Abstract
Pseudoaneurysm of the right ventricular outflow tract (RVOT) has been reported as a rare complication of RVOT reconstruction performed using conduit replacement or patch repair. The RVOT needs to be followed up on echocardiography and if aneurysm a large aneurysm forms, it needs to be operated. Usually progression of aneurysm is slow. Rarely, it may present with symptoms secondary to the compression of adjoining mediastinal structures or thrombus formation inside the aneurysm. We report two cases of rapidly progressing massive RVOT aneurysm needing early surgical intervention. Both patients had ventricular septal defect (VSD) closure and right ventricle to pulmonary artery conduit placement. In both patients Contegra pulmonary valved conduit (Medtronic) had been used.
Keywords: aneurysm, RVOT, bacterial endocarditis, conduit
Case Descriptions
Case 1: Twenty six years old male, a case of large perimembranous VSD, pulmonary atresia with patent ductus arteriosus (PDA). He underwent total correction withright ventricle (RV) to pulmonary artery (PA) conduit at the age of 22 years. His post-operative period was uneventful. Predischarge echocardiography showed no residual shunt, normal functioning RV to PA conduit with normal ventricular function. Four years post surgical intervention he presented in emergency with early fatigability; swelling all over the body including ascites and breathing difficulty. There was no history of fever. These symptoms started 3 months proir and but rapid progression happened in previous 2 weeks. On examination, he was afebrile. There was tachycardia (HR 120/minute), low volume pulses (BP 90/70mmHg), tachypnea, decreased air entry on left side of chest, cardiomegaly and features of right sided failure (raised jugular venous pressure, parasternal heave, hepatomegaly, ascites, edema). Twelve lead electrocardiograms showed sinus tachycardia, right axis deviation and right bundle branch block pattern. Chest x-ray (figure 1) showed cardiomegaly with large homogenous opacity in left upper parasternal area.
Figure 1.
Chest X-ray (postero-anterior view) of case 1 showing cardiomegaly, large homogenous opacity in left hemithorax
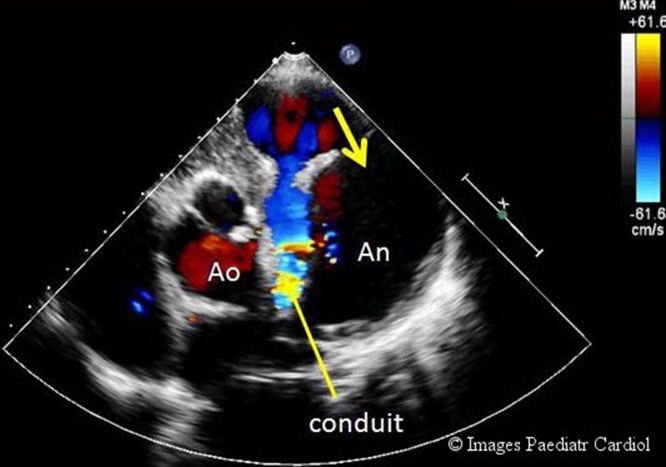
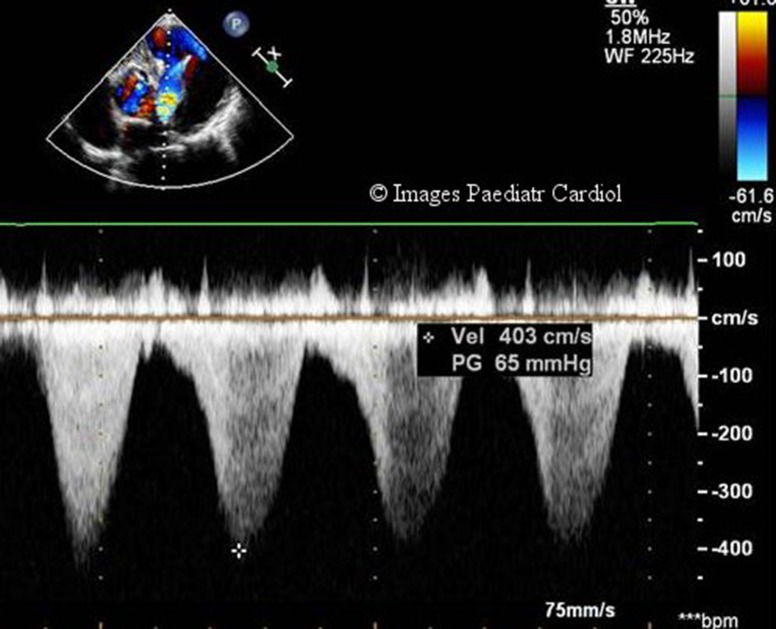
Echocardiography showed dilated right atrium and ventricle, moderate tricuspid regurgitation (high pressure), RV dysfunction, massive aneurysm of RVOT arising just below RV-PA conduit junction (figure 2) with severe distal conduit obstruction (peak gradient 65mmHg - figure 3).
Figure 2.
Echocardiographic images of case 1. Parasternal short axis view at the level of great vessels with color flow mapping showing aneurysm communicating with RVOT just proximal to RV-conduit junction (thick and yellow arrow). Aneurysm is causing compression of conduit. Turbulent flow is seen in conduit (long thin yellow arrow). Ao-aorta, An-aneurysm
Figure 3.
Continuous wave Doppler interrogation of conduit in above case showed peak gradient of 65 mmHg
In view of poor echo windows the distal branch pulmonary arteries could not be profiled. CT pulmonary angiography was done to define the conduit, level of obstruction, pulmonary arteries anatomy and also to look for any evidence of bronchial compression. Three-dimensional reconstructed CT showed huge aneurysm of RVOT arising just proximal to RV-PA conduit junction and compressing distal conduit – PA junction leading to kinking of that area (figures 4, 5).
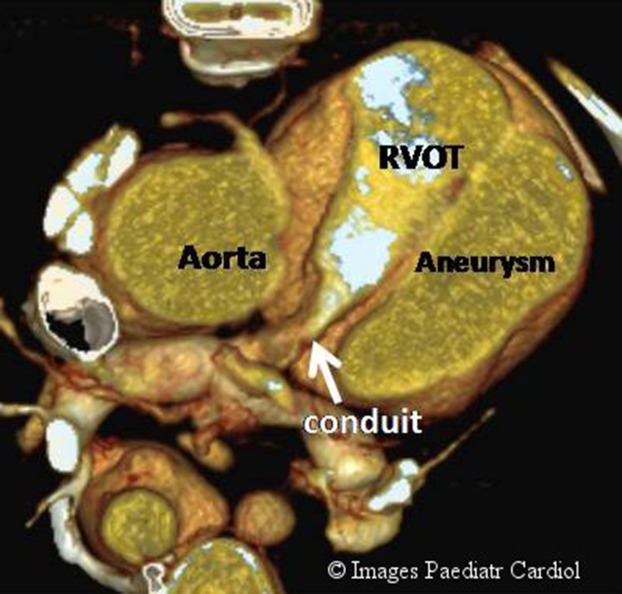
Figure 4.
CT pulmonary angiography images of case 1 showing massive RVOT aneurysm compressing the conduit and causing severe narrowing
Figure 5.
Three Dimensional reconstructedimage of CT pulmonary angiography of case 1 showing giant RVOT aneurysm
Also there was compression of left bronchus by the aneurysm. That kinking was cause of severe RVOT obstruction. Patient underwent surgical intervention (excision of aneurysm). Conduit replacement did not required and kinking and compression due to aneurysm was the cause of RVOT obstruction. Post-operative course was uneventful and he is doing fine 1 year post redo surgical intervention.
Case 2: Seven year old child, operated case of truncus arteriosus at the age of 3 months, underwent redo surgery for conduit replacement. Post-operative course was uneventful. Six months post redo surgery, he presented with a history of low grade fever, pallor, loss of appetite and weight loss for 2 months. Intermittently he was receiving oral antibiotics from his local physician. On examination, child was febrile, severely anemic, malnourished and there was splenomegaly (6cm, firm in consistency). He was diagnosed with bacterial endocarditis (low hemoglobin, high total leucocyte with polymorphonuclear dominance, very high CRP, microscopic hematuria, and on echocardiography there were multiple vegetations in RVOT attached to conduit, dilated RVOT, but no evidence of RVOT obstruction). All his cultures (blood, urine and bone marrow) were sterile. He was treated with broad spectrum intravenous antibiotics for 8 weeks for which he responded (he became afebrile and all inflammatory parameters became negative).
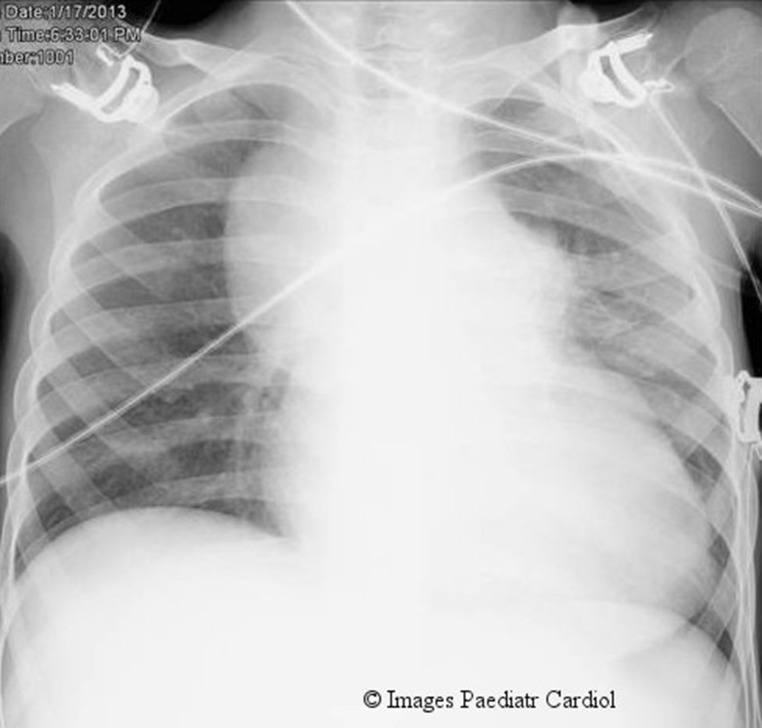
Four weeks later he developed features of recurrence of infection. Blood investigations showed elevated inflammatory markers. Chest x-ray frontal view (figure 6) showed mild cardiomegaly with homogenous opacity in right upper parasternal area.
Figure 6.
Chest X-ray postero-anterior view of case 2 showing homogenous opacity to right of sternum
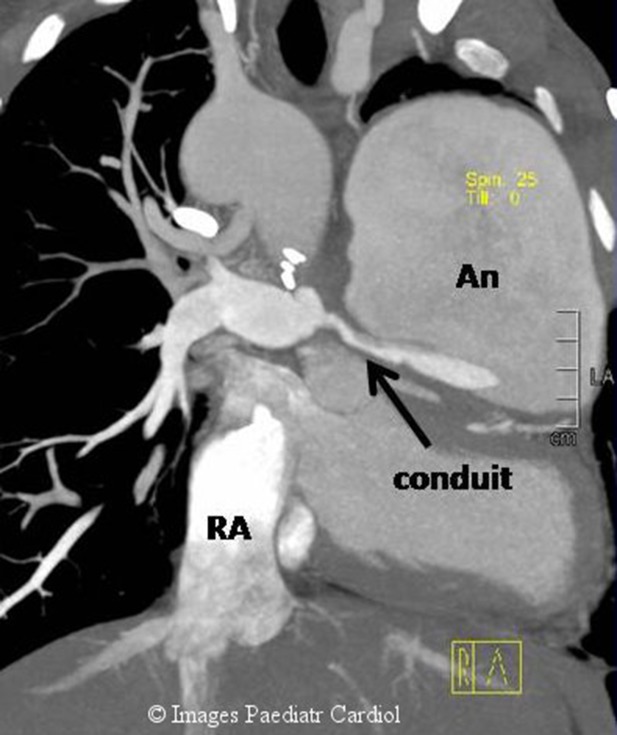
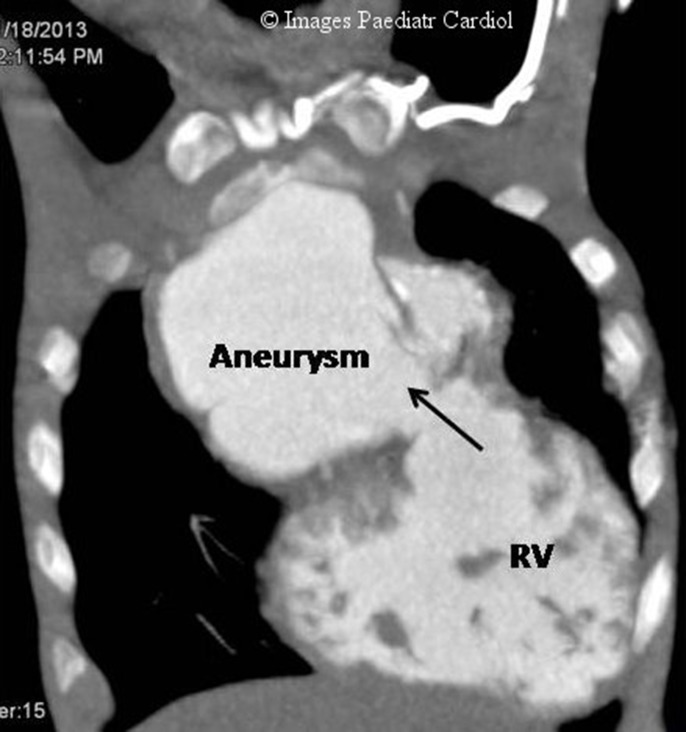
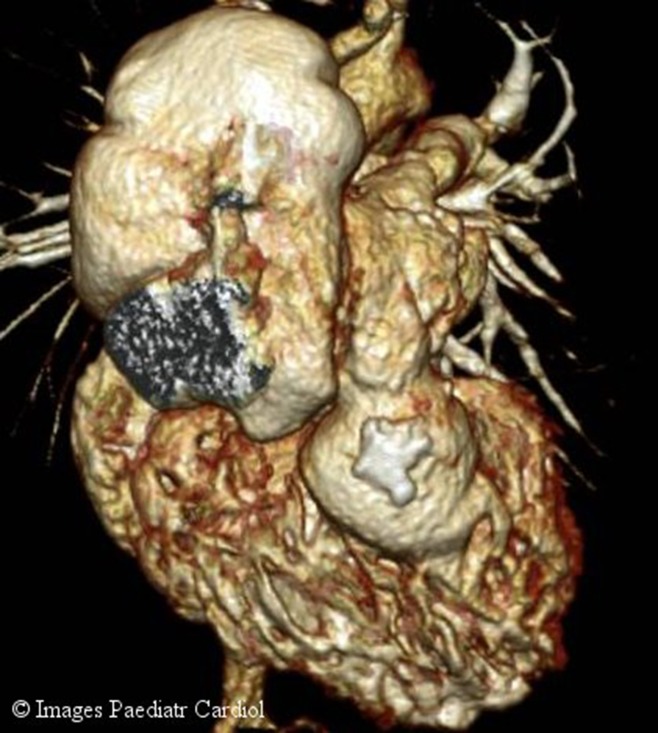
Repeat echocardiography showed large aneurysm of RVOT arising proximal to RV–conduit junction and compressing the conduit leading to conduit obstruction. CT pulmonary angiography was done to evaluated for RVOT aneurysm and showed massive RVOT aneurysm, origin proximal to RV-conduit junction and compressing the conduit from right side (figures 7, 8).
Figure 7.
CT pulmonary angiography images of case 2 showing massive aneurysm arising from RVOT
Figure 8.
Three dimensional reconstruction of CT pulmonary angiography of case 2 showing massive RVOT aneurysm
The child was reoperated (conduit replacement and resection of RVOT aneurysm) after one more course of intravenous antibiotics. His cultures (blood, urine and surgically removed conduit) did not show any growth. Though initial post-operative course was apparently uneventful, he had 3rd recurrence of infection 4 months surgical intervention and succumbed to his illness.
Discussion
In complex TOF physiology group and truncus arteriosus, conduit placement is needed to connect RVOT to pulmonary arteries. Long-term implication of conduit placement is need of replacement due tp inherent chances of stenosis and/or regurgitation of a valved conduit.
Pseudoaneurysm of RVOT is a rare complication and it happens along the suture lines.1 Usually the pseudoaneurysm is slowly progressing but rarely it can be rapidly progressing and life threatening as happened in our cases.
Reported incidence of aneurysms (both true and false) after TOF repair is between 2% and 25%, but most of the cases were of true aneurysms.2 The mean interval to diagnosis of pseudoaneurysm from the primary operation was 15 months (range eight months to three years).2 Primary causative factor considered was high RV pressure due to persistence of RVOT obstruction leading to pseudoaneurysm formation from the ventriculotomy itself or patch dehiscence.3 Other recognized factors for formation of an aneurysm are residual left to right shunt, significant pulmonary regurgitation, faulty suture technique, infection, trauma, and Chagas disease.3-6
Presentation of pseudo aneurysm is varied from asymptomatic incidental diagnosis on routine follow up to presentation in emergency with severe respiratory distress. When the aneurysm is large, the patient presents with symptoms secondary to the compression of adjoining mediastinal structures as superior vena caval syndrome, dyshagia, syncope, acute respiratory distress due to airway compression, or thrombus formation inside the aneurysm.1,7-9
Our cases had rapidly progressing massive aneurysms, communicating with RVOT just proximal to RV-conduit junction and were causing severe RVOT obstruction. Cause of rapidly progressing RVOT aneurysm was bacterial endocarditis in the child (case 2) while in the adult patient (case 1) we could not find any specific cause.
Regular follow up with annual chest X-ray, ECG and echocardiography should be done in all patients operated for TOF physiology or where a conduit has been placed. If needed, CT pulmonary angiography or cardiac MRI should be done especially in grown-up patients.
In both patients CXR suggested the diagnosis, but echocardiography and CT pulmonary angiography were the definitive diagnostic tests. Both patients underwent surgical intervention. In the first patient aneurysm resection with patch closure could suffice while in the child with bacterial endocarditis, conduit replacement with aneurysm repair was done. The first patient did well while the child redeveloped bacterial endocarditis 4 months after surgical intervention and did not survive.
Conclusion
Pseudoaneurysm of the RVOT is an infrequent complication of cardiovascular surgical procedures that involve both a right ventriculotomy and RVOT reconstruction with patch repair or conduit replacement.7
Use of large pericardial patches to reconstruct the RVOT, residual RVOT obstruction, severe pulmonary regurgitation, residual shunts and infection are some of the common causes of RVOT aneurysms reported in the literature.9
Pseudoaneurysm should always be suspected in patients with the relevant symptoms, and such patients must be followed up closely.
Precise and careful preoperative assessment, using echocardiography, CT and MRI angiography, is important for ensuring the safety of surgery performed on these patients.
In case of rapidly increasing aneurysm, it is important to rule out bacterial endocarditis
Reoperation can be performed safely, with low risk of mortality or morbidity.
References
- 1.Sahewalla R, Ross RD, Delius RE, Halas R, Anne P. Large pseudoaneurysm following right ventricle to pulmonary artery homograft placement in an infant. Ann Pediatr Cardiol. 2018. Jan-Apr; 11(1): 106–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenthal A, Gross RE, Pastemac A. Aneurysms of right ventricular outflow patches. J Thorac Cardiovasc Surg 1972;63:735-40. [PubMed] [Google Scholar]
- 3.Samarrai AAR, McCloy R, Ablett MB. Biloculate false aneurysm of the right ventricle after cardiac surgery. Br HeartJ 1976;38:297-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stansl HC Jr, Julian OC, Dye WS. Right ventricular aneurysm. A review of literature and report of a case of successful repair with the aid of temporary cardiopulmonary bypass. J Thorac Cardiovasc Surg 1963;46: 66-76. [PubMed] [Google Scholar]
- 5.Payne WS, Kirklin JW. Late complications after plastic reconstruction of outflow tract in tetralogy of Fallot. Ann Surg 1961;154:53-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pillai SK, Reddy HP, Kulkarni S, Murthy KS, Cherian KM. Pseudoaneurysm of homograft placed in right ventricular outflow tract. Ann Thorac Surg. 2004;78:1068–70 [DOI] [PubMed] [Google Scholar]
- 7.Lee Y, Lee JT, Cho JY, Kim GJ. Pseudoaneurysm of surgically reconstructed right ventricular outflow tract complicated by superior vena cava syndrome. Korean J Thorac Cardiovasc Surg. 2014;47:541–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calabrò R, Santoro G, Pisacane C, Pacileo G, Russo MG, Vosa C, et al. . Repeat syncopal attacks due to postsurgical right ventricular pseudoaneurysm. Ann Thorac Surg. 1999;68:252–4. [DOI] [PubMed] [Google Scholar]
- 9.Peer SM, Bhat PS, Furtado AD, Chikkatur R. Right ventricular outflow tract aneurysm with thrombus. Interactive cardiovascular and thoracic surgery. 2012. January 9;14(4):488-90. [DOI] [PMC free article] [PubMed] [Google Scholar]