Abstract
Purpose
MPPC syndrome has been described as a syndrome that presents with chorioretinal coloboma, posterior megalolenticonus, persistent fetal vasculature, and chorioretinal coloboma. The purpose of our study is to report three patients who present with a variation of MPPC syndrome who each underwent pars plana vitrectomy, pars plana lensectomy, and amblyopic management. Clinical characteristics, ancillary test findings, and post-surgical functional results are compared to what is reported in the literature.
Methods
Retrospective review of medical records of patients who presented with microcornea, persistent fetal vasculature, chorioretinal coloboma, and microphthalmia who underwent surgical correction at Bascom Palmer Eye Institute.
Results
3 patients (6 eyes) were included, two males and one female. All patients were born full term, vaginally, and had no family history of genetic abnormalities affecting the eye. All patients had color fundus images, fluorescein angiography (FA) and echography. Four eyes underwent surgery. Following surgical intervention, patients demonstrated improved visual acuity, and improved functional status.
Conclusion and Importance
Patients with microcornea, PFV, chorioretinal coloboma, and microphthalmos, can benefit from surgical intervention when functional decline or media opacities are noted. Though difficult to assess accurate visual acuity and visual improvement pre-operatively and post-operatively, it is evident that our patients demonstrated improvement in functionality and vision following surgical intervention.
1. Introduction
Chorioretinal coloboma results from an incomplete closure of the embryonic fissure during the sixth or seventh week of fetal development.1 The extent to which vision is impacted is dependent on the size and location of the malformation, associated ocular defects, and syndromic systemic associations.1, 2, 3 Persistent fetal vasculature syndrome (PFV) is a congenital malformation in which there is failure of complete regression of the hyaloid artery and/or the primary vitreous vasculature, leading to a residual vascular stalk between the optic disc and posterior lens capsule.4 Microcornea (horizontal diameter <10 mm; vertical <11 mm) is often present in eyes with PFV.3, 4, 5, 6,24
A syndrome with microcornea, posterior megalolenticonus, persistent fetal vasculature, and chorioretinal coloboma (MPPC) was reported by Ranchod et al.2,4,7 They described the majority of patients presenting bilaterally.7 Posterior megalolenticonus was described as a dysmorphic lens that fills a significant amount of the vitreous cavity, obscuring the view of the fundus.7 Although there have been several syndromes reported in which one or more of the described conditions are present, no genetic cause has been directly linked to this association to date. Due to the poor visual prognosis, technical difficulties, and complicated post-operative management, there is no consensus on how and when to treat these infants.
In this study we described three patients who present with a variation of MPPC syndrome described by Ranchod et al.7 Each presented with microcornea, PFV, chorioretinal coloboma, microphthalmia, that underwent pars plana vitrectomy (PPV), pars plana lensectomy (PPL), and amblyopic management.7 Clinical characteristics, ancillary test findings and post-surgical functional results are compared to what is reported in the literature.
2. Materials and methods
A retrospective review of medical records was performed for patients who presented with a compilation of microcornea, PFV, chorioretinal coloboma, and microphthalmia, who subsequently underwent surgical procedures for resolution at Bascom Palmer Eye Institute (BPEI). Patients were found by reviewing surgical logs of patients with similar syndromic features. The University of Miami Miller School of Medicine institutional review board does not require the submission of a formal application in a case series involving three or fewer patients. It is adherent to the tenets of the Declaration of Helsiniki and is Health Insurance Portability and Accountability Act compliant.
The following data was extracted from the medical record: sex, age at surgery, perinatal information, laterality, ocular and systemic features, family history, axial length, corneal diameter, echography findings, pre-operative and last best corrected visual acuity (BCVA), pre-operative and last refraction, pre-operative and last functional description, pre-operative and last intraocular pressure (IOP), vitrectomy gauge, type of surgery performed, and follow-up time (Table 1).
Table 1.
Patient characteristics.
| Age | Sex | Ethnicity | Axial Length (mm) | Presence of Retrobulbar Cyst (Y/N) | Phenotype | FA | Pre-Sx BCVA | Pre-Sx Rx | Pre-Sx Function | Pre-Sx IOP | Last BCVA | Last Rx | Last IOP | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | ||||||||||||||
| OD | 3 years | M | Greek | 10.5 | Y | Chorioretinal coloboma, opaque microcornea 5.5 mm × 5 mm, microophthalmos, retrobulbar cyst | Not good image quality | NLP | Not possible | Noticed diminished vision | 10 mmHg | HM | Not possible | 19 mmHg |
| OS | 21.64 | N | Chorioretinal coloboma, subluxated cataract, microcornea 7.5 mm × 6.5 mm, cataract | Coloboma: hypo;PFV: hyper;FAZ: present | 2/200 | Not possible | 24 mmHg | 20/60 (far)20/20 (near) | +17.25 | 9 mmHg* | ||||
| Patient 2 | ||||||||||||||
| OD | 3 years | F | Saudi Arabian | 24.2 | N | Chorioretinal coloboma, subluxated crystalline lens, microcornea 9 mm, microophthalmos, closed angles. |
Coloboma: hypo PFV: hypo; FAZ: not identified |
8/400 | Not possible | Non-independent | 27 mmHg | Fix and follow | Not possible | 18* |
| OS | 28.2 | N | Not done | Fix and follow (difficult) | Not possible | 50 mmHg | Fix and follow | Not possible | 28* | |||||
| Patient 3 | ||||||||||||||
| OD | 6 weeks | M | African American | 19.8 | N | Chorioretinal coloboma, subluxated crystalline lens, microcornea 7 mm, microophthalmos, closed angles. | Coloboma: hypo PFV: stalk hypo, anterior insertion hyper | Fix and follow | −12 D | Plays and uses toys | 16 mmHg | HM | Not possible | STP |
| OS | 22.4 | N |
Coloboma: hypo PFV: stalk 6hypo; anterior insertion hyper; FAZ: present |
20/800 | −12 D | 22 mmHg | 20/250 ecc | Not possible | STP | |||||
Summarized information of the pre and post surgical functional status of our three cases with microcornea, persistent fetal vasculature, chorioretinal coloboma, and microophthalmia
BCVA-best corrected visual acuity; EL-endolaser; FAZ-foveal avascular zone; HM-hand motion; IOP- intraocular pressure; IVB- intravitreal bevacizumab; NLDO- nasolacrimal duct obstruction; NLP- no light perception; PPL-pars plana lensectomy; PPV- pars plana vitrectomy; Rx-refraction; STP- soft to palpation; STT-sub-tenon's triamcinolone; Sx-surgery.
*using glaucoma eyedrops.
** 3 months of follow up at BPEI. Now IOP control in Saudi Arabia by glaucoma specialist.
3. Results
A total of three patients (six involved eyes) were included in this series. Two males and one female. The mean age at the time of surgery was 3 years old. All patients were born full term, vaginally, and had no self-reported family history of childhood blindness. All patients had color fundus images, fluorescein angiography (FA) and echography. Four eyes underwent surgery.
3.1. Case 1
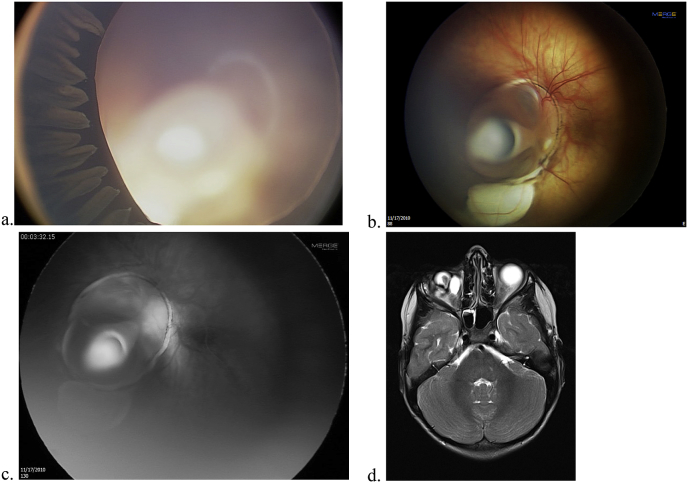
A 3 year-old male of Greek descent was born at 38 weeks gestation and 3175 g. The patient displayed no associated systemic features. At presentation, he had nystagmus. The clinical examination pre and post surgically, as well as the fluorescein angiography (FA) findings are displayed on Table 1. MRI and B-scan showed the coloboma, and a large retrobulbar cyst, on the right eye. He underwent a PPV, PPL, and 360° prophylactic endolaser (EL) with no tamponade to the left eye to remove the cataract and the PFV that caused traction. The patient underwent a sclerosing procedure and drainage of the retrobulbar cyst of the right eye for progressive exophthalmos. He is being monitored closely by the pediatric glaucoma service while controlling the IOP with timolol maleate 0.5% bid on the left eye (Fig. 1a–d).
Fig. 1.
Patient from case 1. a. Elongated ciliary processes with lens opacity and microspherophakia-like appearance due to traction. b. Short stalk of Persistent fetal vasculature with a retinochoroidal coloboma. c. Hyperfluorescence of the stalk and coloboma. d. Retrobulbar cyst of the right eye with microopthalmos.
3.2. Case 2
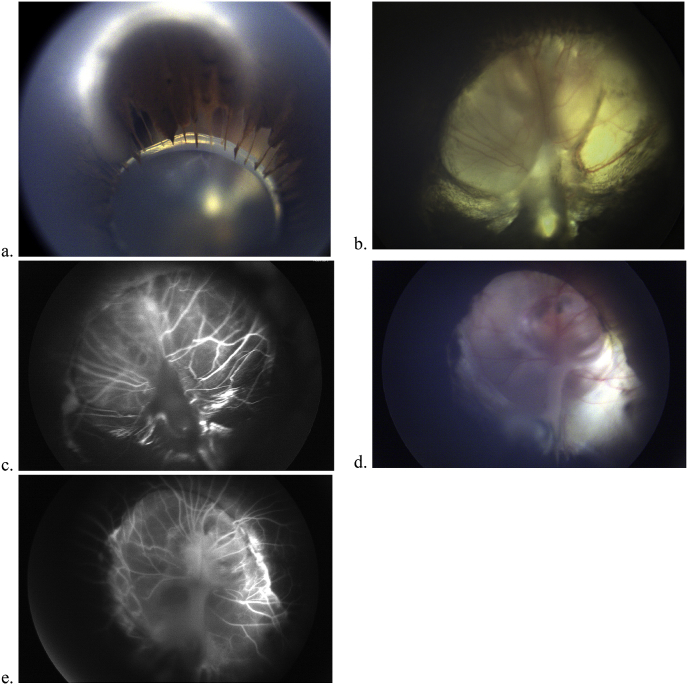
A 3 year-old female from Saudi Arabia born at 42 weeks gestation and 2260 g. She had a nasolacrimal obstruction diagnosed before with placement of a Crawford stent. They were advised not to receive any type of intraocular treatment upon referral nor refractive correction. She was seen at BPEI seeking a second opinion. Systemic associations included syndactyly on both fingers and toes and developmental delay. The clinical examination pre and post surgically, as well as the FA description are found on Table 1. The patient underwent bilateral PPV, PPL, and intravitreal bevacizumab (IVB) on the same day. Glasses and patching of alternate eyes were recommended to improve visual acuity. The last IOP of the right eye was 18 mmHg and 28 mmHg of the left eye, using latanoprost 0.005% and apraclonidine 0.5% on the left eye each one time daily, and dorzolamide-timolol 22.3–6.8 mg/mL bilaterally twice daily. She is followed u in Saudi Arabia for IOP control with a glaucoma specialist. This patient underwent genetic testing by whole exome sequencing where no genetic mutation related to the described phenotype was identified (Fig. 2a–e).
Fig. 2.
a. Patient from Case 2. Inferiorly displaced small lens with elongated ciliary processes. b. Patient from Case 2. Retino-choroidal coloboma with glial tissue and stalk. c.Patient from Case 2. The stalk does not hyperfluoresce in this patient. d. Coloboma that occupies the posterior pole and the macula. Patient from Case 3. e. The stalk has mild hyperfluorescence. Patient from Case 3.
3.3. Case 3
A 6 weeks-old African American male born at 41 weeks gestation and 3764 g who required oxygen for four days with a blood transfusion was referred by the pediatrician. Systemic associations included pelviectasis of the kidney, transitory thrombocytopenia at birth, developmental delay, and torticollis. When the patient reached 3 years old he presented for eye evaluation with nystagmus. Clinical and FA details are shown in Table 1. He had bilateral retrobulbar cysts noted on echography. He received treatment with PPV, PPL, and 360° EL on the right eye. He had no operative intervention on the left eye. He was recommended to use glasses with bifocal lenses and intermittent patching of the left eye daily (Fig. 2d and e).
4. Discussion
The unusual association of microphthalmos, microcornea, PFV, and chorioretinal coloboma has been described separately in the literature. Lee et al. reported that corneal diameters have a strong correlation to total axial length, supporting the prevalence of coexistence of microcornea and microphthalmos.8 A similar association of ocular findings was described in a case report by Seitz et al. whereby the patient presented with bilateral congenital dentiform cataracts, microcornea, uveal colobomas, and PFV.9 Ranchod et al. succeeded at describing MPPC syndrome as a phenotype consisting of: microcornea, posterior megalolenticonus, persistent fetal vasculature, and chorioretinal coloboma.7 Variations are seen in the degree of the extension of the coloboma in the length of both cornea and the axial length, in the presence or absence of PFV, and in the lens measurements (megalolenticonus). We add to this syndromic description of MPPC syndrome, the presence of retrobulbar cysts. A short report by Bowe et al. similarly mentioned the presence of retrobulbar cysts in association with these ocular findings, but does not discuss management.10 The presence of retrobulbar cysts further worsens the patient's final visual acuity and increases the risk of retinal detachment.5
As documented in the literature, PFV has been enucleated for suspicion of retinoblastoma, development of intractable glaucoma or progression to pthisis bulbi.7 Phacoantigenic uveitis and phacolytic glaucoma have also been reported during the natural progression of eyes with PFV, supporting the case for early surgical intervention.7 In patients with MPPC syndrome, there is a dysmorphic lens that fills much of the vitreous cavity, preventing clear visualization of the fundus or formation of clear images by the retina.7 The ciliary processes can obscure the visual axis, and therefore, clearance of the visual axis is needed.
Hypothetical explanations have been made addressing the physio pathological process that leads to multiple malformations to coexist. As described in previous studies, it is possible that the failure of the choroidal fissure to close could be associated with a stimulus preventing regression of the fetal eye vasculature.2 Patients with PFV syndrome often have associated microcornea. The residual vascular stalk seen in PFV occupies space within the eye, causing the anterior and posterior segments to fuse together, arresting proper growth and development of many structures of the eye, including the cornea.4,11,12
While Ranchod et al. were the first to describe what they labeled as MPPC syndrome, there are other publications that report similar findings.2,4,7 Morning glory syndrome manifests with PFV and lens dislocation in association with an optic nerve coloboma.13 We did not see by echography the megalolenticonus, but we evidenced a short stalk adhered to the posterior lens capsule (as opposed to a classical presentation with a large stalk) that, as described by Ranchod et al., is a highly suggestive clinical sign of megalolenticonus.7 Also, the lens was inferiorly subluxated associated to the short PFV and had elongated ciliary processes.
Retrobulbar cysts have been reported alone and in association with several ocular malformations including microphthalmos and colobomas.14 Retrobulbar cysts repeatedly have been shown to worsen visual acuity and increase the potential for retinal detachment in patients with coexisting chorioretinal coloboma.1,5,14,15 Management focuses on early identification and correction of other ocular problems.5
Visual acuity measurements is difficult in children and in our center it is always performed by a pediatric ophthalmologist with Snellen, Lea, or Teller depending on the age group. Visual acuity is greatly impacted by whether the patient has microphthalmos or not, in that patients without microphthalmos have a better visual prognosis.1,3,20 Also, measurements of axial length and refraction are complicated in the setting of retinal pathological conditions such as the case of coloboma.1 Therefore, axial measurement is not totally exact as the only way to calculate it is measuring some part of the excavation caused by the coloboma giving larger measurements. This is the reason why we decided intervention and final results of the procedures by functional status as referred by the parents and from what we can obtain at the outpatient visit.
FA is performed on a regular basis in our clinic. The fibrovascular stalk can be hyperfluorescent or not depending on the status of the intrinsic vasculature. FA of patients with PFV shows the retinal vessels dragged anteriorly with peripheral retinal capillary nonperfusion.9 Coloboma can be associated to vascular occlusions seen on FA.21 Of note, case 2 had hypofluorescent stalk with absence of filling inner vasculature as opposed to hyperfluorescent stalks on cases 1 and 3. We cannot conclude that it is age related. None of our patients displayed vascular occlusion. Interestingly, the two left eyes that had measurable final BCVA from patient 1 and 3, both had FAZ identifiable. This may be a marker to discuss final visual acuity with the family. Further studies are necessary to see consistency of these results.
There is no current definitive treatment for any of these conditions, however, treatment focuses on enhancing the present functional status. Ranchod et al. found that appropriate surgical intervention to clear the visual axis significantly improved visual function.7 The improvement is reliant on retinal development and treatment of other ocular deformities.22 Thus, eliminating what obscures central vision (cataract, lens subluxation, vascular stalk [PFV]), and establishing prompt rehabilitation (contact lens, patching) has proven to be effective in these patients as long as there is remaining chorioretinal tissue that allows for eccentric vision. Multidisciplinary treatment is mandatory: retina, glaucoma, oculoplastics, and pediatric ophthalmologists are equally needed for this purpose.
The treatment for retrobulbar cyst has been discussed elsewhere. Options include aspiration, enucleation of the microphthalmic eye with cyst removal, cyst excision with globe preservation, or cyst sclerosis.15,23 The patient described in case 1 underwent a cyst drainage and sclerosing procedure. The procedure was deemed to be successful as the post-operative MRI demonstrated that the sclerosed cyst remained at a small size within the right lateral orbit.
Part of the objective of the current report is to evaluate the connection among all four ocular deformities and discuss the surgical correction and medical treatment that each patient underwent. All patients underwent PPV, PPL, with or without prophylactic endolaser and/or intravitreal bevacizumab (IVB) and/or sub-Tenon's triamcinolone (STT).
The preferred placement of trocars is the anterior chamber (limbal ports) to avoid abnormal ciliary body and vitreous attachments that could complicate the surgery. The pars plana vitrectomy is used for elimination of the paracentral stalk that subluxates the lens, and removal of existent tractional membranes when present (case 3) with variable success. It is of note, that due to the displacement of the lens due to traction, elongated ciliary processes are usually seen in this setting. In all of these patients, the lensectomy was performed avoiding manipulation of the ciliary body to avoid inflammatory reaction and secondary hypotonia. The lensectomy's primary purpose is to gain access for removal of the persistent fetal vasculature. The addition of prophylactic endolaser, intravitreal bevacizumab (to reduce vasodilators that worsen inflammation while avoiding intraocular steroids to prevent IOP rise) and STT for inflammation control are regularly used by the surgeon (A.M.B.) in complex pediatric cases. The benefits or risks of the prophylactic laser in colobomas may be argued. The rationale for its use is that there is incomplete removal of the hyaloid due to the complex vitreoretinal interface. Because patients present at a very young age, it is difficult for patients to communicate visual changes, making our assessment more challenging.5 Though difficult to assess accurate visual acuity and visual improvement pre-operatively and post-operatively, our patients demonstrated improvement in functionality and vision following surgical intervention. Ranchod et al. demonstrated the achievement of functional vision in 80% of patients who underwent a variation of these surgical procedures.7 Studies show that despite the successful anatomical correction of the procedure, visual acuity remains poor due to the comorbid deformities, one of which is a retrobulbar cyst.5,20 It is important to emphasize the importance of alternate patching (or unilateral patching in case there is only one aphakic eye), along with tight intraocular pressure both done by a pediatric ophthalmologist and glaucoma specialist to achieve better results.
Our study had several limitations including the retrospective nature of chart review, inability to accurately measure visual acuity and/or refraction, and difficulty extrapolating results due to the short series. Because it was difficult to measure refraction in each eye, our results are solely functional. Additionally, the patients each had poor vision prior to the procedure, and thus it is difficult to compare pre-operative and post-operative vision. Each patient studied was a referral to our tertiary referral center.
Additionally, communication with the patient's family is vital to assess whether they are willing and determined to undergo the procedure. This is because long-term follow-up is required for optimal success, and thus if families are non-compliant the results will be sub-optimal.
In conclusion, our study showed that patients with microcornea, persistent fetal vasculature, chorioretinal coloboma, and microphthalmos, can benefit from surgical intervention including PPV, PPL, IVB, and STT. FA showing presence of FAZ can help determine visual potential. Additionally, we stated that the presence of a retrobulbar cyst must be considered as part of the syndromic phenotype. The presence of a retrobulbar cyst further complicates the ocular abnormalities, worsening visual acuity and likely increasing the risk for retinal detachment in the future. To date, there is an underwhelming amount of research outlining the most effective treatment options in patients who present with these manifestations, and thus further research should be focused on the surgical outcomes in the long-term.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Acknowledgements and Disclosures
Authors’ contributions
All authors have contributed substantially to the conception and design of the work, have drafted and revised the manuscript critically, have final approval of the final version, and agree to be accountable for all aspects of the work.
Conflicts of interest
The following authors have no financial disclosures: L.R., L.CE., C.A., C.M., K.T., T.C., A.B.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Funding
No funding or grant support
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2019.01.005.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Uhumwangho O.M., Jalali S. Chorioretinal coloboma in a paediatric population. Eye. 2014;28(6):728–733. doi: 10.1038/eye.2014.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takkar B., Chandra P., Kumar V., Agrawal R. A case of iridofundal coloboma with persistent fetal vasculature and lens subluxation. J AAPOS. 2016;20(2):180–182. doi: 10.1016/j.jaapos.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Hornby S.J., Adolph S., Gilbert C.E., Dandona L., Foster A. Visual acuity in children with coloboma: clinical features and a new phenotypic classification system. Ophthalmology. 2000;107(3):511–520. doi: 10.1016/s0161-6420(99)00140-2. [DOI] [PubMed] [Google Scholar]
- 4.Zigler J.S., Jr., Valapala M., Shang P., Hose S., Goldberg M.F., Sinha D. betaA3/A1-crystallin and persistent fetal vasculature (PFV) disease of the eye. Biochim Biophys Acta. 2016;1860(1 Pt B):287–298. doi: 10.1016/j.bbagen.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venincasa V.D., Modi Y.S., Aziz H.A. Clinical and echographic features of retinochoroidal and optic nerve colobomas. Invest Ophthalmol Vis Sci. 2015;56(6):3615–3620. doi: 10.1167/iovs.15-16596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nischal K.K. Springer; New York: 2002. Corneal abnormalities. Pediatric ophthalmology and strabismus 2e; pp. 391–429. [Google Scholar]
- 7.Ranchod T.M., Quiram P.A., Hathaway N., Ho L.Y., Glasgow B.J., Trese M.T. Microcornea, posterior megalolenticonus, persistent fetal vasculature, and coloboma: a new syndrome. Ophthalmology. 2010;117(9):1843–1847. doi: 10.1016/j.ophtha.2009.12.045. [DOI] [PubMed] [Google Scholar]
- 8.Lee J.S., Lee J.E., Shin Y.G., Choi H.Y., Oum B.S., Kim H.J. Five cases of microphthalmia with other ocular malformations. Kor J Ophthalmol. 2001;15(1):41–47. doi: 10.3341/kjo.2001.15.1.41. [DOI] [PubMed] [Google Scholar]
- 9.Seitz B., Naumann G.O. Bilateral congenital dentiform cataract and extreme microcornea in eyes with uveal colobomas and persistent hyperplastic primary vitreous. Br J Ophthalmol. 1996;80(4):378–379. doi: 10.1136/bjo.80.4.378-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bowe T., Rahmani S., Yonekawa Y. Endoscopic vitrectomy for microcornea, posterior megalolenticonus, persistent fetal vasculature, coloboma syndrome. Ophthalmology. 2017;124(12):1742. doi: 10.1016/j.ophtha.2017.07.028. [DOI] [PubMed] [Google Scholar]
- 11.Hartnett M.E., Trese M., Capone A. Jr., editors. Pediatric Retina: Medical and Surgical Approaches. Lippincott Williams & Wilkins; Philadelphia, PA: 2005. p. 439. [Google Scholar]
- 12.Haddad R., Font R.L., Reeser F. Persistent hyperplastic primary vitreous. A clinicopathologic study of 62 cases and review of the literature. Surv Ophthalmol. 1978;23(2):123–134. doi: 10.1016/0039-6257(78)90091-7. [DOI] [PubMed] [Google Scholar]
- 13.Lytvynchuk L.M., Glittenberg C.G., Ansari-Shahrezaei S., Binder S. Intraoperative optical coherence tomography assisted analysis of pars Plana vitrectomy for retinal detachment in morning glory syndrome: a case report. BMC Ophthalmol. 2017;17(1):134. doi: 10.1186/s12886-017-0533-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y.N., Patel C.K., Kertes P.J., Devenyi R.G., Blaser S., Lam W.C. Retinal detachment and retrobulbar cysts in a large cohort of optic nerve coloboma. Retina. 2018;38(4):692–697. doi: 10.1097/IAE.0000000000001594. [DOI] [PubMed] [Google Scholar]
- 15.KK M. Retrobulbar bilateral optic nerve colobomatous cysts; MRI & CT imaging features. Journal of Cancer Prevention & Current Research. 2016;4 [Google Scholar]
- 20.Ramezani A., Dehghan M.H., Rostami A. Outcomes of retinal detachment surgery in eyes with chorioretinal coloboma. J Ophthalmic Vis Res. 2010;5(4):240–245. [PMC free article] [PubMed] [Google Scholar]
- 21.Shapiro M.J., Chow C.C., Blair M.P., Kiernan D.F., Kaufman L.M. Peripheral nonperfusion and tractional retinal detachment associated with congenital optic nerve anomalies. Ophthalmology. 2013;120(3):607–615. doi: 10.1016/j.ophtha.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 22.Verma A.S., Fitzpatrick D.R. Anophthalmia and microphthalmia. Orphanet J Rare Dis. 2007;2:47. doi: 10.1186/1750-1172-2-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salsamendi J., Ghosh S., Ko A.C., Pereira K., Yang E.Y., Alabiad C. Percutaneous ethanolamine sclerotherapy of a retrobulbar cyst in a child with microphthalmos and proptosis. J Vasc Intervent Radiol. 2015;26(11):1658–1659. doi: 10.1016/j.jvir.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Mashige K.P. A review of corneal diameter, curvature and thickness values and influencing factors. African Vision and Eye Health. 2013;72(4):185–194. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.