Overview
Introduction
When used for strict surgical indications, operative management of chronic symptomatic os subfibulare in children involving fragment excision and ligament repair can significantly improve visual analog scale pain scores and result in high Foot and Ankle Outcome Scores.
Step 1: Indications and Preoperative Planning
Operative indications are chronic pain at the distal part of the fibula, symptoms of instability at the anterior talofibular ligament and/or calcaneofibular ligament, and a radiographic finding of an os fibulare.
Step 2: Ossicle Excision
Perform an approach to the lateral malleolus and excise the fragment while preserving the anterior talofibular ligament and calcaneofibular ligament.
Step 3: Ankle Examination
Examine the ankle for loose bodies or other associated damage.
Step 4: Preparation for Ligament Repair
Repair the anterior talofibular ligament and calcaneofibular ligament to the debrided distal part of the fibula.
Step 5: Preparation for Modified Broström Procedure
Imbricate the lateral capsule to secondarily reconstruct and reinforce the ligaments, adding to the strength of the repair.
Step 6: Repair, Reconstruction, and Closure
Reduce the ankle joint and tie down the sutures.
Step 7: Casting
Patients wear a cast and remain non-weight-bearing for six weeks postoperatively.
Step 8: Postoperative Protocol
Patients advance to full weight-bearing in a CAM boot and start physical therapy at six weeks.
Results
We performed a retrospective case study of the first twenty-three patients treated with our procedure for symptomatic os subfibulare.
Introduction
When used for strict surgical indications, operative management of chronic symptomatic os subfibulare in children involving fragment excision and ligament repair can significantly improve visual analog scale pain scores and result in high Foot and Ankle Outcome Scores.
While ankle sprains are common injuries that typically improve with conservative treatment, some patients may have residual disability after a sprain as a result of a number of potential etiologies1-4. One potential cause of residual disability is a chronic symptomatic os subfibulare, which, rather than being a benign unfused accessory ossification center, may instead result from an avulsion of the anterior talofibular ligament or calcaneofibular ligament5-11.
It may be that os fibulare is a normal variant, but as it is attached to the anterior talofibular ligament and calcaneofibular ligament it can be avulsed, becoming an ununited ossicle. Many clinicians worry about the distinction of etiology: that is, is it an avulsion fragment or accessory ossification? Regardless of its etiology, the real concern for the clinician should be to not ignore the problem when symptoms persist despite conservative treatment.
While we were unable to resolve the debate over the etiology of os subfibulare, we were able to develop a successful surgical treatment protocol for chronic symptomatic os subfibulare and evaluate the long-term outcomes following this treatment. Our surgical treatment consists of excision of the osseous fragment, ligament repair, and a modified Broström procedure (Video 1).
Video 1.
The indications, radiographic findings, and surgical technique are described.
Step 1: Indications and Preoperative Planning
Operative indications are chronic pain at the distal part of the fibula, symptoms of instability at the anterior talofibular ligament and/or calcaneofibular ligament, and a radiographic finding of an os fibulare.
Presenting symptoms include lateral ankle swelling, recurrent lateral “ankle sprains,” and feelings of instability during athletic activity, most notably lateral cutting activities.
On examination, determine if the patient has pain with plantar varus stress testing and point tenderness at the distal anterior aspect of the lateral malleolus, both of which were present in all of the patients in our study12. If the fragment was substantially displaced, there was often a palpable ridge along the distal part of the lateral malleolus. Note that only 13% of our cases had a positive anterior drawer test or opening with a varus stress test (Figs. 1-A and 1-B).
Look for the radiographic findings of an os fibulare (Figs. 1-C through 1-F), which is often displaced from the rest of the fibula.
While magnetic resonance imaging (MRI) and computed tomography (CT) are not necessary for diagnosis in the majority of cases, they may be useful for identifying a displaced cartilaginous fragment as well as localizing the ossicle for preoperative planning (Fig. 1-G). When MRI was initially performed to identify potential lateral ankle ligament tears, no tears were identified in our series12.
Figs. 1-A and 1-B Radiographic demonstration of ankle varus stress testing.
Fig. 1-A.
A normal anteroposterior radiograph of the ankle does not demonstrate any gross deformity.
Fig. 1-B.

However, a varus stress radiograph demonstrates gross instability and incompetence of the lateral ankle ligaments. Note that displacement on varus stress testing was not a consistent finding in our series.
Figs. 1-C through 1-F Radiographic examples of os subfibulare. Note that radiographic findings alone are not an operative indication. The fragments varied in number (Fig. 1-D), displacement (Fig. 1-C), and size (Figs. 1-E and 1-F).
Fig. 1-C.

Fig. 1-D.
Fig. 1-E.
Fig. 1-F.

Fig. 1-G.
Three-dimensional reconstruction of a CT scan can be useful for localizing the ossicle.
Step 2: Ossicle Excision
Perform an approach to the lateral malleolus and excise the fragment while preserving the anterior talofibular ligament and calcaneofibular ligament.
Make a longitudinal or curved “posterior hockey stick” incision over the posterior border of the lateral malleolus.
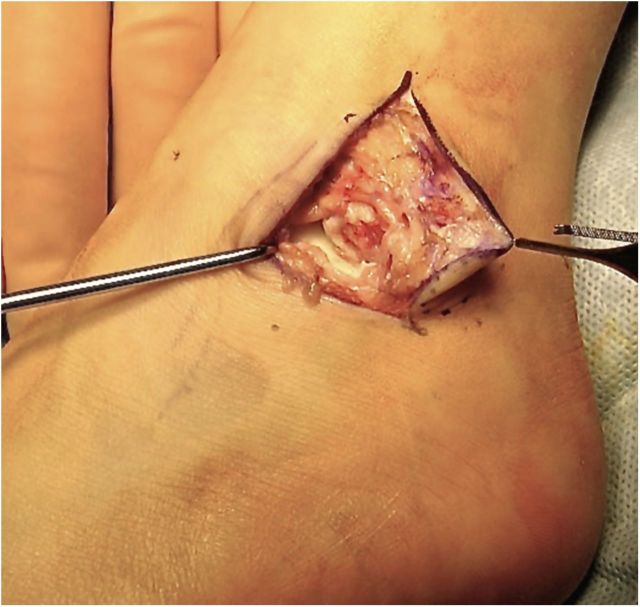
Identify and sharply dissect the fragment from the anterior talofibular ligament and calcaneofibular ligament as it is removed (Fig. 2).
Fig. 2.

Excised os subfibulare.
Step 3: Ankle Examination
Examine the ankle for loose bodies or other associated damage.
Open the capsule to directly visualize the articular surface. Look for loose bodies and damage to the lateral aspect of the talus, which may require debridement. Fluoroscopy may also be used to examine for loose bodies.
Examine the integrity of the remaining ankle ligaments.
Step 4: Preparation for Ligament Repair
Repair the anterior talofibular ligament and calcaneofibular ligament to the debrided distal part of the fibula.
Debride the docking site on the distal part of the fibula down to healthy cancellous bone (Fig. 3-A).
Use nonabsorbable sutures to place a Krackow locking stitch in each of the ligaments.
Drill three tunnels using a 0.62-in (1.575-cm) Kirschner wire from proximal posterior (anterior to the peroneal tendon sheath) to the distal anterior area from which the ossicle was avulsed. Avoid the distal fibular physis—use fluoroscopy. When drilling the bone tunnels, align them so that the sutures will pull the ligaments in a straight line toward the fibula. The anterior talofibular ligament should be pulled to the anterior aspect of the fibula, and the calcaneofibular ligament should be pulled to the inferior tip of the fibula.
Using two large Keith needles, pass the sutures from the Krackow stitches in the anterior talofibular ligament and calcaneofibular ligament through the tunnels. Pass one of the anterior talofibular ligament stitch ends through the proximal tunnel, and the other anterior talofibular ligament stitch end through the middle tunnel. Pass one of the calcaneofibular ligament stitch ends through the middle tunnel (with the one anterior talofibular ligament stitch), and pass the other calcaneofibular ligament stitch end through the most distal hole (Fig. 3-B).
Fig. 3-A.
After removal of the os subfibulare, the fibular bed is debrided to healthy cancellous bone.
Fig. 3-B.
Keith needles passed through the bone tunnels of the fibular epiphysis for passing and anchoring the anterior talofibular ligament and calcaneofibular ligament sutures. Keep bone tunnels away from the distal fibular physis.
Step 5: Preparation for Modified Broström Procedure
Imbricate the lateral capsule to secondarily reconstruct and reinforce the ligaments, adding to the strength of the repair.
Prepare a 1-cm-wide band of the transverse crural ligament (superior extensor retinaculum).
Leave the crural ligament attached near the calcaneus, and leave it long enough to cross over the anteroinferior aspect of the fibula.
Step 6: Repair, Reconstruction, and Closure
Reduce the ankle joint and tie down the sutures.
Thoroughly irrigate the wound.
Hold the ankle in a reduced position: the heel should be everted and laterally rotated, and the ankle joint should be held at 90°.
Tighten and tie down the sutures from the anterior talofibular ligament and the calcaneofibular ligament. Tie the most proximal stitch to one of the middle stitches. Tie the most distal stitch to the other middle stitch.
Securely suture the prepared crural ligament (superior extensor retinaculum) for the Broström lateral ankle reconstruction to the fibula.
Close the incision in layers. We prefer an absorbable subcuticular running closure for the skin.
Step 7: Casting
Patients wear a cast and remain non-weight-bearing for six weeks postoperatively.
Apply a well-padded short leg cast.
Position the ankle at 90° to the tibia and gently evert and laterally rotate the subtalar joint.
Our patients wore the same cast for six weeks, but the cast can be changed if desired or necessary.
Step 8: Postoperative Protocol
Patients advance to full weight-bearing in a CAM boot and start physical therapy at six weeks.
At the six-week appointment, remove the cast and examine the wound. Patients then can advance to a CAM (controlled ankle motion) boot with full weight-bearing.
Have the patient begin physical therapy at six weeks with low-impact range-of-motion and strengthening exercises.
As the subsequent six weeks progress, allow the patient to gradually advance activities as tolerated to normal.
Results
We performed a retrospective case study of the first twenty-three patients treated with our procedure for symptomatic os subfibulare. The senior author (R.S.D.) treated all of the patients at one institution12.
The patients included eight boys and fifteen girls ranging in age from eight to seventeen years at the time of surgery. The mean age was 10.4 years (range, eight to thirteen years) at the time of injury and 13.6 years (range, eight to seventeen years) at the time of surgery, representing an average delay in diagnosis and treatment of 3.2 years (range, six months to five years). At the time of surgery, every bone fragment in our series was attached, either completely or to a portion of either the anterior talofibular ligament or the calcaneofibular ligament.
All patients returned to normal age-appropriate activities and regular gym class within four months postoperatively. None of the patients had tenderness or symptoms of instability in the follow-up period. While three patients returned within the first three days for splitting of a “tight” cast, there were no wound complications, compartment syndromes, or infections.
A telephone survey was conducted at a mean of 4.5 years (range, 2.1 to 13.2 years) postoperatively. The mean Foot and Ankle Outcome Score, which has been shown to be both valid and reliable for the evaluation of patient-relevant outcomes related to ankle reconstruction13, was 91.4 (range, 87 to 98) of 100, with all but one patient returning to the preinjury recreational level. The pain levels improved from a preoperative mean of 7.8 on a visual analog scale to 2.1 at the latest follow-up evaluation.
One patient competed competitively in running events as a senior in college. However, because of the patients’ young age at surgery and the duration of the follow-up period, few were of an age for varsity or college sports at the time of final follow-up.
One patient reported continued lateral ankle swelling when playing pivoting sports but not persistent pain or instability. There were no other long-term complications from the procedure.
What to Watch For
Indications
Pain on plantar varus stress testing and point tenderness at the distal anterior aspect of the lateral malleolus that does not respond to nonoperative treatment.
Radiographic findings of a typically displaced os fibulare.
Recurrent lateral “ankle sprains” and instability during athletic activity.
Contraindications
Asymptomatic os fibulare.
Patients with lateral ankle pain and an os fibulare noted on radiographs who have not yet been treated with conservative measures including rest, immobilization, and a course of physical therapy.
Pitfalls & Challenges
Avoid making bone tunnels through the distal fibular physis in skeletally immature patients.
Space bone tunnels adequately to prevent suture cutout or bone avulsion.
Be vigilant with casting. Avoid ankle contracture by casting at 90° of dorsiflexion. Protect ligament repair by everting and laterally rotating the subtalar joint.
Clinical Comments
-
Two patients in our group had a second lateral ankle ligament disruption nearly one year after their initial surgery and required a revision Broström lateral ankle reconstruction. These patients were both gymnasts who sustained the injury during athletic activities. This leads to two questions:
○ Should patients who undergo this procedure limit their participation in high-impact activities?
○ Is there a subset of patients with an avulsion etiology of os subfibulare who are more prone to recurrent injuries due to physiologic or proprioceptive causes?
Two cases of os subfibulare were treated by a different surgeon at our institution with debridement and screw fixation. It took over six months for these patients to obtain osseous union. Have other surgeons had experiences with attempted screw fixation?
Footnotes
Based on an original article: J Bone Joint Surg Am. 2013 Aug 21;95(16):e115.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Andermahr J, Helling HJ, Maintz D, Mönig S, Koebke J, Rehm KE. The injury of the calcaneocuboid ligaments. Foot Ankle Int. 2000. May;21(5):379-84. [DOI] [PubMed] [Google Scholar]
- 2.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998. Oct;19(10):653-60. [DOI] [PubMed] [Google Scholar]
- 3.Jackson DW, Ashley RL, Powell JW. Ankle sprains in young athletes. Relation of severity and disability. Clin Orthop Relat Res. 1974. Jun;101(101):201-15. [PubMed] [Google Scholar]
- 4.Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995. Apr;21(4):206-15. [DOI] [PubMed] [Google Scholar]
- 5.O’Rahilly R. A survey of carpal and tarsal anomalies. J Bone Joint Surg Am. 1953. Jul;35(3):626-42. [PubMed] [Google Scholar]
- 6.Shands AR, Jr, Wentz IJ. Congenital anomalies, accessory bones, and osteochondritis in the feet of 850 children. Surg Clin North Am. 1953. Dec;66:1643-66. [DOI] [PubMed] [Google Scholar]
- 7.Powell H. Extra Centre of Ossification for the Medial Malleolus in Children. Incidence and Significance. J Bone Joint Surg. 1961. Feb;43(1):107-13. [Google Scholar]
- 8.Griffiths JD, Menelaus MB. Symptomatic ossicles of the lateral malleolus in children. J Bone Joint Surg Br. 1987. Mar;69(2):317-9. [DOI] [PubMed] [Google Scholar]
- 9.Berg EE. The symptomatic os subfibulare. Avulsion fracture of the fibula associated with recurrent instability of the ankle. J Bone Joint Surg Am. 1991. Sep;73(8):1251-4. [PubMed] [Google Scholar]
- 10.Champagne IM, Cook DL, Kestner SC, Pontisso JA, Siesel KJ. Os subfibulare. Investigation of an accessory bone. J Am Podiatr Med Assoc. 1999. Oct;89(10):520-4. [DOI] [PubMed] [Google Scholar]
- 11.Ogden JA, Lee J. Accessory ossification patterns and injuries of the malleoli. J Pediatr Orthop. 1990. May-Jun;10(3):306-16. [DOI] [PubMed] [Google Scholar]
- 12.Pill SG, Hatch M, Linton JM, Davidson RS. Chronic symptomatic os subfibulare in children. J Bone Joint Surg Am. 2013. Aug 21;95(16):e115(1-6). [DOI] [PubMed] [Google Scholar]
- 13.Roos EM, Brandsson S, Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001. Oct;22(10):788-94. [DOI] [PubMed] [Google Scholar]