063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Minor T., Stegemann J., Hirner A., Koetting M. Impaired autophagic clearance after cold preservation of fatty livers correlates with tissue necrosis upon reperfusion and is reversed by hypothermic reconditioning. Liver Transpl. 2009;15:798–805. doi: 10.1002/lt.21751. [DOI] [PubMed] [Google Scholar]
- 413.Wu D., Wang X., Zhou R., Cederbaum A. CYP2E1 enhances ethanol-induced lipid accumulation but impairs autophagy in HepG2 E47 cells. Biochem. Biophys. Res. Commun. 2010;402:116–122. doi: 10.1016/j.bbrc.2010.09.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Stankov M.V., Panayotova-Dimitrova D., Leverkus M., Vondran F.W., Bauerfeind R., Binz A., Behrens G.M. Autophagy inhibition due to thymidine analogues as novel mechanism leading to hepatocyte dysfunction and lipid accumulation. AIDS. 2012;26:1995–2006. doi: 10.1097/QAD.0b013e32835804f9. [DOI] [PubMed] [Google Scholar]
- 415.Sharma S., Mells J.E., Fu P.P., Saxena N.K., Anania F.A. GLP-1 analogs reduce hepatocyte steatosis and improve survival by enhancing the unfolded protein response and promoting macroautophagy. PLoS ONE. 2011;6:e25269. doi: 10.1371/journal.pone.0025269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Jaber N., Dou Z., Chen J.S., Catanzaro J., Jiang Y.P., Ballou L.M., Selinger E., Ouyang X., Lin R.Z., Zhang J., et al. Class III PI3K Vps34 plays an essential role in autophagy and in heart and liver function. Proc. Natl. Acad. Sci. USA. 2012;109:2003–2008. doi: 10.1073/pnas.1112848109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.He Z., Liu H., Agostini M., Yousefi S., Perren A., Tschan M.P., Mak T.W., Melino G., Simon H.U. p73 regulates autophagy and hepatocellular lipid metabolism through a transcriptional activation of the ATG5 gene. Cell Death Differ. 2013;20:1415–1424. doi: 10.1038/cdd.2013.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Wang L., Liu X., Nie J., Zhang J., Kimball S.R., Zhang H., Zhang W.J., Jefferson L.S., Cheng Z., Ji Q., et al. ALCAT1 controls mitochondrial etiology of fatty liver diseases, linking defective mitophagy to steatosis. Hepatology. 2015;61:486–496. doi: 10.1002/hep.27420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Xiong J., Wang K., He J., Zhang G., Zhang D., Chen F. TFE3 Alleviates Hepatic Steatosis through Autophagy-Induced Lipophagy and PGC1alpha-Mediated Fatty Acid beta-Oxidation. Int. J. Mol. Sci. 2016;17:387. doi: 10.3390/ijms17030387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Kim K.Y., Jang H.J., Yang Y.R., Park K.I., Seo J., Shin I.W., Jeon T.I., Ahn S.C., Suh P.G., Osborne T.F., et al. SREBP-2/PNPLA8 axis improves non-alcoholic fatty liver disease through activation of autophagy. Sci. Rep. 2016;6:35732. doi: 10.1038/srep35732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Conlon D.M., Thomas T., Fedotova T., Hernandez-Ono A., Di Paolo G., Chan R.B., Ruggles K., Gibeley S., Liu J., Ginsberg H.N. Inhibition of apolipoprotein B synthesis stimulates endoplasmic reticulum autophagy that prevents steatosis. J. Clin. Investig. 2016;126:3852–3867. doi: 10.1172/JCI86028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Tanaka S., Hikita H., Tatsumi T., Sakamori R., Nozaki Y., Sakane S., Shiode Y., Nakabori T., Saito Y., Hiramatsu N., et al. Rubicon inhibits autophagy and accelerates hepatocyte apoptosis and lipid accumulation in nonalcoholic fatty liver disease in mice. Hepatology. 2016;64:1994–2014. doi: 10.1002/hep.28820. [DOI] [PubMed] [Google Scholar]
- 423.Li S., Dou X., Ning H., Song Q., Wei W., Zhang X., Shen C., Li J., Sun C., Song Z. Sirtuin 3 acts as a negative regulator of autophagy dictating hepatocyte susceptibility to lipotoxicity. Hepatology. 2017;66:936–952. doi: 10.1002/hep.29229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Chao X., Wang S., Zhao K., Li Y., Williams J.A., Li T., Chavan H., Krishnamurthy P., He X.C., Li L., et al. Impaired TFEB-Mediated Lysosome Biogenesis and Autophagy Promote Chronic Ethanol-Induced Liver Injury and Steatosis in Mice. Gastroenterology. 2018;155:865–879. doi: 10.1053/j.gastro.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Lin C.W., Zhang H., Li M., Xiong X., Chen X., Chen X., Dong X.C., Yin X.M. Pharmacological promotion of autophagy alleviates steatosis and injury in alcoholic and non-alcoholic fatty liver conditions in mice. J. Hepatol. 2013;58:993–999. doi: 10.1016/j.jhep.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Schulze R.J., Drizyte K., Casey C.A., McNiven M.A. Hepatic Lipophagy: New Insights into Autophagic Catabolism of Lipid Droplets in the Liver. Hepatol. Commun. 2017;1:359–369. doi: 10.1002/hep4.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Farah B.L., Landau D.J., Sinha R.A., Brooks E.D., Wu Y., Fung S.Y.S., Tanaka T., Hirayama M., Bay B.H., Koeberl D.D., et al. Induction of autophagy improves hepatic lipid metabolism in glucose-6-phosphatase deficiency. J. Hepatol. 2016;64:370–379. doi: 10.1016/j.jhep.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 428.DeBosch B.J., Heitmeier M.R., Mayer A.L., Higgins C.B., Crowley J.R., Kraft T.E., Chi M., Newberry E.P., Chen Z., Finck B.N., et al. Trehalose inhibits solute carrier 2A (SLC2A) proteins to induce autophagy and prevent hepatic steatosis. Sci. Signal. 2016;9:ra21. doi: 10.1126/scisignal.aac5472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Kong X., Yang Y., Ren L., Shao T., Li F., Zhao C., Liu L., Zhang H., McClain C.J., Feng W. Activation of autophagy attenuates EtOH-LPS-induced hepatic steatosis and injury through MD2 associated TLR4 signaling. Sci. Rep. 2017;7:9292. doi: 10.1038/s41598-017-09045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Vescovo T., Romagnoli A., Perdomo A.B., Corazzari M., Ciccosanti F., Alonzi T., Nardacci R., Ippolito G., Tripodi M., Garcia-Monzon C., et al. Autophagy protects cells from HCV-induced defects in lipid metabolism. Gastroenterology. 2012;142:644–653. doi: 10.1053/j.gastro.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 431.Williams J.A., Ni H.M., Ding Y., Ding W.X. Parkin regulates mitophagy and mitochondrial function to protect against alcohol-induced liver injury and steatosis in mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2015;309:G324–G340. doi: 10.1152/ajpgi.00108.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Ma D., Molusky M.M., Song J., Hu C.R., Fang F., Rui C., Mathew A.V., Pennathur S., Liu F., Cheng J.X., et al. Autophagy deficiency by hepatic FIP200 deletion uncouples steatosis from liver injury in NAFLD. Mol. Endocrinol. 2013;27:1643–1654. doi: 10.1210/me.2013-1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Fukada H., Yamashina S., Izumi K., Komatsu M., Tanaka K., Ikejima K., Watanabe S. Suppression of autophagy sensitizes Kupffer cells to endotoxin. Hepatol. Res. 2012;42:1112–1118. doi: 10.1111/j.1872-034X.2012.01024.x. [DOI] [PubMed] [Google Scholar]
- 434.Guo R., Xu X., Babcock S.A., Zhang Y., Ren J. Aldehyde dedydrogenase-2 plays a beneficial role in ameliorating chronic alcohol-induced hepatic steatosis and inflammation through regulation of autophagy. J. Hepatol. 2015;62:647–656. doi: 10.1016/j.jhep.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 435.Inami Y., Yamashina S., Izumi K., Ueno T., Tanida I., Ikejima K., Watanabe S. Hepatic steatosis inhibits autophagic proteolysis via impairment of autophagosomal acidification and cathepsin expression. Biochem. Biophys. Res. Commun. 2011;412:618–625. doi: 10.1016/j.bbrc.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 436.Gonzalez-Rodriguez A., Mayoral R., Agra N., Valdecantos M.P., Pardo V., Miquilena-Colina M.E., Vargas-Castrillon J., Lo Iacono O., Corazzari M., Fimia G.M., et al. Impaired autophagic flux is associated with increased endoplasmic reticulum stress during the development of NAFLD. Cell Death Dis. 2014;5:e1179. doi: 10.1038/cddis.2014.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Fukuo Y., Yamashina S., Sonoue H., Arakawa A., Nakadera E., Aoyama T., Uchiyama A., Kon K., Ikejima K., Watanabe S. Abnormality of autophagic function and cathepsin expression in the liver from patients with non-alcoholic fatty liver disease. Hepatol. Res. 2014;44:1026–1036. doi: 10.1111/hepr.12282. [DOI] [PubMed] [Google Scholar]
- 438.Hruban Z. Ultrastructure of hepatocellular tumors. J. Toxicol. Environ. Health. 1979;5:403–433. doi: 10.1080/15287397909529757. [DOI] [PubMed] [Google Scholar]
- 439.Seglen P.O., Schwarze P.E., Saeter G. Changes in cellular ploidy and autophagic responsiveness during Rat liver carcinogenesis. Toxicol. Pathol. 1986;14:342–348. doi: 10.1177/019262338601400309. [DOI] [PubMed] [Google Scholar]
- 440.Tessitore L., Bonelli G., Cecchini G., Autelli R., Amenta J.S., Baccino F.M. Regulation of protein turnover versus growth state. Studies on the mechanism(s) of initiation of acidic vacuolar proteolysis in cells of stationary ascites hepatoma. Biochem. J. 1988;251:483–490. doi: 10.1042/bj2510483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Pfeifer U., Tessitore L., Bonelli G., Baccino F.M. Regulation of protein turnover versus growth state. III. Growth cessation is associated with activation of autophagy in Yoshida ascites hepatoma AH-340. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 1988;55:363–369. [PubMed] [Google Scholar]
- 442.Ahlberg J., Yucel T., Eriksson L., Glaumann H. Characterization of the proteolytic compartment in rat hepatocyte nodules. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 1987;53:79–88. doi: 10.1007/BF02890228. [DOI] [PubMed] [Google Scholar]
- 443.Kisen G.O., Tessitore L., Costelli P., Gordon P.B., Schwarze P.E., Baccino F.M., Seglen P.O. Reduced autophagic activity in primary rat hepatocellular carcinoma and ascites hepatoma cells. Carcinogenesis. 1993;14:2501–2505. doi: 10.1093/carcin/14.12.2501. [DOI] [PubMed] [Google Scholar]
- 444.Ding Z.B., Shi Y.H., Zhou J., Qiu S.J., Xu Y., Dai Z., Shi G.M., Wang X.Y., Ke A.W., Wu B., et al. Association of autophagy defect with a malignant phenotype and poor prognosis of hepatocellular carcinoma. Cancer Res. 2008;68:9167–9175. doi: 10.1158/0008-5472.CAN-08-1573. [DOI] [PubMed] [Google Scholar]
- 445.Shi Y.H., Ding Z.B., Zhou J., Qiu S.J., Fan J. Prognostic significance of Beclin 1-dependent apoptotic activity in hepatocellular carcinoma. Autophagy. 2009;5:380–382. doi: 10.4161/auto.5.3.7658. [DOI] [PubMed] [Google Scholar]
- 446.Menrad H., Werno C., Schmid T., Copanaki E., Deller T., Dehne N., Brune B. Roles of hypoxia-inducible factor-1alpha (HIF-1alpha) versus HIF-2alpha in the survival of hepatocellular tumor spheroids. Hepatology. 2010;51:2183–2192. doi: 10.1002/hep.23597. [DOI] [PubMed] [Google Scholar]
- 447.Gou X., Ru Q., Zhang H., Chen Y., Li L., Yang H., Xing J., Chen Z. HAb18G/CD147 inhibits starvation-induced autophagy in human hepatoma cell SMMC7721 with an involvement of Beclin 1 down-regulation. Cancer Sci. 2009;100:837–843. doi: 10.1111/j.1349-7006.2009.01113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Sun K., Guo X.L., Zhao Q.D., Jing Y.Y., Kou X.R., Xie X.Q., Zhou Y., Cai N., Gao L., Zhao X., et al. Paradoxical role of autophagy in the dysplastic and tumor-forming stages of hepatocarcinoma development in rats. Cell Death Dis. 2013;4:e501. doi: 10.1038/cddis.2013.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Tian Y., Kuo C.F., Sir D., Wang L., Govindarajan S., Petrovic L.M., Ou J.H. Autophagy inhibits oxidative stress and tumor suppressors to exert its dual effect on hepatocarcinogenesis. Cell Death Differ. 2015;22:1025–1034. doi: 10.1038/cdd.2014.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Liu Z., Wei X., Zhang A., Li C., Bai J., Dong J. Long non-coding RNA HNF1A-AS1 functioned as an oncogene and autophagy promoter in hepatocellular carcinoma through sponging hsa-miR-30b-5p. Biochem. Biophys. Res. Commun. 2016;473:1268–1275. doi: 10.1016/j.bbrc.2016.04.054. [DOI] [PubMed] [Google Scholar]
- 451.Li J., Yang B., Zhou Q., Wu Y., Shang D., Guo Y., Song Z., Zheng Q., Xiong J. Autophagy promotes hepatocellular carcinoma cell invasion through activation of epithelial-mesenchymal transition. Carcinogenesis. 2013;34:1343–1351. doi: 10.1093/carcin/bgt063. [DOI] [PubMed] [Google Scholar]
- 452.Grassi G., Di Caprio G., Santangelo L., Fimia G.M., Cozzolino A.M., Komatsu M., Ippolito G., Tripodi M., Alonzi T. Autophagy regulates hepatocyte identity and epithelial-to-mesenchymal and mesenchymal-to-epithelial transitions promoting Snail degradation. Cell Death Dis. 2015;6:e1880. doi: 10.1038/cddis.2015.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Toshima T., Shirabe K., Matsumoto Y., Yoshiya S., Ikegami T., Yoshizumi T., Soejima Y., Ikeda T., Maehara Y. Autophagy enhances hepatocellular carcinoma progression by activation of mitochondrial beta-oxidation. J. Gastroenterol. 2014;49:907–916. doi: 10.1007/s00535-013-0835-9. [DOI] [PubMed] [Google Scholar]
- 454.Pan H., Wang Z., Jiang L., Sui X., You L., Shou J., Jing Z., Xie J., Ge W., Cai X., et al. Autophagy inhibition sensitizes hepatocellular carcinoma to the multikinase inhibitor linifanib. Sci. Rep. 2014;4:6683. doi: 10.1038/srep06683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Chang C.P., Yang M.C., Liu H.S., Lin Y.S., Lei H.Y. Concanavalin A induces autophagy in hepatoma cells and has a therapeutic effect in a murine in situ hepatoma model. Hepatology. 2007;45:286–296. doi: 10.1002/hep.21509. [DOI] [PubMed] [Google Scholar]
- 456.Lei H.Y., Chang C.P. Induction of autophagy by concanavalin A and its application in anti-tumor therapy. Autophagy. 2007;3:402–404. doi: 10.4161/auto.4280. [DOI] [PubMed] [Google Scholar]
- 457.Chang C.P., Yang M.C., Lei H.Y. Concanavalin A/IFN-gamma triggers autophagy-related necrotic hepatocyte death through IRGM1-mediated lysosomal membrane disruption. PLoS ONE. 2011;6:e28323. doi: 10.1371/journal.pone.0028323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Qian H., Yang Y. Alterations of cellular organelles in human liver-derived hepatoma G2 cells induced by adriamycin. Anticancer Drugs. 2009;20:779–786. doi: 10.1097/CAD.0b013e32832f4e6f. [DOI] [PubMed] [Google Scholar]
- 459.Yang F., Gao Y.H., Wu K.W., Deng R., Li D.D., Wei Z.X., Jiang S., Wu X.Q., Feng G.K., Li H.J., et al. A novel sesquiterpene Hirsutanol A induces autophagical cell death in human hepatocellular carcinoma cells by increasing reactive oxygen species. Chin. J. Cancer. 2010;29:655–660. doi: 10.5732/cjc.009.10702. [DOI] [PubMed] [Google Scholar]
- 460.Xie S.Q., Li Q., Zhang Y.H., Wang J.H., Mei Z.H., Zhao J., Wang C.J. NPC-16, a novel naphthalimide-polyamine conjugate, induced apoptosis and autophagy in human hepatoma HepG2 cells and Bel-7402 cells. Apoptosis. 2011;16:27–34. doi: 10.1007/s10495-010-0537-1. [DOI] [PubMed] [Google Scholar]
- 461.Zhang J.Q., Li Y.M., Liu T., He W.T., Chen Y.T., Chen X.H., Li X., Zhou W.C., Yi J.F., Ren Z.J. Antitumor effect of matrine in human hepatoma G2 cells by inducing apoptosis and autophagy. World J. Gastroenterol. 2010;16:4281–4290. doi: 10.3748/wjg.v16.i34.4281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.Wang N., Feng Y., Zhu M., Tsang C.M., Man K., Tong Y., Tsao S.W. Berberine induces autophagic cell death and mitochondrial apoptosis in liver cancer cells: The cellular mechanism. J. Cell Biochem. 2010;111:1426–1436. doi: 10.1002/jcb.22869. [DOI] [PubMed] [Google Scholar]
- 463.Wang N., Pan W., Zhu M., Zhang M., Hao X., Liang G., Feng Y. Fangchinoline induces autophagic cell death via p53/sestrin2/AMPK signalling in human hepatocellular carcinoma cells. Br. J. Pharmacol. 2011;164:731–742. doi: 10.1111/j.1476-5381.2011.01349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Hou Q., Tang X., Liu H., Tang J., Yang Y., Jing X., Xiao Q., Wang W., Gou X., Wang Z. Berberine induces cell death in human hepatoma cells in vitro by downregulating CD147. Cancer Sci. 2011;102:1287–1292. doi: 10.1111/j.1349-7006.2011.01933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Qian H., Yang Y., Wang X. Curcumin enhanced adriamycin-induced human liver-derived Hepatoma G2 cell death through activation of mitochondria-mediated apoptosis and autophagy. Eur. J. Pharm. Sci. 2011;43:125–131. doi: 10.1016/j.ejps.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 466.Andrzejak M., Price M., Kessel D.H. Apoptotic and autophagic responses to photodynamic therapy in 1c1c7 murine hepatoma cells. Autophagy. 2011;7:979–984. doi: 10.4161/auto.7.9.15865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Hu M., Huang H., Zhao R., Li P., Li M., Miao H., Chen N., Chen M. AZD8055 induces cell death associated with autophagy and activation of AMPK in hepatocellular carcinoma. Oncol. Rep. 2014;31:649–656. doi: 10.3892/or.2013.2890. [DOI] [PubMed] [Google Scholar]
- 468.Kiyono K., Suzuki H.I., Matsuyama H., Morishita Y., Komuro A., Kano M.R., Sugimoto K., Miyazono K. Autophagy is activated by TGF-β and potentiates TGF-β-mediated growth inhibition in human hepatocellular carcinoma cells. Cancer Res. 2009;69:8844–8852. doi: 10.1158/0008-5472.CAN-08-4401. [DOI] [PubMed] [Google Scholar]
- 469.Xie R., Wang F., McKeehan W.L., Liu L. Autophagy enhanced by microtubule- and mitochondrion-associated MAP1S suppresses genome instability and hepatocarcinogenesis. Cancer Res. 2011;71:7537–7546. doi: 10.1158/0008-5472.CAN-11-2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Jung K.H., Noh J.H., Kim J.K., Eun J.W., Bae H.J., Chang Y.G., Kim M.G., Park W.S., Lee J.Y., Lee S.Y., et al. Histone deacetylase 6 functions as a tumor suppressor by activating c-Jun NH2-terminal kinase-mediated beclin 1-dependent autophagic cell death in liver cancer. Hepatology. 2012;56:644–657. doi: 10.1002/hep.25699. [DOI] [PubMed] [Google Scholar]
- 471.Xie H.J., Noh J.H., Kim J.K., Jung K.H., Eun J.W., Bae H.J., Kim M.G., Chang Y.G., Lee J.Y., Park H., et al. HDAC1 inactivation induces mitotic defect and caspase-independent autophagic cell death in liver cancer. PLoS ONE. 2012;7:e34265. doi: 10.1371/journal.pone.0034265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Zou M., Lu N., Hu C., Liu W., Sun Y., Wang X., You Q., Gu C., Xi T., Guo Q. Beclin 1-mediated autophagy in hepatocellular carcinoma cells: Implication in anticancer efficiency of oroxylin A via inhibition of mTOR signaling. Cell Signal. 2012;24:1722–1732. doi: 10.1016/j.cellsig.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 473.Luo Z., Yu G., Lee H.W., Li L., Wang L., Yang D., Pan Y., Ding C., Qian J., Wu L., et al. The Nedd8-activating enzyme inhibitor MLN4924 induces autophagy and apoptosis to suppress liver cancer cell growth. Cancer Res. 2012;72:3360–3371. doi: 10.1158/0008-5472.CAN-12-0388. [DOI] [PubMed] [Google Scholar]
- 474.Yang D., Li L., Liu H., Wu L., Luo Z., Li H., Zheng S., Gao H., Chu Y., Sun Y., et al. Induction of autophagy and senescence by knockdown of ROC1 E3 ubiquitin ligase to suppress the growth of liver cancer cells. Cell Death Differ. 2013;20:235–247. doi: 10.1038/cdd.2012.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Wang Y., Han C., Lu L., Magliato S., Wu T. Hedgehog signaling pathway regulates autophagy in human hepatocellular carcinoma cells. Hepatology. 2013;58:995–1010. doi: 10.1002/hep.26394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Gao M., Yeh P.Y., Lu Y.S., Hsu C.H., Chen K.F., Lee W.C., Feng W.C., Chen C.S., Kuo M.L., Cheng A.L. OSU-03012, a novel celecoxib derivative, induces reactive oxygen species-related autophagy in hepatocellular carcinoma. Cancer Res. 2008;68:9348–9357. doi: 10.1158/0008-5472.CAN-08-1642. [DOI] [PubMed] [Google Scholar]
- 477.Wu G., Zhang R., Ren J., Sun Y. Autophagic cell death of human hepatoma cells induced by endostar, a recombinant human endostatin. Cancer Biother. Radiopharm. 2008;23:735–740. doi: 10.1089/cbr.2008.0518. [DOI] [PubMed] [Google Scholar]
- 478.Liu Y.L., Yang P.M., Shun C.T., Wu M.S., Weng J.R., Chen C.C. Autophagy potentiates the anti-cancer effects of the histone deacetylase inhibitors in hepatocellular carcinoma. Autophagy. 2010;6:1057–1065. doi: 10.4161/auto.6.8.13365. [DOI] [PubMed] [Google Scholar]
- 479.Gong K., Chen C., Zhan Y., Chen Y., Huang Z., Li W. Autophagy-related gene 7 (ATG7) and reactive oxygen species/extracellular signal-regulated kinase regulate tetrandrine-induced autophagy in human hepatocellular carcinoma. J. Biol. Chem. 2012;287:35576–35588. doi: 10.1074/jbc.M112.370585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Chen Y.J., Chi C.W., Su W.C., Huang H.L. Lapatinib induces autophagic cell death and inhibits growth of human hepatocellular carcinoma. Oncotarget. 2014;5:4845–4854. doi: 10.18632/oncotarget.2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 481.Yang Z., Zhao T., Liu H., Zhang L. Ginsenoside Rh2 inhibits hepatocellular carcinoma through beta-catenin and autophagy. Sci. Rep. 2016;6:19383. doi: 10.1038/srep19383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 482.Hsieh M.J., Chen M.K., Chen C.J., Hsieh M.C., Lo Y.S., Chuang Y.C., Chiou H.L., Yang S.F. Glabridin induces apoptosis and autophagy through JNK1/2 pathway in human hepatoma cells. Phytomedicine. 2016;23:359–366. doi: 10.1016/j.phymed.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 483.Jegal K.H., Ko H.L., Park S.M., Byun S.H., Kang K.W., Cho I.J., Kim S.C. Eupatilin induces Sestrin2-dependent autophagy to prevent oxidative stress. Apoptosis. 2016;21:642–656. doi: 10.1007/s10495-016-1233-6. [DOI] [PubMed] [Google Scholar]
- 484.Di Fazio P., Waldegger P., Jabari S., Lingelbach S., Montalbano R., Ocker M., Slater E.P., Bartsch D.K., Illig R., Neureiter D., et al. Autophagy-related cell death by pan-histone deacetylase inhibition in liver cancer. Oncotarget. 2016;7:28998–29010. doi: 10.18632/oncotarget.8585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485.Tzeng C.W., Tzeng W.S., Lin L.T., Lee C.W., Yen F.L., Lin C.C. Enhanced autophagic activity of artocarpin in human hepatocellular carcinoma cells through improving its solubility by a nanoparticle system. Phytomedicine. 2016;23:528–540. doi: 10.1016/j.phymed.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 486.Longo L., Platini F., Scardino A., Alabiso O., Vasapollo G., Tessitore L. Autophagy inhibition enhances anthocyanin-induced apoptosis in hepatocellular carcinoma. Mol. Cancer Ther. 2008;7:2476–2485. doi: 10.1158/1535-7163.MCT-08-0361. [DOI] [PubMed] [Google Scholar]
- 487.Ko H., Kim Y.J., Park J.S., Park J.H., Yang H.O. Autophagy inhibition enhances apoptosis induced by ginsenoside Rk1 in hepatocellular carcinoma cells. Biosci. Biotechnol. Biochem. 2009;73:2183–2189. doi: 10.1271/bbb.90250. [DOI] [PubMed] [Google Scholar]
- 488.Shi M., Wang H.N., Xie S.T., Luo Y., Sun C.Y., Chen X.L., Zhang Y.Z. Antimicrobial peptaibols, novel suppressors of tumor cells, targeted calcium-mediated apoptosis and autophagy in human hepatocellular carcinoma cells. Mol. Cancer. 2010;9:26. doi: 10.1186/1476-4598-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Altmeyer A., Jung A.C., Ignat M., Benzina S., Denis J.M., Gueulette J., Noel G., Mutter D., Bischoff P. Pharmacological enhancement of autophagy induced in a hepatocellular carcinoma cell line by high-LET radiation. Anticancer Res. 2010;30:303–310. [PubMed] [Google Scholar]
- 490.Ganapathy-Kanniappan S., Geschwind J.F., Kunjithapatham R., Buijs M., Syed L.H., Rao P.P., Ota S., Kwak B.K., Loffroy R., Vali M. 3-Bromopyruvate induces endoplasmic reticulum stress, overcomes autophagy and causes apoptosis in human HCC cell lines. Anticancer Res. 2010;30:923–935. [PubMed] [Google Scholar]
- 491.Xie B.S., Zhao H.C., Yao S.K., Zhuo D.X., Jin B., Lv D.C., Wu C.L., Ma D.L., Gao C., Shu X.M., et al. Autophagy inhibition enhances etoposide-induced cell death in human hepatoma G2 cells. Int. J. Mol. Med. 2011;27:599–606. doi: 10.3892/ijmm.2011.607. [DOI] [PubMed] [Google Scholar]
- 492.Jung H.J., Seo I., Casciello F., Jacquelin S., Lane S.W., Suh S.I., Suh M.H., Lee J.S., Baek W.K. The anticancer effect of chaetocin is enhanced by inhibition of autophagy. Cell Death Dis. 2016;7:e2098. doi: 10.1038/cddis.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Liu W., Yu G., Yu W., Ye X., Jin Y., Shrestha A., Yang Q., Sun H. Autophagy Inhibits Apoptosis Induced by agrocybe aegerita Lectin in Hepatocellular Carcinoma. Anticancer Agents Med. Chem. 2017;17:221–229. doi: 10.2174/1871520616666160404112645. [DOI] [PubMed] [Google Scholar]
- 494.Chen X., Tan M., Xie Z., Feng B., Zhao Z., Yang K., Hu C., Liao N., Wang T., Chen D., et al. Inhibiting ROS-STAT3-dependent autophagy enhanced capsaicin-induced apoptosis in human hepatocellular carcinoma cells. Free Radic. Res. 2016;50:744–755. doi: 10.3109/10715762.2016.1173689. [DOI] [PubMed] [Google Scholar]
- 495.Chang Y., Chen L., Liu Y., Hu L., Li L., Tu Q., Wang R., Wu M., Yang J., Wang H. Inhibition of autophagy may suppress the development of hepatoblastoma. FEBS J. 2011;278:4811–4823. doi: 10.1111/j.1742-4658.2011.08381.x. [DOI] [PubMed] [Google Scholar]
- 496.Yan Y., Jiang K., Liu P., Zhang X., Dong X., Gao J., Liu Q., Barr M.P., Zhang Q., Hou X., et al. Bafilomycin A1 induces caspase-independent cell death in hepatocellular carcinoma cells via targeting of autophagy and MAPK pathways. Sci. Rep. 2016;6:37052. doi: 10.1038/srep37052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497.Chang Y., Yan W., He X., Zhang L., Li C., Huang H., Nace G., Geller D.A., Lin J., Tsung A. miR-375 inhibits autophagy and reduces viability of hepatocellular carcinoma cells under hypoxic conditions. Gastroenterology. 2012;143:177–187. doi: 10.1053/j.gastro.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 498.Hui B., Shi Y.H., Ding Z.B., Zhou J., Gu C.Y., Peng Y.F., Yang H., Liu W.R., Shi G.M., Fan J. Proteasome inhibitor interacts synergistically with autophagy inhibitor to suppress proliferation and induce apoptosis in hepatocellular carcinoma. Cancer. 2012;118:5560–5571. doi: 10.1002/cncr.27586. [DOI] [PubMed] [Google Scholar]
- 499.Song J., Qu Z., Guo X., Zhao Q., Zhao X., Gao L., Sun K., Shen F., Wu M., Wei L. Hypoxia-induced autophagy contributes to the chemoresistance of hepatocellular carcinoma cells. Autophagy. 2009;5:1131–1144. doi: 10.4161/auto.5.8.9996. [DOI] [PubMed] [Google Scholar]
- 500.Chen L.H., Loong C.C., Su T.L., Lee Y.J., Chu P.M., Tsai M.L., Tsai P.H., Tu P.H., Chi C.W., Lee H.C., et al. Autophagy inhibition enhances apoptosis triggered by BO-1051, an N-mustard derivative, and involves the ATM signaling pathway. Biochem. Pharmacol. 2011;81:594–605. doi: 10.1016/j.bcp.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 501.Ding Z.B., Hui B., Shi Y.H., Zhou J., Peng Y.F., Gu C.Y., Yang H., Shi G.M., Ke A.W., Wang X.Y., et al. Autophagy activation in hepatocellular carcinoma contributes to the tolerance of oxaliplatin via reactive oxygen species modulation. Clin. Cancer Res. 2011;17:6229–6238. doi: 10.1158/1078-0432.CCR-11-0816. [DOI] [PubMed] [Google Scholar]
- 502.Shimizu S., Takehara T., Hikita H., Kodama T., Tsunematsu H., Miyagi T., Hosui A., Ishida H., Tatsumi T., Kanto T., et al. Inhibition of autophagy potentiates the antitumor effect of the multikinase inhibitor sorafenib in hepatocellular carcinoma. Int. J. Cancer. 2012;131:548–557. doi: 10.1002/ijc.26374. [DOI] [PubMed] [Google Scholar]
- 503.Du H., Yang W., Chen L., Shi M., Seewoo V., Wang J., Lin A., Liu Z., Qiu W. Role of autophagy in resistance to oxaliplatin in hepatocellular carcinoma cells. Oncol. Rep. 2012;27:143–150. doi: 10.3892/or.2011.1464. [DOI] [PubMed] [Google Scholar]
- 504.Xu N., Zhang J., Shen C., Luo Y., Xia L., Xue F., Xia Q. Cisplatin-induced downregulation of miR-199a-5p increases drug resistance by activating autophagy in HCC cell. Biochem. Biophys. Res. Commun. 2012;423:826–831. doi: 10.1016/j.bbrc.2012.06.048. [DOI] [PubMed] [Google Scholar]
- 505.Yu H.C., Lin C.S., Tai W.T., Liu C.Y., Shiau C.W., Chen K.F. Nilotinib induces autophagy in hepatocellular carcinoma through AMPK activation. J. Biol. Chem. 2013;288:18249–18259. doi: 10.1074/jbc.M112.446385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.Xiong H., Ni Z., He J., Jiang S., Li X., He J., Gong W., Zheng L., Chen S., Li B., et al. LncRNA HULC triggers autophagy via stabilizing Sirt1 and attenuates the chemosensitivity of HCC cells. Oncogene. 2017;36:3528–3540. doi: 10.1038/onc.2016.521. [DOI] [PubMed] [Google Scholar]
- 507.Wu B., Cui J., Yang X.M., Liu Z.Y., Song F., Li L., Jiang J.L., Chen Z.N. Cytoplasmic fragment of CD147 generated by regulated intramembrane proteolysis contributes to HCC by promoting autophagy. Cell Death Dis. 2017;8:e2925. doi: 10.1038/cddis.2017.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 508.Shi Y.H., Ding Z.B., Zhou J., Hui B., Shi G.M., Ke A.W., Wang X.Y., Dai Z., Peng Y.F., Gu C.Y., et al. Targeting autophagy enhances sorafenib lethality for hepatocellular carcinoma via ER stress-related apoptosis. Autophagy. 2011;7:1159–1172. doi: 10.4161/auto.7.10.16818. [DOI] [PubMed] [Google Scholar]
- 509.Bareford M.D., Park M.A., Yacoub A., Hamed H.A., Tang Y., Cruickshanks N., Eulitt P., Hubbard N., Tye G., Burow M.E., et al. Sorafenib enhances pemetrexed cytotoxicity through an autophagy-dependent mechanism in cancer cells. Cancer Res. 2011;71:4955–4967. doi: 10.1158/0008-5472.CAN-11-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 510.Zhou Y., Sun K., Ma Y., Yang H., Zhang Y., Kong X., Wei L. Autophagy inhibits chemotherapy-induced apoptosis through downregulating Bad and Bim in hepatocellular carcinoma cells. Sci. Rep. 2014;4:5382. doi: 10.1038/srep05382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Takamura A., Komatsu M., Hara T., Sakamoto A., Kishi C., Waguri S., Eishi Y., Hino O., Tanaka K., Mizushima N. Autophagy-deficient mice develop multiple liver tumors. Genes Dev. 2011;25:795–800. doi: 10.1101/gad.2016211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512.Saito T., Ichimura Y., Taguchi K., Suzuki T., Mizushima T., Takagi K., Hirose Y., Nagahashi M., Iso T., Fukutomi T., et al. p62/Sqstm1 promotes malignancy of HCV-positive hepatocellular carcinoma through Nrf2-dependent metabolic reprogramming. Nat. Commun. 2016;7:12030. doi: 10.1038/ncomms12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 513.Umemura A., He F., Taniguchi K., Nakagawa H., Yamachika S., Font-Burgada J., Zhong Z., Subramaniam S., Raghunandan S., Duran A., et al. p62, Upregulated during Preneoplasia, Induces Hepatocellular Carcinogenesis by Maintaining Survival of Stressed HCC-Initiating Cells. Cancer Cell. 2016;29:935–948. doi: 10.1016/j.ccell.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 514.Taniguchi K., Yamachika S., He F., Karin M. p62/SQSTM1-Dr. Jekyll and Mr. Hyde that prevents oxidative stress but promotes liver cancer. FEBS Lett. 2016;590:2375–2397. doi: 10.1002/1873-3468.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 515.Lee Y.A., Noon L.A., Akat K.M., Ybanez M.D., Lee T.F., Berres M.L., Fujiwara N., Goossens N., Chou H.I., Parvin-Nejad F.P., et al. Autophagy is a gatekeeper of hepatic differentiation and carcinogenesis by controlling the degradation of Yap. Nat. Commun. 2018;9:4962. doi: 10.1038/s41467-018-07338-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 516.Huang Q., Zhan L., Cao H., Li J., Lyu Y., Guo X., Zhang J., Ji L., Ren T., An J., et al. Increased mitochondrial fission promotes autophagy and hepatocellular carcinoma cell survival through the ROS-modulated coordinated regulation of the NFKB and TP53 pathways. Autophagy. 2016;12:999–1014. doi: 10.1080/15548627.2016.1166318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 517.Wu F.Q., Fang T., Yu L.X., Lv G.S., Lv H.W., Liang D., Li T., Wang C.Z., Tan Y.X., Ding J., et al. ADRB2 signaling promotes HCC progression and sorafenib resistance by inhibiting autophagic degradation of HIF1alpha. J. Hepatol. 2016;65:314–324. doi: 10.1016/j.jhep.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 518.Huang D., Li T., Wang L., Zhang L., Yan R., Li K., Xing S., Wu G., Hu L., Jia W., et al. Hepatocellular carcinoma redirects to ketolysis for progression under nutrition deprivation stress. Cell Res. 2016;26:1112–1130. doi: 10.1038/cr.2016.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Jia Y.L., Xu M., Dou C.W., Liu Z.K., Xue Y.M., Yao B.W., Ding L.L., Tu K.S., Zheng X., Liu Q.G. P300/CBP-associated factor (PCAF) inhibits the growth of hepatocellular carcinoma by promoting cell autophagy. Cell Death Dis. 2016;7:e2400. doi: 10.1038/cddis.2016.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 520.Liu K., Lee J., Kim J.Y., Wang L., Tian Y., Chan S.T., Cho C., Machida K., Chen D., Ou J.J. Mitophagy Controls the Activities of Tumor Suppressor p53 to Regulate Hepatic Cancer Stem Cells. Mol. Cell. 2017;68:281–292.e285. doi: 10.1016/j.molcel.2017.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 521.Enomoto M., Tsuchida A., Miyazawa K., Yokoyama T., Kawakita H., Tokita H., Naito M., Itoh M., Ohyashiki K., Aoki T. Vitamin K2-induced cell growth inhibition via autophagy formation in cholangiocellular carcinoma cell lines. Int. J. Mol. Med. 2007;20:801–808. doi: 10.3892/ijmm.20.6.801. [DOI] [PubMed] [Google Scholar]
- 522.Wang B., Li H., Yang R., Zhou S., Zou S. Decitabine inhibits the cell growth of cholangiocarcinoma in cultured cell lines and mouse xenografts. Oncol. Lett. 2014;8:1919–1924. doi: 10.3892/ol.2014.2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Hou Y.J., Dong L.W., Tan Y.X., Yang G.Z., Pan Y.F., Li Z., Tang L., Wang M., Wang Q., Wang H.Y. Inhibition of active autophagy induces apoptosis and increases chemosensitivity in cholangiocarcinoma. Lab. Investig. 2011;91:1146–1157. doi: 10.1038/labinvest.2011.97. [DOI] [PubMed] [Google Scholar]
- 524.Dong L.W., Hou Y.J., Tan Y.X., Tang L., Pan Y.F., Wang M., Wang H.Y. Prognostic significance of Beclin 1 in intrahepatic cholangiocellular carcinoma. Autophagy. 2011;7:1222–1229. doi: 10.4161/auto.7.10.16610. [DOI] [PubMed] [Google Scholar]
- 525.Wang T.T., Cao Q.H., Chen M.Y., Xia Q., Fan X.J., Ma X.K., Lin Q., Jia C.C., Dong M., Ruan D.Y., et al. Beclin 1 deficiency correlated with lymph node metastasis, predicts a distinct outcome in intrahepatic and extrahepatic cholangiocarcinoma. PLoS ONE. 2013;8:e80317. doi: 10.1371/journal.pone.0080317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526.O’Dell M.R., Huang J.L., Whitney-Miller C.L., Deshpande V., Rothberg P., Grose V., Rossi R.M., Zhu A.X., Land H., Bardeesy N., et al. Kras(G12D) and p53 mutation cause primary intrahepatic cholangiocarcinoma. Cancer Res. 2012;72:1557–1567. doi: 10.1158/0008-5472.CAN-11-3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 527.Huang J.L., Hezel A.F. Autophagy in intra-hepatic cholangiocarcinoma. Autophagy. 2012;8:1148–1149. doi: 10.4161/auto.20647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 528.Qu X., Sheng J., Shen L., Su J., Xu Y., Xie Q., Wu Y., Zhang X., Sun L. Autophagy inhibitor chloroquine increases sensitivity to cisplatin in QBC939 cholangiocarcinoma cells by mitochondrial ROS. PLoS ONE. 2017;12:e0173712. doi: 10.1371/journal.pone.0173712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 529.Jia B., Xue Y., Yan X., Li J., Wu Y., Guo R., Zhang J., Zhang L., Li Y., Liu Y., et al. Autophagy inhibitor chloroquine induces apoptosis of cholangiocarcinoma cells via endoplasmic reticulum stress. Oncol. Lett. 2018;16:3509–3516. doi: 10.3892/ol.2018.9131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 530.Thongchot S., Yongvanit P., Loilome W., Seubwai W., Phunicom K., Tassaneeyakul W., Pairojkul C., Promkotra W., Techasen A., Namwat N. High expression of HIF-1alpha, BNIP3 and PI3KC3: Hypoxia-induced autophagy predicts cholangiocarcinoma survival and metastasis. Asian Pac. J. Cancer Prev. 2014;15:5873–5878. doi: 10.7314/APJCP.2014.15.14.5873. [DOI] [PubMed] [Google Scholar]
- 531.Sasaki M., Nitta T., Sato Y., Nakanuma Y. Autophagy may occur at an early stage of cholangiocarcinogenesis via biliary intraepithelial neoplasia. Hum. Pathol. 2015;46:202–209. doi: 10.1016/j.humpath.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 532.Hong Z.F., Zhao W.X., Yin Z.Y., Xie C.R., Xu Y.P., Chi X.Q., Zhang S., Wang X.M. Capsaicin Enhances the Drug Sensitivity of Cholangiocarcinoma through the Inhibition of Chemotherapeutic-Induced Autophagy. PLoS ONE. 2015;10:e0121538. doi: 10.1371/journal.pone.0121538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 533.Ding X., Chaiteerakij R., Moser C.D., Shaleh H., Boakye J., Chen G., Ndzengue A., Li Y., Zhou Y., Huang S., et al. Antitumor effect of the novel sphingosine kinase 2 inhibitor ABC294640 is enhanced by inhibition of autophagy and by sorafenib in human cholangiocarcinoma cells. Oncotarget. 2016;7:20080–20092. doi: 10.18632/oncotarget.7914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 534.Zhang A., He W., Shi H., Huang X., Ji G. Natural compound oblongifolin C inhibits autophagic flux, and induces apoptosis and mitochondrial dysfunction in human cholangiocarcinoma QBC939 cells. Mol. Med. Rep. 2016;14:3179–3183. doi: 10.3892/mmr.2016.5591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 535.Hu F., Guo X.L., Zhang S.S., Zhao Q.D., Li R., Xu Q., Wei L.X. Suppression of p53 potentiates chemosensitivity in nutrient-deprived cholangiocarcinoma cells via inhibition of autophagy. Oncol. Lett. 2017;14:1959–1966. doi: 10.3892/ol.2017.6449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 536.Zhao X., Luo G., Cheng Y., Yu W., Chen R., Xiao B., Xiang Y., Feng C., Fu W., Duan C., et al. Compound C induces protective autophagy in human cholangiocarcinoma cells via Akt/mTOR-independent pathway. J. Cell Biochem. 2018;119:5538–5550. doi: 10.1002/jcb.26723. [DOI] [PubMed] [Google Scholar]
- 537.Ma J., Weng L., Wang Z., Jia Y., Liu B., Wu S., Cao Y., Sun X., Yin X., Shang M., et al. MiR-124 induces autophagy-related cell death in cholangiocarcinoma cells through direct targeting of the EZH2-STAT3 signaling axis. Exp. Cell Res. 2018;366:103–113. doi: 10.1016/j.yexcr.2018.02.037. [DOI] [PubMed] [Google Scholar]
- 538.Thongchot S., Vidoni C., Ferraresi A., Loilome W., Yongvanit P., Namwat N., Isidoro C. Dihydroartemisinin induces apoptosis and autophagy-dependent cell death in cholangiocarcinoma through a DAPK1-BECLIN1 pathway. Mol. Carcinog. 2018;57:1735–1750. doi: 10.1002/mc.22893. [DOI] [PubMed] [Google Scholar]
- 539.Thomas H.E., Mercer C.A., Carnevalli L.S., Park J., Andersen J.B., Conner E.A., Tanaka K., Matsutani T., Iwanami A., Aronow B.J., et al. mTOR inhibitors synergize on regression, reversal of gene expression, and autophagy in hepatocellular carcinoma. Sci. Transl. Med. 2012;4:139ra184. doi: 10.1126/scitranslmed.3003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 540.Klose J., Guerlevik E., Trostel T., Kuhnel F., Schmidt T., Schneider M., Ulrich A. Salinomycin inhibits cholangiocarcinoma growth by inhibition of autophagic flux. Oncotarget. 2018;9:3619–3630. doi: 10.18632/oncotarget.23339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 541.Ait-Goughoulte M., Kanda T., Meyer K., Ryerse J.S., Ray R.B., Ray R. Hepatitis C virus genotype 1a growth and induction of autophagy. J. Virol. 2008;82:2241–2249. doi: 10.1128/JVI.02093-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 542.Sir D., Chen W.L., Choi J., Wakita T., Yen T.S., Ou J.H. Induction of incomplete autophagic response by hepatitis C virus via the unfolded protein response. Hepatology. 2008;48:1054–1061. doi: 10.1002/hep.22464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 543.Guevin C., Manna D., Belanger C., Konan K.V., Mak P., Labonte P. Autophagy protein ATG5 interacts transiently with the hepatitis C virus RNA polymerase (NS5B) early during infection. Virology. 2010;405:1–7. doi: 10.1016/j.virol.2010.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 544.Sir D., Kuo C.F., Tian Y., Liu H.M., Huang E.J., Jung J.U., Machida K., Ou J.H. Replication of hepatitis C virus RNA on autophagosomal membranes. J. Biol. Chem. 2012;287:18036–18043. doi: 10.1074/jbc.M111.320085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 545.Ferraris P., Blanchard E., Roingeard P. Ultrastructural and biochemical analyses of hepatitis C virus-associated host cell membranes. J. Gen. Virol. 2010;91:2230–2237. doi: 10.1099/vir.0.022186-0. [DOI] [PubMed] [Google Scholar]
- 546.Kim J.Y., Wang L., Lee J., Ou J.J. Hepatitis C Virus Induces the Localization of Lipid Rafts to Autophagosomes for Its RNA Replication. J. Virol. 2017;91 doi: 10.1128/JVI.00541-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 547.Mohl B.P., Tedbury P.R., Griffin S., Harris M. Hepatitis C virus-induced autophagy is independent of the unfolded protein response. J. Virol. 2012;86:10724–10732. doi: 10.1128/JVI.01667-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Dreux M., Gastaminza P., Wieland S.F., Chisari F.V. The autophagy machinery is required to initiate hepatitis C virus replication. Proc. Natl. Acad. Sci. USA. 2009;106:14046–14051. doi: 10.1073/pnas.0907344106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 549.Ke P.Y., Chen S.S. Activation of the unfolded protein response and autophagy after hepatitis C virus infection suppresses innate antiviral immunity in vitro. J. Clin. Investig. 2011;121:37–56. doi: 10.1172/JCI41474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 550.Romero-Brey I., Merz A., Chiramel A., Lee J.Y., Chlanda P., Haselman U., Santarella-Mellwig R., Habermann A., Hoppe S., Kallis S., et al. Three-dimensional architecture and biogenesis of membrane structures associated with hepatitis C virus replication. PLoS Pathog. 2012;8:e1003056. doi: 10.1371/journal.ppat.1003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 551.Paul D., Hoppe S., Saher G., Krijnse-Locker J., Bartenschlager R. Morphological and biochemical characterization of the membranous hepatitis C virus replication compartment. J. Virol. 2013;87:10612–10627. doi: 10.1128/JVI.01370-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 552.Shrivastava S., Raychoudhuri A., Steele R., Ray R., Ray R.B. Knockdown of autophagy enhances the innate immune response in hepatitis C virus-infected hepatocytes. Hepatology. 2011;53:406–414. doi: 10.1002/hep.24073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 553.Chan S.T., Lee J., Narula M., Ou J.J. Suppression of Host Innate Immune Response by Hepatitis C Virus via Induction of Autophagic Degradation of TRAF6. J. Virol. 2016;90:10928–10935. doi: 10.1128/JVI.01365-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 554.Estrabaud E., De Muynck S., Asselah T. Activation of unfolded protein response and autophagy during HCV infection modulates innate immune response. J. Hepatol. 2011;55:1150–1153. doi: 10.1016/j.jhep.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 555.Tanida I., Fukasawa M., Ueno T., Kominami E., Wakita T., Hanada K. Knockdown of autophagy-related gene decreases the production of infectious hepatitis C virus particles. Autophagy. 2009;5:937–945. doi: 10.4161/auto.5.7.9243. [DOI] [PubMed] [Google Scholar]
- 556.Shrivastava S., Devhare P., Sujijantarat N., Steele R., Kwon Y.C., Ray R., Ray R.B. Knockdown of Autophagy Inhibits Infectious Hepatitis C Virus Release by the Exosomal Pathway. J. Virol. 2016;90:1387–1396. doi: 10.1128/JVI.02383-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 557.Kim J.Y., Ou J.J. Regulation of Apolipoprotein E Trafficking by Hepatitis C Virus-induced Autophagy. J. Virol. 2018 doi: 10.1128/JVI.00211-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 558.Taguwa S., Kambara H., Fujita N., Noda T., Yoshimori T., Koike K., Moriishi K., Matsuura Y. Dysfunction of autophagy participates in vacuole formation and cell death in cells replicating hepatitis C virus. J. Virol. 2011;85:13185–13194. doi: 10.1128/JVI.06099-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 559.Wang J., Kang R., Huang H., Xi X., Wang B., Wang J., Zhao Z. Hepatitis C virus core protein activates autophagy through EIF2AK3 and ATF6 UPR pathway-mediated MAP1LC3B and ATG12 expression. Autophagy. 2014;10:766–784. doi: 10.4161/auto.27954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 560.Huang H., Kang R., Wang J., Luo G., Yang W., Zhao Z. Hepatitis C virus inhibits AKT-tuberous sclerosis complex (TSC), the mechanistic target of rapamycin (MTOR) pathway, through endoplasmic reticulum stress to induce autophagy. Autophagy. 2013;9:175–195. doi: 10.4161/auto.22791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 561.Ren H., Elgner F., Jiang B., Himmelsbach K., Medvedev R., Ploen D., Hildt E. The Autophagosomal SNARE Protein Syntaxin 17 Is an Essential Factor for the Hepatitis C Virus Life Cycle. J. Virol. 2016;90:5989–6000. doi: 10.1128/JVI.00551-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 562.Wang L., Kim J.Y., Liu H.M., Lai M.M.C., Ou J.J. HCV-induced autophagosomes are generated via homotypic fusion of phagophores that mediate HCV RNA replication. PLoS Pathog. 2017;13:e1006609. doi: 10.1371/journal.ppat.1006609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 563.Zhang M.Q., Li J.R., Peng Z.G., Zhang J.P. Differential Effects of Autophagy-Related 10 Protein on HCV Replication and Autophagy Flux Are Mediated by Its Cysteine(44) and Cysteine(135) Front. Immunol. 2018;9:2176. doi: 10.3389/fimmu.2018.02176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 564.Zhao Q., Hu Z.Y., Zhang J.P., Jiang J.D., Ma Y.Y., Li J.R., Peng Z.G., Chen J.H. Dual Roles of Two Isoforms of Autophagy-related Gene ATG10 in HCV-Subgenomic replicon Mediated Autophagy Flux and Innate Immunity. Sci. Rep. 2017;7:11250. doi: 10.1038/s41598-017-11105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 565.Kim S.J., Syed G.H., Siddiqui A. Hepatitis C virus induces the mitochondrial translocation of Parkin and subsequent mitophagy. PLoS Pathog. 2013;9:e1003285. doi: 10.1371/journal.ppat.1003285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 566.Chu V.C., Bhattacharya S., Nomoto A., Lin J., Zaidi S.K., Oberley T.D., Weinman S.A., Azhar S., Huang T.T. Persistent expression of hepatitis C virus non-structural proteins leads to increased autophagy and mitochondrial injury in human hepatoma cells. PLoS ONE. 2011;6:e28551. doi: 10.1371/journal.pone.0028551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 567.Kim S.J., Syed G.H., Khan M., Chiu W.W., Sohail M.A., Gish R.G., Siddiqui A. Hepatitis C virus triggers mitochondrial fission and attenuates apoptosis to promote viral persistence. Proc. Natl. Acad. Sci. USA. 2014;111:6413–6418. doi: 10.1073/pnas.1321114111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 568.Hara Y., Yanatori I., Ikeda M., Kiyokage E., Nishina S., Tomiyama Y., Toida K., Kishi F., Kato N., Imamura M., et al. Hepatitis C virus core protein suppresses mitophagy by interacting with parkin in the context of mitochondrial depolarization. Am. J. Pathol. 2014;184:3026–3039. doi: 10.1016/j.ajpath.2014.07.024. [DOI] [PubMed] [Google Scholar]
- 569.Mori H., Fukuhara T., Ono C., Tamura T., Sato A., Fauzyah Y., Wada M., Okamoto T., Noda T., Yoshimori T., et al. Induction of selective autophagy in cells replicating hepatitis C virus genome. J. Gen. Virol. 2018 doi: 10.1099/jgv.0.001161. [DOI] [PubMed] [Google Scholar]
- 570.Kurt R., Chandra P.K., Aboulnasr F., Panigrahi R., Ferraris P., Aydin Y., Reiss K., Wu T., Balart L.A., Dash S. Chaperone-Mediated Autophagy Targets IFNAR1 for Lysosomal Degradation in Free Fatty Acid Treated HCV Cell Culture. PLoS ONE. 2015;10:e0125962. doi: 10.1371/journal.pone.0125962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 571.Matsui C., Deng L., Minami N., Abe T., Koike K., Shoji I. Hepatitis C Virus NS5A Protein Promotes the Lysosomal Degradation of Hepatocyte Nuclear Factor 1alpha via Chaperone-Mediated Autophagy. J. Virol. 2018;92 doi: 10.1128/JVI.00639-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 572.Kim N., Kim M.J., Sung P.S., Bae Y.C., Shin E.C., Yoo J.Y. Interferon-inducible protein SCOTIN interferes with HCV replication through the autolysosomal degradation of NS5A. Nat. Commun. 2016;7:10631. doi: 10.1038/ncomms10631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 573.Qu X., Yu J., Bhagat G., Furuya N., Hibshoosh H., Troxel A., Rosen J., Eskelinen E.L., Mizushima N., Ohsumi Y., et al. Promotion of tumorigenesis by heterozygous disruption of the beclin 1 autophagy gene. J. Clin. Investig. 2003;112:1809–1820. doi: 10.1172/JCI20039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 574.Sir D., Ann D.K., Ou J.H. Autophagy by hepatitis B virus and for hepatitis B virus. Autophagy. 2010;6:548–549. doi: 10.4161/auto.6.4.11669. [DOI] [PubMed] [Google Scholar]
- 575.Sir D., Tian Y., Chen W.L., Ann D.K., Yen T.S., Ou J.H. The early autophagic pathway is activated by hepatitis B virus and required for viral DNA replication. Proc. Natl. Acad. Sci. USA. 2010;107:4383–4388. doi: 10.1073/pnas.0911373107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 576.Tian Y., Sir D., Kuo C.F., Ann D.K., Ou J.H. Autophagy required for hepatitis B virus replication in transgenic mice. J. Virol. 2011;85:13453–13456. doi: 10.1128/JVI.06064-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 577.Tang H., Da L., Mao Y., Li Y., Li D., Xu Z., Li F., Wang Y., Tiollais P., Li T., et al. Hepatitis B virus X protein sensitizes cells to starvation-induced autophagy via up-regulation of beclin 1 expression. Hepatology. 2009;49:60–71. doi: 10.1002/hep.22581. [DOI] [PubMed] [Google Scholar]
- 578.Li J., Liu Y., Wang Z., Liu K., Wang Y., Liu J., Ding H., Yuan Z. Subversion of cellular autophagy machinery by hepatitis B virus for viral envelopment. J. Virol. 2011;85:6319–6333. doi: 10.1128/JVI.02627-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 579.Doring T., Zeyen L., Bartusch C., Prange R. Hepatitis B Virus Subverts the Autophagy Elongation Complex Atg5-12/16L1 and Does Not Require Atg8/LC3 Lipidation for Viral Maturation. J. Virol. 2018;92 doi: 10.1128/JVI.01513-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 580.Wang J., Chen J., Liu Y., Zeng X., Wei M., Wu S., Xiong Q., Song F., Yuan X., Xiao Y., et al. Hepatitis B Virus Induces Autophagy to Promote its Replication by the Axis of miR-192-3p-XIAP via NF-kappaB Signaling. Hepatology. 2018 doi: 10.1002/hep.30248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 581.Zhong L., Hu J., Shu W., Gao B., Xiong S. Epigallocatechin-3-gallate opposes HBV-induced incomplete autophagy by enhancing lysosomal acidification, which is unfavorable for HBV replication. Cell Death Dis. 2015;6:e1770. doi: 10.1038/cddis.2015.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 582.Inoue J., Krueger E.W., Chen J., Cao H., Ninomiya M., McNiven M.A. HBV secretion is regulated through the activation of endocytic and autophagic compartments mediated by Rab7 stimulation. J. Cell Sci. 2015;128:1696–1706. doi: 10.1242/jcs.158097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 583.Mao Y., Da L., Tang H., Yang J., Lei Y., Tiollais P., Li T., Zhao M. Hepatitis B virus X protein reduces starvation-induced cell death through activation of autophagy and inhibition of mitochondrial apoptotic pathway. Biochem. Biophys. Res. Commun. 2011;415:68–74. doi: 10.1016/j.bbrc.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 584.Lazar C., Macovei A., Petrescu S., Branza-Nichita N. Activation of ERAD pathway by human hepatitis B virus modulates viral and subviral particle production. PLoS ONE. 2012;7:e34169. doi: 10.1371/journal.pone.0034169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 585.Lan S.H., Wu S.Y., Zuchini R., Lin X.Z., Su I.J., Tsai T.F., Lin Y.J., Wu C.T., Liu H.S. Autophagy suppresses tumorigenesis of hepatitis B virus-associated hepatocellular carcinoma through degradation of microRNA-224. Hepatology. 2014;59:505–517. doi: 10.1002/hep.26659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 586.Wang P., Guo Q.S., Wang Z.W., Qian H.X. HBx induces HepG-2 cells autophagy through PI3K/Akt-mTOR pathway. Mol. Cell Biochem. 2013;372:161–168. doi: 10.1007/s11010-012-1457-x. [DOI] [PubMed] [Google Scholar]
- 587.Zhang H.T., Chen G.G., Hu B.G., Zhang Z.Y., Yun J.P., He M.L., Lai P.B. Hepatitis B virus x protein induces autophagy via activating death-associated protein kinase. J. Viral Hepat. 2014;21:642–649. doi: 10.1111/jvh.12191. [DOI] [PubMed] [Google Scholar]
- 588.Zhong L., Shu W., Dai W., Gao B., Xiong S. Reactive Oxygen Species-Mediated c-Jun NH2-Terminal Kinase Activation Contributes to Hepatitis B Virus X Protein-Induced Autophagy via Regulation of the Beclin-1/Bcl-2 Interaction. J. Virol. 2017;91 doi: 10.1128/JVI.00001-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 589.Fu S., Wang J., Hu X., Zhou R.R., Fu Y., Tang D., Kang R., Huang Y., Sun L., Li N., et al. Crosstalk between hepatitis B virus X and high-mobility group box 1 facilitates autophagy in hepatocytes. Mol. Oncol. 2018;12:322–338. doi: 10.1002/1878-0261.12165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 590.Liu B., Fang M., Hu Y., Huang B., Li N., Chang C., Huang R., Xu X., Yang Z., Chen Z., et al. Hepatitis B virus X protein inhibits autophagic degradation by impairing lysosomal maturation. Autophagy. 2014;10:416–430. doi: 10.4161/auto.27286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 591.Ke P.Y., Chen S.S. Autophagy: A novel guardian of HCV against innate immune response. Autophagy. 2011;7:533–535. doi: 10.4161/auto.7.5.14732. [DOI] [PubMed] [Google Scholar]
- 592.Su W.C., Chao T.C., Huang Y.L., Weng S.C., Jeng K.S., Lai M.M. Rab5 and class III phosphoinositide 3-kinase Vps34 are involved in hepatitis C virus NS4B-induced autophagy. J. Virol. 2011;85:10561–10571. doi: 10.1128/JVI.00173-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 593.Gregoire I.P., Richetta C., Meyniel-Schicklin L., Borel S., Pradezynski F., Diaz O., Deloire A., Azocar O., Baguet J., Le Breton M., et al. IRGM is a common target of RNA viruses that subvert the autophagy network. PLoS Pathog. 2011;7:e1002422. doi: 10.1371/journal.ppat.1002422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 594.Hidvegi T., Ewing M., Hale P., Dippold C., Beckett C., Kemp C., Maurice N., Mukherjee A., Goldbach C., Watkins S., et al. An autophagy-enhancing drug promotes degradation of mutant alpha1-antitrypsin Z and reduces hepatic fibrosis. Science. 2010;329:229–232. doi: 10.1126/science.1190354. [DOI] [PubMed] [Google Scholar]
- 595.Puls F., Goldschmidt I., Bantel H., Agne C., Brocker V., Dammrich M., Lehmann U., Berrang J., Pfister E.D., Kreipe H.H., et al. Autophagy-enhancing drug carbamazepine diminishes hepatocellular death in fibrinogen storage disease. J. Hepatol. 2013;59:626–630. doi: 10.1016/j.jhep.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 596.Yue F., Li W., Zou J., Jiang X., Xu G., Huang H., Liu L. Spermidine Prolongs Lifespan and Prevents Liver Fibrosis and Hepatocellular Carcinoma by Activating MAP1S-Mediated Autophagy. Cancer Res. 2017;77:2938–2951. doi: 10.1158/0008-5472.CAN-16-3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 597.Park M., Kim Y.H., Woo S.Y., Lee H.J., Yu Y., Kim H.S., Park Y.S., Jo I., Park J.W., Jung S.C., et al. Tonsil-derived mesenchymal stem cells ameliorate CCl4-induced liver fibrosis in mice via autophagy activation. Sci. Rep. 2015;5:8616. doi: 10.1038/srep08616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 598.He W., Wang B., Yang J., Zhuang Y., Wang L., Huang X., Chen J. Chloroquine improved carbon tetrachloride-induced liver fibrosis through its inhibition of the activation of hepatic stellate cells: Role of autophagy. Biol. Pharm. Bull. 2014;37:1505–1509. doi: 10.1248/bpb.b14-00297. [DOI] [PubMed] [Google Scholar]
- 599.Lee A.Y., Lee J.W., Kim J.E., Mock H.J., Park S., Kim S., Hong S.H., Kim J.Y., Park E.J., Kang K.S., et al. Dihydroceramide is a key metabolite that regulates autophagy and promotes fibrosis in hepatic steatosis model. Biochem. Biophys. Res. Commun. 2017;494:460–469. doi: 10.1016/j.bbrc.2017.10.110. [DOI] [PubMed] [Google Scholar]
- 600.Ruart M., Chavarria L., Camprecios G., Suarez-Herrera N., Montironi C., Guixe-Muntet S., Bosch J., Friedman S.L., Garcia-Pagan J.C., Hernandez-Gea V. Impaired endothelial autophagy promotes liver fibrosis by aggravating the oxidative stress response during acute liver injury. J. Hepatol. 2018 doi: 10.1016/j.jhep.2018.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 601.Deng J., Huang Q., Wang Y., Shen P., Guan F., Li J., Huang H., Shi C. Hypoxia-inducible factor-1alpha regulates autophagy to activate hepatic stellate cells. Biochem. Biophys. Res. Commun. 2014;454:328–334. doi: 10.1016/j.bbrc.2014.10.076. [DOI] [PubMed] [Google Scholar]
- 602.Zhang Z., Guo M., Zhao S., Shao J., Zheng S. ROS-JNK1/2-dependent activation of autophagy is required for the induction of anti-inflammatory effect of dihydroartemisinin in liver fibrosis. Free Radic. Biol. Med. 2016;101:272–283. doi: 10.1016/j.freeradbiomed.2016.10.498. [DOI] [PubMed] [Google Scholar]
- 603.Kim R.S., Hasegawa D., Goossens N., Tsuchida T., Athwal V., Sun X., Robinson C.L., Bhattacharya D., Chou H.I., Zhang D.Y., et al. The XBP1 Arm of the Unfolded Protein Response Induces Fibrogenic Activity in Hepatic Stellate Cells Through Autophagy. Sci. Rep. 2016;6:39342. doi: 10.1038/srep39342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 604.Ni H.M., Woolbright B.L., Williams J., Copple B., Cui W., Luyendyk J.P., Jaeschke H., Ding W.X. Nrf2 promotes the development of fibrosis and tumorigenesis in mice with defective hepatic autophagy. J. Hepatol. 2014;61:617–625. doi: 10.1016/j.jhep.2014.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 605.Lodder J., Denaes T., Chobert M.N., Wan J., El-Benna J., Pawlotsky J.M., Lotersztajn S., Teixeira-Clerc F. Macrophage autophagy protects against liver fibrosis in mice. Autophagy. 2015;11:1280–1292. doi: 10.1080/15548627.2015.1058473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 606.Testerink N., Ajat M., Houweling M., Brouwers J.F., Pully V.V., van Manen H.J., Otto C., Helms J.B., Vaandrager A.B. Replacement of retinyl esters by polyunsaturated triacylglycerol species in lipid droplets of hepatic stellate cells during activation. PLoS ONE. 2012;7:e34945. doi: 10.1371/journal.pone.0034945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 607.Zhao J., Peng L., Cui R., Guo X., Yan M. Dimethyl alpha-ketoglutarate reduces CCl4-induced liver fibrosis through inhibition of autophagy in hepatic stellate cells. Biochem. Biophys. Res. Commun. 2016;481:90–96. doi: 10.1016/j.bbrc.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 608.Wu L., Zhang Q., Mo W., Feng J., Li S., Li J., Liu T., Xu S., Wang W., Lu X., et al. Quercetin prevents hepatic fibrosis by inhibiting hepatic stellate cell activation and reducing autophagy via the TGF-beta1/Smads and PI3K/Akt pathways. Sci. Rep. 2017;7:9289. doi: 10.1038/s41598-017-09673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 609.Wang B., Yang H., Fan Y., Yang Y., Cao W., Jia Y., Cao Y., Sun K., Pang Z., Du H. 3-Methyladenine ameliorates liver fibrosis through autophagy regulated by the NF-kappaB signaling pathways on hepatic stellate cell. Oncotarget. 2017;8:107603–107611. doi: 10.18632/oncotarget.22539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 610.Park S., Kim S., Kim M.J., Hong Y., Lee A.Y., Lee H., Tran Q., Kim M., Cho H., Park J., et al. GOLGA2 loss causes fibrosis with autophagy in the mouse lung and liver. Biochem. Biophys. Res. Commun. 2018;495:594–600. doi: 10.1016/j.bbrc.2017.11.049. [DOI] [PubMed] [Google Scholar]
- 611.Tan S., Lu Y., Xu M., Huang X., Liu H., Jiang J., Wu B. beta-Arrestin1 enhances liver fibrosis through autophagy-mediated Snail signaling. FASEB J. 2018 doi: 10.1096/fj.201800828RR. [DOI] [PubMed] [Google Scholar]
- 612.Kotsafti A., Farinati F., Cardin R., Cillo U., Nitti D., Bortolami M. Autophagy and apoptosis-related genes in chronic liver disease and hepatocellular carcinoma. BMC Gastroenterol. 2012;12:118. doi: 10.1186/1471-230X-12-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 613.Sasaki M., Miyakoshi M., Sato Y., Nakanuma Y. A possible involvement of p62/sequestosome-1 in the process of biliary epithelial autophagy and senescence in primary biliary cirrhosis. Liver Int. 2012;32:487–499. doi: 10.1111/j.1478-3231.2011.02656.x. [DOI] [PubMed] [Google Scholar]
- 614.Sasaki M., Miyakoshi M., Sato Y., Nakanuma Y. Increased expression of mitochondrial proteins associated with autophagy in biliary epithelial lesions in primary biliary cirrhosis. Liver Int. 2013;33:312–320. doi: 10.1111/liv.12049. [DOI] [PubMed] [Google Scholar]
- 615.Hung T.M., Yuan R.H., Huang W.P., Chen Y.H., Lin Y.C., Lin C.W., Lai H.S., Lee P.H. Increased Autophagy Markers Are Associated with Ductular Reaction during the Development of Cirrhosis. Am. J. Pathol. 2015;185:2454–2467. doi: 10.1016/j.ajpath.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 616.Li J., Hu S.B., Wang L.Y., Zhang X., Zhou X., Yang B., Li J.H., Xiong J., Liu N., Li Y., et al. Autophagy-dependent generation of Axin2+ cancer stem-like cells promotes hepatocarcinogenesis in liver cirrhosis. Oncogene. 2017;36:6725–6737. doi: 10.1038/onc.2017.272. [DOI] [PMC free article] [PubMed] [Google Scholar]