Abstract
Background and Aims:
Transversus abdominis plane (TAP) block is a technique proposed to minimise pain after anterior iliac crest bone harvesting. This study aims to evaluate the postoperative pain in patients who receive ultrasound-guided TAP block to supplement routine wound infiltration.
Material and Methods:
A total of 143 patients aged between 6 and 22 years were randomised into two groups. Patients in group A received supplemental TAP block on the same side. Patients in group B received local anesthetic wound infiltration alone. Pain scores were compared at the first and 24th postoperative hours.
Results:
TAP block significantly reduced pain and delirium in the immediate postoperative period. The mean FLACC (Face, Legs, Activity, Cry, Consolability) score after 10 min was 0.8 in group A versus 1.8 in group B (P = 0.001). The mean Watcha scale at 10 min was 1.0 in group A versus 1.2 in group B (P = 0.001). After 24 h, 81.7% of patients in group A had no pain versus 59.7% in group B (P = 0.004). The incidence of intolerable pain at 24 h was 5.6% in group B versus 0% in group A (P = 0.04). Cumulative ambulation scores were significantly better in group A (P < 0.05). There was a strong and positive correlation between the analgesia and ability to ambulate comfortably at 24 h postop (Pearson's coefficient 0.95).
Conclusion:
Supplemental ultrasound-guided TAP block given intraoperatively reduces the postoperative pain. The incidence of emergence delirium was low. These patients were also able to ambulate earlier.
Keywords: Early ambulation, iliac crest bone graft harvesting, pain postoperative, TAP block
Introduction
Anterior iliac crest bone harvesting is frequently performed during reconstructive surgeries.[1] The primary morbidity is acute postoperative pain.[2] Inadequately treated pain predisposes to chronic pain in about 10–34% of patients.[2,3,4,5] Local anesthetic infiltration at harvest site is routinely practised to provide analgesia.[6] However, the analgesia is often short-lived and unreliable, often necessitating rescue medications.[2]
In the transversus abdominis plane (TAP) block, local anaesthetic is injected in the fascial plane between the transversus abdominis and internal oblique muscles. This blocks the thoracolumbar nerves from T6 to L2, thereby helping to ease the pain at the harvest site.[7]
Our hypothesis is that wound infiltration, when supplemented with TAP block, will help overcome the limitations of the former alone. Our primary aim was to determine whether supplemental ultrasound-guided TAP block given intraoperatively improves the postoperative pain relief at bone graft harvest site. Secondary aims were to assess incidence of emergence delirium, comfort during ambulation after 24 h and incidence of chronic pain.
Material and Methods
This study was approved by the Institutional Research Ethics Committee (ref: 07/16/IEC/JMMC and RI) and registered with Clinicaltrials.gov (ref: NCT02997124). Written informed consent was obtained from all subjects or parents/legal surrogate in minors as applicable.
A pilot study was done for calculating the sample size. Based on the standard deviation (SD) of the FLACC and Watcha score obtained from the pilot study, a minimum sample size of 65 patients was calculated for each group to obtain a power of 80% and confidence interval of 95%. About 143 patients aged between 6 and 22 years scheduled for alveolar bone grafting harvested from anterior iliac crest were assessed. They were allotted into two groups by the simple random sampling method – A (patients received additional TAP block along with local infiltration) and B (patients received wound infiltration only) [Figure 1]. It was a prospective randomised comparative double blind study.
Figure 1.
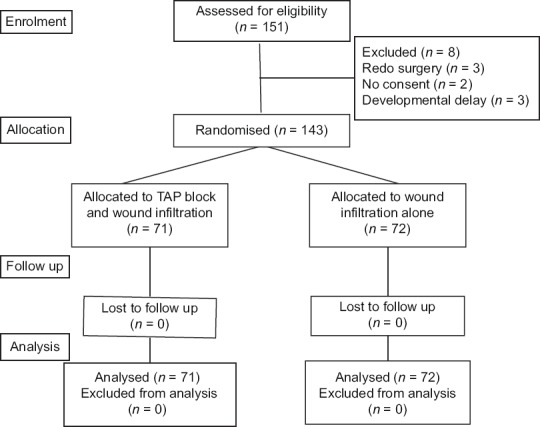
CONSORT diagram for the flow of participants through each stage
Only ASA-PS Class 1/2 patients undergoing alveolar bone grafting as a part of the reconstructive procedure for cleft lip and palate were recruited for the study. Patients who had difficulty in mentation and communication, bleeding disorders, liver and renal dysfunction, abdominal wall infection, allergy to local anaesthetics and those undergoing revision surgeries were excluded.
All patients were pre-medicated with IV midazolam 0.15 mg kg−1 and glycopyrrolate 0.01 mg kg−1. Anaesthesia was induced with propofol 2 mg kg−1 and fentanyl 2 mcg kg−1. Vecuronium 0.1 mg kg−1 was given to facilitate nasotracheal intubation with a Ring-Adair-Elwyn tube. Following induction, patients in group A were given an ultrasound-guided, in plane, TAP block with 0.5 ml/kg of 0.2% ropivacaine (maximum 20 ml). All the blocks were performed by the same anesthesiologist. Anesthesia was maintained with sevoflurane 1.5–2% and nitrous oxide 60% with oxygen. Prior to incision, the surgeon infiltrated the graft harvest site with 0.2% ropivacaine. The average duration of surgery was 60–75 min. Additional doses of fentanyl (0.5 mcg kg−1) were given if indicated.
Just prior to extubation, IV tramadol 0.5 mg kg−1 was given to address the postoperative pain at the alveolus. After reversal, the patients were extubated awake. In the recovery room, pain and emergence delirium were assessed every 10 min for the first hour by an independent observer, using the FLACC Behavioral Pain Assessment scale and Watcha scale, respectively.[8,9] The patients were subsequently shifted to the postoperative ward. Pain was assessed at 3, 6, 12 and 24 h after the surgery to help guide rescue analgesia. The time of administration of the first rescue analgesic was also noted. Inj. tramadol 0.5 mg kg−1 was used as a rescue analgesic postoperatively, on demand, or if the pain score exceeded 2 during assessment at 3, 6, 12 and 24 h. The patients were also assessed after 24 h to confirm the benefits of early ambulation noted in the pilot study.
Pain and ambulatory status were evaluated by an independent observer. Pain was ranked using the 5-point verbal ranking score.[10] Ambulatory status was graded using one-day Cumulated Ambulatory Score[11] Patients were evaluated at 6 and 12 weeks postoperatively in the faciomaxillary clinic to detect chronic pain or numbness at the harvest site.
Data were statistically described in terms of range, mean, SD, frequencies and percentages when appropriate. Comparison of quantitative variables were done using the Mann–Whitney U test. For comparing categorical data, the Chi-square test was performed. All continuous data were expressed as mean (SD), while the categorical data were expressed as percentages. A probability value (P value) <0.05 was considered statistically significant. All statistical calculations were done using the computer programs Microsoft Excel version 7 and SPSS 22 Program for Microsoft Windows.
Results
Patient characteristics were comparable in both the groups [Table 1]. Sex distribution was comparable in both the groups (P value 0.93). Nearly 63% of our patients were children. Group A patients had significant pain relief 10 min after extubation (P value 0.001), with mean FLACC score being 0.8 in group A versus 1.8 in group B. Assessment at the subsequent study points revealed no significant difference between the two groups FLACC scores are shown in Table 2.
Table 1.
Comparison of the patient characteristics in the two groups
| Patient group characteristics | Group | Frequency | Mean | Standard deviation | P |
|---|---|---|---|---|---|
| Age (years) | A | 71 | 10.9 | 5.4 | 0.76 |
| B | 72 | 10.6 | 6.4 | ||
| Weight (kg) | A | 71 | 28.9 | 10.4 | 0.70 |
| B | 72 | 29.7 | 13.5 | ||
| Height (cm) | A | 71 | 133.4 | 20.7 | 0.25 |
| B | 72 | 129.5 | 19.5 |
Table 2.
Comparison of the FLACC scores in the two groups in first postoperative hour
| Time after extubation | Group | Frequency | Mean | SD | P | Median | Percentile | |
|---|---|---|---|---|---|---|---|---|
| 25th | 75th | |||||||
| 10 min | A | 71 | 0.82 | 1.67 | 0.001 | 0.00 | 0.00 | 1.00 |
| B | 72 | 1.82 | 2.0 | 1.00 | 0.00 | 3.50 | ||
| 20 min | A | 71 | 0.93 | 1.32 | 0.050 | 0.00 | 0.00 | 1.00 |
| B | 72 | 1.49 | 2.00 | 1.00 | 0.00 | 3.50 | ||
| 30 min | A | 71 | 0.96 | 1.22 | 0.47 | 1.00 | 0.00 | 1.00 |
| B | 72 | 0.81 | 1.29 | 0.00 | 0.00 | 1.00 | ||
| 40 min | A | 71 | 0.77 | 1.10 | 0.693 | 0.00 | 0.00 | 1.00 |
| B | 72 | 0.69 | 1.32 | 0.00 | 0.00 | 1.00 | ||
| 50 min | A | 71 | 0.59 | 0.87 | 0.706 | 0.00 | 0.00 | 1.00 |
| B | 72 | 0.53 | 1.13 | 0.00 | 0.00 | 0.00 | ||
| 60 min | A | 71 | 0.63 | 0.87 | 0.529 | 0.00 | 0.00 | 1.00 |
| B | 72 | 0.53 | 1.13 | 0.00 | 0.00 | 0.00 | ||
A significant decrease was noted in the postoperative delirium at 10 min after extubation in group A (P value 0.001), with mean Watcha score being 0.9 versus 1.7 in group B. The analysis of data at subsequent points showed no significant difference between the two groups Watcha scores are shown in Table 3. The incidence of pain and delirium in this period correlated strongly (Pearson's coefficient: 0.9) [Figure 2].
Table 3.
Comparison of the WATCHA scale in the two groups in first postoperative hour
| Time after extubation | Group | Frequency | Mean | SD | P | Median | Percentile | |
|---|---|---|---|---|---|---|---|---|
| 25th | 75th | |||||||
| 10 min | A | 71 | 0.94 | 1.03 | 0.001 | 1.00 | 0.00 | 1.00 |
| B | 72 | 1.67 | 1.16 | 1.00 | 1.00 | 2.75 | ||
| 20 min | A | 71 | 1.15 | 0.87 | 0.10 | 1.00 | 1.00 | 2.00 |
| B | 72 | 1.42 | 1.01 | 1.00 | 1.00 | 2.00 | ||
| 30 min | A | 71 | 1.30 | 1.25 | 0.72 | 1.00 | 1.00 | 2.00 |
| B | 72 | 1.24 | 0.66 | 1.00 | 1.00 | 1.00 | ||
| 40 min | A | 71 | 0.99 | 0.55 | 0.14 | 1.00 | 1.00 | 1.00 |
| B | 72 | 1.13 | 0.58 | 1.00 | 1.00 | 1.00 | ||
| 50 min | A | 71 | 0.90 | 0.51 | 0.11 | 1.00 | 1.00 | 1.00 |
| B | 72 | 1.03 | 0.41 | 1.00 | 1.00 | 1.00 | ||
| 60 min | A | 71 | 0.85 | 0.53 | 0.25 | 1.00 | 1.00 | 1.00 |
| B | 72 | 0.94 | 0.50 | 1.00 | 1.00 | 1.00 | ||
Figure 2.
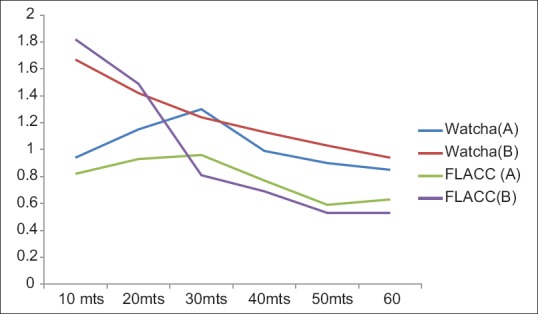
Comparison of the Watcha and FLACC scores in the first postoperative hour
The timing of first rescue analgesic administered to the patients in either group was only marginally different and statistically insignificant [Table 4]. Most patients in both groups required the rescue drug between 6–12 h postop. However, 24 h later group A patients were found to have lower average pain scores [Figure 3]. Significantly higher number of patients in group A had no pain (P = 0.004). Incidence of intolerable pain was significantly higher in group B (P = 0.04). Patients in group A had better ambulation scores, P value being significant at all scores. The average score was 5.7 in group A and 4.9 in group B [Table 5 and Figure 4]. Pain and ambulatory status at 24 h were found to have a strong and positive correlation (Pearson's coefficient: 0.95). At the follow-up clinic, none of the patients in either group had chronic pain or gait disturbances. Two patients in group B had wound infection.
Table 4.
Comparison of the timing of first rescue analgesic administration in the two groups
| Timing of rescue analgesics | Group | Frequency | Percentage | P |
|---|---|---|---|---|
| 0-3 h | A | 0 | 0 | 0.31 |
| B | 1 | 1.4 | ||
| 3-6 h | A | 9 | 12.7 | 0.13 |
| B | 16 | 22.2 | ||
| 6-12 h | A | 61 | 85.9 | 0.07 |
| B | 53 | 73.6 | ||
| 12-24 h | A | 1 | 1.4 | 0.57 |
| B | 2 | 2.8 |
Figure 3.
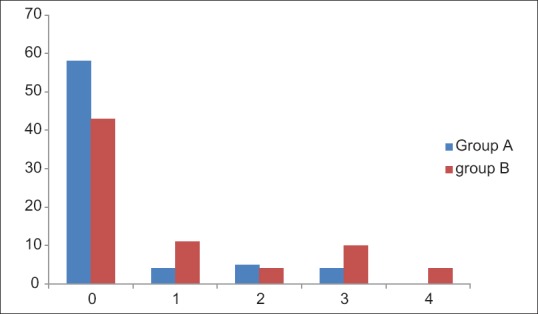
Comparison of pain scores in the two groups after 24 h
Table 5.
Comparison of the pain and cumulated ambulation scores (CAS) in the two groups 24 h later
| Pain scoring | Group | Frequency | Percentage | P | CAS | Group | Frequency | Percentage | P |
|---|---|---|---|---|---|---|---|---|---|
| 0 | A | 58 | 81.7 | 0.004 | 6 | A | 56 | 78.8 | 0.01 |
| B | 43 | 59.7 | B | 43 | 60.6 | ||||
| 1 | A | 4 | 5.6 | 0.06 | 5 | A | 7 | 9.9 | 0.001 |
| B | 11 | 15.3 | B | 5 | 6.9 | ||||
| 2 | A | 5 | 7.04 | 0.71 | 4 | A | 7 | 9.9 | 0.01 |
| B | 4 | 5.6 | B | 8 | 11.1 | ||||
| 3 | A | 4 | 5.6 | 0.09 | 3 | A | 1 | 1.4 | 0.01 |
| B | 10 | 13.9 | B | 6 | 8.3 | ||||
| 4 | A | 0 | 0 | 0.04 | 2 | A | 0 | 0 | 0.01 |
| B | 4 | 5.6 | B | 6 | 8.3 | ||||
| 1 | A | 0 | 0 | 0.01 | |||||
| B | 4 | 5.6 | |||||||
Figure 4.
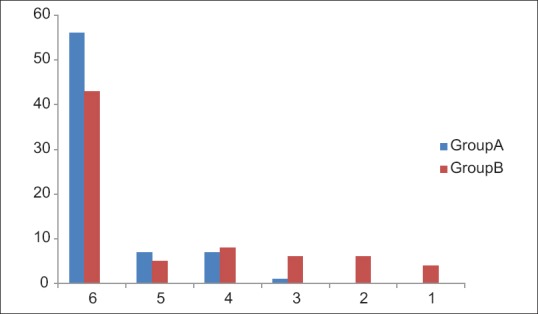
Comparison of ambulation scores (CAS) in the two groups after 24 h
Discussion
We observed that patients who received an additional TAP block had significantly lower levels of pain for the first postoperative day. They were also less agitated in the first 10 min following extubation. Better analgesia on the first postoperative day, correlated with better ambulation scores.
The optimal analgesic regimen should provide safe and effective analgesia, thereby reducing postoperative stress response and accelerating recovery.[12] A multimodal analgesic technique is frequently used to achieve these goals; however, the optimal regimen remains to be elucidated.[13] Another relevant issue pertaining to pain is its chronicisation.[14]
The major drawback of iliac crest bone harvesting is the harvest site morbidity, predominantly pain and sensory disturbances.[15] During the immediate postoperative period, patients may experience more pain at the donor site than at the actual surgical site.[13]
Wound infiltration with local anesthetic is a simple, effective and inexpensive means of providing good analgesia. However well-documented pain relief is reported to last for only 6–8 h.[13] The diffuse innervation of the abdominal wall makes it difficult to achieve a satisfactory analgesia solely with wound infiltration.[16]
A retrospective review conducted by Palmar et al., in patients who had undergone iliac crest bone grafting showed that 46.6% had acute temporary pain, whereas 16.6% had chronic pain at 6 months.[17] Unilateral TAP block has been shown to be effective in providing superior analgesia in first 48 h after appendicectomy in children.[18] TAP block has been proposed to decrease postoperative pain after anterior iliac crest harvest.[8]
This has been supported by our study. However, there was no difference in need for rescue analgesia up to 24 h. After 24 h, 5.6% of the patients in group B had severe, intolerable pain (P value 0.04), as against none in the TAP group. None of our patients had chronic pain.
The anterior iliac crest and its overlying skin are innervated by ventral rami from intercostal nerves T11 and T12 and by the iliohypogastric nerve (L1 and L2). These nerves run in the plane between the transversus abdominis and internal oblique muscles of the abdominal wall. The TAP block permits a sensory block of the lower six thoracic and first lumbar ventral rami.[7] Imaging studies on cadavers and volunteers have demonstrated the spread of solution in a plane between both muscles, with a subsequent sensory blockade from T8 to L1.[19] Therefore, TAP block can provide efficient postoperative analgesia for anterior iliac crest harvest.[1] The use of ultrasound improves the success rate of the block by allowing accurate localisation of the target nerve and placement of the needle in the precise position. It also permits administration of the local anaesthetic at any level between the internal oblique and transversus abdominis muscles. Thus, a kind of ‘natural elastomeric pump’ is produced with a gradual release of the drugs over several hours.[16] Multimodal analgesia when administered during surgery combats peripheral and central ‘windup’ and should last long enough to minimise wound inflammation and hyperalgesia.[12] The above mechanisms probably account for better patient comfort in the study group.
Emergence delirium is a significant problem especially in paediatric patients.[9] The incidence of emergence delirium following general anesthesia in children was 26% using the Watcha scale in a study conducted by Bajwa et al.[20] Emergence delirium (Watcha >2) was lower in our study: 2.4% in patients who had received TAP block, as against 9.5% in the control group. While this can reflect better pain relief, the fact that our study population also included 37% adults could have reduced the overall incidence. The prevalence of emergence delirium in the general population is around 4.7%.[21]
Good perioperative analgesia has been shown to be effective in preventing emergence delirium.[9] Our study also showed that there was a strong and positive correlation between the severity of postoperative pain and emergence delirium (Pearson's coefficient 0.866).
Patients had lower mean pain scores and subsequently shorter length of hospital stay and time to initial ambulation, when graft site infiltration was combined with bupivacaine-soaked sponges.[22] In this study we also evaluated these parameters, thus differing from previous studies using TAP block for iliac crest bone graft harvesting. Similar results were observed for our study. About 81.7% of our patients who had received supplemental TAP block had no pain after 24 h versus 59.7% in group B (P value 0.004). This is also reflected in the better ambulation scores in the study group.
The main limitation of our study was the non-homogenous age group of the subjects. The FLACC score was used as most of the patients were expected to be children. This is not an ideal tool for adult patients. Pain at the recipient site is a confounder. Future similar studies done exclusively in children, and a trial with TAP block as the sole technique, may also help clarify actual benefit.
Conclusion
Supplemental ultrasound-guided TAP block given intraoperatively improves the postoperative pain relief at bone graft harvest site. The incidence of emergence delirium was also low. The reduced pain permits early ambulation with the potential to reduce hospital stay.
Authors contributions
The study was designed and conducted by Usha Shenoy and Vigil Peter. Philip Mathew oversaw the patient recruitment follow up. Data analysis and interpretation was done by Tom Thomas. All the authors contributed to the final draft.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cansiz E, Sitilci TA, Uzun A, Isle SC. Reconstruction of atrophic maxillary by anterior iliac crest bone grafting with via neuraxial blockade technique: A case report. J Istanbul Universal Fac Dent. 2017;51:46–51. doi: 10.17096/jiufd.68600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dimitriou R, Mataliotakis G, Angoules A, Kanakaris N, Giannoudis P. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: A systematic review. Injury. 2011;42(Suppl 2):S3–15. doi: 10.1016/j.injury.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 3.DeOrio JK, Farber DC. Morbidity associated with anterior iliac crest bone grafting in foot and ankle surgery. Foot Ankle Int. 2005;26:147–51. doi: 10.1177/107110070502600206. [DOI] [PubMed] [Google Scholar]
- 4.Clarke A, Flowers MJ, Davies AG, Fernandes J, Jones S. Morbidity associated with anterior iliac crest bone graft harvesting in children undergoing orthopaedic surgery: A prospective review. J Evid Child Orthop. 2015;9:411–6. doi: 10.1007/s11832-015-0698-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim DH, Rhim R, Li L, Martha J, Swaim BH, Banco RJ, et al. Prospective study of iliac crest bone graft harvest site pain and morbidity. Spine J. 2009;9:886–92. doi: 10.1016/j.spinee.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Hahn M, Dover MS, Wheat NM, Moule I. Local bupivacaine infusion following bone graft harvest from the iliac crest. Int J Oral Maxillofac Surg. 1996;25:400–1. doi: 10.1016/s0901-5027(06)80041-x. [DOI] [PubMed] [Google Scholar]
- 7.McDonnell JG, O’Donnell B, Curley G, Hefferman A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomised controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 8.Chiono J, Bernard N, Bringuier S, Biboulet P, Choquet O, Morau D, et al. The ultrasound guided transversus abdominis plane block for anterior iliac crest bone graft postoperative pain relief-a prospective descriptive study. Reg Anaesth Pain Med. 2010;35:520–4. doi: 10.1097/AAP.0b013e3181fa117a. [DOI] [PubMed] [Google Scholar]
- 9.Voepel-Lewis T, Zanotti J, Dammeyer JA, Merkel S. Reliability and validity of the face, legs, activity, cry, consolability behavioural tool in assessing acute pain in critically ill patients. Am J Crit Care. 2010;19:55–61. doi: 10.4037/ajcc2010624. [DOI] [PubMed] [Google Scholar]
- 10.Reduque LL, Verghese ST. UK: Oxford University Press Publishers; 2012. Paediatric Emergence Delirium - CEACCP Advance Access. [Google Scholar]
- 11.Ferreira-Valente MA, Pais-Ribeiro J, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152:2399–404. doi: 10.1016/j.pain.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Scott NB. Wound infiltration for surgery. Anaesthesia. 2010;65(Suppl 1):67–75. doi: 10.1111/j.1365-2044.2010.06241.x. [DOI] [PubMed] [Google Scholar]
- 13.McNaught A, Shastri U, Carmichael N, Awad IT, Columb M, Cheung J, et al. Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth. 2011;106:124–30. doi: 10.1093/bja/aeq306. [DOI] [PubMed] [Google Scholar]
- 14.Juliane Z, Wolfgang H, Michael M, Heiko K. Analysis of postoperative pain at the Anterior Iliac crest harvest site: A prospective study of the intraoperative local administration of ropivacaine. Asian Spine J. 2015;9:39–46. doi: 10.4184/asj.2015.9.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curtis D, Kristensen MT. Cumulated Ambulation score (CAs), English version, manual and score sheet. [Last accessed on 2015 Jan 15]. Available from: https://www.researchgate.net/publication/270888051 .
- 16.Galante D, Caruselli M, Dones F, Meola S, Russo G, Pellico G, et al. Ultrasound Transversus Abdominis Plane block in paediatric patients: Not only a regional technique for adults. Anaesth Pain Intensive Care. 2012;16:201–4. [Google Scholar]
- 17.Palmer W, Crawford-Sykes A, Rose REC. Donor site morbidity following iliac crest bone graft. West Indian Med J. 2008:57:490. [PubMed] [Google Scholar]
- 18.Carney J, Finnerty O, Rauf J, Curley G, McDonnell JG, Laffey JG. Ipsilateral transversus abdominis plane block provides effective analgesia after appendicectomy in children-a randomised controlled trial. Anesth Analg. 2010;111:998–1003. doi: 10.1213/ANE.0b013e3181ee7bba. [DOI] [PubMed] [Google Scholar]
- 19.O’Donnell BD. Cadaveric and radiological evaluation of the transversus abdominis plane block. Reg Anesth Pain Med. 2006;31:3. doi: 10.1016/j.rapm.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 20.Bajwa SA, Costi D, Cyna AM. A comparison of emergence delirium scales following general anaesthesia in children. Paediatric Anaesth. 2010;20:704–11. doi: 10.1111/j.1460-9592.2010.03328.x. [DOI] [PubMed] [Google Scholar]
- 21.Lepousé C, Lautner CA, Liu L, Gomis P, Leon A. Emergence delirium in adults in the post-anaesthesia care unit. Br J Anesth. 2006;96:747–53. doi: 10.1093/bja/ael094. [DOI] [PubMed] [Google Scholar]
- 22.Dashow JE, Lewis CW, Hopper RA, Gruss JS, Egbert MA. Bupivacaine administration and postoperative pain following anterior iliac crest bone grafting for alveolar cleft repair. Cleft Palate Craniofac J. 2009;46:173–8. doi: 10.1597/07-136.1. [DOI] [PubMed] [Google Scholar]


