Abstract
Background:
Prior to 2003, production of new surgeons in Ghana was limited. In 2003, the Ghana College of Physicians and Surgeons (GCPS) initiated the first wholly in-country training and credentialing of surgeons. The purpose of this study was to assess the impact of in-country training of surgeons in Ghana.
Methods:
We interviewed 117 (80%) of the 146 surgeons trained through the GCPS from inception through 2016. We gathered data on type of training, practice location, clinical workload, and administrative and teaching roles. Operations were categorized into those deemed essential (most cost-effective, highest population impact) by the World Bank’s Disease Control Priorities project vs. other.
Results:
In-country retention was 87%-97%. A little more than half (56%) were working in the two largest cities and 44% were working in higher need areas. Twenty-two (19%) were the first surgeon to have worked at their current hospital. The surgeons performed a mean of 13 operations per week (seven electives, six emergencies). 35% of elective and 77% of emergency operations were in the essential category. Most (79%) surgeons were engaged in training/teaching; 46% were engaged in research; and 33% held an administrative office.
Conclusions:
In-country surgical training has led to high retention and wide geographic distribution, including high need areas. The in-country trained surgeons are playing key roles in clinical practice, training, and administration. These data provide support for investments in similar efforts in other low- and middle-income countries.
Keywords: Surgical training, Ghana College of Physicians and Surgeons, Low- and middle-income country, Global surgery
Introduction
A well-recognized component of a nation’s surgical capacity is its ability to train medical doctors to become surgeons and retain them in-country to serve the population. [1] Development of this capacity is critical in low- and middle-income countries (LMICs) whose populations face a large and growing unmet need for surgery.[2-4]
Surgical training for doctors requires a comprehensive infrastructure for instruction, trainee assessments, and quality assurance. Before 2003, graduates of Ghana’s medical schools had two choices if they wanted to become surgeons. First, was to train in-country, with credentialing through the West African College of Surgeons (WACS), requiring repeated trips to Nigeria for multi-stage examinations. This process took most applicants many years to complete, with very few surgeons joining the work force annually. Second, was to leave the country, usually to train in Europe or North America, with very low rates of return to Ghana. As example, only 10% of qualified obstetrician-gynecologists trained abroad through a Carnegie-sponsored program, returned to Ghana [1].
The Ghana College of Physicians and Surgeons (GCPS) was established in 2003 to train and credential specialists, wholly in-country. Fourteen faculties representing the various disciplines were created to oversee curriculum design, trainer and facility accreditation, and trainee examinations. Surgeons are trained through the faculty of surgery.[5] Primary medical education in Ghana lasts six years. This is followed by two years of housemanship (internship) training, after which one can apply to the GCPS for surgical training. Surgical training lasts three years and successful trainees are awarded with a membership certificate, allowing them to practice as specialist surgeons with a broad range of skills. The GCPS also offers advanced training in the various sub-specialties of surgery that lasts 2-3 years with successful trainees awarded a fellowship certificate, which is a requirement for faculty appointments at Ghanaian universities. The adoption of a two-tier (member, fellow) system of specialist training was intended to produce adequate numbers of specialists over a shorter time to serve in hospitals throughout the country, and for a smaller number to undergo further training for more advanced academic and sub-specialty practice. With the establishment of the GCPS, Ghana stopped sponsoring doctors for specialist training abroad.
We aimed to assess the effect of the GCPS initiative on the production and retention of in-country trained surgeons, as well as their surgical output and other measures of impact on the facilities and communities they work. By so doing, we hoped to establish a benchmark for future assessments of the impact of training surgeons locally in Ghana and other LMICs. In addition, our results could assist with efforts to advocate for more resources for training surgeons locally, which could contribute to reducing the large unmet need for surgery that many LMICs face. [6]
Methods
Setting
Ghana is a lower-middle income country in West Africa with a population of 26 million and covering an area of 238,500 sq.km.[7] Hospital-based surgical care is organized at three levels: district (first-level), regional (referral) and tertiary hospitals.[8] District hospitals have 50–100 beds and surgical care is mostly provided by non-surgeon physicians. Regional or tertiary hospitals have larger bed capacities, are staffed by fully-trained surgeons, and offer a broader range of surgical services.[6]
Participants
All graduates of the faculty of surgery of the GCPS since inception until December 31, 2016 were eligible for the study. A total of 146 had completed training. Their contact information was collected from the GCPS records. Nineteen had either permanently left the country or could not be reached with the available contact information. These surgeons were excluded from the study. The remaining 127 surgeons were contacted. Those who consented to the study were surveyed by self-administration (52%) or by face-to-face (41%) or phone interviews (7%).
Survey
The survey was conducted from June 10 to July 20, 2017, with a structured questionnaire. Information on participant demographics, GCPS training, graduation dates, hospital of practice pre- and post-training, clinical workload including the types and numbers of surgical procedures performed, administrative and teaching roles, and research output were collected. Information about changes participants had brought to their hospitals and community service they are involved in was also obtained. Finally, participants’ views were sought on how the large burden of surgical conditions in Ghana could be reduced. The latter two survey items were posed as open-ended questions and participants were allowed to provide multiple responses. Google Maps (https://www.google.com.gh/maps/) was used to determine the geographic coordinates of participants’ hospital of practice pre- and post-training.
Data Analysis
Analyses were conducted with Stata v14 (StataCorp, College Station, TX) and expressed as descriptive statistics. The top three elective and emergency surgical procedures reported by participants were classified as those deemed “essential procedures” by the third edition of the World Bank’s Disease Control Priorities Project (DCP-3) versus “other procedures”.[6, 9] The former has been described by the DCP-3 as those procedures that are most cost-effective and yield the highest population impact.
Responses to the open-ended (qualitative) questions were analyzed using a content analysis framework.[10] Responses were initially grouped into categories by codes that represented similar responses. These were then refined into useful themes and described. Chi-square was used to assess the significance of differences between members and fellows regarding types of procedures performed.
Ethical approval
The study was approved by Kwame Nkrumah University of Science and Technology Committee for Human Research and Publication Ethics.
Results
Demographics
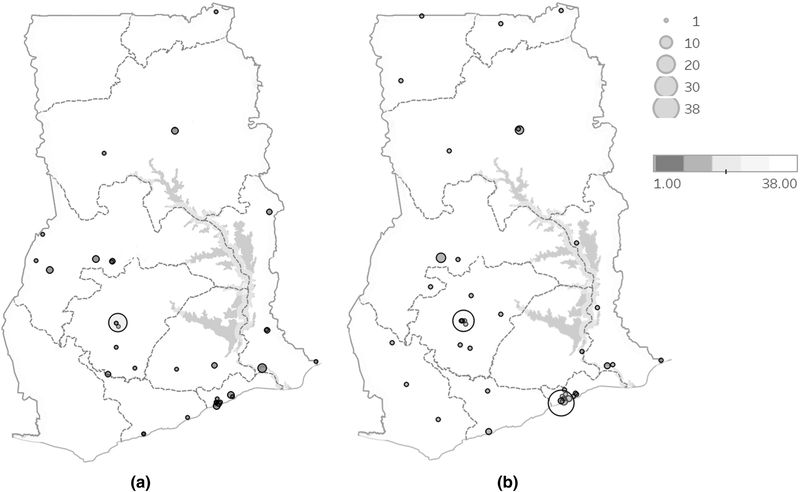
Of the 146 GCPS-trained surgeons at the time of the study, four (3%) were known to have left the country, 15 (10%) could not be reached, and 10 (7%) declined participation in the study (all of whom were working in Ghana). One hundred and seventeen surgeons participated in the survey (response rate 80% total; 93% of those who could be contacted). The retention rate of GCPS-trained surgeons in Ghana was estimated at 87% as a minimum (considering those who could not be reached as having left the country) up to 97% (if those who could not be reached were assumed to be practicing in-country). On analysis of the 117 surgeons who participated in the survey, most were males (105; 90%) and mean age was 39 (range: 30-50) years. One hundred and ten (94%) obtained their primary medical qualification locally; the rest were foreign-trained. The mean duration of general medical practice prior to enrolment into the GCPS training program was 4 (range: 2-12) years. Figure 1 shows the geographic locations of hospitals where participants used to practice prior to training.
Figure 1.
Location of hospitals where Ghana College-trained surgeons (A) practiced pre-training and (B) currently practice
Size of circles shows number of doctors at particular hospital; Colors of circle shows number of doctors at particular hospital.
Surgical training
Participants were trained at one of the two main training sites: Korle-Bu Teaching Hospital in Ghana’s capital, Accra (60; 51%) and Komfo Anokye Teaching Hospital in Ghana’s second largest city, Kumasi (57; 49%). Most (80; 69%) participants completed membership training in the prescribed three years (median duration; 3 (3-5) years). One hundred and four (89%) had a membership certificate, 46 (39%) of whom were currently enrolled in various fellowship programs, while 13 (11%) possessed a fellowship certificate (Table 1). General surgery, trauma and orthopedics, and urology were the sub-specialty programs most pursued by fellows and those training for fellowship (47; 40%) (Table 1).
Table 1.
Characteristics of surgeons trained by the Ghana College of Physicians and Surgeons (2003 – 2017)
| Number | % | |
|---|---|---|
| Age (years) at time of survey; mean, (range) | 39 | (30-50) |
| Years of medical practice pre-GCPS training; mean (range) | 4 | (2-12) |
| Sex | ||
| Male | 105 | 90 |
| Female | 12 | 10 |
| Nationality | ||
| Ghanaian | 113 | 96 |
| Togolese | 2 | 2.0 |
| Gambian | 2 | 2.0 |
| Country of participant's primary medical education | ||
| Ghana | 110 | 94 |
| Cuba | 2 | 2.0 |
| Gambia | 2 | 2.0 |
| Togo | 2 | 2.0 |
| Russia | 1 | 1.0 |
| Current affiliation with GCPS | ||
| Member | 58 | 50 |
| Member in fellowship training | 46 | 39 |
| Fellow | 13 | 11 |
| Additional certification from WACS | 69 | 59 |
| Primary employer | ||
| Ministry of Health | 52 | 44 |
| Ghana Health Service | 30 | 26 |
| Christian Health Association of Ghana | 23 | 20 |
| University | 3 | 3.0 |
| Ministry of Defense/Interior | 5 | 4.0 |
| Private | 4 | 3.0 |
| Fellowship discipline (including fellows and those in fellowship training) (N=68) | ||
| General surgery | 18 | 26 |
| Trauma/orthopedics | 16 | 24 |
| Urology | 13 | 19 |
| Pediatric surgery | 7 | 10 |
| Plastic surgery | 6 | 8.8 |
| Neurosurgery | 5 | 7.4 |
| Cardiothoracic surgery | 3 | 4.4 |
| Number of outpatients seen/week; mean (range) | 48 | 10-200 |
| Number of elective surgeries performed/week; mean,(range) | 7 | 1-25 |
| Number of emergency patients seen/week; mean, (range) | 12 | 1-45 |
| Number of emergency surgeries performed/week; mean,(range) | 6 | 1-20 |
| Holds administrative office at hospital | 39 | 33 |
| Engaged in teaching (students, nurses, intern doctors, etc) | 92 | 79 |
| Engaged in research | 54 | 46 |
| Engaged in active community service | 63 | 54 |
GCPS – Ghana College of Physicians and Surgeons; WACS – West African College of Surgeons
Most participants (98; 84%) reported having a continuous relationship with the institutions where they had their residency training, in the form of consulting for advice on patient management (30; 26%) or attending meetings/programs (14; 12%). Others were in fellowship training at their former training institutions (29; 25%) or had been employed by these institutions after training (25; 21%).
Current practice
Majority (105; 90%) of participants were employed by the Ghana Ministry of Health (responsible directly for tertiary hospitals), the Ghana Health Service (mainly runs public district and regional hospitals) or the Christian Health Association of Ghana (primarily runs faith-based district hospitals). Twenty-two (19%) participants reported that they were the first surgeon ever to have worked at their current hospitals. The geographic location of hospitals where GCPS-trained surgeons currently practiced is shown in Figure 1, indicating an increased geographic distribution (including to rural areas) in comparison to site of practice before specialization. Fifty-six percent were working in the two largest cities while the rest were working in higher need areas.
All participants were engaged in active clinical service, seeing a mean of 48 out-patients per week (range; 10-200 patients) and performing a mean of seven elective surgeries (range; 1-25) per week. They also reported consulting a mean of 12 emergency surgical patients (range; 1-45 patients) per week and performed a mean of six emergency surgeries (range; 1-20) per week. The mean total number of operations per week was 13 (range: 2-36). The interquartile range for total number of operations per week was 9–16. Ten percent of surgeons performed six or less operations per week.
Essential general surgical procedures, including hernia repair, hydrocelectomy, and cholecystectomy (82; 27%) and other general surgical procedures such as soft tissue excision biopsy, mastectomy, and thyroidectomy (98; 32%) were among the most common top three elective surgeries that participants reported performing. Similarly, essential general surgical procedures, including appendectomy, repair of complicated hernia, and repair of perforated hollow viscus, formed majority (201; 66%) of the top three emergency surgeries reportedly performed by participants (Table 2).
Table 2.
Top three elective and emergency surgeries reported by surgeons trained by the Ghana College of Physicians and Surgeons
| Member |
Fellow/ Trainee fellow |
Total |
||||
|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | |
| Elective surgeries | 154 | (100) | 150 | (100) | 304 | (100) |
| Essential general surgical procedures (e.g. hernia repair, hydrocelectomy, cholecystectomy, etc) | 53 | (34) | 29 | (19) | 82 | (27) |
| Essential trauma procedures (e.g. skin grafting, external fixation of fractures, etc) | 7 | (4.5) | 10 | (6.7) | 17 | (5.6) |
| Essential procedues for congenital conditions (e.g., psarp, cleft lip/palate repair, etc) | 2 | (1.3) | 4 | (2.7) | 6 | (2.0) |
| Essential ObGyn (C-section and myomectomy) | 2 | (1.3) | 0 | (0) | 2 | (0.7) |
| Other general surgical procedures (e.g., soft tissue excision biopsy, mastectomy, thyroidectomy, laparotomy, etc) | 59 | (38) | 39 | (26) | 98 | (32) |
| Other urology procedures (e.g., prostatectomy, urethroplasty, hypospadias repair, orchidopexy, etc) | 20 | (13) | 30 | (20) | 50 | (16) |
| Other orthopedic procedures (e.g., orif, corrective osteotomy, arthroplasty, syndactyly separation, etc) | 6 | (3.9) | 28 | (19) | 34 | (11) |
| Other neurosurgical procedures (e.g., vp shunt surgery, laminectomy, repair of neural tube defect, etc) | 2 | (1.3) | 6 | (4.0) | 8 | (2.6) |
| Other cardiothoracic procedures (e.g., valve replacement, vsd closure, pda ligation, etc) | 3 | (1.9) | 4 | (2.7) | 7 | (2.3) |
| Emergency surgeries | 153 | (100) | 152 | (100) | 305 | (100) |
| Essential general surgical procedures (e.g. appendectomy, repair of complicated hernia, repair of perforated hollow viscus, etc) | 118 | (77) | 83 | (55) | 201 | (66) |
| Essential trauma procedures (e.g. suturing lacerations, external fixation of fractures, burr holes, etc) | 13 | (8.5) | 17 | (11) | 30 | (9.8) |
| C-section | 3 | (2.0) | 0 | (0) | 3 | (1.0) |
| Other urology procedures (e.g., prostatectomy, testicular detorsion, urethroplasty, etc) | 9 | (5.9) | 18 | (12) | 27 | (8.9) |
| Other orthopedic procedures (e.g., orif, nerve/vascular repairs, arthroscopy, etc) | 5 | (3.3) | 19 | (13) | 24 | (7.9) |
| Other neurosurgical procedures (e.g., craniotomy, laminectomy, vp shunt surgery, etc) | 0 | (0.0) | 8 | (5.3) | 8 | (2.6) |
| Other general surgical procedures (e.g., amputations) | 3 | (2.0) | 3 | (2.0) | 6 | (2.0) |
| Cardiothoracic procedures (e.g., aortic aneurysm repair, thoracotomy, pacemaker implantation, etc) | 1 | (0.7) | 3 | (2.0) | 4 | (1.3) |
| Other pediatric surgical procedures (e.g., intestinal atresia repair) | 1 | (0.7) | 1 | (0.7) | 2 | (0.7) |
psarp - posterior sagittal anorectoplasty, orif – open reduction and internal fixation, vp shunt – ventriculo-peritoneal shunt,
vsd – ventricular septal defect, pda – patent ductus arteriosus
Each respondent could list up to 3 of their most commonly performed procedures. The above numbers and percents are based on total number of answers. Some respondents listed less than 3 operations. Elective and emergency operations were asked separately.
Ninety-two (79%) participants reported being engaged in teaching/training. They provided teaching services for medical students (69; 59%), nursing students (37; 32%), and students of other allied health professions (56; 48%).
Almost half (54; 46%) of the participants reported being engaged in research activities yielding a mean of four peer-reviewed journal publications (range: 1-10 publications), four oral/poster presentations at national/international conferences (range: 1-28 presentations) and three newspaper/magazine articles (range: 1-10 articles) (Table 1).
One in three participants reported holding an administrative office at their current hospital. Positions they held included being the head of surgical departments/units (19; 16%) where they reported overseeing unit operations by making schedules, providing protocols, training staff, and monitoring clinical performance. Others were medical superintendent/directors of the hospital (11; 9%) with responsibilities of leading the hospital’s management team, overseeing hospital operations, and making financial decisions for the hospital. The rest were clinical coordinators or members of hospital management boards (9; 8%). Participants, however, mostly engaged in clinical care, spending an average of 70% of their time providing clinical service (range: 5%-100%). They also spent on the average 15% (range: 0%-40%), 8% (range: 0%-85%) and 7% (0%-50%) of their time fulfilling teaching/training commitments, conducting research and performing administrative duties respectively.
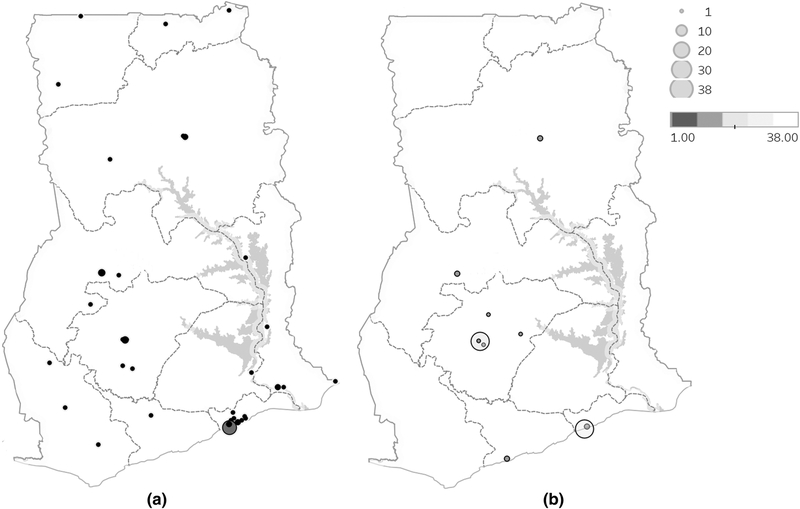
Current practice: member vs fellow.
As noted in the introduction, the GPCS graduates are either members (who have 3 years of surgical training after housemanship (internship) and all of whom are general surgeons) or fellows (who have a total of 5-6 years of surgical training after housemanship, some of whom become university faculty, and many of whom are sub-specialized). Members tended to be more widely distributed. Only 24% of members were currently in the two biggest cities (Accra and Kumasi) with 76% in areas of higher need (Figure 2). Conversely, 86% percent of fellows or fellows in training were currently in the two biggest cities (p<0.001).
Figure 2.
Location of hospitals where Ghana College-trained surgeons currently practice. (A) Surgeons who only hold memberships; (B) Surgeons who hold fellowships/fellows in training.
Size of circles shows number of doctors at particular hospital; Colors of circle shows number of doctors at particular hospital
Members performed more elective operations (mean: 8; range: 1-25) than fellows or fellows in training (mean: 6; range 2-18) (p=0.02). However, they performed similar numbers of emergency operations as fellows or fellows in training (mean: 6; range 1-20 vs mean: 7; range 2-18, p=0.28)
Members also tended to provide higher percentages of essential surgical care. Among the reported top three elective surgical procedures, surgeons with memberships performed more essential procedures than fellows or fellows in training (42% vs 29%, p=0.009). Similarly, they performed more essential emergency procedures than fellows or fellows in training (88% vs 66%, p<0.001) (Table 2).
Other community service
Most participants (63; 54%) reported that they regularly engaged in community service, providing health education and advocacy via radio talks and town hall meetings, health screening, and surgical outreach programs to communities with less access to surgical care. Furthermore, they reported collaboration with international organizations which support their work by periodically providing extra training and specialized surgical care at their hospitals, providing equipment, or helping with financial support for patients.
Changes brought by participants to their hospitals
Participants reported various changes they had brought to their hospitals. These included improved revenue generation through introduction or expansion of surgical services and reduction in outward referrals. Other changes were improved quality of clinical services provided through quality improvement activities and improved patient outcomes resulting in increased patient satisfaction; creation of better academic environment and mentorship programs; and improved public engagement through increased health education and advocacy (Table 3).
Table 3.
Recent changes brought to participants’ hospitals and suggestions to reduce the burden of surgical conditions as reported by participants.
| Changes brought to participants’ hospitals | |
|---|---|
| Theme | Examples of changes reported |
| Improved revenue for hospital | Introduced/expanded variety of surgical services |
| Increased surgical volume | |
| Reduced referrals to other hospitals | |
| Expanded hours of hospital operation at full skill capacity | |
| Improved clinical quality | Case auditing |
| Improved surgical techniques | |
| Improved emergency/trauma surgery capacity | |
| Improved core outcomes (e.g. mortality, morbidity, SSI) | |
| Introduced quality improvement activities | |
| Improved patient satisfaction / attendance | |
| Improved administrative operations for hospital | Hospital efficiency |
| Improved patient flow (reduced wait times, reduced surgical cancellations) | |
| Improved record keeping | |
| Leadership/hospital administration | |
| Changed organizational operations (improving / founding new departments/teams/units) | |
| Fostered academic environment and mentorship | Increased research culture |
| Improved academic environment | |
| Teaching / continuous training of staff/trainees | |
| Inspired other doctors to specialize in surgical field | |
| Improved facilities | Procured necessary equipment, supplies |
| Influenced development of surgery-specific facilities | |
| Improved public engagement | Increased public health education and advocacy |
| Suggestions to reduce burden of surgical conditions in Ghana | |
|---|---|
| Theme | Examples of suggestions |
| Patient-focused interventions (education, prevention, access) | Early detection of disease |
| Improving patient access to appropriate health facility | |
| Patient education on surgical conditions | |
| Patient education on preventive / early care | |
| Increase patient trust in surgeons / surgery | |
| Increase surgical outreach programs | |
| Make surgery affordable | |
| Increase funding | Increase funding for post-graduate training |
| Incentivize specialization | |
| Increase incentives to practice surgery in rural districts | |
| Improve remuneration for surgeons | |
| Incentivize surgeons to perform elective cases | |
| Surgical training / education | Make it easier for doctors to enter post graduate training early |
| Remove sponsorship requirement to encourage training of more surgeons | |
| Improve surgeon training to allow trainees gain more skills faster | |
| Encourage sub-specialization early on | |
| Encourage continuous professional development | |
| Decentralization of services, training, and personnel | Encourage more district outreach programs |
| Institute surgical training at district hospitals via on-site mentorship | |
| Assign consultants to oversee running of surgical units at district hospital | |
| Encourage more surgeons to accept district postings | |
| Increase number of sites for district rotations during training | |
| Train surgeons appropriately based on types of cases seen at district level | |
| Infrastructure / Resources | Improve infrastructure and equipment in rural and urban hospitals |
| Surgical personnel | Train more surgeons |
| Government interventions | Strengthen national health insurance coverage of surgical pathologies |
| Enforce legislation to combat herbalists who delay and worsen surgical pathology | |
Suggestions to reduce the burden of surgical conditions in Ghana
Participants offered suggestions on how to reduce the nation’s large burden of surgical conditions. These included more patient education and advocacy and increased access and funding for surgical training. Other suggestions included decentralization of surgical services, including institution of surgical training at district hospitals through on-site mentorship, encouraging more surgeons to accept district postings and strengthening national health insurance coverage of surgical conditions(Table 3).
Discussion
The Lancet Commission on Global Surgery has recommended at least 5,000 operations per 100,000 population at which LMICs could realize most of the population-wide benefits of surgery.[11] Ghana currently performs 869 operations per 100,000 annually, confirming the country’s large unmet need for surgery.[6] Improving the surgeon-to-population ratio will likely increase Ghana’s surgical rate towards this benchmark. The GCPS was established to train surgeons and specialist physicians in-country, in part, to overcome the shortage of specialists and stem the high attrition rate of medical practitioners sponsored for postgraduate training abroad.[5] In this study, we aimed to assess the effectiveness of the GCPS in meeting these goals by determining the in-country retention rate of surgeons trained by the GCPS and their contributions to the goal of reducing the unmet need for surgery in Ghana. The GCPS had trained 146 surgeons to date with a high retention rate. The surgeons were better distributed in the country than before their training. They performed a wide variety of operations, with essential surgical procedures being more common. They were also engaged in training of other medical personnel, provided other services to the community, and were contributing positively to the growth of their hospitals.
Surgical capacity building in LMICs has been undermined by an inadequate workforce, a major contributor being the emigration of health workers from LMICs.[12] We found a high retention rate of 87%-97% among GCPS-trained surgeons. There is other evidence to suggest that training LMIC surgeons in-country leads to high retention rates. Recent work from 10 countries in the East, Central and Southern Africa region showed that 1,038 surgeons had been trained locally from 1974 to 2013 with 85% of surgeons retained in the countries where they trained and 88% retained in the region.[13] By comparison, previously, only 10% of Ghanaian obstetricians who trained abroad were found to have returned to Ghana.[1]
GCPS-trained surgeons were widely distributed within the country, with 44% in the higher need areas outside the two biggest cities. Also, a significant proportion of the procedures they performed were in the DCP-3 “essential” category, deemed to likely have the highest population-wide impact.[9]
There were interesting differences between the two tiers (members, fellows) of surgeons. In addition to performing a higher proportion of essential procedures, members were more widely geographically disseminated, especially in underserved areas. These factors indicate that the members were meeting more of the population needs and likely having more of an effect on the burden of surgical disease. However, while in the short-term, training more members leads to greater population-wide impact, in the long-term, training more fellows leads to a greater capacity to train more surgeons (members and fellows). These considerations are similar to ongoing discussions about non-physician surgical providers vs doctor-level providers or non-surgeon physicians performing surgery vs surgeons.[9, 14] It is important to have adequate numbers of both fellowship- and membership-level graduates to ensure sustained production of surgeons as well as geographical spread in-country to meet population needs. But to the extent that resources are limited, the differential contributions of the two tiers need to be considered during planning.
The high prevalence of unmet surgical needs in many LMIC communities is the result of many barriers to care that these communities face.[2-4] Community education and advocacy as reported by GCPS-trained surgeons will reduce such barriers and facilitate early presentation of surgically-correctable conditions. In addition, the quality of service provided by GCPS-trained surgeons is reducing the barrier of acceptability where patients are now inclined to prefer surgery to non-orthodox management. This has consequently boosted hospital attendances as reported by many participants.
Additionally, participants reported engaging in periodic surgical outreach to especially underserved areas. They usually provided these services in collaboration with international organizations including Operation Smile, Operation Hernia, and WACS but also with local entities such as Hernia Society of Ghana and ApriDec Medical Outreach Group. Surgical outreach missions have been recognized as one short-term approach to addressing the large unmet need for surgery in LMIC communities.[15] The increased involvement of GCPS-trained surgeons in such activities provides a local, cost-effective, solution to the problem.[16]
GCPS-trained surgeons also reported their involvement in training of other providers including doctors, nurses and physician assistants. Such ongoing training is helping build capacity of other providers involved in patient care. In Ghana, 54% of district hospitals are not staffed by fully-trained surgeons. However, these hospitals lacking fully-trained surgeons perform 36% of all operations performed by district hospitals.[6] The training and supervisory role played by GCPS-trained surgeons in this regard is absolutely critical, if Ghana’s large unmet need for surgery will be reduced, especially at the district level with fewer fully-trained surgeons.
Despite the mostly positive data reported above, one item that could be improved upon is gender equity, as majority (90%) of GCPS-trained surgeons are men. A second item that could probably be improved was the level of operative productivity. The mean of 13 operations per week is a good level of productivity. By comparison, general surgeons in the United States were estimated to perform 8-9 operations per week.[17] However, some of the Ghanaian surgeons performed as little as one elective and one emergency operation each week, indicating a very low level of operative productivity, and an underutilization of this valuable human resource. Similar low productivity has been reported for the surgical workforce in Sierra Leone, with an average of 3 operations per provider per week.[18] Better understanding and addressing limiting factors such as availability of physical resources (equipment and supplies) and of human resources (such as operating room staff) would help to increase utilization of the surgical workforce.
Prior to drawing conclusions from the study, the following limitations must be considered. First, the study was limited by a 20% non-response rate. However, the experiences of those who remained in Ghana after graduation are not expected to be very different from the graduates who participated. Second, quality of care and outcomes were not assessed. Third, the veracity of respondents’ answers, especially as regards types of operations performed, could not be independently validated. However, the overall distribution of types of cases reported is similar to a recent assessment of all operations performed nationwide.[6] Despite these limitations, this study allows us to draw reasonable conclusions about the effectiveness of the training provided by the GCPS and about ways to further increase this effectiveness.
Conclusion
Training surgeons in Ghana through the GCPS has led to high retention rates and produced surgeons spread widely around the country playing key roles in terms of clinical practice, training, administration, and community engagement. Through these roles, they are contributing positively to reducing the large unmet need for surgery in Ghana. This demonstrates the importance of devoting adequate resources to this type of capacity building. This study has also defined the different contributions of the lower tier and higher tier of surgeons; the former performing more operations with the highest population-wide impact and the latter doing more difficult operations and serving as trainers. Both levels are important, but in the context of limited resources, the differential contributions of the two tiers need to be taken into account in planning.
Acknowledgments:
The authors wish to thank all the surgeons who participated in the study. Because of the sensitive nature of the data collected for this study, requests to access the data set from qualified researchers trained in human subject confidentiality protocols may be sent to the corresponding author.
Grant support: This study was funded in part by grant D43TW007267 from the Fogarty International Center, US National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix: Survey tool
Background info
-
1.
Sex: M=1, F=2
-
2.
Age:
-
3.
Are you currently a member or fellow of the college? Member=1, Fellow=2
-
4.
What is your nationality?
-
5.
In which country did you attend medical school?
-
6.
Which year did you graduate from medical school?
-
7.
Which hospital did you used to work before starting your membership?
Name= ; Place=
Training
-
8.
In which hospital did you do your membership?
-
9.
Which year did you start your membership training?
-
10.
Which year did you complete your membership training?
-
11.
Which hospital did you used to work before starting your fellowship?
Name= ; Place=
-
12.
In which hospital did you do your fellowship?
-
13.
Which year did you start your fellowship program?
-
14.
Which year did you complete your fellowship?
-
15.
What discipline did you pursue during fellowship?
Practice
-
16.
At which hospital do you presently work?
Name= ; Place=
-
17.
Who is currently your primary employer?
Ministry of health=1, Ghana health service=2, CHAG=3, UGMS=4, KNUST-SMS=5, UDS- SMHS=6, UCC-SMS=7, Private=8, Ministry of defense or Interior=9, other=10
-
18.
Are you currently engaged in active clinical service? No=0, Yes=1
-
19.
How many outpatients do you see, on the average, per week?
-
20.
How many elective surgeries do you perform, on the average, per week?
-
21.
What are the top 3 elective surgeries you perform?
-
22.
How many emergency patients do you see, on the average, per week?
-
23.
How many emergency surgeries do you perform, on the average, per week?
-
24.
What are the top 3 emergency surgeries you perform?
-
25.
Are you currently engaged in teaching? No=0, Yes=1
-
26.
Medical students? No=0, Yes=1
-
27.
Nursing students? No=0, Yes=1
-
28.
Other Allied health students? No=0, Yes=1
-
29.
Are you a full time or part-time lecturer? Full time=1, Part-time=2
-
30.
Are you currently engaged in active research? No=0, Yes=1
-
31.
How many peer-reviewed articles have you published since graduation?
-
32.
How many oral presentations at national or international conferences have you made since graduation?
-
33.
How many poster presentations at national or international conferences have you made since graduation?
-
34.
How many other articles (newspaper, magazine etc) have you authored since graduation?
-
35.
Are you currently engaged in administration of your hospital or unit? No=0, Yes=1
-
36.
If yes, what position do you hold?
-
37.
Please briefly describe what your administration duties are?
-
38.
What percentage of your current working time do you spend doing the following?
Clinical service - %; Teaching - %; Research - %; Administration - %
-
39.
Do you still have a continuous relationship with the institution where you trained?
No=0, Yes=1
-
40.
If yes, please briefly describe what kind of relationship you have?
Impact
-
41.
Are you engaged in community service (in person or via radio or TV)? No=0, Yes=1
-
42.
If yes, briefly describe your activities
-
43.
Do you work with any community-based organization? No=0, Yes=1
-
44.
Please name them?
-
45.
If yes, briefly describe your activities
-
46.
Do you work with any national and international organizations? No=0, Yes=1
-
47.
Please name them?
-
48.
If yes, briefly describe your activities
-
49.
Are you the first surgeon at your current place of work? No=0, Yes=1
-
50.
What changes have occurred at your current work place because of your joining?
-
51.
How do you think the large burden of essential surgical conditions may be reduced in Ghana?
Thank you for your time.
Footnotes
Conflicts of interest: The authors declare no competing interest in any form related directly or indirectly to the subject of this article.
Contributor Information
Adam Gyedu, Department of Surgery; School of Medical Sciences; Kwame Nkrumah University of Science and Technology, Kumasi, Ghana, University Hospital, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana, drgyedu@gmail.com.
Sam Debrah, Department of Surgery; School of Medical Sciences; University of Cape Coast, Cape Coast, Ghana, sdebrah@aol.com.
Kwabena Agbedinu, Directorate of Surgery; Komfo Anokye Teaching Hospital, Kumasi, Ghana, agbeypapa@yahoo.com.
Stephanie K Goodman, Standford Children’s Health, Palo Alto, California, USA, stephaniekgoodman@gmail.com.
Jacob Plange-Rhule, Ghana College of Physicians and Surgeons, Accra, Ghana, jprhule@gmail.com.
Peter Donkor, Department of Surgery; School of Medical Sciences; Kwame Nkrumah University of Science and Technology, Kumasi, Ghana, petadonkor@yahoo.com.
Charles Mock, Harborview Injury Prevention & Research Center, Seattle, WA, USA, Department of Surgery, University of Washington, Seattle, WA, USA, cmock@u.washington.edu.
References
- 1.Anderson FWJ, Obed SA, Boothman EL et al. (2014) The Public Health Impact of Training Physicians to Become Obstetricians and Gynecologists in Ghana. American Journal of Public Health 104(Suppl 1):S159–S165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gyedu A, Abantanga F, Boakye G et al. (2016) Barriers to essential surgical care experienced by women in the two northernmost regions of Ghana: a cross-sectional survey. BMC Womens Health 16:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart BT, Gyedu A, Abantanga F et al. (2015) Barriers to Essential Surgical Care in Low- and Middle-Income Countries: A Pilot Study of a Comprehensive Assessment Tool in Ghana. World journal of surgery 39(11):2613–2621. [DOI] [PubMed] [Google Scholar]
- 4.Gyedu A, Boakye G, Dally CK et al. (2017) Assessment of Barriers to Essential Surgical Care in Two Communities in the Upper West Region, Ghana. J Health Care Poor Underserved 28(1):175–190. [DOI] [PubMed] [Google Scholar]
- 5.Ghana College of Physicians and Surgeons. Accra. 2014. [1 January, 2017]; Available from: https://gcps.edu.gh/?page_id=3279.
- 6.Gyedu A, Stewart B, Gaskill C et al. (2017) Improving Benchmarks for Global Surgery: Nationwide Enumeration of Operations Performed in Ghana. Ann Surg 268(2):282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The World Bank Group. World Development Indicators. 2017; Available from: http://data.worldbank.org/indicator.
- 8.Zakariah A, Degbotse D, Osei D et al. Holistic Assessment of the Health Sector Programme of Work 2013. Accra, Ghana: Ghana Ministry of Health 2014. [Google Scholar]
- 9.Debas H, Donkor P, Gawande A et al. , editors. Essential Surgery Disease Control Priorities. 3rd ed. Washington, DC: World Bank; 2015. [PubMed] [Google Scholar]
- 10.Bradley EH, Curry LA, Devers KJ (2007) Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health services research 42(4):1758–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meara JG, Leather AJ, Hagander L et al. (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624. [DOI] [PubMed] [Google Scholar]
- 12.Myles PS, Haller G (2010) Global distribution of access to surgical services. Lancet 376(9746):1027–1028. [DOI] [PubMed] [Google Scholar]
- 13.Hutch A, Bekele A, O'Flynn E et al. (2017) The Brain Drain Myth: Retention of Specialist Surgical Graduates in East, Central and Southern Africa, 1974-2013. World journal of surgery 41(12):3046–3053. [DOI] [PubMed] [Google Scholar]
- 14.Bolkan HA, van Duinen A, Waalewijn B et al. (2017) Safety, productivity and predicted contribution of a surgical task-sharing programme in Sierra Leone. The British journal of surgery 104(10):1315–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World journal of surgery 32(4):533–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gyedu A, Gaskill C, Boakye G et al. (2017) Cost-Effectiveness of a Locally Organized Surgical Outreach Mission: Making a Case for Strengthening Local Non-Governmental Organizations. World journal of surgery 41(12):3074–3082. [DOI] [PubMed] [Google Scholar]
- 17.Ritchie WP Jr., Rhodes RS, Biester TW (1999) Work loads and practice patterns of general surgeons in the United States, 1995-1997: a report from the American Board of Surgery. Ann Surg 230(4):533–542; discussion 542-533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolkan HA, Hagander L, von Schreeb J et al. (2016) The Surgical Workforce and Surgical Provider Productivity in Sierra Leone: A Countrywide Inventory. World journal of surgery 40(6):1344–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]