Abstract
Objective:
To perform a systematic review of the properties and results of the studies that their approaches are lean management in emergency departments and the factors which influence on their performance.
Method:
The necessary information in the first stage was collected by searching these keywords: "Lean principles" “Lean Six Sigma", "Lean Process", “Lean thinking”, “Lean Methodology”, “Toyota Production System lean processing”, "lean techniques", "emergency department”, “emergency medicine”, “emergency room” and “emergency care ” . And in the next stage the keywords such as “lean management” and “emergency” was collected from SID, Medlib, IranDoc, Google Scholar, MagIran, IranMedex data bases. For extracting the data data-extracting forms was prepared. The information we got from the forms was organized in information-extracting forms and was analyzed manually. The diagrams were drawn in Excel: 2010.
Results:
Finally, 26 essays have been included. Most of the studies were accomplished in Canada and U.S.A. only in one of the cases, the authors used the control group. Each of these terms, “lean techniques” and “lean principals”, with five times repetitions had the highest frequency. The most important team of implementation of lean management included: hospital management team or the manager of Emergency department, physicians, nurses, staffs and external counselors. Generally, 51 indicators were studied which among them the length of stay and the timing had the most frequency. After implementation of lean management, almost all studied indicators have significantly improved. 14 barriers, 14 facilitators and 10 effective factors were recognized in implementing the lean management.
Conclusion:
According to the studies, responsibility of organization’s senior management and his/her supports; increasing the knowledge of the characteristics and dimension of lean among the providers of health service; and decreasing the resistance and consulting with external counselors can have great effect on the success of lean management.
Key Words: Lean management, Improving the quality, Barriers, Facilitators, Effective factors, Emergency
Introduction
Emergency is one of the most important parts of a hospital. The operational and effective function of the Emergencies can have a great effect on the quality and quantity of the operation of other departments and satisfaction of the people who receive healthcare services [1]. Because of its importance and sensitivity Emergency in each hospital must be structurally and organizationally set in order to give the healthcare processes carefully and with a high quality and have a suitable function in presenting services to patients [2]. Emergency is a department that patients often get their first experience of the hospital there [3, 4]. During last years, because of the population increase, increase in intentional and unintentional harms and drugs abuse Emergency departments in hospitals have lots of costumers, but number of these parts has not increased that much [5-7]. Emergency departments face with a serious problem of not presenting suitable healthcare services, because of the demographic changes of the population and the appearance of the illnesses such as increase in age average and hope for life, outbreak of ailments such as cancers and heart diseases, and at the same time since people have got more knowledge in relation to the growth and keep of health, they want to receive high qualified and high quantity of health cares in Emergency departments [8-10].
In order to solve the problem of patients’ high numbers in Emergency departments and after that problems of high qualified healthcare services most of the managers of the healthcare systems and deciders think that implementing quality improvement models for reaching to this goal is inevitable. Lean management is one of the methods that have been very popular in the last two decades [11-13]. Lean management is a term used in industry to improve the production capacity and omit wastes in the process and has been well known especially after being implemented by Toyota. By developing the success of this method of management, other organizations such as hospitals used its principles to make their work process reliable and stable and get achievements in work capacity increase, costs decrease, costumers’, staff’s satisfaction and reinforcing leadership [14-16]. Although the healthcare part got involved in Lean management later, but recently many healthcare organizations implement this method and have been able to make impressive improvement in offering qualified services to patients and reduce costs, damages and wastes, and these results got possible just by cultural preparation and gradual improvement [17-18]. Lean management includes five main principles, its guidance and instruction and it leads the company and the organization which present a service or product toward a stable and seeking system. The main principle in Lean is to delete the production wastes. In Lean management costumer has a very important place and it believes that for improving the system and considering the costumer and improving the value we have to forget our competitors and concentrate just on ourselves. We should recognize the wastes and delete it and then with a perfectionisms approach stay in the improvement cycle [19, 20].
In recent years many researches have been done and designed in hospitals, especially the Emergency departments by using the lean management and the results show the impressive effect of this management method in improving the services quality to patients [21-27]. Since this management method is newly implemented in hospitals and the Emergency units are very important, in choosing and applying this method we should have precise and enough information about the previous researches’ properties and results. We should also analyze the important factors in success or probable failure of this method. Hence the present study is planned to review the properties and the results of the previous studies with Lean management approach in Emergency units and the effective elements in implementing that.
Materials and Methods
Search Strategy
This study is a systematic review done in 2016 and has used the systematic review of studying from the book named “Systematic reviews to support evidence based Medicine” [28]. We collected the necessary information in the first step by searching these key words “Lean principles”, “Lean Six Sigma”, “Lean Process”, “Lean thinking”, “Lean Methodology”, “Toyota Production System lean processing”, “lean techniques”, “emergency department”, “emergency medicine”, “emergency room” and “emergency care " in PubMed, web of Knowledge, Google Scholar, Scopus database and in the second step by using “Lean management” and “Emergency” in SID, Medlib, IranDoc, Google Scholar, MagIran, IranMedex. Time period for searching these articles was 2000 to 2016. After searching these data bases, in order to identify and cover most of the published articles we searched some of the authentic magazines (Am J Med Qual, BMC Health Serv Res, Int J Health Care Qual Assur, J Healthc Qual, Jt Comm J Qual Patient Saf, Qual Manag Health Care, and World Hosp Health Serv). After deleting the essays having weak connection with the study and choosing the main essays, the references of the chosen essays were searched again to make sure that we have chosen the right ones.
Inclusion and Exclusion Criteria
The eligibility criteria for include or exclude of articles are summaries in Table1.
Table 1.
Inclusion and excluded criteria
| Inclusion Criteria | Excluded Criteria |
|---|---|
| Original researching essays | Short essays, letter to editor, educational essays, the essays presented in seminars |
| The study being done in Emergency department | Studies done in other parts of the hospital/also being in common with other departments |
| Indicating the effective factors of success and failure | Essays not having enough information |
| Studies done in pilot method | |
| Studies with English language | Publication languages other than English |
Data Extraction
Quality of the report in selected essays was evaluated after getting extracted from the databases by using the mentioned key words. The check list of (STROBE) Strengthening the Reporting of Observational and studies in Epidemiology was helpful here. For extracting the data first, we prepared two data-extracting forms in Excel. First form was for the descriptive studies section including: writer, country, publishing year, words applied, duration of the Lean management implementation, type of study, members of the Lean management team, assessable indicators and the total conclusion of the research. First data of the 5 essays were extracted experimentally for the form and the inefficiencies and problems of the present form were solved. The second form was allocated for the information about the barriers/challenges, facilitators/ success factors and effective factors. The information extracted in this form was: writer, country, publishing year, barriers/challenges, facilitators/ success factors and effective factors.
Data Analysis The information we got from the forms first was organized in information-extracting forms and was analyzed manually. The diagrams were drawn in Excel:2010.
Results
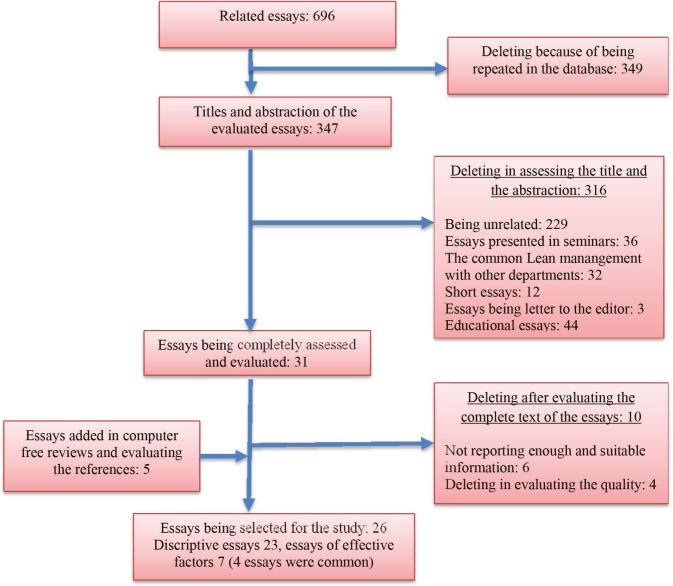
Eventually from the 696 essays, 26 essays that had a link with the purpose of the study were selected (Figure 1).
Fig 1.
Searches and inclusion process
Descriptive results of the Lean management implementation in Emergency departments are shown in Table 2.
Table 2.
Descriptive results in implementing lean in hospitals’ emergency units
| Au-Cu-Ye | model | Lean implementation Length of time (month) | Methods | Project Team Composition | Indicator | results |
|---|---|---|---|---|---|---|
| Vermeulen et al., [31] | Lean Process | 7 | before and after | senior leaders, managers, and staff from a variety of departments | Length of Stay | Both 90th percentile and median ED length of stay and time to physician assessment were significantly lower after the program |
| Naik et al., [32] | lean principles | 18 | before and after | members of departmentalleadership and key stakeholders relatedto ED administration (e.g., finance and hospitaloperations) | median ED patient visits, median login to disposition time, median login to triage time, Provider productivity | ED patient visits per month rose 7.3%, median login to disposition time declined from 4.6 hr to 4.0 hr. median login to triage time decreased from 0.6 hr to 0.3 hr. Provider productivity improved by 18.8% |
| McCulloch et al., [25] | lean principles | 8 | Interrupted time series | Academic expert in Lean, two members of a consultancy specializing in Lean improvement techniques, senior and junior surgeons, and a human factors expert. | Correct administration of prophylaxis for deep vein thrombosis, Correct use of venous site infection protocol, direct verbal communication between medical and nursing teams on daily rounds, Adequate monitoring of patients’ vital signs and recording of their risk scores, Patients without a drug prescribing error | Compliance with the five process measures targeted for Lean intervention ) but not the two that were not) improved significantly (relative improvement 28% to 149%; P<0.007) |
| Mazzocato et al., [30] | lean thinking | 1 | before and after | Physician, nurse, hospital management team | waiting and lead times | Improvements in waiting and lead times (19-24%) |
| Sanders JH & Karr T. [33] | Lean Six Sigma | - | Cross-sectional, case study | ED registered nurses (RNs), Hematology and Chemistry Lab personnel, and process improvement team members | turn-around-times | 30 percent decrease in complete blood count analysis (CBCA) Median TAT, a 50 percent decrease in CBCA TAT Variation, a 10 percent decrease in Troponin TAT Variation, a 18.2 percent decrease in URPN TAT Variation, and a 2-5 minute decrease in ED registered nurses rainbow draw time |
| Chan et al., [34] | Lean techniques | 10 | before-and-after study | - | Triage waiting time, consultation waiting time, blood result time, admission waiting time, total processing time and ED length of stay | The triage waiting time and end waiting time for consultation were significantly decreased. The admission waiting time of emergency medical ward (EMW) was significantly decreased from 54.76 minutes to 24.45 minutes after implementation of PAT program (P<0.05). |
| Niemeijer et al., [27] | Lean Six Sigma | 2 | before-and-after study | - | length of stay (LOS) | The average LOS of trauma patients at the TND at the beginning of the project was 10.4 days. After the implementation of the improvements, the average LOS was 8.5 days |
| Dickson et al., [35] | Lean | - | before-and-after study | Frontline workers, ED management, | length of stay, patient volume, patient satisfaction | One year post-Lean, length of stay was reduced in 3 of the EDs despite an increase in patient volume in all 4. Each observed an increase of patient satisfaction lagging behind by at least a year |
| Ng et al., [36] | Lean principles of the Toyota Production System | 12 | before-and-after study | emergency physicians; nurses; nurse practitioners; porters; clerks; cleaning staff; administrators; the ED director, unit manager and educator; the hospital’s senior vice-president; and representatives from diagnostic imaging, laboratory, respiratory therapy, home care and information services | mean registration to physician time, patients who left without being, length of stay | The mean registration to physician time has decreased from 111 minutes to 78 minutes. The number of patients who left without being seen has decreased from 7.1% to 4.3%. The length of stay (LOS) for discharged patients has decreased from a mean of 3.6 to 2.8 hours, an improvement in ED patient satisfaction scores. |
| Tejedor-Panchón et al., [37] | lean methods | before-and-after study | patient's time spent in the examination area of the department, wait time before the first visit by a physician, and the percentage of patients who left before being seen | The mean (95% CI) time spent in the examining areas by patients with the simplest emergencies was reduced from 80.4 (75.3-85.6) minutes to 61.6 (57.7-65.5) minutes (P<.001). Mean (SD) delays until first contact with a physician were also reduced significantly (P<.001) from 58.0 (6.3) minutes to 49.1 (3.7) minutes. The percentage of patients leaving before seeing a physician also decreased, from 2.8% (0.5%) to 2.0% (0.9%) (P<.001). | ||
| USA, 2013[38] | lean techniques | before-and-after study | - | Daily visits, patient satisfaction. | daily visits to the ED have increased from 42 to 54, and patient satisfaction scores have jumped 25 points on Press Ganey surveys | |
| USA, 2012[39] | lean techniques | before-and-after study | - | patient volume | patient volume is up by about 25% at all three hospitals | |
| Dickson et al., [40] | lean manufacturing techniques | 12 | before-and-after study | 2 ED physicians, 2 EDnurses, an ED physician assistant, 2 non-ED physicians , 2 radiology technicians, a laboratory technician, 5industrial engineers, and 5 external participants from alocal business council | patient satisfaction, expense per patient, ED lengthof stay (LOS), and patient volume | Patient visits increased by 9.23% in 2006. Despite this increase, LOS decreased slightly and patient satisfaction increased significantly without raising the inflation adjusted cost per patient |
| Piggott et al., [41] | Lean principles | 10 | before-and-after study | senior management, external Lean consultants, emergency administrators, nurses, physicians, residents, porters | proportions of care milestones (first electrocardiogram [ECG], ECG interpretation, physician assessment, and acetylsalicylic acid [ASA] administration) meeting target times | The proportion of cases with 12-lead ECGs completed within 10 minutes of patient triage increased by 37.4% (p, 0.0001). The proportion of cases with physician assessment initiated within 60 minutes increased by 12.1% (p 5 0.0251). Times to ECG, physician assessment, and ASA administration also continued to improve significantly over time (p values , 0.0001). |
| Murrell et al., [42] | Lean principles | 6 | before-and-after study | Physician, nurse | ED length of stay, ED arrival to physician start time, ED without being seen by a doctor (LWBS) | ED length of stay was longer in the period before Rapid Triage and Treatment (RTT) than after. Mean ED arrival to physician start time was 62.2 minutes prior to RTT and 41.9 minutes after. The LWBS rate for the six months prior to RTT was 4.5% and 1.5% after RTT initiation. |
| El Sayed et al., [43] | Lean Methodology | 20 | before-and-after study | ED chairperson, the ED medical director, 2 nurses including the ED nurse manager, case management, clerks, and registration staff | door to doctor time, Length of stay | There was a statistically significant decrease in the mean door to doctor time. Length of stay of both admitted and discharged patients dropped from 2.6 to 2.0 hours and 9.0 to 5.5 hours |
| Kane et al., [44] | Lean Manufacturing techniques | - | before-and-after study | Physician, nursing leadership, operational leaders, performance excellence consultants | waiting time, length of stay, patient throughput, patient satisfaction | decreased patients’ wait times and length of stay, while improving patient throughput and reported satisfaction |
| Eller [45] | lean tools | 18 | Cross-sectional | Staff members | LWBS, LOS, diversion time | reducing the average length of stay for all emergency department patients by 45 minutes, diversion by 55%, and patients who left without being seen by 28% |
| King et al., [46] | Lean Thinking | - | before-and-after study | patient care assistants, clerical staff, junior and senior nursing, medical staff | waiting times, total durations of stay in the ED | All groups of patients spent significantly less overall time in the department and the average number of patients in the ED at any time decreased |
| Richardson et al., [29] | Lean Methodology | 40 | before-and-after study | Nurses | nursing time in obtaining needed supplies in an ED | significantly decreases the number of searches by nurses for supplies |
| White et al., [47] | Lean | 6 | controlled before-and-after | - | LOS, percent of patients discharged within one hour, time in exam room | Median LOS among discharged patients was reduced by 15 minutes. The number of patients discharged in <1 hr increased by 2.8%. Median exam room time decreased by 34 minutes. |
| Damato and Rickard [48] | Lean-Six Sigma | 4 | before-and-after study | - | Hemolysis | ECC hemolysis decreased by 91%— from 9.8% to 0.88%. Housewide hemolysis decreased by 59%—from 3.4% to 1.39%. |
| Dickson et al., [49] | Lean | 24 | Cross-sectional | 2 ED physicians, 2 EDnurses, an ED physician assistant, 2 non-ED physicians , 2 radiology technicians, a laboratory technician, 5industrial engineers, and 5 external participants from alocal business council | LOS, expense per patient, patient satisfaction | Total length of stay has decreased 3%. 9% decrease in the direct expense per patient. 9% increase in patient satisfaction |
As we can see in Table 2 most of the studies in this department are done in the U.S.A: 12 of 23 studies, Canada with 3 studies, England 2 studies, China 1 study, and Australia 1 study. Spain 1 study, Sweden 1 study, Netherland 1 study and Lebanon 1 study. Most of these studies are done after 2010.
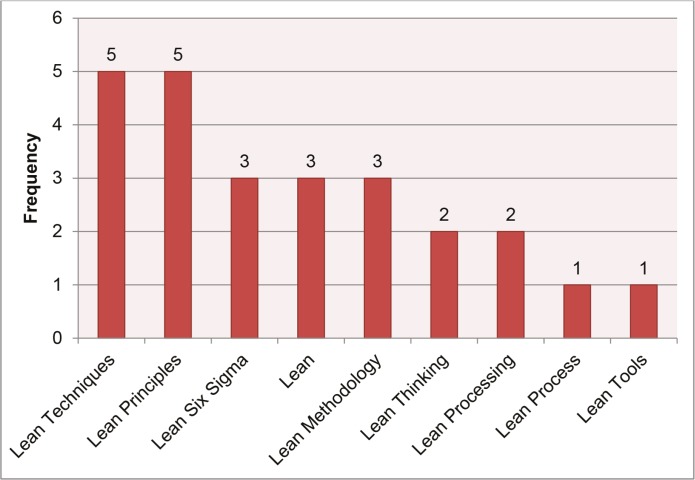
Different terms were used for Lean management in different studies. These terms are shown in Figure 2 according to the numbers of repetition. As you can see, Lean techniques and lean principles are five more times repeated and stand in the first place.
Fig. 2.
Different terms which were used in lean management
Among 23 studies evaluated in this part of our study, we could extract the duration of implementing the Lean management in 16 studies. According to the findings the longest time of implementing Lean management was for the study of Richardson et al., [29] hat was 40 months. And the shortest time was 1 month in Mazzocato et al., [30]. Totally in all 16 studies Lean management was run for 198 months (12.3 months’ average for each study). The average time for implementing the Lean management was 10 months.
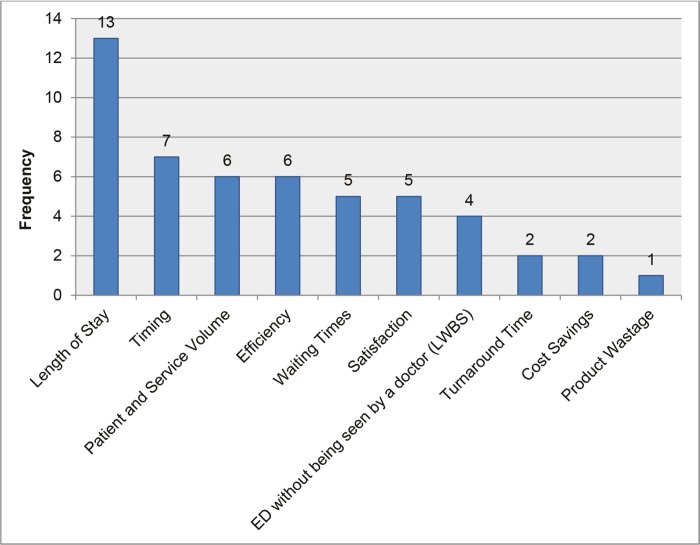
18 studies from 23 studies were done evaluating the last and next assessments. 3 studies analyzed the results after implementing the Lean management cross-sectionally. In one study time series studies were applied. Only in one of the studies controlled studies were used. The most important members of implementing lean management included: the hospital management team or the Emergency department head, physicians, nurses, staffs and external counselors. In the assessment, totally we mentioned 51 indicators shown in Figure 3 according to the repeating times. As it is seen length of stay and timing have the most frequency among the studies. Nearly all the evaluated indicators in the studies have made a noticeable improvement after implementing the Lean management. In all of the studies length of stay both in discharged patients and hospitalized patients have been reduced. Time duration of doing the first treatments in the first possible time had a considerable reduction. Also the waiting time in emergency department was lower. Patients’ satisfaction had a rise too. Ed without being seen by a doctor (LWBS) in the Emergency department had an appreciable reduction. In two studies focusing on the expenses it was shown that they had costs’ decrease.
Fig. 3.
Evaluated indicators in studying the lean management in hospitals’ emergency units
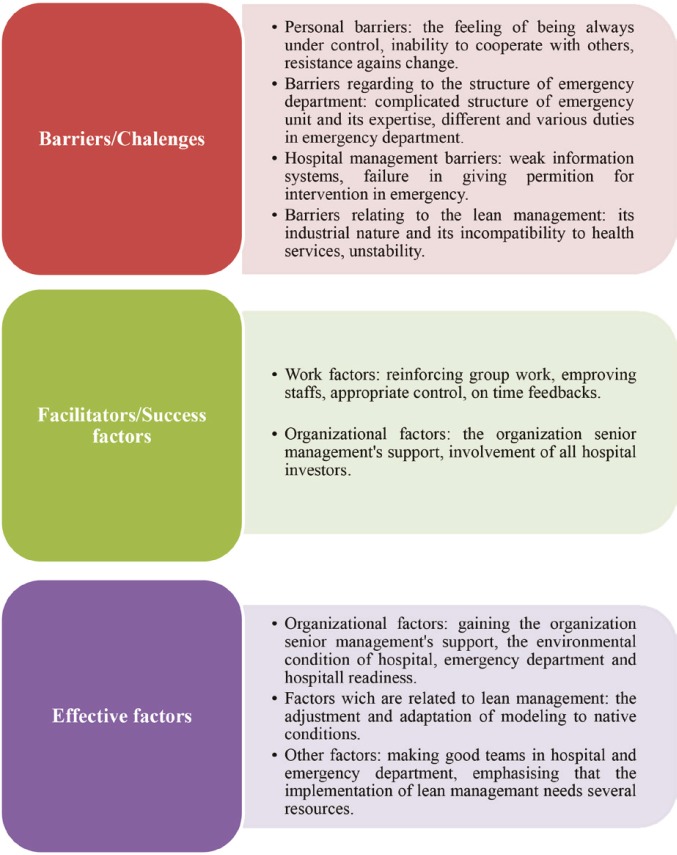
7 studies pointed to the barriers/challenges, facilitators/ and successes and failure factors in Lean management implementation (Table 3). Among them we see 2 essays in U.S.A, 1 in Ghana, 1 in England, 1 in Sweden, 1 in New Zealand and 1 in Lebanon. 4 studies worked on the barriers, 4 studies on facilitators and 2 studies pointed to the effective factors. In Lean management 14 barriers, 14 facilitators and 10 effective factors were identified. By content analysis the barriers/challenges, facilitators/success and effective factors in Lean management were classified in the framework of Figure 4.
Table 3.
Barriers/ challenges, facilitators/ success factors and effective factors in implementing lean management in emergency units
| Au-Cu-Ye | Challenge/barriers | Facilitators/ enablers | Effected factors |
|---|---|---|---|
| Mazzocato et al., [1] |
|
|
- |
| Timmons et al., [23] |
|
- | - |
| Sanders JH & Karr T. [4] |
|
- | - |
| El Sayed et al., [15] | - |
|
- |
| Carter et al., [24] | - | - |
|
| Rees et al., [25] |
|
||
| Dickson et al., [22] | - |
|
- |
Fig. 4.
Barriers/ challenges, facilitators/ success factors and effective factors in implementing lean management in emergency units
Discussion
In applying the methods of quality improvement such as lean management, the Emergency department, because of providing extended services for patients as well as its special place in quality of hospital service and customer satisfaction has great importance. In most cases the Emergency department is the first experience of patients. And since the patients need special and immediate caring and treatment, understanding the patients’ problem in this department is highly necessary for gaining their satisfaction. In recent decades, several factors such as population growth, increasing intentional and unintentional harms and drug abuse have increased the number of emergency unit’s clients. But the number of emergency units has not increased that much in the period [53, 54].
In the study among 696 recognized essays, finally 26 essays were selected (23 of them were related to descriptive section and 7 of them were related to section of factors [some of these essays were in both categories]). Most of the studies were accomplished after 2010 in Canada and United State. Among the 23 descriptive studies, 18 of them were accomplished before and after lean implementation. And 3 of them surveyed the result only after the implementation. Two terms of “lean techniques” and “lean principals”, with five repetitions had the highest frequency. The most important members of implementing team of lean management were hospital management team or the Emergency department head, physicians, nurses, staffs and external counselors. Generally, 51 indicators were studied which among them the length of stay and the timing had the most frequency. After lean management implementation, almost all studied indicators have significantly improved. 7 essays pointed to barriers/challenges, facilitator/success factors and effective factors in implementing lean in Emergency department; and 14 barriers, 14 facilitators and 10 effective factors were recognized in implementing lean management. Studies’ results show that like most of the improving quality models, lean management approach has been more considered in the developed countries. This is more explicit in the models like lean management which has their root in industry; because there are many developed industry in such countries. Hence, the developing countries which demand to use these models must use these models cautiously and vocalize them according to their economic and cultural conditions and especially according to their health systems.
Two terms of “lean techniques” and “lean principals”, with five repetitions had the highest frequency. Regarding the importance of common language in methods of improving quality [55], to gain a common language in lean management can have an effective role in its well implementing.
Among the 23 descriptive studies, 18 of them were accomplished before and after lean implementation. Only in 1 study, the control group was used. Because of the equality of conditions in after and before assessments, the corruption chance of interventions results is really high, so the use of a control group in interventional studies is proposed in order to minimize the effect of confounders as well as increasing the ability of comprising and analyzing the result [56, 57]. Therefore, we propose that future studies use a control group.
Among the different indicators surveyed in these studies, the length of stay and the timing had the highest frequency. In precise focusing on types and frequencies of the used indicators it has been considered that the lean management in these studies focuses more on indicators relating to the time (time of the first offering service, waiting time, hospitalization time, circulation time). The main reason of this can be extension, importance and easy improvement of time indicators [58- 60]. Considering the shortage of recourses and time as well as the complication of measuring and improving the other indicators, the time indicators can be good samples for intervention and improvement. However beside this, we shouldn’t ignore the importance and place of the other indicators such as financial ones and indicators related to the patient satisfaction and efficiency.
The most important members of implementing team of lean management were hospital management team or the head of Emergency department, physicians, nurses, staffs and external counselors. One of the most important persons in implementing lean management is the external consultant who is expert in this field. Since the lean management is a model rooted in industry and has its special complications, and staffs in health systems especially Emergency department are not familiar with dimension and complications of the model; so it seems that it is necessary to use the consultants and experts of the model in lean management group [61]. The other important member of the group is organization’s senior manager with his/her responsibility. Lean management makes a great change in offering services and management style in each department; and it is obvious that any change requires the organization senior manager responsibility. Otherwise, not only there will be many organizational and structural problems in implementing the project, but also others will lose their motivation for implementing lean [62,63].
One of the personal barriers for implementing lean management addressed in the studies was the resistance against the change which in studying other department often had been addressed [64-67]. Since the implementation of lean management is an invisible change, the staff resistance is apparently inevitable. But it is required to decrease the staff resistance with different ways such as considering their feeling, talking with them, trusting them and giving them the freedom [68-70]. For there is no doubt that lean management like other intervention in hospitals and health systems, will be unsuccessful by resistance of staffs and without their cooperation.
Another barrier is that the origin of the lean management is in industry and it doesn’t have enough compatibility with health system. One of the most important results of the barrier is the shortage of knowledge about the model in health system. Poksinska who studied the lean management position in health system pointed that this shortage of knowledge of lean management in health system could be due to the origin of the model [64]. It is pointed out that it is better for lean management team to include external consultant and experts of lean management. So it seems that using these experts and consultants as trainers of the model beside implementing the Lean management can be a good solution for the barrier. But the problem of using these experts is that they are not familiar with health system and they use technical and industrial language [71]. So it is better to work with a team in training. Namely such a group should be included both the experts of health systems and the experts of lean management. Furthermore, as it is stated in the section of the effective factors, the adaptation of the model with native condition can make the performance of the model better.
Another limitation of the study was the language, because researchers could search for only English and Persian studies. Furthermore because of the great inconsistency in implementing the studies and their results, it was impossible to apply the Meta analyses.
Conclusion
Countries with high income had numerous experiences in implementing lean management; so transferring such experiences to low-income countries will have a great role in successfully implementing lean management in these countries. This study suggests further studies in lean management in emergency departments by using control groups. In order to successfully extend lean management in health system especially in Emergency departments, it is necessary to reach to a common language between researchers, health services providers, health systems managers and programmers. According to the results of the studies some factors which have a great role in lean management are: responsibility of the senior management and his/her supports, increasing the knowledge of health services providers about the properties and the dimensions of lean management, decreasing staff’s resistance and using the consultants and experts in the field.
Acknowledgments
This study was part of a PhD thesis supported by Iran University of Medical Sciences, International Campus (Grant No: IUMS/SHMIS-I. 9223652208/2016).
Funding:
This study was funded by Iran University of Medical Sciences.
Conflicts of interest:
The authors declare that they have no competing interests.
References
- 1.Shah N, Hossain N, Shoaib R, Hussain A, Gillani R, Khan NH. Socio-demographic characteristics and the three delays of maternal mortality. Int J Gynaecol Obstet. 2009;105(1):86–91. [PubMed] [Google Scholar]
- 2.Burchett HE, Mayhew SH. Maternal mortality in low-income countries: what interventions have been evaluated and how should the evidence base be developed further? J Coll Physicians Surg Pak. 2009;19(2):95–8. doi: 10.1016/j.ijgo.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 3.Garcia Gigorro R, Talayero-Gimenez de Azcarate M, Saez-de la Fuente I, Chacon-Alves S, Molina-Collado Z, Lazaro-Martin N, et al. Impact of emergency department length of stay before icu admission on patient outcome. Intensive Care Med Exp. 2015;3(Suppl1):S1–A151. [Google Scholar]
- 4.Mollaoglu M, Celik P. Evaluation of emergency department nursing services and patient satisfaction of services. J Clin Nurs. 2016;6(10):13272. doi: 10.1111/jocn.13272. [DOI] [PubMed] [Google Scholar]
- 5.Afilal M, Yalaoui F, Dugardin F, Amodeo L, Laplanche D, Blua P. Forecasting the Emergency Department Patients Flow. J Med Syst. 2016;40(7):016–0527. doi: 10.1007/s10916-016-0527-0. [DOI] [PubMed] [Google Scholar]
- 6.Leary M, Schweickert W, Neefe S, Tsypenyuk B, Falk SA, Holena DN. Improving Providers' Role Definitions to Decrease Overcrowding and Improve In-Hospital Cardiac Arrest Response. Am J Crit Care. 2016;25(4):335–9. doi: 10.4037/ajcc2016195. [DOI] [PubMed] [Google Scholar]
- 7.Ng CJ, Liao PJ, Chang YC, Kuan JT, Chen JC, Hsu KH. Predictive factors for hospitalization of nonurgent patients in the emergency department. Medicine. 2016;95(26):e4053. doi: 10.1097/MD.0000000000004053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buttigieg SC, Dey PK, Cassar MR. Combined quality function deployment and logical framework analysis to improve quality of emergency care in Malta. Int J Health Care Qual Assur. 2016;29(2):123–40. doi: 10.1108/IJHCQA-04-2014-0040. [DOI] [PubMed] [Google Scholar]
- 9.Jones P, Wells S, Harper A, LeFevre J, Stewart J, Curtis E, et al. Is a national time target for emergency department stay associated with changes in the quality of care for acute asthma? A multicentre pre-intervention post-intervention study. Emerg Med Australas. 2016;28(1):48–55. doi: 10.1111/1742-6723.12529. [DOI] [PubMed] [Google Scholar]
- 10.McCaughey D, Erwin CO, DelliFraine JL. Improving Capacity Management in the Emergency Department: A Review of the Literature, 2000-2012. J Healthc Manag. 2015;60(1):63–75. [PubMed] [Google Scholar]
- 11.Burgess N, Radnor Z. Evaluating Lean in healthcare. Int J Health Care Qual Assur. 2013;26(3):220–35. doi: 10.1108/09526861311311418. [DOI] [PubMed] [Google Scholar]
- 12.Holden RJ, Eriksson A, Andreasson J, Williamsson A, Dellve L. Healthcare workers' perceptions of lean: A context-sensitive, mixed methods study in three Swedish hospitals. Appl Ergon. 2015;47:181–92. doi: 10.1016/j.apergo.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balle M, Regnier A. Lean as a learning system in a hospital ward. Leadersh Health Serv. 2007;20(1):33–41. doi: 10.1108/17511870710721471. [DOI] [PubMed] [Google Scholar]
- 14.Dammand J, Hørlyck M, Jacobsen TL, Lueg R, Röck RL. Lean management in hospitals: Evidence from Denmark. Administratie si Management Public. 2014;23:19–35. [Google Scholar]
- 15.Davis J, Adams J. The 'Releasing Time to Care--the Productive Ward' programme: participants' perspectives. J Nurs Manag. 2012;20(3):354–60. doi: 10.1111/j.1365-2834.2011.01266.x. [DOI] [PubMed] [Google Scholar]
- 16.Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med. 2006;1(3):191–9. doi: 10.1002/jhm.68. [DOI] [PubMed] [Google Scholar]
- 17.Kruskal JB, Reedy A, Pascal L, Rosen MP, Boiselle PM. Quality initiatives: lean approach to improving performance and efficiency in a radiology department. Radiographics. 2012;32(2):573–87. doi: 10.1148/rg.322115128. [DOI] [PubMed] [Google Scholar]
- 18.Leggat SG, Bartram T, Stanton P, Bamber GJ, Sohal AS. Have process redesign methods, such as Lean, been successful in changing care delivery in hospitals? A systematic review. Public Money and Manage. 2015;35(2):161–8. [Google Scholar]
- 19.Andersen H, Røvik KA, Ingebrigtsen T. Lean thinking in hospitals: Is there a cure for the absence of evidence? A systematic review of reviews. BMJ Open. 2014;4(1) doi: 10.1136/bmjopen-2013-003873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Call R. 'Lean' approach gives greater efficiency. Health Estate. 2014;68(2):23–5. [PubMed] [Google Scholar]
- 21.Hwang P, Hwang D, Hong P. Lean practices for quality results: a case illustration. Int J Health Care Qual Assur. 2014;27(8):729–41. doi: 10.1108/ijhcqa-03-2014-0024. [DOI] [PubMed] [Google Scholar]
- 22.Iannettoni MD, Lynch WR, Parekh KR, McLaughlin KA. Kaizen method for esophagectomy patients: improved quality control, outcomes, and decreased costs. Ann Thorac Surg. 2011;91(4):1011–7. doi: 10.1016/j.athoracsur.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JE, Smith AL, Mastro KA. From Toyota to the bedside: nurses can lead the lean way in health care reform. Nurs Adm Q. 2012;36(3):234–42. doi: 10.1097/NAQ.0b013e318258c3d5. [DOI] [PubMed] [Google Scholar]
- 24.Lodge A, Bamford D. Health service improvement through diagnostic waiting list management. Leadersh Health Serv. 2007;20(4):254–65. doi: 10.1108/17511870710829364. [DOI] [PubMed] [Google Scholar]
- 25.McCulloch P, Kreckler S, New S, Sheena Y, Handa A, Catchpole K. Effect of a "Lean" intervention to improve safety processes and outcomes on a surgical emergency unit. Bmj. 2010;2(341):c5469. doi: 10.1136/bmj.c5469. [DOI] [PubMed] [Google Scholar]
- 26.Miller R, Chalapati N. Utilizing lean tools to improve value and reduce outpatient wait times in an indian hospital Leadersh. Health Serv. 2015;28(1):57–69. doi: 10.1108/LHS-01-2014-0001. [DOI] [PubMed] [Google Scholar]
- 27.Niemeijer GC, Trip A, Ahaus KT, Does RJ, Wendt KW. Quality in trauma care: improving the discharge procedure of patients by means of Lean Six Sigma. J Trauma. 2010;69(3):614–8. doi: 10.1097/TA.0b013e3181e70f90. [DOI] [PubMed] [Google Scholar]
- 28.S Khan K, Kunz R, Kleijnen J, Antes G. Systematic reviews to support evidence-based medicine. Mazurek Melnyk B. 2011 [Google Scholar]
- 29.Richardson DM, Rupp VA, Long KR, Urquhart MC, Ricart E, Newcomb LR, et al. Using lean methodology to decrease wasted RN time in seeking supplies in emergency departments. J Nurs Adm. 2014;44(11):606–11. doi: 10.1097/NNA.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 30.Mazzocato P, Holden RJ, Brommels M, Aronsson H, Backman U, Elg M, et al. How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children's hospital, Stockholm, Sweden. BMC Health Serv Res. 2012;12(28):1472–6963. doi: 10.1186/1472-6963-12-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vermeulen MJ, Stukel TA, Guttmann A, Rowe BH, Zwarenstein M, Golden B, et al. Evaluation of an Emergency Department Lean Process Improvement Program to Reduce Length of Stay. Ann Emerg Med. 2014;64:427–38. doi: 10.1016/j.annemergmed.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Naik T, Duroseau Y, Zehtabchi S, Rinnert S, Payne R, McKenzie M, et al. A structured approach to transforming a large public hospital emergency department via lean methodologies. J Healthc Qual. 2012;34(2):86–97. doi: 10.1111/j.1945-1474.2011.00181.x. [DOI] [PubMed] [Google Scholar]
- 33.Sanders JH, Karr T. Improving ED specimen TAT using Lean Six Sigma. Int J Health Care Qual Assur. 2015;28(5):428–40. doi: 10.1108/IJHCQA-10-2013-0117. [DOI] [PubMed] [Google Scholar]
- 34.Chan H, Lo S, Lee L, Lo W, Yu W, Wu Y, et al. Lean techniques for the improvement of patients’ flow in emergency department. World J Emerg Med. 2014;5(1):24–8. doi: 10.5847/wjem.j.issn.1920-8642.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dickson E, Anguelov Z, Vetterick D, Eller A, Singh S. Use of lean in the emergency department: a case series of 4 hospitals. Ann Emerg Med. 2009;54(4):504–10. doi: 10.1016/j.annemergmed.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 36.Ng D, Vail G, Thomas S, Schmidt N. Applying the Lean principles of the Toyota Production System to reduce wait times in the emergency department. Cjem. 2010;12(1):50–7. doi: 10.1017/s1481803500012021. [DOI] [PubMed] [Google Scholar]
- 37.Tejedor-Panchón F, Montero-Pérez FJ, Tejedor-Fernández M, Jiménez-Murillo L, Calderón De La Barca-Gázquez JM, Quero-Espinosa FB. Improvement in hospital emergency department processes with application of lean methods. Emergencias. 2014;26(2):84–93. [Google Scholar]
- 38.Lean-driven improvements eliminate waste, boost patient satisfaction in a matter of weeks. ED Manag. 2013;25(12):136–9. [PubMed] [Google Scholar]
- 39.Lean-driven improvements slash wait times, drive up patient satisfaction scores. ED Manag. 2012;24(7):79–81. [PubMed] [Google Scholar]
- 40.Dickson EW, Singh S, Cheung DS, Wyatt CC, Nugent AS. Application of lean manufacturing techniques in the Emergency Department. J Emerg Med. 2009;37(2):177–82. doi: 10.1016/j.jemermed.2007.11.108. [DOI] [PubMed] [Google Scholar]
- 41.Piggott Z, Weldon E, Strome T, Chochinov A. Application of Lean principles to improve early cardiac care in the emergency department. Cjem. 2011;13(5):325–32. doi: 10.2310/8000.2011.110284. [DOI] [PubMed] [Google Scholar]
- 42.Murrell KL, Offerman SR, Kauffman MB. Applying Lean: Implementation of a Rapid Triage and Treatment System. West J Emerg Med. 2011;12(2):184–91. [PMC free article] [PubMed] [Google Scholar]
- 43.El Sayed MJ, El-Eid GR, Saliba M, Jabbour R, Hitti EA. Improving Emergency Department Door to Doctor Time and Process Reliability: A Successful Implementation of Lean Methodology. Medicine. 2015;94(42):e1679. doi: 10.1097/MD.0000000000001679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kane M, Chui K, Rimicci J, Callagy P, Hereford J, Shen S, et al. Lean Manufacturing Improves Emergency Department Throughput and Patient Satisfaction. J Nurs Adm. 2015;45(9):429–34. doi: 10.1097/NNA.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 45.Eller A. Rapid assessment and disposition: applying LEAN in the emergency department. J Healthc Qual. 2009;31(3):17–22. doi: 10.1111/j.1945-1474.2009.00026.x. [DOI] [PubMed] [Google Scholar]
- 46.King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of Lean Thinking to health care. Emerg Med Australas. 2006;18(4):391–7. doi: 10.1111/j.1742-6723.2006.00872.x. [DOI] [PubMed] [Google Scholar]
- 47.White BA, Chang Y, Grabowski BG, Brown DF. Using lean-based systems engineering to increase capacity in the emergency department. West J Emerg Med. 2014;15(7):770–6. doi: 10.5811/westjem.2014.8.21272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Damato C, Rickard D. Using Lean-Six Sigma to reduce hemolysis in the emergency care center in a collaborative quality improvement project with the hospital laboratory. Jt Comm J Qual Patient Saf. 2015;41(3):99–107. doi: 10.1016/s1553-7250(15)41014-1. [DOI] [PubMed] [Google Scholar]
- 49.Dickson EW, Anguelov Z, Bott P, Nugent A, Walz D, Singh S. The sustainable improvement of patient flow in an emergency treatment centre using Lean. Int J Six Sigma and Competitive Advantage. 2008;4(3):289–304. [Google Scholar]
- 50.Timmons S, Coffey F, Vezyridis P. Implementing lean methods in the emergency department: the role of professions and professional status. J Health Organ Manag. 2014;28(2):214–28. doi: 10.1108/JHOM-10-2012-0203. [DOI] [PubMed] [Google Scholar]
- 51.Carter PM, Desmond JS, Akanbobnaab C, Oteng RA, Rominski SD, Barsan WG, et al. Optimizing clinical operations as part of a global emergency medicine initiative in Kumasi, Ghana: application of Lean manufacturing principals to low-resource health systems. Acad Emerg Med. 2012;19(3):338–47. doi: 10.1111/j.1553-2712.2012.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rees GH. Organisational readiness and Lean Thinking implementation: findings from three emergency department case studies in New Zealand. Health Serv Manage Res. 2014;27(1-2):1–9. doi: 10.1177/0951484814532624. [DOI] [PubMed] [Google Scholar]
- 53.Zohoor A, Pilevar-zadeh M. Study of speed of offering services in emergency department at Kerman Bahonar hospital in 2000. J Iran Unive Med Sci. 2003;10(35):413–20. [Google Scholar]
- 54.Weiss S, Steven J, Derlet R, Arndahl J, Ernst A, Richards J, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the national ED overcrowding study(NEDOCS) Academic Emerg Med. 2004;11(1):38–50. doi: 10.1197/j.aem.2003.07.017. [DOI] [PubMed] [Google Scholar]
- 55.Lambert MF, Shearer H. Developing a common language for evaluation questions in quality and safety improvement. Qual Saf Health Care. 2010;19(4):266–70. doi: 10.1136/qshc.2008.029009. [DOI] [PubMed] [Google Scholar]
- 56.Stang A. Randomized Controlled Trials—an Indispensible Part of Clinical Research. Dtsch Arztebl Int. 2011;108(39):661–2. doi: 10.3238/arztebl.2011.0661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sibbald B, Roland M. Understanding controlled trials: Why are randomised controlled trials important? Bmj. 1998;316(7126) doi: 10.1136/bmj.316.7126.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Salinas M, Lopez-Garrigos M, Santo-Quiles A, Gutierrez M, Lugo J, Lillo R, et al. Customising turnaround time indicators to requesting clinician: a 10-year study through balanced scorecard indicators. J Clin Pathol. 2014;67(9):797–801. doi: 10.1136/jclinpath-2014-202333. [DOI] [PubMed] [Google Scholar]
- 59.Amina S, Barrati A, Sadeghifar J, Sharifi M, Toulideh Z, Gorji HA, et al. Measuring and Analyzing Waiting Time Indicators of Patients' Admitted in Emergency Department: A Case Study. Glob J Health Sci. 2015;8:1. doi: 10.5539/gjhs.v8n1p143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang JL, Chen J, Wu M, Wang C, Fan WX, Mu JS, et al. Several time indicators and Barthel index relationships at different spinal cord injury levels. Spinal Cord. 2015;53(9):679–81. doi: 10.1038/sc.2014.206. [DOI] [PubMed] [Google Scholar]
- 61.Glasgow J. Introduction to Lean and Six Sigma approaches to quality improvement. Agency Healthcare Research Quality: Advancing Excellence in Health Care. 2011 [Google Scholar]
- 62.Joosten T, Bongers I, Janssen R. Application of lean thinking to health care: issues and observations. Int J Qual Health Care. 2009;21(5):341–7. doi: 10.1093/intqhc/mzp036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Goodridge D, Westhorp G, Rotter T, Dobson R, Bath B. Lean and leadership practices: development of an initial realist program theory. BMC Health Serv Res. 2015;7(15):015–1030. doi: 10.1186/s12913-015-1030-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Poksinska B. The current state of Lean implementation in health care: literature review. Qual Manag Health Care. 2010;19(4):319–29. doi: 10.1097/QMH.0b013e3181fa07bb. [DOI] [PubMed] [Google Scholar]
- 65.Jacobs G. "Take control or lean back?" Barriers to practicing empowerment in health promotion. Health Promot Pract. 2011;12(1):94–101. doi: 10.1177/1524839909353739. [DOI] [PubMed] [Google Scholar]
- 66.Aij KH, Simons FE, Widdershoven GA, Visse M. Experiences of leaders in the implementation of Lean in a teaching hospital-barriers and facilitators in clinical practices: a qualitative study. BMJ Open. 2013;3(10):e003605. doi: 10.1136/bmjopen-2013-003605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hung D, Martinez M, Yakir M, Gray C. Implementing a Lean Management System in Primary Care: Facilitators and Barriers From the Front Lines. Qual Manag Health Care. 2015;24(3):103–8. doi: 10.1097/QMH.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 68.Cummings TG, Worley CG. Organization development and change: Cengage learning. 2014. [Google Scholar]
- 69.Mazurowski J. Change management or resistance management? Radiol Manage. 1998;20(2):18–20. [PubMed] [Google Scholar]
- 70.van Rossum L, Aij KH, Simons FE, van der Eng N, Ten Have WD. Lean healthcare from a change management perspective. J Health Organ Manag. 2016;30(3):475–93. doi: 10.1108/JHOM-06-2014-0090. [DOI] [PubMed] [Google Scholar]
- 71.Philibert M, Deneux-Tharaux C, Bouvier-Colle MH. Can excess maternal mortality among women of foreign nationality be explained by suboptimal obstetric care? J Health Popul Nutr. 2008;26(3):280–94. doi: 10.1111/j.1471-0528.2008.01860.x. [DOI] [PubMed] [Google Scholar]