Overview
Introduction
We describe the surgical treatment of tears to the abductor tendons of the hip, which are typically progressive and can lead to recalcitrant pain and progressive weakness, leading to considerable difficulties with walking.
Step 1: Perform the Exposure and Identify the Tear
Place the patient in the lateral decubitus position, expose the lateral peritrochanteric space, and then identify the extent of the tear.
Step 2: Mobilize the Tendon(s)
Mobilize the typically scarred-in tendons from the surrounding tissue to allow the tendon to be brought back down to the trochanter.
Step 3: Prepare the Tendon and Greater Trochanter
Debride the tendon, and lightly burr the greater trochanter to maximize the healing of the tendon to the bone.
Step 4: Locate the Insertional Site of the Tendons and Place the Suture Anchors or Drill Holes Into This Site
Identify the area of the footprint for each of the tendons; all suture anchors should be placed in the footprint, and the transosseous drill holes should straddle the near and far edges of the footprint.
Step 5: Reattach the Tendons
After all of the sutures are placed, tie them down, starting with the pull sutures first, to bring the tendon back to bone; then secure the tendon down with the simple sutures.
Step 6: Reinforce Larger Tears
Reinforce larger tears to protect them and aid in their healing.
Step 7: Postoperative Protocol
The postoperative protocol period consists of partial weight-bearing for specific periods of time, followed by vigorous physical therapy for strengthening and gait retraining.
Results
Surgical repair can improve function and reliably decreases pain in patients with a hip abductor tear.
Introduction
We describe the surgical treatment of tears to the abductor tendons of the hip, which are typically progressive and can lead to recalcitrant pain and progressive weakness, leading to considerable difficulties with walking.
Awareness of tears of the gluteus medius and minimus of the hip has been increasingly recognized as a cause of lateral hip pain and substantial disability1-12. This awareness has been aided by improvement in the imaging of the peritrochanteric space with magnetic resonance imaging (MRI)13-16. The prevalence of such tears in patients with a hip fracture or total hip replacement has been shown to range from 20% to 25%5,11,17. Surgical management has been recommended and has been resulted in consistent pain relief and functional improvement18-20.
The surgical treatment is similar to that of repair of the rotator cuff tear of the shoulder. The extent of the tear must first be evaluated on the basis of both preoperative MRI and intraoperative findings. We will present our classification that both directs our technique and allows us to counsel our patients.
The retracted tendons are mobilized to allow for placement back to their insertion site on the greater trochanter. The trochanteric bed is prepared by removing any extraneous soft tissue and is lightly burred to obtain some bleeding to aid in healing of the tendon to the bone.
With the tendon mobilized and the bed prepared, the tendon must be securely attached to the bone. This can be accomplished with suture anchors for smaller tears with minimal retraction. However, for larger tears, we prefer transosseous fixation through paired tunnels to allow for the usage of both pull and simple sutures. This combination allows us to bring the tendon back down to the bone with the pull sutures and then further secure it with the simple sutures. A number of adjuvants may be added on the basis of the complexity of the tear and the quality of the tissue to reinforce the repair and maximize it chance of healing.
The procedure is performed with the following steps.
Step 1: Perform the Exposure and Identify the Tear
Place the patient in the lateral decubitus position, expose the lateral peritrochanteric space, and then identify the extent of the tear (Video 1).
Make a standard lateral or posterior approach to the hip. Place the leg on a padded Mayo stand, which helps control adduction/abduction. Incise the iliotibial band, and split the gluteus maximus muscle in line with its fibers.
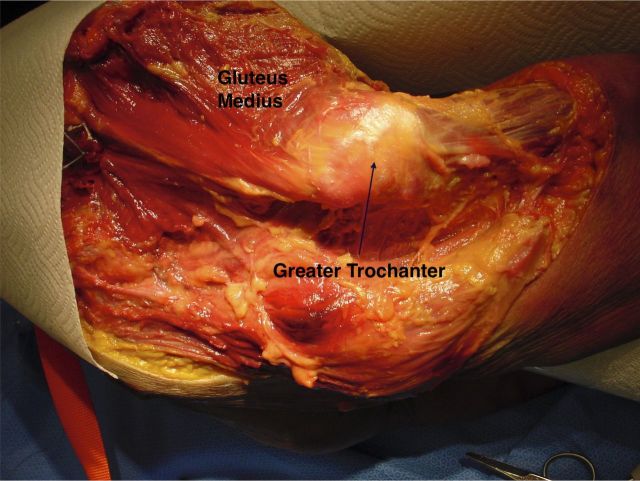
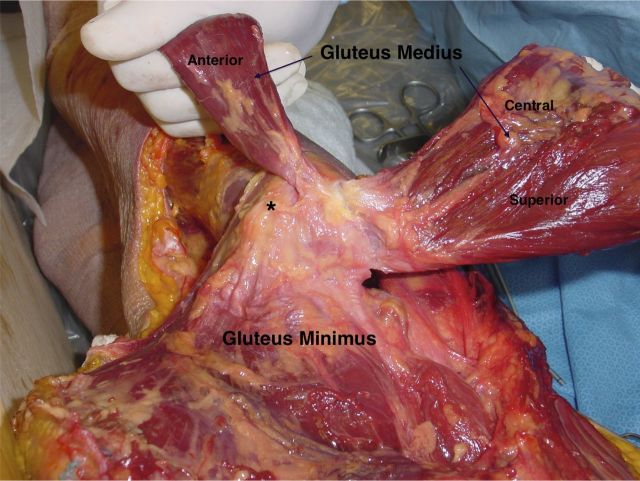
Remove the trochanteric bursae when present in patients with smaller tears to uncover the gluteal tendons. The gluteus medius is fan-shaped, originating from the aponeurosis and the ilium between the inferior and posterior gluteal lines, inserting on the lateral surface of the greater trochanter (Fig. 1). The gluteus minimus, which is deep to the gluteus medius, originates from the ilium between the inferior and anterior gluteal lines. It inserts onto both the anterior aspect of the capsule and via its long head onto the anterior surface of the greater trochanter (Fig. 2).
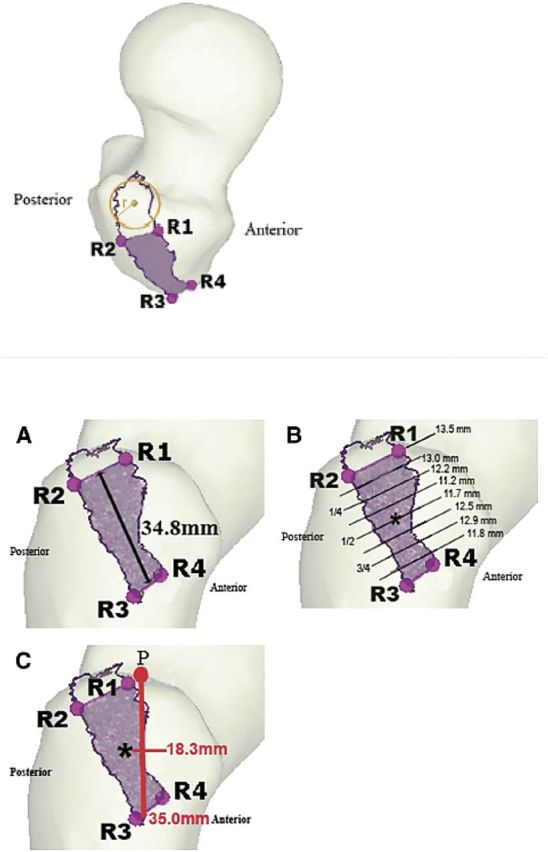
Identify and grade the tear on basis of its size (see Milwaukee classification, Fig. 3). The specific surgical technique is based on its relative size.
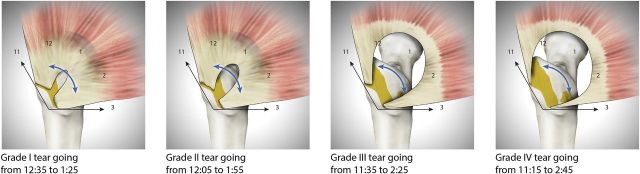
The tears typically start in the central fibers of the gluteus medius and then progress inferiorly and posteriorly from that spot (Fig. 4).
Attempt to identify and separate the long head of the gluteus minimus from the overlying gluteus medius to allow for its separate repair.
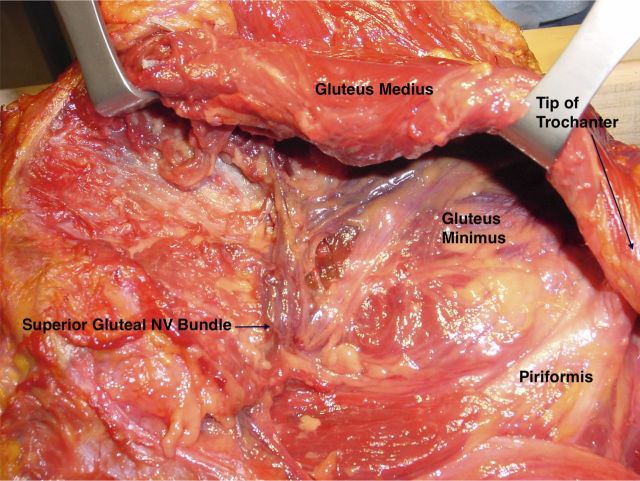
Fig. 1.
A cadaveric dissection demonstrating the anatomy of the gluteus medius.
Fig. 2.
A cadaveric dissection demonstrating the anatomy of the gluteus minimus, as viewed looking caudally from a cephalad position. The gluteus minimus originates from the ilium between the inferior and anterior gluteal lines. It inserts onto both the anterior part of the capsule and via the long head onto its discrete facet (*) onto the anterior surface of the greater trochanter.
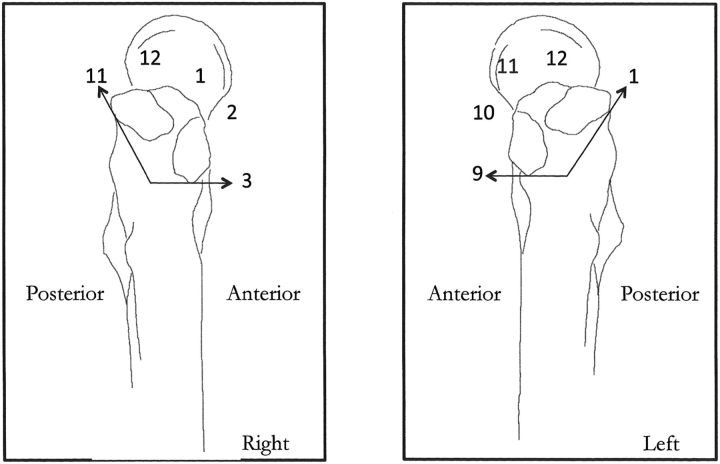
Fig. 3.
The classification system for tears of the hip abductors for the right and left hips. It is based on the hours of the clock. In a right hip, the gluteus medius inserts between the 11 o’clock and 3 o’clock positions; in a left hip, it inserts between 9 o’clock and 1 o’clock. Each grade of the tear is equal to one hour of the clock. A Grade-I tear involves one hour; Grade II, two hours, and so on.
Fig. 4.
A drawing demonstrating the appearances of the various grades of tears in a right hip, showing their progression. Tears typically begin in the central fibers of the gluteus medius at about 1 o’clock (right hip) and then extend inferiorly and posteriorly, increasing the grade as the tear progresses (blue arrows).
Video 1.
Identification of the tear.
Step 2: Mobilize the Tendon(s)
Mobilize the typically scarred-in tendons from the surrounding tissue to allow the tendon to be brought back down to the trochanter (Video 2).
When the gluteus medius is retracted, mobilize it from the overlying gluteus maximus and tensor muscles above and the gluteus minimus below by blunt dissection.
Mobilize the gluteus minimus from the overlying gluteus medius and from the ilium and capsule below. Take care when elevating the gluteus minimus off of the ilium as you can encounter bleeding from the multiple perforating vessels. Mobilization in primary repairs rarely requires extensive dissection either proximally or anteriorly as it is only the tendon that becomes adherent to the adjacent structures. In revisions, which require a more extensive dissection, widespread muscle-muscle scarring can occur. The long head of the gluteus minimus, which inserts into its own facet on the anterior aspect of the trochanter, is the most robust and important portion of this tendon to repair.
The superior gluteal neurovascular bundle must be identified and protected with cephalad dissection >3 cm superior to the greater trochanter (Fig. 5).
With anterior dissection, you may encounter bleeding from the ascending lateral femoral circumflex vessels.
Be aware of the terminal branches of the superior gluteal neurovascular bundle that supply the tensor fasciae latae muscle that lies between it and the gluteus medius muscle. Fortunately, it is usually well medial and superior to the dissection.
Fig. 5.
A cadaveric dissection demonstrating the anatomy of the superior gluteal neurovascular (NV) bundle.
Video 2.
Mobilizing the tendons.
Step 3: Prepare the Tendon and Greater Trochanter
Debride the tendon, and lightly burr the greater trochanter to maximize the healing of the tendon to the bone (Video 3).
Debride the frayed, fibrillated, and poorly vascularized tissues from the ends of the tendons. However, make every attempt to preserve the bulk of the tendon as it is relatively short and the anterior and central fibers of the gluteus medius are rather thin.
Release the torn portions of the tendon that are still attached to the bone. This assists in mobilization of the tendon and allows for an adequate osseous surface for placement of either the suture anchors or the transosseous drill holes.
After removing any extraneous tissue, lightly burr the lateral cortical surface of the greater trochanter to elicit subchondral bleeding to aid in healing. Minimize the burring to avoid decorticating the very thin cortex overlying the trochanter. Remove all osteophytes.
Video 3.
Preparing the greater trochanter.
Step 4: Locate the Insertional Site of the Tendons and Place the Suture Anchors or Drill Holes Into This Site
Identify the area of the footprint for each of the tendons; all suture anchors should be placed in the footprint, and the transosseous drill holes should straddle the near and far edges of the footprint.
Repair of Grade-I and Most Grade-II Tears
Some smaller tears are undersurface tears and cannot be seen from the trochanteric bursal side. Most tears start in the central fibers of the gluteus medius and then progress inferiorly, eventually involving the long head of the gluteus minimus, and then posteriorly toward the superior fibers of the gluteus medius (Fig. 4). The MRI can act as a road map for the position of the tear. Conversely, with abduction and internal rotation, a waviness or laxity can be seen overlying the undersurface tear. Incise the tendon longitudinally in the direction of its fibers to discover the tear.
Whenever possible, perform a separate repair of the long head of the gluteus minimus. It is uncommon for smaller tears to be isolated tears of the gluteus minimus. However, Grade-III and Grade-IV tears commonly involve the gluteus minimus. As the gluteus medius is rarely retracted in Grade-I and II tears, they are typically repaired with a suture-anchor-only technique.
- We have changed from using the 6.5-mm metal or PEEK (polyether ether ketone) suture anchor with three number-2 sutures to using a 2.3-mm all-suture anchor with two number-5 Force Fibers (ICONIX All Suture Anchor; Stryker, Mahwah, New Jersey) to solve a number of problems:
- » Most importantly, our experience with a limited number of failures demonstrated cutting through of the number-2 sutures as one of the main modes of failure.
- » Often these repairs are done in the presence of a femoral component that does not allow full seating or optimal placement of a screw-in anchor.
- » The small hole size is important, especially when used in concert with multiple transosseous drill holes and in a compromised trochanter to prevent its fracture.
- » The all-suture implant aids in minimizing artifacts that can be seen, even with the PEEK anchors, when MRI is required to evaluate the integrity of the tendon repair postoperatively.
Place all sutures and position the lower limb in approximately 20° of abduction and 20° of internal rotation prior to tying the sutures down.
Repair of Grade-III and IV Tears (Figs. 6 and 7)
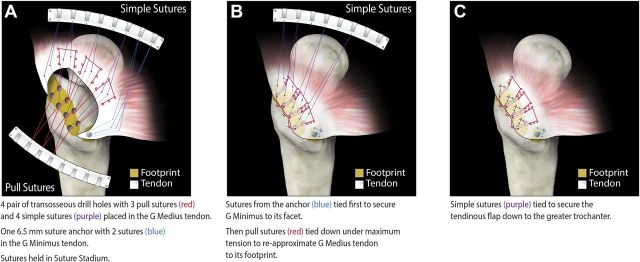
Fig. 6.
Two illustrations of the insertion sites of the gluteus medius. (Reproduced, with permission from Elsevier, from: Robertson WJ, Gardner MJ, Barker JU, Boraiah S, Lorich DG, Kelly BT. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008 Feb;24[2]:130-6.)
Fig. 7.
Repair of a Grade-IV tear in a right hip. Fig. 7-A Two rows of transosseous holes placed parallel to the anterior and posterior margins of the lateral and superior-posterior facets as described by Robertson et al.21 create tunnels. Krackow stitches with number-5 FiberWire are woven into the tendon to create pull sutures that exit 7 to 10 mm from the underside of the tendon edge. These pull sutures are routed through tunnels, drawing the tendon over the footprint site. Additional simple stitches are placed through each tunnel to secure the tendon margin to the abductor footprint. The sutures from a 6.5-mm suture anchor are placed in the tendon of the long head of the gluteus minimus (G Minimus). Fig. 7-B The sutures from the suture anchor secure the gluteus minimus down to its anterior facet, and then pull sutures are tied down under maximum tension, drawing the gluteus medius (G Medius) tendon back down to its footprint on the greater trochanter. Fig. 7-C The tendon, having been reduced into its position, is further secured with the simple sutures.
For larger tears, and for those of the stouter fibers of the gluteus medius, employ transosseous drill holes with alternating number-5 sutures of Force Fiber and FiberWire (Arthrex, Naples, Florida), which have different coloration, again to assist with suture management.
When possible, perform an isolated repair of the long head of the gluteus minimus with a suture anchor (Video 4). The anterior facet for the long head is just anterior to the lateral facet of the gluteus medius. Its facet has a thick cortex, and its insertion site is rather focal, which is ideal for repair with a suture anchor.
For higher-grade tears with a compromised tendon, weave a backing suture of number-5 Mersilene (Ethicon) through the muscle just deep to the musculotendinous junction. Place the leading limb of the simple sutures and the deep locking stitch of the leading pull sutures just proximal to this to prevent their pullout (Video 5).
Identify the anatomic footprint as described by Robertson et al.21 (Fig. 6) for the gluteus medius. The gluteus medius attaches via two distinct attachment sites. The stout posterior fibers insert into the posterior-superior facet, whereas the anterior and central fibers insert into the lateral facet (Video 6).
Place transosseous tunnels side by side perpendicular to the axis of the footprint and in line with the direction of the fibers of the gluteus medius. This will assume a curvilinear shape similar to the outline of the footprint from the posterior-superior tip, to the inferior-most point of the anterior fibers of the gluteus medius. A general rule of thumb is that the number of transosseous tunnels equals the grade of the tear—i.e., two tunnels for a Grade-II tear (if it is not repairable with simple suture anchors), three tunnels for a Grade-III tear, and four tunnels for a Grade-IV tear (Video 7).
Place the medial holes in the near edge of the footprint, and the lateral holes in the far edge. This allows for the proximal portion of the tendon to be secured to the medial edge of the footprint while leaving the distal flap to be secured over the footprint itself. To accomplish this, we employ the Tornier tunneling device. It provides an excellent osseous bridge, allows for variable depth of the tunnel (especially important in the presence of an implant), is straightforward, and facilitates the passage of multiple number-5 sutures. Straight tunnels often need to be drilled too deep (difficult with an implant present) and typically cannot be kept within the anatomic footprint.
- Then place a combination of multiple simple and pull sutures (Fig. 7-A).
- » Route the pull suture through the bone tunnel distal to proximal, weave it through the tendon with the use of a Krackow-type cross-stitch, and then route it back out through the adjacent drill hole. The stitch enters 7 to 10 mm proximal to the torn edge of the tendon and goes proximal toward, and sometimes includes, the musculotendinous junction. When traction is applied, this draws that portion of the tendon to the medial edge of the footprint.
- » Simple sutures, which were passed simultaneously through each tunnel with the pull sutures, enter and exit each tunnel at the medial and lateral holes, respectively. Pass the leading limb through the tendon to the musculotendinous juncture and pass the distal limb with a free needle just proximal to the torn tendon edge. When tied, this secures the flap onto the entirety of the osseous footprint. This simulates a double-row repair and allows for a very broad area for healing of the tendon.
- » Suture management is paramount. After each suture is placed, secure it in the suture stadium, which is numbered and subdivided further as A or B. Place all pull sutures in the more distal stadium in the A dividers and the simple sutures in the more proximal stadiums in the B dividers.
Video 4.
Isolated repair of the gluteus minimus.
Video 5.
Placement of the backing suture.
Video 6.
Insertion sites of the gluteus medius.
Video 7.
Transosseous drill holes and sutures.
Step 5: Reattach the Tendons
After all of the sutures are placed, tie them down, starting with the pull sutures first, to bring the tendon back to bone; then secure the tendon down with the simple sutures (Video 8).
Tie the pull sutures with the lower limb in 20° of internal rotation and 20° of abduction. Placement of the lower limb on a Mayo stand aids in positioning.
With tension applied, sequentially and securely tie the pull sutures. As they exit adjacent tunnels, there is little chance of them cutting through the osseous bridge even with maximum tension applied (Fig. 7-B).
Then tie the simple sutures sequentially with only enough force to approximate the tendon down to the osseous bed to avoid either strangulating the tendon or cutting through the roof of the tunnel (Fig. 7-C).
Video 8.
Tying down the sutures and reattaching the tendon.
Step 6: Reinforce Larger Tears
Reinforce larger tears to protect them and aid in their healing (Video 9).
When a patient has a larger tear, it is important to reinforce the repair. We employ a human dermal fascial supplement that is approximately 5 × 7 cm and 1.8 to 2.2 mm thick. This adds both structural support and scaffolding for cellular repopulation and vascularization, which are presumed to improve healing. Rao et al.22 used a similar suture technique and a dermal graft and reported good results in twelve patients at an average of twenty-two months.
Lay the graft obliquely over the repair with the edge slightly overhanging the most distal and lateral portions of the repair.
Secure the corners and midpoint of the longer sides with a number-1 nonabsorbable suture. Tie it down under some stretch. Next run a number-2 absorbable suture around the entire edge.
Tears of the abductor tendons of the hip, like all other diseases, are highly variable. They encompass the entire spectrum from small undersurface Grade-I tears with minimum muscular atrophy to massive retracted tears (a bald trochanter) with profound muscle atrophy. Each is addressed with guiding principles of secure fixation back down to its anatomical insertion site and maximization of the potential for healing. The various adjuvants (instruments and implants) are utilized in a graduated stepwise fashion, with the augments added as the situation demands, to satisfy these principles. While one must always be cognizant of the costs, the adjuvants allow for an efficient operative procedure (minimizing the operating-room time-related costs) and have hopefully decreased the incidence of retears and reoperations, both of which have associated societal and economic costs.
Video 9.
Placement of the dermal graft.
Step 7: Postoperative Protocol
The postoperative protocol period consists of partial weight-bearing for specific periods of time, followed by vigorous physical therapy for strengthening and gait retraining.
We treat all patients with the same deep venous thrombosis prophylaxis as we use for our patients after total hip arthroplasty.
All of our patients, regardless of the size of the tear, begin with 25% weight-bearing, but they maintain it for variable periods of time: six weeks for Grade-I tears, eight weeks for Grade-II, ten weeks for Grade-III, and twelve weeks for Grade-IV. They are enrolled in a prehabilitation program to assist them in partial weight-bearing.
All patients are instructed to avoid adduction. A hip orthosis is often utilized when a noncompliant patient has a larger (Grade-IV) tear.
A physical therapy protocol for strengthening of the abductors and gait retraining, specific to the size of the tear, is begun at the above time intervals.
Results
Twenty-two patients (twenty-three hips) were included in our original study23. They were evaluated both preoperatively and postoperatively with use of the Trendelenburg test and Medical Research Council (MRC) muscle strength grading system. Their outcomes were measured with use of the Harris hip score24 (HHS) and the Lower-Extremity Activity Scale (LEAS)25 in addition to a satisfaction survey. The tears were graded with use of the Milwaukee classification (Fig. 3).
Ninety-one percent of the patients were women, and the mean age in the series was 67.7 years. Seventy-eight percent of the hips had a larger (Grade-III or IV) tear. All of the hips were evaluated at one year, and 83% were evaluated at five years.
The mean HHS improved from 53 points preoperatively to 87 points at one year. The mean LEAS score likewise improved, from 6.7 to 8.9 points, in this time interval. There was no statistically detectable difference between the groups. However, as expected, there was an obvious trend for better results the smaller the tear. These results were maintained over the five-year time interval, with a mean HHS of 88 points and a mean LEAS score of 8.8 points. Muscle strength improved by 1.6 grades on average. Seventy-nine percent of the patients had a negative Trendelenburg sign, and 84% used no ambulatory aids. Pain relief was reliable obtained (90% improvement according to patient report), as was improvement in function (80% improvement). At five years, sixteen of the nineteen patients were satisfied with their result and stated that they would undergo the procedure again if required. No major orthopaedic or medical complications occurred.
Surgical repair can improve function and reliably decreases pain in patients with a hip abductor tear. The clinical function was maintained over the five-year time frame.
What to Watch For
Indications
Clinical symptoms of peritrochanteric pain and weakness.
An MRI-documented tear of the gluteus medius or minimus tendon of the hip. Ultrasound may be used if the patient is unable to undergo MRI and you have the technical ability at your facility.
Contraindications
These tears typically occur in elderly patients, some of whom might not be suitable medical candidates for an orthopaedic hip procedure.
Insufficient quality of the tendon and substantial muscle atrophy and fatty infiltration. The MRI must be scrutinized for these factors, particularly for larger tears.
Pitfalls & Challenges
To date, twelve of 610 procedures have been followed by revision. At the time of revision, the typical failure has been either rupture or pull-through of the number-2 suture. The tension exerted on the abductor tendon repair during daily activities appears to require a stouter suture.
- With a femoral implant in place, the technique has to be slightly modified to avoid interference from the implant.
- » When using suture anchors, we have switched to using an all-suture implant and have placed this at an angle slightly greater than the typical 90° that is recommended for most other anchors.
- » For the transosseous holes, we can modify the depth of the tunnel by modifying the angle of the tunneling device so that the implant does not deflect the loop of the shuttle suture.
- The quality of this relatively short and thin (central and anterior portions of the gluteus medius) tendon can be moderately or severely attenuated. This can be addressed in three different ways:
- » Run a reinforcing umbilical tape at the musculotendinous junction and place the proximal-most limb of the suture just proximal to it to improve the grab of the suture.
- » Add a BioFiber scaffolding patch (Tornier), which works like a grommet, to the construct to prevent the sutures from pulling through the compromised tendon.
- » If the muscle is not too atrophic but the tendon is severely compromised, reinforce the construct with an Achilles tendon graft as described by Fehm et al.26.
With severe atrophy, especially with considerable fatty infiltration, we supplement the repair with a tensor fasciae latae and gluteus maximus transfer27. Whiteside et al. reported good results after a transfer of the gluteus maximus28. The Milwaukee classification system has recently been modified to account for muscle atrophy.
In cases of tendon destruction secondary to adverse local tissue reaction (ALTR), the remaining tendon is often seriously destroyed and devoid of any vascularity and therefore any healing potential. Consider either an Achilles tendon graft reinforcement or a musculotendinous transfer, which is our preferred technique for this situation.
Clinical Comments
What percentage of patients undergoing total hip replacement have been shown to have a tear of the abductor mechanism?
What neurovascular structures are at greatest risk with superior dissection during mobilization of the gluteus medius?
What modifications are required with this technique in patients with either poor remaining tendon or profound muscle atrophy and fatty infiltration?
Acknowledgments
Note: The authors acknowledge Jon Haven for his artistic assistance with the figures, Mr. Thomas Kaemmerling for his editorial assistance with the video clips, and Mr. Jon Schneck for his assistance with the making of the video.
Footnotes
Based on an original article: J Bone Joint Surg Am. 2013 Aug 7;95(15):1420-5.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. In addition, one or more of the authors receives royalties that are broadly relevant to the work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Karpinski MR, Piggott H. Greater trochanteric pain syndrome. A report of 15 cases. J Bone Joint Surg Br. 1985. November;67(5):762-3. [DOI] [PubMed] [Google Scholar]
- 2.Schapira D, Nahir M, Scharf Y. Trochanteric bursitis: a common clinical problem. Arch Phys Med Rehabil. 1986. November;67(11):815-7. [PubMed] [Google Scholar]
- 3.Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanter pain syndrome). Mayo Clin Proc. 1996. June;71(6):565-9. [DOI] [PubMed] [Google Scholar]
- 4.Walker P, Kannangara S, Bruce WJ, Michael D, Van der Wall H. Lateral hip pain: does imaging predict response to localized injection? Clin Orthop Relat Res. 2007. April;(457):144-9. [DOI] [PubMed] [Google Scholar]
- 5.Bunker TD, Esler CN, Leach WJ. Rotator-cuff tear of the hip. J Bone Joint Surg Br. 1997. July;79(4):618-20. [DOI] [PubMed] [Google Scholar]
- 6.Chung CB, Robertson JE, Cho GJ, Vaughan LM, Copp SN, Resnick D. Gluteus medius tendon tears and avulsive injuries in elderly women: imaging findings in six patients. AJR Am J Roentgenol. 1999. August;173(2):351-3. [DOI] [PubMed] [Google Scholar]
- 7.Fisher DA, Almand JD, Watts MR. Operative repair of bilateral spontaneous gluteus medius and minimus tendon ruptures. A case report. J Bone Joint Surg Am. 2007. May;89(5):1103-7. [DOI] [PubMed] [Google Scholar]
- 8.Kagan A., 2nd Rotator cuff tears of the hip. Clin Orthop Relat Res. 1999. November;(368):135-40. [PubMed] [Google Scholar]
- 9.Lonner JH, Van Kleunen JP. Spontaneous rupture of the gluteus medius and minimus tendons. Am J Orthop. 2002. October;31(10):579-81. [PubMed] [Google Scholar]
- 10.Ozçakar L, Erol O, Kaymak B, Aydemir N. An underdiagnosed hip pathology: apropos of two cases with gluteus medius tendon tears. Clin Rheumatol. 2004. October;23(5):464-6. Epub 2004 May 14. [DOI] [PubMed] [Google Scholar]
- 11.Howell GE, Biggs RE, Bourne RB. Prevalence of abductor mechanism tears of the hips in patients with osteoarthritis. J Arthroplasty. 2001. January;16(1):121-3. [DOI] [PubMed] [Google Scholar]
- 12.LaBan MM, Weir SK, Taylor RS. ‘Bald trochanter’ spontaneous rupture of the conjoined tendons of the gluteus medius and minimus presenting as a trochanteric bursitis. Am J Phys Med Rehabil. 2004. October;83(10):806-9. [DOI] [PubMed] [Google Scholar]
- 13.Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001. September;44(9):2138-45. [DOI] [PubMed] [Google Scholar]
- 14.Blankenbaker DG, Ullrick SR, Davis KW, De Smet AA, Haaland B, Fine JP. Correlation of MRI findings with clinical findings of trochanteric pain syndrome. Skeletal Radiol. 2008. October;37(10):903-9. Epub 2008 Jun 20. [DOI] [PubMed] [Google Scholar]
- 15.Kingzett-Taylor A, Tirman PF, Feller J, McGann W, Prieto V, Wischer T, Cameron JA, Cvitanic O, Genant HK. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings. AJR Am J Roentgenol. 1999. October;173(4):1123-6. [DOI] [PubMed] [Google Scholar]
- 16.Cvitanic OL, Henzie GR, Skezas NI, Lyons JA, Minter JO. MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus). AJR Am J Roentgenol. 2004. January;182(1):137-43. [DOI] [PubMed] [Google Scholar]
- 17.Hendry J, Biant LC, Breusch SJ. Abductor mechanism tears in primary total hip arthroplasty. Arch Orthop Trauma Surg. 2012. November;132(11):1619-23. Epub 2012 Jul 05. [DOI] [PubMed] [Google Scholar]
- 18.Davies H, Zhaeentan S, Tavakkolizadeh A, Janes G. Surgical repair of chronic tears of the hip abductor mechanism. Hip Int. 2009. Oct-Dec;19(4):372-6. [DOI] [PubMed] [Google Scholar]
- 19.Voos JE, Shindle MK, Pruett A, Asnis PD, Kelly BT. Endoscopic repair of gluteus medius tendon tears of the hip. Am J Sports Med. 2009. April;37(4):743-7. Epub 2009 Feb 09. [DOI] [PubMed] [Google Scholar]
- 20.Walsh MJ, Walton JR, Walsh NA. Surgical repair of the gluteal tendons: a report of 72 cases. J Arthroplasty. 2011. December;26(8):1514-9. Epub 2011 Jul 27. [DOI] [PubMed] [Google Scholar]
- 21.Robertson WJ, Gardner MJ, Barker JU, Boraiah SB, Lorich DG, Kelly BT. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008. February;24(2):130-6. [DOI] [PubMed] [Google Scholar]
- 22.Rao BM, Kamal TT, Vafaye J, Taylor L. Surgical repair of hip abductors. A new technique using Graft Jacket allograft acellular human dermal matrix. Int Orthop. 2012. October;36(10):2049-53. Epub 2012 Aug 08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davies JF, Stiehl JB, Davies JA, Geiger PB. Surgical treatment of hip abductor tendon tears. J Bone Joint Surg Am. 2013. August 7;95(15):1420-5. [DOI] [PubMed] [Google Scholar]
- 24.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969. June;51(4):737-55. [PubMed] [Google Scholar]
- 25.Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buyea CM, Krackow KA. Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am. 2005. September;87(9):1985-94. [DOI] [PubMed] [Google Scholar]
- 26.Fehm MN, Huddleston JI, Burke DW, Geller JA, Malchau H. Repair of a deficient abductor mechanism with Achilles tendon allograft after total hip replacement. J Bone Joint Surg Am. 2010. October 6;92(13):2305-11. [DOI] [PubMed] [Google Scholar]
- 27.Nogler M. Department of Experimental Orthopaedics, Innsbruck, Austria. Personal communication, 2013.
- 28.Whiteside LA, Nayfeh T, Katerberg BJ. Gluteus maximus flap transfer for greater trochanter reconstruction in revision THA. Clin Orthop Relat Res. 2006. December;(453):203-10. [DOI] [PubMed] [Google Scholar]