Abstract
Background:
The aim of the study was to determine the effects of coenzyme Q10 (CoQ10) supplementation on biomarkers of inflammation and oxidative stress among diabetic hemodialysis (HD) patients.
Methods:
Sixty diabetic HD patients participated in the randomized, double blind, placebo-controlled clinical trial. They were randomly assigned into two groups to intake either 60 mg CoQ10 supplements (n = 30) or placebo (n = 30) twice a day for 12 weeks.
Results:
After 12 weeks of intervention, CoQ10 supplementation significantly increased total antioxidant (TAC) (54.921 ± 26.437 vs. −126.781 ± 26.437, P < 0.001) and nitric oxide (NO) levels (4.121 ± 1.314 vs. −1.427 ± 1.314, P = 0.006) and decreased C-reactive protein (CRP) (−1.302 ± 0.583 vs. 0.345 ± 0.583, 0.042) levels compared with the placebo. We did not observe any significant effect of CoQ10 supplementation on malondialdehyde (MDA) and glutathione (GSH) levels compared with the placebo.
Conclusions:
Overall, our study showed that CoQ10 supplementation to diabetic HD patients for 12 weeks was associated with increased levels of TAC and NO levels and decreased level of high-sensitivity CRP (hs-CRP) levels, but did not have any beneficial effects on MDA and GSH.
Keywords: Coenzyme Q10 supplementation, hemodialysis, inflammatory markers, oxidative stress
Introduction
Diabetes which induces diabetic nephropathy has increased worldwide.[1] Kidney disease is a common complication of many chronic diseases. The prevalence of kidney disease among people with type 2 diabetes mellitus is 43.5%.[2] Cardiovascular disease (CVD) is strongly associated with kidney disease.[3] Hemodialysis (HD) correlates with endothelial dysfunction[4] and decreased levels of nitric oxide (NO) levels.[5] In addition, HD is correlated with insulin resistance, which in turn is associated with increased levels of oxidative stress and inflammation[6,7,8,9,10] It was reported that 51.1% of patients with kidney disease suffer from hypertension.[11,12] Coenzyme Q10 (CoQ10) is one kind of antioxidant which synthesizes in the body[13] and involves in the ATP production and electron transfer chain.[14] It can protect lipids against free radicals.[15]
Previous studies have demonstrated that CoQ10 production decreases in HD patients due to β-cells impairment,[14] hyperglycemia which in turn induces oxidative stress[16] and decreased conversion of ubiquinine to an active form (ubiquinol).[17] Also, circulating CoQ10 levels was significantly lower in HD patients than in those of controls.[18,19] Previous studies have demonstrated that CoQ10 supplementation can improve inflammation and oxidative stress in end-stage renal disease (ESRD) patients.[20,21] Several studies have reported a significant association between Q10 intake and biomarkers of inflammation and oxidative stress. In a study by Zahed et al.,[10] CoQ10 supplementation at a dosage of 100 mg/day for 3 months to HD patients reduced C-reactive protein (CRP) levels as an inflammatory marker. In another study, taking CoQ10 supplements for 4 months by HD patients significantly decreased F2-isoprostanes levels.[22] Furthermore, trolox equivalent antioxidant capacity, oxygen radical antioxidant capacity, and indicators of total antioxidant (TAC) capacity significantly decreased following the CoQ10 administration for 6 months in HD patients.[23] Also, a significant improvement in biomarkers of oxidative stress and mitochondrial function was seen after a short-term CoQ10 supplementation among HD patients.[24] These evidences suggest the importance of CoQ10 supplementation in diabetic HD patients.
To our knowledge, data on the effects of CoQ10 supplementation on biomarkers of inflammation and oxidative stress in diabetic HD patients are scarce. Therefore, the current study was conducted to determine the effects of CoQ10 supplementation on biomarkers of inflammation oxidative stress, including serum high-sensitivity CRP (hs-CRP), plasma NO, TAC, glutathione (GSH), and malondialdehyde (MDA) levels in diabetic HD subjects.
Methods
Study design and participants
This randomized, double-blinded, placebo-controlled clinical trial lasted for 12 weeks. It was registered with the Iranian Registry of Clinical Trials (http://www.irct.ir: IRCT2016081811763N30). Sixty diabetic HD patients of the Akhavan Clinic in Kashan, Iran, aged 18–80 years, enrolled in this trial from April 2017 to October 2017. The study protocol was approved by the ethics committee of the Isfahan University of Medical Sciences (IUMS) and informed consent forms were signed by all participants prior to the intervention. Pregnant women, medical illness, acute cardiovascular events, taking antioxidant and/or anti-inflammatory supplements within 3 months prior to the enrollment in the study, and patients who required changes in medications during the study were not included in the current study.
Study procedures
Sixty diabetic HD patients were randomly assigned into two group to intake either 60 mg CoQ10 supplements (n = 30) or placebo (n = 30) twice a day for 12 weeks. We used 120 mg/day CoQ10 based on the previous studies.[10,25,26,27] Randomization assignment was carried out using the computer-generated random numbers. The randomized allocation sequence, enrolling participants, and allocating them to interventions were performed by a trained nutritionist at the clinic. The CoQ10 supplements and its placebos were manufactured by the Zahravi Company (Tabriz, Iran) and Barij Essence Pharmaceutical Company (Kashan, Iran), respectively. They were completely identical in terms of their appearance. To increase compliance rates, all participants received short messages on their cell phones every day to remind them about taking capsules. In addition, to evaluate the compliance, we counted the remaining supplements. Participants were requested to keep their habitual diet and routine levels of physical activity and not to take any medication which can affect the outcome throughout the study period. All participants completed three dietary records (two week days and one weekend). Nutritionist IV software used to determine macro-and micro-nutrient intakes[28] (First Databank, San Bruno, CA, USA) modified for Iranian foods.
Assessment of outcomes
About 10 mL fasting blood samples were obtained from each patient at the baseline and after the end of treatment at the Akhavan Clinic Laboratory in Kashan, Iran. Serum hs-CRP levels were determined using a commercial enzyme-linked immunosorbent assay (ELISA) kit (LDN, Northern, Germany) with intra- and inter-assay coefficients of variation (CVs) of <7%. The plasma NO concentrations were determined using the Griess method.[29] The plasma TAC concentrations were measured using the ferric reducing antioxidant power developed by Benzie and Strain,[30] GSH were measured by the method of Beutler and Gelbart,[31] and MDA concentrations were measured by the thiobarbituric acid-reactive substances spectrophotometric test.[32]
Statistical methods
The Kolmogorov-Smirnov test is used to determine the normality of the variables. An independent sample t-test was used to determine anthropometric measures as well as macro- and micro-nutrient dietary intakes between the two groups. To determine the effects of CoQ10 on biomarkers of inflammation and oxidative stress, we used one-way repeated measures analysis of variance. Analysis of covariance (ANCOVA) was used to determine different effects of CoQ10 supplementation on biomarkers of inflammation and oxidative stress between two groups. P values <0.05 were considered statistically significant. All statistical analyses were conducted using the Statistical Package for Social Science version 18 (SPSS Inc., Chicago, Illinois, USA).
Results
Our clinical trial conducted by 60 diabetic HD patients [CoQ10 (n = 30) and placebo (n = 30)] [Figure 1]. On an average, patient's compliance to supplement administration was good. No side effects following the CoQ10 supplementation were reported in diabetic HD patients throughout the intervention.
Figure 1.
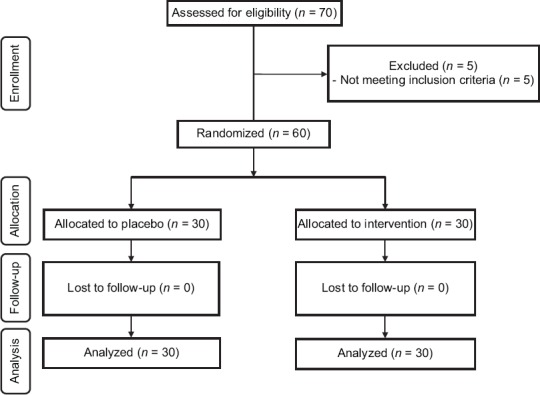
Summary of patient flow diagram
Mean age (64.8 ± 11.5 vs. 59.4 ± 12.2 years, P = 0.08), height (167.2 ± 9.6 vs. 162.6 ± 10.8 cm; P = 0.09), and baseline weight (75.2 ± 12.8 vs. 70.8 ± 13.9 kg; P = 0.20) of the study participants were not significantly different comparing CoQ10 supplements and placebo groups (data not shown). In addition, the use of antidiabetic or anti-lipidemic drugs, angiotensin-converting enzymes inhibitors, aldosterone receptor blockers, and phosphate binders were not statistically different between the two groups at baseline or at the end of the trial.
We observed no significant difference in dietary macro- and micro-nutrient intakes between the two groups throughout the trial (data not shown).
After 12 weeks of intervention, CoQ10 supplementation significantly increased TAC (54.921 ± 26.437 vs. −126.781 ± 26.437, P < 0.001) and NO levels (4.121 ± 1.314 vs. −1.427 ± 1.314, P = 0.006) and decreased hs-CRP level (−1.302 ± 0.583 vs. 0.345 ± 0.583, 0.042) compared with the placebo. We did not observe any significant effect of CoQ10 supplementation on MDA and GSH levels compared with the placebo [Table 1]. Mean HbA1c at baseline (7.2 ± 1.7 vs. 7.5 ± 1.7%; P = 0.75) of the study participants were not significantly different comparing CoQ10 supplements and placebo groups.
Table 1.
Metabolic profiles at baseline and after the 12-week intervention in patients with diabetic hemodialysis that received either CoQ10 supplements or placebo
| Placebo group (n=30) | Q10 group (n=30) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | End-of-trial | Mean±SD | P1 | Baseline | End-of-trial | Mean±SD | P1 | P2 | |
| TAC (mmol/L) | 846.079±144.443 | 743.923±149.011 | −126.781±26.437 | 0.002 | 650.470±87.829 | 680.765±108.302 | 54.921±26.437 | 0.26 | <0.001 |
| 883.430 (514.50-1182.03) | 716.430 (513.20-1156.54) | 644.650 (528.24-816.28) | 659.570 (528.24-893.88) | ||||||
| GSH (µmol/L) | 520.653±0.212 | 5.02±3.42 | 60.750±32.617 | 0.711 | 415.155±58.467 | 420.82±67.762 | -34.895±32.617 | 0.745 | 0.053 |
| 0.460 (0.27-9.93) | 3.96 (326.1118.03) | 391.590 (362.12-601.10) | 393.220 (358.85-597.82) | ||||||
| MDA (µmol/L) | 3.3277±1.195 | 4.048±2.817 | 0.547±0.265 | 0.084 | 15.39±6.34 | 2.900±0.260 | −0.129±0.265 | 0 | 0.09 |
| 2.825 (1.87-6.63) | 2.465 (0.64-10.23) | 14.05 (3.40-33) | 2.885 (2.30-3.44) | ||||||
| hs-CRP (mg/L) | 6.793±3.520 | 7.110±3.769 | 0.345±0.583 | 0.398 | 7.340±6.378 | 6.066±4.699 | −1.302±0.583 | 0.07 | 0.042 |
| 6.250 (0.90-14.40) | 6.150 (0.80-18.70) | 6.100 (1.00-30.50) | 34.050 (31.35-45.14) | ||||||
| NO (µmol/L) | 44.480±6.165 | 43.173±7.636 | −1.427±1.314 | 0.362 | 34.050 (31.35-45.14) | 38.085 (31.03-48.00) | 4.121±1.314 | 0.001 | 0.006 |
| 41.770 (36.00-61.82) | 41.140 (32.00-64.50) | ||||||||
1Data are means±SDs. 2Obtained from repeated measures ANOVA test, TAC=Total antioxidant capacity, GSH=Total glutathione, MDA=Malondialdehyde, hs-CRP=High-sensitivity C-reactive protein, NO=Nitric oxide, ANOVA=Analysis of variance
Discussion
Effect on oxidative stress
This study documented that CoQ10 supplementation for 12 weeks significantly increased TAC levels in HD patients, but did not influence MDA and GSH levels. Few studies have reported that CoQ10 supplementation had beneficial effects on antioxidant system in patients without HD.[33,34,35,36] In addition, supplementing athletes by 100 mg/day CoQ10 for 2 months significantly increased TAC concentrations.[37] Daily intake of 100 mg CoQ10 supplements among patients with metabolic syndrome for 8 weeks had beneficial effect on TAC levels.[38] Taking 150 mg/day CoQ10 supplements by patients with coronary artery disease for 12 weeks did not decrease MDA levels.[17] However, in a study conducted by Gokbel et al.,[39] CoQ10 supplementation at a dosage of 200 mg/day for 12 weeks by HD patients did not influence markers of oxidative stress.[40] Abnormal glucose status in all stage kidney disease increases radical oxidative stress formation by activating stress-activated protein kinase/c-Jun NH2-terminal kinase, functional proteins glycosylation, and glucose autoxidation. CoQ10 intake may reduce oxidative damage through inhibiting NF-kB (nuclear factor-kappaB) and protein kinases.[41] In addition, CoQ10 reduces free radical by delivering them to vitamin E in antioxidant cycle.[42]
Effects on inflammatory markers
Our study showed that CoQ10 supplementation to HD patients for 12 weeks significantly increased plasma NO and significantly reduced CRP levels. Previous studies have reported conflicting results. In a study by Zahed et al.,[10] 100 mg/day CoQ10 supplementation to HD patients for 3 months significantly decreased CRP levels. Lower inflammatory markers were also observed after 300 mg/day CoQ10 supplementation for 12 weeks in people with CVD during statin therapy.[43] Furthermore, CoQ10 administration was associated with improved gene expression of inflammatory markers in patients with polycystic ovary syndrome.[26] However, 100 mg/day CoQ10 supplementation to HD patients could significantly decrease CRP levels.[10] In another study, 200 mg CoQ10 supplementation for 12 weeks did not affect any beneficial effect on inflammatory markers among obese subjects.[40] CoQ10 intake may reduce CRP through inhibiting gene expression of NF-kB and tumor necrosis factor alpha.[44]
This study had some limitations. One limitation of the study was the duration of the study, long-term intervention may result in significant changes in MDA and GSH levels. In addition, we did not assess circulating levels of CoQ10 in our cohort before and after intervention as an indicator of patient's adherence. Also, we did not examine the purity of the CoQ10 supplements at the baseline. Oliguric patients were not considered as a separate group; maybe this was necessary as urine flow decrease blood levels of inflammatory markers. Furthermore, we did not evaluate gene expression related to biomarkers of inflammation and oxidative stress.
Conclusions
Overall, our study showed that CoQ10 supplementation to diabetic HD patients for 12 weeks associated with increased levels of TAC and NO, and decreased level of hs-CRP, but did not have any beneficial effects on MDA and GSH.
Clinical registration
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ritz E, Zeng XX, Rychlik I. Clinical manifestation and natural history of diabetic nephropathy. Contrib Nephrol. 2011;170:19–27. doi: 10.1159/000324939. [DOI] [PubMed] [Google Scholar]
- 2.Nafar M, Mousavi SM, Mahdavi-Mazdeh M, Pour-Reza-Gholi F, Firoozan A, Einollahi B, et al. Burden of chronic kidney disease in Iran: A screening program is of essential need. Iran J Kidney Dis. 2008;2:183–92. [PubMed] [Google Scholar]
- 3.Liu M, Li XC, Lu L, Cao Y, Sun RR, Chen S, et al. Cardiovascular disease and its relationship with chronic kidney disease. Eur Rev Med Pharmacol Sci. 2014;18:2918–26. [PubMed] [Google Scholar]
- 4.Gkaliagkousi E, Gavriilaki E, Triantafyllou A, Douma S. Clinical significance of endothelial dysfunction in essential hypertension. Curr Hypertens Rep. 2015;17:85. doi: 10.1007/s11906-015-0596-3. [DOI] [PubMed] [Google Scholar]
- 5.Abrantes DC, Brunini TM, Matsuura C, Mury WV, Correa CR, Santos SF, et al. Diminished nitric oxide generation from neutrophils suppresses platelet activation in chronic renal failure. Mol Cell Biochem. 2015;401:147–53. doi: 10.1007/s11010-014-2302-1. [DOI] [PubMed] [Google Scholar]
- 6.Sohrabi Z, Eftekhari MH, Eskandari MH, Rezaeianzadeh A, Sagheb MM. Malnutrition-inflammation score and quality of life in hemodialysis patients: Is there any correlation? Nephrourol Mon. 2015;7:e27445. doi: 10.5812/numonthly.7(3)2015.27445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jakuszewski P, Czerwienska B, Chudek J, Wiecek A. Which components of malnutrition-inflammation-atherosclerosis syndrome are more common in haemodialysis patients with diabetic nephropathy? Nephrology (Carlton, Vic) 2009;14:643–9. doi: 10.1111/j.1440-1797.2009.01096.x. [DOI] [PubMed] [Google Scholar]
- 8.Yen TH, Lin JL, Lin-Tan DT, Hsu KH. Cardiothoracic ratio, inflammation, malnutrition, and mortality in diabetes patients on maintenance hemodialysis. Am J Med Sci. 2009;337:421–8. doi: 10.1097/MAJ.0b013e31819bbec1. [DOI] [PubMed] [Google Scholar]
- 9.Hodgson JM, Watts GF, Playford DA, Burke V, Croft KD. Coenzyme Q10 improves blood pressure and glycaemic control: A controlled trial in subjects with type 2 diabetes. Eur J Clin Nutr. 2002;56:1137–42. doi: 10.1038/sj.ejcn.1601464. [DOI] [PubMed] [Google Scholar]
- 10.Zahed NS, Ghassami M, Nikbakht H. Effects of coenzyme Q10 supplementation on C-reactive protein and homocysteine as the inflammatory markers in hemodialysis patients; a randomized clinical trial. J Nephropathol. 2016;5:38–43. doi: 10.15171/jnp.2016.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans M, Grams ME, Sang Y, Astor BC, Blankestijn PJ, Brunskill NJ, et al. Risk factors for prognosis in patients with severely decreased GFR. Kidney Int Rep. 2018;3:625–37. doi: 10.1016/j.ekir.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parati G, Ochoa JE, Stergiou G. Masked hypertension and chronic kidney disease: The role of out-of-office blood pressure monitoring. J Hypertens. 2018;36:1468–71. doi: 10.1097/HJH.0000000000001781. [DOI] [PubMed] [Google Scholar]
- 13.Littarru GP, Tiano L. Bioenergetic and antioxidant properties of coenzyme Q10: Recent developments. Mol Biotechnol. 2007;37:31–7. doi: 10.1007/s12033-007-0052-y. [DOI] [PubMed] [Google Scholar]
- 14.Chew GT, Watts GF. Coenzyme Q10 and diabetic endotheliopathy: Oxidative stress and the ‘recoupling hypothesis’. QJM. 2004;97:537–48. doi: 10.1093/qjmed/hch089. [DOI] [PubMed] [Google Scholar]
- 15.Lenaz G, Fato R, Castelluccio C, Cavazzoni M, Estornell E, Huertas JF, et al. An updating of the biochemical function of coenzyme Q in mitochondria. Mol Aspects Med. 1994;15(Suppl. 1):s29–36. doi: 10.1016/0098-2997(94)90010-8. [DOI] [PubMed] [Google Scholar]
- 16.Molyneux SL, Florkowski CM, George PM, Pilbrow AP, Frampton CM, Lever M, et al. Coenzyme Q10: An independent predictor of mortality in chronic heart failure. J Am Coll Cardiol. 2008;52:1435–41. doi: 10.1016/j.jacc.2008.07.044. [DOI] [PubMed] [Google Scholar]
- 17.Lee BJ, Huang YC, Chen SJ, Lin PT. Coenzyme Q10 supplementation reduces oxidative stress and increases antioxidant enzyme activity in patients with coronary artery disease. Nutrition (Burbank, Los Angeles County, Calif) 2012;28:250–5. doi: 10.1016/j.nut.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 18.Lippa S, Colacicco L, Calla C, Sagliaschi G, Angelitti AG. Coenzyme Q10 levels, plasma lipids and peroxidation extent in renal failure and in hemodialytic patients. Mol Aspects Med. 1994;15(Suppl):s213–9. doi: 10.1016/0098-2997(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 19.Mehmetoglu I, Yerlikaya FH, Kurban S, Erdem SS, Tonbul Z. Oxidative stress markers in hemodialysis and peritoneal dialysis patients, including coenzyme Q10 and ischemia-modified albumin. Int J Artif Organs. 2012;35:226–32. doi: 10.5301/ijao.5000078. [DOI] [PubMed] [Google Scholar]
- 20.Fukuda S, Koyama H, Kondo K, Fujii H, Hirayama Y, Tabata T, et al. Effects of nutritional supplementation on fatigue, and autonomic and immune dysfunction in patients with end-stage renal disease: A randomized, double-blind, placebo-controlled, multicenter trial. PLoS One. 2015;10:e0119578. doi: 10.1371/journal.pone.0119578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gokbel H, Atalay H, Okudan N, Solak Y, Belviranli M, Turk S. Coenzyme Q10 and its relation with oxidant and antioxidant system markers in patients with end-stage renal disease. Ren Fail. 2011;33:677–81. doi: 10.3109/0886022X.2011.589941. [DOI] [PubMed] [Google Scholar]
- 22.Rivara MB, Yeung CK, Robinson-Cohen C, Phillips BR, Ruzinski J, Rock D, et al. Effect of coenzyme Q10 on biomarkers of oxidative stress and cardiac function in hemodialysis patients: The CoQ10 biomarker trial. Am J Kidney Dis. 2017;69:389–99. doi: 10.1053/j.ajkd.2016.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakata T, Furuya R, Shimazu T, Odamaki M, Ohkawa S, Kumagai H. Coenzyme Q10 administration suppresses both oxidative and antioxidative markers in hemodialysis patients. Blood Purif. 2008;26:371–8. doi: 10.1159/000135605. [DOI] [PubMed] [Google Scholar]
- 24.Yeung CK, Billings FTt, Claessens AJ, Roshanravan B, Linke L, Sundell MB, et al. Coenzyme Q10 dose-escalation study in hemodialysis patients: Safety, tolerability, and effect on oxidative stress. BMC Nephrol. 2015;16:183. doi: 10.1186/s12882-015-0178-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heidari A, Hamidi G, Soleimani A, Aghadavod E, Asemi Z. Effects of coenzyme Q10 supplementation on gene expressions related to insulin, lipid, and inflammation pathways in patients with diabetic nephropathy. Iran J Kidney Dis. 2018;12:14–21. [PubMed] [Google Scholar]
- 26.Rahmani E, Jamilian M, Samimi M, Zarezade Mehrizi M, Aghadavod E, Akbari E, et al. The effects of coenzyme Q10 supplementation on gene expression related to insulin, lipid and inflammation in patients with polycystic ovary syndrome. Gynecol Endocrinol. 2018;34:217–22. doi: 10.1080/09513590.2017.1381680. [DOI] [PubMed] [Google Scholar]
- 27.Samimi M, Zarezade Mehrizi M, Foroozanfard F, Akbari H, Jamilian M, Ahmadi S, et al. The effects of coenzyme Q10 supplementation on glucose metabolism and lipid profiles in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Clin Endocrinol (Oxf) 2017;86:560–6. doi: 10.1111/cen.13288. [DOI] [PubMed] [Google Scholar]
- 28.Azar M, Sarkisian E. Tehran: Shaheed Beheshti University; 1980. Food Composition Table of Iran: National Nutrition and Food Research Institute. [Google Scholar]
- 29.Tatsch E, Bochi GV, Pereira Rda S, Kober H, Agertt VA, de Campos MM, et al. A simple and inexpensive automated technique for measurement of serum nitrite/nitrate. Clin Biochem. 2011;44:348–50. doi: 10.1016/j.clinbiochem.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 30.Benzie IF, Strain JJ. The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: The FRAP assay. Anal Biochem. 1996;239:70–6. doi: 10.1006/abio.1996.0292. [DOI] [PubMed] [Google Scholar]
- 31.Beutler E, Gelbart T. Plasma glutathione in health and in patients with malignant disease. J Lab Clin Med. 1985;105:581–4. [PubMed] [Google Scholar]
- 32.Janero DR. Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury. Free Radic Biol Med. 1990;9:515–40. doi: 10.1016/0891-5849(90)90131-2. [DOI] [PubMed] [Google Scholar]
- 33.Nadjarzadeh A, Shidfar F, Amirjannati N, Vafa MR, Motevalian SA, Gohari MR, et al. Effect of Coenzyme Q10 supplementation on antioxidant enzymes activity and oxidative stress of seminal plasma: A double-blind randomised clinical trial. Andrologia. 2014;46:177–83. doi: 10.1111/and.12062. [DOI] [PubMed] [Google Scholar]
- 34.Abdollahzad H, Aghdashi MA, Asghari Jafarabadi M, Alipour B. Effects of Coenzyme Q10 supplementation on inflammatory cytokines (TNF-alpha, IL-6) and oxidative stress in rheumatoid arthritis patients: A randomized controlled trial. Arch Med Res. 2015;46:527–33. doi: 10.1016/j.arcmed.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 35.Sanoobar M, Eghtesadi S, Azimi A, Khalili M, Jazayeri S, Reza Gohari M. Coenzyme Q10 supplementation reduces oxidative stress and increases antioxidant enzyme activity in patients with relapsing-remitting multiple sclerosis. Int J Neurosci. 2013;123:776–82. doi: 10.3109/00207454.2013.801844. [DOI] [PubMed] [Google Scholar]
- 36.Yen CH, Chu YJ, Lee BJ, Lin YC, Lin PT. Effect of liquid ubiquinol supplementation on glucose, lipids and antioxidant capacity in type 2 diabetes patients: A double-blind, randomised, placebo-controlled trial. Br J Nutr. 2018;120:57–63. doi: 10.1017/S0007114518001241. [DOI] [PubMed] [Google Scholar]
- 37.Mancini A, Milardi D, Bianchi A, Festa R, Silvestrini A, De Marinis L, et al. Increased total antioxidant capacity in seminal plasma of varicocele patients: A multivariate analysis. Arch andrology. 2007;53:37–42. doi: 10.1080/01485010600840756. [DOI] [PubMed] [Google Scholar]
- 38.Raygan F, Rezavandi Z, Tehrani SD, Farrokhian A, Asemi Z. The effects of coenzyme Q10 administration on glucose homeostasis parameters, lipid profiles, biomarkers of inflammation and oxidative stress in patients with metabolic syndrome. Eur J Nutr. 2016;55:2357–64. doi: 10.1007/s00394-015-1042-7. [DOI] [PubMed] [Google Scholar]
- 39.Gokbel H, Turk S, Okudan N, Atalay H, Belviranli M, Gaipov A, et al. Effects of coenzyme Q10 supplementation on exercise performance and markers of oxidative stress in hemodialysis patients: A double-blind placebo-controlled crossover trial. Am J Ther. 2016;23:e1736–43. doi: 10.1097/MJT.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 40.Lee YJ, Cho WJ, Kim JK, Lee DC. Effects of coenzyme Q10 on arterial stiffness, metabolic parameters, and fatigue in obese subjects: A double-blind randomized controlled study. J Med Food. 2011;14:386–90. doi: 10.1089/jmf.2010.1202. [DOI] [PubMed] [Google Scholar]
- 41.Zahedi H, Eghtesadi S, Seifirad S, Rezaee N, Shidfar F, Heydari I, et al. Effects of CoQ10 supplementation on lipid profiles and glycemic control in patients with type 2 diabetes: A randomized, double blind, placebo-controlled trial. J Diabetes Metab Disord. 2014;13:81. doi: 10.1186/s40200-014-0081-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arroyo A, Kagan VE, Tyurin VA, Burgess JR, de Cabo R, Navas P, et al. NADH and NADPH-dependent reduction of coenzyme Q at the plasma membrane. Antioxid Redox Signal. 2000;2:251–62. doi: 10.1089/ars.2000.2.2-251. [DOI] [PubMed] [Google Scholar]
- 43.Lee BJ, Tseng YF, Yen CH, Lin PT. Effects of coenzyme Q10 supplementation (300 mg/day) on antioxidation and anti-inflammation in coronary artery disease patients during statins therapy: A randomized, placebo-controlled trial. Nutr J. 2013;12:142. doi: 10.1186/1475-2891-12-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carmona MC, Lefebvre P, Lefebvre B, Galinier A, Benani A, Jeanson Y, et al. Coadministration of coenzyme Q prevents rosiglitazone-induced adipogenesis in ob/ob mice. Int J Obes (Lond) 2009;33:204–11. doi: 10.1038/ijo.2008.265. [DOI] [PubMed] [Google Scholar]


