Abstract
Introduction:
Obstructive pulmonary disease outcomes in the United States differ between Latinos and non-Hispanic whites. There is little objective data about diagnosis prevalence and primary care visit frequency in these disease processes.
Methods:
We used electronic health record data to perform a retrospective cohort analysis of 34,849 low-income patients seen at Oregon community health centers between 2009–2013 to assess joint racial/ethnic and insurance disparities in diagnosis and visit rates between Latino and non-Hispanic white patients.
Results:
The overall study prevalence of obstructive lung disease was 18%. Latinos had lower odds of obstructive lung disease diagnosis (OR=0.37, 95% CI=0.30–0.44). Among those diagnosed prior to 2009, the uninsured (regardless of race/ethnicity) had lower visit rates during 2009–2013 than the insured.
Discussion:
This study identified racial/ethnic disparities in the diagnosis of obstructive pulmonary disease between Latinos and non-Hispanic Whites, confirming trends observed in survey research but controlling for important confounders. Health insurance was associated with basic care utilization, suggesting that lack of health insurance could lessen the quality of care for obstructive pulmonary disease in Latino and non-Hispanic white patients.
Keywords: asthma, chronic obstructive Lung Disease, Hispanic, primary care, healthcare disparities, health insurance
INTRODUCTION
Obstructive pulmonary disease (asthma and chronic obstructive pulmonary disease (COPD)) outcomes are worse among Latinos compared to Non-Hispanic whites in the United States (US). (1) In these lung diseases, appropriate diagnosis and regular primary care appointments are markers of quality care, (2) but diagnosis rates vary across studies between Latinos, Non- Hispanic whites and even within Latino subgroups. (3) It is uncertain if these differences are due to biologic differences in disease prevalence or differences in quality of/access to care (prompt and complete documentation of diagnosis). Cross-sectional survey designs, which are commonly used in asthma and COPD research, do not necessarily capture diagnosis and primary care utilization objectively over time and may have limits in shedding light on these differences, as self report of asthma diagnosis has limited sensitivity when compared to provider reported rates or other objective measures. (4) Rates of care utilization in those diagnosed, adjusted for demographics that could impact diagnosis and care utilization, are difficult to find in the health services literature. Additionally, insurance status is an important factor in accessing some primary care services in low-income Latino populations. (5) However, little research has examined insurance and race/ethnicity in asthma diagnosis and utilization over a substantial time period. Therefore, our objective was to evaluate the joint disparities of race and ethnicity and insurance status on two basic care quality metrics (diagnosis and visit frequency) using an objective data source. To do this, we used electronic health record (EHR) data to 1) evaluate disparities in the prevalence of obstructive pulmonary disease diagnosis among approximately 35,000 low-income Latinos and Non-Latino whites, over a 5 year time period, accessing care at community health centers (CHCs) in Oregon and 2) evaluate racial/ethnic and insurance disparities in care utilization rates, in 1,164 patients with a lung disease diagnosis prior to 2009, over this subsequent five-year study period.
METHODS
We performed a retrospective cohort analysis of 34,849 low-income (100% of the US Federal Poverty level (FPL) or below) Latino and non-Latino white adults (age 21–79) who had at least one primary care visit between 2009–2013 at one of 23 Oregon CHCs, which share a linked EHR. We categorized our population into 4 cohorts: Latino insured (insured at any encounter during the study period), Latino uninsured (never insured during the study period), non-Hispanic white insured, and non-Hispanic white uninsured. We used insurance at at least one encounter to qualify a patient for an “insured” cohort to differentiate between those with evidence of some access to public health insurance and those without any access, likely due to immigration status. Insurance in our cohort was almost exclusively public, as described in a previous analysis. (6)We used logistic regression to estimate the relative odds of obstructive pulmonary diagnosis (asthma or COPD diagnosis, identified using ICD-9 codes, on problem list or in a visit encounter) by cohort adjusted for sex, age, body mass index (BMI), pregnancy, and number of visits in the study period (as a proxy for utilization (7)). Among patients diagnosed prior to 2009, we utilized Poisson regression to assess differences in CHC visit rates in 20092013, by cohorts, adjusting for covariates. All models utilized robust standard errors to account for clustering of patients within CHCs. This study was approved by the Institutional Review Board of Oregon Health & Science University.
RESULTS
In our study population (n=34,849), Latinos were more likely to be, younger, female, and pregnant as compared to Non-Latino whites (Table 1). Similar differences by race/ethnicity were seen among patients with a diagnosis prior to 2009 (n=1,164, Appendix Table 1). The overall prevalence of obstructive pulmonary disease was 18% and varied between 6.2% among uninsured Latino and 23.9% in non-Hispanic white patients.
Table 1.
Patient characteristics by race-ethnicity/insurance (N, column %)
| Demographic | Non-Hispanic White Insured (n=19,194) |
Non-Hispanic White Uninsured (n=7,507) |
Latino Insured (n=3,675) |
Latino Uninsured (n=4,473) |
Overall p-value |
|---|---|---|---|---|---|
| Sex | <0.001 | ||||
| Female | 10,533 (54.9) | 3,290 (43.8) | 1,524 (41.5) | 2,276 (50.9) | |
| Male | 6,908 (36.0) | 4,093 (54.5) | 1,035 (28.2) | 1,795 (40.1) | |
| Female Pregnancy |
1,733 (9.1) | 124 (1.7) | 1,116 (30.4) | 402 (9) | |
| Age (in years) at study initiation | <0.001 | ||||
| 21–30 | 5,620 (29.3) | 2,087 (27.8) | 1,410 (38.4) | 1,408 (31.5) | |
| 31–40 | 4,321 (22.5) | 1,767 (23.5) | 1,077 (29.3) | 1,649 (36.9) | |
| 41–50 | 4,542 (23.7) | 2,143 (28.6) | 568 (15.5) | 799 (17.9) | |
| 51–60 | 3,256 (16.7) | 1,398 (18.6) | 318 (8.7) | 419 (9.4) | |
| 61–64 | 648 (3.4) | 89 (1.2) | 108 (2.9) | 76 (1.7) | |
| 65 | 807 (4.2) | 23 (0.3) | 194 (5.3) | 122 (2.7) | |
| Office Visits from 2009–2013 | <0.001 | ||||
| 1 | 3,018 (15.7) | 2,778 (37.0) | 493 (13.4) | 1,192 (26.7) | |
| 2–5 | 5,793 (30.2) | 3,304 (44.0) | 1,160 (31.6) | 1,890 (42.3) | |
| >5 | 10,383 (54.1) | 1,425 (19.0) | 2,022 (55) | 1,391 (31.1) | |
| Body Mass Index (kg/m2) | <0.001 | ||||
| <30 | 12,996 (67.7) | 5,306 (70.7) | 2,397 (65.2) | 3,055 (68.3) | |
| ≥30 | 6,198 (32.3) | 2,201 (29.3) | 1,278 (34.8) | 1,418 (31.7) | |
| Pulmonary (Asthma/COPD) diagnosis between 2009–2013 | <0.001 | ||||
| Yes | 4,588 (23.9) | 965 (12.6) | 438 (11.9) | 278 (6.2) | |
| No | 14,606 (76.1) | 6,542 (87.4) | 3,237 (88.1) | 4,195 (93.8) | |
Note: p-value comparing race-ethnicity/insurance groups estimated from chi-square test.
Appendix Table 1.
Patient characteristics by race-ethnicity/insurance groups among patients diagnosed with obstructive pulmonary disease (asthma/COPD) diagnosis prior to 2009 (N, column %)
| Demographic | Non-Hispanic White Insured (n=983) |
Non-Hispanic White Uninsured (n=79) |
Latino Insured (n=69) |
Latino Uninsured (n=33) |
Overall p-value |
|---|---|---|---|---|---|
| Sex | <0.001 | ||||
| Female | 638 (64.9) | 43 (54.4) | 36 (52.2) | 24 (72.7) | |
| Male | 292 (29.7) | 34 (43) | 21 (30.4) | 5 (15.2) | |
| Female Pregnancy |
53 (5.4) | 2 (2.5) | 12 (17.4) | 4 (12.1) | |
| Age (in years) | at study initiation | <0.001 | |||
| 21–30 | 129 (13.1) | 11 (13.9) | 11 (15.9) | 7 (21.2) | |
| 31–40 | 191 (9.4) | 11 (13.9) | 21 (30.4) | 14 (42.4) | |
| 41–50 | 292 (29.7) | 32 (40.5) | 13 (18.8) | 7 (21.2) | |
| 51–60 | 247 (25.1) | 22 (27.9) | 13 (18.8) | 2(6.1) | |
| 61–64 | 60 (6.1) | 2 (2.5) | 3 (4.4) | 2(6.1) | |
| ≥65 | 64 (6.5) | 1(1.3) | 8 (11.6) | 1(3) | |
|
BMI <30 ≥30 |
571 (58.1) 412 (41.9) |
53 (67.1) 26 (32.9) |
40 (58) 29 (42) |
17 (51.5) 16 (48.5) |
0.37 |
Note: p-value comparing race-ethnicity/insurance groups estimated from chi-square test.
Non-Hispanic whites exhibited nearly twice the odds of having an obstructive lung disease diagnosis than Latinos of similar insurance status. Latinos had lower odds of being diagnosed with obstructive pulmonary disease (OR=0.37, 95% CI=0.30–0.44) compared to non-Hispanic whites. Decreasing odds of diagnosis were observed among uninsured Non-Hispanic whites (OR=0.68, 95% CI=0.60–0.78), insured Latinos (OR=0.45, 95% CI=0.37–0.46), and uninsured Latinos (OR=0.26, 95% CI=0.21–0.32) compared to insured Non-Hispanic whites (Figure 1, x- axis).
Figure 1.
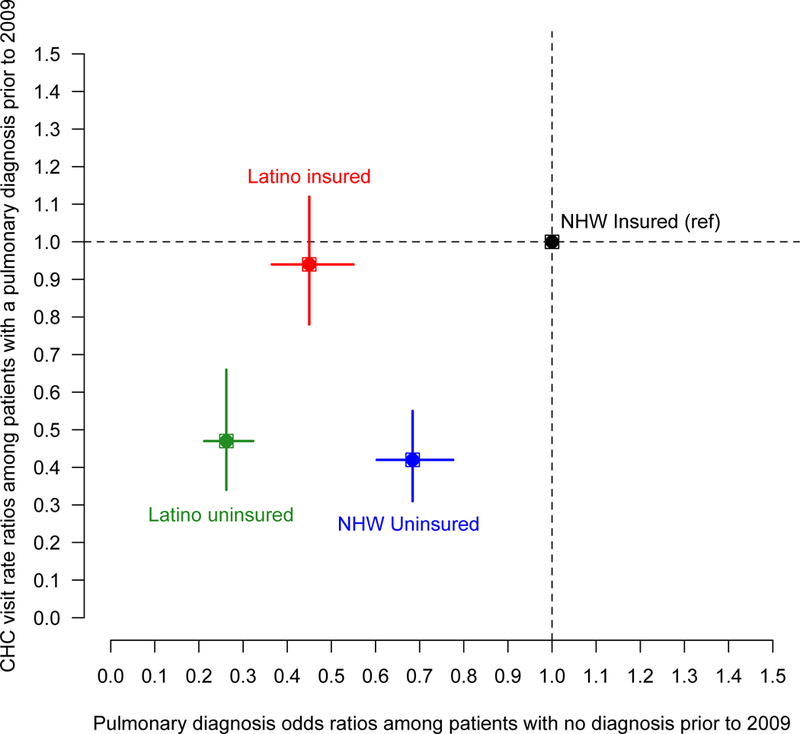
Adjusted odds ratios of obstructive pulmonary disease during 2009–1013 among all study patients (x-axis) and community cealth center (CHC) visit rate ratios during 2009– 2013 among patients with a diagnosis prior to 2009 (y-axis) by race-ethnicity/insurance cohorts.Note for Figure 1: CHC, Community Health Center; NHW, Non-Hispanic White. Among n=34,849 study patients (x-axis), we utilized logistic regression to estimate the relative odds of pulmonary diagnosis during the study period (2009-2013) by cohort adjusted for sex, age, body mass index, pregnancy, and number of visits in the study period. Among patients diagnosed prior to 2009 (y-axis), we utilized Poisson regression to assess differences in CHC visit rates in 2009-2013, by cohorts, adjusting for covariates. Both models utilized robust standard errors to account for clustering within CHCs.
Among patients diagnosed with obstructive lung disease prior to 2009, the uninsured (regardless of race/ethnicity) had significantly lower visit rates over 5 years (2009–2013) than their insured race/ethnic counterparts (Non-Latino whites 58% lower visit rates, Latinos 53% lower visit rates, both p<0.001, Figure 1, y-axis).
DISCUSSION
This study used objective data to assess disparities in the diagnosis of obstructive lung disease and visit frequency after diagnosis between insured/uninsured Latinos and Non-Latino whites among a large sample of low-income patients in Oregon. Overall, the prevalence of asthma and COPD in our study population was slightly higher (2–3%) than rates reported in cross-sectional surveys, (8, 9) suggesting the possibility that national surveys may underestimate the disease burden seen in the healthcare safety net. Latinos had significantly lower odds of diagnosis than Non-Latino whites, which corresponds to nationally reported trends (1, 8) (especially in Latinos of Mexican heritage, which is the primary heritage of our population (7)). While these disparities could represent differences in the prevalence of disease in populations or differences in accurate and prompt diagnosis, the documentation of such a disparity in a large, objective dataset, uncomplicated by recall bias, validates previous findings based on self-report. Our ability to account for income level in the study inclusion criteria, insurance status, and overall care utilization (clinic visits) further adds to the knowledge base by considering confounders that are often unobserved in many studies. Our findings refute the hypothesis that disparities in obstructive lung disease diagnoses are solely due to lack of access of care, since our population included those who accessed clinical care within the study period; further investigation into the etiology of these differences is warranted.
Lack of insurance was associated with reduced odds of diagnosis and reduced utilization of primary care in both racial/ethnic groups. Despite these differences, uninsured persons still averaged approximately 2 visits/year, demonstrating some access to CHCs even among those with significant barriers. This reinforces the value/importance of CHCs in the care of chronic illness in vulnerable populations. Previous research in our network demonstrates that many patients in this cohort gained insurance with the Affordable Care Act(6) which may have resulted in increased diagnosis rates among this group. Current discussions of legislative changes to insurance coverage in the US, if enacted, could threaten quality care for pulmonary disease among low-income and ethnic minority populations. Populations without access to public insurance because of their immigration status, would benefit from insurance coverage to provide basic care utilization for their chronic disease.
Our analysis was limited by lack of data on symptoms related to obstructive lung disease, disease severity, and tobacco use and other risk factors. Patients also could have also received care outside of our network; however, we have shown that patients in our network seldom seek ambulatory care elsewhere.(10) Next steps in research would involve a larger sample of Latino patients across multiple states, including children, and examining associations between diagnosis and presenting symptoms of obstructive pulmonary disease.
CONCLUSION
In Oregon CHCs, Latinos have significantly lower odds of having a diagnosis of obstructive pulmonary disease. A lack of insurance further decreases the odds of having a diagnosis, with proportionally lower odds in uninsured Latinos compared with insured Non-Hispanic whites. Having insurance is associated with more visits once an obstructive pulmonary disease diagnosis is made, but even patients without insurance with lung disease are seen in Oregon CHCs. Reducing insurance coverage for low-income and minority patients may be detrimental to the quality of care for obstructive pulmonary disease.
REFERENCES
- 1.Oraka E, Iqbal S, Flanders WD, Brinker K, Garbe P. Racial and ethnic disparities in current asthma and emergency department visits: findings from the National Health Interview Survey, 2001–2010. Journal of Asthma.50(5):488–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Heart Lung, and Blood Institute. Asthma Care Quick Reference DIAGNOSING AND MANAGING ASTHMA 2011 [Available from: https://www.nhlbi.nih.gov/files/docs/guidelines/asthma_qrg.pdf.
- 3.Akinbami LJ, Simon AE, Rossen LM. Changing Trends in Asthma Prevalence Among Children. Pediatrics. 2016;137(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toren K, Brisman J, Jarvholm B. Asthma and asthma-like symptoms in adults assessed by questionnaires. A literature review. Chest.104(2):600–8. [DOI] [PubMed] [Google Scholar]
- 5.Heintzman J, Bailey SR, Cowburn S, Dexter E, Carroll J, Marino M. Pneumococcal Vaccination in Low-Income Latinos: An Unexpected Trend in Oregon Community Health Centers. Journal of health care for the poor and underserved. 2016;27(4):1733–44. [DOI] [PubMed] [Google Scholar]
- 6.Heintzman J, Bailey SR, DeVoe J, Cowburn S, Kapka T, Duong TV, et al. In Low-Income Latino Patients, Post-Affordable Care Act Insurance Disparities May Be Reduced Even More than Broader National Estimates: Evidence from Oregon J Racial Ethn Health Disparities. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foster A, Jordan K, Croft P. Is frequent attendance in primary care disease-specific? Family practice. 2006;23(4):444–52. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Chronic Obstructive Pulmonary Disease Among Adults- United States, 2011 2012 [Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6146a2.htm.
- 9.Centers for Disease Control and Prevention. Most Recent Asthma State or Territory Data 2017 [Available from: https://www.cdc.gov/asthma/most_recent_data_states.htm].
- 10.O’Malley JP, O’Keeffe-Rosetti M, Lowe RA, Angier H, Gold R, Marino M, et al. Health Care Utilization Rates After Oregon’s 2008 Medicaid Expansion: Within-Group and Between- Group Differences Over Time Among New, Returning, and Continuously Insured Enrollees. Med Care. 2016;54(11):984–91. [DOI] [PMC free article] [PubMed] [Google Scholar]


