Abstract
Introduction
Successful immunization programs have diminished parental fear of diseases and increased fear of vaccines. Children with nonmedical exemptions to school immunization requirements are at increased risk of acquiring and transmitting disease. We explored differences in vaccine attitudes, beliefs, and information sources among parents of exempt and vaccinated children.
Methods
Self-administered surveys were mailed to 780 parents of children with nonmedical exemptions (cases) and 1491 parents of fully-vaccinated children (controls).
Results
Vaccines most often refused by exempt children were varicella (49%) and hepatitis B (30%). The most common reason for claiming exemptions was vaccine might cause harm (57%). Parents of vaccinated children were less likely than parents of exempt children to report concern about vaccine safety, question the need for immunization, and oppose immunization requirements. Nearly 25% of parents of vaccinated children reported that children get more immunizations than are good for them and 34% expressed concern that children’s immune systems could be weakened by too many immunizations. Both groups received information from health care professionals; parents of exempt children were more likely to also consult other sources.
Conclusions
Our findings support the need for improved methods to communicate vaccine safety information. Further studies to explore vaccine safety concerns among parents are needed.
INTRODUCTION
The tremendous success of immunizations in controlling vaccine-preventable diseases has unfortunately resulted in diminishing parental fear of these illnesses and an increase in fear of the vaccines themselves.1 Reductions of barriers to receiving vaccinations, coupled with strong support from health care professionals, and laws requiring specific vaccinations for school entrance have contributed to improving and sustaining high rates of vaccine uptake.2–3 Nonetheless, many parents have concerns about vaccine safety.4 Vaccine safety concerns were identified as the primary reason for vaccine refusal during investigation of a recent measles outbreak in Indiana, the largest such outbreak in the United States in a decade.5
While all states require children entering schools to receive vaccines, 48 states allow nonmedical exemptions, and the prevalence of nonmedical exemptions have increased in states that make them easily available to parents.6 In addition, children with a nonmedical exemption have been shown to be at increased risk of acquiring and transmitting measles and pertussis.7–8
The percentages of students with a nonmedical exemption in grades kindergarten through 12 (K-12) have been steadily increasing in Wisconsin, from 0.8% during the 1992–1993 school year to 3.1% during the 2005–2006 school year.6 However, specific reasons for this statewide increase remain unclear. Wisconsin allows immunization exemption for reasons of health, religion, or personal conviction. The objective of this study was to determine differences in vaccine attitudes, beliefs, and information sources among parents of children with nonmedical exemptions to ≥1 vaccines compared with parents of fully-vaccinated children in Wisconsin.
METHODS
Survey Procedures
Using probability proportional to size sampling, to ensure that each child with a nonmedical exemption (exempt child) in the state had an equal probability of being selected, 19 high schools (schools with grade 12) and 61 elementary and middle schools (schools with no grade 12) were randomly selected. Amish and Mennonite schools were excluded from the sample because these communities are relatively isolated and difficult to sample. Wisconsin Division of Public Health (WDPH) staff sent letters to each selected school describing the purpose of the study and requesting the school officials to randomly select up to 15 exempt children and 30 fully-vaccinated children (vaccinated children), matched by grade. Detailed instructions describing how to randomly select children from student rosters were included.
Of the 80 schools contacted by WDPH staff, 66 (83%) agreed to participate in the study (17 of 20 with grade 12 and 49 of 61 with no grade 12). Participating schools provided WDPH with the names and addresses of parents of the randomly selected children. Self-administered surveys were mailed to 780 parents of children with nonmedical exemptions for ≥1 vaccines (cases) and 1491 control parents; several schools could not supply the requested number of controls. The survey packets included a letter from WDPH describing the study, the survey questionnaire, a postage-paid postcard, and a postage-paid return envelope. Questionnaires contained no personal identifiers and were returned to Johns Hopkins University (JHU) to ensure completed questionnaires could not be traced back to respondents. The postcards were returned to WDPH to denote study participation, refusal, or non-response. Two additional copies of the survey materials were mailed to non-responders. The study was approved by the Institutional Review Boards of JHU, WDPH, and the Centers for Disease Control and Prevention.
Survey Content
Parents of exempt children were asked to verify that their child had not received at least 1 of the vaccines required for school entry. The survey also asked whether the child received the complete or less than complete number of doses for each vaccine series. When parents with an exemption on file with the school reported that their children had received all of the required vaccines, the survey asked why the school had an exemption on file for their child. The survey also asked parents for the reasons that led to their decision not to vaccinate their child.
The survey was based on the Health Belief Model.9 All respondents were asked to use a 5-point Likert scale to estimate: the probability that an unimmunized Wisconsin child would contract during a 10-year period each of the 12 diseases against which vaccines were recommended for elementary school children (“impossible” to “very likely”); how serious it would be for an 8-year-old child to develop 1 of these diseases (“not at all serious” to “very serious”); how effective the vaccines are in preventing children from getting these childhood diseases (“not at all protective” to “very protective”); and how safe the vaccine is (“dangerous” to “very safe”). Respondents were also asked to use a 5-point Likert scale (“strongly disagree” to “strongly agree”) to indicate the extent of their agreement/dis-agreement pertaining to 14 questions regarding “key immunization beliefs”; who benefits from vaccination (child, community, doctors, government, and companies that make vaccines) and to what extent (“not at all” to “a great deal”); 4 questions that measured “trust in health care professionals;”2–3 5 questions that measured “trust in government”; and questions regarding where they received information about vaccines, the quality of sources for vaccine information (“extremely poor source” to “excellent source”), and the type of practitioner they consider to be the child’s primary health care professional.
Respondents were asked to indicate the grade of their child, their own age (10 age categories), highest education (7 grade-completed categories), household income (starting with < $20,000 and increasing by $10,000 intervals to > $70,000), and race or ethnic group. Surveys took 15–20 minutes to complete.
Data Analysis
Data for age, education, and income was dichotomized as ≤ the median versus > the median; race was either “white” or “all other.”
General constructs were created for respondents’ assessments of disease susceptibility and severity, and vaccine efficacy and safety using the respondent’s mean scores for all antigens/diseases; a general construct for trust in health care professionals by establishing a mean for responses to the 4 questions; and a general construct score for trust in the government by establishing a mean for the responses to the 5 questions. We used Cronbach’s alpha statistic to measure internal consistency of scales for trust in health care professionals and trust in government. Construct scores were dichotomized by <4 versus ≥4 (corresponding to higher levels of trust). We used logistic regression models to compare differences in independent variables between cases and controls. The final model for assessing the constructs in the Health Belief Model included disease susceptibility, disease severity, vaccine efficacy, and vaccine safety.
Answers to key belief questions were dichotomized into “strongly agree or agree” versus all other responses; perception of benefit from vaccination into “a moderate amount or a great deal of benefit” versus all other responses; each source for vaccine information into “a good or excellent source” versus all lower levels. Logistic regression models were used to compare differences in these independent variables between cases and controls.
ZIP codes of responders and non-responders were linked to demographic characteristics of the community through US Census Bureau data, including education (percent with high school education or more), race (percent minority), age (proportion of population < 18 years), income (median household and proportion below poverty), and population density (proportion urban). Census data from ZIP codes of respondents and non-respondents was compared using the Wilcoxon rank sum test.
RESULTS
Surveys were completed by 236 parents of exempt children (response rate=30.3%) and 727 parents of vaccinated children (response rate=48.8%), for a total response rate of 42.4%. Among respondents, the median age range was 41–45 years, the median education was some college, and the median household income was $60,000–69,999. The majority (92.2%) of respondents were white. Demographic features of the respondents did not vary between cases and controls. Responders and non-responders did not differ in their community measures of race, age, income, and population density, but did differ significantly (however only modestly) in the community measure of proportion of the population with a high school education or more (84.3% versus 85.8%, P<0.01).
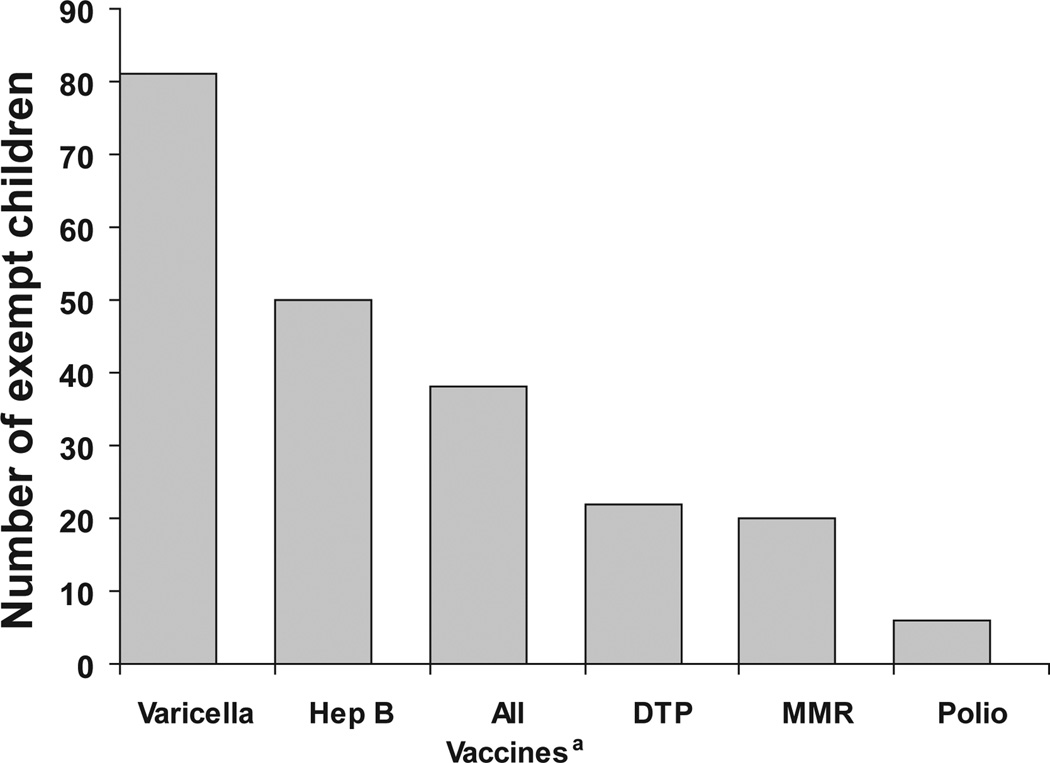
The 2 vaccines most often not received by exempt children were varicella vaccine (49%) and hepatitis B vaccine (30%) (Figure 1); 38 (16%) exempt children received no vaccines. Thirty percent of parents of exempt children (70) reported their children had received all recommended vaccines and provided the following reasons for why the school might have an exemption on file: vaccine record lost (11); vaccine received before date required by law (7); other including vaccinated in other country, vaccinated elsewhere, up-to-date, and varicella history (8); and don’t know (31).
Figure 1.
Vaccines included in the Wisconsin School Immunization law that were not received by children (n=166) with nonmedical exemptions.
a The term “all vaccines” means the child received no vaccines. Parents of an additional 70 children with nonmedical exemptions reported their children had received all recommended vaccines.
The most common reason reported for parents claiming nonmedical exemptions for their child was the vaccine might cause harm (57%). Additional reasons reported by 20% or more of the parental respondents include the following: it was better to get natural disease than a vaccine, the child was not at risk for the disease(s), risk of autism, safety concerns regarding thimerosal, vaccines might overload the immune system, and that the disease(s) were not dangerous (Table 1).
Table 1.
The Frequency of Reported Reasons Provided by Parents for Claiming Nonmedical Exemptions for Their Children (n=166)
| Reason for Not Vaccinatinga | Frequency | % |
|---|---|---|
| Vaccine might cause harm | 95 | 57 |
| Better to get natural disease than a vaccine | 63 | 38 |
| My child not at risk for the disease(s) | 61 | 37 |
| Autism | 51 | 31 |
| Thimerosal | 49 | 30 |
| Vaccines might overload immune system | 48 | 29 |
| Disease(s) not dangerous | 34 | 20 |
| Vaccine might not work | 27 | 16 |
| Ethical or moral issues | 22 | 13 |
| Fetal tissue | 16 | 10 |
| To get my child enrolled in school without delay or hassle | 16 | 10 |
| Distrust of government | 16 | 10 |
| Contrary to religious beliefs | 2 | 1 |
| Encouraged by school official | 1 | <1 |
Note: Seventy parents who reported their children were fully vaccinated not included.
Not mutually exclusive
Parents of vaccinated children were more likely than parents of exempt children to report a moderate amount or great deal of individual benefit from vaccination (93% versus 61%, Odds Ratio [OR]=9.09; 95% Confidence Interval [CI]=6.25–14.29) and community benefit from vaccination (88% versus 57%; OR=5.26; CI=3.85–7.69). Parents of vaccinated children were less likely than parents of exempt children to report a moderate amount or great deal of benefit for vaccine companies when a child is fully vaccinated (74% versus 82%; OR=0.63; CI=0.43–0.91). The trust in health care professional construct showed high internal consistency (Cronbach’s Alpha=0.89) with parents of vaccinated children being more likely to report high trust in health care professionals than parents of exempt children (87% versus 68%; OR=3.13; CI=2.22–4.35). The trust in government construct had a Cronbach’s Alpha=0.92, with parents of vaccinated children being more likely to have high trust in government compared to parents of exempt children (35% versus 24%; OR=1.67; CI=1.19–2.33).
Among the key immunization beliefs (Table 2), parents of vaccinated children were less likely than parents of exempt children to report concern about vaccine safety, question the need for immunization, and oppose immunization requirements. However, nearly 25% of parents of vaccinated children reported that children get more immunizations than are good for them, and 34% expressed concern that children’s immune systems could be weakened by too many immunizations. In addition, parents of vaccinated children were more likely than parents of exempt children to report high disease susceptibility, greater disease severity, that vaccines were very safe, and vaccines were very effective. These differences remained statistically significant in multivariate analysis (Table 3).
Table 2.
The Frequency of Parents Agreeing with Vaccine Related Beliefs by Child’s Vaccination Status, and Odds Ratios of Child Being Fully Vaccinated
| Agree or Strongly Agree (%) | ||||
|---|---|---|---|---|
| Statement | Exempt n=236a |
Vaccinated n=727 |
Odds Ratio |
95% Confidence Interval |
| Children should only be immunized against serious diseases | 66.3 | 59.2 | 0.74 | 0.53–1.03 |
| Children get more immunizations than are good for them | 62.7 | 23.4 | 0.18b | 0.13–0.26 |
| I am concerned that children’s immune system could be weakened by too many immunizations | 64.9 | 33.7 | 0.27b | 0.19–0.39 |
| I am more likely to trust immunizations that have been around a while compared with new vaccines | 71.5 | 82.8 | 1.92b | 1.33–2.78 |
| Immunizations are one of the safest forms of medicine ever developed | 42.0 | 73.6 | 3.85b | 2.63–5.56 |
| Immunizations are getting better and safer all of the time, as a result of medical research | 61.1 | 94.4 | 11.11b | 6.25–20.00 |
| Vaccines strengthen the immune system | 43.9 | 84.2 | 6.67b | 4.35–11.11 |
| It is better for a child to develop immunity by getting sick than to get a vaccine | 43.8 | 14.5 | 0.22b | 0.14–0.33 |
| Healthy children need immunizations | 82.5 | 98.8 | 16.67b | 8.33–33.33 |
| Immunizations do more harm than good | 26.3 | 2.3 | 0.07b | 0.03–0.12 |
| I am opposed to immunization requirements because they go against freedom of choice | 29.3 | 6.3 | 0.16b | 0.11–0.25 |
| I am opposed to immunization requirements because parents know what is best for their children | 19.0 | 4.9 | 0.22b | 0.13–0.36 |
| Immunization requirements protect children from getting diseases from unimmunized children | 68.9 | 92.2 | 5.26b | 3.45–8.33 |
| Parents should be allowed to send their children to school even if not vaccinated | 73.6 | 34.2 | 0.19b | 0.13–0.27 |
Includes parents with an exemption on file with the school who did and did not confirm that child had not received all vaccine required for school entry.
Odds Ratio P<0.05.
Table 3.
Proportion and Odds Ratio of Parents with High Levels of Perception of Vaccine Preventable Disease Susceptibility and Severity and Vaccine Efficacy and Safety by Child’s Vaccination Status
| Percent in High Categorya | Unadjusted | Adjustedb | ||||
|---|---|---|---|---|---|---|
| Construct | Exempt N=236 |
Vaccinated N=727 |
Odds Ratio |
95% Confidence Interval |
Odds Ratio |
95% Confidence Interval |
| Disease Susceptibilityc | 14.4 | 28.0 | 2.33d | 1.54–3.45 | 1.89d | 1.22–2.94 |
| Disease Severitye | 28.3 | 40.8 | 1.75d | 1.27–2.44 | 1.27 | 0.88–1.82 |
| Vaccine Efficacyf | 41.2 | 64.7 | 2.63d | 1.92–3.57 | 2.17d | 1.54–3.03 |
| Vaccine Safetyg | 21.5 | 37.7 | 2.22d | 1.54–3.13 | 1.49d | 1.01–2.22 |
High category defined as >4.0 on 1–5 scale.
Adjusted for all other construct variables.
How likely an unimmunized child in Wisconsin is to acquire vaccine-preventable diseases on 5 point Likert scale (very unlikely to very likely)—mean of 12 diseases.
Odds Ratio P<0.05.
How serious it would be if an 8-year-old child acquired vaccine-preventable diseases on 5 point Likert scale (not at all serious to very serious)—mean of 12 diseases.
How protective vaccines are on 5 point Likert scale (not protective at all to very protective)—mean for 6 vaccines.
How safe children’s vaccines are on 5 point Likert scale (very unsafe to very safe)—mean for 6 vaccines.
The vast majority of parents of vaccinated and exempt children reported receiving vaccine information from their health care professionals and that these professionals were good or excellent sources of vaccine information (Table 4). Parents of vaccinated children were significantly less likely to report receiving vaccine information from 11 of the 17 information sources including 5 of the internet Web sites. Besides the Wisconsin Immunization Program, there were no information sources parents of vaccinated children were more likely to use than parents of exempt children. However, parents of vaccinated children were more likely than parents of exempt children to consider 9 of the 11 listed medical or public health sources to be good or excellent for vaccine information (Table 4).
Table 4.
Parent(s) Use and the Credibility of 17 Sources of Vaccine Information by Vaccination Status of Child and Odds Ratios of Child Being Fully Vaccinated
| Used in Past | Rated Good or Excellent | |||||
|---|---|---|---|---|---|---|
| Source | Exempt n=236 |
Vaccinated n=727 |
Odds Ratio (95% Confidence Interval) |
Exempt n=236 |
Vaccinated n=727 |
Odds Ratio (95% Confidence Interval) |
| Health Care Professionals | 91.1 | 91.5 | 1.05 (0.63–1.75) | 81.3 | 98.1 | 12.50 (6.25–25.00) |
| Vaccine Information Statement | 71.6 | 67.5 | 0.83 (0.60–1.14) | 77.5 | 96.7 | 8.33 (5.00–14.29) |
| School Nurse or Health Officials’ advice | 49.6 | 50.6 | 1.04 (0.78–1.39) | 73.7 | 96.0 | 8.33 (5.00–14.29) |
| Local/state health dept | 44.9 | 40.0 | 0.82 (0.61–1.10) | 78.9 | 97.8 | 8.33 (4.55–14.29) |
| Media | 43.2 | 26.5 | 0.42 (0.35–0.65) | 42.0 | 56.3 | 1.79 (1.20–2.63) |
| Parents/friends | 40.3 | 29.7 | 0.63 (0.46–0.85) | 58.2 | 54.1 | 0.85 (0.58–1.23) |
| Professional (medical) orgs | 26.7 | 17.2 | 0.57 (0.40–0.81) | 81.6 | 97.2 | 7.69 (4.00–14.29) |
| Alternative HCP | 19.9 | 3.7 | 0.16 (0.09–0.26) | 62.0 | 57.4 | 0.83 (0.53–1.30) |
| Vaccine companies | 12.7 | 2.9 | 0.20 (0.11–0.36) | 44.2 | 71.1 | 3.13 (2.13–4.55) |
| Pharmacists | 8.1 | 6.7 | 0.83 (0.48–1.43) | 74.5 | 92.0 | 3.85 (2.44–6.25) |
| Religious leaders/orgs | 3.4 | 0.8 | 0.24 (0.08–0.69) | 18.5 | 18.5 | 1.00 (0.57–1.75) |
| Internet Web sites such as: | ||||||
| CDC | 14.0 | 7.0 | 0.47 (0.29–0.74) | 80.8 | 96.7 | 7.14 (3.45–14.29) |
| NVIC | 7.6 | 2.8 | 0.34 (0.18–0.66) | 77.9 | 94.9 | 5.26 (2.56–11.11) |
| Dissatisfied Parents Together | 4.2 | 0.3 | 0.06 (0.01–0.29) | 42.0 | 28.3 | 0.55 (0.28–1.05) |
| FDA | 3.8 | 1.5 | 0.39 (0.16–0.94) | 69.2 | 87.5 | 3.13 (1.79–5.26) |
| Wisconsin Immunization Program | 3.0 | 3.3 | 1.11 (0.47–2.63) | 75.3 | 95.0 | 6.25 (3.13–12.5) |
| Immunization Action Coalition | 2.1 | 0.1 | 0.06 (0.01–0.55) | 65.1 | 69.1 | 1.20 (0.58–2.44) |
Abbreviations: NVIC, National Vaccine Information Center; CDC, Centers for Disease Control and Prevention; NIP, National Immunization Project; FDA, (US) Food and Drug Administration.
Odds Ratios in Bold=P<0.05.
The majority of parents of vaccinated (92%) and exempt (84%) children reported their child’s primary health care professional to be a doctor or physician, although parents of vaccinated children were more likely to rely on doctors or physicians for primary care (OR=2.38; CI=1.54–3.70). Among parents of exempt children, 11 (5%) relied on chiropractors and 11 (5%) on naturopathic doctors as their primary health care professionals; no vaccinated children relied on these types of professionals as their primary health care professional.
DISCUSSION
In Wisconsin, parents of fully vaccinated children perceived susceptibility to and severity of vaccine preventable diseases and the safety and efficacy of vaccines to be greater compared with parents of exempt children. Nonetheless, 25%–34% of parents of vaccinated children had vaccine safety concerns that are not supported by available data. Parents of both vaccinated and exempt children most frequently received vaccine information from health care professionals. However, parents of exempt children were more likely to consult with other sources for vaccine information. In addition, parents of vaccinated children were more likely than parents of exempt children to consider medical and public health sources as good or excellent for vaccine information.
These findings are concordant with those in a similar 4-state study conducted in Massachusetts, Missouri, Colorado, and Washington10 demonstrating a reasonable level of consistency between parents of vaccinated versus exempt children in different geographical areas. The 4-state study found that 22% of parents with children having an exemption on file in the school reported that their children were fully vaccinated, but it did not explore the reasons why schools had exemptions on file despite parents reporting their children were fully vaccinated. This study found that 30% of parents of exempt children reported that their children were fully vaccinated despite the school having an exemption on file and investigated why this may have occurred. Less than half of these parents believed their children were immune, and the reasons provided for waivers remaining on file were diverse.
This finding is important for at least 2 reasons. First, state level estimates of exemptions may overestimate the number of children who are actually susceptible to vaccine preventable diseases. Second, studies that have examined the relative risk of measles and pertussis for exempt compared to vaccinated children (exempt incidence divided by vaccinated incidence) included all children with exemptions in school records in the denominator for exempt incidence.7–8 Coupled with the finding that about 50% of parents of children with exemptions report their children were vaccinated with measles- and pertussis-containing vaccines, these studies may have considerably underestimated the risks of measles and pertussis for exempt children. The number of children with exemptions in the denominator of the disease incidence among exempt children was more than 2 times higher than it should have been.
It is important to understand the reasons why some parents are claiming nonmedical exemptions to school immunization requirements, given the increase in these exemptions in Wisconsin and other states that readily or easily grant exemptions.6 The dramatic increase in nonmedical exemptions for philosophical reasons in Wisconsin is in sharp contrast to religious and medical waivers, which have remained relatively constant among school attendees in Wisconsin during the past 13 years (0.1% and 0.2–0.3%, respectively).11 The effect of the decreased vaccine coverage has resulted in an increase of individual susceptibility and a decrease of herd immunity among Wisconsin children, leaving this population more susceptible to vaccine-preventable disease outbreaks. The role of nonmedical exemptions may be especially important for pertussis, which remains endemic in the United States and has been increasing in incidence during the past decade.12–15 An increase in the number of people unprotected against pertussis may lead to unvaccinated individuals acquiring pertussis and transmitting it to others, as happened in a recent large community-wide outbreak in eastern Wisconsin.16 Children with nonmedical exemptions have been central to ongoing measles outbreaks in several states.17
Limitations of our study include the potential for non-response bias. Analysis of potential non-response bias suggests that, measured at the community level, responders were very similar to non-responders when considering demographic factors. However, data on individual level differences between responders and non-responders were not available. Response rates differed significantly between parents of exempt and vaccinated children. However, spatial clustering analysis indicated that non-participation did not cluster differently by vaccination status (data available on request). Exclusion of Amish and Mennonite schools would not impact internal validity but would limit the findings of the study to schools that are not primarily Amish or Mennonite. The consistency in findings in our study with those in the aforementioned 4-state study of parents of exempt and vaccinated children10 enhances the generalizability of our findings to other populations. Parental vaccine attitudes of exempt parents who reported their children were fully vaccinated tended to be somewhere in between parents who confirmed that their children were not fully vaccinated and parents of fully-vaccinated children (data available on request). To be conservative, these parents were included in the exempt category as this had the potential to bias our results towards the null. Thus the differences in parental attitudes and beliefs between the true exemptors and the fully vaccinated may be larger than what was reported.
These findings support the need for improved methods to communicate scientifically validated vaccine safety information to the public and to educate parents regarding the risks that vaccine-preventable diseases pose to their children. Further studies to explore vaccine safety concerns among parents are needed. This includes examining and applying options such as how to improve parental understanding of the vaccine safety system and of the available evidence demonstrating the safety of vaccines. Novel approaches should also be explored. Working with alternative health care professionals such as chiropractors and naturopaths might be helpful given the increased likelihood that parents of exempt children rely on these types of health care professionals for pediatric primary health care compared with parents of vaccinated children. Additionally, there may be value in having vaccine safety studies conducted by independent investigators who are not funded by pharmaceutical companies and having improved vaccine risk communication from information sources that are considered credible by parents. School requirements are being updated in many states to reflect new Advisory Committee on Immunization Practices recommendations (ie, second dose varicella and tetanus, diphtheria and pertussis [Tdap]) and there is always the possibility of new requirements. With each new requirement, there is a risk of an increase in exemptions and it is important to understand how best to communicate with parents the importance of these vaccines so that their children are protected from serious diseases.
Acknowledgments
Funding/Support: This research was funded by grant UIP000032A from the Centers for Disease Control and Prevention (CDC).
Footnotes
Financial Disclosures: Jeffrey P. Davis, MD, is a consultant to Glaxo Smith Kline. Neal A. Halsey, MD, has been a consultant for the Data Safety Monitoring Boards for Merck, Novartis, and Medimmune and has also received grants for vaccine studies in Guatemala from Wyeth and sanofi pasteur
REFERENCES
- 1.Chen RT, Hibbs B. Vaccine safety: current and future challenges. Pediatr Ann. 1998;27:445–455. doi: 10.3928/0090-4481-19980701-11. [DOI] [PubMed] [Google Scholar]
- 2.Orenstein WA, Douglas RG, Rodewald LE, Hinman AR. Immunizations in the United States: success, structure, and stress. Health Aff (Millwood) 2005;24:599–610. doi: 10.1377/hlthaff.24.3.599. [DOI] [PubMed] [Google Scholar]
- 3.Orenstein WA, Hinman AR. The immunization system in the United States—the role of school immunization laws. Vaccine. 1999;17(S3):S19–S24. doi: 10.1016/s0264-410x(99)00290-x. [DOI] [PubMed] [Google Scholar]
- 4.Gellin BG, Maiback EW, Marcuse EK. Do parents understand immunization? a national telephone survey. Pediatrics. 2000;106:1097–1102. doi: 10.1542/peds.106.5.1097. [DOI] [PubMed] [Google Scholar]
- 5.Parker AA, Staggs W, Dayan GH, et al. Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States. N Engl J Med. 2006;355:447–455. doi: 10.1056/NEJMoa060775. [DOI] [PubMed] [Google Scholar]
- 6.Omer SB, Pan WK, Halsey NA, et al. Nonmedical exemptions to school immunization requirements: secular trends and association of state policies with pertussis incidence. JAMA. 2006;296:1757–1763. doi: 10.1001/jama.296.14.1757. [DOI] [PubMed] [Google Scholar]
- 7.Salmon DA, Haber M, Gangarosa EJ, Phillips L, Smith N, Chen RT. Health consequences of religious and philosophical exemptions from immunization laws: individual and societal risks of measles. JAMA. 1999;282:47–53. doi: 10.1001/jama.282.1.47. [DOI] [PubMed] [Google Scholar]
- 8.Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE. Individual and community risks of measles and pertussis associated with personal exemptions to immunizations. JAMA. 2000;284:3145–3150. doi: 10.1001/jama.284.24.3145. [DOI] [PubMed] [Google Scholar]
- 9.Becker M. The health belief model and personal health behavior. Health Education Monogr. 1974;2:324–501. [Google Scholar]
- 10.Salmon DA, Moulton LH, Omer SB, DeHart P, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines: a case-control study. Arch Pediatr Adolesc Med. 2005;159:470–476. doi: 10.1001/archpedi.159.5.470. [DOI] [PubMed] [Google Scholar]
- 11.National Center for Immunization and Respiratory Diseases. Grantee Immunization Information. [Accessed January 2, 2009]; http://www2a.cdc.gov/nip/irar/grantee/granteeinfo.asp#grptg.
- 12.Cherry JD. The epidemiology of pertussis and pertussis immunization in the United Kingdom and the United States: a comparative study. Curr Probl Pediatr. 1984;14:1–78. doi: 10.1016/0045-9380(84)90016-1. [DOI] [PubMed] [Google Scholar]
- 13.Hopkins RS, Jajosky RA, Hall PA, et al. Summary of notifiable diseases—United States, 2003. MMWR Morbidity Mortal Weekly Report. 2005;52:1–85. [PubMed] [Google Scholar]
- 14.Plotkin SL, Plotkin SA. A Short History of Vaccination. In: Plotkin SA, Orenstein WA, editors. Vaccines. 4th ed. Philadelphia, Pa: Saunders; 2004. pp. 1–15. [Google Scholar]
- 15.Broder KR, Cortese MM, Iskander JK, et al. Preventing tetanus, diphtheria, and pertussis among adolescents: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccines recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recommendations and Reports. 2006;55:1–34. [PubMed] [Google Scholar]
- 16.Sotir MJ, Cappozzo DL, Warshauer DM, et al. A county-wide outbreak of pertussis: initial transmission in a high school weight room with subsequent substantial impact on adolescents and adults. Arch Pediatr Adol Med. 2008;162:79–85. doi: 10.1001/archpediatrics.2007.7. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Measles–United States January 1-April 25, 2008. MMWR Morbidity Mortal Weekly Report. 2008;57:494–498. [PubMed] [Google Scholar]