Abstract
Purpose
To report one case of homonymous paracentral scotoma with corresponding optical coherence tomography (OCT) findings in a young woman after injury to the left occipital lobe tip.
Observations
A young woman with past medical history of Hodgkin's lymphoma and large B-cell lymphoma metastatic to the left occipital lobe status post resection presented to the eye clinic with a chief complaint of a “blind spot” in the right eye since her surgery. Humphrey visual field (HVF) showed a right homonymous paracentral scotoma corresponding to the non-decussating and decussating optic radiation for central vision originating from the left lateral geniculate nucleus (LGN). OCT confirmed atrophy of the right nasal hemifovea with fibers originating from the papillomacular bundle and the left temporal hemifovea with fibers originating from the superior temporal segment of the optic nerve. These fibers correspond to the central vision involved with the left posterior occipital lobe tip.
Conclusions and Importance
We report a case of right homonymous central vision loss as a result of injury to the left posterior occipital lobe tip with certain unique features. Here, a small lesion in the posterior visual pathway led to a relatively large loss of ganglion cell layer.
Keywords: Ganglion cell layer, Nerve fiber layer, Homonymous hemianopia, Thinning
1. Introduction
Previous studies have demonstrated topographic correlation between lesions in the posterior visual pathway and retinal nerve fiber layer (RNFL)1,2 or ganglion cell layer (GCL)3, 4, 5, 6, 7, 8, 9, 10 thinning on optical coherence tomography (OCT). Several distributions of retinal thinning have been described corresponding with homonymous hemianopia or homonymous quadrantanopsia1, 2, 3, 4, 5, 6, 7, 8,10; however, to our knowledge fewer studies have examined the relatively rare case of isolated macular-involving scotoma from injury to the occipital tip.9 We describe this pattern of RNFL and retinal ganglion cell (RGC) complex loss from retrograde trans-synaptic neuronal degeneration.
1.1. Case report
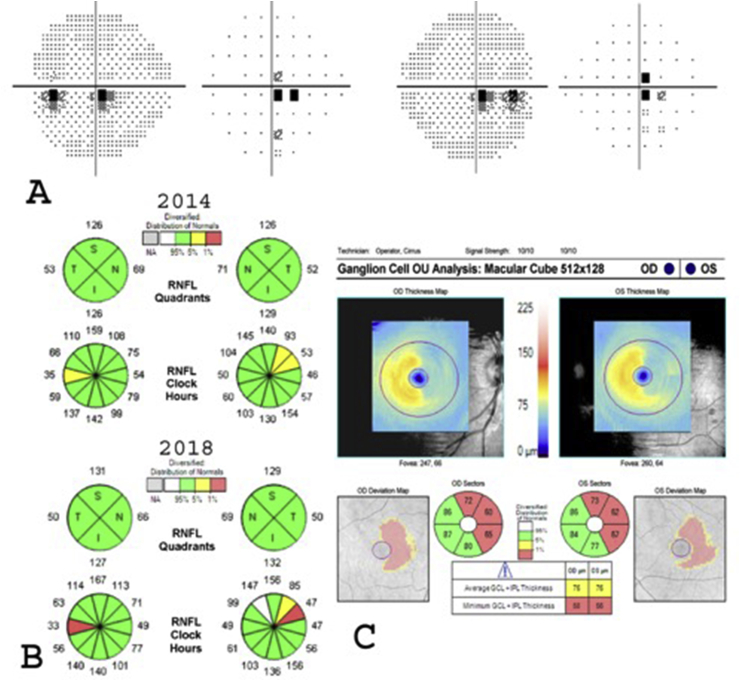
A 23-year-old female with a past medical history of Hodgkin's lymphoma and diffuse large B-cell lymphoma metastatic to left occipital lobe status post resection (Fig. 1A–D) presented to the eye clinic with a chief complaint of a “blind spot” in the right eye since her surgery seven years ago. On presentation, visual acuity was 20/25 in the right eye and 20/30 in the left. No afferent pupillary defect was present. Slit lamp examination was unremarkable; dilated fundoscopy showed mild bilateral temporal atrophy of the optic nerve. Humphrey visual field (HVF) analysis revealed right homonymous paracentral scotoma (Fig. 2A) consistent with prior occipital lobe pathology. OCT demonstrated normal average RNFL thickness (94 μm OD and 95 μm OS), but segmental analysis showed mild focal temporal thinning OD and superotemporal thinning OS (Fig. 2B). The focal RNFL thinning slowly progressed over seven years of follow-up. The papillomacular (PM) bundle damage OD corresponded to temporal visual field defect in the right eye, while superotemporal RNFL damage OS corresponded to inferior nasal visual field defect OS. OCT-RGC showed more localized left homonymous RGC loss, corresponding to the NFL thinning and VF defects (Fig. 2C). HVF testing was stable for five years of follow-up.
Fig. 1.
Magnetic Resonance Imaging Showing Left Occipital Lobe Lymphoma Before and After Resection. A: Axial post contrast T1 weighted image demonstrates a dural based left occipital mass (arrow), with severe mass effect on the left occipital lobe before surgery. B: Axial postcontrast T1 weighted image demonstrates no abnormal enhancement in the surgical bed (arrow) to suggest residual or recurrent tumor, C & D: Six years after surgery, axial FLAIR (C) and T2 weighted (D) images demonstrate small focal encephalomalacia and gliosis at the posterior tip of the left occipital lobe (arrows).
Fig. 2.
The visual field defect on Humphrey visual field (HVF) with corresponding retinal nerve fiber layer (RNFL) thinning on optical coherence tomography (OCT). A: HVF showing a right central scotomatous homonymous visual defect. B: OCT-nerve fiber layer (OCT-NFL) showing sectoral peripapillary RNFL thinning OU. OD with central papillomacular (PM) bundle thinning, while OS with superior temporal RNFL thinning. Noted focal RNFL thinning slowly progressed from 2014 to 2018. C: OCT-retinal ganglion cell (OCT-RGC) complex showing ganglion cell layer + inner plexiform layer (GCL + IPL) complex thinning of nasal hemifovea OD and temporal hemifovea OS.
2. Discussion
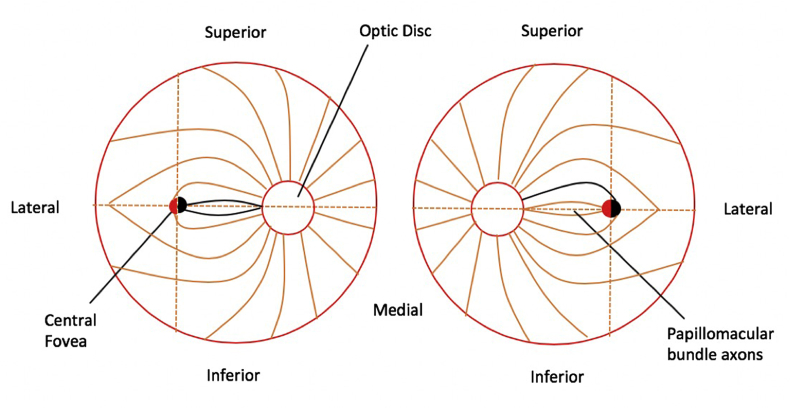
We present a unique case of injury to the left posterior tip of the occipital lobe after resection of lymphoma, resulting in a small central homonymous scotoma with relatively large corresponding atrophy of the nasal and temporal RGC and macular fibers in the right and left eyes, respectively (Fig. 3). Further imaging with OCT showed macular GCL + inner plexiform layer (IPL) hemi-foveal thinning with good anatomical correlation of the decussated and non-decussated fibers in the left lateral geniculate nucleus (LGN). This hemi-foveal thinning corresponded to the central visual field defects observed on HVF. These results are consistent with prior work on trans-synaptic degeneration first described by Matthews et al. after enucleation of macaque monkeys.11
Fig. 3.
Schematic of retinal nerve fiber layer thinning. Schematic of bilateral temporal segmental nerve fiber thinning in the optic nerve corresponding to nasal macular retinal ganglion cell (RGC) injury (black line) and nasal hemifovea injury (black semicircle) consistent with temporal visual field defect in the right eye, whereas superior temporal fiber thinning corresponding to superior temporal macular RGC injury (black line) and temporal hemifovea injury (black semicircle) is consistent with inferior nasal visual field defect in the left eye.
Since the introduction of OCT, several studies have identified patterns of RNFL loss that correspond with anatomic lesions of the posterior visual pathways.1, 2, 3, 4, 5, 6, 7, 8, 9, 10 Most commonly, homonymous hemianopsia and quadrantanopsia have been described1, 2, 3, 4, 5, 6, 7, 8, but isolated occipital tip injury with trans-synaptic retrograde degeneration is rare. The only other reported case is by Meier et al., who describe a similar pattern to ours: after presenting with headaches and dense homonymous hemianopia, the patient eventually underwent surgical resection of a circumscribed occipital lobe abscess.9 Two years later, there was significant improvement in his visual field deficits but persistent small inferior homonymous scotoma. The timeline (two years after surgery) and size of GCL atrophy is nearly identical to ours, suggesting that the occipital tip represents a location at which a small-sized lesion can cause significant retinal thinning with a relatively small scotoma.
GCL + IPL has been established as a sensitive marker of retinal thinning from acquired damage to the posterior visual pathways.3, 4, 5, 6, 7, 8, 9, 10 This is intuitive, as half of all RGCs exist within the fovea and are responsible for central vision. Like Herro et al. and Shin et al., we also found there to be significant GCL thinning in the absence of any RNFL atrophy, again confirming that GCL is a more specific measure of inner retinal thinning from retrograde neuronal degeneration.4,7
Not all patients develop retinal thinning after occipital lobe injury, and the reasons for this are unknown. Jindahra et al. previously reported that size of the lesion was predictor of retinal ganglion thinning, except where the lesion affected the lateral geniculate nucleus.1 In this instance, even a small lesion produce retinal thinning. Our case is consistent with this finding, suggesting that the location of the lesion (either in the occipital lobe or the LGN) matters more than the size of the lesion. Another possibility is due to structural or neurotransmitter changes in the lateral geniculate nucleus that vary among individuals. For future studies, we would consider conducting a high-resolution neuroimaging study of the lateral geniculate body to observe if any remodeling occurs after retrogeniculate lesions.
One limitation of this study is that the patient only presented to our clinic two years after her surgery, so we are unable to determine if the visual field defect was initially larger or smaller than what we observed. However, we note that the patient did not report any visual field changes until she presented for evaluation of her symptomatic scotoma. Additionally, we were not able to perform serial GCL + IPL measurements due to reimbursement issues in patient's earlier follow-up visits, so we are unsure what the exact timeframe of the GCL changes are. However, Yamashista et al. reported a time course of GCL + IPL thinning of 0.36 micrometers per month, and our single measurement is on the multivariable regression line from this study.6
We recommend GCL + IPL thinning as a sensitive measure to detect retinal pathology in individuals with retrogeniculate lesions.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Conflicts of interest
The following authors have no financial disclosures: S.NW., S.A., J.S., S.S., C.Z.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Funding
No funding or grant support.
Acknowledgements
None.
References
- 1.Jindahra P., Petrie A., Plant G.T. The time course of retrograde trans-synaptic degeneration following occipital lobe damage in humans. Brain : J Neurol. 2012;135(Pt 2):534–541. doi: 10.1093/brain/awr324. [DOI] [PubMed] [Google Scholar]
- 2.Mehta J.S., Plant G.T. Optical coherence tomography (OCT) findings in congenital/long-standing homonymous hemianopia. Am J Ophthalmol. 2005;140(4):727–729. doi: 10.1016/j.ajo.2005.03.059. [DOI] [PubMed] [Google Scholar]
- 3.Moon H., Yoon J.Y., Lim H.T., Sung K.R. Ganglion cell and inner plexiform layer thickness determined by spectral domain optical coherence tomography in patients with brain lesions. Br J Ophthalmol. 2015;99(3):329–335. doi: 10.1136/bjophthalmol-2014-305361. [DOI] [PubMed] [Google Scholar]
- 4.Shin H.Y., Park H.Y., Choi J.A., Park C.K. Macular ganglion cell-inner plexiform layer thinning in patients with visual field defect that respects the vertical meridian. Graefe's Arch Clin Exp Ophthalmol = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2014;252(9):1501–1507. doi: 10.1007/s00417-014-2706-3. [DOI] [PubMed] [Google Scholar]
- 5.Yamashita T., Miki A., Goto K. Retinal ganglion cell atrophy in homonymous hemianopia due to acquired occipital lesions observed using cirrus high-definition-OCT. J Ophthalmol. 2016;2016:2394957. doi: 10.1155/2016/2394957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yamashita T., Miki A., Iguchi Y., Kimura K., Maeda F., Kiryu J. Reduced retinal ganglion cell complex thickness in patients with posterior cerebral artery infarction detected using spectral-domain optical coherence tomography. Jpn J Ophthalmol. 2012;56(5):502–510. doi: 10.1007/s10384-012-0146-3. [DOI] [PubMed] [Google Scholar]
- 7.Herro A.M., Lam B.L. Retrograde degeneration of retinal ganglion cells in homonymous hemianopsia. Clin Ophthalmol. 2015;9:1057–1064. doi: 10.2147/OPTH.S81749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keller J., Sanchez-Dalmau B.F., Villoslada P. Lesions in the posterior visual pathway promote trans-synaptic degeneration of retinal ganglion cells. PLoS One. 2014;9(5):e97444. doi: 10.1371/journal.pone.0097444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meier P.G., Maeder P., Kardon R.H., Borruat F.X. Homonymous ganglion cell layer thinning after isolated occipital lesion: macular OCT demonstrates transsynaptic retrograde retinal degeneration. J Neuro Ophthalmol. 2015;35(2):112–116. doi: 10.1097/WNO.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell J.R., Oliveira C., Tsiouris A.J., Dinkin M.J. Corresponding ganglion cell atrophy in patients with postgeniculate homonymous visual field loss. J Neuro Ophthalmol. 2015;35(4):353–359. doi: 10.1097/WNO.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 11.Matthews M.R. Further observations on transneuronal degeneration in the lateral geniculate nucleus of the macaque monkey. J Anat. 1964;98:255–263. [PMC free article] [PubMed] [Google Scholar]