Abstract
Background:
Currently, most US states have adopted legislation requiring hospitals to submit healthcare-associated infection (HAI) data. We evaluated the perceived impact of state HAI laws on infection prevention and control (IPC) departments.
Methods:
Web-based survey of a national sample of all non-VA hospitals enrolled in the National Healthcare Safety Network was conducted in Fall 2011. Variations in IPC department resources and characteristics in states with and without laws were compared using χ2, Wilcoxon-Mann-Whitney and Student’s t tests. Multinomial logistic regression was used to identify increases or decreases, versus no change, in perceived resources, time, influence and visibility of the IPC department in states with and without HAI laws.
Results:
1,036 IPC departments provided complete data (30% response rate); 755 (73%) were located in states with laws. Respondents in states with reporting laws were more likely to report less time for routine IPC activities and less visibility of the IPC department (OR=1.61, 95% CI 1.12–2.31 and OR=1.70, 95% CI 1.12–2.58, respectively) than respondents in states without laws, after controlling for geographic region, setting and the presence of a Hospital Epidemiologist.
Conclusion:
Respondents in states with laws reported negative effects on their IPC department, beyond what was required by federal mandates. Further research should examine resources necessary to comply with state HAI laws, and evaluate unintended consequences of state HAI laws.
INTRODUCTION
Healthcare-associated infections (HAI) result in significant morbidity, mortality and costs in the acute care setting (1). In the past 15 years, policy makers have instituted a variety of federal and state policies and initiatives in an effort to improve patient safety and increase transparency and accountability (2–3). For example, federal mandates currently require hospitals to report HAIs through the Centers for Medicare & Medicaid Services’ Hospital Inpatient Quality Reporting Program (3). On the state level, the majority of US states and territories have adopted legislation requiring HAI data submission to their health departments (2,4).
The evidence that state-mandated reporting laws have increased patient safety and improved process and outcome measures is inconsistent (5). Studies examining the association between state HAI laws and HAI rates have found mixed-results and have mostly been focused on examining the impact on rates of central line associated bloodstream infections (CLABSI) (5–9). A cross-sectional, national study using data from 159 hospitals found that HAI laws did not impact CLABSI rates (6). However, another study of CLABSI rates showed a larger decline in Pennsylvania as compared with control states without HAI laws (8). Using national, longitudinal data, we found that controlling for the overall time trend, Intensive Care Units (ICUs) in states with HAI reporting laws had lower CLABSI rates as compared to ICUs in states without HAI reporting laws (9).
Several researchers have examined the impact of state HAI laws on infection prevention and control (IPC) departments and the Infection Preventionists (IPs) who are charged with fulfilling these mandates and have found that the resources needed to comply with reporting mandates are considerable (10–13). Concerns have also been raised that mandatory reporting may have important unintended consequences (14) such as diverting scarce resources away from infection prevention and control and toward fulfilling reporting requirements (15). A recent ethnographic study of IPC departments conducted by Szymczak and colleagues found three unintended consequences of public reporting including decreased credibility of hospital IP staff, staff focusing on inconsistencies in infection definitions instead of focusing on gaps in practice, and perceptions that other hospitals are likely to engage in gaming of reported infection data (16).
Apart from the evidence generated in these single-state and qualitative studies, there has been no large, nationally representative study evaluating the impact of state HAI laws on IPC departments. The aim of this study was to evaluate differences in IP perceptions of resources, available time for infection prevention and control, and influence and visibility of the IPC department between hospital in states with and without HAI reporting mandates.
METHODS
This secondary analysis was part of a larger study, Prevention of Nosocomial Infections and Cost Effectiveness Refined (P-NICER; NINR R01NR010107) which is described in detail elsewhere (17). Briefly, in Fall 2011, a web-based survey was sent to the IPC departments of non-veteran hospitals enrolled in the National Healthcare Safety Network (NHSN). Participants were asked to indicate how mandatory reporting has affected the following: 1) resources to department to assist infection control, 2) time for routine infection control activities besides mandatory reporting, 3) influence of the IPC Department on hospital decision making, and 4) visibility of the IPC Department. The answer choices for each questions were as follows: 1 = much less, 2 = slightly less, 3 = about the same, 4 = slightly more, 5 = much more. For the analysis, the answer choices were combined into three categories: “more,” “less,” or “the same.”
The survey also collected the following data on the characteristics of the IPC department: geographic region (i.e., Northeast, Midwest, West and South), setting (i.e., urban, suburban, rural), number of beds, presence of physician hospital epidemiologist, at least one IP certified in infection control (CIC), and participation in an HAI reduction initiative. Additional information on hospital and IPC department characteristics was obtained from a subset of participating hospitals that provided the research team with access to their NHSN annual survey data. These data included information on type of hospital (i.e., general, other), ownership status (i.e., profit, including government and physician owned, and not for profit), medical school affiliation, number of patient days and patient admissions in 2011.
States and territories with HAI laws (for at least one HAI) with effective dates prior to Fall 2011 were identified using systematic legal review for all US states, the District of Columbia, and Puerto Rico (2). State HAI coordinators were contacted to validate the accuracy of the information collected and to provide missing information.
Variations in IPC department and hospital characteristics in states with and without HAI laws were assessed using χ2, Student’s t, or Wilcoxon-Mann-Whitney tests, as appropriate. Multinomial logistic regression was used to evaluate perceived increases or decreases (versus no change) in department resources, time, influence, and visibility in states with and without HAI laws. These models were adjusted for hospital and IPC department characteristics found to be associated with mandatory reporting (P <0.10) (i.e. geographic region, setting, presence of a hospital epidemiologist). Two secondary analyses were conducted. First, we incorporated clustering by state to account for unmeasured state-level dependence. Second, we compared the perceived impact of state mandates between IPs from hospitals in states that mandate state reporting through NHSN versus IPs from hospitals in states that require reporting through a different reporting mechanism. Analyses were conducted using Stata, Version 11 (College Station, TX). This study was approved by the Institutional Review Boards at Columbia University Medical Center and RAND Corporation.
RESULTS
Completed surveys were received from 1064 hospitals (out of 3374 hospitals, 29% response rate). Of these, 1036 provided complete data on how mandatory reporting impacted their IPC department. Additionally, NHSN annual survey data from 2011 were available for 710 of those hospitals. The majority of hospitals (n=755, 73%) were located in states with HAI reporting laws. Of these, 598 (79%) were located in states that specifically required reporting of HAI data to NHSN at the time the survey was conducted.
Characteristics of hospitals in states with and without HAI laws are summarized in Table 1. Hospitals in states with laws were more likely to be located in the Northeast, in either urban or suburban settings, to employ a full- and/or part-time physician hospital epidemiologist, and to have a greater number of admissions and patient days in 2011 compared to hospitals in states without laws (P < 0.01). Bed size, IP certification, participation in HAI reduction initiatives, being part of a larger system that shares IP resources, hospital type, ownership status, and medical school affiliation were not associated with being in a state with HAI laws.
Table 1.
Infection prevention and control department resources and characteristics in hospitals located in states with and without healthcare-associated infection laws
| No. (%) of hospitals | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Hospital characteristics | Hospitals in states with laws (n=755) | Hospitals in states without laws (n=281) | Total (n=1036) | P | |||||
| Geographic region | <0.0001 | ||||||||
| Northeast | 189 (25.0) | 0 | 189 (18.2) | ||||||
| Midwest | 150 (19.9) | 138 (49.1) | 288 (27.8) | ||||||
| West | 129 (17.1) | 47 (16.7) | 176 (17.0) | ||||||
| South | 287 (38.0) | 96 (34.2) | 383 (36.8) | ||||||
| Setting, n=1030 | 0.004 | ||||||||
| Urban | 206 (27.4) | 61 (21.9) | 267 (25.9) | ||||||
| Suburban | 257 (34.2) | 79 (28.3) | 336 (32.6) | ||||||
| Rural | 288 (38.4) | 139 (49.8) | 427 (41.5) | ||||||
| Number of beds, n=1008 | 0.117 | ||||||||
| ≤200 | 387 (52.9) | 166 (60.1) | 553 (54.9) | ||||||
| 201 – 500 | 268 (36.6) | 85 (30.8) | 353 (35.0) | ||||||
| >500 | 77 (10.5) | 25 (9.1) | 102 (10.1) | ||||||
| Presence of full- and/or part-time physician hospital epidemiologist, n=1016 | 384 (51.7) | 117 (42.9) | 501 (49.3) | 0.013 | |||||
| At least one IP certified in | 368 (63.2) | 123 (58.9) | 491 (62.1) | 0.263 | |||||
| infection control, n=791 | |||||||||
| Part of a larger hospital system that shares IP resources, n=1022 | 211 (28.4) | 93 (33.5) | 304 (29.8) | 0.113 | |||||
| Participates in HAI reduction initiative | 501 (66.4) | 185 (65.8) | 686 (66.2) | 0.875 | |||||
| Hospital type, n=710 | 0.933 | ||||||||
| General | 504 (95.5) | 174 (95.6) | 678 (95.5) | ||||||
| Other (Children’s or Specialty) |
24 (4.6) | 8 (4.4) | 32 (4.5) | ||||||
| Ownership status, n=710 | 0.669 | ||||||||
| Profit (includes government and physician owned) | 128 (24.2) | 47 (25.8) | 175 (24.7) | ||||||
| Not for profit | 400 (75.8) | 135 (74.2) | 535 (75.4) | ||||||
| Affiliated with a medical school, n=710 | 200 (37.9) | 58 (31.9) | 258 (36.3) | 0.146 | |||||
| Number of patient days in 2011, n=707 | 0.014 | ||||||||
| <37,000 | 250 (47.6) | 106 (58.2) | 356 (50.4) | ||||||
| ≥37,000 | 275 (52.4) | 76 (41.8) | 351 (49.7) | ||||||
| Number of admissions in 2011, n=707 | 0.013 | ||||||||
| <8,000 | 243 (46.2) | 103 (56.9) | 346 (48.9) | ||||||
| ≥8,000 | 283 (53.8) | 78 (43.1) | 361 (51.1) | ||||||
| Number of hours per week spent fulfilling reporting requirements, mean (SD) | 16.9 (17.1) | 12.4 (12.9) | 15.7 (16.2) | <0.0001 | |||||
Notes: p-values were estimated using χ2, Student’s t, and Wilcoxon-Mann-Whitney tests, as appropriate; Denominators less than 1036 are indicated; HE = hospital epidemiologist; IP = infection preventionist; HAI = healthcare-associated infections
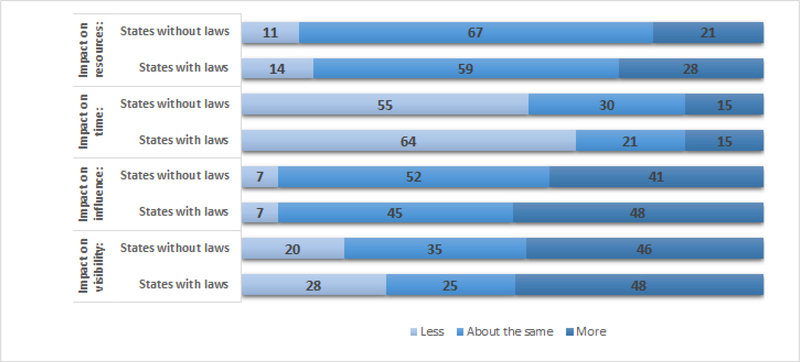
The perceived impact of mandatory reporting on resources, time, influence and visibility of the IPC department in hospitals in states with and without HAI reporting laws is summarized in Figure 1. IPs in states with HAI laws reported more resources available to assist with infection control (28% vs. 21%), and more influence of the department on hospital decision-making (48% vs. 41%) as compared to IPs in states without HAI laws. Conversely, IPs in states with HAI laws reported less time for routine infection control activities (64% vs. 55%) and less visibility of the department (28% vs. 20%).
Figure 1.
Perceived impact of mandatory reporting on resources, time, influence, and visibility in hospitals located in states with and without healthcare-associated infection laws
The numbers indicate the proportion of participants endorsing one of the three response categories (less, about the same, more) when asked to indicate how mandatory reporting has affected the following: 1) resources to department to assist infection control, 2) time for routine infection control activities besides mandatory reporting, 3) influence of the infection prevention and control department on hospital decision making, and 4) visibility of the infection prevention and control department.
These differences in perceptions were further explored using unadjusted multinomial models to evaluate increases or decreases (versus no change) in department resources, time, influence, and visibility in states with and without HAI laws (Table 2). In the unadjusted models, IPs in states with reporting laws were more likely to report having more resources to assist with infection control (OR=1.49, 95% CI 1.07–2.08) and more influence in hospital decision making (OR=1.36, 95% CI 1.03–1.82), but less time for routine infection control activities (OR=1.62, 95% CI 1.17–2.23) as compared to IPs in states without HAI laws. After adjusting for geographic region, setting, and presence of a hospital epidemiologist (Table 2), IPs in states with HAI laws were more likely to report having less time for routine infection control activities (OR=1.61, 95% CI 1.12–2.31) and less visibility of the department within the hospital (OR=1.70, 95% CI 1.12–2.58) as compared to IPs in states without HAI laws.
Table 2.
Unadjusted and Adjusted Analyses of perceived impact of mandatory reporting on resources, time, influence, and visibility
| Unadjusted | Adjusted* | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Resources to assist with infection control | ||||||
| Less vs. Same | 1.44 | 0.93, 2.21 | 0.099 | 1.37 | 0.85, 2.20 | 0.197 |
| More vs. Same | 1.49 | 1.07, 2.08 | 0.019 | 1.39 | 0.96, 2.01 | 0.078 |
| Time for routine infection control activities | ||||||
| Less vs. Same | 1.62 | 1.17, 2.23 | 0.003 | 1.61 | 1.12, 2.31 | 0.010 |
| More vs. Same | 1.41 | 0.91, 2.18 | 0.127 | 1.37 | 0.84, 2.25 | 0.208 |
| Influence in hospital decision making | ||||||
| Less vs. Same | 1.23 | 0.71, 2.15 | 0.463 | 1.26 | 0.69, 2.30 | 0.448 |
| More vs. Same | 1.36 | 1.03, 1.82 | 0.033 | 1.28 | 0.94, 1.76 | 0.121 |
| Visibility | ||||||
| Less vs. Same | 1.98 | 1.35, 2.91 | 0.000 | 1.70 | 1.12, 2.58 | 0.013 |
| More vs. Same | 1.47 | 1.07, 2.02 | 0.016 | 1.34 | 0.94, 1.90 | 0.104 |
Adjusted for geographic region, setting, and presence of any Hospital Epidemiologist
In unadjusted analysis, IPs in states with HAI laws reported spending more hours per week fulfilling reporting requirements as compared to IPs in states without HAI laws (on average, 16.9 vs. 12.4; P <0.0001). However, the results were no longer statistically significant after adjusting for geographic region, setting and presence of a hospital epidemiologist (OR = 2.18, 95% CI −0.17–4.52, P = 0.068). The results were similar upon adjustment for number of hospital admissions and patient days and/or for state-level clustering (data not shown). Among states with HAI laws, there were no perceived differences in resources, time available for routine infection control activities, and influence and visibility of the IPC department when comparing states that were required to report to NHSN as opposed to a state entity.
DISCUSSION
Our study evaluated the impact of mandatory reporting laws on IP perceptions of hospital resources, available time for infection control, and influence and visibility of the IPC department. In recent years, the role of the IP has been changing due to shifts in the healthcare system and demand for quality care and transparency of outcomes in healthcare. Published studies have reported that on, average, IPs spent half of their time in their offices and on surveillance activities (17–18). The need to fulfill reporting mandates and increased shift to additional surveillance activities has an important impact on the traditional role of the IP, potentially diverting IPs from activities such as education and prevention to increased surveillance and administrative work (19).
We found that IPs in states with reporting laws perceived that they had less time for routine IPC activities. To meet the additional burden that reporting requires, IPs did report receiving increased resources to offset increased demands on time for routine activities. However, our study did not specifically quantify how many additional resources were received or examine whether the increase in resources was sufficient to effectively comply with reporting requirements. Previous qualitative work indicates that although IPC departments have received additional staffing resources in recognition of additional IP responsibilities, these resources have not increased in proportion to the increase in demand on IP time (19).
Surprisingly, our findings suggest that IPs in states with HAI reporting laws were more likely to report less visibility of the IPC department within the hospital as compared to states without HAI reporting laws. This is in contrast to findings from our earlier qualitative work, where we found that mandatory reporting had a positive effect on hospital administrators in recognizing the importance of infection prevention in their facility and in gaining further support for infection prevention efforts (15,20). However, there is evidence that in recent years IPs have perceived a shift in their professional role where the responsibility of preventing infections no longer resides solely within the IPC department but has diffused to frontline clinicians (15,20). This shift to a more consultative role has resulted in feelings of uncertainty and loss (19) and may account for the perception of decreased visibility of the IPC department found in our current study. Since frontline clinicians have become increasingly knowledgeable about the importance of preventing infections as a possible effect of mandatory reporting, the IP may not perceive themselves to be as visible in the hospital as previously.
In a similar study conducted in 2011, Linkin and colleagues (21) surveyed 110 hospitals participating in the Society for Healthcare Epidemiology of America Research Network to assess whether public reporting influenced perceived time spent on HAI surveillance and IPC resources available and HAI rates over the previous 3 years. The researchers found no differences in these outcomes between IPs in states with and without HAI laws; however, the study did not specifically inquire about these outcomes in relation to HAI reporting mandates. Our study presented data from over 700 hospitals, whereas Linkin and colleagues surveyed mostly large, academic hospitals participating in a research network. There is a risk of a selection bias because a hospital that participates in a research network may have different resources available. As our results suggest, hospital differences in type of setting and patient capacity may impact whether hospitals have the resources available to meet state requirements. Large, academic hospitals most likely have the financial resources available to successfully comply with reporting requirements and IPs working in these facilities are probably less likely to be influenced by mandatory reporting requirements as compared to IPs working in smaller hospitals with fewer resources.
Limitations
This study has several limitations including a moderate response rate, which may limit the generalizability of the study findings. This study was a cross-sectional survey limiting our ability to assess whether IP perceptions differed by different time periods after the implementation of state reporting laws. At the time of the survey, there was a large increase in the number of facilities joining NHSN. However, we did not assess whether the perceived benefits or burden of HAI reporting differed between early vs. late adapters of NHSN, nor did we examine differences in perceived burden by type of HAI law or by how long the facility was engaged in reporting prior to the state mandate. Additionally, our survey focused on perceived resources, time, influence and visibility of the IPC department and did not collect data on a myriad of other potential consequences of reporting laws. Nevertheless, our study provides important evidence as to the effect that these reporting requirements may have on IPC departments. Further research is needed to provide a deeper understanding of the unintended consequences that state HAI reporting laws have on IPC departments, IPs and frontline clinicians. Future work should evaluate whether the impact of reporting requirements differs by type and focus of reporting requirements, the extent to which state laws complement or duplicate federal reporting requirements and the resources necessary to comply with these mandates.
Conclusion
This study identified perceived differences in terms of time for routine IPC activities and visibility of the IPC department between IPs in states with and without HAI reporting laws. Further research should examine resources necessary to comply with state HAI laws, and evaluate unintended consequences of state HAI laws.
ACKNOWLEDGEMENTS
We would like to thank all of the hospitals that participated in this study for their contribution.
Funding source: This work was supported by the National Institute of Nursing Research at the National Institutes of Health (R01 NR010107, PI: Stone) and from the Agency for Healthcare Research and Quality (1K08HS024339–01) Mentored Clinical Scientist Research Career Development Award. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health and the Agency for Healthcare Research and Quality. The study sponsor had no role in the design or conduct of the study; in the collection, analysis, or interpretation of the data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Footnotes
Previous presentation of the data: These finding have been presented at IDWeek 2014 as a poster titled “The Impact of State Mandated Healthcare-Associated Infection Reporting on Infection Prevention and Control Departments in Acute Care Hospitals: Results from a National Survey.”
Conflicts of interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Monika Pogorzelska-Maziarz, Thomas Jefferson University, Jefferson College of Nursing Philadelphia, PA USA.
Pamela B. de Cordova, Rutgers, the State University of New Jersey Newark, NJ USA.
Carolyn T.A. Herzig, Columbia University School of Nursing, Center for Health Policy New York, NY USA.
Andrew Dick, Rand Corporation Boston, MA.
Julie Reagan, Georgia Southern University Statesboro, GA.
Patricia W. Stone, Columbia University School of Nursing, Center for Health Policy New York, NY USA.
REFERENCES
- 1.Magill SS, Edwards JR, Bamberg W, et al. Multistate Point-Prevalence Survey of Health Care–Associated Infections. JAMA 2014;370:1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herzig CT, Reagan J, Pogorzelska-Maziarz M, Srinath D, Stone PW. State-Mandated Reporting of Health Care-Associated Infections in the United States: Trends Over Time. Am J Med Qual 2015;30:417–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Hospital Inpatient Quality Reporting Program. Accessed on May 16, 2018. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalRHQDAPU.html
- 4.Reagan J, Hacker C. Laws pertaining to healthcare-associated infections: a review of 3 legal requirements. Infect Control Hosp Epidemiol 2012;33:75–80. [DOI] [PubMed] [Google Scholar]
- 5.Campanella P, Vukovic V, Parente P, et al. The impact of public reporting on clinical outcomes: a systematic review and meta-analysis. BMC Health Serv Res 2016;16:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pakyz AL, Edmond MB. Influence of state laws mandating reporting of healthcare-associated infections: the case of central line-associated bloodstream infections. Infect Control Hosp Epidemiol 2013;34:780–784. [DOI] [PubMed] [Google Scholar]
- 7.Zachariah P, Reagan J, Furuya et al. The association of state legal mandates for data submission of central line-associated bloodstream infections in neonatal intensive care units with process and outcomes measures. Infect Control Hosp Epidemiol 2014;35:1133–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Black BS, Kim HK. The Effect of Mandated Quality Reporting on Outcomes and on Reporting: Evidence from Infection Reporting in Pennsylvania. Northwestern Law & Econ Research Paper No. 11–19. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1641459.Published 2014. Accessed May 16, 2018. [Google Scholar]
- 9.Liu H, Herzig CTA, Dick AW et al. Impact of state reporting laws in central-line associated bloodstream infection rates in U.S. Adult Intensive Care Units. Health Serv Res 2017;52:1079–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stone PW, Pogorzelska M, Graham D, Jia H, Uchida M, Larson EL. California hospitals response to state and federal policies related to health care-associated infections. Policy Polit Nurs Pract 2011;12:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pegues DA. Translating and scaling the HHS Action Plan to Prevent Healthcare-associated Infections to the local level: experience of a Los Angeles Health System. Med Care 2014;52:S60–65. [DOI] [PubMed] [Google Scholar]
- 12.Stricof RL, Van Antwerpen C, Smith PF, Birkhead GS. Lessons learned while implementing mandatory health care-associated infection reporting in New York State. J Public Health Manag Pract 2013;19:294–299. [DOI] [PubMed] [Google Scholar]
- 13.Vostok J, Lapsley W, McElroy N, et al. Assessment of the burden of mandatory reporting of health care-associated infection using the National Healthcare Safety Network in Massachusetts. Am J Infect Control 2013;41:466–468. [DOI] [PubMed] [Google Scholar]
- 14.McKibben L, Horan TC, Tokars JI, et al. Guidance on public reporting of health care-associated infections: recommendations of the Healthcare Infection Control Practices Advisory Committee. Infect Control Hosp Epidmiol 2005;26:580–7. [DOI] [PubMed] [Google Scholar]
- 15.Uchida M, Stone PW, Conway LJ, Pogorzelska M, Larson EL, Raveis VH. Exploring Infection Prevention: Policy Implications from a Qualitative Study. Policy Polit Nurs Pract 2011;12:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szymczak JE. How mandatory public reporting undermined IP: an ethnographic study of HAI surveillance and public reporting In: Program and abstracts of the 2014 Meeting of the Infectious Diseases Society of America (ID Week); October 8–12, 2014; Philadelphia, PA Abstract 906. [Google Scholar]
- 17.Stone PW. Pogorzelska-Maziarz M, Herzig CT State of infection prevention in US hospitals enrolled in the National Health and Safety Network. Am J Infect Control 2014;42:94–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stricof RL, Schabses KA, Tserenpuntsag B. Infection control resources in New York State hospitals, 2007. Am J Infect Control 2008;36:702–5. [DOI] [PubMed] [Google Scholar]
- 19.Conway LJ, Raveis VH, Pogorzelska-Maziarz M. Tensions inherent in the evolving role of the infection preventionist. Am J Infect Control 2013;41:959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stone PW, Pogorzelska-Maziarz N, Reagan J, et al. Impact of laws aimed at healthcare-associated infection reduction: a qualitative study. BMJ Qual Saf 2015;24:637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Linkin DR, Fishman NO, Shea JA, Yang W, Cary MS, Lautenbach E. Public reporting of hospital-acquired infections is not associated with improved processes or outcomes. Infect Control Hosp Epidemiol 2013;34:844–846. [DOI] [PMC free article] [PubMed] [Google Scholar]