Abstract
Background
Because of diverse topographical habitats, the Chenab River wetland harbors a wealth of medicinal and food plant species. This paper presents first quantitative assessment on the ethnobotanical use of plants by the local peoples residing in the Chenab riverine area.
Methods
The ethnobotanical data were collected from six parts of the Chenab River wetland: Mandi Bahuddin, Gujranwala, Gujrat, Sargodha, and Sialkot during 2014 to 2015, using semi-structured interviews. Quantitative indices including informant consensus factor (FCI), relative frequency of citation (RFC), relative importance level (RIL), use value (UV), fidelity level (FL), and corrected fidelity level (CFL) were used to analyze the data.
Results
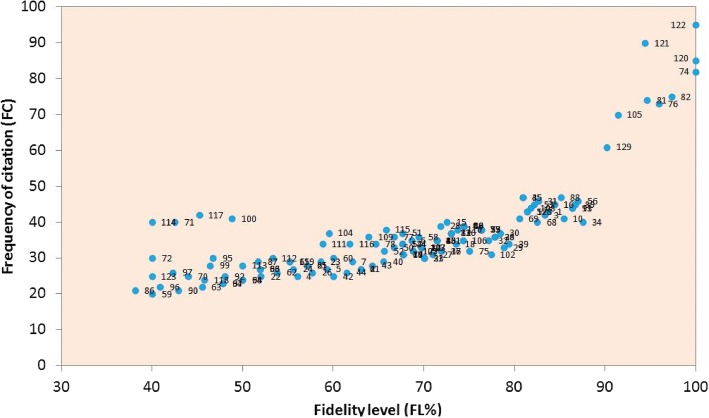
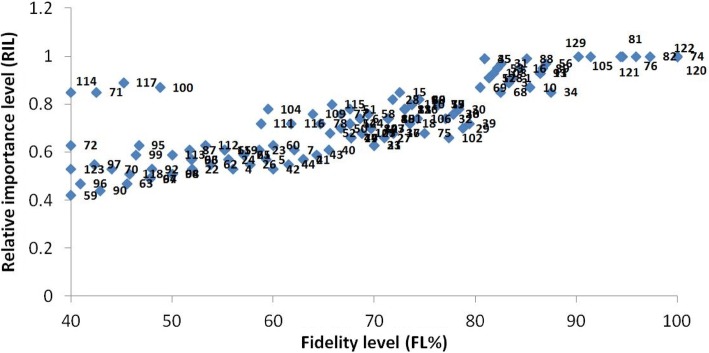
On the whole, 129 medicinal plant species belonging to 112 genera of 59 families were reported, with herbs as dominant life forms (51%). Poaceae was the leading family with 13 species, and leaves were the most frequently utilized plant parts (28%). Herbal medicines were mostly used in the form of powder or decoction, and were mainly taken orally. Withania somnifera, Solanum surattense, Solanum nigrum, Azadirachta indica, Ficus benghalensis, Morus nigra, Morus alba, Polygonum plebeium, and Tribulus terrestris were among the highly utilized plant species, with highest UV, RFC, RIL, FL, and CFL values. The reported ailments were grouped into 11 categories based on FCI values, whereas highest FIC was recorded for gastrointestinal diseases and glandular diseases (0.41 and 0.34, respectively). The use report (UR) and frequency of citation (FC) depicted strong positive correlation (r = 0.973; p = 0.01). The value of determination (r2 = 0.95) indicating 95% variation in UR can be explained in terms of the FC.
Conclusion
The significant traditional knowledge possessed by local communities depicts their strong relation with phytodiversity. Reported data could be helpful in sustainable use and protection of plant species in the Chenab wetland, with special emphasis on medicinal plants. Furthermore, screening of plant-borne active ingredients and in vivo/in vitro pharmacological activities could be of interest for novel drug synthesis.
Electronic supplementary material
The online version of this article (10.1186/s13002-019-0285-4) contains supplementary material, which is available to authorized users.
Keywords: Ethnobotany, Medicinal plants, Quantitative analysis, Chenab riverine, Pakistan
Background
In traditional health care system, botanical or herbal medicines are based on plant extracts or use of plant parts that may be ingested or applied externally. Herbal drugs are prepared as powders, decoctions, infusions, or as poultice, and are operated in a variety of methods [1]. Herbal medicine is very popular around the globe, with particular reference to South Asia, e.g., Pakistan, India, Bangladesh, and Sri Lanka. The main reasons for the popularity of herbal medicines are (i) the belief that plants are close to nature, hence safer than modern synthetic drugs; (ii) easy accessibility; (iii) plants providing a cheaper method of treatment; and (iv) the idea that plants show less side effects or antagonistic reactions as compared to modern drugs [2]. Still today, the majority of the world population, especially rural people in developing countries like Pakistan, Bangladesh, India, or Nepal, partially or entirely rely on herbal medicine [3].
Ethnobotanical studies are important for the discovery of novel medicines from plant species, which are indigenous heritage of global importance [4]. Medicinal plants help in relieving human distress and are widely used as cosmetics, flavors, oil, bitters, spices, sweeteners, insecticides, and dying agents. About 50 thousands angiospermic plants are used as medicinal purpose [5], out of the total 422 thousands angiospermic plants reported around the globe [6]. An estimated 60% of total population in world, including 80% of the population in underdeveloped countries, use traditional phytomedicine to cure several ailments [7]. In Pakistan, about 2000 plant species have been documented to have biochemical properties. About 600 species are used in different Tibb-e Islami dawakhana (herbal drug markets) by general practitioners (GPs). Besides this, about 50,000 tabibs (GPs of Unani medicine), Ayurveda (GPs of folk medicine), and a number of unlicensed health practitioners spread in remote hilly and rural areas are using more than 200 plant species in herbal drugs [8].
Over the last few decades, there has been a considerable interest worldwide in traditional medicine, specifically in herbal medicines. The World Health Organization (WHO) also described the main role of herbal medicines in preventive, promotive, and curative healthcare system, especially in underdeveloped countries [9]. National Center of Complementary and Alternative medicine (NCCAM), U.S. National Institutes of Health (NIH), classifies complementary and traditional therapies into five major catagories such as whole body system (Unani, Homeopathy, Ayurveda, Chinese medicine); body-mind medicine (mental healing, mediation, prayers); bio-based practices (vitamins, herbs, food); therapeutic and alternative body massages (osteopathy, chiropractic); and bio-field therapies [10]. In Pakistan, herbal drugs have been a strong part of our traditional culture and could have played an important role in providing health care to a large part of the population. In the last few years, mainly three categories, i.e., Ayurveda, Tibb-e-Unani, and homeopathy, are in vogue, whereas Chinese traditional medicine (CTM), aromatherapy, and acupuncture have been introduced in different areas of Pakistan [11].
Chenab River is one of the largest rivers of the Indus basin, spanning a length of 960 km. It is an important wetland of the Punjab, with a flora characteristic of tropical thorn forest [12]. This wetland is rich in biodiversity of vegetables, fodder species, fruits, and medicinal plants. In the Chenab revirine area, the caste system is hundreds of years old and still dominates the social structure of the local communities. For a long time, the people of the Hinjra and Aheer castes have settled in the research area. However, before the partition of Pakistan and India, Bhatti, Kharal, and Tarar were the major castes. Though Muslims always were in the majority, Hindus (Barhaman, Khatri, Kapur, Arorah, Khama, and Chopra), Sikh, and Jatt were also common inhabitants and had great influence on the socio-economic setup. The majority of Hindus and Sikhs migrated to India after partition. Presently, the Chenab riverine area is mainly populated with Muslims, which are divided into Awan, Syyeds, Chattha, Tarar, Kharal, Lodhi, and Hinjrah casts. The majority of the population speaks the Punjabi language, while Siraiki and Urdu are also spoken. Although the young generation is fond of modern culture, the majority of the population prefers Islamic traditions due to strong religious bonds.
The local inhabitants of this area possess significant traditional knowledge and are well aware of plant species used with the aim to treat various diseases. Though, Umair et al. [13], Umair et al. [14], and Mahmood et al. [15] reported ethnobotany of neighboring areas, i.e., Hafizabad, Head Khanki, and Gujranwala districts, but these studies were restricted to these three areas only. The local healers of the Chenab wetland hold knowledge about the utilization of native plant species, particularly to treat health disorders. Therefore, the present study was designed with the aim (i) to compile an inventory of the plant species with medicinal scopes; (ii) to document the traditional knowledge of local communities about medicinal plants along with methods of preparation, dosage, and applications; (iii) to compare the ethnobotanic uses for medicinal scopes with previous reports conducted in neighboring areas; and (iv) to compute importance and fidelity indices of ethnomedicinal uses, which could be helpful to evaluate species or preparations for further evidence-based pharmacological screenings.
Methods
The study site
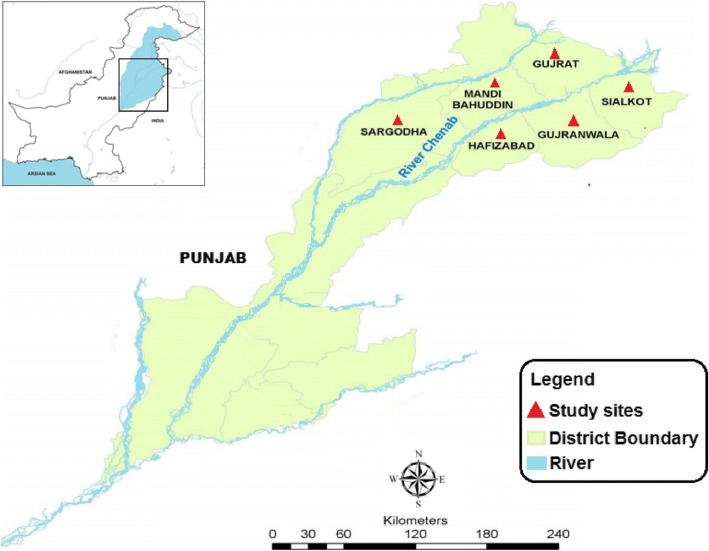
The study was conducted on local communities from six districts of Punjab province, Pakistan viz. Hafizabad, Mandi Bahuddin, Gujranwala, Gujrat, Sargodha, and Sialkot sited around the Chenab River (Fig. 1). The source of river Chenab is in Lahul and Spite district in Himachal Pradesh, India. It entered in Pakistan near Diawara town of district Sialkot at 77°–30° E and 32°–50° N (see Additional file 1). The total length of the river is 960 km. The study area spreads over 20,724 km2. Climate of this area is semi-arid with an annual average temperature from 48 °C during summer to 1 °C during winter [16]. The mean annual precipitation varies from 340 mm in the south to 780 mm in the upper reaches of Chenab River. The pH of the water is alkaline and averages from 7.9 to 8.1 [17]. The soil is fertile and rich in the medicinal plants diversity due to plain topography. Vegetation of the study area is dominated by grass lands and shrub land [15]. Prominent aquatic vegetation of the study area includes Hydrilla verticillata, Nymphaea lotus, Zannichellia palustris, Phragmites karka, Potamogeton crispus, Nelumbo nucifera, Typha angustata, Vallisneria spiralis, and Chara species. The natural vegetation of the surrounding plains includes Tamarix aphylla, Prosopis cineraria, Saccharum spontaneurn, Eleusine compressa, Dalbergia sissoo, and Ziziphus mauritiana. Most common weeds of the area are Tribulus terrestris, Xanthium strumarium Euphorbia prostrata, Parthenium hysterophorus, Achyranthes aspera, Cynodon dactylon, Amaranthus viridis, and Cannabis sativa [18]. There are about 13 million inhabitants in the study area, with a population density of 594 persons per km2. With the growth of human settlement over the centuries, Punjab has cleared most of its forest cover, and over a large part of the Chenab area, bush vegetation has succeeded trees as a result of this land conversion. Nonetheless, a high diversity of grass, herbs, and shrubs persist in this area, which play a key role in herbal medical system [15].
Fig. 1.
River Chenab and its surrounding areas–Pakistan
Documentation and identification of plant species
Field surveys were conducted from April 2014 to July 2015 in four seasons to collect traditional information on therapeutic uses of plant species. Prior consent and approval were taken from departmental ethical committee (Department of Environmental Sciences, COMSATS University Abbottabad Campus) before field survey. Moreover, ethical guidelines of the International Society of Ethnobiology (http://www.ethnobiology.net) were strictly followed during field survey. To collect ethnomedicinal data, questionnaires or semi-structured interviews were conducted with 321 informants (farmers, fishermen, traditional healers/hakeems, housewives, hunters, shopkeepers, and teachers) following the method adopted by Heinrich et al. [19]. Informants were selected on the base of their traditional knowledge on medicinal plants used in health practices. All interviews were conducted after obtaining prior informed consent from the participants (see Additional file 2).
Plant species having medicinal value were collected, dried, pressed, and mounted on herbarium sheets. Voucher specimens were deposited at the Herbarium of Quaid-i-Azam University Islamabad (ISL). Plant species were preliminarily identified during collection, and the identifications were confirmed by expert taxonomist Prof. Dr. Rizwana Aleem Qureshi (Quaid-i-Azam University, Islamabad), and by using the Flora of Punjab and Flora of Pakistan [20–22]. Furthermore, the International Plant Name Index (http://www.ipni.org), the Plant List (www.theplantlist.org), and Germplasm Resources Information Network (GRIN) (http://www.ars-grin.gov/cgi-bin/npgs/html/queries.pl) were used to verify scientific names of plant species, with the nomenclature of families following angiosperm phylogeny group (APG) [23].
Informant consensus factor
The informant consensus factor (FCI) value is used to describe consensus of informants on the consumption of medicinal plant species and evaluates variability in mode of utilization against reported diseases. All the reported ailments are broadly categorized into 11 categories that include gastrointestinal disorder (GIT), dermatological disorders, glandular disorders, respiratory diseases, sexual diseases, urinary disorders, muscles and skeletal disorders cardiovascular disorders, body energizers, nervous disorders, and ear/nose/eye/mouth diseases (ENEM). FCI values ranges from 0.00 to1.00. High FCI (approaching 1) of an ailment category is recorded when one or few species are reported to be used for that ailment by a large proportion of local people due to their authenticity regarding diseases, whereas a low FCI value indicates that the inhabitants use this species arbitrarily to treat reported ailments. The FCI value is calculated using the formula as described in previous studies [19]:
where “Nur” is the total number of use reports for each disease category and “Nt” indicates the number of species used in the said category.
Relative frequency of citation
Relative frequency of citation (RFC) presents the local importance of each species in a study area [24]. To calculate RFC, number of respondents citing a useful species (FC) is divided by total number of respondents in the field survey (N) as explained in previous work [25]. RFC value varies from 1 (when all the respondents refer to a plant as a useful one) to 0 (when nobody refers to a plant as a valuable species). RFC was calculated from the following formula:
Relative importance level
The relative importance level (RIL) presents the level of prominence of each species in a study site. The RIL value was calculated using the method described by Friedman et al. [26]. This index is obtained by dividing the number of respondents mentioning a useful species (FC) with total number of respondents of all species (FCt). A correction scale (CS) is therefore used, in which all the reported plant species are separated into important and unimportant classes. The relative importance level (RIL) varies from 0 to 1.0, with “1” being full importance of a medicinal plant for particular diseases and “0” no ailment cured by a plant species. When all plant species are frequently used to treat some major ailments, relative importance index would be maximum (1.0); then decrease toward zero as the relative importance of the species diverge away from important side. The RIL index value is logically chosen to equal unity for popular plants (i.e., RIL = 1).
Use value
Use value (UV) is a numerical method that proves the relative importance regarding medicinal uses of plant species and is obtained using the following formula:
1here UVi indicates use value of ith species, Ui is the number of uses recorded for ith species, and ni shows the number of respondents who mentioned that species.
Fidelity level
The fidelity level is the percentage of respondents mentioning the uses of a specific plant to treat particular disease. The fidelity level (FL) index was obtained using the given formula [26, 27]:
where FCp is the frequency of citation for a particular disease and FC is the total frequency of citation for any particular disease. A high FL index indicates high frequency and popularity of plant utilization for curing a specific disease by the inhabitants of a study site.
Corrected fidelity level
The corrected fidelity level (CFL) of plant species is used as correction factor to accurately rank the plant species with different FL and RIL values. The CFL is derived from FL, by multiplying FL with RIL values. The CFL index was obtained by the given formula [26, 28].
Pearson correlation coefficient
The Pearson correlation coefficient (PCC) also called as bivariate correlation measures the strength and statistically quantifies the reason of the linear association between two component variables. The data obtained in the interviews were arranged, presented into numeric codes, and subjected to analyses with SPSS 16.0 (SPSS Inc., Chicago, IL). Pearson correlation analysis was analyzed between the frequency of citation (FC) and use reports (UR); the r2 was also measured to calculate species variability and cross relation in term of FC described by variance in UR.
Results and discussion
Demographic features of respondents
A total of 321 local informants which is made up of 265 males and 56 females were interviewed. Based on demographic data, these informants were classified into different classes as given in Table 1. In general, traditional healing is a gender-based practice in which both men and women perform this practice [29]. We found a predominance of male participants in survey (82.55%). Such a frequency is likely due to caution of females to converse with male strangers (the interviewers). It was found that among 321 respondents interviewed, 86% were indigenous peoples (IPs) compared to only 14% of traditional health practitioners (THPs). The indigenous peoples were farmers, fishermen, traditional healers/hakeems, housewives, hunters, shopkeepers, and teachers. The age of informants ranged from 18 to 80 years. Maximum informants (23%) were 60 to 80 years old have significant traditional knowledge, whereas little information was provided by young informants. In view of the fact is that traditional knowledge is passed on from one generation to another over time [30]. Approximately, 64 informants (19.94%) were illiterates; other informants had different level of education as follows: < 5 years’ education (18.38%), 8 years’ education (16.82%), 10 years’ education (14.95%), 12 years’ education (11.84%), 14 years’ education (10.28%), and > 16 years’ education (7.79%). This specifies that a certain proportion of people do make a living from using medicinal plants. According to the World Health Organization (WHO), 80% of the world’s people depend on traditional medicine for their primary healthcare needs [9]. THPs have important information on the medicinal uses of plant species to treat different diseases. The maximum numbers of respondents of THPs having more than 20 years’ experience were 14 (Table 1). This may be due to a close relation and wide interaction of indigenous peoples with plant species. Similar distributions were indicated for other areas in Bangladesh [31] and Turkey [32, 33].
Table 1.
Demographic data of respondents (DDI) from study area
| S. # | Variable | Categories | No. of persons | % |
|---|---|---|---|---|
| 1 | Gender | Female | 56 | 17.45 |
| Male | 265 | 82.55 | ||
| 2 | Informant category | Traditional health practitioners | 45 | 14.02 |
| Indigenous peoples | 276 | 85.98 | ||
| 3 | Age | ≤ 20 years | 33 | 10.28 |
| 20–30 years | 42 | 13.08 | ||
| 30–40 years | 50 | 15.58 | ||
| 40–50 years | 56 | 17.45 | ||
| 50–60 years | 65 | 20.25 | ||
| ≥ 60 years | 75 | 23.36 | ||
| 4 | Educational background | Illiterate | 64 | 19.94 |
| ≤ 5 years | 59 | 18.38 | ||
| 8 years | 54 | 16.82 | ||
| 10 years | 48 | 14.95 | ||
| 12 years | 38 | 11.84 | ||
| 14 years | 33 | 10.28 | ||
| ≥ 16 years | 25 | 7.79 | ||
| 5 | Experience of THPs | < 2 years | 5 | 11.11 |
| 2–5 years | 6 | 13.33 | ||
| 5–10 years | 12 | 26.67 | ||
| 10–20 years | 8 | 17.78 | ||
| > 20 years | 14 | 31.11 |
Taxonomic classification
Overall, 129 medicinal plant species belonging to 112 genera and 59 families were reported (Table 2). Poaceae was the most dominant family with the largest number of species (13), followed by Asteraceae (12), Fabaceae (11), Moraceae (7), Euphorbiaceae (6), Chenopodiaceae and Malvaceae (5 species each), Amaranthaceae, and Solanaceae (4 species each), whereas other families contributed with only 2 or less species (Table 3). The utilization of plant species belonging to Poaceae was similar in ethnobotanical reports from Pakistan and Bangladesh [34, 35].
Table 2.
Medicinal plant species used by the local communities of River Chenab and its surrounding areas
| S.# | Plant species and accession number | Family | Local name | Common name | Life Habits/ Life formsa | Part(s)/mode of utilizationb | Application mode | Therapeutic uses | Quantitative indicesc | Previously usedd | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FC | RFC | UR | UV | RIL | FL | CFL | ||||||||||||
| 1. |
Justicia adhatoda L. ISNI-RC-86 |
Acanthaceae | Baykr | Vasak | P | S | W | LE. powder, decoction, juice; FL. decoction; RT. decoction | Oral, Gargle | Malaria, diabetes, asthma, abortion, toothache | 43 | 0.13 | 28 | 0.65 | 0.91 | 83.7 | 75 | 1♦2♦3♦4♦5♦6■7♦8●9♦10■11●12♦13♦14♦15■16♦17♦18■19♦20♦21♦22♦ |
| 2. |
Trianthema portulacastrum L. ISNI-RC-88 |
Aizoaceae | Itst | Horse parslane | P | H | W | WP. powder; RT. powder, decoction; LE. extract | Oral | Anthelmintic, liver infection, asthma, diuretic, jaundice, | 27 | 0.08 | 11 | 0.41 | 0.57 | 63.0 | 35 | 1■2♦3■4♦5♦6■7♦8♦9♦10♦11♦12♦13■14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 3. |
Achyranthes aspera L. ISNI-RC-01 |
Amaranthaceae | Puth kanda | Prickly-Chaff flower | P | H | W | WP. decoction, extract; ST. powder; LE. paste, powder; RT. decoction; RT. juice | Topical, Oral and as Toothbrush | Kidney stone, pneumonia, chest pain, puncture wounds, ulcer, dysmenorrhea, aerodontalgia, asthma | 42 | 0.13 | 26 | 0.62 | 0.89 | 83.3 | 73 | 1♦2■3■4●5♦6■7●8♦9♦10■11♦12♦13♦14●15♦16♦17♦18♦19♦20■21♦22♦ |
| 4. |
Alternanthera sessilis (L.) R.Br. ex DC. ISNI-RC-128 |
Amaranthaceae | Waglon | Alligator weed | A/P | H | W | LE. juice, cooked, juice; WP. paste; RT. decoction; ST. decoction | Topical, Oral | Eye pain, galactagogue, leucorrhea, snake bite, diarrhea | 25 | 0.08 | 10 | 0.40 | 0.53 | 56.0 | 29 | 1♦2●3●4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 5. |
Amaranthus spinosus L. ISNI-RC-02 |
Amaranthaceae | Gnar | Spiny Pigweed | A | H | W | LE. cooked, juice, extract; RT. juice, decoction; SD. powder; BA. decoction | Gargle, Oral | Vermifuge, dyspepsia, diuretic, odontalgia, cataract, constipation | 27 | 0.08 | 12 | 0.44 | 0.57 | 59.3 | 33 | 1♦2●3♦4■5●6♦7■8●9♦10♦11♦12■13♦14♦15♦16■17♦18♦19♦20♦21♦22♦ |
| 6. |
Amaranthus viridis L. ISNI-RC-03 |
Amaranthaceae | Ganhar | Slender amaranth | A | H | W | LE. extract, cooked, juice, paste; SD. powder; RT. decoction | Oral and Topical | Painful urination, eye pain, constipation, piles, snakebite, cough and asthma | 35 | 0.11 | 19 | 0.54 | 0.74 | 68.6 | 50 | 1♦2●3♦4●5♦6●7■8♦9♦10■11●12■13■14■15♦16■17♦18●19♦20♦21♦22■ |
| 7. |
Mangifera indica L. ISNI-RC-04 |
Anacardiaceae | Aamb | Mango | P | T | C | BA. and LE. latex; LE. decoction, paste, infusion; FR. juice; SD. extract | Topical, Oral | Heel fissures, dysentery, febricity, hypoglycemia, blood pressure, snake bite | 29 | 0.09 | 14 | 0.48 | 0.61 | 62.1 | 38 | 1♦2●3♦4♦5♦6♦7♦8♦9■10♦11♦12♦13●14■15♦16♦17♦18♦19♦20♦21♦22■ |
| 8. |
Polyalthia longifolia (Sonn.) Hook.f. & Thomson * ISNI-RC-25 |
Annonaceae | Ultha ashok | Mast Tree | P | T | C | BA. juice, decoction; LE. Paste | Topical, Oral | Stomachache, body pain, fever, liver tonic | 35 | 0.11 | 18 | 0.51 | 0.74 | 71.4 | 52 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 9. |
Anethum graveolens L. ISNI-RC-82 |
Apiaceae | Sowa | Dil | A/P | H | W/C | SD. powder; LE. infusion, powder | Oral | Gastritis, chronic bronchitis, carminative | 39 | 0.12 | 22 | 0.56 | 0.82 | 74.4 | 60 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10■11♦12♦13■14♦15♦16♦17♦18♦19♦20♦21■22♦ |
| 10. |
Nerium oleander L. ISNI-RC-87 |
Apocynaceae | Kunair | Oleander | P | S | W | RT. powder; ST.; LE. Juice | Oral, Toothbrush and as Eardrops | Aborficient, toothache, ear infection | 41 | 0.13 | 25 | 0.61 | 0.87 | 85.4 | 73 | 1●2♦3●4●5♦6■7♦8♦9♦10♦11●12♦13♦14♦15■16♦17♦18●19■20■21■22♦ |
| 11. |
Pistia stratiotes L.* ISNI-RC-127 |
Araceae | Sabs booti | Water lettuce | P | H | W | WP. decoction; LE. juice, extract; RT. paste | Topical, Oral and as Anal | Painful urination, piles, swelling joint, eczema and leprosy, cough and asthma | 37 | 0.12 | 22 | 0.59 | 0.78 | 73.0 | 56 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 12. |
Schefflera arboricola (Hayata) Hayata ex Merr. * ISNI-RC-89 |
Araliaceae | Choti chatri | Dwarf schefflera | P | H | C | FR.; RT. extract; RT. paste; WP. decoction | Topical, Oral | Ingestion, blood circulation, cut and wounds, abdominal pain | 33 | 0.10 | 21 | 0.64 | 0.70 | 69.7 | 48 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 13. |
Calotropis procera W.T.Aiton ISNI-RC-05 |
Asclepiadaceae | Akh | Milk weed | P | S | W | LE. extract, paste, poultice. Latex; ST. and LE. decoction; ST. latex | Topical, Oral and as Inhale | Cut and wounds, asthma, odontalgia, hepatitis, T.B., malaria, skin burns, lice-infestation | 44 | 0.14 | 28 | 0.64 | 0.93 | 86.4 | 79 | 1■2■3■4♦5♦6♦7●8♦9♦10■11●12■13■14●15■16♦17●18♦19♦20■21■22■ |
| 14. |
Caralluma edulis Benth. ex Hook.f. ISNI-RC-90 |
Asclepiadaceae | Chonga | Caralluma | P | H | W | LE. juice, extract; WP. powder | Oral | Anthelmintic, diuretic, diabetes | 31 | 0.10 | 17 | 0.55 | 0.66 | 67.7 | 44 | 1♦2♦3♦4♦5♦6■7♦8♦9♦10■11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 15. |
Ageratum conyzoides L. ISNI-RC-06 |
Asteraceae | Knar | Goat weed | A | H | W | LE. paste, juice, extract; FL. decoction; ST. powder; WP. juice; RT. juice | Topical, Oral and as Eye drop | Jaundice, wounds, febricity, cough, flu, sexual dysfunction,, hair fall, cataract, indigestion | 40 | 0.12 | 19 | 0.48 | 0.85 | 72.5 | 60 | 1♦2■3●4♦5●6♦7■8♦9♦10♦11♦12♦13♦14■15♦16♦17♦18♦19♦20♦21♦22♦ |
| 16. |
Artemisia scoparia Waldst. & Kit. ISNI-RC-91 |
Asteraceae | Chaou | Wormwood | B | H | W | LE. extract;WP. powder; FL.; SH. Decoction | Topical, Oral | Hair tonic, antidote, malarial fever, laxative | 45 | 0.14 | 27 | 0.60 | 0.95 | 84.4 | 79 | 1♦2♦3♦4♦5♦6■7♦8♦9♦10●11♦12●13♦14♦15■16♦17♦18♦19♦20♦21■22● |
| 17. |
Carthamus oxyacantha M.Bieb. ISNI-RC-92 |
Asteraceae | Pholi | Wild safflower | A | H | W | SD. oil; FL. | Oral | Jaundice, obesity, ulcer, male infertility, bronchitis, thrombosis | 32 | 0.10 | 15 | 0.47 | 0.68 | 71.9 | 48 | 1●2♦3♦4♦5♦6●7♦8♦9♦10●11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 18. |
Cirsium arvense (L.) Scop. ISNI-RC-07 |
Asteraceae | Kandaal | Creeping thistle | P | H | W | LE. Juice; FL.; RT. decoction; ST. | Topical, Oral | Ringworm, hepatic ulcer, body tonic, cough, asthma | 34 | 0.11 | 15 | 0.44 | 0.72 | 73.5 | 52 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17●18♦19♦20♦21♦22♦ |
| 19. |
Conyza bonariensis L. Cornq. ISNI-RC-08 |
Asteraceae | Gider booti | Hairy fleabane | A/P | H | W | WP. Extract; RT. decoction; LE. Infusion, juice | Oral | Irregular menstruation, diarrhea, rheumatoid, hyperglycemia, high blood pressure, dysentery | 38 | 0.12 | 19 | 0.50 | 0.80 | 76.3 | 60 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12■13♦14■15♦16♦17♦18♦19■20■21♦22♦ |
| 20. |
Lepidium didymum L. ISNI-RC-09 |
Asteraceae | Jangli halon | Swine cress | A/B | H | W | ST. powder; LE. infusion; WP. Juice; SH. extract; FL. decoction | Topical, Oral | Bone fracture, tumors, rheumatism, blood purifier, nerve tonic, cold, flu and fever | 36 | 0.11 | 19 | 0.53 | 0.76 | 77.8 | 58 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 21. |
Eclipta prostrata L. ISNI-RC-10 |
Asteraceae | Sofed banghara | Trailing eclipta plant | P | H | W | WP. poultice, powder, decoction; LE. juice/tea, powder; RT. decoction | Topical, Oral | Blood purifier, malaria, skin burns, hepatic tumor, hair oil | 30 | 0.09 | 14 | 0.47 | 0.63 | 70.0 | 44 | 1♦2●3●4♦5♦6●7■8♦9♦10♦11♦12■13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 22. |
Launaea procumbens Roxb. Ramayya & Rajagopal ISNI-RC-94 |
Asteraceae | Pili dodhak | Creeping launaea | P | H | W | LE. paste, extract, juice, decoction; WP. decoction | Topical, Oral and as Bath | Sexual disorder, skin infection, febricity, blood purification, renal disorder | 25 | 0.08 | 9 | 0.36 | 0.53 | 52.0 | 27 | 1♦2♦3♦4♦5♦6♦7●8♦9♦10♦11♦12♦13♦14♦15♦16■17♦18♦19♦20♦21♦22♦ |
| 23. |
Parthenium hysterophorus L. ISNI-RC-14 |
Asteraceae | Gandi boti | Feverfew | A/P | H | W | RT. Juice; FL. powder; WP. decoction, juice; LE. juice, extract | Oral | Laxative, emmenagogue odontalgia, anthelminthic, hyperglycemia, body tonic | 29 | 0.09 | 12 | 0.41 | 0.61 | 58.6 | 35 | 1♦2♦3♦4♦5♦6●7■8♦9♦10■11●12●13■14♦15♦16♦17♦18♦19●20●21♦22♦ |
| 24. |
Sonchus asper Hill. ISNI-RC-11 |
Asteraceae | Asgandh, Dodak | Spiny leaved Sowhistle | A | H | W | WP. powder; LE. paste; SH. decoction; RT. and L.E. decoction | Topical, Oral | Febricity, cough, bronchial asthma, purgative, wounds, indigestion | 27 | 0.08 | 12 | 0.44 | 0.57 | 55.6 | 31 | 1♦2♦3♦4♦5♦6♦7●8♦9♦10♦11♦12♦13■14■15■16■17♦18●19♦20♦21♦22● |
| 25. |
Taraxacum campylodes G.E.Haglund ISNI-RC-93 |
Asteraceae | Peeli booti | Dandilion | A | H | W | LE. paste, powder, decoction; RT. decoction | Topical, Oral | Antidote, diabetes, constipation, liver disorder | 28 | 0.09 | 11 | 0.39 | 0.59 | 57.1 | 33 | 1♦2♦3♦4♦5●6■7♦8●9♦10●11♦12♦13♦14♦15♦16●17♦18■19■20♦21♦22■ |
| 26. |
Xanthium strumarium L. ISNI-RC-13 |
Asteraceae | Chhota Dhatura | Cocklebur | A | H | W | RT. powder; FR. decoction; LE. powder, decoction | Topical, Oral and as Toothbrush | Malaria, skin ulcer, spinal trauma, indigestion, small pox, scrofulous tumors, odontalgia |
26 | 0.08 | 11 | 0.42 | 0.55 | 57.7 | 31 | 1♦2♦3●4♦5♦6●7■8♦9♦10♦11♦12●13♦14♦15♦16♦17♦18♦19♦20♦21■22■ |
| 27. |
Heliotropium strigosum Willd. ISNI-RC-95 |
Boraginaceae | Gorkh paan | Hairy heliotrope | A/P | H | W | WP. powder, extract; LE. extract | Oral | Blood purifier, urinary tract infection, liver tonic | 31 | 0.10 | 16 | 0.52 | 0.66 | 71.0 | 46 | 1●2♦3♦4♦5♦6■7♦8♦9♦10■11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 28. |
Trichodesma indicum (L.) Lehm. ISNI-RC-96 |
Boraginaceae | Kulfa | Tricodescum | A | H | W | LE. decoction, extract, paste | Topical, Oral | Fever, diarrhea, antidote, rheumatism, diuretic | 39 | 0.12 | 19 | 0.49 | 0.82 | 71.8 | 58 | 1♦2♦3♦4♦5♦6■7♦8♦9♦10♦11♦12♦13♦14♦15■16♦17♦18■19●20●21♦22♦ |
| 29. |
Brassica rapa L. ISNI-RC-16 |
Brassicaceae | Sarsoon | Field mustard | B | H | C | SD. powder; WP. cocked; LE. decoction | Topical, Oral | Eczema, blood purification, body tonic |
33 | 0.10 | 16 | 0.48 | 0.70 | 78.8 | 54 | 1●2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13●14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 30. |
Sisymbrium irio L. ISNI-RC-15 |
Brassicaceae | Khoob Kalan | London rocket | A | H | W | SD. poultice; FR. powder, decoction, infusion; WP. juice | Topical, Oral | Ophthalmia, indigestion, mumps and measles, skin ulcer, wounds | 37 | 0.12 | 17 | 0.46 | 0.78 | 78.4 | 60 | 1♦2♦3♦4♦5♦6♦7●8♦9♦10●11♦12●13■14♦15♦16♦17♦18♦19♦20♦21■22♦ |
| 31. |
Cannabis sativa L. ISNI-RC-83 |
Cannabaceae | Bhang | Marijuana | P | S | W/C | LE. paste, extract, infusion; WP. powder; SD. decoction; LE. and SD. juice | Inhale,Topical and as Oral | Constipation, dysentery sedative, snake bite intoxicant, lice infestation, diuretic, purgative, asthma, | 46 | 0.14 | 29 | 0.63 | 0.97 | 82.6 | 79 | 1●2♦3♦4♦5♦6■7●8●9♦10■11♦12■13■14♦15♦16♦17♦18●19♦20♦21■22■ |
| 32. |
Capparis decidua (Forssk.) Edgew ISNI-RC-18 |
Capparidaceae | kerda, kair | Caper plant | P | T | W | LE. paste; ST. and FL. powder; SH. decoction; BA. powder; SD and FL. decoction; FR.; RT. powder | Topical, Oral | Male sexual dysfunction, hemolytic anemia, anthelminthic, indigestion, hepatic disorder, boils, sciatic and joint pain | 35 | 0.11 | 17 | 0.49 | 0.74 | 77.1 | 56 | 1♦2♦3♦4●5♦6♦7■8♦9■10■11■12♦13♦14■15♦16♦17■18♦19♦20♦21♦22♦ |
| 33. |
Stellaria media (L.) vill. ISNI-RC-19 |
Caryophyllaceae | Gandhar | Chickweed | A | H | W | LE. paste, poultice, extract WP. decoction; SD. | Topical, Oral | Bone fracture, constipation, itching, wounds, joint pain | 30 | 0.09 | 14 | 0.47 | 0.63 | 70.0 | 44 | 1♦2♦3♦4♦5●6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16■17♦18♦19♦20♦21♦22♦ |
| 34. |
Ceratophyllum demersum L.* ISNI-RC-129 |
Ceratophyllaceae | Kind-e-Hill | Common contail | P | H | W | LE. juice, decoction, paste | Topical, Oral | Gastric ulcer, diarrhea Biliousness, scorpion stings |
40 | 0.12 | 27 | 0.68 | 0.85 | 87.5 | 73 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 35. |
Chenopodium album L. ISNI-RC-20 |
Chenopodiaceae | Bathu | Lamb’s quarter | A | H | W/C | SH. and FL. juice; WP. cooked; RT. decoction; LE. juice, infusion | Oral | Purgative, indigestion, hepatic disorder, urodynia, rheumatic pain, anthelminthic | 47 | 0.15 | 31 | 0.66 | 0.99 | 80.9 | 79 | 1●2■3♦4♦5♦6■7●8♦9■10■11♦12■13■14■15♦16■17■18♦19♦20♦21■22■ |
| 36. |
Chenopodium ambrosioides L. ISNI-RC-21 |
Chenopodiaceae | Chandan bathwa | Sweet pigweed | A/P | H | W | SH. and FL. juice; WP. juice; LE. decoction, powder, infusion | Topical, Oral | High blood pressure, irregular menstruation, piles, odontalgia, laxative, indigestion | 32 | 0.10 | 15 | 0.47 | 0.68 | 71.9 | 48 | 1♦2●3♦4♦5●6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22■ |
| 37. |
Chenopodium murale L. ISNI-RC-22 |
Chenopodiaceae | Karund | Australian-spinach | A | H | W | SD. powder; ST. and LE. paste; WP. decoction; LE. powder, decoction | Topical, Oral and as Snuff | Indigestion, backbone pain, cold and cough, sexual dysfunction, anthelminthic | 38 | 0.12 | 17 | 0.45 | 0.80 | 76.3 | 60 | 1●2♦3♦4♦5♦6♦7■8♦9■10♦11●12■13●14■15♦16♦17♦18♦19♦20♦21♦22♦ |
| 38. |
Bassia indica (Wight) A.J.Scott ISNI-RC-24 |
Chenopodiaceae | Boi | Indian bassia | A/B | H | W | LE. oil, decoction; FR. | Gargle, Oral | Heart oil, urodynia, odontalgia, tumors | 36 | 0.11 | 16 | 0.44 | 0.76 | 77.8 | 58 | 1♦2♦3♦4♦5♦6♦7●8♦9♦10♦11●12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 39. |
Suaeda vermiculata Forssk. ex J.F.Gmel. ISNI-RC-23 |
Chenopodiaceae | Khaari | Akali seepweed | P | S | W | WP. decoction; ST. ash, decoction; LE. decoction, juice | Topical, Oral | Urodynia, blood purifier, hepatic tumor, snakebite, kidney and bladder stone, hair oil | 34 | 0.11 | 17 | 0.50 | 0.72 | 79.4 | 56 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10●11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 40. |
Convolvulus arvensis L. ISNI-RC-25 |
Convolvulaceae | Lehli/Vahri | Deer’s Foot | A/P | H | W | LE. paste, juice; WP. extract, cooked; RT. | Topical, Oral | Laxative, blood purifier, joint pain, hair oil, ulcer | 29 | 0.09 | 9 | 0.31 | 0.61 | 65.5 | 40 | 1●2♦3♦4♦5♦6●7■8♦9■10●11■12●13●14■15●16♦17●18♦19♦20♦21■22♦ |
| 41. |
Bryophyllum pinnatum (Lam.) Oken ISNI-RC-97 |
Crassulaceae | Zakhm-i-hayat | Air Plant | P | H | C | LE. extract, paste, juice; RT. infusion | Topical, Oral | Wound healing, dysentery, kidney and pancreatic stone, epilepsy | 27 | 0.08 | 9 | 0.33 | 0.57 | 63.0 | 35 | 1♦2♦3♦4♦5♦6■7♦8♦9♦10■11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 42. |
Citrullus colocynthis (L.) Schrad. ISNI-RC-98 |
Cucurbitaceae | Tuma | Bitter apple | P | H | W | FR.; SD. oil | Topical, Oral | Laxtive, amenorrhea Stomachaches, hair tonic constipation, jaundice |
25 | 0.08 | 8 | 0.32 | 0.53 | 60.0 | 31 | 1■2♦3♦4♦5♦6■7♦8♦9■10■11♦12♦13■14■15♦16♦17■18♦19♦20♦21■22● |
| 43. |
Cucumis melo L. ISNI-RC-99 |
Cucurbitaceae | Jangli Kharboza | Pickling melon | A | H | W | FR. decoction; LE. paste; FR. | Topical, Oral | Dysuria, leucorrhea Eczema, purgative |
28 | 0.09 | 8 | 0.29 | 0.59 | 64.3 | 38 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10■11♦12♦13●14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 44. |
Cuscuta reflexa Roxb. ISNI-RC-100 |
Cuscutaceae | Neeli Taar | Giant dodder | A | H | W | SD.; WP. decoction, paste; ST. decoction | Topical, Oral | Urinary disorder, headache, carminative and anodyne, constipation | 26 | 0.08 | 8 | 0.31 | 0.55 | 61.5 | 33 | 1●2■3♦4♦5♦6■7♦8●9♦10●11♦12♦13♦14♦15♦16♦17●18♦19♦20♦21♦22♦ |
| 45. |
Cyperus rotundus L. ISNI-RC-26 |
Cyperaceae | Daila | Nut grass | P | H | W/C | RH. paste, powder, decoction; LE. decoction, paste; RT. infusion | Topical, Oral | Urodynia, anthelminthic, dermatitis, indigestion, lactation, hypersplenism | 47 | 0.15 | 32 | 0.68 | 0.99 | 80.9 | 79 | 1♦2●3♦4♦5♦6■7●8●9♦10■11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 46. |
Chrozophora tinctoria (L.) A.Juss. ISNI-RC-27 |
Euphorbiaceae | Neeli Booti | Giradol | A | H | W | ST. juice; LE. extract decoction, juice | Eye drop, Oral | Indigestion, Throat ache, vomiting, eye redness | 39 | 0.12 | 25 | 0.64 | 0.82 | 74.4 | 60 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 47. |
Croton bonplandianus Baill. ISNI-RC-32 |
Euphorbiaceae | Ban tulsi | Herbel piment | P | H | W | WP. juice, decoction; RT. powder; LE. juice, decoction, poultice; ST. juice | Topical, Oral | Bone Fracture, gastric ulcer, hemorrhage, hair tonic, dermatitis, dengue fever, cardiac tonic | 31 | 0.10 | 21 | 0.68 | 0.66 | 67.7 | 44 | 1♦2●3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 48. |
Euphorbia dracunculoides Lam. ISNI-RC-31 |
Euphorbiaceae | Bamburi | Dragon spurge | A/P | H | W | FR. juice; LE. powder, paste, juice | Topical, Oral | Lice infestation, head ache, snakebite, skin parasites, epilepsy | 35 | 0.11 | 23 | 0.66 | 0.74 | 71.4 | 52 | 1♦2♦3♦4●5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 49. |
Euphorbia helioscopia L. ISNI-RC-28 |
Euphorbiaceae | Chhatri Dodak | Sun euphorbia | A | H | W | WP. powder, latex, juice; SH.; RT.; SD. | Topical, Oral and as Eye drop |
Anthelminthic, athlete’s foot, eye sores, asthma, constipation, cholera | 39 | 0.12 | 23 | 0.59 | 0.82 | 74.4 | 60 | 1♦2♦3♦4●5♦6♦7■8♦9■10■11●12■13■14■15♦16♦17♦18♦19■20■21♦22♦ |
| 50. |
Euphorbia pilulifera L. ISNI-RC-29 |
Euphorbiaceae | Aam dodak, Doddak | Asthma weed | A | H | W | WP. juice, latex, decoction; SD.and FL. powder; LE. juice | Topical, Oral and as Eye drop | Cough, bronchial asthma, indigestion, diarrhea, eye pain, skin burns, cut and wounds | 33 | 0.10 | 22 | 0.67 | 0.70 | 66.7 | 46 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12●13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 51. |
Euphorbia prostrate Aiton. ISNI-RC-30 |
Euphorbiaceae | Doodi Buti | Creeping spurge | P | H | W | LE. infusion, latex, decoction; WP. extract | Topical, Oral | Dysentery, hepatic ulcer, eczema, blood purifier, hyperglycemia, bladder stone, diarrhea | 37 | 0.12 | 22 | 0.59 | 0.78 | 67.6 | 52 | 1♦2●3♦4●5♦6●7■8●9■10■11♦12♦13■14■15♦16♦17♦18■19♦20♦21♦22♦ |
| 52. |
Acacia modesta Wall. ISNI-RC-42 |
Fabaceae | Phulai | Amritsar gum | P | T | W | ST. extract, gum; ST. and LE. latex; LE. extract; BA. ash, powder | Topical, Oral and as Toothbrush | Aerodontalgia, flatulence, tonic, body tonic, joint pain, bronchitis | 32 | 0.10 | 21 | 0.66 | 0.68 | 65.6 | 44 | 1●2♦3♦4♦5♦6■7■8♦9■10■11■12♦13■14♦15■16♦17●18♦19♦20♦21■22♦ |
| 53. |
Acacia nilotica (L.) Delile ISNI-RC-41 |
Fabaceae | Kikar | Babul acacia | P | T | W | FL. powder; LE. decoction, paste; BA. powder, ash, decoction; ST. gum; | Oral, Anal and as Toothbrush | Hyperglycemia, indigestion, dysentery, backbone and joints pain, odontalgia, piles, jaundice | 45 | 0.14 | 31 | 0.69 | 0.95 | 82.2 | 77 | 1●2●3♦4♦5♦6■7●8♦9■10■11■12●13■14♦15●16♦17■18■19♦20♦21♦22♦ |
| 54. |
Albizia lebbeck (L.) Benth. ISNI-RC-104 |
Fabaceae | Sharin | Lebbeck tree | P | T | W | FL.; SD.; ST. (Branches); FR. Decoction | Oral | Sexual disorders, impotency tonic, diuretic, blood purifier, asthma |
34 | 0.11 | 22 | 0.65 | 0.72 | 67.6 | 48 | 1♦2♦3●4♦5♦6■7♦8♦9♦10♦11●12●13♦14♦15♦16♦17■18♦19■20■21♦22♦ |
| 55. |
Alhagi maurorum Medik. ISNI-RC-58 |
Fabaceae | Jawansa | Camel thorn | P | S | W | BA. decoction, powder; BA. ash; LE. decoction, paste; FL. powder; ST. gum | Oral, Toothbrush and as Anal | Hyperglycemia, indigestion, dysentery, backbone and joints pain, odontalgia, piles, jaundice | 38 | 0.12 | 25 | 0.66 | 0.80 | 76.3 | 60 | 1●2♦3♦4♦5♦6●7●8♦9■10●11♦12♦13♦14■15♦16♦17♦18♦19♦20♦21■22♦ |
| 56. |
Cassia fistula L. ISNI-RC-105 |
Fabaceae | Amaltas | Golden shower | P | T | W | SD. powder; FL. powder; RT. extract; LE. poultice | Topical, Oral | Gastric, diarrhea, hyperglycemia, pustule | 46 | 0.14 | 29 | 0.63 | 0.97 | 87.0 | 83 | 1♦2●3■4♦5♦6♦7●8●9♦10♦11♦12■13■14♦15●16♦17♦18♦19♦20♦21♦22■ |
| 57. |
Dalbergia sissoo DC. ISNI-RC-57 |
Fabaceae | Tali | Indian rose wood | P | T | W | WP. decoction; RT. decoction; LE. decoction; FR. powder; RT. infusion; SD. powder | Topical, Oral | Bladder and kidney stone, laxative, piles, bronchial asthma, cough, rheumatism, skin burn, blood purifier | 43 | 0.13 | 28 | 0.65 | 0.91 | 81.4 | 73 | 1●2♦3●4♦5♦6●7●8♦9■10●11●12●13■14■15●16♦17■18♦19■20■21♦22♦ |
| 58. |
Indigofera linifolia (L.f.) Retz. ISNI-RC-107 |
Fabaceae | Gorakh pan | Common Indigo |
A | H | W | WP. decoction; LE. extract; RT. paste; SD. | Topical, Oral | Skin eruption, emollient, swelling joints, tonic | 36 | 0.11 | 21 | 0.58 | 0.76 | 69.4 | 52 | 1♦2♦3♦4♦5♦6●7♦8♦9♦10♦11♦12●13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 59. |
Melilotus indicus (L.) All. ISNI-RC-108 |
Fabaceae | Sinjahi | Sweet clover | A | H | W | LE. paste; WP. powder | Oral | Emollient, diarrhea swellings, bowl complaints, carminative, digestive, skin rash | 20 | 0.06 | 6 | 0.30 | 0.42 | 40.0 | 17 | 1♦2♦3♦4♦5■6♦7♦8♦9■10♦11♦12■13♦14■15♦16■17♦18♦19♦20♦21♦22♦ |
| 60. |
Pongamia pinnata (L.) Pierre ISNI-RC-56 |
Fabaceae | Such chain | Pongam oiltree | P | T | C | LE. powder; FL. powder; BA. decoction; RT. juice, SD. oil; ST. | Topical, Oral | Tooth pain, rheumatic pain, anthelminthic, flatulence, hyperglycemia, wounds and skin ulcer | 30 | 0.09 | 12 | 0.40 | 0.63 | 60.0 | 38 | 1♦2●3♦4♦5♦6■7■8♦9♦10■11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 61. |
Prosopis cineraria (L.) Druce ISNI-RC-43 |
Fabaceae | Jhand | Prosopis | P | S | W/C | FR. powder, paste; ST. decoction; BA. powder; FL. powder; LE. paste, juice | Topical, Oral and as Eye drop | Bladder stone, skin boils, scorpion sting, eye infection, leucorrhoea, dysentery, hepatic ulcer | 28 | 0.09 | 9 | 0.32 | 0.59 | 57.1 | 33 | 1♦2♦3♦4♦5♦6♦7■8♦9■10●11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 62. |
Prosopis juliflora (Sw.) DC. ISNI-RC-40 |
Fabaceae | Mosquet pod | Honey mesquite | P | T | W | BA. powder; LE. poultice, juice; FL. infusion; WP. decoction; ST. | Toothbrush, Topical and as Oral | Bladder stones, tooth pain, breast tumor, bronchial asthma, galactagogue, boils | 26 | 0.08 | 9 | 0.35 | 0.55 | 53.8 | 29 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21■2♦ |
| 63. |
Trifolium resupinatum L. ISNI-RC-55 |
Fabaceae | Loosin | Reversed clover | A | H | W | FL. powder; WP. infusion, decoction | Gargle, Oral | Throat ache, cough, skin ulcer, sedative, liver tonic, indigestion | 22 | 0.07 | 9 | 0.41 | 0.47 | 45.5 | 21 | 1♦2♦3♦4♦5●6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 64. |
Fumaria indica (Hausskn.) Pugsley ISNI-RC-101 |
Fumariaceae | Papra | Indian fumitory | A | H | W | WP. decoction; FL. decoction; FR. Juice; LE. Infusion, tea | Oral | Malaria, constipation, cancer, flu, blood purifier | 24 | 0.07 | 9 | 0.38 | 0.51 | 50.0 | 25 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10■11●12●13♦14♦15♦16♦17♦18♦19■20■21■22■ |
| 65. |
Najas graminea Delile* ISNI-RC-12 |
Hydrocharitaceae | Naiad | Ricefield Waternymph | A | H | W | WP.; LE. paste | Topical | Goiter and boils, anticancer | 29 | 0.09 | 16 | 0.55 | 0.61 | 55.2 | 33 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 66. |
Vallisneria spiralis L.* ISNI-RC-122 |
Hydrocharitaceae | Sawala | tape grass | P | H | W | WP.; LE. paste | Topical, Oral | Leucorrhea, rheumatism | 27 | 0.08 | 16 | 0.59 | 0.57 | 51.9 | 29 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 67. |
Lemna minor L.* ISNI-RC-17 |
Lemnaceae | Cheetri | Duck weed | A | H | W | LE. poultice; WP. decoction, powder | Topical, Oral | Skin rashes, antipyretic, diuretic | 23 | 0.07 | 9 | 0.39 | 0.49 | 47.8 | 23 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 68. |
Abutilon indicum (L.) Sweet. ISNI-RC-102 |
Malvaceae | Pelae | Indian mallow | A/B | H | W | LE. paste, decoction; SD.; WP. powder | Topical, Oral | Syphilis, laxative, piles, bronchial asthma |
40 | 0.12 | 26 | 0.65 | 0.85 | 82.5 | 69 | 1♦2■3●4♦5♦6●7♦8♦9♦10●11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 69. |
Hibiscus rosa-sinensis L. ISNI-RC-37 |
Malvaceae | Gurhal | Rose mallow | P | S | C | RT. powder; LE. tea, juice, paste; FL. juice, powder; FL. | Topical, Oral | Sexual dysfunction, leucorrhoea, asthma, skin ulcer, cardiac pain, carminative, diarrhea | 41 | 0.13 | 25 | 0.61 | 0.87 | 80.5 | 69 | 1♦2●3♦4♦5♦6●7■8♦9♦10♦11♦12♦13■14■15♦16♦17♦18♦19♦20♦21♦22♦ |
| 70. |
Malva parviflora L. ISNI-RC-34 |
Malvaceae | Sonchal | Cheese-weed | A | H | W | SH. and SD. decoction; SH.; LE. decoction, extract, poultice | Topical, Oral | Constipation, abortifacient, sore throat, cough, febricity, scorpion bite | 25 | 0.08 | 7 | 0.28 | 0.53 | 44.0 | 23 | 1●2♦3♦4♦5♦6■7♦8♦9♦10■11●12♦13●14♦15♦16■17♦18♦19♦20♦21♦22♦ |
| 71. |
Malvastrum coromandelianum (L.) Garcke ISNI-RC-35 |
Malvaceae | Dhamni Buti | False mallow | A | H | W | WP. powder; LE. poultice, decoction, paste | Topical, Oral | Skin sores, eczema, wounds, diarrhea, asthma | 40 | 0.12 | 23 | 0.58 | 0.85 | 42.5 | 35 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12■13●14♦15♦16♦17♦18♦19■20■21♦22♦ |
| 72. |
Malvaviscus arboreus Cav. ISNI-RC-36 |
Malvaceae | Max mallow | Sleeping hibiscus | P | S | C | LE. juice, decoction; FL. infusion, decoction | Topical, Oral | Throat ache, diarrhea, febricity, Skin eruption | 30 | 0.09 | 17 | 0.57 | 0.63 | 40.0 | 25 | 1♦2♦3♦4♦5♦6♦7■8●9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 73. |
Marsilea minuta L.* ISNI-RC-103 |
Marsiliaceae | Chopatti | Water clover | P | F | W | LE. juice, decoction; FL. infusion, decoction | Topical, Oral | Throat ache, diarrhea, febricity, lice-infestation | 38 | 0.12 | 21 | 0.55 | 0.80 | 76.3 | 60 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 74. |
Azadirachta indica A. Juss. ISNI-RC-39 |
Meliaceae | Neem | Neem | P | T | W/C | LE. decoction, infusion, paste; SD. oil; ST; BA. decoction; LE. paste | Oral, Toothbrush and as Topical | Hyperglycemia, malarial fever, Blood purifier, vermifuge, headache, small pox, aerodontalgia, hepatic ulcer, rheumatic pain | 82 | 0.26 | 61 | 0.74 | 1.00 | 100.0 | 100 | 1■2■3●4♦5♦6♦7●8●9♦10♦11♦12●13■14♦15♦16♦17■18♦19♦20♦21♦22♦ |
| 75. |
Melia azedarach L. ISNI-RC-38 |
Meliaceae | Dhraikh | Chinaberry | P | T | W/C | ST. decoction; BA. powder; LE. juice, decoction, paste, infusion, extract | Topical, Oral and as Bath | Malaria, itching, wound healing, urinary stones, hypertension, hyperglycemia, blood purification | 32 | 0.10 | 18 | 0.56 | 0.68 | 75.0 | 50 | 1♦2●3♦4♦5♦6●7●8●9♦10■11■12■13■14♦15■16♦17♦18♦19♦20♦21♦22■ |
| 76. |
Ficus benghalensis L. ISNI-RC-106 |
Moraceae | Bohr | Banyan tree | P | T | W | ST. latex; LE. decoction | Oral | Premature ejaculation, syphilis and gonorrhea, male sexual power | 73 | 0.23 | 53 | 0.73 | 1.00 | 95.9 | 96 | 1■2●3♦4♦5♦6■7♦8♦9♦10●11♦12●13■14♦15♦16♦17●18♦19♦20♦21♦22♦ |
| 77. |
Ficus benjamina L. ISNI-RC-44 |
Moraceae | Kabar | Weeping Fig | P | T | W | ST. decoction; BA. and LE. cocked; LE. decoction; FR.; WP. powder | Topical, Oral | Stomachache, skin ulcers, flatulence, rheumatic pain, blood purification | 36 | 0.11 | 19 | 0.53 | 0.76 | 66.7 | 50 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦15● |
| 78. |
Ficus racemosa L. ISNI-RC-45 |
Moraceae | Gular | Cluster tree | P | T | W/C | ST. latex; FR.; BA. decoction, powder; LE. juice | Topical, Oral and as Anal | Diarrhea, adiposity, flatulence, piles, ulcer and boils | 34 | 0.11 | 16 | 0.47 | 0.72 | 64.7 | 46 | 1♦2■3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 79. |
Ficus religiosa L. ISNI-RC-46 |
Moraceae | Pipal | Sacred Fig | P | T | W | RT. extract; ST. powder; FR. powder; LE. infusion, paste, decoction | Topical, Oral | Body tonic, bronchial asthma, heart blockage, leucorrhea, ulcer, hypoglycemia | 31 | 0.10 | 15 | 0.48 | 0.66 | 67.7 | 44 | 1♦2●3♦4♦5♦6♦7●8♦9●10♦11♦12■13●14■15♦16♦17●18♦19♦20♦21♦22♦ |
| 80. |
Ficus virens Aiton ISNI-RC-47 |
Moraceae | Palakh | White Fig | P | T | W | ST. latex; BA. infusion; FR. powder | Oral | Hyperglycemia, ulcer, breast tumor | 39 | 0.12 | 20 | 0.51 | 0.82 | 74.4 | 60 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 81. |
Morus alba L. ISNI-RC-48 |
Moraceae | Shahtoot | White mulberry | P | T | C | LE. and BA. decoction; WP. decoction; ST. latex; LE. juice; FR. juice, decoction | Topical, Oral | Cough, constipation, hepatic ulcer, tonsils, snake bite, hypoglycemia | 74 | 0.23 | 54 | 0.73 | 1.00 | 94.6 | 95 | 1♦2♦3♦4♦5♦6♦7■8♦9■10■11♦12■13■14■15■16♦17●18■19♦20♦21■22■ |
| 82. |
Morus nigra L. ISNI-RC-49 |
Moraceae | Kala toot | Black mulberry | P | T | C | RT. Powder; LE. infusion, decoction; FR. juice, decoction; WP. decoction | Gargle, Oral | Sore throat, cough, asthma, flu, aerodontalgia, hypoglycemia, constipation, vermifuge, carminative | 75 | 0.23 | 52 | 0.69 | 1.00 | 97.3 | 97 | 1♦2♦3♦4♦5♦6●7■8♦9♦10■11●12♦13■14♦15■16♦17♦18■19♦20♦21♦22■ |
| 83. |
Eucalyptus camaldulensis Dehnh. ISNI-RC-51 |
Myrtaceae | Safaida | River red-gum | P | T | W | LE. oil, extract, juice, decoction | Gargle, Oral | Sinusitis, sore throat, cold, cough, febrifuge, flu | 37 | 0.12 | 18 | 0.49 | 0.78 | 73.0 | 56 | 1■2♦3♦4♦5♦6♦7■8♦9♦10■11♦12♦13●14♦15♦16♦17■18♦19♦20♦21♦22♦ |
| 84. |
Psidium guajava L. ISNI-RC-50 |
Myrtaceae | Amrud | Guava | P | S | C | FL. decoction; LE. extract, decoction, infusion; FR. | Gargle, Oral | Diarrhea, hyperglycemia, urodynia, carminative, cough, vermifuge, aerodontalgia, febricity, flu | 33 | 0.10 | 15 | 0.45 | 0.70 | 69.7 | 48 | 1♦2♦3♦4♦5♦6♦7■8●9♦10■11♦12♦13■14■15♦16♦17♦18♦19♦20♦21♦22♦ |
| 85. |
Nelumbo nucifera Gaertn.* ISNI-RC-118 |
Nelumbonaceae | Sacred lotus | Kanwal | P | H | W | RT. paste; FL. Juice; LE. paste; RH. paste | Oral, Topical | Piles, diarrhea, headache, ring worm, cardio-tonic | 35 | 0.11 | 18 | 0.51 | 0.74 | 71.4 | 52 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 86. |
Boerhavia diffusa L. ISNI-RC-52 |
Nyctaginaceae | Itsit | Horse-purslane | A/P | H | W | RT. powder, decoction; LE. paste; WP. infusion | Topical, Oral | Dysmenorrhea, cough, snake bite, bronchial asthma, kidney failure, flu | 21 | 0.07 | 6 | 0.29 | 0.44 | 38.1 | 17 | 1●2♦3■4♦5♦6♦7●8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 87. |
Nymphaea lotus L.* ISNI-RC-119 |
Nymphaeaceae | Kamiyan | Lotus | P | H | W | LE. and BA. decoction; WP. powder; RT. | Oral | Malarial fever, diuretic, enteritis | 29 | 0.09 | 13 | 0.45 | 0.61 | 51.7 | 31 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 88. |
Jasminum officinale L. ISNI-RC-53 |
Oleaceae | Malti | Poet’s jasmine | P | S | C | LE. extract; FL. decoction; WP. extract; ST. extract, juice | Topical, Oral | Febricity, cough, anthelmintic, scabies, conjunctivitis, diarrhea, heart burn | 47 | 0.15 | 28 | 0.60 | 0.99 | 85.1 | 83 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15■16♦17♦18♦19♦20♦21♦22♦ |
| 89. |
Jasminum sambac (L.) Ait. ISNI-RC-54 |
Oleaceae | Motia | Arabian jasmine | P | S | C | RT. decoction; LE. paste, juice, decoction, extract; FL. juice | Topical, Oral | Conjunctivitis, wound and cuts, emmenagogue, febricity, breast cancer, ulcer, insomnia | 45 | 0.14 | 26 | 0.58 | 0.95 | 86.7 | 81 | 1♦2■3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 90. |
Oxalis corniculata L. ISNI-RC-33 |
Oxalidaceae | Khatti Buti | Clover sorrel | P | H | W | RT. decoction; WP. powder, decoction; LE. paste, cooked | Topical, Oral and as Eye drop | Diarrhea and dysentery, hepatitis C, wounds, eye inflammation, vermifuge, sexual dysfunction | 21 | 0.07 | 9 | 0.43 | 0.44 | 42.9 | 19 | 1♦2♦3●4♦5●6●7●8●9♦10■11♦12●13■14●15■16●17●18■19♦20♦21♦22● |
| 91. |
Argemone mexicana L. ISNI-RC-109 |
Papaveraceae | Stianasi | Mexican poppy | P | H | W | FL. powder; LE. extract | Topical, Oral | Sexual problems, premature ejaculation, spermatoria, emollient, purgative | 44 | 0.14 | 24 | 0.55 | 0.93 | 86.4 | 79 | 1♦2♦3●4♦5●6■7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 92. |
Avena sativa L. ISNI-RC-110 |
Poaceae | Jungli jai | Common oat | A | G | W | WP. powder; LE. infusion | Oral | Nerve tonic, antispasmodic, diuretic | 25 | 0.08 | 9 | 0.36 | 0.53 | 48.0 | 25 | 1♦2♦3♦4♦5♦6■7♦8♦9■10♦11♦12●13■14■15♦16♦17●18♦19♦20♦21♦22♦ |
| 93. |
Cenchrus pennisetiformis
Hoschst. & Steud. ISNI-RC-60 |
Poaceae | Cheetah gha | White buffel grass | A/P | G | W | ST. juice; FR. decoction; LE. infusion, juice, extract | Topical, Oral | Eczema, cough, T.B., asthma, skin irritation, epilepsy, piles | 27 | 0.08 | 11 | 0.41 | 0.57 | 51.9 | 29 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 94. |
Cynodon dactylon (L.) Pers. ISNI-RC-61 |
Poaceae | Khanbal gha | Bermuda grass | P | G | W | RT. infusion; WP. juice, paste, decoction; RH. Decoction, oil | Topical, Oral and as Eardrops | Stomachache, bladder stones, eye inflammation, high blood pressure, itching, earache | 23 | 0.07 | 11 | 0.48 | 0.49 | 47.8 | 23 | 1♦2●3♦4♦5♦6●7■8●9■10●11●12■13●14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 95. |
Dactyloctenium aegyptium (L.) Willd. ISNI-RC-62 |
Poaceae | Madhana gha | Crow’s foot grass | A | G | W | WP. paste; RT.; SD. | Topical, Oral | Uterine prolapse, kidney stones, indigestion, ulcer and wounds | 30 | 0.09 | 14 | 0.47 | 0.63 | 46.7 | 29 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 96. |
Dichanthium annulatum (Forssk.) Stapf ISNI-RC-63 |
Poaceae | Murgha gha | Ringed dichanthium | P | G | W | ST. and LE. decoction; ST. powder; LE. juice, infusion, paste; | Topical, Oral | Abortifacient, diarrhea, indigestion, piles, antispasmodic, scabies | 22 | 0.07 | 7 | 0.32 | 0.47 | 40.9 | 19 | 1♦2♦3♦4♦5♦6♦7■8♦9■10♦11♦12♦13♦14●15♦16♦17♦18♦19♦20♦21♦22♦ |
| 97. |
Eleusine indica (L.) Gaertn. ISNI-RC-64 |
Poaceae | Madhani | Goose grass | A | G | W | LE. juice; RT. powder; RH. extract; WP. decoction, tea, infusion | Topical, Oral | Febricity, dysentery, irregular menstruation, hyperglycemia, hair tonic, food poisoning | 26 | 0.08 | 10 | 0.38 | 0.55 | 42.3 | 23 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12●13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦15● |
| 98. |
Imperata cylindrica (L.) Raeusch. ISNI-RC-65 |
Poaceae | Dabh gha | Cogon grass | P | G | W | RT. decoction; RH. decoction; LE. paste; SH. and LE. paste | Topical, Oral | Body tonic, hypertension, wounds and cuts, urodynia, febricity | 24 | 0.07 | 9 | 0.38 | 0.51 | 50.0 | 25 | 1♦2♦3●4♦5♦6♦7■8●9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 99. |
Panicum antidotale Retz. ISNI-RC-123 |
Poaceae | Sonali | Giant panic | A | G | W | ST. decoction; LE. juice, infusion | Topical, Oral | Respiratory tract infection, appetite, gonorrhea, skin diseases | 28 | 0.09 | 13 | 0.46 | 0.59 | 46.4 | 27 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10■11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 100. |
Phragmites karka (Retz.) Trin. ex Steud. ISNI-RC-120 |
Poaceae | Nur | Common reed | P | G | W | RT. paste; WP. decoction | Topical, Oral | broken bones, rheumatic pain, diaphoretic | 41 | 0.13 | 25 | 0.61 | 0.87 | 48.8 | 42 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12●13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 101. |
Saccharum spontaneum L.* ISNI-RC-124 |
Poaceae | Kahn | Wild cane | P | G | W | RT. decoction; WP. powder; LE. paste | Topical, Oral | Skin eruption, fever, body pain, vermifuge, wounds | 35 | 0.11 | 19 | 0.54 | 0.74 | 71.4 | 52 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 102. |
Setaria glauca (L.) P.Beauv. ISNI-RC-66 |
Poaceae | Bajra | Yellow foxtail | A/P | G | W | SD.; LE. infusion, juice; ST. decoction | Topical | Wound healing, dermatitis, ring worm, tonic, hair tonic | 31 | 0.10 | 17 | 0.55 | 0.66 | 77.4 | 50 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 103. |
Sorghum halepense (L.) Pers. ISNI-RC-67 |
Poaceae | Baru | Johnson grass | P | G | W | ST. juice; SD. powder; RT. decoction | Topical, Oral | Stomachache, emollient, boils, cough | 33 | 0.10 | 19 | 0.58 | 0.70 | 69.7 | 48 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 104. |
Triticum aestivum L. ISNI-RC-59 |
Poaceae | Kanak | Wheat | A | G | C | SH. decoction; SD. decoction, paste, powder; RT. decoction | Topical, Oral | Colon cancer, wound healing, anemia, asthma, late puberty, hyperglycemia | 37 | 0.12 | 21 | 0.57 | 0.78 | 59.5 | 46 | 1●2♦3♦4♦5♦6♦7●8●9♦10♦11♦12■13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 105. |
Polygonum plebeium R. Br. ISNI-RC-68 |
Polygonaceae | Hind rani | Small knotweed | A | H | W | RT. decoction, LE. extract; SH. decoction; WP. powder, paste | Topical, Oral | Eczema, galactagogue, pneumonia, liver-tonic, heartburn, regular bowl | 70 | 0.22 | 50 | 0.71 | 1.00 | 91.4 | 91 | 1♦2♦3●4♦5♦6●7■8♦9♦10●11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 106. |
Rumex dentatus L. ISNI-RC-69 |
Polygonaceae | Jangli palak | Toothed dock | A | H | W | WP. decoction; LE. and RH. poultice; RT. powder, decoction | Topical, Oral | Eczema, wounds and cuts, constipation, body tonic | 35 | 0.11 | 21 | 0.60 | 0.74 | 74.3 | 54 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14■15■16■17♦18♦19■20■21♦22■ |
| 107. |
Eichhornia crassipes (Mart.) Solms. ISNI-RC-111 |
Pontederiaceae | Dasi Kulfa | Water-hyacinth | A | H | W | LE. infusion, paste; ST. powder | Topical, Oral | Piles, constipation, cold, flu, respiratory diseases, vermifuge, antiseptic | 32 | 0.10 | 18 | 0.56 | 0.68 | 68.8 | 46 | 1♦2♦3♦4♦5♦6●7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 108. |
Portulaca quadrifida L. ISNI-RC-112 |
Portulacaceae | Kulfa | Common purslane | A | H | W | WP. powder, LE. infusion | Oral | Jaundice, liver and spleen problems | 44 | 0.14 | 26 | 0.59 | 0.93 | 81.8 | 75 | 1♦2♦3●4♦5♦6●7♦8♦9♦10♦11♦12♦13♦14♦15♦16●17♦18♦19♦20♦21♦22♦ |
| 109. |
Anagallis arvensis L. ISNI-RC-70 |
Primulaceae | Bilibooti | Scarlet pimpernel | A | H | W | ST. powder; LE. and FL. decoction; WP. juice, paste | Topical, Oral | Skin ulcer, leprosy, hepatitis C, epilepsy | 36 | 0.11 | 20 | 0.56 | 0.76 | 63.9 | 48 | 1♦2♦3●4♦5♦6♦7■8♦9●10♦11♦12■13♦14●15♦16♦17♦18♦19♦20♦21♦22♦ |
| 110. |
Ranunculus laetus wall. ex Hook. f. & J.W. Thomson* ISNI-RC-113 |
Ranunculaceae | Sarsoon booti | Celery-leaved buttercup | A | H | W | LE. paste; FL. extract; SD.; RT. extract | Topical, Oral | Skin infection, conjunctivitis, body tonic, antirheumatic | 38 | 0.12 | 20 | 0.53 | 0.80 | 73.7 | 58 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 111. |
Ranunculus sceleratus L. ISNI-RC-71 |
Ranunculaceae | Gul-e-ashrafi | Blister buttercup | A/B | H | W | WP. infusion, juice, decoction; RT. paste; SD. | Topical, Oral | Febricity, body tonic, asthma, muscle hamstring, urinary incontinence, anthelmintic | 34 | 0.11 | 18 | 0.53 | 0.72 | 58.8 | 42 | 1♦2♦3♦4♦5♦6♦7●8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 112. |
Oligomeris linifolia (Vahl ex Hornmen) J.F. Macbr.* ISNI-RC-114 |
Resedaceae | Shootk | Lineleaf oligomeris | A | H | W | SD.; WP. infusion, juice; LE. tea | Oral | Diarrhea, jaundice, throat pain and cough, menstrual problems | 30 | 0.09 | 16 | 0.53 | 0.63 | 53.3 | 33 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 113. |
Ziziphus nummularia (Burm. f.) Wight and Arn. ISNI-RC-73 |
Rhamnaceae | baer | Jujube | P | S | W | LE. paste, decoction; BA. decoction; FR. powder | Topical, Oral | Body tonic, hyperglycemia, constipation, scabies, sore throat and cold | 28 | 0.09 | 13 | 0.46 | 0.59 | 50.0 | 29 | 1♦2♦3■4♦5♦6●7■8♦9♦10■11■12♦13♦14♦15♦16♦17♦18■19●20●21■22♦ |
| 114. |
Ziziphus mauritiana Lam. ISNI-RC-72 |
Rhamnaceae | bairi | Chinese apple | P | T | W | BA. and LE. decoction; BA. powder; LE. decoction, extract, juice; RT. decoction | Topical, Oral, Bath and as Gargle | Chicken pox, ulcers, diarrhea, asthma, toothache, jaundice | 40 | 0.12 | 24 | 0.60 | 0.85 | 40.0 | 33 | 1♦2●3●4♦5♦6♦7■8●9♦10♦11●12●13●14♦15♦16♦17■18♦19♦20♦21●22♦ |
| 115. |
Murraya koenigii (L.) spreng. ISNI-RC-74 |
Rutaceae | Kari patta | Curry leaf | P | T | C | LE. decoction, juice, infusion, paste; BA. powder; SD. | Topical, Oral | Hyperglycemia, skin eruption, diarrhea, rheumatic pain, eye inflammation, hair oil | 38 | 0.12 | 21 | 0.55 | 0.80 | 65.8 | 52 | 1♦2●3■4♦5♦6♦7■8♦9♦10♦11♦12●13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 116. |
Salvadora oleoides Decne. ISNI-RC-115 |
Salvadoraceae | Pelo | Toothbrush tree | P | S | W | ST (Branches); FR. | Oral, Toothbrush | Tonic, stomachache, toothache | 34 | 0.11 | 16 | 0.47 | 0.72 | 61.8 | 44 | 1♦2♦3♦4♦5♦6■7♦8♦9■10■11♦12♦13♦14■15♦16♦17■18♦19♦20♦21♦22♦ |
| 117. |
Veronica polita Fr. ISNI-RC-75 |
Scrophulariaceae | Veroni | Greyfield speedwell | A | H | W | ST. and LE. cooked; LE. tea, juice; ST. and LE. decoction | Oral | Stomachache, blood purifier, nerve-tonic, cough | 42 | 0.13 | 4 | 0.10 | 0.89 | 45.2 | 40 | 1♦2♦3♦4♦5♦6♦7●8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 118. |
Misopates orontium (L.) Raf.* ISNI-RC-116 |
Scrophulariaceae | Kutta Phool | Snapdragon | A | H | W | WP. extract; LE. poultice, Juice | Topical, Oral and as Eye drop | Contusions, tumors and ulcers, eye inflammation | 24 | 0.07 | 13 | 0.54 | 0.51 | 45.8 | 23 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 119. |
Datura innoxia Mill. ISNI-RC-79 |
Solanaceae | Datura | Thorn apple | P | S | W | WP. powder; SD. paste; LE. decoction, extract; FR.; ST. infusion; RT. decoction | Oral, Inhale and as Topical | Rabies, piles, cough, asthma, lice-infestation, premature ejaculation, purgative, narcotic and sedative | 29 | 0.09 | 15 | 0.52 | 0.61 | 55.2 | 33 | 1♦2♦3●4●5♦6●7■8♦9♦10♦11■12♦13●14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 120. |
Solanum nigrum L. ISNI-RC-76 |
Solanaceae | Mako | Night shade | A | H | W | LE. powder, cocked, decoction; LE. extract; LE. and FL. juice; RT. pate; WP. Decoction | Topical, Oral and as Eye drop | Breast cancer, diarrhea, febricity, ulcer, chicken pox, hyperglycemia, piles, cardiac pain, sore eyes, cuts and wounds | 85 | 0.26 | 69 | 0.81 | 1.00 | 100.0 | 100 | 1♦2●3●4●5♦6●7●8●9■10■11♦12♦13■14■15■16■17■18■19♦20♦21♦22■ |
| 121. |
Solanum surattense Burm.f. ISNI-RC-77 |
Solanaceae | Kundiari | Thorny nightshade | P | H | W | WP. cooked, decoction; FR. paste; RT. decoction; LE. and FR. decoction | Oral, Topical | Kidney stones, febricity, heel cracks, anthelmintic, asthma, wound healing, liver tonic, rheumatic arthritis | 90 | 0.28 | 74 | 0.82 | 1.00 | 94.4 | 94 | 1●2●3●4●5♦6●7■8●9■10■11●12♦13♦14■15■16♦17●18●19♦20♦21♦22● |
| 122. |
Withania somnifera (L.) Dunal. ISNI-RC-78 |
Solanaceae | Asgandh | Winter cherry | P | H | W | LE. paste, decoction, powder; WP. powder; FR.; FL. powder; RT. powder | Oral, Topical and as Snuff | Malarial fever, stomachache, night mare, hyperglycemia, asthma, irregular menstruation, breast cancer, wounds | 95 | 0.30 | 80 | 0.84 | 1.00 | 100.0 | 100 | 1■2♦3♦4■5♦6■7■8♦9■10■11■12■13■14■15♦16♦17♦18♦19♦20♦21♦22♦ |
| 123. |
Pterospermum acerifolium (L.) Willd ISNI-RC-80 |
Starculiaceae | Kanakchanpa | Maple-leaved Bayur tree | P | T | W/C | FL. paste, infusion, decoction; BA. powder | Topical, Oral | Piles, vermifuge, impotency, body tonic, swellings | 25 | 0.08 | 12 | 0.48 | 0.53 | 40.0 | 21 | 1♦2♦3♦4♦5♦6♦7■8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 124. |
Tamarix aphylla (L.) H.Karst. ISNI-RC-81 |
Tamaricaceae | Athel tamarisk | Rukh | P | T | W | LE. poultice, paste, decoction; BA. ash | Topical, Oral | Febricity, wound and boils eye infection, cough and cold | 34 | 0.11 | 17 | 0.50 | 0.72 | 67.6 | 48 | 1●2♦3♦4♦5♦6♦7●8♦9■10■11♦12♦13♦14■15♦16♦17♦18♦19♦20♦21♦22♦ |
| 125. |
Tamarix dioica Roxb. ex Roth ISNI-RC-117 |
Tamaricaceae | Rukh | Tamarisk | P | S | W | BA. powder; LE. | Oral | Pile, tonic, cough, diarrhea, antiseptic, spleen disorder and liver problems | 32 | 0.10 | 15 | 0.47 | 0.68 | 68.8 | 46 | 1♦2♦3♦4♦5♦6■7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17■18♦19♦20♦21♦22♦ |
| 126. |
Trapa bispinosa Roxb.* ISNI-RC-126 |
Trapaceae | Singhara | Water chestnut | A | H | W/C | FR.; SD. powder, paste | Oral | Diarrhea and dysentery, dysuria, body energizer, menstrual disorder | 37 | 0.12 | 19 | 0.51 | 0.78 | 73.0 | 56 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11♦12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 127. |
Typha angustata Bory & Chaub. ISNI-RC-121 |
Typhaceae | Kundar | Long Cattails | P | H | W | RH. paste; FL. | Oral | Diarrhea and dysentery, mumps and measles, gonorrhea | 33 | 0.10 | 18 | 0.55 | 0.70 | 69.7 | 48 | 1♦2♦3♦4♦5♦6♦7♦8♦9♦10♦11●12♦13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 128. |
Lantana camara L. ISNI-RC-84 |
Verbenaceae | Lantana | Lantana | P | S | W | RT. extract; FL. extract; LE. juice, decoction, paste | Topical, Oral | Ringworm, headache, aerodontalgia, malarial fever, rheumatoid arthritis, cuts and wounds, injuries, cough, cold, | 43 | 0.13 | 25 | 0.58 | 0.91 | 81.4 | 73 | 1♦2♦3♦4♦5●6♦7■8♦9■10♦11♦12■13♦14♦15♦16♦17♦18♦19♦20♦21♦22♦ |
| 129. |
Tribulus terrestris L. ISNI-RC-85 |
Zygophyllaceae | Gukhro | Puncture vine | A/B | H | W | FR. powder, decoction; LE. paste; WP. powder, decoction | Topical, Oral | Dysentery and diarrhea, urodynia, irregular menstruation, wounds, dyspepsia | 61 | 0.19 | 41 | 0.67 | 1.00 | 90.2 | 90 | 1■2♦3♦4♦5♦6♦7■8♦9■10■11♦12♦13■14♦15●16♦17■18♦19♦20♦21♦22♦ |
aLife habits/life forms: C cultivated, W wild, G grass, S shrubs, H herbs, T trees, P perennial, B biennial, A annual
bPlant parts: RH rhizome, BA bark, FL flower, SD seed, WP whole plant, SH shoot, ST stem, RT root, FR fruit, LE leaf
cQuantitative indices: FC frequency of citation, RFC relative frequency of citation, UR use report, UV use value, RIL relative importance level, FL fidelity level, CFL corrected fidelity level
*Plants species which are newly reported in this study
(■) = Plant with similar use(s); (●) = plant with dissimilar use (s); (♦) = plant not reported in previous study
Previously used: (1) Ullah et al. [62]; (2) Mollik et al. [79]; (3) Verma et al. [80]; (4) Rahman et al. [72]; (5) Chaitanya et al. [73]; (6) Mahmood et al. [15]; (7) Umair et al. [13]; (8) Luitel et al. [74]; (9) Ahmed et al. [75]; (10) Malik et al. [76]; (11) Murad et al. [46]; (12) Zahoor et al. [61]; (13) Rehman et al. [77]; (14) Ahmed et al. [78]; (15) Ahmed et al. [81]; (16) Abbasi et al. [82]; (17) Mussarat et al. [83]; (18) Rashid et al. [84]; (19) Amjad et al. [43]; (20) Shaheen et al. [85]; (21) Aziz et al. [86]; (22) Hussain et al. [87]
Table 3.
Family wise distribution of medicinal plants in the study area
| Families | No. of genera | % age contribution | No. of species | % age contribution |
|---|---|---|---|---|
| Poaceae | 13 | 11.61 | 13 | 10.08 |
| Asteraceae | 12 | 10.71 | 12 | 9.30 |
| Fabaceae | 11 | 9.82 | 12 | 9.30 |
| Moraceae | 2 | 1.79 | 7 | 5.43 |
| Euphorbiaceae | 3 | 2.68 | 6 | 4.65 |
| Chenopodicaeae | 3 | 2.68 | 5 | 3.88 |
| Malvaceae | 5 | 4.46 | 5 | 3.88 |
| Amaranthaceae | 3 | 2.68 | 4 | 3.10 |
| Solanaceae | 3 | 2.68 | 4 | 3.10 |
| Asclepiadaceae | 2 | 1.79 | 2 | 1.55 |
| Boraginaceae | 2 | 1.79 | 2 | 1.55 |
| Brassicaceae | 2 | 1.79 | 2 | 1.55 |
| Cucurbitaceae | 2 | 1.79 | 2 | 1.55 |
| Hydrocharitaceae | 2 | 1.79 | 2 | 1.55 |
| Meliacea | 2 | 1.79 | 2 | 1.55 |
| Myrtaceae | 2 | 1.79 | 2 | 1.55 |
| Oleaceae | 1 | 0.89 | 2 | 1.55 |
| Polygonaceae | 2 | 1.79 | 2 | 1.55 |
| Ranunculaceae | 1 | 0.89 | 2 | 1.55 |
| Rhamnaceae | 1 | 0.89 | 2 | 1.55 |
| Scharopholariaceae | 2 | 1.79 | 2 | 1.55 |
| Tamaricaceae | 1 | 0.89 | 2 | 1.55 |
| Acanthaceae | 1 | 0.89 | 1 | 0.78 |
| Aizoaceae | 1 | 0.89 | 1 | 0.78 |
| Anacardiaceae | 1 | 0.89 | 1 | 0.78 |
| Annonaceae | 1 | 0.89 | 1 | 0.78 |
| Apiaceae | 1 | 0.89 | 1 | 0.78 |
| Apocynaceae | 1 | 0.89 | 1 | 0.78 |
| Araceae | 1 | 0.89 | 1 | 0.78 |
| Araliaceae | 1 | 0.89 | 1 | 0.78 |
| Cannabaceae | 1 | 0.89 | 1 | 0.78 |
| Capparidaceae | 1 | 0.89 | 1 | 0.78 |
| Caryophyllaceae | 1 | 0.89 | 1 | 0.78 |
| Ceratophyllaceae | 1 | 0.89 | 1 | 0.78 |
| Convolvulaceae | 1 | 0.89 | 1 | 0.78 |
| Crassulaceae | 1 | 0.89 | 1 | 0.78 |
| Cuscutaceae | 1 | 0.89 | 1 | 0.78 |
| Cyperaceae | 1 | 0.89 | 1 | 0.78 |
| Fumariaceae | 1 | 0.89 | 1 | 0.78 |
| Lemnaceae | 1 | 0.89 | 1 | 0.78 |
| Marsiliaceae | 1 | 0.89 | 1 | 0.78 |
| Nelumbonaceae | 1 | 0.89 | 1 | 0.78 |
| Nyctaginaceae | 1 | 0.89 | 1 | 0.78 |
| Nymphaeaceae | 1 | 0.89 | 1 | 0.78 |
| Oxalidaceae | 1 | 0.89 | 1 | 0.78 |
| Papaveraceae | 1 | 0.89 | 1 | 0.78 |
| Pontederiaceae | 1 | 0.89 | 1 | 0.78 |
| Portulacaceae | 1 | 0.89 | 1 | 0.78 |
| Primulaceae | 1 | 0.89 | 1 | 0.78 |
| Resedaceae | 1 | 0.89 | 1 | 0.78 |
| Rutaceae | 1 | 0.89 | 1 | 0.78 |
| Salvadoraceae | 1 | 0.89 | 1 | 0.78 |
| Starculiaceae | 1 | 0.89 | 1 | 0.78 |
| Trapaceae | 1 | 0.89 | 1 | 0.78 |
| Typhaceae | 1 | 0.89 | 1 | 0.78 |
| Verbenaceae | 1 | 0.89 | 1 | 0.78 |
| Zygophyllaceae | 1 | 0.89 | 1 | 0.78 |
| Total | 112 | 100 | 129 | 100 |
The wild herbaceous flora constituted 51% of the reported plant species (Fig. 2). Perennial herbs were the most common life habit in the study area. Often, the medicinal plants indicated have perennial life cycles [36, 37]. Wild trees contributed to 13% of the medicinal flora; wild grass and shrubs 8% each; cultivated herbs, shrubs, and grasses 7%, 6%, and 5% respectively; and cultivated grass and wild ferns 1% each (Fig. 2). These findings were similar to previous reports [1, 35]. The common use of wild herbs may be due to their easy availability and efficiency in the treatment of different ailments compared to other life habit. The Engineers India Research Institute (EIRI) [38] reported that wild herbs are more efficient and effective for use in medicines than those grown in garden. Probably, traditional healers used mostly herbs and trees compared to other life forms as medicine due to their availability in nature [39]. Local people usually collected medicinal plants from roadsides, swamp or swamp edges, woodlots, wet grasslands, grassland, bush land, forest, forest edge, fallow land, home garden, and cropland. Species range limits are alienated by the species ecological niche [40], which are often found to be linked with spatial gradients in ecological factors (e.g., precipitation, temperature) and are explained by a set of factors, e.g., climate, habitat structure, and predators or competitors pairs [41]. According to the local informants, herb sellers often collect plants from the wild and supply to herbal market (Pansara) without paying any attention to their conservation. Although some of the listed plants are presented in the study area, some of them are rare due to harvesting or deforestation.
Fig. 2.
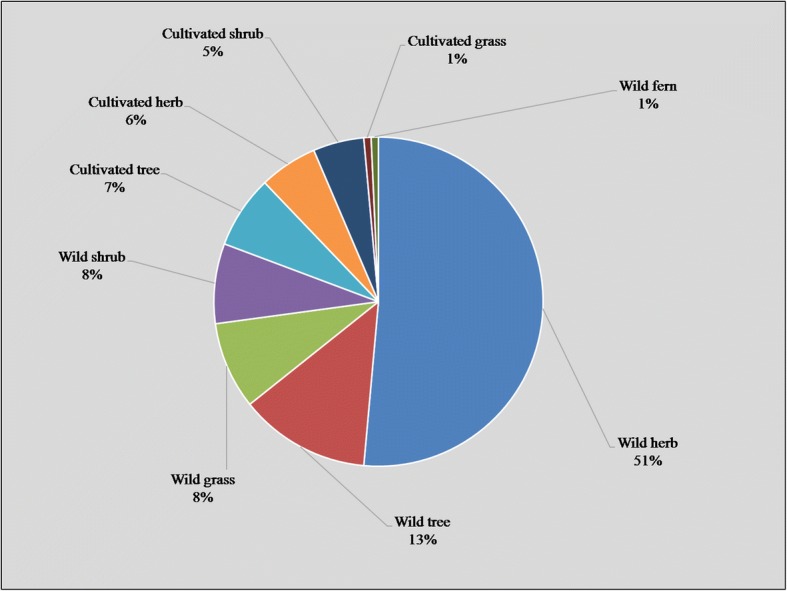
Life forms and habits of medicinal plant species
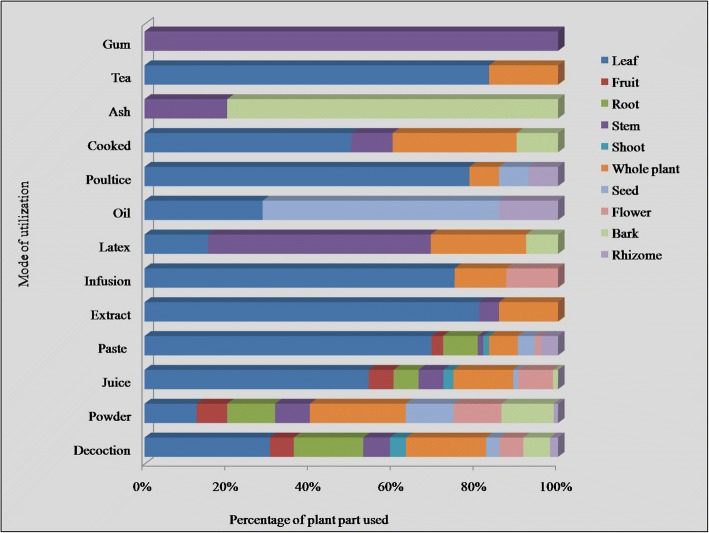
Plant part(s) used
The use of plant parts in the preparation of recipes depends upon their availability and knowledge of local people. Leaves were the most frequently utilized plant part with 28% applications in traditional herbal medicine, followed by whole plant (15%), root (13%), stem (10%), seed and flower (8% each), fruit (7%), bark (6%), shoot (3%), and rhizome (2%) (Fig. 3). Leaves are commonly used in herbal medicines because they are rich in bioactive secondary metabolites. Leaves are the main photosynthetic organs and also act as storages for exudates or photosynthates; some of which defend the plants against destructive entities or are of medicinal values to the human body [24, 42]. In previous studies, leaves were also reported as the most frequently utilized plant part [13, 43]. Apart from leaves, the use of whole plants has also been reported in many studies [44–46]. In some cases, the same plant part was used to treat different ailments, e.g., leaves of Withania somnifera were taken orally to treat asthma and malarial disease, and applied externally to heal wounds. Similar uses of plants parts of many other species are mentioned in Table 2.
Fig. 3.
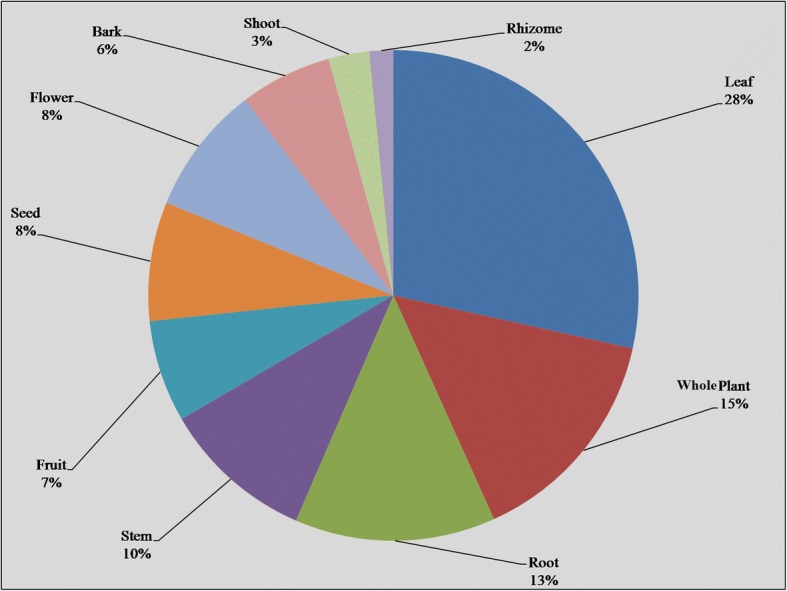
Plant parts used in traditional recipes
Toxic plants
Some plant species such as Croton sparsiflorus, Datura innoxia, Lantana camara, Nerium oleander, Calotropis procera, Solanum spp., Euphobia spp., and Ranunculus sceleratus show toxic effects, if taken in excessive amount [13, 47]. Nerium oleander (Kunair) causes gastrointestinal disorder (laxative effect) and mental instability (hemorrhage) when used in excess. Likewise, Lantana camara (Lantana) is claimed to cause itchy feelings. The approach for drug development from plant species depends on several ways in which this can be done, including toxicity, chemical content, traditional use, randomized selection, or combination of several criteria. Beneficial or adverse effects of plant-based medicines depend on method of herbal drug preparation and its utilization in herbal medicine [48]. In general, the indigenous peoples of the study area use above-mentioned species in minimal quantities to avoid their poisonous effects, which suggest that they may have at least some empiric knowledge of their dangerousness.
Mode of preparation and application
Herbal medications were prescribed in different forms including powder, decoction, juice, extract, paste, poultice, infusion, ash, etc. (Fig. 4). Decoction was the most commonly used method of herbal preparation with 31%, followed by powder, juice, paste, and extract (19, 17, 14, and 4%, respectively), while the remaining preparations (infusion, poultice, latex, cooked food, oil, tea, ash, and gum) were used for less than 3% of indications. According to Umair et al. [13], decoction was the most used method for herbal preparations in Hafizabad region of Punjab province. Decoctions are often used as one of the major forms of preparations in traditional healthcare system, because they are easy to prepare by mixing herbs with water, tea, or soup [49, 50]. To make decoctions, plant parts are boiled in water until the original volume of the water is reduced to one-fourth [51], whereas plant extract is prepared by crushing or squeezing the plant parts before extraction [52].
Fig. 4.
Preparations used in herbal recipes
Usually, traditional recipes were based on a single plant species. However, in some cases, more than one plant species was used in drug preparation [53]. For instance, the treatment of cough and asthma was done by using a decoction prepared from S. surattense and Tinospora cordifolia. Yamamoto et al. [54] reported that a traditional herbal medicine prepared from eight medicinal plants (Dai-Saiko-to) is used to lower the lipid levels in human body suffering from diabetic hyperlipidemia. In most herbal preparations, water was used as a solvent; however, honey, oil, milk, or tea were also used to enhance the acceptability and hypothesizing their implication in the enhancement of the medicinal properties of the preparation, e.g., root powder of Boerhavia diffusa is commonly mixed with honey and used to treat cough, asthma, and flu.
In the present work, plant-based medications were most frequently utilized to treat different ailments including gastrointestinal disorders (stomachache, gastric ulcer, gas trouble, intestinal worms, vomiting, constipation, dysentery, diarrhea), respiratory problems (asthma, cough, flu, throat ache), skin infections (chicken pox, measles, eczema, rashes, cuts, and wounds), fever, diabetes, kidney problems, cancer, toothache, earache, eye pain, cardiac problems, jaundice, inflammation, menstrual disorders, piles, bone fracture, rheumatism, snake bite, scorpion sting, milk production, and general weakness. The most often utilized mode of administration was oral (48%), followed by topical (36%), as toothbrush (4%), eye drops and gargle (3% each), anal application (2%) and bathe, inhale, eardrops, and snuff (1% each) (Fig. 5). Similar modes of applications were reported in Hafizabad district [13].
Fig. 5.
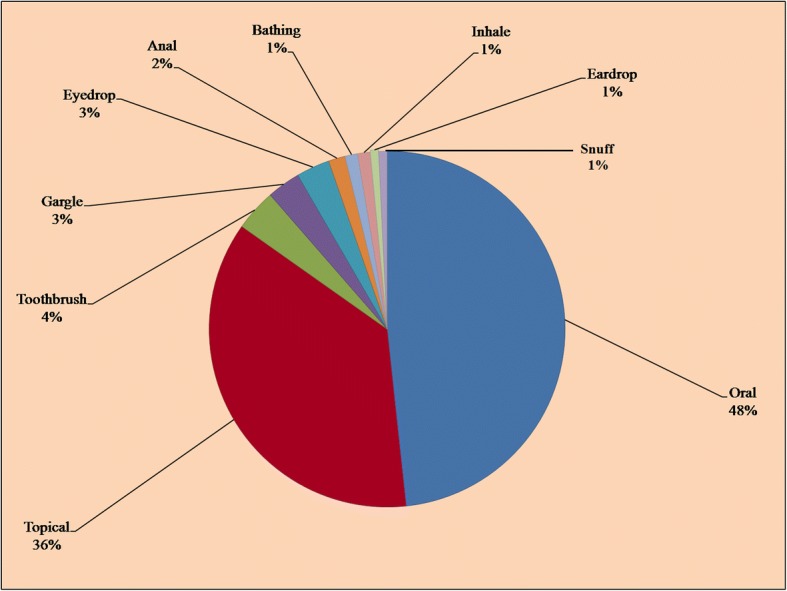
Mode of application of medicinal plants
It has been reported that oral mode of administration is the most preferred route (76%) among the communities of Gujranwala district, Pakistan [15]. The practice of oral administration may be linked to the use of some additives or solvents (milk, tea, hot coffee, fruit juice, and water) that are commonly believed to serve as a vehicle to transport the herbal medicines. The additives or solvents are also important to improve the taste, minimize soreness, and decrease adverse effects such as diarrhea, vomiting, and increase the efficacy and healing conditions [55]. These results are in agreement to other studies [31, 56]. Leaves of Melia azedarach and Zizyphus mauritiana were used in medicinal baths to treat skin diseases, i.e., allergy and chicken pox. Li et al. [57] reported that medicinal baths are an important traditional method to cure and prevent common ailments among the traditional Yao communities of Jinping County, China. Medicinal baths are commonly used to prevent and treat skin diseases, rheumatic diseases, injuries, and gynecological disorders.
Informant consensus factor
To determine the informant consensus factor (FIC), all the reported ailments were first grouped into 11 different disease categories on the basis of their use reports (Table 4). The uppermost FCI value is recorded for GIT diseases (0.41), followed by glandular diseases (0.34), dermatological disorder, and respiratory diseases (0.29). The mean FIC for all ailments categories was 0.17, which was similar to previously published studies reported from Pakistan [13, 58, 59]. Among the three major disease categories, GIT diseases were dominated with 154 use-reports, followed by dermatological disorders, and glandular complaints (120 and 103 use-reports, respectively) as mentioned in Table 4. Around 71.3% plant species were used to treat GIT disorders, followed by glandular complaints (65.9%), respiratory diseases (52.7%), ENEM diseases (40.3%), sexual diseases (31.0%), urinary problems, muscle and skeletal disorders (27.1% each), cardiovascular disorders (24%), body energizer (14%), and nervous disorders (7.8%). These results show that GIT and dermatological diseases are common in the study area. Similar findings have already been reported from other regions [31, 60]. Dermatological disorders with respect to FCI ranked as third category. The local people of the study area mostly prefer to use these plant-based treatments against skin diseases, insects bites, and scorpion sting.
Table 4.
Informants consensus factor (FCI) by categories of ailments in the study area
| Category of ailments | Nur. | % of use reports | Nt. | % of species | Nur-Nt | Nur-1 | FCI |
|---|---|---|---|---|---|---|---|
| GIT diseases | 154 | 23.2 | 92 | 71.3 | 62 | 153 | 0.41 |
| Dermatological disorders | 120 | 18.1 | 85 | 65.9 | 35 | 119 | 0.29 |
| Glandular disorders | 103 | 15.5 | 68 | 52.7 | 35 | 102 | 0.34 |
| Respiratory diseases | 73 | 11.0 | 52 | 40.3 | 21 | 72 | 0.29 |
| ENEM diseases | 43 | 6.5 | 40 | 31.0 | 3 | 42 | 0.07 |
| Sexual diseases | 42 | 6.3 | 35 | 27.1 | 7 | 41 | 0.17 |
| Urinary disorders | 36 | 5.4 | 35 | 27.1 | 1 | 35 | 0.03 |
| Muscles and Skeletal disorders | 32 | 4.8 | 28 | 21.7 | 4 | 31 | 0.13 |
| Cardiovascular disorders | 32 | 4.8 | 31 | 24.0 | 1 | 31 | 0.03 |
| Body energizers | 18 | 2.7 | 18 | 14.0 | 0 | 17 | 0.00 |
| Nervous disorders | 11 | 1.7 | 10 | 7.8 | 1 | 10 | 0.10 |
| Mean FCI | – | – | – | – | – | – | 0.17 |
Relative frequency of citation and use report
In our study, relative frequency of citation (RFC) of the encountered plant species varied from 0.30 to 0.06 (Table 2). Maximum RFC value was calculated for species W. somnifera (0.30) followed by Solanum surattense (0.28), Solanum nigrum and Azadirachta indica (0.26 for each), Ficus benghalensis, Morus nigra, M. alba (0.23 for each), Polygonum plebeium (0.22), and Tribulus terrestris (0.19). Melilotus indica has the lowest RFC (0.06) in the area while Zahoor et al. [61] reported that M. indica has the highest RFC (0.78) which is contrary to our results. It can be seen that plants with the highest RFC are the most frequent medicinal plant in that region and majority of the people agreed by its medicinal value [58]. Use report value varied from 4 to 80 in the present study. W. somnifera, S. surattense, S. nigrum, A. indica, M. alba, Ficus benghalensis, M. nigra, P. plebeium, and T. terrestris were the most used plant species. Bibi et al. [58] reported the lowest use report of S. nigrum and T. terrestris (2 UR). The differences may be due to variation in vegetation and geo-climate of the area.
Use value and potential of medicinal plants
The use value (UV) index is a method of the types of uses attributed to specific plant species and families for a population. In the present study, UV of the encountered plant species ranged from 0.84 to 0.1 (Table 2). The use value of W. somnifera, S. surattense, S. nigrum, A. indica, M. nigra, F. benghalensis, P. plebeium, and M. alba were 0.84, 0.82, 0.81, 0.74, 0.73, 0.73, and 0.71 respectively. Zahoor et al. [61] reported the lowest UV of W. somnifera (0.0085), M. alba (0.02), and A. indica (0.03), which is contrary to our results. The low UV of Veronica polita, Malva parviflora, Cucumis melo, and B. diffusa may be due to poor availability and lack of knowledge. These results were comparable with previous reports from Gujranwala and Hafizabad district, Pakistan [13, 15]. However, differences in most of the mentioned species and their quantitative values were also observed. In a field survey carried out by Ullah et al. [62], Plantago ovata and Lawsonia inerm were the most important species with the highest use value (0.98), while Bibi et al. [58] reported that Berberis balochistanica and Citrullus colocynthis had maximum use value (0.18 each), followed by Descurainia sophia (0.15). These differences may be due to variation in geo-climate, vegetation, traditional knowledge of informants, and their culture.
In Pakistan, majority of the people rely on medicinal plants to find treatments for their minor and major diseases [63]. Medicinal plants are growing abundantly in the wild, or some are cultivated on farmlands in the Punjab, Sindh, KPK, Baluchistan, and Azad Kashmir [64]. W. somnifera is an important wild medicinal plant used in Pakistan from the old time by the herbalists in making different medicines [65]. Withanolides extracted from W. somnifera are reported to be effective in protecting against β-amyloid-induced neurotoxicity [66]. In our study, leaves and berries of S. nigrum and Solanum xanthocarpum are commonly used for the treatment of gastric ulcers and cracked heel. Abbas et al. [67] assured the possible potential of antifungal as well as antimicrobial activity of fruit extracts of two Solanaceous plants (S. nigrum and S. xanthocarpum).
Relative importance level
The importance of a plant species increases as it is used to treat more infirmities by the informants. For species mentioned by 20 to 48 respondents, the relative importance level (RIL) value increases directly with the increase in number of respondents. The RIL value of plant species mentioned by 48 or more respondents does not accelerate with the increased number of respondents (Fig. 6). One hundred twenty-three plant species, which were mentioned by 47 or less respondents, were classified as unimportant, whereas the 6 plant species cited by 48 respondents or more were declared as important. W. somnifera, S. surattense, S. nigrum, A. indica, F. benghalensis, M. nigra, M. alba, and T. terrestris were the most significant plant species with 1.0 RIL (Table 2). Umair et al. [13] reported the high popularity of S. surattense, S. nigrum, and W. somnifera in Hafizabad district, Pakistan. It can be seen that plants with high RIL value may attributed to their high efficacy and the awareness of local peoples which specifies their use as herbal medicine. These results were in agreement with previous reports on the medicinal use of plant species, e.g., among the local peoples of Negev district, Israel [26] and Palestinian area [28]. The high RIL value of plant species might be attributed to a wider geographic distribution, cultural knowledge and informant’s awareness.
Fig. 6.
Relationship between numbers of informants and relative importance level (RIL). Numbers represent the plant names as they appear in Table 2
Fidelity level
The fidelity level (FL) index is used to notify plant species that are most favored by the indigenous peoples to treat certain diseases [68]. Plant species with highest medicinal uses in a given area have maximum value of FL, i.e., 100%. In the present investigation, the FL value of the 129 plant species varied from 14.3 to 100% (Fig. 7). Generally, the high fidelity level of a species shows the abundance of a particular disease in a specific area and the utilization of plant species by the local people to treat it [58, 69]. The fidelity levels calculated for M. nigra (asthma), F. benghalensis (male sexual power), M. alba (cough), S. surattense (kidney stones), P. plebeium (pneumonia), and T. terrestris (urodynia) were 97.3, 95.9, 94.6, 94.4, 91.4, and 90.2%, respectively (Table 2). The most commonly used medical plants in the study area with 100% FL were A. indica, S. nigrum, and W. somnifera, which were used as blood purifier, to treat breast cancer and as stomachache, respectively. Comparatively, fidelity levels of these species were very high than previous reports [13] against gastrointestinal disorders, respiratory tract infections, urinary disorders, cardiovascular diseases, fever, pain, inflammation, and urological disorders with almost similar fidelity level. Additionally, in the present study, same species were reported to treat more diseases compared to previous report [14]. Plant species having high FL are seen as particularly interesting for biological, phytochemical, and pharmacological studies to evaluate and prove their validity to introduce novel drugs and herbal products.
Fig. 7.
Relationship between numbers of informants claimed use of certain plant for particular disease. Numbers represent the plant names as they appear in Table 2
Corrected fidelity level
The corrected fidelity level (CFL) index is used to properly rank the plant species with different FL and RIL values. The resultant RIL values given in Table 2 were used as correction factor (CF) to adjust the FL values. The measured level of CFL of each plant species is mentioned in Table 2. The CFL value of only nine species was above 90. W. somnifera, S. nigrum, and A. indica were the highest utilized species with maximum CFL = 100, followed by M. nigra, F. benghalensis, M. nigra, S. surattense, P. plebeium, and C. sativa (97, 96, 95, 94, 91, and 90, respectively). This was probably due to increasing popularity of traditional medicines among the local peoples of the study area. Additionally, the respondents of the rural areas had more interaction and information about medicinal uses of plant species compared to urban areas. These findings were analogous to previous results from Hafizabad district [13], Negev district, Israel [26], and Palestinian area [28].
Statistical analysis
The Pearson correlation coefficient (PCC) measures the power of a linear association between two component variables. The PCC index between UR and FC was 0.973 at p = 0.01 level. This reflects a highly significant positive association between the number of informants mentioning certain plant species and the number of applications reported. Furthermore, this shows that frequent use of plant species by the inhabitants tend to rise the applications number of usable species (y = 0.9269x − 13.637; correlation coefficient r2 = 0.947). In the present investigation, the value of r2 was 0.95 which indicates that around 95% of the variation in UR could be described in terms of the FC (Table 5). The plant species with higher FC value most have higher UR, such as W. somnifera and S. surattense. The present results are in accordance with previous reports. For example, Amjad et al. [43], Bano et al. [70], and Vijayakumar et al. [71] reported Pearson correlation coefficient between RFC and UV of 0.732, 0.638, and 0.881, respectively, with r2 = 0.54, 0.41, and 0.77 in respective order.
Table 5.
Correlation coefficient between frequency of citation (FC) and use reports (UR)
| Correlations | ||
|---|---|---|
| Variables | UR | FC |
| UR | ||
| Pearson Correlation | 1 | 0.973** |
| Sig. (two-tailed) | 0.000 | |
| N | 129 | 129 |
| FC | ||
| Pearson Correlation | 0.973** | 1 |
| Sig. (two-tailed) | 0.000 | |
| N | 129 | 129 |
**Correlation is significant at the 0.01 level (two-tailed)
r2 = 0.947
Novelty and future impact
To find the novelty index, data on ethnomedicinal uses of encountered species were compared with previous published reports from neighboring areas and Pakistan (Table 3). A total of 22 published studies were chosen for comparative analysis. W. somnifera shows maximum similarity with previously reported work from the surrounding areas [13, 15, 46, 61, 62, 72–78]. The ethnomedicinal data recorded from the study site discloses significant variations in the herbal preparation, dosage, applications, and utilization of plant parts recorded from other neighboring areas. About 12.47% uses of encountered species were comparable to previous reports. Moreover, 47% uses of the reported species were similar to previous study conducted in Hafizabad district [13]. Notably, 78.82% uses of the documented medicinal plant species were not reported in the previous studies used for comparative and novelty index obtained by dividing no use reports with all use reports for species multiply by 100. The percentage of novel uses (8.77%) of encountered species with respect to previous reports was obtained by dividing dissimilar use reports with all use reports for species multiply by 100. The comparison with neighboring areas depicted significant resemblances due to the traditional knowledge and culture exchange, while farther study areas had lower similarities due to the difference in traditions and cultures.
The comparative analysis between the uses of medicinal plants confirms the reported data.
To best of our knowledge, medicinal uses of Polyalthia longifolia (fever), Pistia stratiote (painful urination), Schefflera arboricola (blood circulation), Ceratophyllum demersum (diarrhea), Najas graminea (goiter and boils), Vallisneria spiralis (rheumatism), Lemna minor (antipyretic), Marsilea minuta (diarrhea), Nelumbo nucifera (ring worm), Nymphaea lotus (malarial fever), Saccharum spontaneum (skin eruption), Ranunculus laetus (antirheumatic), Oligomeris linifolia (throat pain and cough), Misopates orontium (tumors), and Trapa bispinosa (body energizer) were documented for the first time. Therefore, new medicinal uses of encountered species with high RIL and CFL value are suggested to be evaluated for in depth screening of bioactive compounds and related pharmacological activities.
Conclusion
On the whole, 129 medicinal species used by the inhabitants of the investigation area to cure various diseases were reported. About nine plant species including Withania somnifera, Solanum surattense, S. nigrum, Azadirachta indica, Ficus benghalensis, Morus nigra, M. alba, Polygonum plebeium, and Tribulus terrestris were highly utilized with maximum UV, RFC, RIL, FL, and CFL values. A significantly positive correlation between UR and FC (r = 0.973 at p = 0.01) reflects strong association between the number of respondents mentioning a particular encountered species and uses reports. The determination value (r2) was 0.95, which indicates that 95% of variation in UR can be described in terms of the FC. Our findings revealed that the local people of the study area have close relation with their surrounding environment and still hold significant information on medicinal plant species. The comparative evaluation with published scientific reports exposed 10% resemblance and 14% dissimilarity to previous reported data; however, majority of the medicinal uses of the encountered plant species have rarely been reported before from this region. As metablomics and biomarker tools are increasingly used in drug discovery to understand the mechanism of disease pathology and improved the therapeutic strategies for upcoming challenges. Consequently, screening for biological active ingredients and in vivo/in vitro evaluation of pharmacological activities in reported medicinal plant species with high CFL and FL could be interesting for future drug discovery. Additionally, conservation measures should be taken to protect the flora of the River Chenab wetland, with special emphasis on medicinal plant species.
Additional files
Coordinates, area, population density and climate of the study sites. Source: Government of the Punjab [88]. (DOCX 17 kb)
Ethnobotanical questionnaire form. (DOCX 17 kb)
Acknowledgements
We are appreciative to local informants for sharing the traditional knowledge.
Funding
We have not received any funding for this study, and thus also requested a full waiver of publication costs from the Editorial office of JEE.
Availability of data and materials
All data have already been included in the manuscript.
Authors’ contributions
MU conducted field work and prepare first draft, MA was involved in field survey and data collection, RWB contributed in final write up, and AMA was involved in data analysis, interpolation, and final write up. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study is based on a field survey rather than human or animal trails. So, ethical approval was not applicable. However, formal prior informed consent was taken from participants regarding data collection and publication. In addition, the ethical guidelines of the International Society of Ethnobiology (http://www.ethnobiology.net/) were strictly followed.
Consent for publication
Not applicable to our study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Muhammad Umair, Email: umair450@yahoo.com.
Muhammad Altaf, Email: altaf_mughal450@yahoo.com.
Rainer W. Bussmann, Email: rbussmann@gmail.com
Arshad Mehmood Abbasi, Email: arshad799@yahoo.com.
References
- 1.Tabuti J, Lye K, Dhillion S. Traditional herbal drugs of Bulamogi, Uganda: plants, use and administration. J Ethnopharmacol. 2003;88:19–44. doi: 10.1016/S0378-8741(03)00161-2. [DOI] [PubMed] [Google Scholar]
- 2.Khan N, Abbasi AM, Dastagir G, Nazir A, Shah GM, Shah MM, Shah MH. Ethnobotanical and antimicrobial study of some selected medicinal plants used in Khyber Pakhtunkhwa (KPK) as a potential source to cure infectious diseases. BMC Complement Altern Med. 2014;14:122. doi: 10.1186/1472-6882-14-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Islam MK, Saha S, Mahmud I, Mohamad K, Awang K, Uddin SJ, Rahman MM, Shilpi JA. An ethnobotanical study of medicinal plants used by tribal and native people of Madhupur forest area, Bangladesh. J Ethnopharmacol. 2014;151:921–930. doi: 10.1016/j.jep.2013.11.056. [DOI] [PubMed] [Google Scholar]
- 4.Balunas MJ, Kinghorn AD. Drug discovery from medicinal plants. Life Sci. 2005;78:431–441. doi: 10.1016/j.lfs.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Schippmann U, Leaman DJ, Cunningham A. Impact of cultivation and gathering of medicinal plants on biodiversity: global trends and issues. Biodiversity and the ecosystem approach in agriculture, forestry and fisheries. World. 2002;422:000. [Google Scholar]
- 6.Govaerts R. How many species of seed plants are there? Taxon. 2001;50:1085–1090. doi: 10.2307/1224723. [DOI] [Google Scholar]
- 7.Shrestha PM, Dhillion SS. Medicinal plant diversity and use in the highlands of Dolakha district, Nepal. J Ethnopharmacol. 2003;86:81–96. doi: 10.1016/S0378-8741(03)00051-5. [DOI] [PubMed] [Google Scholar]
- 8.Shinwari MI, Shinwari M. Ethnobotany of medicinal and aromatic plants in Pakistan-An overview. In: IVth International Congress of Ethnobotany. Istanbul: Yeditepe University. 2006. p. 115–122.
- 9.World Heath Organization (WHO). Traditional Medicine and Alternative Medicines In: Fact Sheet No 271. Geneva: Department of Essential Drugs and Medicines Policy; 2002.
- 10.Shaikh SH, Malik F, James H, Abdul H. Trends in the use of complementary and alternative medicine in Pakistan: a population-based survey. J Altern Complement Med. 2009;15:545–550. doi: 10.1089/acm.2008.0232. [DOI] [PubMed] [Google Scholar]
- 11.Hussain S, Malik F, Khalid N, Qayyum MA, Riaz H. Alternative and Traditional Medicines Systems in Pakistan: History, Regulation, Trends, Usefulness, Challenges, Prospects and Limitations. In A Compendium of Essays on Alternative Therapy. London: InTech. 2012. p. 67.
- 12.Altaf M, Javid A, Khan A, Umair M, Irfan, Ashraf S, Idnan M, Haider M, Ali Z. Assessment of water fowl diversity of river Chenab, Pakistan. J Anim Plant Sci. 2015;25:382–388. [Google Scholar]
- 13.Umair M, Altaf M, Abbasi AM. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district, Punjab-Pakistan. PLoS One. 2017;12:e0177912. doi: 10.1371/journal.pone.0177912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Umair M, Rashid Z, Muhammad N, Khan A. Study of ethnomedicinal plants of head Khanki, Pakistan. J Wildlife Ecol. 2017;1:25–36. [Google Scholar]
- 15.Mahmood A, Mahmood A, Malik RN, Shinwari ZK. Indigenous knowledge of medicinal plants from Gujranwala district, Pakistan. J Ethnopharmacol. 2013;148:714–723. doi: 10.1016/j.jep.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 16.Siddiqi T, Tahir-Kheli S. WASSA. 2004. Water and security in South Asia; p. 234. [Google Scholar]
- 17.Irrigation and Power Department Punjab. Surface water quality monitoring in Punjab, Moghalpura, Lahore: Directorate of Land Reclamation Punjab; 2007.
- 18.Umair M, Ilyas U, Altaf M. Diversity and Ecology of Parthenium weeds ar head khanki, Pakistan. Saarbrücken: Lambert Academic Publishing; 2013.
- 19.Heinrich M, Edwards S, Moerman DE, Leonti M. Ethnopharmacological field studies: a critical assessment of their conceptual basis and methods. J Ethnopharmacol. 2009;124:1–17. doi: 10.1016/j.jep.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 20.Ali SI, Qaiser M, editors. Flora of Pakistan. Pakistan: Department of Botany, University of Karachi; 1993. [Google Scholar]
- 21.Ahmad S. Monograph 9–10. Lahore: Biological Society of Pakistan; 1980. Flora of Punjab; pp. 1–126. [Google Scholar]
- 22.Ali SI, Nasir YJ, editors. Flora of Pakistan. PARC, Islamabad, Department of Botany, University of Karachi and National Herbarium; 1989–1991.
- 23.Stevens PF. Angiosperm Phylogeny Website 2001 onwards. [http://www.mobot.org/MOBOT/research/APweb/]. Accessed 4 July 2017.
- 24.Ahmad M, Sultana S, Fazl-i-Hadi S, Ben Hadda T, Rashid S, Zafar M, Khan MA, Khan MPZ, Yaseen G. An ethnobotanical study of medicinal plants in high mountainous region of Chail valley (district swat-Pakistan) J Ehnobiol Ethnomed. 2014;10:36. doi: 10.1186/1746-4269-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tardío J, Pardo-de-Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of southern Cantabria (northern Spain) 1. Econ Bot. 2008;62:24–39. doi: 10.1007/s12231-007-9004-5. [DOI] [Google Scholar]
- 26.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J Ethnopharmacol. 1986;16:275–287. doi: 10.1016/0378-8741(86)90094-2. [DOI] [PubMed] [Google Scholar]
- 27.Alexiades MN, Sheldon JW. Selected guidelines for ethnobotanical research: a field manual. Boranx: The New York Botanical Garden; 1996. [Google Scholar]
- 28.Ali-Shtayeh MS, Yaniv Z, Mahajna J. Ethnobotanical survey in the Palestinian area: a classification of the healing potential of medicinal plants. J Ethnopharmacol. 2000;73:221–232. doi: 10.1016/S0378-8741(00)00316-0. [DOI] [PubMed] [Google Scholar]
- 29.Oliver SJ. The role of traditional medicine practice in primary health care within aboriginal Australia: a review of the literature. J Ehnobiol Ethnomed. 2013;9:46. doi: 10.1186/1746-4269-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamalebo HM, Malale HNSW, Ndabaga CM, Degreef J, De Kesel A. Uses and importance of wild fungi: traditional knowledge from the Tshopo province in the Democratic Republic of the Congo. J Ehnobiol Ethnomed. 2018;14:13. doi: 10.1186/s13002-017-0203-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kadir MF, Sayeed MSB, Mia M. Ethnopharmacological survey of medicinal plants used by indigenous and tribal people in Rangamati, Bangladesh. J Ethnopharmacol. 2012;144:627–637. doi: 10.1016/j.jep.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 32.Cakilcioglu U, Khatun S, Turkoglu I, Hayta S. Ethnopharmacological survey of medicinal plants in Maden (Elazig-Turkey) J Ethnopharmacol. 2011;137:469–486. doi: 10.1016/j.jep.2011.05.046. [DOI] [PubMed] [Google Scholar]
- 33.Hayta S, Polat R, Selvi S. Traditional uses of medicinal plants in Elazığ (Turkey) J Ethnopharmacol. 2014;155:171–184. doi: 10.1016/j.jep.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 34.Ahmed N, Mahmood A, Tahir S, Bano A, Malik RN, Hassan S, Ashraf A. Ethnomedicinal knowledge and relative importance of indigenous medicinal plants of Cholistan desert, Punjab Province, Pakistan. J Ethnopharmacol. 2014;155:1263–1275. doi: 10.1016/j.jep.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 35.Kadir MF, Sayeed MSB, Setu NI, Mostafa A, Mia M. Ethnopharmacological survey of medicinal plants used by traditional health practitioners in Thanchi, Bandarban Hill tracts, Bangladesh. J Ethnopharmacol. 2014;155:495–508. doi: 10.1016/j.jep.2014.05.043. [DOI] [PubMed] [Google Scholar]
- 36.Arshad M, Ahmad M, Ahmed E, Saboor A, Abbas A, Sadiq S. An ethnobiological study in kala Chitta hills of Pothwar region, Pakistan: multinomial logit specification. J Ehnobiol Ethnomed. 2014;10:13. doi: 10.1016/j.jep.2014.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shinwari MI, Khan MA. Folk use of medicinal herbs of Margalla hills national park, Islamabad. J Ethnopharmacol. 2000;69:45–56. doi: 10.1016/S0378-8741(99)00135-X. [DOI] [PubMed] [Google Scholar]
- 38.EIRI . Handbook of Ayurvedic medicines with formulations: a complete handbook on Ayurvedic and herbal medicines. Delhi: Engineers India Research Institute; 2006. [Google Scholar]
- 39.Uniyal SK, Singh K, Jamwal P, Lal B. Traditional use of medicinal plants among the tribal communities of Chhota Bhangal, Western Himalaya. J Ehnobiol Ethnomed. 2006;2:14. doi: 10.1186/1746-4269-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sexton JP, McIntyre PJ, Angert AL, Rice KJ. Evolution and ecology of species range limits. Annu Rev Ecol Evol Syst. 2009;40 10.1146/annurev.ecolsys.110308.120317.
- 41.Holt RD, Keitt TH. Species’ borders: a unifying theme in ecology. Oikos. 2005;108:3–6. doi: 10.1111/j.0030-1299.2005.13145.x. [DOI] [Google Scholar]
- 42.Passalacqua N, Guarrera P, De Fine G. Contribution to the knowledge of the folk plant medicine in Calabria region (southern Italy) Fitoterapia. 2007;78:52–68. doi: 10.1016/j.fitote.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 43.Amjad MS, Qaseem MF, Ahmad I, Khan SU, Chaudhari SK, Malik NZ, Shaheen H, Khan AM. Descriptive study of plant resources in the context of the ethnomedicinal relevance of indigenous flora: a case study from Toli peer National Park, Azad Jammu and Kashmir, Pakistan. PLoS One. 2017;12:e0171896. doi: 10.1371/journal.pone.0180917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng X-l, F-w X. Ethnobotanical study on medicinal plants around Mt. Yinggeling, Hainan Island, China. J Ethnopharmacol. 2009;124:197–210. doi: 10.1016/j.jep.2009.04.042. [DOI] [PubMed] [Google Scholar]
- 45.Shah GM, Abbasi AM, Khan N, Guo X, Khan MA, Hussain M, Bibi S, Nazir A, Tahir AA. Traditional uses of medicinal plants against malarial disease by the tribal communities of lesser Himalayas–Pakistan. J Ethnopharmacol. 2014;155:450–462. doi: 10.1016/j.jep.2014.05.047. [DOI] [PubMed] [Google Scholar]
- 46.Murad W, Azizullah A, Adnan M, Tariq A, Khan KU, Waheed S, Ahmad A. Ethnobotanical assessment of plant resources of Banda Daud Shah, District Karak, Pakistan. J Ehnobiol Ethnomed. 2013;9:77. doi: 10.1186/1746-4269-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eddouks M, Maghrani M, Lemhadri A, Ouahidi M-L, Jouad H. Ethnopharmacological survey of medicinal plants used for the treatment of diabetes mellitus, hypertension and cardiac diseases in the south-east region of Morocco (Tafilalet) J Ethnopharmacol. 2002;82:97–103. doi: 10.1016/S0378-8741(02)00164-2. [DOI] [PubMed] [Google Scholar]
- 48.Rates SMK. Plants as source of drugs. Toxicon. 2001;39:603–613. doi: 10.1016/S0041-0101(00)00154-9. [DOI] [PubMed] [Google Scholar]
- 49.Ssegawa P, Kasenene JM. Medicinal plant diversity and uses in the Sango bay area, Southern Uganda. J Ethnopharmacol. 2007;113:521–540. doi: 10.1016/j.jep.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 50.Rokaya MB, Münzbergová Z, Timsina B. Ethnobotanical study of medicinal plants from the Humla district of western Nepal. J Ethnopharmacol. 2010;130:485–504. doi: 10.1016/j.jep.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 51.Kayani S, Ahmad M, Zafar M, Sultana S, Khan MPZ, Ashraf MA, Hussain J, Yaseen G. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies–Abbottabad, Northern Pakistan. J Ethnopharmacol. 2014;156:47–60. doi: 10.1016/j.jep.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 52.Cechinel-Filho V. Plant bioactives and drug discovery: principles, practice, and perspectives. vol. 17, Hoboken: Wiley; 2012.
- 53.Abbasi AM, Shah MH, Khan MA. Wild edible vegetables of lesser Himalayas: Ethnobotanical and nutraceutical aspects. Vol.1, Cham: Springer; 2015.
- 54.Yamamoto K, Ogawa Y, Yanagita T, Morito F, Fukushima N, Ozaki I, Mizuta T, Setoguchi Y, Sakai T. Pharmacological effects of Dai-saiko-to on lipid biosynthesis in cultured human hepatocyte HepG2 cells. J Ethnopharmacol. 1995;46:49–54. doi: 10.1016/0378-8741(95)01227-5. [DOI] [PubMed] [Google Scholar]
- 55.Sori T, Bekana M, Adugna G, Kelbessa E. Medicinal plants in the ethnoveterinary practices of Borana pastoralists, southern Ethiopia. Int J Appl Res Vet M. 2004;2:220–225. [Google Scholar]
- 56.Ignacimuthu S, Ayyanar M. Ethnobotanical investigations among tribes in Madurai district of Tamil Nadu (India) J Ehnobiol Ethnomed. 2006;2:25. doi: 10.1186/1746-4269-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li S, Long C, Liu F, Lee S, Guo Q, Li R, Liu Y. Herbs for medicinal baths among the traditional Yao communities of China. J Ethnopharmacol. 2006;108:59–67. doi: 10.1016/j.jep.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 58.Bibi T, Ahmad M, Tareen RB, Tareen NM, Jabeen R, Rehman S-U, Sultana S, Zafar M, Yaseen G. Ethnobotany of medicinal plants in district Mastung of Balochistan province-Pakistan. J Ethnopharmacol. 2014;157:79–89. doi: 10.1016/j.jep.2014.08.042. [DOI] [PubMed] [Google Scholar]
- 59.Abbasi AM, Khan SM, Ahmad M, Khan MA, Quave CL, Pieroni A. Botanical ethnoveterinary therapies in three districts of the Lesser Himalayas of Pakistan. J Ehnobiol Ethnomed. 2013;9:84. doi: 10.1186/1746-4269-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Singh AG, Kumar A, Tewari DD. An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. J Ehnobiol Ethnomed. 2012;8:19. doi: 10.1186/1746-4269-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zahoor M, Yousaf Z, Aqsa T, Haroon M, Saleh N, Aftab A, Javed S, Qadeer M, Ramazan H. An ethnopharmacological evaluation of Navapind and Shahpur Virkanin district Sheikupura, Pakistan for their herbal medicines. J Ehnobiol Ethnomed. 2017;13:27. doi: 10.1186/s13002-017-0151-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ullah S, Khan MR, Shah NA, Shah SA, Majid M, Farooq MA. Ethnomedicinal plant use value in the Lakki Marwat District of Pakistan. J Ethnopharmacol. 2014;158:412–422. doi: 10.1016/j.jep.2014.09.048. [DOI] [PubMed] [Google Scholar]
- 63.Shinwari ZK. Medicinal plants research in Pakistan. J Med Plant Res. 2010;4:161–176. [Google Scholar]
- 64.Malik F, Hussain S, Mirza T, Hameed A, Ahmad S, Riaz H, Shah PA, Usmanghani K. Screening for antimicrobial activity of thirty-three medicinal plants used in the traditional system of medicine in Pakistan. J Med Plant Res. 2011;5:3052–3060. [Google Scholar]
- 65.Ali K, Shuaib M, Ilyas M, Hussain F, Hussain F. Medicinal uses of chemical extracts from Withania somnifera and its antimicrobial activity: a mini-review. PSM Microbiol. 2017;2:20–23. [Google Scholar]
- 66.Kurapati KRV, Atluri VSR, Samikkannu T, Nair MP. Ashwagandha (Withania somnifera) reverses β-amyloid1-42 induced toxicity in human neuronal cells: implications in HIV-associated neurocognitive disorders (HAND) PLoS One. 2013;8:e77624. doi: 10.1371/journal.pone.0077624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abbas K, Niaz U, Hussain T, Saeed MA, Javaid Z, Idrees A, Rasool S. Antimicrobial activity of fruits of Solanum nigrum and Solanum xanthocarpum. Acta Pol Pharm. 2014;71:415–421. [PubMed] [Google Scholar]
- 68.Altaf M, Javid A, Umair M, Iqbal KJ, Rasheed Z, Abbasi AM. Ethnomedicinal and cultural practices of mammals and birds in the vicinity of river Chenab, Punjab-Pakistan. J Ehnobiol Ethnomed. 2017;13:41. doi: 10.1186/s13002-017-0168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Srithi K, Balslev H, Wangpakapattanawong P, Srisanga P, Trisonthi C. Medicinal plant knowledge and its erosion among the Mien (Yao) in northern Thailand. J Ethnopharmacol. 2009;123:335–342. doi: 10.1016/j.jep.2009.02.035. [DOI] [PubMed] [Google Scholar]
- 70.Bano A, Ahmad M, Hadda TB, Saboor A, Sultana S, Zafar M, Khan MPZ, Arshad M, Ashraf MA. Quantitative ethnomedicinal study of plants used in the skardu valley at high altitude of Karakoram-Himalayan range, Pakistan. J Ehnobiol Ethnomed. 2014;10:43. doi: 10.1186/1746-4269-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vijayakumar S, Yabesh JM, Prabhu S, Manikandan R, Muralidharan B. Quantitative ethnomedicinal study of plants used in the Nelliyampathy hills of Kerala, India. J Ethnopharmacol. 2015;161:238–254. doi: 10.1016/j.jep.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 72.Rahman MA, Mossa JS, Al-Said MS, Al-Yahya MA. Medicinal plant diversity in the flora of Saudi Arabia 1: a report on seven plant families. Fitoterapia. 2004;75:149–161. doi: 10.1016/j.fitote.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 73.Chaitanya M, Dhanabal S, Rajan S. Pharmacodynamic and ethnomedicinal uses of weed speices in nilgiris, Tamilnadu state, India: a review. Afr J Agric Res. 2013;8:3505–3527. doi: 10.5897/ajar2013.7042. [DOI] [Google Scholar]
- 74.Luitel DR, Rokaya MB, Timsina B, Münzbergová Z. Medicinal plants used by the Tamang community in the Makawanpur district of Central Nepal. J Ehnobiol Ethnomed. 2014;10:5. doi: 10.1186/1746-4269-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ahmed N, Mahmood A, Ashraf A, Bano A, Tahir SS, Mahmood A. Ethnopharmacological relevance of indigenous medicinal plants from district Bahawalnagar, Punjab, Pakistan. J Ethnopharmacol. 2015;175:109–123. doi: 10.1016/j.jep.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 76.Malik S, Ahmad S, Sadiq A, Alam K, Wariss HM, Ahmad I, Hayat MQ, Anjum S, Mukhtar M. A comparative ethno-botanical study of Cholistan (an arid area) and Pothwar (a semi-arid area) of Pakistan for traditional medicines. J Ethnobiol Ethnomed. 2015;11:31. doi: 10.1186/s13002-015-0018-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rehman MN, Ahmad M, Sultana S, Zafar M, Edwards S. Relative popularity level of medicinal plants in Talagang, Punjab Province, Pakistan. Rev Bras Farmacogn. 2017;27:751–775. doi: 10.1016/j.bjp.2017.09.004. [DOI] [Google Scholar]
- 78.Ahmed N, Mahmood A, Mahmood A, Sadeghi Z, Farman M. Ethnopharmacological importance of medicinal flora from the district of Vehari, Punjab province, Pakistan. J Ethnopharmacol. 2015;168:66–78. doi: 10.1016/j.jep.2015.02.048. [DOI] [PubMed] [Google Scholar]
- 79.Mollik MAH, Hossan MS, Paul AK, Taufiq-Ur-Rahman M, Jahan R, Rahmatullah M. A comparative analysis of medicinal plants used by folk medicinal healers in three districts of Bangladesh and inquiry as to mode of selection of medicinal plants. Ethnobot Res Appl. 2010;8:195–218. doi: 10.17348/era.8.0.195-218. [DOI] [Google Scholar]
- 80.Verma AK, Kumar M, Bussmann RW. Medicinal plants in an urban environment: the medicinal flora of Banares Hindu University, Varanasi, Uttar Pradesh. J Ehnobiol Ethnomed. 2007;3:35. doi: 10.1186/1746-4269-3-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ahmed E, Arshad M, Saboor A, Qureshi R, Mustafa G, Sadiq S, Chaudhari SK. Ethnobotanical appraisal and medicinal use of plants in Patriata, New Murree, evidence from Pakistan. J Ethnobiol Ethnomed. 2013;9:13. doi: 10.1186/1746-4269-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Abbasi AM, Khan MA, Shah MH, Shah MM, Pervez A, Ahmad M. Ethnobotanical appraisal and cultural values of medicinally important wild edible vegetables of Lesser Himalayas-Pakistan. J Ethnobiol Ethnomed. 2013;9:66. doi: 10.1186/1746-4269-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mussarat S, AbdEl-Salam NM, Tariq A, Wazir SM, Ullah R, Adnan M. Use of ethnomedicinal plants by the people living around Indus River. eCAM. 2014;2014:14. doi: 10.1155/2014/212634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rashid N, Gbedomon RC, Ahmad M, Salako VK, Zafar M, Malik K. Traditional knowledge on herbal drinks among indigenous communities in Azad Jammu and Kashmir, Pakistan. J Ethnobiol Ethnomed. 2018;14:16. doi: 10.1186/s13002-018-0217-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shaheen H, Qaseem MF, Amjad MS, Bruschi P. Exploration of ethno-medicinal knowledge among rural communities of Pearl Valley; Rawalakot, District Poonch Azad Jammu and Kashmir. PLoS One. 2017;12:e0183956. doi: 10.1371/journal.pone.0183956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Aziz MA, Adnan M, Khan AH, Shahat AA, Al-Said MS, Ullah R. Traditional uses of medicinal plants practiced by the indigenous communities at Mohmand agency, FATA, Pakistan. J Ethnobiol Ethnomed. 2018;14:2. doi: 10.1186/s13002-017-0204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hussain W, Badshah L, Ullah M, Ali M, Ali A, Hussain F. Quantitative study of medicinal plants used by the communities residing in Koh-e-Safaid Range, northern Pakistani-Afghan borders. J Ethnobiol Ethnomed. 2018;14:30. doi: 10.1186/s13002-018-0229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Government of the Punjab. Punjab development statistics. Lahore: Bureau of Statistics Government of the Punjab; 1999.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coordinates, area, population density and climate of the study sites. Source: Government of the Punjab [88]. (DOCX 17 kb)
Ethnobotanical questionnaire form. (DOCX 17 kb)
Data Availability Statement
All data have already been included in the manuscript.