Abstract
Background
Anaemia is a condition in which the number of red blood cells is insufficient to meet physiologic needs; it is caused by many conditions, particularly iron deficiency. Traditionally, daily iron supplementation has been a standard practice for preventing and treating anaemia. However, its long‐term use has been limited, as it has been associated with adverse side effects such as nausea, constipation, and teeth staining. Intermittent iron supplementation has been suggested as an effective and safer alternative to daily iron supplementation for preventing and reducing anaemia at the population level, especially in areas where this condition is highly prevalent.
Objectives
To assess the effects of intermittent oral iron supplementation, alone or in combination with other nutrients, on anaemia and its associated impairments among menstruating women, compared with no intervention, a placebo, or daily supplementation.
Search methods
In February 2018, we searched CENTRAL, MEDLINE, Embase, nine other databases, and two trials registers. In March 2018, we also searched LILACS, IBECS and IMBIOMED. In addition, we examined reference lists, and contacted authors and known experts to identify additional studies.
Selection criteria
Randomised controlled trials (RCTs) and quasi‐RCTs with either individual or cluster randomisation. Participants were menstruating women; that is, women beyond menarche and prior to menopause who were not pregnant or lactating and did not have a known condition that impeded the presence of menstrual periods. The intervention was the use of iron supplements intermittently (one, two or three times a week on non‐consecutive days) compared with placebo, no intervention, or the same supplements provided on a daily basis.
Data collection and analysis
Both review authors independently assessed the eligibility of studies against the inclusion criteria, extracted data from included studies, checked data entry for accuracy, assessed the risk of bias of the included studies, and rated the quality of the evidence using GRADE.
Main results
We included 25 studies involving 10,996 women. Study methods were not well described in many of the included studies and thus assessing risk of bias was difficult. The main limitations of the studies were lack of blinding and high attrition. Studies were mainly funded by international organisations, universities, and ministries of health within the countries. Approximately one third of the included studies did not provide a funding source.
Although quality across studies was variable, the results consistently showed that intermittent iron supplementation (alone or with any other vitamins and minerals) compared with no intervention or a placebo, reduced the risk of having anaemia (risk ratio (RR) 0.65, 95% confidence interval (CI) 0.49 to 0.87; 11 studies, 3135 participants; low‐quality evidence), and improved the concentration of haemoglobin (mean difference (MD) 5.19 g/L, 95% CI 3.07 to 7.32; 15 studies, 2886 participants; moderate‐quality evidence), and ferritin (MD 7.46 μg/L, 95% CI 5.02 to 9.90; 7 studies, 1067 participants; low‐quality evidence). Intermittent regimens may also reduce the risk of having iron deficiency (RR 0.50, 95% CI 0.24 to 1.04; 3 studies, 624 participants; low‐quality evidence), but evidence was inconclusive regarding iron deficiency anaemia (RR 0.07, 95% CI 0.00 to 1.16; 1 study, 97 participants; very low‐quality evidence) and all‐cause morbidity (RR 1.12, 95% CI 0.82 to 1.52; 1 study, 119 participants; very low‐quality evidence). Women in the control group were less likely to have any adverse side effects than those receiving intermittent iron supplements (RR 1.98, 95% CI 0.31 to 12.72; 3 studies, 630 participants; moderate‐quality evidence).
In comparison with daily supplementation, results showed that intermittent supplementation (alone or with any other vitamins and minerals) produced similar effects to daily supplementation (alone or with any other vitamins and minerals) on anaemia (RR 1.09, 95% CI 0.93 to 1.29; 8 studies, 1749 participants; moderate‐quality evidence). Intermittent supplementation may produce similar haemoglobin concentrations (MD 0.43 g/L, 95% CI −1.44 to 2.31; 10 studies, 2127 participants; low‐quality evidence) but lower ferritin concentrations on average (MD −6.07 μg/L, 95% CI −10.66 to −1.48; 4 studies, 988 participants; low‐quality evidence) compared to daily supplementation. Compared to daily regimens, intermittent regimens may also reduce the risk of having iron deficiency (RR 4.30, 95% CI 0.56 to 33.20; 1 study, 198 participants; very low‐quality evidence). Women receiving iron supplements intermittently were less likely to have any adverse side effects than those receiving iron supplements daily (RR 0.41, 95% CI 0.21 to 0.82; 6 studies, 1166 participants; moderate‐quality evidence). No studies reported on the effect of intermittent regimens versus daily regimens on iron deficiency anaemia and all‐cause morbidity.
Information on disease outcomes, adherence, economic productivity, and work performance was scarce, and evidence about the effects of intermittent supplementation on these outcomes unclear.
Overall, whether the supplements were given once or twice weekly, for less or more than three months, contained less or more than 60 mg of elemental iron per week, or given to populations with different degrees of anaemia at baseline did not seem to affect the findings. Furthermore, the response did not differ in areas where malaria was frequent, although very few trials were conducted in these settings.
Authors' conclusions
Intermittent iron supplementation may reduce anaemia and may improve iron stores among menstruating women in populations with different anaemia and malaria backgrounds. In comparison with daily supplementation, the provision of iron supplements intermittently is probably as effective in preventing or controlling anaemia. More information is needed on morbidity (including malaria outcomes), side effects, work performance, economic productivity, depression, and adherence to the intervention. The quality of this evidence base ranged from very low to moderate quality, suggesting that we are uncertain about these effects.
Keywords: Adolescent; Adult; Female; Humans; Young Adult; Administration, Oral; Anemia, Iron-Deficiency; Anemia, Iron-Deficiency/prevention & control; Dietary Supplements; Drug Administration Schedule; Ferritins; Ferritins/adverse effects; Ferritins/blood; Ferrous Compounds; Ferrous Compounds/administration & dosage; Iron Deficiencies; Iron, Dietary; Iron, Dietary/administration & dosage; Menstruation; Micronutrients; Micronutrients/administration & dosage; Randomized Controlled Trials as Topic
Plain language summary
Iron supplements taken one, two or three times a week for preventing anaemia, and its consequences in menstruating women
What is the issue?
Across the globe, approximately one out of three non‐pregnant women of reproductive age are anaemic; i.e. have fewer red blood cells or less haemoglobin (a red substance that combines with oxygen and carries it around the body) in each red blood cell than normal. Although there are several causes of anaemia, it very often results from sustained iron deficiency. The standard practice to prevent or treat anaemia in women has been daily iron supplementation (sometimes combined with folic acid and other vitamins and minerals) for three months. However, it is frequently associated with side effects such as nausea or constipation. Intermittent supplementation (that is, the consumption of supplements one, two or three times a week on non‐consecutive days) has been proposed as an effective and safer alternative to daily supplementation.
Why is this important?
Women with anaemia may have less energy for physical work and become more prone to infections. Most women throughout the world enter pregnancy with anaemia, putting them at greater risk of having low birth‐weight babies and other complications during delivery.
Some scientists believe that taking iron a few times a week – instead of every day – can help women with anaemia to feel better and improve their haemoglobin without giving them as many side effects. If women have fewer side effects, they may be more likely to take iron supplements more regularly and for longer periods.
What evidence did we find?
We reviewed the evidence in February 2018. We included 25 randomised controlled trials (a type of experiment in which participants are randomly assigned to one or more treatment groups) involving 10,996 women. We included studies examining the administration of intermittent iron supplements versus no intervention, a placebo (dummy pill) or the same supplements given on a daily basis. Most studies were implemented in school settings and were mainly funded by international organisations, universities, and ministries of health within the countries. Approximately one‐third of the included studies did not provide a funding source.
The findings show that women receiving intermittent supplementation with iron alone, or in combination with folic acid or other nutrients, were less likely to be anaemic or iron deficient than those women who received no iron supplements or a placebo. They also had higher concentrations of haemoglobin and ferritin (a protein that carries iron) but reported more side effects.
In addition, the findings indicate that intermittent supplementation was as effective as daily supplementation in reducing the prevalence of anaemia and increasing haemoglobin concentrations, with fewer side effects. It may have reduced the risk of having iron deficiency also, but it had no effect on raising ferritin concentrations more than the daily dose.
We found scarce evidence on the effect of intermittent supplementation compared to placebo or daily supplementation on iron deficiency anaemia, all‐cause morbidity, disease outcomes, adherence, economic productivity, and work performance.
What does this mean?
Intermittent iron supplementation in menstruating women may be an effective intervention for reducing anaemia and improving haemoglobin concentrations compared to no treatment, placebo or daily supplementation. Intermittent supplementation may be associated with fewer side effects compared to daily supplementation. The findings were not affected by whether the supplements were given once or twice weekly, for less or more than three months, contained less or more than 60 mg of elemental iron per week, or given to populations with different degrees of anaemia at baseline (starting point for comparisons). The evidence base was of overall low quality.
Summary of findings
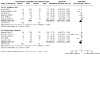
Summary of findings 1. Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo in menstruating women.
| Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo in menstruating women | ||||||
| Patient or population: adolescent and adult menstruating women Setting: community settings Intervention: intermittent iron supplementation (alone or with any other micronutrients) Comparison: no supplementation or placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with no supplementation or placebo | Risk with intermittent iron supplementation (alone or with any other micronutrients) | |||||
| Anaemia (haemoglobin concentration below a cut‐off defined by the trialists, adjusted by altitude and smoking as appropriate) Follow‐up: range 2 months to 6 months | Study population | RR 0.65 (0.49 to 0.87) | 3135 (11 studies) | ⊕⊕⊝⊝ Lowa | Includes seven cluster‐randomised trials b | |
| 39 per 100 | 25 per 100 (19 to 34) | |||||
| Haemoglobin (g/L) Follow‐up: range 2 months to 6 months | The mean haemoglobin g/L in the control groups ranged from −0.24 to 133.20 | The mean haemoglobin g/L in the intervention groups was 5.19 higher (3.07 higher to 7.32 higher) | ‐ | 2886 (15 studies) | ⊕⊕⊕⊝ Moderatec | Includes five cluster‐randomised trials b |
| Iron deficiency (as defined by trialists by using indicators of iron status such as ferritin or transferrin) Follow‐up: range 3 months to 4 months | Study population | RR 0.50 (0.24 to 1.04) | 624 (3 studies) | ⊕⊕⊝⊝ Lowd | Includes one cluster‐randomised trial b | |
| 49 per 100 | 25 per 100 (12 to 51) | |||||
| Ferritin (µg/L) Follow‐up: range 3 months to 6 months | The mean ferritin µg/L in the control groups ranged from −5.31 to 41 | The mean ferritin μg/L in the intervention groups was 7.46 higher (5.02 higher to 9.90 higher) | ‐ | 1067 (7 studies) | ⊕⊕⊝⊝ Lowe | Includes one cluster‐randomised trial b |
| Iron deficiency anaemia (as defined by the presence of anaemia plus iron deficiency diagnosed with an indicator of iron status selected by the trialists) Follow‐up: 4 months | Study population | RR 0.07 (0.00 to 1.16) | 97 (1 study) | ⊕⊕⊝⊝ Lowf | The included trial is a cluster‐randomised trial b | |
| 7 per 100 | 1 per 100 (0 to 8) | |||||
|
All‐cause morbidity (the most frequent event associated with the intervention, independent of the cause, as defined by the trialists) Follow‐up: 4 months |
Study population | RR 1.12 (0.82 to 1.52) | 119 (1 study) | ⊕⊕⊝⊝ Lowg | ‐ | |
| 55 per 100 | 61 per 100 (45 to 83) | |||||
| Any adverse side effects | 13 per 100 |
26 per 100 (4 to 100) |
RR 1.98 (0.31 to 12.72) |
630 (3 studies) |
⊕⊕⊕⊝ Moderateh | |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level due to study limitations (in several trials the method of allocation concealment was not clear and there was a lack of blinding) and one level due to inconsistency (high heterogeneity) (I2 = 83%). bFor cluster‐randomised trials (C), the analyses only include the estimated effective sample size, after adjusting the data to account for the clustering effect. cDowngraded one level due to inconsistency (high heterogeneity) (I2 = 85%). dDowngraded one level due to imprecision (wide CI) and one level due to inconsistency (high heterogeneity) (I2 = 89%). eDowngraded one level due to study limitations (in several trials the method of allocation concealment was not clear and there was a lack of blinding) and one level due to imprecision (wide CI) (I2 = 48%). fDowngraded one level due to lack of blinding and one level due to imprecision (wide CI and not enough information to detect a precise estimate of the effect ‐ only one study reported on this outcome) (I2 = not estimable). gDowngraded one level due to study attrition and one level due to imprecision (not enough information to detect a precise estimate of the effect ‐ only one study reported on this outcome) (I2 = not estimable). hDowngraded one level due to inconsistency (high heterogeneity) (l2 = 91%)
Summary of findings 2. Intermittent iron supplementation versus daily iron supplementation in menstruating women.
| Intermittent iron supplementation versus daily iron supplementation in menstruating women | ||||||
| Patient or population: adolescent and adult menstruating women Setting: community settings Intervention: intermittent iron supplementation alone or with any other micronutrients Comparison: daily iron supplementation alone or with any other micronutrients | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with daily iron supplementation | Risk with intermittent iron supplementation | |||||
| Anaemia (haemoglobin concentration below a cut‐off defined by the trialists, adjusted by altitude and smoking as appropriate) Follow‐up: range 2 months to 4 months | Study population | RR 1.09 (0.93 to 1.29) | 1749 (8 studies) | ⊕⊕⊕⊝ Moderatea | Includes two cluster‐randomised trials* b | |
| 23 per 100 | 25 per 100 (22 to 30) | |||||
| Haemoglobin (g/L) Follow‐up: range 2 months to 1 year | The mean haemoglobin g/L in the control groups ranged from 7.40 g/L to 132.00 g/L | The mean haemoglobin g/L in the intervention groups was 0.43 g/L higher (1.44 lower to 2.31 higher) | ‐ | 2127 (10 studies) | ⊕⊕⊝⊝ Lowc | Includes two cluster‐randomised trials* b |
| Iron deficiency (as defined by the trialists using indicators of iron status such as ferritin or transferrin) Follow‐up: mean 3 months | Study population | RR 4.30 (0.56 to 33.20) | 198 (1 study) | ⊕⊝⊝⊝ Very lowd | ‐ | |
| 2 per 100 | 7 per 100 (1 to 52) | |||||
| Ferritin (µg/L) Follow‐up: range 2 months to 1 year | The mean ferritin µg/L in the control groups ranged from 16.70 µg/L to 62.00 µg/L | The mean ferritin µg/L in the intervention groups was 6.07 µg/L lower (10.66 lower to 1.48 lower) | ‐ | 988 (4 studies) | ⊕⊕⊝⊝ Lowe | Includes one cluster‐randomised trial b |
| Iron deficiency anaemia (as defined by the presence of anaemia plus iron deficiency, diagnosed with an indicator of iron status selected by the trialists) | Not estimable | ‐ | (0 studies) | ‐ | ‐ | |
| All‐cause morbidity (the most frequent event associated with the intervention, independent of the cause, as defined by the trialists) | Not estimable | ‐ | (0 studies) | ‐ | ‐ | |
| Any adverse side effects | 29 per 100 |
2 per 100 (6 to 24) |
RR 0.41 (0.21 to 0.82) |
1166 (6 studies) |
⊕⊕⊕⊝ Lowf | Includes one cluster‐randomised trial b |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level due to study limitations (in several trials the method of allocation concealment was not clear and there was a lack of blinding) (I2 = 12%). bFor cluster‐randomised studies (C), the analyses only include the estimated effective sample size, after adjusting the data to account for the clustering effect. cDowngraded two levels due to inconsistency (in the direction of the effect and the CI of some of the included studies cross the line of no effect, and high heterogeneity) (I2 = 78%). dDowngraded two levels due to imprecision (only one study with 25 losses to follow‐up reported data on this outcome; wide CI) and one level for study limitations (concerns about attrition) (l2 = not estimable). eDowngraded two levels due to inconsistency (in the direction of the effect and the CI of some of the included studies cross the line of no effect, and high heterogeneity) (I2 = 91%). f Downgraded two levels due to inconsistency (in the direction of the effect and the CI of some of the included studies cross the line of no effect, and high heterogeneity) (I2 = 82%).
Background
Description of the condition
Anaemia is a condition in which the oxygen‐carrying capacity of the blood is insufficient to meet the physiologic needs of body tissues. The global prevalence of this condition in non‐pregnant women of reproductive age is estimated to be 29.0% (WHO 2015), and it is more frequent in low‐ and middle‐income countries or among women who belong to a low socioeconomic stratum (Soekarjo 2001; Bodnar 2002; Bentley 2003). Anaemia has multiple direct causes that very often coexist: it can result from parasitic infections (Kumar 2007; Anah 2008); inflammatory disorders (Yip 1988); inherited disorders of haemoglobin structure; oxidative stress (i.e. imbalance between free radicals and antioxidants) and vitamin and mineral deficiencies such as that of vitamins A and B12, and folate (Herbert 1987; Hercberg 1992; Jimenez 2010), and especially iron, which is responsible for at least half of the cases of anaemia (WHO 2001).
Iron deficiency results from long‐term imbalance caused by inadequate dietary iron intake, poor iron absorption or utilisation, increased iron requirements, or chronic blood loss (Alleyne 2008). Individual iron requirements vary considerably throughout the human life cycle (Lynch 2007), and both physiological (for example, pregnancy or early postpartum) or pathological (for example, HIV infection) conditions affect iron requirements (WHO 2001). Postmenarchal women are at higher risk of developing iron deficiency because of menstrual losses, and if they do not have an adequate iron intake, this condition can progress to anaemia (known as iron deficiency anaemia or IDA).
Iron deficiency is one of the most prevalent forms of malnutrition globally. It is estimated that 50% of anaemia is attributable to iron deficiency worldwide (WHO 2001). Iron deficiency, even in the absence of anaemia, may either cause disability directly or be a risk factor for it (Stoltzfus 2003). For example, it causes impaired muscle function and impaired resistance to infections in all age groups (Beard 2005), and it is associated with reduced physical capacity and work performance in adolescents and adults (Beard 2001; WHO 2001; Clark 2008). Most women throughout the world enter pregnancy with less than desirable iron reserves, which reduce their reproductive performance (Viteri 2005). In addition to iron deficiency, women are frequently deficient in other vitamins and minerals that play important roles in the body (Ramakrishnan 2002; Kontic‐Vucinic 2006; Ahmed 2008). An adequate folate intake during the periconceptional period, for example, is crucial to reducing the risk of having a baby with neural tube defects (NTDs) (De‐Regil 2015); vitamin B12 and folate deficiencies are major causes of anaemia (Green 2017), while vitamin A regulates many critical functions, including vision, integrity of epithelial tissue (i.e. membranous tissue covering internal organs and other internal surfaces of the body), the expression of several hundred genes, and its deficiency also contributes to nutritional anaemia (WHO 2011a). Although these deficiencies may not translate into a comparable prevalence of anaemia, supplementation of these nutrients in women may improve their health throughout life, as there is some indication that these deficiencies are of public health concern in certain countries (McLean 2008).
Anaemia in women of reproductive age is diagnosed when the haemoglobin concentration in the blood is below 120 g/L, a cut‐off that varies with residential elevation above sea level (altitude) and smoking (WHO 2011b). Iron deficiency anaemia is diagnosed by the combined presence of anaemia and iron deficiency, measured by ferritin (< 15 μg/L) or any other indicator of iron status such as serum transferrin receptors or zinc protoporphyrin (WHO 2011c).
Description of the intervention
Daily iron plus folic acid supplementation remains the standard approach for the prevention and treatment of anaemia among menstruating women, since dietary changes alone usually cannot correct this condition, as the iron content in the diet is relatively constant and difficult to increase (DeMaeyer 1989). The recommended daily, supplemental dosage for non‐pregnant women of reproductive age living in countries where anaemia is highly prevalent (i.e. above 40%) is 60 mg of elemental iron and 400 µg of folic acid for three months (WHO 2001). The use of folic acid prior to pregnancy aims to improve folate status, and this dose has been shown to be effective for preventing NTDs in women who become pregnant (WHO 2001). Despite its proven efficacy, the main problem with the daily regimen is lack of compliance, due to side effects such as diarrhoea, constipation, dark stools, metallic taste, teeth staining, and nausea (Yip 1994).
Intermittent oral iron supplementation (i.e. one, two or three times a week on non‐consecutive days) has been suggested as an effective alternative to daily iron supplementation to prevent anaemia at the population level. The efficacy of intermittent iron supplementation for the prevention of anaemia and iron deficiency has been studied over the last 15 years in children, adolescents and pregnant and non‐pregnant women of reproductive age. A review of 22 trials performed in all of these groups concluded that both daily and once‐weekly iron supplementation were efficacious under favourable conditions in reducing anaemia (Beaton 1999). Subsequent trials in menstruating women have confirmed these findings (Crape 2005; Khan 2005; Paulino 2005), although some study authors have suggested that the weekly intake of supplemental iron may be insufficient to meet women's needs and have proposed the use of iron supplements twice a week (Kianfar 2000; Olsen 2000). Recent trials have used a variety of intermittent iron supplementation schemes such as: a double dose, once‐ and twice‐a‐week scheme, which reduced iron deficiency efficiently (Ahmed 2012); and a once‐a‐week scheme, with and without other micronutrients, which improved iron status (Bansal 2016) and haemoglobin concentration significantly (Kätelhut 1996).
The international recommendation for weekly supplementation for non‐pregnant women of reproductive age is that supplements should contain 60 mg of elemental iron in the form of ferrous sulphate and 2800 µg (2.8 mg) of folic acid (WHO 2011d). Although evidence for the effective dose of folic acid for intermittent supplementation is very limited, the current recommendation is based on the rationale of providing seven times the recommended daily dose to prevent NTDs, and experimental evidence that high weekly doses can improve red blood cell folate concentrations to levels that have been associated with a reduced risk of NTDs (Martinez‐de Villareal 2001; Martinez‐de Villareal 2002; Norsworthy 2004; Nguyen 2008). However, some countries have chosen to give a higher dose in their programmes. India, for example, provides 100 mg of elemental iron (Vir 2008) under supervised and unsupervised conditions, decreasing the prevalence of anaemia from 73.3% to 25.4%. The provision of vitamins and minerals other than iron and folic acid on an intermittent basis may also help to supplement women's diets and therefore improve health and development throughout the life cycle (Allen 2009a; Allen 2009b; Dalmiya 2009).
How the intervention might work
Intestinal cells turn over every five to six days in humans. Hence, providing iron on an intermittent basis would expose this nutrient to new mucosal cells (made up of epithelial tissue) only, improving absorption efficiency (Viteri 1995), and reducing oxidative stress and side effects (Viteri 2005). It may also reduce absorption blockage due to high iron levels in the gut lumen (i.e. inside space of the gut) and in the enterocyte (i.e. intestinal cell) (Anderson 2005; Oates 2007). Intermittent regimens may be perceived as more tolerable, ergo increasing adherence to supplementation (Casanueva 2006). In order to improve the success of this intervention, the World Health Organization (WHO) encourages the integration of intermittent iron supplementation programmes with other public health measures, including deworming to prevent hookworm infections, improved bioavailable dietary iron intake, and interventions to control other prevalent causes of anaemia, particularly malaria, other infections, and vitamin A deficiency (WHO 2011d).
The endemicity of malaria in a given region is an important consideration when providing iron supplements at the population level. Malaria, which is responsible for more than a million deaths per year (Gajida 2010), causes anaemia through several mechanisms. Provision of iron in malaria‐endemic areas, particularly to children, has been a long‐standing controversy due to concerns that iron therapy may exacerbate infections, particularly malaria (Oppenheimer 2001; Okabe 2011). Although the mechanisms by which additional iron can benefit the parasite are far from clear (Prentice 2007), intermittent supplementation might be an effective option to prevent anaemia and improve malaria treatment in malaria‐endemic areas since less iron is available for the parasite.
Why it is important to do this review
Improving iron and folate nutrition of adolescent and adult menstruating women may contribute to adequate mental and physical performance and reproductive health, which may, in turn, significantly enhance maternal and infant health outcomes. Intermittent supplementation is proposed as a viable approach for improving iron and folate status in populations, especially in areas where anaemia is highly prevalent, and where mass fortification of staple foods with iron and folic acid is not available and not likely to be available in the near future.
After the publication of the first version of this review (Fernández‐Gaxiola 2011a), WHO published guidelines on intermittent iron supplementation (WHO 2011d), and WHO Member States committed to the World Health Assembly to halve anaemia in pregnant and non‐pregnant women of reproductive age by 2025 (WHO 2014). To date, weekly iron supplementation has been implemented in more than 10 countries in Asia and Africa, but there is still a need for the literature to be systematically reviewed so there is updated evidence on the efficacy, effectiveness, and safety of this intervention, to inform a possible scale‐up as part of public health programmes.
This is an update of the previous review (Fernández‐Gaxiola 2011a), which was to inform the WHO guideline on intermittent supplementation in menstruating women (WHO 2011d). The evidence will complement the findings of other Cochrane Reviews exploring the effects of intermittent regimens among pregnant women (Peña‐Rosas 2015), the effects of intermittent iron supplementation in children under 12 years of age (De‐Regil 2011), and the effect of oral iron supplementation on preventing and treating anaemia among children in malaria‐endemic areas (Okabe 2011).
Objectives
To assess the effects of intermittent oral iron supplementation, alone or in combination with other nutrients, on anaemia and its associated impairments among menstruating women, compared with no intervention, a placebo, or daily supplementation.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐RCTs with randomisation at either the individual or cluster level. Quasi‐RCTs are trials that use systematic methods to allocate participants to treatment groups such as alternation or assignment based on date of birth or case record number (Reeves 2011).
Types of participants
Menstruating women; that is, women beyond menarche and prior to menopause who are not pregnant or lactating or have any condition that impedes the presence of menstrual periods, regardless of their baseline iron status or anaemia status, ethnicity, country of residence, or level of endurance.
We did not include studies targeting women with conditions affecting iron metabolism such as intestinal malabsorption conditions, ongoing excessive blood loss (including ongoing blood donations), inflammatory bowel disease, cancer, chronic congestive cardiac failure, chronic renal failure, chronic liver failure, or chronic infectious disease.
Types of interventions
Interventions involving an intermittent dosage of oral iron, either alone or with other vitamins and minerals, versus no intervention or placebo or the same supplements provided on a daily basis.
Oral iron supplementation refers to the delivery of iron compounds directly to the oral cavity, either as a tablet, capsule, dispersible tablet or liquid. For the purpose of this review, intermittent supplementation is defined as the provision of iron supplements one, two or three times a week on non‐consecutive days.
We performed the following comparisons:
intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo; and
intermittent iron supplementation versus daily iron supplementation.
We included studies that combined iron supplementation with other cointerventions, such as education or deworming, but only if the other cointerventions were the same in both the intervention and comparison groups.
We excluded studies examining tube feeding, parenteral nutrition or supplementary food‐based interventions such as mass fortification of staple or complementary foods, home fortification with micronutrient powders, lipid‐based supplements or foodlet (i.e. food‐like) tablets, or biofortification.
Types of outcome measures
Primary outcomes
Anaemia (haemoglobin concentration below a cut‐off defined by the trialists, adjusted by altitude and smoking, as appropriate)*
Haemoglobin (g/L)*
Iron deficiency (as defined by the trialists using indicators of iron status such as ferritin or transferrin)*
Ferritin (µg/L)*
Iron deficiency anaemia (as defined by the presence of anaemia plus iron deficiency, diagnosed with an indicator of iron status selected by the trialists)*
All‐cause morbidity (the most frequent event associated with the intervention, independent of the cause, as defined by the trialists)*
* Outcomes included in the 'Summary of findings' tables.
Secondary outcomes
Diarrhoea (number of women with at least three liquid stools in one day)
Respiratory infections (as defined by the trialists)
Any adverse side effects (e.g. nausea, vomiting, constipation, gastrointestinal discomfort, as defined by the trialists)
Work performance and economic productivity (as defined by the trialists)
School performance and cognitive function (for adolescents) (as defined by the trialists)
Depression (as defined by trialists)
Adherence (percentage of participants who consumed 70% or more of the prescribed dosage throughout the trial)
We considered the following outcomes in malaria settings only.
Malaria incidence (as defined by the trialists)
Malaria severity (as defined by the trialists)
All outcomes were evaluated at the end of the intervention or at the time point closest to the end.
Search methods for identification of studies
We analysed the indexing terms in the MEDLINE records for the included studies in the first version of this review using Yale MeSH Analyser (Grossetta Nardini 2017), and concluded that a number of indexing terms used in the previous strategy were redundant. We revised the search strategy for this update by removing these terms, which increased the precision of the search (Appendix 1). Search strategies for the previous version of this review are in Appendix 2. We limited our searches to studies published from 1980 onwards since the first trials on this intervention were published after this year. We did not apply any language restrictions. For those articles written in a language other than English, we commissioned their translation into English, to assess them for eligibility according to the prespecified selection criteria (Criteria for considering studies for this review).
Electronic searches
For this update, we searched the electronic databases and trials registers listed below up to February 2018, apart from Scientific Electronic Library Online (SciELO), IBECS and IMBIOMED, which we searched in March 2018.
Cochrane Central Register of Controlled Trials (CENTRAL; 2018, Issue 1) in the Cochrane Library, which contains the Developmental, Psychosocial and Learning Problems Specialised Register (searched 20 February 2018).
MEDLINE Ovid (1946 to February week 2 2018).
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid (searched 20 February 2018).
MEDLINE Epub Ahead of Print Ovid (searched 20 February 2018).
Embase Ovid (1974 to week 8 2018).
CINAHL Plus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1937 to 21 February 2018).
Science Citation Index Web of Science (SCI; 1970 to 20 February 2018).
Conference Proceedings Citation Index ‐ Science Web of Science (CPCI‐S; 1990 to 20 February 2018).
Cochrane Databse of Systematic Reviews (CDSR; 2017, Issue 12), in the Cochrane Library (searched 20 February 2018).
Database of Abstracts of Reviews of Effectiveness (DARE; 2015, Issue 2), in the Cochrane Library (final issue of DARE searched 13 January 2017).
POPLINE (www.popline.org; searched 22 February 2018).
SciELO (www.scielo.org/php/index.php?lang=es; searched 8 March 2018).
LILACS (Latin American and Caribbean Health Science Information database; lilacs.bvsalud.org/en; searched 20 February 2018).
IBECS (ibecs.isciii.es; searched 5 March 2018).
IMBIOMED (www.imbiomed.com.mx/1/1/catalogo.html; searched 10 March 2018).
ClinicalTrials.gov (clinicaltrials.gov; searched 22 February 2018).
WHO International Clinical Trials Registry Platform (ICTRP; apps.who.int/trialsearch; searched 22 February 2018).
See Differences between protocol and review for changes to the search methods used in this update.
Searching other resources
We contacted authors and known experts in the field for additional or unpublished data in order to identify any ongoing or unpublished studies. We also contacted the Departments of Nutrition for Health and Development, regional offices of the WHO, the nutrition section of the US Centers for Disease Control and Prevention (CDC), United Nations Children's Fund (UNICEF), the World Food Programme (WFP), the Micronutrient Initiative (MI), Helen Keller International (HKI), and the Sight and Life Foundation. In addition, we screened the reference lists of previously published reviews in order to identify other possible studies. One review author (LD‐R) searched these additional sources.
Data collection and analysis
We summarised the methods that we had planned to use, as per our published protocol (Fernández‐Gaxiola 2011b), but did not in Table 3. We may use these methods in future updates of this review.
1. Unused methods.
| Method | Approach | Reason for non‐use |
| Measures of treatment effects |
Continuous data We had planned to use the SMD to combine trials that measured the same outcome but used different methods. |
There was no need to use the SMD to combine trials as outcomes were measured with the same methods. |
| Sensitivity analysis | We had planned to conduct a sensitivity analysis to examine the effects of removing studies at high risk of bias (studies with unclear or high risk of bias for sequence generation and allocation concealment, and either high levels of attrition or no blinding) from the analyses and comparing the effect. | It was not possible to conduct this analysis because only two studies were considered at low risk of bias according to our predefined criteria (Hall 2002 (C) and Nguyen 2008). |
| We had planned to conduct a sensitivity analysis to explore the effect of missing data. | We were not able to conduct this analysis given that 13 out of 25 studies had attrition, and 22 out of 25 studies had unclear risk of reporting bias. |
SMD: standardised mean difference
Selection of studies
Using Covidence systematic review software (Covidence 2017), both reviewers (AF‐G; LD‐R) independently screened titles and abstracts of all records yielded by the searches against the selection criteria (Criteria for considering studies for this review), discarding those that were clearly irrelevant. Next, they both obtained the full‐text reports of all relevant or potentially relevant studies that seemed to meet the inclusion criteria, and assessed them for eligibility. There were a few disagreements, due to oversights of either one of the review authors, which they resolved through discussion.
We recorded the decisions of our selection process in a PRISMA diagram (Moher 2009).
Data extraction and management
Both review authors (AF‐G; LD‐R) independently extracted data from eligible studies using Covidence (Covidence 2017) and a form designed to collect other detailed data for this review. AF‐G entered the data into Review Manager 5 (RevMan 5) (Review Manager 2014), and LD‐R carried out checks for accuracy. We resolved any discrepancies through discussion. If the information regarding any of the studies was unclear, we attempted to contact the authors of the original reports, to ask them to provide further details.
We completed the data collection form electronically and recorded information (as set out below) on: study design; setting and participants (inclusion and exclusion criteria); study methods and assessment of risk of bias (see Assessment of risk of bias in included studies); intervention (for example, compound, dose, regimen, duration of intervention); outcomes (with details of how and when measured); and results.
-
Trial methods:
method of allocation and unit of randomisation;
masking of participants and outcomes; and
exclusion of participants after randomisation and proportion of losses at follow‐up.
-
Participants:
country of origin;
sample size;
age;
sex;
socioeconomic status; and
inclusion and exclusion criteria, as described under Criteria for considering studies for this review.
-
Intervention:
type;
dose;
frequency;
duration and length of time in follow‐up; and
cointervention.
-
Control:
control, placebo, or daily supplementation.
-
Outcomes:
primary and secondary outcomes, as outlined under Types of outcome measures.
Assessment of risk of bias in included studies
Each reviewer independently assessed the risk of bias in each included study using a simple contingency form that followed the domain‐based evaluation (sequence generation; allocation concealment; blinding; incomplete outcome data; selective reporting bias; other sources of bias), described in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b) and set out in Appendix 3. If there was insufficient information to assess the risk of bias, we rated the domain at 'unclear risk of bias', until further information was published or made available to us. If there was sufficient information, we categorised the domain as being either at 'low risk of bias' or 'high risk of bias' accordingly. We resolved any disagreements by discussion.
Overall risk of bias
We summarised the risk of bias at two levels: within studies (across domains) and across studies.
For the first, we made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). With reference to the domains listed above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We considered a study to be at low risk of bias overall if it was assessed at low risk of bias for both sequence generation and allocation concealment and either blinding or incomplete outcome data.
For the second, we assessed the quality of the evidence for each individual outcome using the GRADE approach (Balshem 2010; Schünemann 2011); see 'Summary of findings' tables (beneath Data synthesis) below.
We reported the results of our assessment in the 'Risk of bias in included studies' section, in the 'Risk of bias' tables (beneath the Characteristics of included studies tables), in Table 1 and Table 2, and graphically.
Measures of treatment effect
Dichotomous data
We presented dichotomous outcome data as average risk ratios (RRs) with 95% confidence intervals (CIs).
Continuous data
We presented continuous outcome data as mean differences (MD) with 95% CIs, measured at the end of the intervention. If studies did not provide this information but reported the mean change, we included these data as suggested in Chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
See also Table 1 and Fernández‐Gaxiola 2011b.
Unit of analysis issues
Cluster‐randomised studies
We included cluster‐randomised studies in the analyses with individually‐randomised studies; cluster‐randomised studies are labelled with a (C). We estimated effective sample sizes for each one of them in order to perform correct analyses according to Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
We obtained the intra‐cluster correlation coefficients (ICC) from Hall 2002 (C) (ICC = 0.0698; average cluster size (ACS) = 18.55; design effect (DE) = 2.22) and Roschnik 2003 (C) (ICC = 0.1123; ACS = 29.0, DE = 4.35), which we imputed to all cluster studies except Roschnik 2003 (C). We then calculated the ACS from the reports and estimated each study's effective sample size. Based on other reports (Okabe 2011), we assumed an average cluster size of 32 for classes, when the average cluster size or number of clusters and individuals were not clear (Agarwal 2003 (C); Soekarjo 2004 (C)). In summary, we used the following information to account for the effect clustering in the data: Jayatissa 1999 (C) (ACS = 25.6; DE = 2.71); Muro 1999 (C) (ACS = 43.1; DE = 3.94); Agarwal 2003 (C) (ACS = 32; DE = 3.16); Soekarjo 2004 (C) (ACS = 32; DE = 3.16); Mozaffari 2010 (C) (ACS = 25; DE = 2.68).
Additionally, we conducted sensitivity analyses to examine the potential effect of clustering on the CI of the summary estimates, by removing cluster‐RCTs from the analyses and comparing the effects (Sensitivity analysis).
Studies with more than two treatment groups
For studies with more than two intervention groups (multi‐arm studies), we included the directly relevant arms only. When we identified studies with various relevant arms, we combined the groups into a single pair‐wise comparison (Higgins 2011a), and included the disaggregated data in the corresponding subgroup category. When the control group was shared by two or more study arms, we divided the control group (events and total population) over the number of relevant subgroup categories to avoid double counting the participants. The details are described in the Characteristics of included studies tables.
Cross‐over trials
As specified in our protocol (Fernández‐Gaxiola 2011b), we did not include cross‐over trials.
Dealing with missing data
For included studies, we noted the levels of attrition and reported it in the 'Risk of bias' tables (beneath the Characteristics of included studies tables).
We carried out analyses, as far as possible, on an intention‐to‐treat (ITT) basis; that is, by attempting to include all participants randomised to each group in the analyses. If this was not possible, we performed an available case analysis, in which we analysed the data for each and every participant for whom the outcome was obtained.
Assessment of heterogeneity
We assessed methodological heterogeneity by examining the risk of bias of the studies, and clinical heterogeneity by examining the similarity between the types of participants, interventions and outcomes. For statistical heterogeneity, we examined the forest plots from meta‐analyses to look for heterogeneity among studies, and used the I2 statistic, Tau2 and Chi2 tests as heterogeneity statistics to quantify the level of heterogeneity among the studies included in each analysis. When we identified moderate or substantial heterogeneity (I2 greater than approximately 30%), we explored it by conducting prespecified subgroup analyses (see Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
When we suspected reporting bias (see 'Selective reporting bias' under Assessment of risk of bias in included studies), we attempted to contact the study authors to ask them to provide missing outcome data. We investigated reporting biases (such as possible publication bias) using funnel plots, assessing asymmetry visually.
Data synthesis
We carried out statistical analyses using RevMan 5 (Review Manager 2014). We used random‐effects meta‐analyses due to possible heterogeneity in the interventions, populations and methods used in different trials. We used Mantel‐Haenszel weighting for dichotomous outcomes and inverse variance for continuous outcomes, to adjust the effect measure according to the extent of its variation both between and within studies.
'Summary of findings' table
We presented the main findings of the review in 'Summary of findings' tables, which we prepared using GRADE profiler software (GRADEpro 2015). We created two 'Summary of findings' tables for both main comparisons: 1. Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo (Table 1); and 2. intermittent iron supplementation versus daily iron supplementation (Table 2). We included the following primary outcomes at the end of the intervention or at the time point closest to the end in these tables: anaemia (haemoglobin concentration below a cut‐off defined by trialists); haemoglobin (g/L); iron deficiency (as defined by trialists by using indicators of iron status such as ferritin or transferrin); ferritin (µg/L); iron deficiency anaemia (defined by the presence of anaemia plus iron deficiency diagnosed with an indicator of iron status selected by trialists); all‐cause morbidity (the most frequent event associated with the intervention independent of the cause, as defined by the trialists) (see Primary outcomes). We also listed estimates of relative effects along with the number of participants and studies contributing data for each outcome.
Both review authors independently assessed the quality of the evidence for each individual outcome using the GRADE approach (Balshem 2010; Schünemann 2011), which involves consideration of within‐study risk of bias (methodological quality), directness of evidence, heterogeneity, precision of effect estimates, and risk of publication bias. The results were expressed as one of four levels of quality (high, moderate, low, or very low).
Subgroup analysis and investigation of heterogeneity
When data were available and it was appropriate, we carried out the following subgroup analyses on three primary outcomes (anaemia, haemoglobin, and ferritin concentrations), to look for possible differences between studies (note, we pragmatically decided not to conduct subgroup analyses on those outcomes with three trials or fewer).
Composition: iron alone; iron + folic acid; iron + multiple micronutrients
Anaemia status at baseline (haemoglobin < 120 g/L, adjusted by altitude and smoking, as appropriate): anaemic; non‐anaemic; mixed/unknown
Iron status at baseline (as defined by the trialists): iron deficient; not iron deficient; mixed/unknown
Dose of elemental iron per week in the intermittent group: 60 mg of iron or less; more than 60 mg of iron
Duration of supplementation: three months or less; more than three months
Malaria status of the area at the time of the trial (as reported by trialists): yes; no/unknown
We examined differences between subgroups by visual inspection of the subgroups’ CI, with non‐overlapping CI suggesting a statistically significant difference in treatment effect between subgroups. We also used the Borenstein 2008 approach to formally investigate differences between two or more subgroup categories.
Sensitivity analysis
We conducted sensitivity analyses ad hoc to examine the potential effect of clustering on the CI of the summary estimates, by removing cluster‐RCTs from the analyses and comparing the effects (see Appendix 4). We conducted an additional sensitivity analysis ad hoc with two studies (Hall 2002 (C); Roschnik 2003 (C)), in which approximately half of the participants were young females (< 12 years of age) to see their effect on the analyses (see Effects of interventions).
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies.
Results of the search
The search strategy for the first publication of this review identified 9484 records for possible inclusion, 2706 of which were duplicates. We assessed 52 full‐text reports and: included 21 studies (from 25 reports); excluded 20 studies (from 24 reports); identified two studies (from three reports) as awaiting classification; and identified two ongoing studies (see Fernández‐Gaxiola 2011a).
The updated search identified 7532 records through database searches and 296 additional records through searching other sources. Having removed duplicates, we screened 5098 records on the basis of title and abstract, and removed 5074 clearly ineligible records. We retrieved 24 full‐text reports, which we assessed against the inclusion criteria (Criteria for considering studies for this review). We excluded 18 reports (related to: eight newly excluded studies (12 reports), two previously excluded studies (two reports), and one previously ongoing study (four reports)) from the review, and included four new studies (from four reports). We also identified two studies (from three reports) as awaiting classification (of which, one study (two reports) was previously ongoing), and one new ongoing study (from one report).
Altogether this review excluded 28 studies (from 38 reports), included 25 studies (from 29 reports), has four studies (from six reports) awaiting classification, and one ongoing study (from one report).
Figure 1 depicts the process for assessing and selecting the studies.
1.

Study flow diagram.
Included studies
We included 25 studies, involving 10,996 participants, all of which met the pre‐established inclusion criteria (Criteria for considering studies for this review). All studies were published between 1997 and 2018. Most studies focused on the prevention of anaemia and iron deficiency by improving iron status indicators (Primary outcomes); few studies reported data on the prespecified secondary outcomes (Secondary outcomes). See the Characteristics of included studies tables for more detail.
Settings
Studies were conducted in 15 different countries, most of them low‐ and middle‐income countries: Bangladesh, Brazil, France, Guatemala, India, Indonesia, Iran, Kenya, Malawi, Mali, Mexico, Nepal, Pakistan, Peru, Sri Lanka and Tanzania. One study was conducted in Europe (Riuvard 2006), four in Latin America (Dos Santos 1999; Zavaleta 2000; Gonzalez‐Rosendo 2002; Nguyen 2008), five in Africa (Muro 1999 (C); Beasley 2000; Hall 2002 (C); Roschnik 2003 (C); Leenstra 2009), and 15 in Asia (Angeles‐Agdeppa 1997; Jayatissa 1999 (C); Kianfar 2000; Ahmed 2001; Gilgen 2001; Februhartanty 2002; Shah 2002; Agarwal 2003 (C); Shobha 2003; Soekarjo 2004 (C); Mozaffari 2010 (C); Joshi 2013; Gupta 2014; Rezaeian 2014; Jalambo 2018).
Most studies were conducted in school settings; however, five studies implemented the intervention in rural and urban communities, health centres, and villages (Dos Santos 1999; Beasley 2000; Gilgen 2001; Nguyen 2008; Joshi 2013), and one study was conducted among garment factory workers (Ahmed 2001). Five studies explicitly mentioned that they were conducted in areas with some degree of malaria endemicity (Muro 1999 (C); Beasley 2000; Februhartanty 2002; Hall 2002 (C); Leenstra 2009).
Participants
Participants' ages ranged from six (Hall 2002 (C) to 49 (Nguyen 2008) years of age. While we did not include studies specifically recruiting premenarchal girls ‐ as these are the subject of a separate review (De‐Regil 2011) ‐ two studies recruited young females and separate data were not available for postmenarchal girls only (Hall 2002 (C); Roschnik 2003 (C)). Based on the age range reported in these studies, we assumed that at least half of the participants fulfilled our inclusion criteria and thus we decided to retain them in the review. If the disaggregated data are made available to us, we will include them in future updates of the review.
Most studies involved a mix of anaemic and non‐anaemic women, with the exception of six studies that included women with mild‐to‐moderate anaemia (Dos Santos 1999; Ahmed 2001; Shobha 2003; Leenstra 2009; Joshi 2013; Gupta 2014), one of which, Shobha 2003, included only severely anaemic women (i.e. women with haemoglobin concentrations ≤ 8 g/dL). The remaining studies excluded these severely anaemic women and gave them treatment or referred them to health care (or both). Only two studies specifically included iron‐deficient women (i.e. women with serum ferritin concentrations ≤ 15 mcg/L) (Riuvard 2006; Jalambo 2018).
Samples size varied among included studies, ranging from 24 in Riuvard 2006 to 2461 in Soekarjo 2004 (C); however, for cluster‐randomised studies, the analyses only include the estimated effective sample size, after adjusting the data to account for the clustering effect.
Interventions (intermittent regimens, supplement composition and iron dose)
Intermittent regimens
Most studies provided intermittent iron supplementation once a week and compared it to control (i.e. no intervention), placebo, daily iron supplementation or other nutrients or dosages also given intermittently once a week. Five studies provided supplements twice a week compared with: once weekly supplementation (Kianfar 2000; Gupta 2014); daily supplementation (Shobha 2003; Riuvard 2006); or control (Rezaeian 2014). One study provided iron supplements three days a week and compared this with daily supplementation and placebo (Zavaleta 2000).
Duration of the intervention
Duration of the intervention varied greatly among studies. In 13 studies, women were supplemented for three months or less (Angeles‐Agdeppa 1997; Dos Santos 1999; Jayatissa 1999 (C); Muro 1999 (C); Kianfar 2000; Ahmed 2001; Hall 2002 (C); Shobha 2003; Soekarjo 2004 (C); Riuvard 2006; Nguyen 2008; Joshi 2013; Jalambo 2018). The duration of the intervention was: three and a half months in three studies (Shah 2002; Agarwal 2003 (C); Roschnik 2003 (C)); four months in six studies (Beasley 2000; Zavaleta 2000; Februhartanty 2002; Gonzalez‐Rosendo 2002; Mozaffari 2010 (C); Rezaeian 2014); five months in one study (Leenstra 2009); and six months in one study (Gilgen 2001). The maximum duration of supplementation was one year (Gupta 2014).
Supplements composition
In 11 studies, women were supplemented with iron only (Dos Santos 1999; Beasley 2000; Kianfar 2000; Zavaleta 2000; Gonzalez‐Rosendo 2002; Shobha 2003; Riuvard 2006; Leenstra 2009; Mozaffari 2010 (C); Rezaeian 2014; Jalambo 2018). In the remaining studies, women received iron plus folic acid supplements in 10 studies (Jayatissa 1999 (C); Muro 1999 (C); Gilgen 2001; Februhartanty 2002; Hall 2002 (C); Shah 2002; Agarwal 2003 (C); Roschnik 2003 (C); Gupta 2014; Joshi 2013), iron plus multiple micronutrients supplements in two studies (Angeles‐Agdeppa 1997; Nguyen 2008), and iron plus folic acid and iron plus multiple nutrients in one (Ahmed 2001) and iron plus folic acid or vitamin A or iron plus folic acid plus vitamin A in another (Soekarjo 2004 (C)).
Most studies supplemented iron with ferrous sulphate, with the exception of three studies that used ferrous fumarate (Gilgen 2001; Joshi 2013; Jalambo 2018) and one study that used ferrous chloride (Riuvard 2006). Six studies did not specify the form of iron used for supplementing women (Angeles‐Agdeppa 1997; Muro 1999 (C); Agarwal 2003 (C); Shobha 2003; Nguyen 2008; Mozaffari 2010 (C)). All studies used supplements as tablets or caplets.
Iron dose
The 25 studies tested several supplemental doses of iron in the intermittent group but none of the studies exceeded 120 mg of elemental iron per week. See below.
10 mg of elemental iron (one study: Rezaeian 2014)
30 mg of elemental iron (one study: Mozaffari 2010 (C))
50 mg of elemental iron (two studies: Kianfar 2000; Riuvard 2006)
60 mg of elemental iron (seven studies: Dos Santos 1999; Jayatissa 1999 (C); Zavaleta 2000; Februhartanty 2002; Gonzalez‐Rosendo 2002; Shobha 2003; Soekarjo 2004 (C))
65 mg of elemental iron (five studies: Muro 1999 (C); Hall 2002 (C); Roschnik 2003 (C); Jalambo 2018)
66 mg of elemental iron (one study: Gilgen 2001)
70 mg of elemental iron (one study: Shah 2002)
100 mg of elemental iron (three studies: Agarwal 2003 (C); Joshi 2013; Gupta 2014)
120 mg of elemental iron (three studies: Beasley 2000; Ahmed 2001; Leenstra 2009)
Angeles‐Agdeppa 1997 and Nguyen 2008 examined the effects of two different doses of elemental iron: 60 mg and 120 mg of elemental iron per week.
Funding sources
Five studies were partially funded (Soekarjo 2004 (C)) or fully funded by international organisations (Jayatissa 1999 (C); Gilgen 2001; Hall 2002 (C); Agarwal 2003 (C)). Four studies were partially funded by government organisations; two by the Department for International Development in the UK (Beasley 2000; Ahmed 2001) and two by the Ministry of Health within the country (Kianfar 2000; Soekarjo 2004 (C)). Four studies were funded by universities and institutes (Kianfar 2000; Shah 2002; Mozaffari 2010 (C); Rezaeian 2014), and four were partially funded by a pharmaceutical company, as they provided the supplements used (Angeles‐Agdeppa 1997; Ahmed 2001; Riuvard 2006; Leenstra 2009). Two studies were partially funded by a technical collaboration (an agreement whereby a developed country agrees to provide technical assistance to a developing country) (Angeles‐Agdeppa 1997; Februhartanty 2002) and two were partially funded by a foundation (Beasley 2000; Leenstra 2009). Only two studies declared no funding source was used to implement their study (Shobha 2003; Jalambo 2018). Seven studies did not provide a funding source (Dos Santos 1999; Muro 1999 (C); Zavaleta 2000; Gonzalez‐Rosendo 2002; Roschnik 2003 (C); Nguyen 2008; Joshi 2013).
Excluded studies
We excluded 28 studies: 13 studies were not RCTs (Cook 1995; Jackson 2003; Siddiqui 2003; Berger 2005; Crape 2005; Horjus 2005; López de Romaña 2006; Deshmukh 2008; Vir 2008; Casey 2009; Pasricha 2009; Joseph 2013; Shah 2016); two were reviews (Beaton 1999; Dwividi 2006); one was a commentary on another study (Perrin 2002); nine compared interventions outside the scope of this review (Bruner 1996; Kätelhut 1996; Tee 1999; Viteri 1999; Ahmed 2005; Ahmed 2010; Ahmed 2012; Moretti 2015; Bansal 2016); two used a different population (Ramakrishnan 2012; Sen 2012); and one excluded postmenarchal girls because the anthelmintic drug given along with the iron supplementation was not safe in cases of pregnancy (Taylor 2001).
See the Characteristics of excluded studies tables for a detailed description of the studies and the reasons for their exclusion.
Studies awaiting classification
Four studies are awaiting classification (Olsen 2000; Sharma 2000; Brabin 2014; Malhotra 2013); two of these four RCTs are from Africa (Olsen 2000; Brabin 2014) and the other two are from India (Sharma 2000; Malhotra 2013). Olsen 2000 compared the efficacy of twice‐weekly iron supplementation versus placebo. Brabin 2014 compared the efficacy of once‐weekly iron‐folate supplementation versus folate (control). Sharma 2000 compared the efficacy of once‐weekly versus daily iron and folic acid supplementation plus the effect of added ascorbic acid on the efficacy of iron‐folate supplementation. Malhotra 2013 compared the efficacy of twice‐weekly iron‐folate supplementation versus control versus twice‐weekly iron‐folate supplementation plus the effect of nutrition education versus nutrition education only on haematological status.
The dosages of elemental iron used in the studies were: 60 mg in Olsen 2000 and Malhotra 2013, 100 mg in Sharma 2000, and unclear for Brabin 2014.
We were unable to extract data for our outcomes from Olsen 2000 as the data were not disaggregated by sex, or from Sharma 2000 as the data were categorised by percentages. Malhotra 2013 was only available as an abstract and did not provide data for our comparisons. The Brabin 2014 report included only the qualitative part of the RCT and was missing the quantitative part for our meta‐analysis. In addition, the participants in Brabin 2014 were young women enrolled prior to their first pregnancy, and more information is needed to clarify the study's eligibility for inclusion in the review.
Ongoing studies
We found one ongoing study from India (CTRI/2017/11/010453). This study is comparing the efficacy of once‐a‐week versus daily iron supplementation at controlling anaemia in adolescent school girls aged 12 to 16 years with anaemia. The trial will provide 60 mg of elemental iron for three months. Recruitment has been completed and some results have been already published. See Characteristics of ongoing studies table.
Risk of bias in included studies
Overall, many included studies did not describe study methods completely, which made it difficult to assess risk of bias. We contacted some study authors for support and are still awaiting a reply at the time of publication of this review. With the exception of two studies (Hall 2002 (C); Nguyen 2008), we considered all of the studies included in this update to be at high risk of bias (or of low quality).
See the 'Risk of bias' tables (under the Characteristics of included studies tables) for an assessment of the risk of bias of each included trial, and Figure 2 and Figure 3 for an overall graphical summary of the risk of bias of all included trials. In the 'Summary of findings' tables, we presented the overall quality of the evidence for each primary outcome, by comparison (Table 1; Table 2).
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation
Nine studies adequately randomised the participants to the intervention group (Dos Santos 1999; Gilgen 2001; Gonzalez‐Rosendo 2002; Hall 2002 (C); Riuvard 2006; Nguyen 2008; Joshi 2013; Gupta 2014; Rezaeian 2014). Of these nine studies, four used a random number generator (Gilgen 2001; Gonzalez‐Rosendo 2002; Hall 2002 (C); Nguyen 2008), one used drawing of lots (Dos Santos 1999), one used a randomisation table (Riuvard 2006), one used a generated block (Joshi 2013), one used a lottery method (Gupta 2014), and another used a simple draw (Rezaeian 2014).
Sixteen studies did not state the method used to generate the random sequence clearly, so we rated these at unclear risk of bias (Angeles‐Agdeppa 1997; Jayatissa 1999 (C); Muro 1999 (C); Beasley 2000; Kianfar 2000; Zavaleta 2000; Ahmed 2001; Februhartanty 2002; Shah 2002; Agarwal 2003 (C); Roschnik 2003 (C); Shobha 2003; Soekarjo 2004 (C); Leenstra 2009; Mozaffari 2010 (C); Jalambo 2018).
Allocation concealment
Ten studies reported adequate allocation concealment (Jayatissa 1999 (C); Zavaleta 2000; Ahmed 2001; Hall 2002 (C); Agarwal 2003 (C); Roschnik 2003 (C); Soekarjo 2004 (C); Nguyen 2008; Leenstra 2009; Mozaffari 2010 (C)). Of these 10 studies, three kept the code secure until all data were entered into the computer (Ahmed 2001) or until after study completion (Nguyen 2008; Leenstra 2009), and seven were randomised at cluster level and we considered that the risk of selection bias at the individual level was unlikely (Jayatissa 1999 (C); Zavaleta 2000; Hall 2002 (C); Agarwal 2003 (C); Roschnik 2003 (C); Soekarjo 2004 (C); Mozaffari 2010 (C)).
In 15 studies, the method used to conceal the allocation was unclear or not mentioned (Angeles‐Agdeppa 1997; Dos Santos 1999; Muro 1999 (C); Beasley 2000; Kianfar 2000; Gilgen 2001; Februhartanty 2002; Gonzalez‐Rosendo 2002; Shah 2002; Shobha 2003; Riuvard 2006; Joshi 2013; Gupta 2014; Rezaeian 2014; Jalambo 2018).
Blinding
We rated 13 studies at low risk of performance and detection bias (Angeles‐Agdeppa 1997; Dos Santos 1999; Jayatissa 1999 (C); Beasley 2000; Kianfar 2000; Zavaleta 2000; Ahmed 2001; Gilgen 2001; Februhartanty 2002; Roschnik 2003 (C); Leenstra 2009; Nguyen 2008; Rezaeian 2014). Of these 13 studies, nine were described as being single or double blinded (Angeles‐Agdeppa 1997; Dos Santos 1999; Jayatissa 1999 (C); Beasley 2000; Zavaleta 2000; Ahmed 2001; Gilgen 2001; Februhartanty 2002; Nguyen 2008), and of these nine, five specified that the placebos were of identical appearance (Angeles‐Agdeppa 1997; Jayatissa 1999 (C); Zavaleta 2000; Nguyen 2008; Gilgen 2001). Four studies did not mention or describe blinding in the study, so we rated them at unclear risk of performance and detection bias (Hall 2002 (C); Agarwal 2003 (C); Joshi 2013; Jalambo 2018). We rated eight studies at high risk of performance and detection bias because participants, personnel and outcome assessors seemed to be aware of the treatments (Muro 1999 (C); Gonzalez‐Rosendo 2002; Shah 2002; Shobha 2003; Soekarjo 2004 (C); Riuvard 2006; Mozaffari 2010 (C); Gupta 2014).
Incomplete outcome data
Loss to follow‐up varied greatly among studies, from 1% in Agarwal 2003 (C) to 41% in Roschnik 2003 (C). We rated six studies, which lost more than 20% of randomised participants or had imbalanced losses between study groups (or both), at high risk of attrition bias (Angeles‐Agdeppa 1997; Dos Santos 1999; Beasley 2000; Ahmed 2001; Roschnik 2003 (C); Nguyen 2008). We judged a further seven studies, which did not mention attrition making it difficult to judge whether the lack of data were due to no losses to follow‐up or to incomplete reporting, at unclear risk of attrition bias (Gilgen 2001; Gonzalez‐Rosendo 2002; Shobha 2003; Joshi 2013; Gupta 2014; Rezaeian 2014; Jalambo 2018). We considered the remaining 12 studies to be at low risk of attrition bias (Jayatissa 1999 (C); Muro 1999 (C); Kianfar 2000; Zavaleta 2000; Februhartanty 2002; Hall 2002 (C); Shah 2002; Agarwal 2003 (C); Soekarjo 2004 (C); Riuvard 2006; Leenstra 2009; Mozaffari 2010 (C)).
Selective reporting
Although it was difficult to assess reporting bias, because we did not have access to study protocols, we did not find a clear indication of reporting or publication bias by assessing funnel plot asymmetry visually.
Of the 25 included studies, we rated 22 at unclear risk of reporting bias. We rated one study at low risk of reporting bias because there was apparently no selective reporting (Jalambo 2018). We considered two studies to be at high risk of reporting bias (Agarwal 2003 (C); Joshi 2013). In Agarwal 2003 (C), data for plasma ferritin concentrations were estimated only in some girls and it was unclear how the selection was made. In Joshi 2013, there was missing information on compliance at the individual level that was recorded through home visits and postintervention interviews.
Other potential sources of bias
We rated 14 studies, which appeared to be free of other sources of bias, at low risk of other bias (Dos Santos 1999; Jayatissa 1999 (C); Muro 1999 (C); Kianfar 2000; Zavaleta 2000; Gilgen 2001; Agarwal 2003 (C); Soekarjo 2004 (C); Riuvard 2006; Nguyen 2008; Mozaffari 2010 (C); Joshi 2013; Rezaeian 2014; Jalambo 2018).
We rated eight studies at unclear risk of other sources of bias (Angeles‐Agdeppa 1997; Beasley 2000; Ahmed 2001; Gonzalez‐Rosendo 2002; Hall 2002 (C); Roschnik 2003 (C); Shobha 2003; Leenstra 2009). In Angeles‐Agdeppa 1997, the intervention was unsupervised during the four‐week period, as the supplements were provided on a take‐home basis. In Beasley 2000, the control group was given vitamin B12, which could have potentially impacted anaemia status. Ahmed 2001 had some variability in the administration of the supplements depending on the factory (i.e. supplements were given before versus after lunch, with an empty stomach versus having eaten little). In Roschnik 2003 (C), the results were affected by a famine in Malawi at the time of the trial. In Angeles‐Agdeppa 1997, Gonzalez‐Rosendo 2002, Hall 2002 (C) and Shobha 2003, the distribution of anaemia was not shown. In Leenstra 2009, most of the results for the four randomised groups were presented in graphs that were difficult to interpret (and consequently have not been included in our Data and analyses tables), and data on several outcomes were described as non‐significant but were not shown (side effects, including vomiting and diarrhoea).
We rated three studies at high risk of other sources of bias (Februhartanty 2002; Shah 2002; Gupta 2014). In Februhartanty 2002, there was a higher prevalence of anaemia in the group that received supplements weekly. In Shah 2002, the daily group were not explicitly supervised while those in the weekly group were supervised. Finally, Gupta 2014 had missing information on side effects that were recorded by the intervention group.
Effects of interventions
The summary of results is organised by comparisons. In the analyses, we have provided overall totals along with subtotals for subgroups and the statistics for subgroup differences. See the Data and analyses section for detailed results on primary and secondary outcomes.
Intermittent supplementation of iron (alone or plus any other micronutrients) versus no supplementation or placebo
Eighteen studies involving 8988 women examined intermittent iron supplementation versus no supplementation or placebo (Angeles‐Agdeppa 1997; Muro 1999 (C); Jayatissa 1999 (C); Beasley 2000; Kianfar 2000; Zavaleta 2000; Ahmed 2001; Gilgen 2001; Februhartanty 2002; Hall 2002 (C); Shah 2002; Agarwal 2003 (C); Roschnik 2003 (C); Soekarjo 2004 (C); Leenstra 2009; Mozaffari 2010 (C); Rezaeian 2014; Jalambo 2018). Nine of these studies met the prespecified criteria mentioned above (see Assessment of risk of bias in included studies) for being at lower risk of bias.
Primary outcomes
Anaemia
Eleven studies reported data on this outcome (Angeles‐Agdeppa 1997; Jayatissa 1999 (C); Muro 1999 (C); Zavaleta 2000; Ahmed 2001; Hall 2002 (C); Shah 2002; Agarwal 2003 (C); Roschnik 2003 (C); Soekarjo 2004 (C); Mozaffari 2010 (C)). We pooled these studies in a meta‐analysis and found evidence that women receiving intermittent supplementation were less likely to have anaemia at the end of the intervention than those women who received no intervention or placebo (RR 0.65, 95% CI 0.49 to 0.87; 3135 participants; Analysis 1.1). However, treatment effect sizes varied between studies (T2= 0.16; Chi2= 58.75 (P < 0.001); I2= 83%).
1.1. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 1: Anaemia (All)
We conducted a subgroup analysis and found no evidence to suggest that the composition of the supplement (iron only, iron plus folic acid, or iron plus any other micronutrients) affected anaemia (Analysis 1.2). However, we did find evidence that mixed/unknown anaemic women in the intervention group were less likely to have anaemia than anaemic women in the intervention group (RR 0.71, 95% CI 0.55 to 0.93; 2913 participants; Analysis 1.3; Test for subgroup differences: Chi2 = 9.38 (P = 0.002); l2= 89.3%). All studies reported iron status as mixed/unknown at baseline so we were not able to conduct subgroup analysis (Analysis 1.4). In further subgroup analyses, we found no evidence to suggest that dose of elemental iron per week in the intervention group (Analysis 1.5), duration of supplementation (Analysis 1.6), or malaria endemicity at the time when the study was conducted (Analysis 1.7) affected anaemia. There was a high level of heterogeneity between the studies in these analyses (between 79% and 84%). We rated the quality of this evidence as low.
1.2. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 2: Anaemia (by supplement composition)
1.3. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 3: Anaemia (by anaemia status at baseline)
1.4. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 4: Anaemia (by iron status at baseline): Mixed/Unknown
1.5. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 5: Anaemia (dose of elemental iron per week in the intermittent group)
1.6. Analysis.
Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 6: Anaemia (by duration of supplementation)
1.7. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 7: Anaemia (by malaria endemicity)
Haemoglobin
Fifteen studies examined haemoglobin concentrations (Angeles‐Agdeppa 1997; Jayatissa 1999 (C); Beasley 2000; Kianfar 2000; Ahmed 2001; Gilgen 2001; Februhartanty 2002; Hall 2002 (C); Roschnik 2003 (C); Agarwal 2003 (C); Soekarjo 2004 (C); Leenstra 2009; Mozaffari 2010 (C); Rezaeian 2014; Jalambo 2018). We pooled these studies in a meta‐analysis and found evidence that women receiving iron supplements intermittently had 5.19 more grams of haemoglobin per litre (95% CI 3.07 to 7.32; 2886 participants; Analysis 1.8), than those who received no intervention or a placebo. Again, treatment effect sizes varied between studies (T2 = 14.01; Chi2 = 87.02 (P < 0.001); I2 = 84%).
1.8. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 8: Haemoglobin in g/L (All)
We conducted subgroup analyses and found no evidence to suggest that the composition of the supplement (iron only, iron plus folic acid, or iron plus any other micronutrients) (Analysis 1.9), or anaemia status at baseline (anaemic status before the supplementation) (Analysis 1.10) affected haemoglobin. Not enough studies contributed data for the analysis on women's iron status at baseline (iron deficiency before the supplementation) so that most women had a mixed/unknown iron status (Analysis 1.11). In further subgroup analyses, we found no evidence to suggest that dose of elemental iron per week in the intervention group (Analysis 1.12), duration of supplementation (Analysis 1.13), or malaria endemicity at the time when the study was conducted (Analysis 1.14) affected haemoglobin. There was a high level of heterogeneity between the studies in these analyses (around 85%). We rated the quality of this evidence as moderate.
1.9. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 9: Haemoglobin in g/L (by supplement composition)
1.10. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 10: Haemoglobin in g/L (by anaemia status at baseline)
1.11. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 11: Haemoglobin in g/L (by iron status at baseline)
1.12. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 12: Haemoglobin in g/L (by dose of elemental iron per week in the intermittent group)
1.13. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 13: Haemoglobin in g/L (by duration of supplementation)
1.14. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 14: Haemoglobin in g/L (by malaria endemicity)
Iron deficiency
Three studies reported data on iron deficiency (Angeles‐Agdeppa 1997; Ahmed 2001; Mozaffari 2010 (C)). We pooled these studies in a meta‐analysis and found no evidence that iron deficiency differed between the groups (RR 0.50, 95% CI 0.24 to 1.04; 624 participants; Analysis 1.15). The heterogeneity was high but the directions of the results were consistent (T2 = 0.36, Chi2 = 17.52 (P < 0.001); I2 = 89%) . We rated the quality of this evidence as low.
1.15. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 15: Iron deficiency (All)
Ferritin
Seven studies examined ferritin concentrations (Angeles‐Agdeppa 1997; Beasley 2000; Ahmed 2001; Gilgen 2001; Februhartanty 2002; Mozaffari 2010 (C); Jalambo 2018). We pooled these studies in a meta‐analysis and found evidence in favour of the intervention group (MD 7.46 μg/L, 95% CI 5.02 to 9.90; 1067 participants, Analysis 1.16). The heterogeneity was moderate (T2 = 4.10; Chi2 = 10.94 (P = 0.09); I2 = 45%). We rated the quality of this evidence as low.
1.16. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 16: Ferritin in µg/L (All)
We conducted subgroup analyses and found no evidence to suggest that the composition of the supplement (iron only, iron plus folic acid, or iron plus any other micronutrients) (Analysis 1.17) or anaemic status at baseline (Analysis 1.18) affected ferritin. Not enough studies contributed data for the analysis on women's iron status at baseline (iron deficiency before the supplementation) so that most women had a mixed/unknown iron status (Analysis 1.19). In further subgroup analyses, we found no evidence to suggest that dose of elemental iron per week in the intervention group (Analysis 1.20), duration of supplementation (Analysis 1.21), or malaria endemicity at the time when the study was conducted (Analysis 1.22) affected ferritin.
1.17. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 17: Ferritin in µg/L (by supplement composition)
1.18. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 18: Ferritin in µg/L (by anaemia status at baseline)
1.19. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 19: Ferritin in µg/L (by iron status at baseline)
1.20. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 20: Ferritin in µg/L (by dose of elemental iron per week in the intermittent group)
1.21. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 21: Ferritin in µg/L (by duration of supplementation)
1.22. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 22: Ferritin in µg/L (by malaria endemicity)
Iron deficiency anaemia
A single study reported data on this outcome (Mozaffari 2010 (C)). It found no difference in iron deficiency anaemia between those women who received iron supplements intermittently and those women who did not receive iron (RR 0.07, 95% CI 0.00 to 1.16; 97 participants; see the illustrative forest plot in Analysis 1.23). We rated the quality of this evidence as low.
1.23. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 23: Iron deficiency anaemia (All)
All‐cause morbidity
A single study reported data on this outcome (Beasley 2000). It found no difference in all‐cause morbidity between those women who received iron supplements intermittently and those who women did not receive iron (RR 1.12, 95% 0.82 to 1.52; 119 participants; see the illustrative forest plot in Analysis 1.24). We rated the quality of this evidence as low.
1.24. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 24: All cause morbidity (All)
Secondary outcomes
Diarrhoea
A single study reported data on diarrhoea (Angeles‐Agdeppa 1997). It found no evidence that diarrhoea differed between the groups (RR 0.28, 95% CI 0.05 to 1.49; 209 participants; see the illustrative forest plot in Analysis 1.25).
1.25. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 25: Diarrhoea
Any adverse side effects
Three studies examined any adverse side effects (Angeles‐Agdeppa 1997; Gilgen 2001; Leenstra 2009). We pooled these studies in a meta‐analysis and found no evidence that adverse side effects differed between the groups (RR 1.98, 95% CI 0.31 to 12.72; 630 participants; Analysis 1.26).
1.26. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 26: Any adverse side effects
Adherence
Two studies examined adherence (Zavaleta 2000; Ahmed 2001). We pooled these studies in a meta‐analysis and found no evidence that women receiving iron supplements intermittently adhered to the intervention better than those women who did not receive iron (RR 0.99, 95% CI 0.96 to 1.02; 417 participants; Analysis 1.27).
1.27. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 27: Adherence
Malaria outcomes
Two studies reported data on malaria outcomes (Beasley 2000; Leenstra 2009). We pooled these studies in a meta‐analysis and found no evidence that the prevalence (Analysis 1.28) and incidence Analysis 1.29) of parasitaemia, prevalence of high‐density parasitaemia (Analysis 1.30), and clinical malaria (Analysis 1.31) differed between those women who received iron supplements intermittently and those women who did not receive iron.
1.28. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 28: Prevalence of malaria parasitaemia
1.29. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 29: Any malaria parasitaemia (Incidence rate; per 1000 person months)
1.30. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 30: High density malaria parasitaemia (parasites 200/wbc)
1.31. Analysis.

Comparison 1: Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo, Outcome 31: Clinical malaria
No studies reported on our other prespecified secondary outcomes: respiratory infections; school performance and cognitive function; or depression.
Sensitivity analyses
We conducted sensitivity analyses by reanalysing the data for anaemia, haemoglobin, iron deficiency and ferritin with cluster‐RCTs excluded (Jayatissa 1999 (C); Muro 1999 (C); Hall 2002 (C); Agarwal 2003 (C); Roschnik 2003 (C); Soekarjo 2004 (C); Mozaffari 2010 (C), and found no significant differences in the results. See Appendix 4.
In two studies (Hall 2002 (C); Roschnik 2003 (C)), approximately half of the participants (276 participants and 376 participants, respectively) were young females (< 12 years of age). We conducted a sensitivity analysis ad hoc and found that excluding these studies changed the estimate for anaemia from RR 0.65 (95% CI 0.49 to 0.87) to RR 0.58 (95% CI 0.40 to 0.86; results not shown), and haemoglobin from MD 5.19 g/L (95% CI 3.07 to 7.32) to MD 5.67 g/L (95% CI 3.37 to 7.97; results not shown). As the interpretation of our results did not change, we decided to retain these trials in our analyses and thus minimise the risk of publication bias.
Intermittent iron supplementation versus daily iron supplementation
We included 13 studies involving 6213 women in this comparison (Angeles‐Agdeppa 1997; Dos Santos 1999; Jayatissa 1999 (C); Kianfar 2000; Zavaleta 2000; Gonzalez‐Rosendo 2002; Shah 2002; Agarwal 2003 (C); Shobha 2003; Riuvard 2006; Nguyen 2008; Joshi 2013; Gupta 2014). We considered only two of these studies to be at higher risk of bias overall (Shah 2002 and Gupta 2014) and six of these to be at lower risk of bias overall (Jayatissa 1999 (C); Kianfar 2000; Zavaleta 2000; Gonzalez‐Rosendo 2002; Soekarjo 2004 (C); Nguyen 2008.
Primary outcomes
Anaemia
Eight studies reported data on this outcome (Angeles‐Agdeppa 1997; Dos Santos 1999; Jayatissa 1999 (C); Zavaleta 2000; Gonzalez‐Rosendo 2002; Shah 2002; Agarwal 2003 (C); Joshi 2013). We pooled these studies in a meta‐analysis and found evidence that women receiving iron supplements daily were as likely to have reduced anaemia at the end of the intervention as those women receiving iron supplements intermittently (RR 1.09, 95% CI 0.93 to 1.29; 1749 participants; Analysis 2.1). The heterogeneity was low (T2 = 0.01; Chi2 = 7.93 (P = 0.34); I2= 12%). We rated the quality of this evidence as moderate.
2.1. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 1: Anaemia (All)
We conducted subgroup analyses and found no evidence to suggest that the composition of the supplement affected anaemia (Analysis 2.2). We found inconclusive results that anaemia status at baseline (anaemia status before the supplementation) affected anaemia (Analysis 2.3), and no studies reported data for the analysis exploring the effects of iron status at baseline (Analysis 2.4). Almost an even number of studies provided 60 mg of elemental iron or less per week (four studies) or more than 60 mg of elemental iron per week (five studies), and we found no evidence to suggest that the dose in the intervention group affected anaemia (Analysis 2.5). In further subgroup analyses, we found no evidence to suggest that the duration of the intervention (Analysis 2.6) or the malaria endemicity at the time when the study was conducted (Analysis 2.7) affected anaemia.
2.2. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 2: Anaemia (by supplement composition)
2.3. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 3: Anaemia (by anaemia status at baseline)
2.4. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 4: Anaemia (by iron status at baseline): Mixed/Unknown
2.5. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 5: Anaemia (by dose of elemental iron per week in the intermittent group)
2.6. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 6: Anaemia (by duration of supplementation)
2.7. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 7: Anaemia (by malaria endemicity)
Haemoglobin
Ten studies reported data on this outcome (Angeles‐Agdeppa 1997; Dos Santos 1999; Jayatissa 1999 (C); Kianfar 2000; Gonzalez‐Rosendo 2002; Agarwal 2003 (C); Shobha 2003; Riuvard 2006; Joshi 2013; Gupta 2014). We pooled these studies in a meta‐analysis and found no evidence that mean haemoglobin concentrations differed between women receiving intermittent iron supplementation and women receiving daily iron supplementation (MD 0.43, 95% CI −1.44 to 2.31; 2127 participants; Analysis 2.8). The level of heterogeneity was high (T2 = 6.45; Chi2 = 40.60 (P < 0.001); I2 = 78%). We rated the quality of the evidence as low.
2.8. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 8: Haemoglobin in g/L (All)
We conducted subgroup analyses and found no evidence that the composition of the supplement (iron only, iron plus folic acid, or iron plus other micronutrients) affected haemoglobin (Analysis 2.9). However, we did find evidence that anaemic women had a stronger response to intermittent supplementation than women with mixed/unknown anaemia status (MD 0.43, 95% CI ‐1.44 to 2.31; 804 participants; Analysis 2.10), but only four studies contributed to this analysis so the results should be interpreted with caution. Not enough studies contributed data for the analysis on women's iron status at baseline (iron deficiency before the supplementation) so that most women had a mixed/unknown iron status (Analysis 2.11). Almost an even number of studies provided 60 mg of elemental iron or less per week (six studies) and more than 60 mg of iron per week (five studies); there was no statistical difference between the groups. In Angeles‐Agdeppa 1997, women who received 60 mg or less intermittently showed higher haemoglobin concentrations than women who received higher doses (Analysis 2.12). We found no evidence of any subgroup differences by duration of the intervention (Analysis 2.13) or malaria endemicity at the time when the study was conducted (Analysis 2.14). There was substantial heterogeneity between the studies in these analyses (between 76% and 80%).
2.9. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 9: Haemoglobin in g/L (by supplement composition)
2.10. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 10: Haemoglobin in g/L (by anaemia status at baseline)
2.11. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 11: Haemoglobin in g/L (by iron status at baseline)
2.12. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 12: Haemoglobin in g/L (by dose of elemental iron per week in the intermittent group)
2.13. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 13: Haemoglobin in g/L (by duration of supplementation)
2.14. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 14: Haemoglobin in g/L (by malaria endemicity)
Iron deficiency
Only a single study reported data on this outcome (Angeles‐Agdeppa 1997). It found no evidence that iron deficiency differed between the groups (RR 4.30, 95% CI 0.56 to 33.20; 198 participants; see the illustrative forest plot in Analysis 2.15). We rated the quality of this evidence as very low.
2.15. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 15: Iron deficiency (All)
Ferritin
Four studies reported data on this outcome (Angeles‐Agdeppa 1997; Agarwal 2003 (C); Riuvard 2006; Gupta 2014). We pooled these studies in a meta‐analysis and found evidence that women receiving iron supplements daily had higher concentrations of ferritin at the end of the intervention than those women receiving iron supplements intermittently (MD −6.07 μg/L, 95% CI −10.66 to −1.48; 988 participants; Analysis 2.16). The heterogeneity was high (T2 = 15.55; Chi2 = 33.80 (P < 0.001); I2= 91%). We rated the quality of this evidence as very low.
2.16. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 16: Ferritin in µg/L (All)
We found statistical differences in all subgroup analyses: daily supplementation was more effective than intermittent supplementation at increasing ferritin concentrations in women regardless of the composition of the supplement (Analysis 2.21), anaemia (Analysis 2.18) or iron status at baseline (Analysis 2.19), dose of elemental iron (Analysis 2.20), duration of supplementation (Analysis 2.17), or malaria endemicity at the time when the study was conducted (Analysis 2.22). However, it should be noted that most subgroups had only one study or included all four studies in the same subgroup, or had no studies, and that there was substantial heterogeneity between studies in these analyses (between 74.4% and 91%). Therefore, results were inconclusive and should be interpreted with caution.
2.21. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 21: Ferritin in µg/L (by supplement composition)
2.18. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 18: Ferritin in µg/L (by anaemia status at baseline)
2.19. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 19: Ferritin in µg/L (by iron status at baseline)
2.20. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 20: Ferritin in µg/L (by dose of elemental iron per week in the intermittent group)
2.17. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 17: Ferritin in µg/L (by duration of supplementation)
2.22. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 22: Ferritin in µg/L (by malaria endemicity): No malaria/Unknown
None of the included studies reported data on the other prespecified primary outcomes: iron‐deficiency anaemia and all‐cause morbidity.
Secondary outcomes
Diarrhoea
Only a single study reported data on this outcome (Angeles‐Agdeppa 1997). It found no evidence that diarrhoea differed between the groups (RR 2.41, 95% CI 0.12 to 49.43; 198 participants; see the illustrative forest plot in Analysis 2.23).
2.23. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 23: Diarrhoea
Any adverse side effects
Six studies reported data on this outcome (Angeles‐Agdeppa 1997; Jayatissa 1999 (C); Shobha 2003; Nguyen 2008; Joshi 2013; Gupta 2014). We pooled these studies in a meta‐analysis and found evidence that women receiving iron supplements intermittently were less likely to have any adverse side effects than those women receiving iron supplements daily (RR 0.41, 95% CI 0.21 to 0.82; 1166 participants; Analysis 2.24).
2.24. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 24: Any adverse side effects
Depression
Only a single study reported data on this outcome (Nguyen 2008). It found no evidence that depression differed between the groups (RR 0.82, 95% CI 0.63 to 1.07; 369 participants; see the illustrative forest plot in Analysis 2.25).
2.25. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 25: Depression
Adherence
Four studies reported data on this outcome (Dos Santos 1999; Gonzalez‐Rosendo 2002; Shah 2002; Riuvard 2006). We pooled these studies in a meta‐analysis and found no evidence that adherence to intermittent supplementation differed from that for daily supplementation (RR 1.04, 95% CI 0.99 to 1.09; 507 participants; Analysis 2.26).
2.26. Analysis.

Comparison 2: Intermittent iron supplementation versus daily iron supplementation, Outcome 26: Adherence
None of the included studies reported data on the other prespecified secondary outcomes: respiratory infections; work performance and economic productivity; school performance and cognitive function; and malaria incidence and severity.
Sensitivity analyses
We conducted sensitivity analyses to examine the potential effect of clustering on the CI of the summary estimates, by removing cluster‐RCTs from the analysis and comparing the effect for anaemia, haemoglobin, and ferritin. We found no significant differences in the results. See Appendix 4.
Discussion
Summary of main results
Available data indicate that, among menstruating women, intermittent oral supplementation with iron (alone or plus any other nutrients) increases haemoglobin and ferritin concentrations and reduces the prevalence of anaemia compared to no supplementation or placebo. Overall, this positive response does not differ when providing iron supplementation weekly or twice weekly; nor does it differ with the duration of the intervention, dose used, or malaria endemicity. As the quality of the evidence was, on average, low, the confidence in the effect estimate is limited and the true effect may be substantially different from the estimate of the effect.
Compared with daily supplementation, findings suggest that intermittent supplementation has a similar effect in reducing the prevalence of anaemia and increasing haemoglobin concentrations at the end of the intervention. However, information from a fewer number of trials shows that women receiving intermittent supplementation are more likely to have lower ferritin concentrations and fewer side effects at the end of the intervention. As the quality of the evidence was also, on average, low, the confidence in the effect estimate is limited and the true effect may be substantially different from the estimate of the effect.
Information on morbidity (including malaria outcomes), work performance and economic productivity, depression, and adherence to the intervention was scarce, but, thus far, there is no evidence that intermittent supplementation has any effect on these outcomes, either when compared with a placebo, no intervention, or with daily iron supplementation. There were no data for the subgroup analysis of the effect of iron status at baseline on anaemia for intermittent iron supplementation compared to placebo or no intervention; and, for the other outcomes, there was only one trial.
Overall completeness and applicability of evidence
This review included a total of 25 RCTs involving 10,996 women; most of them were conducted in low‐ and middle‐income countries in Latin America, Africa, and Asia where anaemia is a public health problem. The overall quality of the evidence was, on average, low, and the main limitation of the studies was the lack of blinding and high attrition.
Intermittent iron supplementation regimens have been proposed as an efficacious and efficient approach to the prevention and control of anaemia and at least 100 studies on intermittent iron supplementation regimens in different age groups have been published during the last 15 years. Although the real effect of an intervention is context‐specific, the results of this review showed that weekly or twice weekly iron supplementation regimens are effective in reducing the prevalence of anaemia and improving haemoglobin and ferritin concentrations in menstruating women in comparison with no supplementation or placebo. There was insufficient information to assess with certainty the effect of this intervention on other health and nutrition outcomes.
The results suggest that the provision of supplements once a week with 60 mg to 120 mg of iron is enough to produce a positive haematological response in populations with different degrees of anaemia. The efficacy of this intervention to treat anaemia was similar to the efficacy of daily supplementation. Furthermore, in all of the studies in which anaemia was an inclusion criterion, there was a higher increase in haemoglobin concentrations among women who received supplements intermittently. This finding was true even in different settings and with different levels of supervision. Folic acid merits a special mention, as its consumption did not have a differential effect on anaemia and haemoglobin concentrations; however, its use during the periconceptional period has been proven to reduce the risk of having babies with NTDs, an outcome that was outside the scope of this review (De‐Regil 2015).
According to our review, daily supplementation was more effective at increasing ferritin concentrations, compared with the provision of supplements once or twice a week. This may have implications for the use of intermittent iron supplementation regimens in populations with a high prevalence of iron deficiency where increasing ferritin concentrations are needed.
Although improved adherence and fewer side effects have been proposed as an advantage of intermittent supplementation over daily supplementation, there is no evidence that in relatively well‐controlled environments and for short periods of supplementation, women adhere better to intermittent regimens. However, there was no difference when women were compared with those receiving a placebo either. Clearly, there are gaps on how the duration, frequency and intensity of side effects affect short‐ and long‐term adherence to supplementation.
One study (459 participants) reported on the incidence of hospitalisation (Nguyen 2008) and one study (24 participants) reported on oxidative stress post‐supplementation (expressed as the Ferric Reducing Ability of the Plasma or FRAP) (Riuvard 2006). These studies found no evidence that the effects of intermittent supplementation on these indicators were different from that produced by daily supplementation. None of the other included studies reported data on these outcomes.
Quality of the evidence
We found the overall quality of the available evidence ranged between moderate to low in comparison 1 and comparison 2, both primarily due to substantial heterogeneity, risk of bias, and methodological inconsistency. Most outcomes with very low quality evidence have only one included study.
Study limitations/risk of bias in included studies
With the exception of two studies (Hall 2002 (C); Nguyen 2008), we considered all of the studies included in this update to be at high risk of bias (see Risk of bias in included studies; Figure 2; Figure 3). Most studies did not describe the methods used to randomly assign participants and conceal allocation. Generally, blinding of participants, care providers and outcome assessors was not attempted, although some studies reported that technical staff carrying out laboratory investigations were unaware of group allocation. This lack of blinding could represent a potentially serious source of bias. Inconsistency was also a problem in many of these studies.
Inconsistency
We considered that clinical inconsistency was unlikely for our outcomes. Variability in participants characteristics, interventions, and outcomes across the included studies was likely to be low (Ryan 2016). However, methodological inconsistency was a potentially important factor in the overall assessment of evidence for our outcomes. We found differences between studies in terms of methodological factors, specifically blinding and allocation concealment, that may have led to differences in the observed intervention effects (Higgins 2011a). We found substantial heterogeneity in some outcomes, especially anaemia and haemoglobin, that could be partly explained by subgroup analyses. Although this does not necessarily mean that the true intervention effect varies, results should be interpreted with some caution.
Imprecision
Imprecision due to small sample sizes or few events in the included studies was unlikely. However, we considered imprecision in continuous outcomes (i.e. haemoglobin and ferritin measurements) an important factor in the overall assessment of the evidence. There was a lot of variation in the effects of the intervention among participants for continuous outcomes, as results showed wide CIs around the effect estimate (Ryan 2016).
Indirectness
We considered that indirectness was unlikely. We found no indirectness regarding population, interventions, or outcomes assessed across studies. The study populations paralleled those of clinical and public health interest under real conditions. The evidence summarised in the review comes from studies addressing the main review questions, especially for our primary outcomes; and our secondary outcomes were almost not addressed.
Publication bias
We considered that publication bias was unlikely. Data used in the analyses came from representative samples from the studies that have been conducted. Overall, included studies had large sample sizes and numbers of events (i.e. more than 300) (Ryan 2016). However, some subgroup analyses had small sample sizes.
Potential biases in the review process
We attempted to minimise bias in several ways. We tried to be as inclusive as possible to avoid potential bias in the search strategy and found publications in different languages in journals from all continents, although the literature identified was predominantly written in English. We were also able to obtain some unpublished information. Both review authors independently assessed the eligibility of studies for inclusion, participated in data extraction, and conducted the 'Risk of bias' assessments. One review author entered the data into a form design for the review and the other checked the data for accuracy. However, carrying out reviews is not an exact science and may require a number of subjective judgements; it is possible that a different review team may have reached different decisions regarding assessments of eligibility and risk of bias. We would encourage readers to examine the Characteristics of included studies tables to assist in the interpretation of results.
Several studies had selection bias, with both unclear random sequence generation and unclear concealment of the allocation sequence, which could have introduced bias at the group level in terms of differences between the baseline characteristics of the groups that were compared. When the intervention was allocated at class level or studies were cluster (C) RCTs, such as Jayatissa 1999 (C) and Agarwal 2003 (C), we assumed that bias at the individual level was unlikely. We also assumed a low risk of bias when tablets had the same colour and shape, or were manufactured by the same laboratory, although some studies did not describe the method to conceal the allocation, such as Zavaleta 2000 and Leenstra 2009.
Agreements and disagreements with other studies or reviews
To our knowledge, only one meta‐analysis of RCTs has been conducted previously on the efficacy of intermittent iron supplementation in the control of iron deficiency anaemia (Beaton 1999). That review included the results of 22 studies completed before 1999 in different age groups. Of the included studies, nine were carried out among adolescents and compared once or twice a week versus daily supplementation; most of them also assessed a control group that did not receive iron. All studies reported results for haemoglobin and three also measured ferritin. The Beaton 1999 review did not include adult non‐pregnant women, and the review authors pooled the results from school‐aged children and adolescents.
Like us, the authors of Beaton 1999 concluded that intermittent supplementation increased haemoglobin and ferritin levels and reduced anaemia when compared with no intervention or a placebo. However, findings from Beaton 1999 and Fernández‐Gaxiola 2011a suggested that intermittent supplementation was less efficacious than daily supplementation in reducing anaemia (RR 1.44, 95% CI 1.33 to 1.56; and RR 1.26: 95% CI 1.04 to 1.52, respectively), but there were no statistical differences in haemoglobin concentrations between regimens. The authors of Beaton 1999 concluded that weekly supplementation should be considered for school‐aged children and adolescents only in situations where there is strong assurance of supervision and high adherence.
A more recent unpublished review included 12 studies evaluating the effects of weekly iron and folic acid supplementation among non‐pregnant women of reproductive age (Margetts 2007). The results suggested that the consumption of supplements containing 60 mg of elemental iron with folic acid for at least 12 weeks, with or without deworming treatment, increased iron status, as judged by increased haemoglobin and, in some studies, serum ferritin levels. The effect of weekly supplementation on haemoglobin concentration was similar to that reported for daily supplementation, except in subsets of women who were severely anaemic at baseline where daily supplementation was more effective.
Overall, the findings of these reviews agree with the findings of this Cochrane Review. The 25 studies included in our review, conducted in different age groups, contexts and with different levels of supervision, show that intermittent supplementation may be an effective public health intervention. In contexts where daily supplementation has failed, has not been implemented or there is a strong need to increase coverage in at‐risk populations and economic resources are limited, the feasibility of delivering intermittent supplementation could make this intervention a viable alternative to consider.
The results of the present review are only applicable to menstruating women. However, another systematic review assessing the benefits and safety of this intervention in preschool‐aged and school‐aged children concurs with our findings (De‐Regil 2011). From the programme implementation perspective, a recent narrative review reports that weekly iron and folic acid supplementation has been successfully implemented in Cambodia, Egypt, India, Laos, the Philippines, and Vietnam, reaching over half a million menstruating women (WHO‐WPRO 2011).
Authors' conclusions
Implications for practice.
Intermittent supplementation with iron alone or in combination with other micronutrients may reduce anaemia and may improve iron stores among menstruating women in populations with different anaemia and malaria backgrounds. Women receiving supplements intermittently can probably reduce their anaemia and may achieve similar haemoglobin concentrations at the end of the intervention than women receiving supplements daily. With the current evidence, there is no indication that this intervention has detrimental effects on women's health and other indicators of nutritional status. Good supervision and adherence is fundamental for the intervention to succeed. Intermittent iron supplementation is a feasible intervention for reaching other populations in a variety of settings, outside antenatal‐care (ANC) visits, immunisation programmes, and health programmes for adolescents and women of reproductive age.
Most studies provided 60 mg of elemental iron or more on a weekly basis, and the effect on the haematological status may not be affected by the duration of the intervention. The provision of micronutrients other than iron may not alter the haematological response. Iron and folic acid supplementation, therefore, have the possibility of impacting not only menstruating women, but also of benefiting those women who become pregnant and their babies, and improving their nutritional status and impacting other indicators of micronutrients status and health.
The evidence on the efficacy and effectiveness of this intervention is uncertain due to the low quality of the evidence base. The true effect may be substantially different from the estimate of the effect.
Implications for research.
This review has highlighted the need for further research in this area, particularly on:
side effects and adherence to the intervention;
patient‐important outcomes and adverse effects;
the effects of the provision of multiple micronutrients on an intermittent basis and their effect on iron status and other indicators of micronutrients status and health;
the periodicity of intermittent iron supplementation to maintain an adequate iron status throughout the reproductive years;
the effective and safe dose of folic acid that should be used along with iron to supplement women intermittently;
the effects of intermittent iron supplementation regimens on work performance and productivity outcomes;
economic analyses; and
the effects of intermittent iron supplementation regimens on malaria outcomes.
Lack of methodological rigor in some RCTs included in this review has resulted in low‐quality evidence in the review. Improving the quality of primary studies is needed.
What's new
| Date | Event | Description |
|---|---|---|
| 14 May 2020 | Amended | Minor edits made to the 'What evidence did we find?' section of the PLS for added clarity and improved consistency with the Abstract. |
History
Protocol first published: Issue 7, 2011 Review first published: Issue 12, 2011
| Date | Event | Description |
|---|---|---|
| 3 October 2018 | New citation required and conclusions have changed | Conclusions on the equivalence between daily and intermittent supplementation changed: both interventions produce a similar effect on anaemia and haemoglobin concentrations. |
| 3 October 2018 | New search has been performed | Review updated. Four new studies included following searches in January 2017 and February 2018. |
| 4 September 2018 | New search has been performed | Reviewers comments and suggestions incorporated and updated with another included trial |
| 20 April 2018 | Feedback has been incorporated | Editorial suggestions have been incorporated and search has been updated as indicated |
Acknowledgements
We would like to thank the study authors who contributed additional data for this review. We would also like to thank Dr Mona Nasser for her contributions during the protocol stage (Fernández‐Gaxiola 2011a), and to all the staff at the editorial office of Cochrane Developmental, Psychosocial and Learning Problems (CDPLP) for their support in the preparation of this review.
As part of the pre‐publication editorial process, the text has been commented on by three peers (an editor and two referees who are external to the editorial team) and one of the CDPLP's statisticians. We are grateful for their feedback.
Ana Cecilia Fernández‐Gaxiola received partial financial support from the Evidence and Programme Guidance, World Health Organization, to update the review.
Appendices
Appendix 1. Search strategies 2011 onwards
Cochrane Central Register of Controlled Trials (CENTRAL)
#1MeSH descriptor Iron, this term only #2MeSH descriptor Iron, Dietary, this term only #3MeSH descriptor Anemia, Iron‐Deficiency, this term only #4MeSH descriptor Folic Acid, this term only #5iron* or folic* or folate* or folvite* or folacin* or pteroylglutamic* #6MeSH descriptor Ferric Compounds, this term only #7MeSH descriptor Ferrous Compounds, this term only #8ferrous* or ferric* or fe #9{or #1‐#8} #10MeSH descriptor Drug Administration Schedule, this term only #11MeSH descriptor Dose‐Response Relationship, Drug explode all trees #12MeSH descriptor Time Factors, this term only #13week* or biweek* or bi next week* or intermittent* or alternat* #14{or #10‐#13} #15#9 and #14 #16(iron near/3 (dose* or dosage or administer* or administration or frequency or schedule)) #17#15 or #16 #18MeSH descriptor Adolescent, this term only #19MeSH descriptor Adult, this term only #20MeSH descriptor Middle Aged, this term only #21(adult* or teen* or adoles* or pubert* or pubescen*) #22{or #18‐#21} #23MeSH descriptor: [Female] explode all trees #24girl* or female* #25#23 or #24 #26#22 and #25 #27wom*n* #28#26 or #27 #29#17 and #28 Publication Year from 2011 to 2017, in Trials #30#17 and #28 Publication Year from 2016 to 2018, in Trials
MEDLINE
1 Iron/ 2 Anemia, Iron‐Deficiency/ 3 Iron, Dietary/ 4 Folic Acid/ 5 iron$.tw. 6 (folic$ or folate$ or folvite$ or folacin$ or pteroylglutamic$).tw. 7 Ferric Compounds/ 8 Ferrous Compounds/ 9 (ferrous$ or ferric$ or fe).tw. 10 or/1‐9 11 Drug Administration Schedule/ 12 Time Factors/ ) 13 (week$ or biweek$ or bi‐week$ or intermittent$ or alternat$).tw. 14 or/11‐13 15 10 and 14 16 (iron adj3 (dose$ or dosage or administer$ or administration or frequency or regimen$ or supplement$)).tw. 17 15 or 16 18 adolescent/ or adult/ or middle aged/ 19 (adult$ or teen$ or adoles$ or pubert$ or pubescen$).tw. 20 18 or 19 21 Female/ 22 (girl$ or female$).tw. 23 or/21‐22 24 20 and 23 25 wom#n.tw. 26 24 or 25 27 randomized controlled trial.pt. 28 controlled clinical trial.pt. 29 randomi#ed.ab. 30 placebo$.ab. 31 drug therapy.fs. 32 randomly.ab. 33 trial.ab. 34 groups.ab. 35 or/27‐34 36 exp animals/ not humans.sh. 37 35 not 36 38 17 and 26 and 37 39 limit 38 to ed=20110502‐20180208
MEDLINE In‐Process & Other Non‐Indexed Citations
1 iron$.tw. 2 (folic acid or folate$ or folvite$ or folacin$ or pteroylglutamic$).tw. 3 (ferric or ferrous or ferritin$).tw. 4 or/1‐3 5 (week$ or biweek$ or bi‐week$ or intermittent$ or alternat$).tw. 6 4 and 5 7 (iron adj3 (dose$ or dosage or administer$ or administration or frequency or regimen$ or schedule or supplement$)).tw. 8 6 or 7 9 (adult$ or teen$ or adoles$ or pubert$ or pubescen$).tw. 10 (girl$ or female$).tw. 11 9 and 10 12 wom#n$.tw. 13 11 or 12 14 8 and 13 15 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw. 16 14 and 15
MEDLINE Epub Ahead of Print
1 iron$.tw. 2 (folic acid or folate$ or folvite$ or folacin$ or pteroylglutamic$).tw. 3 (ferric or ferrous or ferritin$).tw. 4 or/1‐3 5 (week$ or biweek$ or bi‐week$ or intermittent$ or alternat$).tw. 6 4 and 5 7 (iron adj3 (dose$ or dosage or administer$ or administration or frequency or regimen$ or schedule or supplement$)).tw. 8 6 or 7 9 (adult$ or teen$ or adoles$ or pubert$ or pubescen$).tw. 10 (girl$ or female$).tw. 11 9 and 10 12 wom#n$.tw. 13 11 or 12 14 8 and 13
Embase Ovid
1 iron/ 2 iron intake/ 3 iron deficiency anemia/ 4 folic acid/ 5 iron$.tw. 6 (folic$ or folate$ or folvite$ or folacin$ or pteroylglutamic$).tw. 7 ferric ion/ 8 ferrous ion/ 9 or/1‐8 10 drug administration/ 11 drug dose regimen/ 12 (week$ or biweek$ or bi‐week$ or intermittent$ or alternat$).tw. 13 or/10‐12 14 9 and 13 15 (iron adj3 (dose$ or dosage or administer$ or administration or frequency or shedule)).tw. 16 14 or 15 17 adult/ or middle aged/ or adolescent/ 18 (teen$ or adoles$ or pubert$ or pubescen$).tw. 19 17 or 18 20 female/ 21 (girl$ or female$).tw. 22 20 or 21 23 wom#n.tw. 24 (19 and 22) or 23 25 16 and 24 26 Randomized controlled trial/ 27 controlled clinical trial/ 28 Single blind procedure/ 29 Double blind procedure/ 30 triple blind procedure/ 31 Crossover procedure/ 32 (crossover or cross‐over).tw. 33 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 34 Placebo/ 35 placebo.tw. 36 prospective.tw. 37 factorial$.tw. 38 random$.tw. 39 assign$.ab. 40 allocat$.tw. 41 volunteer$.ab. 42 or/26‐41 43 25 and 42 44 limit 43 to yr="2011 ‐Current"
CINAHL Plus (Cumulative Index to Nursing and Allied Health Literature)
S1(MH "Iron") S2(MH "Iron Compounds") S3(MH "Ferric Compounds") S4(MH "Ferrous Compounds") S5(MH "Folic Acid") S6(MH "Anemia, Iron Deficiency") S7(MH "Anemia, Iron Deficiency") S8TI(iron*) OR AB(iron*) S9TI(folic* or folate* or folvite* or folacin* or pteroylglutamic*) OR AB(folic* or folate* or folvite* or folacin* or pteroylglutamic*) S10S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 S11(MH "Drug Administration Schedule") S12(MH "Time Factors") S13(week* or biweek* or bi‐week*or bi week* or intermittent* or alternat* or regimen*) S14S11 OR S12 OR S13 S15S10 AND S14 S16(iron N3 dose*) or (iron N3 dosage) or (iron N3 administer*) or (iron N3 administration) or (iron N3 frequency) or (iron N3 supplement*) or (iron* N3 schedule) S17S15 OR S16 S18(AG adolescent or AG adult or AG middle aged) OR (adolescen* or pubert* or pubescen* or adult*) S19CT female or TI(female* or girl*) OR AB(female* or girl*) S20S18 AND S19 S21(MH "Women") or TI(women or woman) OR AB(women or woman) S22S20 OR S21 S23S17 AND S22 S24(MH "Clinical Trials+") S25MH random assignment S26(MH "Meta Analysis") S27(MH "Crossover Design") S28(MH "Quantitative Studies") S29PT randomized controlled trial S30PT Clinical trial S31(clinical trial*) or (control* N2 trial*) S32("follow‐up study" or "follow‐up research") S33(prospectiv* study or prospectiv* research) S34(evaluat* N2 study or evaluat* N2 research) S35(MH "Program Evaluation") S36(MH "Treatment Outcomes") S37TI(single N2 mask* or single N2 blind*) OR AB(single N2 mask* or single N2 blind*) S38TI((doubl* N2 mask*) or (doubl* N2 blind*)) OR AB((doubl* N2 mask*) or (doubl* N2 blind*)) S39TI ((tripl* N2 mask*) or (tripl* N2 blind*)) or ((trebl* N2 mask*) or (trebl* N2 blind*)) OR AB((tripl* N2 mask*) or (tripl* N2 blind*)) or ((trebl* N2 mask*) or (trebl* N2 blind*) S40random* S41S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 S42S23 AND S41 S43EM 20110501‐ S44S42 AND S43
Science Citation Index (SCI)
#7 #6 AND #5 Indexes=SCI‐EXPANDED Timespan=2011‐2018 # 6 TS=(random* or RCT or trial* or allocat* or assign* or placebo* or cross‐over or crossover or "cross over" or factorial* or "double blind*" or "single blind") Indexes=SCI‐EXPANDED Timespan=2011‐2018 # 5 #4 AND #1 Indexes=SCI‐EXPANDED Timespan=2011‐2018 # 4 #3 OR #2 Indexes=SCI‐EXPANDED Timespan=2011‐2018 # 3 TS=(women* or woman*) Indexes=SCI‐EXPANDED Timespan=2011‐2018 # 2 TS=((female* or girl*) and (adult* or adolescen* or teen* or pubert* or pubescen*)) Indexes=SCI‐EXPANDED Timespan=2011‐2018 # 1 TS=((iron* or "folic acid" or ferrous or ferric ) near/10 (alternate* or dose* or week* or intermittent or biweek* or bi‐week* or schedule or supplement* )) Indexes=SCI‐EXPANDED Timespan=2011‐2018
Conference Proceedings Citation Index‐ Science (CPCI‐S)
#7 #6 AND #5 Indexes=CPCI‐S Timespan=2011‐2018 # 6 TS=(random* or RCT or trial* or allocat* or assign* or placebo* or cross‐over or crossover or "cross over" or factorial* or "double blind*" or "single blind") Indexes=CPCI‐S Timespan=2011‐2018 # 5 #4 AND #1 Indexes=CPCI‐S Timespan=2011‐2018 # 4 #3 OR #2 Indexes=CPCI‐S Timespan=2011‐2018 # 3 TS=(women* or woman*) Indexes=CPCI‐S Timespan=2011‐2018 # 2 TS=((female* or girl*) and (adult* or adolescen* or teen* or pubert* or pubescen*)) Indexes=CPCI‐S Timespan=2011‐2018 # 1 TS=((iron* or "folic acid" or ferrous or ferric ) near/10 (alternate* or dose* or week* or intermittent or biweek* or bi‐week* or schedule or supplement* )) Indexes=CPCI‐S Timespan=2011‐2018
Cochrane Database of Systematic Reviews (CDSR)
#1MeSH descriptor Iron, this term only #2MeSH descriptor Iron, Dietary, this term only #3MeSH descriptor Anemia, Iron‐Deficiency, this term only #4MeSH descriptor Folic Acid, this term only #5iron* or folic* or folate* or folvite* or folacin* or pteroylglutamic* #6MeSH descriptor Ferric Compounds, this term only #7MeSH descriptor Ferrous Compounds, this term only #8ferrous* or ferric* or fe:TI,AB #9{or #1‐#8} #10MeSH descriptor Drug Administration Schedule, this term only #11MeSH descriptor Dose‐Response Relationship, Drug explode all trees #12MeSH descriptor Time Factors, this term only #13(week* or biweek* or bi next week* or intermittent* or alternat*):TI,AB #14{or #10‐#13} #15#9 and #14 #16(iron near/3 (dose* or dosage or administer* or administration or frequency or schedule)):TI,AB #17#15 or #16 #18MeSH descriptor Adolescent, this term only #19MeSH descriptor Adult, this term only #20MeSH descriptor Middle Aged, this term only #21(adult* or teen* or adoles* or pubert* or pubescen*):TI,AB #22{or #18‐#21} #23MeSH descriptor: [Female] explode all trees #24(girl* or female*):TI,AB #25#23 or #24 #26#22 and #25 #27wom*n*:TI,AB #28#26 or #27 #29#17 and #28 in Cochrane Reviews (Reviews and Protocols)
Database of Abstracts of Reviews of Effect (DARE)
#1MeSH descriptor Iron, this term only #2MeSH descriptor Iron, Dietary, this term only #3MeSH descriptor Anemia, Iron‐Deficiency, this term only #4MeSH descriptor Folic Acid, this term only #5iron* or folic* or folate* or folvite* or folacin* or pteroylglutamic* #6MeSH descriptor Ferric Compounds, this term only #7MeSH descriptor Ferrous Compounds, this term only #8ferrous* or ferric* or fe:TI,AB #9{or #1‐#8} #10MeSH descriptor Drug Administration Schedule, this term only #11MeSH descriptor Dose‐Response Relationship, Drug explode all trees #12MeSH descriptor Time Factors, this term only #13(week* or biweek* or bi next week* or intermittent* or alternat*):TI,AB #14{or #10‐#13} #15#9 and #14 #16(iron near/3 (dose* or dosage or administer* or administration or frequency or schedule)):TI,AB #17#15 or #16 #18MeSH descriptor Adolescent, this term only #19MeSH descriptor Adult, this term only #20MeSH descriptor Middle Aged, this term only #21(adult* or teen* or adoles* or pubert* or pubescen*):TI,AB #22{or #18‐#21} #23MeSH descriptor: [Female] explode all trees #24(girl* or female*):TI,AB #25#23 or #24 #26#22 and #25 #27wom*n*:TI,AB #28#26 or #27 #29#17 and #28 in Other Reviews
POPLINE
((((iron*) OR (folic*) OR (folate*) OR (supplement*))) AND (((week*) OR ('bi\‐weekly') OR ('bi weekly') OR (biweekly) OR (alternat*) OR (intermittent*))) AND (((women*) OR (girl*) OR (female*) OR (women*))) AND (((random*) OR (placebo*) OR (group*) OR (trial*) OR (control*) OR (blind*))))
Scientific Electronic Library Online (SciElo)
iron AND supplementation AND women
LILACS (Latin American and Caribbean Health Science Information database)
iron AND supplementation AND women
IBECS
iron AND supplementation AND women
IMBIOMED
iron AND supplementation AND women
ClinicalTrials.gov
Interventional Studies | iron OR folic OR ferrous OR ferric | (female* OR women OR girl*) NOT pregnant | Studies received from 05/01/2011 to 02/20/2018
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP)
Advanced search. TITLE: women NOT pregnant OR girl NOT pregnant OR female NOT pregnant AND Intervention:ferrous OR ferric OR iron OR folic Date of registration 01/05/2011 to 22/02/2018
Appendix 2. Search strategies up to 2011
CENTRAL
#1MeSH descriptor Iron, this term only #2MeSH descriptor Iron, Dietary, this term only #3MeSH descriptor Anemia, Iron‐Deficiency, this term only #4MeSH descriptor Folic Acid, this term only #5MeSH descriptor Dietary Supplements, this term only #6MeSH descriptor Trace Elements, this term only #7folic* or folate* or folvite* or folacin* or pteroylglutamic* #8diet* NEAR/3 supplement* #9micro‐nutrient* or micronutrient* or multi‐nutrient* or multinutrient* #10MeSH descriptor Ferric Compounds, this term only #11MeSH descriptor Ferrous Compounds, this term only #12ferrous* or ferric* or fe #13MeSH descriptor Micronutrients, this term only #14(#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13) #15MeSH descriptor Drug Administration Schedule, this term only #16MeSH descriptor Dose‐Response Relationship, Drug explode all trees #17MeSH descriptor Time Factors, this term only #18week* or biweek* or bi NEXT week* or intermittent* or alternat* #19(#15 OR #16 OR #17 OR #18) #20(#14 AND #19) #21(iron NEAR/3 (dose* or dosage or administer* or administration or frequency)) #22(#20 OR #21) #23MeSH descriptor Adolescent, this term only #24MeSH descriptor Adult, this term only #25MeSH descriptor Middle Aged, this term only #26(teen* or adoles* or pubert* or pubescen*) #27(#23 OR #24 OR #25 OR #26) #28(girl* or female* or woman* or women*) #29(#27 AND #28) #30(#22 AND #29) #31(#30), from 1980 to 2011
MEDLINE
1 Iron/ 2 Anemia, Iron‐Deficiency/ 3 Iron, Dietary/ 4 Folic Acid/ 5 iron$.tw. 6 (folic$ or folate$ or folvite$ or folacin$ or pteroylglutamic$).tw. 7 Ferric Compounds/ 8 Ferrous Compounds/ 9 (ferrous$ or ferric$ or fe).tw. 10 micronutrients/ 11 (micro‐nutrient$ or micronutrient$ or multi‐nutrient$ or multinutrient$).tw. 12 Dietary Supplements/ 13 (diet$ adj3 supplement$).tw. 14 or/1‐13 15 Drug Administration Schedule/ 16 Time Factors/ 17 (week$ or biweek$ or bi‐week$ or intermittent$ or alternat$).tw. 18 or/15‐17 19 14 and 18 20 (iron adj3 (dose$ or dosage or administer$ or administration or frequency or regimen$ or supplement$)).tw. 21 19 or 20 22 adolescent/ or adult/ or middle aged/ 23 (teen$ or adoles$ or pubert$ or pubescen$).tw. 24 22 or 23 25 Female/ 26 (girl$ or female$ or wom#n).tw. 27 or/25‐26 28 24 and 27 29 randomized controlled trial.pt. 30 controlled clinical trial.pt. 31 randomi#ed.ab. 32 placebo$.ab. 33 randomly.ab. 34 trial.ab. 35 clinical trials as topic.sh. 36 or/29‐35 37 exp animals/ not humans.sh. 38 36 not 37 39 21 and 28 and 38 40 limit 39 to yr="1980 ‐Current"
Embase
1 iron/ 2 iron intake/ 3 iron deficiency anemia/ 4 folic acid/ (32481) 5 diet supplementation/ 6 trace element/ 7 iron$.tw. 8 (folic$ or folate$ or folvite$ or folacin$ or pteroylglutamic$).tw. 9 (diet$ adj3 supplement$).tw. 10 (micro‐nutrient$ or micronutrient$ or multi‐nutrient$ or multinutrient$).tw. 11 ferric ion/ 12 ferrous ion/ 13 or/1‐12 14 drug administration/ 15 drug dose regimen/ 16 (week$ or biweek$ or bi‐week$ or intermittent$ or alternat$).tw. 17 or/14‐16 18 13 and 17 19 (iron adj3 (dose$ or dosage or administer$ or administration or frequency)).tw. 20 18 or 19 21 adult/ or middle aged/ or adolescent/ 22 (teen$ or adoles$ or pubert$ or pubescen$).tw. 23 21 or 22 24 female/ 25 (girl$ or female$ or wom#n).tw. 26 24 or 25 ( 27 23 and 26 28 20 and 27 29 Randomized controlled trial/ 30 Randomization/ 31 Single blind procedure/ 32 Double blind procedure/ 33 Crossover procedure/ 34 Placebo/ (178428) 35 Randomi#ed.tw. 36 RCT.tw. 37 (random$ adj3 (allocat$ or assign$)).tw. 38 randomly.ab. 39 groups.ab. 40 trial.ab. 41 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 42 Placebo$.tw. 43 Prospective study/ 44 (crossover or cross‐over).tw. 45 prospective.tw. 46 or/29‐45 47 28 and 46
CINAHL Plus
S42 S23 and S41 S41 S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 S40 (MH "Evaluation Research") OR (MH "Summative Evaluation Research") OR (MH "Program Evaluation") S39 (MH "Treatment Outcomes") S38 (MH "Comparative Studies") S37 TI (evaluat* study or evaluat* research) or AB (evaluate* study or evaluat* research) or TI (effectiv* study or effectiv* research) or AB (effectiv* study or effectiv* research) OR TI (prospectiv* study or prospectiv* research) or AB(prospectiv* study or prospectiv* research) or TI (follow‐up study or follow‐up research) or AB (prospectiv* study or prospectiv* research) S36 "cross over*" S35 crossover* S34 (MH "Crossover Design") S33 (tripl* N3 mask*) or (tripl* N3 blind*) S32 (trebl* N3 mask*) or (trebl* N3 blind*) S31 (doubl* N3 mask*) or (doubl* N3 blind*) S30 (singl* N3 mask*) or (singl* N3 blind*) S29 (clinic* N3 trial*) or (control* N3 trial*) S28 (random* N3 allocat* ) or (random* N3 assign*) S27 randomis* or randomiz* S26 (MH "Meta Analysis") S25 (MH "Clinical Trials+") S24 MH random assignment S23 S17 and S22 S22 S20 or S21 S21 (MH "Women's Health") S20 18 and 19 S19 CT female or ( woman or women or female* or girl*) S18 (AG adolescent or AG adult or AG middle aged) OR (adolescen* or pubert* or pubescen*) S17 S15 or S16 S16 (iron N3 dose*) or (iron N3 dosage) or (iron N3 administer*) or (iron N3 administration) or (iron N3 frequency) or (iron N3 supplement*) S15 S10 and S14 S14 S11 or S12 or S13 S13 (week* or biweek* or bi‐week*or bi week* or intermittent* or alternat* or regimen*) S12 (MH "Time Factors") S11 (MH "Drug Administration Schedule") S10 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 S9 micro‐nutrient* or micronutrient* or micro nutrient* multi‐nutrient* or multinutrient* or multi nutrient* S8 ferrous* or ferric* or "fe" S7 diet* N3 supplement* S6 folic* or folate* or folvite* or folacin* or pteroylglutamic* S5 iron* 5 S4 (MH "Micronutrients") S3 (MH "Dietary Supplements") S2 (MH "Folic Acid") S1 (MH "Iron") OR (MH "Anemia, Iron Deficiency") OR (MH "Iron Compounds") OR (MH "Ferric Compounds") OR (MH "Ferrous Compounds")
SCI
#7 #6 AND #5 #6 TS=(random* or RCT or trial* or allocat* or assign* or placebo* or cross‐over or crossover or "cross over" or factorial* or "double blind*" or "single blind") #5 #4 AND #3 #4 TS=(women or woman or female* or girl*) #3 #1 same #2 #2 TS=(iron or "folic acid" or ferrous or ferric or micronutrient* or multiutrient* or micro‐nutrient* or multi‐nutrient* ) #1 TS= (alternate* or week* or intermittent or biweek* or bi‐week* or "bi week*" or supplement* )
CPCI‐S
#7 #6 AND #5 #6 TS=(random* or RCT or trial* or allocat* or assign* or placebo* or cross‐over or crossover or "cross over" or factorial* or "double blind*" or "single blind") #5 #4 AND #3 #4 TS=(women or woman or female* or girl*) #3 #1 same #2 #2 TS=(iron or "folic acid" or ferrous or ferric or micronutrient* or multiutrient* or micro‐nutrient* or multi‐nutrient* ) #1 TS= (alternate* or week* or intermittent or biweek* or bi‐week* or "bi week*" or supplement* )
BIOSIS
#7 #6 AND #5 #6 TS=(random* or RCT or trial* or allocat* or assign* or placebo* or cross‐over or crossover or "cross over" or factorial* or "double blind*" or "single blind") #5 #4 AND #3 #4 TS=(women or woman or female* or girl*) #3 #1 same #2 #2 TS=(iron or "folic acid" or ferrous or ferric or micronutrient* or multiutrient* or micro‐nutrient* or multi‐nutrient* ) #1 TS= (alternate* or week* or intermittent or biweek* or bi‐week* or "bi week*" or supplement* )
POPLINE
(iron* /folic* / folate* /supplement*/micronutrient*/micro‐nutrient*) & (week* /bi‐week* / bi week* / biweek* / intermittent / alternat*) & (women / woman /girl* / female*)
SciElo
iron AND supplementation AND women
LILACS
iron AND supplementation AND women
IBECS
iron AND supplementation AND women
IMBIOMED
iron AND supplementation AND women
WHO ICTRP
Iron supplementation AND women Iron supplementation AND girls
metaRegister
Iron supplementation AND women Iron supplementation AND girls
Appendix 3. Criteria for assessing risk of bias
Sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence. We assessed the method as follows.
Low risk of bias: any truly random process (for example, random number table; computer random number generator)
High risk of bias: any non‐random process (for example, odd or even date of birth; hospital or clinic record number)
Unclear risk of bias: insufficient information to facilitate a judgement of low or high risk of bias
Allocation concealment (checking for possible selection bias)
For each included study we described the method used to conceal the allocation sequence (when applicable) and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment. We assessed the method as follows.
Low risk of bias: concealed allocation using, for example, telephone or central randomisation, consecutively numbered sealed opaque envelopes (or equivalent)
High risk of bias: allocation based on, for example, open random allocation, unsealed or non‐opaque envelopes
Unclear risk of bias: insufficient information to facilitate a judgement of low or high risk of bias
Blinding (checking for possible performance and detection bias)
For each included study we described the methods used to blind performance and outcome assessment. For the first one, we described the methods used, if any, for blinding: 1. study participants and 2. personnel, from knowledge of the allocated intervention during the study. For the second one, we described the methods used, if any, for blinding: 3. outcome assessors, from knowledge of which intervention a participant reviewed. Whilst we reported these judgements separately, we combined the results into one judgement of overall risk of bias associated with blinding as follows (Higgins 2011a).
Low risk of bias: blinding of participants, key study personnel and outcome assessment ensured, and unlikely that blinding could have been broken; or none or incomplete blinding but the review authors judged that the outcome or outcome measurement was unlikely to be influenced by lack of blinding
High risk of bias: blinding of key study participants and personnel or outcome assessment attempted, but likely that blinding could have been broken and the outcome or outcome measurement influenced by the lack of blinding; or no blinding or incomplete blinding, and the outcome or outcome measurement was likely to be influenced by lack of blinding
Unclear risk of bias: insufficient information to facilitate a judgement of low or high risk of bias
Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
For each included study we described the completeness of data, including attrition and exclusions from the analysis, and noted if attrition levels were higher for one prespecified outcome or group of outcomes. We also noted whether missing data were imbalanced across groups, the reasons for attrition or exclusions where reported, or whether data were imputed (and, if so, the methods used). We assessed the methods as follows.
Low risk of bias: fewer than 20% of cases lost to follow‐up and balanced in numbers across intervention groups
High risk of bias: 20% or cases lost to follow‐up or outcome data imbalanced in numbers across intervention groups
Unclear risk of bias: insufficient information to facilitate a judgement of low or high risk of bias
Selective reporting bias
For each included study we described how we investigated the possibility of selective outcome reporting bias and what we found. We assessed the methods as follows.
Low risk of bias: it was clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review were reported
High risk of bias: not all the study’s prespecified outcomes were reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so could not be used; the study failed to include the results of a key outcome that was expected to be reported
Unclear risk of bias: insufficient information to facilitate a judgement of low or high risk of bias
Other sources of bias
For each included study we described any important concerns we had about other possible sources of bias and assessed them as follows.
Low risk of bias: study appeared to be free of other sources of bias
High risk of bias: there was at least one important risk of bias; for example, the study had a potential source of bias related to the specific study design as not being blinded or selective outcome reporting
Unclear risk of bias: insufficient information to facilitate a judgement of low or high risk of bias
Appendix 4. Sensitivity analyses for clustering effect
We conducted sensitivity analyses by reanalysing the data for the primary outcomes with cluster‐RCTs excluded. Below, we present the results.
Intermittent iron supplementation (alone or plus any other micronutrients) versus no supplementation or placebo
Anaemia
Anaemia with cluster‐RCT: RR 0.65, 95% CI 0.49 to 0.87; 3135 participants; Analysis 1.1; T2 = 0.16, z = 2.90; P < 0.001 Anaemia without cluster‐RCT: RR 0.38, 95% CI 0.24 to 0.62; 765 participants; T2= 0.16, z = 3.93; P = 0.02
Haemoglobin
Haemoglobin with cluster‐RCT: MD 5.19 g/L, 95% CI 3.07 to 7.32; 2886 participants; Analysis 1.8; T2 = 14.01, z = 5.42; P < 0.001 Haemoglobin without cluster‐RCT: MD 6.58 g/L, 95% CI 4.20 to 8.96; 1603 participants; T2 = 10.34, z = 5.42; P < 0.001
Iron deficiency
Iron deficiency with cluster‐RCT: RR 0.50, 95% CI 0.24 to 1.04; 624 participants; Analysis 1.15; T2 = 0.36, z = 1.86; P < 0.001 Iron deficiency without cluster‐RCT: RR 0.37, 95% CI 0.07 to 1.91; 431 participants; T2 = 1.32, z = 1.18; P = 0.24
Ferritin
Ferritin with cluster‐RCT: MD 7.46 μg/L, 95% CI 5.02 to 9.90; 1067 participants, Analysis 1.16; T2 = 4.10, z = 6.00; P < 0.001 Ferritin without cluster‐RCT: MD 7.25 μg/L, 95% CI 4.72 to 9.79; 970 participants; T2 = 4.32, z = 5.61; P < 0.001
Intermittent iron supplementation versus daily iron supplementation
Anaemia
Anaemia with cluster‐RCT: RR 1.09, 95% CI 0.93 to 1.29; 1749 participants; Analysis 2.1; T2 = 0.01, z = 1.04; P = 0.30 Anaemia without cluster‐RCT: RR 1.04, 95% CI 0.82 to 1.32; 1145 participants; T2 = 0.02, z = 0.30; P = 0.08
Haemoglobin
Haemoglobin with cluster‐RCT: MD 0.43, 95% CI −1.44 to 2.31; 2127 participants; Analysis 2.8; T2= 6.45, z = 0.45; P = 0.65 Haemoglobin without cluster‐RCT: MD 01.38, 95% CI 0.06 to 2.71; 1523 participants; T2= 1.38, z = 2.04; P = 0.10
Ferritin
Ferritin with cluster‐RCT: MD −6.07 μg/L, 95% CI −10.66 to −1.48; 988 participants; Analysis 2.16; T2= 15.55, z = 2.59; P = 0.10 Ferritin without cluster‐RCT: MD −10.54 μg/L, 95% CI −24.00 to 2.92; 550 participants; T2= 129.36, z = 1.53; P = 0.12
Footnotes
MD: mean difference RCT: randomised controlled trial RR: risk ratio
Data and analyses
Comparison 1. Intermittent iron supplementation (alone or with any other micronutrients) versus no supplementation or placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Anaemia (All) | 11 | 3135 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.49, 0.87] |
| 1.2 Anaemia (by supplement composition) | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.2.1 Iron alone | 2 | 292 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.09, 2.13] |
| 1.2.2 Iron plus folic acid | 8 | 1871 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.52, 0.97] |
| 1.2.3 Iron plus multiple micronutrients | 3 | 972 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.25, 1.07] |
| 1.3 Anaemia (by anaemia status at baseline) | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.3.1 Anaemic | 1 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.30, 0.52] |
| 1.3.2 Mixed/Unknown | 10 | 2913 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.55, 0.93] |
| 1.4 Anaemia (by iron status at baseline): Mixed/Unknown | 11 | 3135 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.49, 0.87] |
| 1.5 Anaemia (dose of elemental iron per week in the intermittent group) | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.5.1 60 mg of iron or less per week | 5 | 1855 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.43, 1.10] |
| 1.5.2 More than 60 mg of iron per week | 7 | 1280 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.42, 0.91] |
| 1.6 Anaemia (by duration of supplementation) | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.6.1 3 months or less | 6 | 2176 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.44, 1.00] |
| 1.6.2 More than 3 months | 5 | 959 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.34, 1.04] |
| 1.7 Anaemia (by malaria endemicity) | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.7.1 No malaria/Unknown | 9 | 2937 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.41, 0.86] |
| 1.7.2 Malaria | 2 | 290 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.56, 1.30] |
| 1.8 Haemoglobin in g/L (All) | 15 | 2886 | Mean Difference (IV, Random, 95% CI) | 5.19 [3.07, 7.32] |
| 1.9 Haemoglobin in g/L (by supplement composition) | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.9.1 Iron alone | 6 | 893 | Mean Difference (IV, Random, 95% CI) | 7.16 [3.40, 10.92] |
| 1.9.2 Iron plus folic acid | 8 | 1671 | Mean Difference (IV, Random, 95% CI) | 3.56 [1.11, 6.01] |
| 1.9.3 Iron plus multiple micronutrients | 2 | 322 | Mean Difference (IV, Random, 95% CI) | 7.94 [2.37, 13.52] |
| 1.10 Haemoglobin in g/L (by anaemia status at baseline) | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.10.1 Anaemic | 3 | 439 | Mean Difference (IV, Random, 95% CI) | 7.21 [3.05, 11.37] |
| 1.10.2 Mixed/Unknown | 12 | 2447 | Mean Difference (IV, Random, 95% CI) | 4.71 [2.30, 7.13] |
| 1.11 Haemoglobin in g/L (by iron status at baseline) | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.11.1 Iron deficient | 1 | 87 | Mean Difference (IV, Random, 95% CI) | 4.80 [1.42, 8.18] |
| 1.11.2 Mixed/Unknown | 14 | 2725 | Mean Difference (IV, Random, 95% CI) | 5.59 [3.47, 7.72] |
| 1.12 Haemoglobin in g/L (by dose of elemental iron per week in the intermittent group) | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.12.1 60 mg of iron or less per week | 6 | 971 | Mean Difference (IV, Random, 95% CI) | 5.21 [2.06, 8.36] |
| 1.12.2 More than 60 mg of iron per week | 10 | 1915 | Mean Difference (IV, Random, 95% CI) | 5.24 [2.43, 8.04] |
| 1.13 Haemoglobin in g/L (by duration of supplementation) | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.13.1 3 months or less | 7 | 1387 | Mean Difference (IV, Random, 95% CI) | 6.37 [3.37, 9.37] |
| 1.13.2 More than 3 months | 8 | 1499 | Mean Difference (IV, Random, 95% CI) | 3.95 [1.28, 6.63] |
| 1.14 Haemoglobin in g/L (by malaria endemicity) | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.14.1 No malaria/Unknown | 12 | 2389 | Mean Difference (IV, Random, 95% CI) | 5.63 [3.18, 8.09] |
| 1.14.2 Malaria | 3 | 497 | Mean Difference (IV, Random, 95% CI) | 3.04 [0.52, 5.56] |
| 1.15 Iron deficiency (All) | 3 | 624 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.24, 1.04] |
| 1.16 Ferritin in µg/L (All) | 7 | 1067 | Mean Difference (IV, Random, 95% CI) | 7.46 [5.02, 9.90] |
| 1.17 Ferritin in µg/L (by supplement composition) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.17.1 Iron alone | 3 | 291 | Mean Difference (IV, Random, 95% CI) | 6.01 [3.89, 8.13] |
| 1.17.2 Iron plus folic acid | 3 | 455 | Mean Difference (IV, Random, 95% CI) | 5.87 [3.23, 8.52] |
| 1.17.3 Iron plus multiple micronutrients | 2 | 321 | Mean Difference (IV, Random, 95% CI) | 11.05 [2.94, 19.17] |
| 1.18 Ferritin in µg/L (by anaemia status at baseline) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.18.1 Anaemic | 2 | 309 | Mean Difference (IV, Random, 95% CI) | 6.17 [4.47, 7.88] |
| 1.18.2 Mixed/Unknown | 5 | 758 | Mean Difference (IV, Random, 95% CI) | 9.15 [4.36, 13.95] |
| 1.19 Ferritin in µg/L (by iron status at baseline) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.19.1 Iron deficient | 1 | 87 | Mean Difference (IV, Random, 95% CI) | 5.79 [3.55, 8.03] |
| 1.19.2 Mixed/Unknown | 6 | 980 | Mean Difference (IV, Random, 95% CI) | 8.32 [4.97, 11.66] |
| 1.20 Ferritin in µg/L (by dose of elemental iron per week in the intermittent group) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.20.1 60 mg of iron or less per week | 3 | 269 | Mean Difference (IV, Random, 95% CI) | 12.37 [7.06, 17.69] |
| 1.20.2 More than 60 mg of iron per week | 5 | 798 | Mean Difference (IV, Random, 95% CI) | 6.60 [4.30, 8.91] |
| 1.21 Ferritin in µg/L (by duration of supplementation) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.21.1 3 months or less | 3 | 518 | Mean Difference (IV, Random, 95% CI) | 8.32 [4.38, 12.26] |
| 1.21.2 More than 3 months | 4 | 549 | Mean Difference (IV, Random, 95% CI) | 6.31 [2.82, 9.81] |
| 1.22 Ferritin in µg/L (by malaria endemicity) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.22.1 No malaria/Unknown | 5 | 895 | Mean Difference (IV, Random, 95% CI) | 7.74 [4.79, 10.69] |
| 1.22.2 Malaria | 2 | 172 | Mean Difference (IV, Random, 95% CI) | 6.79 [0.48, 13.10] |
| 1.23 Iron deficiency anaemia (All) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.24 All cause morbidity (All) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.25 Diarrhoea | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.26 Any adverse side effects | 3 | 630 | Risk Ratio (M‐H, Random, 95% CI) | 1.98 [0.31, 12.72] |
| 1.27 Adherence | 2 | 417 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.96, 1.02] |
| 1.28 Prevalence of malaria parasitaemia | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.29 Any malaria parasitaemia (Incidence rate; per 1000 person months) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.30 High density malaria parasitaemia (parasites 200/wbc) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.31 Clinical malaria | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 2. Intermittent iron supplementation versus daily iron supplementation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Anaemia (All) | 8 | 1749 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.93, 1.29] |
| 2.2 Anaemia (by supplement composition) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.2.1 Iron alone | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.97, 1.99] |
| 2.2.2 Iron plus folic acid | 4 | 861 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.81, 1.30] |
| 2.2.3 Iron plus multiple micronutrients | 1 | 198 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.30, 2.46] |
| 2.3 Anaemia (by anaemia status at baseline) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.3.1 Anaemic | 2 | 270 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.76, 1.16] |
| 2.3.2 Mixed/Unknown | 6 | 1479 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [1.01, 1.47] |
| 2.4 Anaemia (by iron status at baseline): Mixed/Unknown | 7 | 1629 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.01, 1.45] |
| 2.5 Anaemia (by dose of elemental iron per week in the intermittent group) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.5.1 60 mg of iron or less per week | 4 | 614 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.82, 1.85] |
| 2.5.2 More than 60 mg of iron per week | 5 | 1135 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.85, 1.35] |
| 2.6 Anaemia (by duration of supplementation) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.6.1 3 months or less | 4 | 631 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.77, 1.16] |
| 2.6.2 More than 3 months | 4 | 1118 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.99, 1.54] |
| 2.7 Anaemia (by malaria endemicity) | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.7.1 No malaria/Unknown | 7 | 1629 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.01, 1.45] |
| 2.7.2 Malaria | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.73, 1.14] |
| 2.8 Haemoglobin in g/L (All) | 10 | 2127 | Mean Difference (IV, Random, 95% CI) | 0.43 [‐1.44, 2.31] |
| 2.9 Haemoglobin in g/L (by supplement composition) | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.9.1 Iron alone | 4 | 671 | Mean Difference (IV, Random, 95% CI) | 0.31 [‐1.15, 1.78] |
| 2.9.2 Iron plus folic acid | 4 | 1138 | Mean Difference (IV, Random, 95% CI) | 0.39 [‐4.18, 4.96] |
| 2.9.3 Iron plus multiple micronutrients | 2 | 318 | Mean Difference (IV, Random, 95% CI) | 0.84 [‐1.08, 2.76] |
| 2.10 Haemoglobin in g/L (by anaemia status at baseline) | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.10.1 Anaemic | 4 | 804 | Mean Difference (IV, Random, 95% CI) | 2.82 [1.56, 4.09] |
| 2.10.2 MIxed/Unknown | 6 | 1323 | Mean Difference (IV, Random, 95% CI) | ‐1.14 [‐3.15, 0.87] |
| 2.11 Haemoglobin in g/L (by iron status at baseline) | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.11.1 Iron deficient | 1 | 21 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐7.94, 5.94] |
| 2.11.2 Mixed/Unknown | 8 | 1986 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐1.77, 2.49] |
| 2.12 Haemoglobin in g/L (by dose of elemental iron per week in the intermittent group) | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.12.1 60 mg of iron or less per week | 6 | 843 | Mean Difference (IV, Random, 95% CI) | 1.14 [‐0.34, 2.62] |
| 2.12.2 More than 60 mg of iron per week | 5 | 1284 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐3.44, 2.76] |
| 2.13 Haemoglobin in g/L (by duration of supplementation) | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.13.1 3 months or less | 7 | 1059 | Mean Difference (IV, Random, 95% CI) | 1.36 [0.19, 2.53] |
| 2.13.2 More than 3 months | 3 | 1068 | Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐5.41, 3.98] |
| 2.14 Haemoglobin in g/L (by malaria endemicity) | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.14.1 No malaria/Unknown | 10 | 2416 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐1.65, 1.98] |
| 2.14.2 Malaria | 1 | 120 | Mean Difference (IV, Random, 95% CI) | 2.00 [‐1.40, 5.40] |
| 2.15 Iron deficiency (All) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.16 Ferritin in µg/L (All) | 4 | 988 | Mean Difference (IV, Random, 95% CI) | ‐6.07 [‐10.66, ‐1.48] |
| 2.17 Ferritin in µg/L (by duration of supplementation) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.17.1 3 months or less | 2 | 219 | Mean Difference (IV, Random, 95% CI) | ‐17.42 [‐23.44, ‐11.41] |
| 2.17.2 More than 3 months | 2 | 769 | Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐3.59, 1.48] |
| 2.18 Ferritin in µg/L (by anaemia status at baseline) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.18.1 Anaemic | 1 | 331 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.73, 0.93] |
| 2.18.2 Mixed/Unknown | 3 | 657 | Mean Difference (IV, Random, 95% CI) | ‐11.32 [‐22.61, ‐0.02] |
| 2.19 Ferritin in µg/L (by iron status at baseline) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.19.1 Iron deficient | 1 | 21 | Mean Difference (IV, Random, 95% CI) | ‐14.80 [‐22.99, ‐6.61] |
| 2.19.2 Mixed/Unknown | 3 | 967 | Mean Difference (IV, Random, 95% CI) | ‐3.80 [‐8.08, 0.47] |
| 2.20 Ferritin in µg/L (by dose of elemental iron per week in the intermittent group) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.20.1 60 mg or iron or less per week | 2 | 123 | Mean Difference (IV, Random, 95% CI) | ‐16.29 [‐23.09, ‐9.48] |
| 2.20.2 More than 60 mg of iron per week | 3 | 865 | Mean Difference (IV, Random, 95% CI) | ‐2.08 [‐5.44, 1.29] |
| 2.21 Ferritin in µg/L (by supplement composition) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.21.1 Iron alone | 1 | 21 | Mean Difference (IV, Random, 95% CI) | ‐14.80 [‐22.99, ‐6.61] |
| 2.21.2 Iron plus folic acid | 2 | 769 | Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐3.59, 1.48] |
| 2.21.3 Iron plus multiple micronutrients | 1 | 198 | Mean Difference (IV, Random, 95% CI) | ‐18.50 [‐27.37, ‐9.63] |
| 2.22 Ferritin in µg/L (by malaria endemicity): No malaria/Unknown | 4 | 988 | Mean Difference (IV, Random, 95% CI) | ‐8.27 [‐16.21, ‐0.32] |
| 2.23 Diarrhoea | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.24 Any adverse side effects | 6 | 1166 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.21, 0.82] |
| 2.25 Depression | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.26 Adherence | 4 | 507 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.99, 1.09] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Agarwal 2003 (C).
| Study characteristics | ||
| Methods |
Design: 3‐arm, cluster‐randomised trial Unit of randomisation: class; "As school teachers did not agree to randomization at the individual girl level, the randomization was done at the class section level for the 60 class sections (all class sections taken)" (quote) |
|
| Participants |
Setting/location: 4 government senior secondary schools (all of these schools cater to the middle socioeconomic group population) in North‐East Delhi, India Sample size: 2088 girls Age range: 10‐17 years Baseline prevalence of anaemia: ~ 48% Inclusion criteria: secondary school girls aged 10‐17 years old Exclusion criteria: girls with haemoglobin < 7.0 g/dL |
|
| Interventions |
Intervention: 60 class sections were allocated to 1 of 3 groups.
Length of the intervention: 100 days (we did not consider the second period in which group 1 and 3 received supplementation) |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: August 1996 Study end date: February 1999 Funding source: UNICEF, Delhi Conflicts of interest: Not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: randomisation was done at the class section level for 60 class sections. Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Comment: not mentioned; however, since randomisation was performed at class section level, selection bias at individual level was unlikely |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: not described for participants, personnel nor outcome assessors; however, seems unlikely to have been blinded, and no placebo was used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 7 girls in the daily administered group during the second week of intervention complained of gastric side effects and requested not to continue in the study and were excluded |
| Selective reporting (reporting bias) | High risk | Comment: girls with haemoglobin < 70 g/L (0.3%) were eliminated from the analysis. Plasma ferritin and C‐reactive proteins (CRP) were estimated in every tenth girl of the study groups; it is unclear how each girl was selected for these analyses. Data not available for the second measurement |
| Other bias | Low risk | Comment: appears to be free of other bias |
Ahmed 2001.
| Study characteristics | ||
| Methods |
Design: 2 × 2, randomised, double‐blind, placebo‐controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: garment factories in Dhaka City, Bangladesh Sample size: 480 postmenarchal, non‐pregnant teenagers Age range: 14–19 years Baseline prevalence of anaemia: ~ 90% Inclusion criterion: haemoglobin concentration between 80 and 120 g/L (anaemic) Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 4 groups.
All groups received weekly supplementation. Length of the intervention: 12 weeks For the purposes of this review, we combined groups 3 and 4, only presenting them separately for the subgroup analysis by nutrient. We compared the combined group with group 1. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: March 1998 Study end date: September 1998 Funding source: supported by a grant from the Department for International Development, UK. Beximco Pharmaceutical Company, Dhaka, Bangladesh, provided the iron and folate preparation and the Opsonin Pharmaceutical Company, Barisal, Bangladesh, provided the vitamin A preparation. Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants were randomly allocated to 1 of the study groups. Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Comment: an independent person coded the preparations and the code was not broken until all data had been entered into the computer |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants, personnel and outcome assessors were not aware of the treatment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 289 out of 480 (60%) participants completed the study and the losses were unbalanced among groups: 41%, 44%, 38% and 35% for groups 1, 2, 3, & 4, respectively. Participants were lost to follow‐up for the following reasons: 75% left their job or moved to another factory; 3% became pregnant; 5% refused to give a second blood sample; 12% were absent on the day of blood collection; and 5% did not take the supplements for the full 12‐week supplementation period |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Unclear risk | Comment: some variability in the administration of the supplements, depending on the factory management. In some factories, supplements were given before lunch and in some they were given after lunch. Many participants came to work after having eaten little or no breakfast and ate only a small lunch. Distribution of mild, moderate and severe anaemia not shown |
Angeles‐Agdeppa 1997.
| Study characteristics | ||
| Methods |
Design: 3‐arm, randomised, double‐blind, placebo‐controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: governmental senior high schools in East Jakarta, Indonesia Sample size: 363 girls Age range: 14‐18 years Baseline prevalence of anaemia: 21% Inclusion criterion: presence of regular menstruation Exclusion criteria: apparently none |
|
| Interventions | Participants were allocated to 1 of 4 groups.
Length of the intervention: 12 weeks For the purposes of the review, we combined groups 2 and 3, splitting them only for the subgroup analysis by dose. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: 1995 Study end date: 1995 Funding source: supported by Kimia Farma, Jakarta, Indonesia, and the German‐Indonesian Technical Cooperation (project number 85.2534.1‐01.100) Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants were randomly selected and then randomly assigned to 1 of the study groups. Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned, but study had a double‐masked placebo design |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants and personnel were not aware of the treatment; outcome assessors were not described but likely did not know the treatments. Supplements and placebos had the same red colour and shape, and were not distinguishable by sight |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 75% of the participants completed the study and the losses were unbalanced among study groups: 30%, 24%, 30%, 19% for groups 1, 2, 3, & 4, respectively |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Unclear risk | Comment: intervention supervised during the first 8 weeks. During weeks 9‐12 the supplements were provided on a take‐home basis after the girls had received careful instruction on tablet intake (because the last 4 weeks of supplementation fell in the Muslim fasting month). Distribution of mild, moderate, and severe anaemia not shown |
Beasley 2000.
| Study characteristics | ||
| Methods |
Design: 2‐arm, randomised, single‐blind, controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: rural area of Muheza District in villages of Misongeni, Ubembe and Kilometa Saba, Tanzania Sample size: 234 females Age range: 12‐18 years Baseline prevalence of anaemia: 27% had a haemoglobin < 110 g/L Inclusion criteria:
Exclusion criterion: haemoglobin concentration lower than 70 g/L |
|
| Interventions | Participants were allocated to 1 of 2 groups.
Both groups were treated for infection with albendazol before the intervention. Length of the intervention: 16 weeks, where supplementation was given at intervals of "at least once a week" |
|
| Outcomes |
|
|
| Notes |
Comments: Malaria is holo‐endemic in the study area. Study start date: April 1996 Study end date: August 1996 Funding source: support from the Wellcome Trust and the Department for International Development, UK Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: randomisation took place before anthelmintic treatment. Groups were matched for intensity of infection with hookworm and S. haematobium. Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: unclear for participants (although a control was used, it is unclear whether pills had the same appearance); personnel were aware of the treatment; outcome assessors did not know the treatment group |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: of the girls included in the study, 119 (51% of those recruited) received 12 doses of iron or control treatment and completed all follow‐up measures. It is unclear why children dropped out of the study or failed to receive all 12 doses of treatment |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Unclear risk | Comment: control was vitamin B12, which could have potentially improved anaemia status. However, macrocytosis was observed in only 8% of blood films taken at baseline. Distribution of mild, moderate, and severe anaemia not shown |
Dos Santos 1999.
| Study characteristics | ||
| Methods |
Design: 2‐arm, randomised, blinded trial Unit of randomisation: individual level |
|
| Participants |
Location/setting: low‐income community in the city of Recife, Pernambuco, Brazil Sample size: 193 women Age range: 15‐45 years Baseline prevalence of anaemia: not available; all were anaemic with haemoglobin between 75 g/L and 119 g/L Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 2 groups.
Length of the intervention: 12 weeks |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: not available Study end date: not available Funding source: not available Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: women were randomly allocated to the treatments by drawing of lots |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants were aware of the treatments; personnel staff in charge of haematological measurements did not know the study hypothesis, objectives and treatments received by the participants; not described for outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 150 out of 187 (80.2%) participants completed the study but the losses were unbalanced among groups; 26.0% and18.5% for groups 1 & 2, respectively |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: no evidence of other bias |
Februhartanty 2002.
| Study characteristics | ||
| Methods |
Design: 3‐arm, single‐blind, community trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: junior high schools in Kupang, East Nusa Tenggara, in the eastern part of Indonesia Sample size: 150 postmenarchal adolescent girls, students from 2 different public high schools. 100 were selected from 1 school and allocated randomly to placebo or weekly groups and a further 50 adolescent student girls recruited at random from a different public high school and allocated to the menstruation group Age range: ~ 14‐15 years Baseline prevalence of anaemia: 58% Inclusion criteria: postmenarchal adolescent girls from two different high schools located in relatively similar urban areas Exclusion criteria: none stated |
|
| Interventions | Participants were allocated to 1 of 3 groups.
Length of the intervention: 16 weeks For the purposes of this review, we compared groups 1 and 2 only. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: August 1998 Study end date: December 1998 Funding source: SEAMEO‐TROPMED Regional Center for Community Nutrition, Jakarta Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants were allocated randomly only to placebo or weekly groups. Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants were not aware of treatments; not described for personnel or outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: final data set consisted of 48 participants in each study group (4% dropout per group). Common reasons for dropping out were refusal to undergo blood collection, absent from class on the day of blood collection, and transfer to another school |
| Selective reporting (reporting bias) | Unclear risk | Comment: after excluding extreme values (serum ferritin changes of more than 50 μg/L), a complete data set of serum ferritin levels covered 34 participants in the placebo group and 31 participants in the weekly group |
| Other bias | High risk | Comment: higher prevalence of anaemia in the weekly group. Distribution of mild, moderate, and severe anaemia not shown |
Gilgen 2001.
| Study characteristics | ||
| Methods |
Design: 4‐arm, randomised, double‐blind trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: North‐East Bangladesh Sample size: 553 non‐pregnant and non‐breastfeeding tea pluckers Age range: 14‐66 years of age (mean age = 39.6 years) Baseline prevalence of anaemia: 85.7% Inclusion criteria: female tea pluckers, non‐pregnant and non‐breastfeeding Exclusion criteria: pregnant and breastfeeding women |
|
| Interventions | Participants were allocated to 1 of 4 groups.
Length of the intervention: 24 weeks For the purposes of this review, we only compared groups 1 and 4. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: November 1995 Study end date: March 1997 Funding source: UNICEF and The Nestle Foundation. D Gilgen received bursaries from Lucy Cavendish College, Cambridge, the Cambridge Philosophical Society and the University of Cambridge Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: participants were randomly assigned to 1 of the study groups. The random number generator in SPSS (Version 7.5) was used to create 4 groups of equal size and the process was repeated until there was no statistically significant difference between the randomised groups in mean age, years of plucking experience, productivity of the previous plucking season, haemoglobin and ferritin values, and prevalence and egg counts of Ascaris, Trichuris and hookworms. |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: study described as double‐blind. Participants and personnel were not aware of the treatments; not described for outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: not mentioned |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: no evidence of other bias |
Gonzalez‐Rosendo 2002.
| Study characteristics | ||
| Methods |
Design: 3‐arm, randomised clinical trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: 15 public schools from rural areas in Morelos, Mexico Sample size: 637 adolescents girls, mixed anaemic and non‐anaemic Age range: 12‐18 years Baseline prevalence of anaemia: 28% Inclusion criteria: adolescent girls signed‐up in the selected schools Exclusion criteria: adolescents diagnosed with gastritis or taking supplements |
|
| Interventions | Participants were allocated to 1 of 3 groups.
Length of the intervention: 16 weeks For the purposes of this review, we compared groups 1 and 2 only. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: not available Study end date: not available Funding source: not available Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: participants were randomly assigned to either the weekly or daily group by using a computer‐generated random sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: participants, personnel and outcome assessors were aware of the treatments |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: not described; apparently there were no losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Unclear risk | Comment: distribution of mild, moderate, and severe anaemia not shown |
Gupta 2014.
| Study characteristics | ||
| Methods |
Design: 3‐arm, randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: 9 selected schools in Shimla district of Himachal Pradesh, India Sample size: 331 adolescent girls with mild to moderate anaemia Age range: aged 10‐19 years Baseline prevalence of anaemia: not available Inclusion criteria: anaemic adolescent girls from selected schools Exclusion criteria: refusal to participate |
|
| Interventions | Participants were allocated to 1 of 3 groups.
Length of the intervention: 1 year For the purposes of this review, we combined groups 1 and 2 to make a single pair‐wise comparison with group 3. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: not available Study end date: not available Funding source: Indian Council of Medical Research, New Delhi Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: study girls were assigned to the 3 intervention groups by lottery method |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: participants, personnel and outcome assessors aware of the treatments; iron‐folic acid tablets were the same for the 3 intervention groups |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: not described; apparently there were no losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | High risk | Comment: missing information on self‐reported side effects (vomiting, loose stools, and constipation) that was recorded and is not shown by intervention groups. Distribution of mild, moderate, and severe anaemia not shown |
Hall 2002 (C).
| Study characteristics | ||
| Methods |
Design: 2‐arm, cluster‐randomised trial Unit of randomisation: school level (60 schools, 30 per arm; approximately 20 randomly selected children (10 boys and 10 girls) in each school) |
|
| Participants |
Setting/location: rural informal community schools in the Kolondieba district of Mali, Africa Sample size: 552 girls Age range: 6‐19 years (mean age = 11.4 years) Baseline prevalence of anaemia: ~ 55% Inclusion criteria: children that could read and write (for a separate study of educational achievements) Exclusion criterion: any child with severe anaemia (haemoglobin = 80 g/L or lower) |
|
| Interventions | Schools were allocated to 1 of 2 groups.
Length of the intervention: 10 weeks |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: January 2000 Study end date: not available Funding source: Save the Children, USA, and Helen Keller International, Mali Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: 60 schools were randomly assigned to either a treatment or a comparison group by using a computer‐generated random number list (information communicated by the author) |
| Allocation concealment (selection bias) | Low risk | Comment: not reported; however, since the intervention was allocated at school level, selection bias at individual level was unlikely |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: not reported for participants, personnel or outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 93% children followed up |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Unclear risk | Comment: distribution of moderate and mild anaemia not shown |
Jalambo 2018.
| Study characteristics | ||
| Methods |
Design: 3‐arm, randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: secondary schools in Gaza. 1 or 2 class(es) were selected randomly from grades 10, 11, and 12 in the selected schools, according to the population of the governorate Sample size: 131 adolescent school girls with iron deficiency or iron deficiency anaemia Age range: 15‐19 years Baseline prevalence of anaemia: not available Inclusion criteria: unmarried and non‐pregnant adolescent girls with iron deficiency and iron‐deficiency anaemia (mild and moderate) Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 3 groups.
Length of the intervention: 3 months For the purposes of this review, we used groups 1 and 3. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: October 2015 Study end date: April 2016 Funding source: none Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: schools, grades and girls were randomly selected; however, the method was not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: not reported for participants, personnel or outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: not described; apparently there were no losses to follow‐up |
| Selective reporting (reporting bias) | Low risk | Comment: apparently there was no selective reporting |
| Other bias | Low risk | Comment: distribution of moderate and mild anaemia not shown |
Jayatissa 1999 (C).
| Study characteristics | ||
| Methods |
Design: 3‐arm, double‐blinded, placebo‐controlled clinical trial Unit of randomisation: class level |
|
| Participants |
Setting/location: schools in the district of Colombo, Sri Lanka Sample size: 690 adolescents Age range: 10‐17 years (mean age = 11.4 years) Baseline prevalence of anaemia: 21.1% Inclusion criteria: adolescent girl from each grade from years 6 to 10 was randomly selected Exclusion criteria:
|
|
| Interventions | Classes were allocated to 1 of 4 groups.
Length of the intervention: 8 weeks |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: not available Study end date: not available Funding source: WHO representative and its staff in Sri Lanka Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: it is stated that treatments were randomly allocated by classes. Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Comment: not reported; however, since the intervention was allocated at class level, selection bias at individual level is unlikely |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: supplements and placebos had the same colour and shape and were not distinguishable by sight. Girls, teachers, and interviewers were not aware of differences among the treatment regimens |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: dropout rate was 4.5%. The reasons for dropping out were side effects (16 girls, 52%), leaving school (10 girls, 32%), or doctor’s advice not to take the tablet with other treatment (5 girls, 16%) |
| Selective reporting (reporting bias) | Unclear risk | Comment: ferritin samples were taken from a randomly selected subsample |
| Other bias | Low risk | Comment: study appears to be free of other bias |
Joshi 2013.
| Study characteristics | ||
| Methods |
Design: 2‐arm, randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: Urban Health and Training Centre in urban slum area in India Sample size: 120 anaemic adolescent girls. All girls who visited the Urban Health and Training Centre during the study period were interviewed as per pre‐tested proforma and had their haemoglobin assessed. Those with haemoglobin < 12 g/dL and who consented were included in the study. Age range: 10‐19 years Baseline prevalence of anaemia: all were anaemic; 61.6% = mild anaemic, 36.6% = moderate anaemic, 1.66% = severe anaemic Inclusion criteria: adolescent girls with haemoglobin < 12 g/dL consenting for this study Exclusion criteria:
|
|
| Interventions | All included participants were dewormed at the start of the study and 15 days later with 400 mg of albendazole, and given related health education in separate sessions. Girls were randomly allocated to 1 of 2 groups.
Length of the intervention: 3 months |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: June 2011 Study end date: October 2012 Funding source: not available Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: randomisation done using computer‐generated block randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned. Every adolescent girl with haemoglobin < 12 g/dL selected for inclusion in the study was allocated randomly to either group by a laboratory technician until the required quota of 60 participants in each group was reached |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: not described; apparently there were no losses to follow‐up |
| Selective reporting (reporting bias) | High risk | Comment: missing information on compliance at individual level, which was recorded through home visits and postintervention interviews |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
Kianfar 2000.
| Study characteristics | ||
| Methods |
Design: 2 × 4, randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: 4 high schools in urban areas of Zahedan and Rasht, Iran Sample size: 523 female adolescents (selected from students in grades 1‐3) Age range: not reported (mean age = 16.1 years) Baseline prevalence of anaemia: 48.5% Inclusion criterion: written consent secured from participants' families Exclusion criteria: no exclusion criteria listed |
|
| Interventions | Participants were allocated to 1 of 4 groups.
Length of the intervention: 3 months For the purposes of this review, we combined groups 2 and 3, only presenting their individual results in the subgroup analysis by scheme. |
|
| Outcomes |
Data in each group reported only by anaemia status (anaemic, non‐anaemic), so we combined them within each group to include the trial's information. |
|
| Notes |
Comments:
Study start date: 1996‐1997, during a 3‐month period Study end date: 1996‐1997, during a 3‐month period Funding source: Undersecretariat for Research, Ministry of Health and Medical Education, Chancellors of Zahedan and Rasht Medical Universities, as well as Miss A Houshiar‐Rad and F Nasseri, and Mr A Rashidi M Kar Andish and M Karajibani Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants stratified by anaemia status were randomly allocated to the groups. Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants were aware of the treatment; staff did not know the treatment group; not reported for outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 88/92 (95.6%), 108/112 (96.4%), 168/171 (98.2%), 145/148 (97.9%) of the participants finished the study in groups 1, 2, 3, and 4, respectively. |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
Leenstra 2009.
| Study characteristics | ||
| Methods |
Design: 2 × 2, randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: 10 schools in the City of Kisumu in Nyanza Province, western Kenya Sample size: 279 non‐pregnant school girls with mild‐to‐moderate anaemia (haemoglobin < 70 g/L but > 120 g/L) Age range: 12‐18 years Baseline prevalence of anaemia: ~ 30% (iron deficiency = ~ 40%) Inclusion criteria: school girls aged 12–18 years, from public primary schools Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 4 groups.
Length of the intervention: 5 months For the purposes of this review, we compared groups 2 and 4 only. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: April 1998 Study end date: November 1998 Funding source: The Netherlands Foundation for the Advancement of Tropical Research (WOTRO) Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: balanced block randomisation (block size 12). Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Comment: placebo‐controlled trial. Individual packs were left for girls in the study schools. Active and placebo supplements were manufactured by Laboratory and Allied Limited (Nairobi, Kenya) and the key was only revealed after completion of the study. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants, personnel, and outcome assessors were not aware of the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 249 out of 279 participants completed the study (89%). Loss to follow‐up appeared balanced across groups and reasons were explained. Analyses were done on an intention‐to‐treat basis |
| Selective reporting (reporting bias) | Unclear risk | Comment: data on several outcomes described as non‐significant but not shown (side effects including vomiting and diarrhoea) |
| Other bias | Unclear risk | Comment: groups appeared similar at baseline. Most of the results for the 4 randomised groups were presented in graphs which were difficult to interpret (and have not been included in our data and analysis tables). Data on several outcomes were described as non‐significant but were not shown (side effects, including vomiting and diarrhoea). Placebo figures were not reported. Distribution of mild, moderate, and severe anaemia not shown |
Mozaffari 2010 (C).
| Study characteristics | ||
| Methods |
Design: 2‐arm, cluster‐randomised, community‐based supplementation trial Unit of randomisation: school level |
|
| Participants |
Setting/location: high schools in Yazd City in central Iran Sample size: 200 high school girls Age range: 14‐16 years Baseline prevalence of anaemia: ~ 13% Inclusion criteria: first grade adolescent girls in each high school Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 2 groups:
Length of the intervention: 16 weeks For the purposes of this review, we analysed both groups. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: October 2007 Study end date: November 2008 Funding source: Department of Research Administration, Shahid Sadoughi University of Medical Sciences, Yazd, Iran Conflicts of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: study described as a community‐based randomised trial. Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Comment: not mentioned; however, since this is a cluster trial, selection bias at individual level is unlikely |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: participants, personnel, and outcome assessors were aware of the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 4 girls from the iron‐supplemented group and 3 girls from the non‐supplemented group dropped out on grounds of travel, illness, or some personal reasons |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
Muro 1999 (C).
| Study characteristics | ||
| Methods |
Design: 3‐arm, cluster‐randomised, community‐based, controlled trial Unit of randomisation: school level |
|
| Participants |
Setting/location: 5 schools in Dar‐es‐Salaam, Tanzania Sample size: 237 adolescent girls Age range: 14‐17 years Baseline prevalence of anaemia: ~ 48% Inclusion criteria:
Exclusion criterion: girls suffering from infection with fever at the time of the interview |
|
| Interventions | Participants were allocated to 1 of 3 groups.
Length of the intervention: 8 weeks For the purposes of this review, we compared groups 2 and 3 only. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: August 1996 Study end date: November 1996 Funding source: not available Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: each group should have contained a similar number of girls. However, this goal was not reached, because after the schools had been randomly assigned to the 3 groups, the parents of the girls in school 4, who were assigned to receive iron supplementation without communication, did not approve of their daughters receiving iron tablets. The girls from this school were added to the non‐intervention group |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: participants and personnel were aware of the treatment; outcome assessors seemed to be aware of the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 100% of participants finished the treatment |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
Nguyen 2008.
| Study characteristics | ||
| Methods |
Design: 4‐arm, randomised double‐blind, controlled trial Unit of randomisation: individual level |
|
| Participants |
Settinglocation: Concepción, Chiquirichapa, in the western highlands of Guatemala Sample size: 459 healthy women Age range: 15 to 49 years Baseline prevalence of anaemia: prevalent, but percentage not reported Inclusion criteria: non‐pregnant, non‐lactating, anaemic (mild or moderate) women Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 4 groups.
The weekly‐dose groups received 6 placebos and 1 active pill on the 3rd day of the week. Daily records were kept to track the participants’ health. Length of the intervention: 12 weeks For the purposes of this review, we combined groups 1 and 2 and compared them with groups 3 and 4, which we also combined. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: March 2006 Study end date: June 2006 Funding source: not available Conflict of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer‐generated random numbers used to assigned women to 1 of the treatment groups |
| Allocation concealment (selection bias) | Low risk | Comment: code allocation was kept secure at Emory University and was only revealed after completion of the study |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: participants, personnel and outcome assessors were not aware of the treatment. All supplements were identical in appearance and taste, and were coded with lot numbers at the factory, corresponding to 1 of 4 treatment arms |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Comment: of the 459 women randomised to 1 of the treatment groups, 369 completed the 12‐week study protocol:
|
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
Rezaeian 2014.
| Study characteristics | ||
| Methods |
Design: 2‐arm, randomised, blinded, clinical controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: high school students in Shirvan, Khorasan, Iran Sample size: 200 female high school students (anaemic and not anaemic); enrolled from the general population Age range: 14‐18 years Baseline prevalence of anaemia: not available Inclusion criteria: anaemic and non‐anaemic girls Exclusion criteria: students with high levels of haemoglobin (≥ 16 g/dL) |
|
| Interventions | Participants were allocated to 1 of 2 groups:
Length of the intervention: 16 weeks |
|
| Outcomes |
|
|
| Notes |
Comments: distribution of the supplements, compliance and side effects were not mentioned. Study start date: not available Study end date: not available Funding source: Vice Chancellor of the Islamic Azad University of Bojnourd, Iran Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: the high school was selected using a simple draw method from the 4 female high schools in Shirvan, Khorasan, Iran, that enrolled students from the general population. Simple draw method was also used to determine whether the morning of afternoon shift was assigned as the control or intervention group. Using systematic random sampling, 25 students were selected from each age group |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: the examiner did not know whether the individual tested belonged to the case or control group. The person in charge of the data analysis did not know whether the data belonged to the control or case group. Although the participants were aware of whether they had or had not consumed the supplement, the nature of the study indicators used were objective or approximately objective (blood tests and attention scores), so it is unlikely that the participant's awareness of the consumption of the supplement would have had a major effect on the results |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: missing data of dropouts and withdrawals, and compliance |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: missing data on complete blood count and demographics |
Riuvard 2006.
| Study characteristics | ||
| Methods |
Design: 2‐arm, randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: Internal Medicine Department, CHU de (University Hospital of) Clermont‐Ferrand, France Sample size: 24 women Age range: 18 to 30 years Baseline prevalence of anaemia: not available Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 2 groups.
Length of the intervention: 3 months |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: not available Study end date: not available Funding source: supported, in part, by a grant from UCB Pharma (France) Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: participants were randomly assigned to 1 of the study groups with the aid of a randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: participants, personnel, and outcome assessors were aware of the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 3 participants withdrew from the study: 2 from group 1 and 1 from group 2 |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
Roschnik 2003 (C).
| Study characteristics | ||
| Methods |
Design: 2‐arm, cluster‐randomised trial Unit of randomisation: school level (40 schools) and stratified by sponsorship status |
|
| Participants |
Setting/location: 40 primary schools in the Mangochi District, Malawi Sample size: 752 boys and girls (from 1160 randomised) Age range: for 371 girls; ~ 7–8 years (standard 2 grade) and ~ 12‐15 years (standard 6 grade) Baseline prevalence of anaemia: around 54% Inclusion criteria: registered children Exclusion criteria: not available |
|
| Interventions | 371 girls were randomly allocated to 1 of 2 groups.
Length of the intervention: 15 weeks |
|
| Outcomes |
*(at school level) |
|
| Notes |
Comments:
Study start date: July 2001 Study end date: not available Funding source: not available Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: 40 primary schools in the Mangochi District were randomly divided into the intervention (1st iron group) and comparison group (2nd iron group). Each group included 10 sponsorship schools and 10 non‐sponsorship schools. Method of sequence generation not specified |
| Allocation concealment (selection bias) | Low risk | Comment: not reported; however, since the intervention was allocated at school level, selection bias at individual level is unlikely |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: not mentioned; however, as randomisation was at class level, it is unlikely that participants were blinded. Not reported for personnel or outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 1280 were randomised, 1160 had haemoglobin levels at baseline and 752 were followed up. 41.2% children lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Unclear risk | Comment: children attending sponsored schools responded better to the treatment |
Shah 2002.
| Study characteristics | ||
| Methods |
Design: 3‐arm, randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: government girls school of the Dharan Municipality, an urban foothill town in Nepal Sample size: 209 girls Age range: 11 to 18 years Baseline prevalence of anaemia: 48% Inclusion criteria: girls aged 11 to 18 years Exclusion criteria:
|
|
| Interventions | Participants were allocated to 1 of 3 groups.
Length of the intervention: 90 to 100 days (~ 14 weeks) |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: March 1998 Study end date: March 1999 Funding source: Research Committee of BP Koirala Institute of Health Sciences, Dharan Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants randomly assigned to 1 of 3 groups. Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: participants, personnel, and outcome assessors were aware of the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: of the 209 girls who met the inclusion criteria, 181 completed the study (87%); losses were balanced among groups. Severe adverse effects, non‐compliance to treatment, and non‐availability for final haematocrit measurement were listed as reasons for losses. Numbers of participants who left for each reason was not documented |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | High risk | Comment: participants in the daily regimen group were not supervised and only asked to maintain a record of the supplements consumption, while those in the weekly group were supervised by an investigator. |
Shobha 2003.
| Study characteristics | ||
| Methods |
Design: 3 × 2 randomised controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: Andhra Pradesh Social Welfare Residential School, located in Ranga Reddy district, India Sample size: 244 females Age range: 13 to 15 years Baseline prevalence of anaemia: 83% Inclusion criteria: not available Exclusion criteria: not available |
|
| Interventions | Adolescents were allocated to 1 of 2 groups.
Length of the intervention: 84 days |
|
| Outcomes |
For the purposes of this review, we pooled all girls in group 1, independently of the degree of anaemia, and did the same for group 2. *Based on initial haemoglobin levels, participants were classified as normal (higher than 120 g/L), mildly anaemic (100‐119.9 g/L), moderately anaemic (80‐99.9 g/L), or severely anaemic (80 g/L), as per the WHO standard. |
|
| Notes |
Comments:
Study start date: not available Study end date: not available Funding source: none Conflicts of interest: none stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants stratified by grade of anaemia (mild, moderate, or severe) and randomly divided into study groups. Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not mentioned |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: not mentioned for participants, personnel, or outcome assessors. However, there was no placebo for girls under the once weekly regimen (for the rest of the days), while the girls under the intermittent regimen took a tablet every day in the same school |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: not mentioned |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Unclear risk | Comment: distribution of mild, moderate, and severe anaemia not shown |
Soekarjo 2004 (C).
| Study characteristics | ||
| Methods |
Design: 4‐arm, cluster‐randomised, school‐based supplementation trial Unit of randomisation: class level |
|
| Participants |
Setting/location: 4 rural or urban schools selected from 2 districts (Bangkalan and Sampang) on the island of Madura, representing both main school types in Indonesia Sample size: 1460 postmenarchal adolescents Age range: 12‐15 years Baseline prevalence of anaemia: 22.9%‐26.1% Inclusion criteria: school students Exclusion criteria: not available |
|
| Interventions | 15 intervention schools. All children (n = 2990) received supplements and were divided into 3 groups according to their grade.
A fourth group (9 schools; n = 923) did not receive the intervention. Length of the intervention: 3 months Given that it was unclear how the 9 schools were allocated to receive no intervention, and that the 3 intervention groups were allocated at random to each intervention, we only compared groups 1 and 3. |
|
| Outcomes |
|
|
| Notes |
Comments:
Study start date: October 1996 Study end date: May 1997 Funding source: Helen Keller International in cooperation with the Ministry of Health of the Government of Indonesia as part of the GIRLS (Gizi: Intervensi Remaja Lewat Sekolah/Nutrition Intervention for Adolescents through Schools) Project Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: adolescents from 15 schools were randomly selected to receive weekly supplements, while adolescents in the other 9 schools served as controls. In each of the schools receiving supplements, each of the 3 grades was randomly allocated to receive 1 of the 3 supplementation regimens. Method of sequence generation not mentioned |
| Allocation concealment (selection bias) | Low risk | Comment: not mentioned; however, since this is a cluster trial, selection bias at individual level is unlikely |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: participants were aware of the treatment; but randomisation was done at class levels. Likely that personnel and outcome assessors were also aware of the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 4810 out of 5116 participants (96%) completed the study. Losses were mainly caused by absenteeism on several consecutive days during the end‐line data collection. There was no difference in dropout rate between the 4 groups |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
Zavaleta 2000.
| Study characteristics | ||
| Methods |
Design: 3‐arm, double‐blind, placebo‐controlled trial Unit of randomisation: individual level |
|
| Participants |
Setting/location: public secondary school in Villa El Salvador, a peri‐urban shanty town in Lima, Peru Sample size: 312 adolescent girls Age range: 12‐18 years Baseline prevalence of anaemia: ~ 19% Inclusion criteria:
Exclusion criterion: multi‐vitamin/mineral supplement intake in the last 6 months |
|
| Interventions | Participants were allocated to 1 of 3 groups.
All tablets had the same brick colour and shape. Length of the intervention: 17 weeks |
|
| Outcomes |
We were not able to use continuous data for haemoglobin because standard deviations and number of cases and controls were not reported at follow‐up. Changes in haemoglobin levels by initial anaemia status in adolescents were presented in graphs (final haemoglobin concentrations for daily, intermittent, and control groups were 123.7 g/L, 120 g/L and 110.4 g/L, respectively). |
|
| Notes |
Comments:
Study start date: August 1996 Study end date: December 1996 Funding source: not available Conflicts of interest: not available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants randomly assigned to treatments. Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Comment: all tablets had the same brick colour and shape and were distributed in coded blister packages |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Comment: all tablets looked similar and were administered in coded packages. Participants and personnel were not aware of the treatment; not described for outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: a total of 312 girls started the study and 16 (5.1%) dropped out. Of these 16, 8 moved to another school, 2 disliked the tablets, 4 complained of side effects and withdrew, and 2 were absent at the time of final evaluation |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: study appeared to be free of other bias |
AUC: area under the curve Fe: iron IFA: iron and folic acid MCH: mean corpuscular haemoglobin MCHC: mean corpuscular haemoglobin concentration MCV: mean corpuscular volume RBC: red blood cells SEAMEO‐TROPMED: Southeast Asian Ministers of Education Tropical Medicine and Public Health Network TfR: transferrin receptor UNICEF: United Nations International Children's Emergency Fund UCB: Union Chimique Belge WBC: white blood cells WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmed 2005 | Randomised, double‐blind clinical trial conducted in Bangladesh. Anaemic (haemoglobin less than 120 g/L) girls (n = 197) aged 14‐18 years old from rural schools in Dhaka District were entered into a randomised double‐blind trial and received twice‐weekly supplements of iron and folic acid or multiple micronutrients (15 micronutrients, including iron and folic acid for 12 weeks). Found that twice‐weekly multiple micronutrients supplementation for 12 weeks significantly improved the status of the micronutrients assessed, but was not more efficacious than supplementation with iron and folic acid alone in improving the haematologic status of anaemic adolescent girls. We excluded the study because the authors did not compare intermittent iron supplementation versus daily supplementation or placebo and hence it was outside the scope of this review. |
| Ahmed 2010 | Randomised, double‐blind trial conducted in Bangladesh. Anaemic adolescent girls (n = 324) aged 11‐17 years, attending rural schools, were given once‐ or twice‐weekly multiple micronutrient supplements or twice‐weekly iron‐folic acid supplements, containing 60 mg of elemental iron/dose in both supplements, for 52 weeks. Both once‐ and twice‐weekly multiple micronutrient supplements significantly improved riboflavin, vitamin A, and vitamin C status compared with iron‐folic acid supplements. Overall, once‐weekly multiple micronutrient supplements was less efficacious than twice‐weekly multiple micronutrient supplements in improving iron, riboflavin, red blood cell folate, and vitamin A levels. Micronutrient supplementation beyond 26 weeks was likely important in sustaining improved micronutrient status. We excluded the study because the authors did not compare intermittent iron supplementation versus daily supplementation or placebo and hence it was outside the scope of this review. |
| Ahmed 2012 | Randomised, double blind controlled trial with 324 adolescent girls to investigate the effect of long‐term once‐weekly and twice‐weekly UNIMMAP dose using a double dose of all nutrients except for folic acid. 3 supplementation groups: 1) double UNIMMAP dose and a placebo once weekly; 2) double UNIMMAP dose twice weekly; 3) routine standard dose of iron‐folic acid twice weekly. An equal number of 324 rural school girls aged 11‐17 years old were randomly assigned to each intervention group. Blood samples were collected at baseline, 26 and 52 weeks. MMN‐1 was found to be less effective than MMN‐2 in improving iron, vitamins A and B2 and folic acid status. Receiving MMN beyond 26 weeks showed little additional benefit in improving micronutrients status. In conclusion, given twice weekly for 26 weeks, MMN supplements improved micronutrient status effectively with no significant increase in haemoglobin concentration compared with iron‐folic acid alone in non‐anaemic adolescent Bangladeshi girls. We excluded the study because the comparison was outside the scope of this review. |
| Bansal 2016 | Community‐based, randomised, double‐blind controlled trial conducted among anaemic adolescent girls (n = 446) 11‐18 years of age. Sought to assess and compare the impact of weekly iron‐folic acid supplementation with or without vitamin B12 on reduction in prevalence of anaemia and blood concentrations of haemoglobin, ferritin, folic acid, and vitamin B12. Weekly supervised supplementation was given for 26 weeks. Group A (n = 222): iron (100 mg), folic acid (500 mcg) and placebo; Group B (n = 224): iron (100 mg), folic acid (500 mcg) and cyanocobalamin (500 mcg for 6 weeks and 15 mcg for 20 weeks). Haemoglobin, serum ferritin, folic acid and vitamin B12 levels were assessed at baseline and after intervention. A total of 373 participants completed 26 weeks of supplementation successfully. The study showed that iron‐folic acid supplementation with or without vitamin B12 was an effective method of curing anaemia. We excluded the study because the comparison was outside the scope of this review. |
| Beaton 1999 | A report based on the analysis of 22 completed trials of iron supplementation. The major objective of the analysis was to determine, to the extent possible, the situations in which the apparent efficacy of intermittent supplementation was maximised. We excluded the report because it was a review. |
| Berger 2005 | Community‐based trial in all 19 communes of the Thanh Mien district in the Hai Duong province in Hanoi, Vietnam. Women were informed by the social marketing campaign about the benefits of taking preventive iron folic‐acid supplementation before and during pregnancy, combined with improved diets. Women recruited were married, nulliparous and planning to have a child. They were allocated to 2 treatments according to their pregnancy status at baseline: daily supplements containing 60 mg of elemental iron + 250 μg (0.25 mg) of folic acid to pregnant women or weekly intervention to non‐pregnant women. We excluded the study because it was not randomised and did not have a control group. |
| Bruner 1996 | Double‐blind, placebo‐controlled clinical trial that assessed the effects of iron supplementation on cognitive function in adolescent girls (n = 716) with non‐anaemic iron deficiency. Girls who enrolled at 4 high schools in Baltimore, USA, were screened for non‐anaemic iron deficiency (serum ferritin = 12 μg/L or less with normal haemoglobin). 98 (13.7%) girls had non‐anaemic iron deficiency, 81 of whom were enrolled in the trial. Participants were randomly assigned oral ferrous sulphate (650 mg twice daily) or placebo for 8 weeks. The effect of iron treatment was assessed by questionnaires and haematological and cognitive tests, which were done before treatment started and repeated after the intervention. Authors used 4 tests of attention and memory to measure cognitive functioning. Intention‐to‐treat and per‐protocol analyses were done. Of the 81 enrolled girls with non‐anaemic iron deficiency, 78 (96%) completed the study (39 in each group). 5 girls (3 = control, 2 = treatment) developed anaemia during the intervention and were excluded from the analyses. Thus, 73 girls were included in the per‐protocol analysis. Ethnic distribution, mean age, serum ferritin concentrations, haemoglobin concentrations, and cognitive test scores of the groups did not differ significantly at baseline. Postintervention haematological measures of iron status were significantly improved in the treatment group (serum ferritin = 27.3 vs 12.1 μg/L, P < 0.001). Regression analysis showed that girls who received iron performed better on a test of verbal learning and memory than girls in the control group (P < 0.02). In this urban population of non‐anaemic, iron‐deficient adolescent girls, iron supplementation improved verbal learning and memory. We excluded the study because the authors did not compare intermittent iron supplementation versus daily supplementation or placebo and hence the study was outside the scope of this review. |
| Casey 2009 | Distribution of weekly iron and folic acid supplementation and deworming were integrated with routine health services and made available to 52,000 women. Demographic data and blood and stool samples were collected at baseline and 3‐ and 12‐month post‐implementation surveys using a population‐based, stratified, multi‐stage cluster sampling design. Authors concluded that a free, universal, weekly iron and folic acid supplementation programme with regular deworming was associated with reduced prevalence and severity of anaemia, iron deficiency, and hookworm infection when made available to Vietnamese women over a 12‐month period. We excluded the study because it was not randomised and did not have a control group. |
| Cook 1995 | Study designed to examine inhibition in absorption from iron taken on the previous day by measuring iron absorption from 50 mg of radiolabeled ferrous sulphate in 23 female volunteer participants divided into 2 groups. In the first group, a labelled ferrous sulphate supplement was given with water, and in the second group it was given with a rice‐based meal. In both groups, absorption was measured in a randomised fashion twice in each participant, once with daily and once with weekly supplementation. Those tested for daily supplementation were given an iron supplement daily for 6 days before testing whereas those tested for weekly supplementation were given no iron for 6 days before testing. When the labelled iron supplement was given with water only, absorption averaged 8.5% with daily and 9.8% with weekly administration compared with 2.3% and 2.6%, respectively, when given with food. The 13% lower absorption observed with daily administration in both groups was not statistically significant (P > 0.20). These results indicated that there was no significant absorptive advantage in giving iron less often than once daily. We excluded the study because it was not a controlled trial. |
| Crape 2005 | A social marketing programme promoting weekly iron‐folic acid supplementation improved haemoglobin levels in women of reproductive age in Cambodia. Supplementation was increasingly effective among women of higher socioeconomic status. We excluded the study because it was not randomised and did not have a control group. |
| Deshmukh 2008 | Effectiveness trial of a weekly, iron supplementation regimen through the government health system among urban slum, rural, and tribal girls of Nashik district, India. Participants were adolescent girls (14‐18 years old) who were given supplements containing 100 mg of iron and 500 μg (0.5 mg) of folic acid and were trained for three hours every day for three days. The overall prevalence of anaemia came down significantly to 54.3% from 65.3%. We excluded the study because it was not randomised and did not have a control group, and hence was outside the scope of this review. |
| Dwividi 2006 | Review of programmes in India of weekly iron supplementation to control anaemia in adolescent girls. Programmes, implemented in 13 states with varying coverage, targeted 2 different groups: girls in school and girls out of school. The objective of the review was to summarise and analyse the status/characteristics of the various adolescent anaemia programmes in India, summarise and analyse the results of the impact assessments that have already been conducted, and to estimate and analyse the costs of the programmes. From results, it was evident that weekly iron/folic acid supplementation in adolescents girls led to a marked decrease in the prevalence of anaemia. In some cases, a large long‐term impact (70%, 2 years) was reported. Reasons for the small but significant decrease in the prevalence of anaemia included low compliance and a possible multicausality of anaemia as deficiency in other vitamins and minerals or genetic causes. It could also be that a larger reduction in anaemia prevalence may be achieved only after prolonged supplementation. Supplementation programmes should continue until other sources of iron intake become available, be it from natural dietary sources or from fortified foods, or both. Programmes targeting out‐of‐school girls can be successful as the interventions targeting these girls also resulted in significant decreases in anaemia prevalence. Success factors included: ensuring compliance; counselling not only the beneficiaries but the community; ensuring continuous tablet supply and regular monitoring; among others. It is clear that if well conceived, the supplementation component of an overall package of services for the adolescent girl costs very little. We excluded this record because it was a review. |
| Horjus 2005 | Pre‐post study to assess the programme effectiveness of 2 school‐based weekly iron‐folic acid supplementation regimens: 5 months versus 8 months. In both groups, participant girls received 60 mg of elemental iron and 400 µg (0.4 mg) of folic acid. All girls received a single dose of mebendazole at the beginning of the study and at 6 months. The study found that school‐based weekly supplementation is a feasible and effective intervention to prevent seasonal drops in haemoglobin concentration and increases in anaemia prevalence. We excluded the study because it was not randomised and the comparisons did not fit the scope of this review. |
| Jackson 2003 | Randomised trial to ascertain whether short‐term supplementation with iron was effective in reducing anaemia. Assigned 608 girls with mild‐to‐moderate anaemia from high schools to 3 treatment groups. Supplementation included 60 mg of iron per week, 3500 μg (3.5 mg) of folic acid per week, iron + folic acid (same dose), and a control group. In conclusion, 8 weeks of supplements given on a weekly basis were well tolerated and caused few symptoms, and the regimen was effective in reducing anaemia by 30‐40%. We excluded the study because the control group was not randomised and included it non‐anaemic classmates (with normal haemoglobin values). |
| Joseph 2013 | To assess if weekly iron‐folic acid dose (150 mg of ferrous sulphate + 0.5 mg of folic acid along with vitamin C (100 mg)) in the workplace could reduce the prevalence of anaemia. The study setting was 7 apparel manufacturing factories and it lasted 16 weeks. A sample of 515 workers were included and given a single dose of albendazole before the supplementation period. Haemoglobin levels of a randomly‐selected sample of workers were tested before and after the intervention. Found that the workplace might be an ideal location for weekly iron supplementation to tackle anaemia effectively and possibly improve working efficiency. We excluded the study because it was not a randomised controlled trial. |
| Kätelhut 1996 | Randomised effectiveness study to investigate whether a supplement containing iron and folic acid, vitamin A, and vitamin C would be more effective than a supplement containing only iron and a smaller amount of folic acid in improving the iron status of young women. A total of 84 menstruating anaemic and non‐anaemic girls were included and randomly assigned to 2 groups. Group 1 received weekly supplements containing 60 mg of elemental iron + 500 mcg folic acid + 20,000 IU vitamin A and 60 mg ascorbic acid for 5 weeks. Group 2 received weekly supplements containing only 60 mg of elemental iron and 250 mcg of folic acid. Haemoglobin, mean cell volume, and serum ferritin increased in both groups, confirming that weekly supplementation was effective in improving iron status in a short time. We excluded the study because the comparison was outside the scope of this review. |
| López de Romaña 2006 | Cluster trial conducted in Peru among women and adolescent girls of childbearing age and children under 5 years of age, to assess the impact of a campaign on the growth of children and on anaemia among children and among women and adolescent girls of childbearing age. Weekly multi‐micronutrient supplementation was provided for 8 weeks in communities with a high prevalence of stunting; control households were selected from communities with a lower prevalence of stunting. There were no significant effects of weekly multi‐micronutrient supplementation on anaemia or growth. We excluded the study because it was not randomised. |
| Moretti 2015 | Authors conducted 3 separate studies with the aim of measuring acute iron‐induced increase in hepcidin. They used a cross‐over design study to assess iron status markers. In study 1, participants were randomly assigned to take 2 iron challenges either as a single dose or as 2 doses given on consecutive days; hepcidin response was assessed after 48 hours. In study 2, 2 single doses of 60 mg of elemental iron were administered on 2 consecutive days and, similarly hepcidin response was assessed after 48 hours. In study 3, the effect of administering 60 mg of iron twice daily during 24 hours on hepcidin levels and iron absorption was assessed. The duration of hepcidin response supported alternate days of supplementation. We excluded the study because the setting, population and intervention were outside the scope of this review. |
| Pasricha 2009 | Multi‐stage, cluster‐sampling study. A programme of weekly iron and folic acid supplementation and deworming every 4 months for all women of reproductive age living in Yen Bai province, Vietnam, was implemented by active distribution through the existing primary health structure. Women received ferrous sulphate and folic acid tablets. After 3 months, anaemia prevalence fell to 58/221 (26.2%), and the mean haemoglobin change was + 3.5 g/L (95% CI 0.9 to 6.6). We excluded the study because it was not randomised and did not have a control group, and hence was outside the scope of this review. |
| Perrin 2002 | We excluded this record because it was a commentary paper on Shah 2002. |
| Ramakrishnan 2012 | Double‐blind, randomised controlled trial with 5011 women, to evaluate whether providing additional, pre‐pregnancy, weekly iron‐folic acid or multiple micronutrient supplements improves iron status and anaemia during pregnancy and early postpartum, compared to folic acid only. Women were provided with weekly supplements containing either only 2800 mcg of folic acid (control group), 60 mg iron + 2800 mcg of folic acid, or 15 micronutrients with similar amounts of iron and folic acid. All women who became pregnant (n = 1813) in each of the 3 groups received daily supplements (60 mg of iron + 400 mcg of folic acid) through delivery. Haematological indicators were assessed at baseline (pre‐pregnancy), during pregnancy, postpartum, and in cord blood. We excluded the study because, although supplements were given during pre‐pregnancy, no outcomes on pre‐pregnancy (i.e. menstruating women) were reported, only pregnancy and postpartum. |
| Sen 2012 | Randomised, efficacy controlled trial to assess the impact of iron‐folic acid supplementation on hemanitic status and growth of school girls. The trial was conducted in primary urban schools with girls (aged 9‐13 years) only. 4 schools were randomly assigned to either treatment or control: 100 mg of elemental iron + 0.5 mg of folic acid once weekly, twice weekly, daily, and no treatment in the control group. Haemoglobin levels increased significantly in all intervention schools, with higher increases among anaemic girls. Twice‐weekly supplementation was comparable to daily supplementation with regard to impact on haemoglobin and growth, at less cost and greater feasibility. We excluded the study because it did not include menstruating girls: girls who attained their menarche (n = 18), prior to or during the study, were excluded from the analysis though they received the supplements. |
| Shah 2016 | Community‐based, cross‐sectional study in 5 tribal villages in India to describe the burden of anaemia. The study included adolescent boys (n = 127) and girls (n =117) aged 10‐19 years. They were provided weekly with iron‐folic acid supplements containing 100 mg of elemental iron and 500 mcg of folic acid, along with the distribution of abendazole tablets for bi‐annual deworming. Awareness sessions were conducted for mothers and adolescents. Results showed a significant reduction in anaemia of all severity among adolescents boys and girls. We excluded the study because it was not a randomised controlled trial. |
| Siddiqui 2003 | Study to compare improvement in haemoglobin, mean corpuscular volume, mean corpuscular haemoglobin and ferritin levels in children (aged 5‐10 years ) and women of reproductive age (15‐45 years of age), who were supplemented orally with single and double doses of ferrous sulphate daily and once weekly. 20 children received 200 mg of ferrous sulphate daily and 20 received the same dose once weekly for 2 months. 10 women received 300 mg of ferrous sulphate daily, 10 received the same dose once weekly, and 10 received 600 mg of ferrous sulphate once weekly for 1 month. All parameters improved significantly in children who received 200 mg of ferrous sulphate daily and weekly. Similarly, the parameters improved significantly in women who received 300 mg of ferrous sulphate daily and 600 mg of ferrous sulphate weekly. In conclusion, weekly supplementation of iron was far better at controlling iron deficiency anaemia, due to cost‐effectiveness and better compliance. We excluded the study because it was not randomised and did not have a control group, and hence was outside the scope of this review. |
| Taylor 2001 | Randomised controlled trial with 428 primary school students stratified into 6 groups by age, sex, and intervention, with the objective of measuring the effect of different anthelmintic treatments and iron supplementation regimens provided twice at 6‐monthly intervals for 1 year. Half of the students received iron supplementation (200 mg of ferrous fumarate weekly for 10 weeks). Students received 2 anthelmintic regimens, either 400 mg of albendazole plus 40 mg/kg of praziquantel or 400 mg of albendazole on 3 consecutive days plus 40 mg/kg of praziquantel, or placebo. 12 months after treatment there was a significant increase in haemoglobin levels (P = 0.02) among pupils receiving triple‐dose albendazole, praziquantel and ferrous fumarate; students receiving no anthelmintic treatment showed a significant decrease, as did pupils who received triple‐dose albendazole and praziquantel but no iron. We excluded the study because postmenarchal girls were excluded from the study due to risk of pregnancy and treatments were not secure during pregnancy (at the moment, the safety of albendazole during pregnancy has not been established). |
| Tee 1999 | Study that investigated whether long‐term, weekly iron and folic acid supplements administered at school would improve haemoglobin and ferritin concentrations in adolescent girls, including those with mild‐to‐moderate anaemia and haemoglobin concentrations indicating borderline anaemia. 266 girls with haemoglobin concentrations of 80–119.9 g/L (group A) and 358 girls with haemoglobin concentrations of 120–130 g/L (group B) who were otherwise healthy took part; group C did not receive supplements but was not followed‐up. All 266 girls in group A and 268 (out of 358) girls in group B were randomly assigned to receive either 60 mg or 120 mg of elemental iron plus 3500 μg (3.5 mg) of folic acid weekly for 22 weeks. 90 of the girls in group B were randomly assigned to receive only 5000 μg (5 mg) of folic acid weekly. Authors concluded that long‐term, weekly iron‐folic acid supplementation was a practical, safe, effective, and inexpensive method for improving iron nutrition in adolescent school girls. We excluded the study because girls in both arms were given iron on a weekly basis. |
| Vir 2008 | Study performed in school and non‐school girls aged 11‐18 years that aimed to assess the effectiveness of weekly iron‐folic acid supplementation in reducing the prevalence of anaemia in adolescent girls. The project provided weekly iron‐folic acid tablets, family life education, and deworming tablets every 6 months to 150,700 adolescent school and non‐school girls of a total district population of 3,647,834. Groups were not evaluated simultaneously. In 4 years, the overall prevalence of anaemia was reduced from 73.3% to 25.4%. Haemoglobin levels and anaemia prevalence were influenced significantly at 6 months. No difference in the impact on haemoglobin or anaemia prevalence was observed between supervised and unsupervised girls. We excluded the study because it was not randomised and did not have a control group. |
| Viteri 1999 | Randomised, double‐blind trial involving 239 healthy, menstruating women, older than 18 years of age (some anaemic and some iron deficient) from the University of California, Berkely community, USA. Exclusion criteria: blood donation during the previous 6 months, pregnancy, pregnancy terminated during the previous year, lactating, meno‐metrorrhagia, having a chronic condition interfering with normal iron metabolism, currently taking or having taken therapeutic iron during the last 6 months, and predicted impossibility to comply with the experimental protocol. Group 1 received 60 mg of elemental iron + 250 µg (0.25 mg) of folic acid daily for 3 months and 250 µg (0.25 mg) of folic acid weekly for 4 months. Group 2 received 60 mg of elemental iron + 250 µg (0.25 mg) of folic acid daily for 3 months and 60 mg of elemental iron + 250 µg (0.25 mg) of folic acid weekly (same dose) for 4 months. Group 3 received 250 µg (0.25 mg) of folic acid daily for 3 months and 250 µg (0.25 mg) of folic acid (same dose) weekly for 4 months. We excluded the study because the intervention groups did not match the comparisons of interest in this review. |
CI: confidence intervals MMN: multiple micronutrients N: number UNIMMAP: United Nations International Multiple Micronutrient Preparation VS: versus
Characteristics of studies awaiting classification [ordered by study ID]
Brabin 2014.
| Methods |
Design: randomised, double‐blind, controlled trial Unit of randomisation: individual level |
| Participants |
Setting/location: highly malarious areas in Africa Sample size: ~ 1800 young women of childbearing age (enrolled prior to their first pregnancy) Age range: not reported (median = 16 years) Inclusion criteria: not available Exclusion criteria: not available |
| Interventions | Women were allocated to 1 of 2 groups.
Supplements were given under the observation of field workers during weekly home visits. Women who remained non‐pregnant continued weekly iron‐folic acid supplementation for 18 months. Those who became pregnant continued weekly iron‐folic acid supplementation until the first antenatal visit by the study team. |
| Outcomes |
|
| Notes |
Comment: This was the qualitative report of the randomised controlled trial. It was missing the quantitative results that may be included in the review, when available. Study start date: April 2011 Study end date: June 2013 Funding source: National Institutes of Health (NIH) and Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Conflicts of interest: not available |
Malhotra 2013.
| Methods |
Design: 4‐arm, randomised controlled trial Unit of randomisation: individual level |
| Participants |
Setting/location: outside Delhi, India Sample size: 140 adolescent girls Age range: 14‐19 years Inclusion criteria: not available Exclusion criteria: not available |
| Interventions | Participants were allocated to1 of 4 groups.
|
| Outcomes |
|
| Notes |
Comment: Population was mixed anaemic and non‐anaemic girls. Available abstract did not provide quantitative data for extraction for meta‐analysis. Study start date: not available Study end date: not available Funding source: Indian Council of Medical Research, New Delhi Conflicts of interest: none declared |
Olsen 2000.
| Methods |
Design: 2 × 2, randomised, double‐blind, placebo‐controlled trial Unit of randomisation: individual level |
| Participants |
Setting/location: in the villages of Asino, Ohala and Pith‐Kodhiambo, which lie in the Kisumu district of Nyanza province, Western Kenya Sample size: school children (from schools with highest prevalence of helminth infections) Age range: 8‐18 years Inclusion criteria: moderately low blood concentrations of haemoglobin (i.e. 80–130 g/L if a child aged 4–14 years or a non‐pregnant female aged > 14 years of age, and 80–135 g/L if male and aged > 14 years) Exclusion criteria:
These participants were offered relevant treatment. |
| Interventions | 877 children were randomly allocated to 1 of 2 groups.
Additionally, each participant was independently randomised to: multi‐helminth chemotherapy or identical looking placebo. Length of the intervention: 4 weeks |
| Outcomes |
|
| Notes |
Comment: We were unable to obtain the data for girls separately. Study start date: November 1994 Study end date: January 1996 Fundind source: Institute for Health Research and Development financially supported this work and SmithKline Beecham in Nairobi generously supplied the albendazole used. Conflict of interest: not available |
Sharma 2000.
| Methods |
Design: 3‐arm, randomised experimental trial Unit of randomisation: individual level |
| Participants |
Setting/location: poor communities in urban areas of Delhi and rural parts of Bharatpu Sample size: 270 adolescent girls Age range: not available Inclusion criterion: haemoglobin levels of > 12 g/dL Exclusion criteria: not available |
| Interventions | Participants were allocated to 1 of 4 groups.
Length of the intervention: 6 months For the purposes of this review, we combined groups 1 and 3, separating them only for the subgroup analysis by composition. |
| Outcomes |
|
| Notes |
Comment:
Study start date: not available Study end date: not available Funding source: not available Conflicts of interest: not available |
IFA: iron and folic acid KAP: knowledge, attitudes and practices NE: nutrition education
Characteristics of ongoing studies [ordered by study ID]
CTRI/2017/11/010453.
| Study name | Efficacy of once a week versus daily iron supplementation for control of anaemia in school‐going adolescent girls: a randomised clinical trial |
| Methods | Randomised controlled trial. 2‐arm study design |
| Participants |
Setting: selected schools of higher primary and high schools of Handignur PHC Target sample size: 588 Participants: anaemic adolescent girls Age: 12‐16 years old Inclusion criteria:
Exclusion criteria:
|
| Interventions | Participants were allocated to 1 of the following groups:
Length of the intervention: 3 months |
| Outcomes |
Primary outcomes:
|
| Starting date | October 2017 Current status: not known |
| Contact information |
Name: Dr Sangeeta A Moreshwar Affilitation: PD Bharatesh College of Nursing, Halaga, Belgaum, India Email: smoreshwar@yahoo.co.in |
| Notes |
Funding source: not available Conflicts of interest: not available |
Differences between protocol and review
There are a number of differences between this review and our protocol (Fernández‐Gaxiola 2011b).
-
General
We cited the relevant chapters of the Cochrane Handbook of Systematic Reviews of Interventions, instead of the book, when presenting the methods used in the review, in order to direct the reader to the most relevant sections.
-
Given that the population of menstruating women includes premenarcheal girls and adult women, and each group uses a different cutoff for anaemia, we changed our previous definition of anaemia from "'haemoglobin concentration < 120 g/L, adjusted by altitude where appropriate" to "haemoglobin concentration below a cut‐off defined by trialists, adjusted by altitude where appropriate".
We also changed the name of the outcome "any other side effects" to "any adverse side effects", to avoid mixing negative effects, such as nausea or vomiting, with positive effects such as improved awareness or activity.
-
We revised the search strategy to improve its precision.
-
We did not search the following three databases, which are listed in the protocol for this review (Fernández‐Gaxiola 2011b):
BIOSIS, as it was no longer available to us;
metaRegister of Controlled Trials, as it was under review at the time of this update; and
Networked Digital Library of Theses and Dissertations, as it was not available at the time of this update.
We searched two additional Ovid MEDLINE segments, which are updated daily: MEDLINE In‐Process & Other Non‐Indexed Citations; and MEDLINE Epub Ahead of Print.
We also searched CinicalTrials.gov and IMBIOMED to look for any relevant registered clinical trials.
-
Subgroup analysis and investigation of heterogeneity
As very few studies reported data for most of the outcomes, we limited the subgroup analyses to the following three primary outcomes: anaemia, haemoglobin, and ferritin concentrations.
In addition to visually examining the forest plots, we also used the Borenstein 2008 approach, to formally investigate differences between two or more subgroups.
-
We conducted sensitivity analyses ad hoc to examine the potential effect of clustering on the CI of the summary estimates, by removing cluster‐RCTs from the analyses and comparing the effects. We reported the results of this analysis in Appendix 4.
We conducted an additional sensitivity analysis ad hoc with two studies (Hall 2002 (C); Roschnik 2003 (C)), in which approximately half of the participants were young females (< 12 years of age), to assess their effect on our analyses.
Contributions of authors
Both review authors contributed to drafting the text of the review and approved the final manuscript. AG is the main guarantor of the review.
Sources of support
Internal sources
-
Nutrition International, Ottawa, Canada
Salary support for Luz Maria De‐Regil.
External sources
-
Evidence and Programme Unit, Department of Nutrition for Health and Development, World Health Organization, Switzerland
Ana C Fernández‐Gaxiola received partial financial support for updating this work.
Declarations of interest
Ana Cecilia Fernández‐Gaxiola (AG) is a Consultant at the Instituto Nacional de Salud Pública, Mexico, and a Professor at the Universidad Iberoamericanca Ciudad de México. AG declares that she received partial payment from the Evidence and Programme Guidance, World Health Organization (WHO), to update the review.
Luz Maria De‐Regil (LD‐R) is a full‐time staff member of Nutrition International (NI) (formerly the Micronutrient Initiative), an international non‐for‐profit organisation that delivers multiple micronutrient interventions to children, women of reproductive age and pregnant women; LD‐R did not assess any study funded by NI that met the inclusion criteria of this review, nor did she extract data, assess risk of bias, or rate the quality of the evidence from those studies. The Canadian Department of Foreign Affairs, Trade and Development provides funds to NI to implement programmes with different micronutrient interventions in different populations.
Disclaimer: The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policies, or views of the WHO, NI, or the Canadian Department of Foreign Affairs, Trade and Development.
Edited (no change to conclusions)
References
References to studies included in this review
Agarwal 2003 (C) {published data only}
- Agarwal KN, Gomber H, Bisht H, Som M. Anemia prophylaxis in adolescent school girls by weekly or daily iron-folate supplementation. Indian Pediatrics 2003;40:296-301. [CENTRAL: CN-00437242] [PMID: ] [PubMed] [Google Scholar]
Ahmed 2001 {published data only}
- Ahmed F, Rahman K, Jackson AA. Concomitant supplemental vitamin A enhances the response to weekly supplemental iron and folic acid in anemic teenagers in urban Bangladesh. American Journal of Clinical Nutrition 2001;74:108-15. [DOI: 10.1093/ajcn/74.1.108] [PMID: ] [DOI] [PubMed] [Google Scholar]
Angeles‐Agdeppa 1997 {published data only}
- Angeles-Agdeppa I, Schultink W, Sastroamidjojo S, Gross R, Karyadi D. Weekly micronutrient supplementation to build iron stores in female Indonesian adolescents. American Journal of Clinical Nutrition 1997;66:177-83. [DOI: 10.1093/ajcn/66.1.177] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beasley 2000 {published data only}
- Beasley NMR, Tomkins AM, Hall A, Lorri W, Kihamia CM, Bundy DAP. The impact of weekly iron supplementation on the iron status and growth of adolescent girls in Tanzania. Tropical Medicine and International Health 2000;5(11):794-9. [DOI: 10.1046/j.1365-3156.2000.00641.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dos Santos 1999 {published data only}
- Dos Santos Lopes MC, Cardoso-Ferreira LO, Batista-Filho M. Use of daily and weekly ferrous sulfate to treat anemic childbearing-age women [Uso diário e semanal de sulfato ferroso no tratamento de anemia em mulheres no período reprodutivo]. Cadernos de Saúde Pública 1999;15(4):799-808. [PMID: ] [DOI] [PubMed] [Google Scholar]
Februhartanty 2002 {published data only}
- Februhartanty J, Dillon D, Khusun H. Will iron supplementation given during menstruation improve iron status better than weekly supplementation? Asia Pacific Journal of Clinical Nutrition 2002;1:36-41. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gilgen 2001 {published data only}
- Gilgen D, Mascie-Taylor CG, Rosetta L. Intestinal helminth infections, anaemia and labour productivity of female tea pluckers in Bangladesh. Tropical Medicine and International Health 2001;6(6):449-57. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gilgen D, Mascie-Taylor CG. The effect of anthelmintic treatment on helminth infection and anaemia. Parasitology 2001;122:105-10. [PMID: ] [DOI] [PubMed] [Google Scholar]
- *.Gilgen D, Mascie-Taylor CG. The effect of weekly iron supplementation on anaemia and on iron deficiency among female tea pluckers in Bangladesh. Journal of Human Nutrition and Dietetics 2001;14(3):185-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gonzalez‐Rosendo 2002 {published data only}
- González-Rosendo G, Fernández-Ballart JD, Rodríguez-Jerez JJ, Sánchez-Muñoz J, Quintero-Gutiérrez AG. Weekly iron single dose for adolescent girls in Morelos (Mexico) [Dosis semanal de hierro en mujeres adolescentes de Morelos (Mexico)]. Ciencia y Tecnologia Alimentaria 2008;6(2):137-42. [DOI: 10.1080/11358120809487638] [DOI] [Google Scholar]
- *.González-Rosendo G. Comparación de la dosis única semanal de hierro con la dosis diaria para el tratamiento y prevención de la anemia ferropénica en mujeres adolescentes Mexicanas (Doctoral dissertation). Barcelona, Spain: Universitat Autonoma de Barcelona, 2002. [www.tdx.cat/bitstream/handle/10803/5595/ggr1de1.pdf?sequence=1] [Google Scholar]
Gupta 2014 {published data only}
- Gupta A, Parashar A, Thakur A, Sharma D, Bhardwaj P, Jaswal S. Combating iron deficiency anemia among school going adolescent girls in a Hilly State of north India: effectiveness of intermittent versus daily administration of iron folic acid tablets. International Journal of Preventive Medicine 2014;5(11):1475-9. [PMC4274556] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Hall 2002 (C) {published and unpublished data}
- *.Hall A, Roschnik N, Ouattara F, Toure I, Maiga F, Sacko M, et al. A randomised trial in Mali of the effectiveness of weekly iron supplements given by teachers on the haemoglobin concentrations of schoolchildren. Public Health Nutrition 2002;5(3):413-8. [DOI: 10.1079/PHNPHN2001327] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jalambo 2018 {published data only}
- Jalambo M, Karim N, Naser I, Sharif R. Effects of iron supplementation and nutrition education on haemoglobin, ferritin and oxidative stress on iron-deficient female adolescents in Palestine: randomized control trial. Eastern Mediterranean Health Journal 2018;24(6):560-8. [DOI: 10.26719/2018.24.6.560] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jayatissa 1999 (C) {published data only}
- Jayatissa R, Piyasena P. Adolescent schoolgirls: daily or weekly iron supplementation. Food and Nutrition Bulletin 1999;20(4):429-34. [DOI: 10.1177/156482659902000407] [DOI] [Google Scholar]
Joshi 2013 {published data only}
- Joshi M, Gumashta R. Weekly iron folate supplementation in adolescent girls - an effective nutritional measure for the management of iron deficiency anaemia. Global Journal of Health Science 2013;5(3):188-94.. [DOI: 10.5539/gjhs.v5n3p188] [PMID: 23618489] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kianfar 2000 {published data only}
- Kianfar H, Kimiagar M, Ghaffarpour M. Effect of daily and intermittent iron supplementation on iron status of high school girls. International Journal of Vitamin and Nutriton Research 2000;70(4):172-7. [DOI: 10.1024/0300-9831.70.4.172] [PMID: 10989766 ] [DOI] [PubMed] [Google Scholar]
Leenstra 2009 {published data only}
- Leenstra T, Kariuki SK, Kurtis JD, Oloo AJ, Kager PA, Ter Kuile FO. The effect of weekly iron and vitamin A supplementation on hemoglobin levels and iron status in adolescent schoolgirls in western Kenya. European Journal of Clinical Nutrition 2009;63(2):173-82. [DOI: 10.1038/sj.ejcn.1602919] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mozaffari 2010 (C) {published data only}
- Mozaffari-Khosravi H, Noori-Shadkam M, Fatehi F, Naghiaee Y. Once-weekly low dose iron supplementation effectively improved iron status in adolescent girls. Biological Trace Elements Research 2010;135:22-30. [DOI: 10.1007/s12011-009-8480-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Muro 1999 (C) {published data only}
- Muro GS, Gross U, Gross R, Wahyuniar L. Increase in compliance with weekly iron supplementation of adolescent girls by an accompanying communication programme in secondary schools in Dar-es-Salaam, Tanzania. Food and Nutrition Bulletin 1999;20(4):435-44. [DOI: 10.1177/156482659902000408] [DOI] [Google Scholar]
Nguyen 2008 {published data only}
- *.Nguyen P, Grajeda R, Melgar P, Marcinkevage J, Flores R, Martorell R. Weekly may be as efficacious as daily folic acid supplementation in improving folate status and lowering serum homocysteine concentrations in Guatemalan women. Journal of Nutrition 2008;138(8):1491-8. [DOI: 10.1093/jn/138.8.1491] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Nguyen PH, Grajeda R, Melgar P, Marcinkevage J, DiGirolamo AM, Flores R, et al. Micronutrient supplementation may reduce symptoms of depression in Guatemalan women. Archivos Latinoamericanos de Nutrición 2009;59(3):278-86. [PMID: ] [PubMed] [Google Scholar]
Rezaeian 2014 {published data only}
- Rezaeian A, Ghayour-Mobarhan M, Mazloum SR, Yavari M, Jafari S. Effects of iron supplementation twice a week on attention score and haematologic measures in female high school students. Singapore Medical Journal 2014;55(11):587-92. [PMC4294008] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Riuvard 2006 {published data only}
- Ruivard M, Feillet-Coudray C, Rambeau M, Gerbaud L, Mazur A, Rayssiguier Y, et al. Effect of daily versus twice weekly long-term iron supplementation on iron absorption and status in iron-deficient women: a stable isotope study. Clinical Biochemistry 2006;39(7):700-7. [DOI: 10.1016/j.clinbiochem.2006.02.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Roschnik 2003 (C) {unpublished data only}
- Roschnik N, Phiri V, Mukaka M. The impact of weekly school-based iron supplementation. Mangochi District, Malawi. Unpublished manuscript 2003.
Shah 2002 {published data only}
- Shah BK, Gupta P. Weekly vs daily iron and folic acid supplementation in adolescent Nepalese girls. Archives of Pediatric & Adolescent Medicine 2002;156:131-5. [DOI: 10.1001/archpedi.156.2.131] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shobha 2003 {published data only}
- Shobha S, Sharada D. Efficacy of twice weekly iron supplementation in anemic adolescent girls. Indian Pediatrics 2003;40(12):1186-90. [PMID: 14722370] [PubMed] [Google Scholar]
Soekarjo 2004 (C) {published data only}
- Soekarjo DD, De Pee S, Kusin JA, Schreurs WH, Schultink W, Muhilal, et al. Effectiveness of weekly vitamin A (10,000 IU) and iron (60mg) supplementation for adolescent boys and girls through schools in rural and urban East Java, Indonesia. European Journal of Clinical Nutrition 2004;58:927-37. [DOI: 10.1038/sj.ejcn.1601914] [PMID: 15164114 ] [DOI] [PubMed] [Google Scholar]
Zavaleta 2000 {published data only}
- Zavaleta N, Respicio G, Garcia T. Efficacy and acceptability of two iron supplementation schedules in adolescent school girls in Lima, Peru. Journal of Nutrition 2000;130(2):462S-4S. [DOI: 10.1093/jn/130.2.462S] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ahmed 2005 {published data only}
- Ahmed F, Khan MR, Akhtaruzzaman M, Karim R, Marks GC, Banu CP, et al. Efficacy of twice-weekly multiple micronutrient supplementation for improving the hemoglobin and micronutrient status of anemic adolescent schoolgirls in Bangladesh. American Journal of Clinical Nutrition 2005;82(4):829-35. [DOI: 10.1093/ajcn/82.4.829] [PMID: 16210713] [DOI] [PubMed] [Google Scholar]
Ahmed 2010 {published data only}
- Ahmed F, Khan MR, Akhtaruzzaman M, Karim R, Williams G, Torlesse H, et al. Long-term intermittent multiple micronutrient supplementation enhances hemoglobin and micronutrient status more than iron + folic acid supplementation in Bangladeshi rural adolescent girls with nutritional anemia. Journal of Nutrition 2010;140(10):1879-86. [DOI: 10.3945/jn.109.119123] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ahmed 2012 {published data only}
- Ahmed F, Khan M, Akhataruzzaman M, Karim R, Williams G, Torlesse H, et al. Effect of long-term intermittent multiple micronutrient supplementation in Bangladeshi rural adolescent girls with nutritional anemia. Annals of Nutrition & Metabolism 2013;63(Suppl 1):691. [DOI: 10.1159/000354245] [DOI] [PubMed] [Google Scholar]
- *.Ahmed F, Khan MR, Akhtaruzzaman M, Karim R, Williams G, Banu CP, et al. Effect of long-term intermittent supplementation with multiple micronutrients compared with iron-and-folic acid supplementation on Hb and micronutrient status of non-anaemic adolescent schoolgirls in rural Bangladesh. British Journal of Nutrition 2012;108(8):1484-93. [DOI: 10.1017/S0007114511006908] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bansal 2016 {published data only}
- Bansal PG, Toteja GS, Bhatia N, Vikram NK, Siddhu A. Impact of weekly iron folic acid supplementation with and without vitamin B12 on anaemic adolescent girls: a randomised clinical trial. European Journal of Clinical Nutrition 2016;70(6):730-7. [DOI: 10.1038/ejcn.2015.215] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beaton 1999 {published data only}
- Beaton G, McCabe G. Efficacy of Intermittent Iron Supplementation in the Comparison of Iron Deficiency Anemia in Developing Countries: an Analysis of Experience: Final Report to the Micronutrient Initiative. Ottawa, Canada: Micronutrient Initiative, 1999. [ISBN189421708X] [Google Scholar]
Berger 2005 {published data only}
- *.Berger J, Thanh HTK, Cavalli-Sforza T. Community mobilization and social marketing to promote weekly iron-folic acid supplementation in women of reproductive age in Vietnam: impact on anaemia and iron status. Nutrition Reviews 2005;63(Suppl 2):S95-S108. [DOI: 10.1111/j.1753-4887.2005.tb00167.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Khan NC, Thanh HTK, Berger J, Hoa PT, Quang ND, Smitasiri S, et al. Community mobilization and social marketing to promote weekly iron-folic acid supplementation: a new approach toward controlling anemia among women of reproductive age in Vietnam. Nutrition Reviews 2005;63(Suppl 2):S87-S94. [DOI: 10.1111/j.1753-4887.2005.tb00166.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bruner 1996 {published data only}
- Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet 1996;348(9033):992-6. [DOI: 10.1016/S0140-6736(96)02341-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Casey 2009 {published data only}
- Casey GJ, Jolley D, Phuc TQ, Tinh TT, Tho DH, Montresor A, et al. Long-term weekly iron-folic acid and de-worming is associated with stabilised haemoglobin and increasing iron stores in non-pregnant women in Vietnam. PLOS One 2010;5(12):e15691. [DOI: 10.1371/journal.pone.0015691] [PMC3012714] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Casey GJ, Phuc TQ, MacGregor L, Montresor A, Mihrshahi S, Thach TD, et al. A free weekly iron-folic acid supplementation and regular deworming program is associated with improved hemoglobin and iron status indicators in Vietnamese women. BMC Public Health 2009;9:261. [DOI: 10.1186/1471-2458-9-261] [ PMC2720967] [PMID: 19630954] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey GJ, Tinh TT, Tien NT, Hanieh S, Cavalli-Sforza LT, Montresor A, et al. Sustained effectiveness of weekly iron-folic acid supplementation and regular deworming over 6 years in women in rural Vietnam. PLOS Neglected Tropical Diseases 2017;11(4):e0005446. [DOI: 10.1371/journal.pntd.0005446] [ PMC5404882 ] [PMID: 28406909] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cook 1995 {published data only}
- Cook JD, Reddy MB. Efficacy of weekly compared with daily iron supplementation. American Journal of Clinical Nutrition 1995;62(1):117-20. [DOI: 10.1093/ajcn/62.1.117] [PMID: 7598053 ] [DOI] [PubMed] [Google Scholar]
Crape 2005 {published data only}
- *.Crape CL, Kenefick E, Cavalli-Sforza T, Busch-Hallen J, Milani S, Kanal K. Positive impact of a weekly iron-folic acid supplement delivered with social marketing to Cambodian women: compliance, participation, and hemoglobin levels increase with higher socioeconomic status. Nutrition Reviews 2005;63(Suppl 2):S134-8. [DOI: 10.1111/j.1753-4887.2005.tb00159.x] [PMID: 16466089] [DOI] [PubMed] [Google Scholar]
- Kanal K, Busch-Hallen J, Cavalli-Sforza T, Crape B, Smitasiri S. Weekly iron-folic acid supplements to prevent anemia among Cambodian women in three settings: process and outcomes of social marketing and community mobilization. Nutrition Reviews 2005;63(Suppl 2):S126-33. [DOI: 10.1111/j.1753-4887.2005.tb00158.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deshmukh 2008 {published data only}
- Deshmukh PR, Garg BS, Bharambe MS. Effectiveness of weekly supplementation of iron to control anaemia among adolescent girls of Nashik, Maharashtra, India. Journal of Health, Population and Nutrition 2008;26(1):74-8. [PMC2740684] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Dwividi 2006 {published data only}
- Dwividi A, Schultink W. Reducing anaemia among Indian adolescent girls through once-weekly supplementation with iron and folic acid. Sub-Committe on Nutrition News 2006;31:19-23. [Google Scholar]
Horjus 2005 {published data only}
- Horjus P, Aguayo VM, Roley JA, Pene MC, Meershoek SP. School-based iron and folic acid supplementation for adolescent girls: findings from Manica Province, Mozambique. Food and Nutrition Bulletin 2005;26(3):281-6. [DOI: 10.1177/156482650502600305] [PMID: 16222919] [DOI] [PubMed] [Google Scholar]
Jackson 2003 {published data only}
- Jackson R, Al-Mousa Z, Al-Raqua M, Prakash P. Effect of short-term weekly supplementation on anemia and symptoms in adolescent Kuwaiti girls. Kuwait Medical Journal 2003;35(4):275-80. [Google Scholar]
Joseph 2013 {published data only}
- Joseph B, Ramesh N. Weekly dose of iron-folate supplementation with vitamin C in the workplace can prevent anaemia in women employees. Pakistan Journal of Medical Sciences 2013;29(1):47-52. [DOI: 10.12669/pjms.291.3016] [PMC3809215] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kätelhut 1996 {published data only}
- Kätelhut A, Schultink W, Angeles I, Gross R, Pietrzik K. The effects of weekly iron supplementation with folic acid, vitamin A, vitamin C on iron status of Indonesian adolescents. Asia Pacific Journal of Clinical Nutrition 1996;5(3):181-5. [PMID: ] [PubMed] [Google Scholar]
López de Romaña 2006 {published data only}
- Gross U, Valle C, Diaz MM. Effectiveness of distribution of multimicronutrient supplements in children and in women and adolescent girls of childbearing age in Chiclayo, Peru. Food and Nutrition Bulletin 2006;27(4 Suppl 4):S122-9. [DOI: 10.1177/15648265060274S403] [PMID: 17455398 ] [DOI] [PubMed] [Google Scholar]
- *.López de Romaña D, Verona S, Aquino O, Gross R. Protective effect of multimicronutrient supplementation against anemia among children, women, and adolescent girls in lower-income areas of Chiclayo, Peru. Food and Nutrition Bulletin 2006;27(4 Suppl 4):S143-50. [DOI: 10.1177/15648265060274S405] [PMID: ] [DOI] [PubMed] [Google Scholar]
Moretti 2015 {published data only}
- Morreti D, Goede JS, Zeder C, Jiskra M, Chatzinakou V, Tjalsma H, et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood 2015;126(17):1981-9. [DOI: 10.1182/blood-2015-05-642223] [NCT01785407] [NCT02050932] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pasricha 2009 {published data only}
- Pasricha SR, Casey GJ, Phuc TQ, Mihrshashi S, MacGregor L, Montresor A, et al. Baseline iron indices as predictors of hemoglobin improvement in anemic Vietnamese women receiving weekly iron-folic acid supplementation and deworming. American Journal of Tropical Medicine and Hygiene 2009;81(6):1114-9. [DOI: 10.4269/ajtmh.2009.09-0162] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Perrin 2002 {published data only}
- Perrin E, Rothman R, Coyne-Beasley T, Ford C. Is weekly iron and folic acid supplementation as effective as daily supplementation for decreasing incidence of anemia in adolescent girls? Archives of Pediatrics and Adolescent Medicine 2002;156:128-30. [DOI: 10.1001/archpedi.156.2.128] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ramakrishnan 2012 {published data only}
- Gonzalez-Casanova I, Nguyen PH, Young MF, Harding KB, Reinhart GT, Nguyen H, et al. Predictors of adherence to micronutrient supplementation before and during pregnancy in Vietnam. BMC Public Health 2017;17(1):452. [DOI: 10.1186/s12889-017-4379-4] [NCT01665378] [PMC5434576] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen PH, Lowe AE, Martorell R, Nguyen H, Pham H, Nguyen S, et al. Rationale, design, methodology and sample characteristics for the Vietnam pre-conceptual micronutrient supplementation trial (PRECONCEPT): a randomized controlled study. BMC Public Health 2012;12:898. [DOI: 10.1186/1471-2458-12-898] [NCT01665378] [PMC3533960] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen PH, Young M, Gonzalez-Casanova I, Pham HQ, Nguyen H, Truong TV, et al. Impact of preconception micronutrient supplementation on anemia and iron status during pregnancy and postpartum: a randomized controlled trial in rural Vietnam. PLOS One 2016;11(12):e0167416. [DOI: 10.1371/journal.pone.0167416] [NCT01665378] [PMC5137891] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ramakrishnan U, Nguyen PH, Gonzalez-Casanova I, Pham H, Hao W, Nguyen H, et al. Neither preconceptional weekly multiple micronutrient nor iron-folic acid supplements affect birth size and gestational age compared with a folic acid supplement alone in rural Vietnamese women: a randomized controlled trial. Journal of Nutrition 2016;146(7):1445S-52S. [DOI: 10.3945/jn.115.223420] [NCT01665378] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sen 2012 {published data only}
- Sen A, Kanani S. Intermittent iron folate supplementation: impact on hematinic status and growth of school girls. International Scholarly Research Notices Hematology 2012;2012:482153. [DOI: 10.5402/2012/482153] [PMC3412096] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shah 2016 {published data only}
- Shah SP, Shah P, Desai S, Modi D, Desai G, Arora H. Effectiveness and feasibility of weekly iron and folic acid supplementation to adolescent girls and boys through peer educators at community level in tribal area of Gujarat. Indian Journal of Community Medicine 2016;41(2):158-61. [DOI: 10.4103/0970-0218.173498] [PMC4799641] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siddiqui 2003 {published data only}
- *.Siddiqui IA, Jaleel A, Rahman MA. Preventive strategy to control iron deficiency anemia in children and adults. Journal of the Pakistan Medical Association 2003;53(4):131-3. [PMID: ] [PubMed] [Google Scholar]
- Siddiqui IA, Rahman MA, Jaleel A. Efficacy of daily vs weekly supplementation of iron in schoolchildren with low iron status. Journal of Tropical Pediatrics 2004;50(5):276-8. [DOI: 10.1093/tropej/50.5.276] [PMID: 15510758] [DOI] [PubMed] [Google Scholar]
Taylor 2001 {published data only}
- Taylor M, Jinabhai CC, Couper I, Kleinschmidt I, Jogessar VB. The effect of different anthelmintic treatment regimens combined with iron supplementation on the nutritional status of schoolchildren in KwaZulu-Natal, South Africa: a randomized controlled trial. Transactions of the Royal Society of Tropical Medicine and Hygiene 2001;95(2):211-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tee 1999 {published data only}
- Tee ES, Kandiah M, Awin N, Chong SM, Satgunasingam N, Kamarudin L, et al. School-administered weekly iron-folate supplements improve hemoglobin and ferritin concentrations in Malaysian adolescent girls. American Journal of Clinical Nutrition 1999;69(6):1249-56. [DOI: 10.1093/ajcn/69.6.1249] [PMID: ] [DOI] [PubMed] [Google Scholar]
Vir 2008 {published data only}
- Vir SC, Singh N, Nigam AK, Jain R. Weekly iron and folic acid supplementation with counseling reduces anemia in adolescent girls: a large-scale effectiveness study in Uttar Pradesh, India. Food and Nutrition Bulletin 2008;29(3):186-94. [DOI: 10.1177/156482650802900304] [PMID: 18947031 ] [DOI] [PubMed] [Google Scholar]
Viteri 1999 {published data only}
- Viteri FE, Ali F, Tujague J. Long-term weekly iron supplementation improves and sustains nonpregnant women's iron status as well or better than currently recommended short-term daily supplementation. Journal of Nutrition 1999;129(11):2013-20. [DOI: 10.1093/jn/129.11.2013] [PMID: 10539778 ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Brabin 2014 {published data only}
- * Compaore A, Gies S, Brabin BJ, Tinto H, Brabin L. "There is iron and iron..." Burkinabe women's perceptions of iron supplementation: a qualitative study. Maternal and Child Health Journal 2014;18(8):1976-84. [DOI: 10.1007/s10995-014-1443-x] [PMC4167572] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compaore A, Gies S, Brabin BJ, Tinto H, Brabin L. A qualitative study of the acceptability of weekly iron supplementation prior to the first pregnancy in Burkina Faso. Tropical Medicine and International Health 2017;22(Suppl 1):98. [DOI: 10.1111/tmi.12978] [8S2.4] [DOI] [Google Scholar]
Malhotra 2013 {published data only}
- Malhotra A, Tyagi A. Effect of nutrition education and biweekly IFA supplementation on anaemia related knowledge and iron status of underprivileged adolescent girls. Annals of Nutrition & Metabolism 2013;63(Suppl 1):320. [DOI: 10.1159/000354245] [DOI] [Google Scholar]
Olsen 2000 {published data only}
- *.Olsen A, Nawiri J, Friis H. The impact of iron supplementation on reinfection with intestinal helminths and Schistosoma mansoni in western Kenya. Transactions of the Royal Society of Tropical Medicine and Hygiene 2000;94:493-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Olsen A, Nawiri J, Magnussen P, Krarup H, Friis H. Failure of twice-weekly iron supplementation to increase blood haemoglobin and serum ferritin concentrations: results of a randomized controlled trial. Annals of Tropical Medicine and Parasitology 2006;100(3):251-63. [DOI: 10.1179/136485906X91486] [PMID: 16630383 ] [DOI] [PubMed] [Google Scholar]
Sharma 2000 {published data only}
- Sharma A, Prasad K, Rao KV. Identification of an appropriate strategy to control anemia in adolescent girls of poor communities. Indian Pediatrics 2000;37:261-7. [PMID: ] [PubMed] [Google Scholar]
References to ongoing studies
CTRI/2017/11/010453 {published data only}
- CTRI/2017/11/010453. Weekly and daily ferrous sulphate supplementation for control of anaemia in menstruating adolescents [Efficacy of once a week vs daily iron supplementation for control of anaemia in school going adolescent girls - a randomized clinical trial]. apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/11/010453 (first received 10 November 2017). [CTRI/2017/11/010453]
Additional references
Ahmed 2008
- Ahmed F, Khan MR, Banu CP, Qazi MR, Akhtaruzzaman M. The coexistence of other micronutrient deficiencies in anaemic adolescent schoolgirls in rural Bangaldesh. European Journal of Clinical Nutrition 2008;62(3):365-72. [DOI: 10.1038/sj.ejcn.1602697] [PMID: ] [DOI] [PubMed] [Google Scholar]
Allen 2009a
- Allen LH, Peerson JM, Maternal Micronutrient Supplementation Study Group (MMSSG). Impact of multiple micronutrient versus iron-folic acid supplements on maternal anemia and micronutrient status in pregnancy. Food and Nutrition Bulletin 2009;30(4 Suppl 4):S527-32. [DOI: 10.1177/15648265090304S407] [PMID: ] [DOI] [PubMed] [Google Scholar]
Allen 2009b
- Allen LH, Peerson JM, Olney DK. Provision of multiple rather than two or fewer micronutrients more effectively improves growth and other outcomes in micronutrient deficient children and adults. Journal of Nutrition 2009;139(5):1022-30. [DOI: 10.3945/jn.107.086199] [PMID: 19321586] [DOI] [PubMed] [Google Scholar]
Alleyne 2008
- Alleyne M, Horne MK, Miller JL. Individualized treatment for iron-deficiency anemia in adults. American Journal of Medicine 2008;121(11):943-8. [DOI: 10.1016/j.amjmed.2008.07.012] [PMID: 18954837 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anah 2008
- Anah MU, Ikpeme OE, Etuk IS, Yong KE, Ibanga I, Asuquo BE. Worm infestation and anemia among pre-school children of peasant farmers in Calabar, Nigeria. Nigerian Journal of Clinical Practice 2008;11(3):220-4. [PMID: ] [PubMed] [Google Scholar]
Anderson 2005
- Anderson GJ, Frazer DM, McKie AT, Vulpe CD, Smith A. Mechanisms of haem and non-haem iron absorption: lessons from inherited disorders of iron metabolism. BioMetals 2005;18(4):339-48. [DOI: 10.1007/s10534-005-3708-8] [DOI: 16158226] [DOI] [PubMed] [Google Scholar]
Balshem 2010
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401-6. [DOI: 10.1016/j.jclinepi.2010.07.015] [PMID: 21208779 ] [DOI] [PubMed] [Google Scholar]
Beard 2001
- Beard JL. Iron biology in immune function, muscle metabolism and neuronal functioning. Journal of Nutrition 2001;131(2):568S-80S. [DOI: 10.1093/jn/131.2.568S] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beard 2005
- Beard JL, Hendricks MK, Perez EM, Murray-Kolb LE, Berg A, Vernon-Feagans L, et al. Maternal iron deficiency anemia affects postpartum emotions and cognition. Journal of Nutrition 2005;135(2):267-72. [DOI: 10.1093/jn/135.2.267] [PMID: 15671224 ] [DOI] [PubMed] [Google Scholar]
Bentley 2003
- Bentley ME, Griffiths PL. The burden of anemia among women in India. European Journal of Clinical Nutrition 2003;57(1):52-60. [DOI: 10.1038/sj.ejcn.1601504] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bodnar 2002
- Bodnar LM, Cogswell ME, Scanlon KS. Low income postpartum women are at risk of iron deficiency. Journal of Nutrition 2002;132(8):2298-302. [DOI: 10.1093/jn/132.8.2298] [PMID: 12163678 ] [DOI] [PubMed] [Google Scholar]
Borenstein 2008
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis (Statistics in Practice). Chichester (UK): John Wiley & Sons, 2008. [Google Scholar]
Casanueva 2006
- Casanueva E, Viteri FE, Mares-Galindo M, Meza-Camacho C, Loría A, Schnaas L, et al. Weekly iron as a safe alternative to daily supplementation for nonanemic pregnant women. Archives of Medical Research 2006;37(5):674-82. [DOI: 10.1016/j.arcmed.2005.11.011] [PMID: 16740440 ] [DOI] [PubMed] [Google Scholar]
Clark 2008
- Clark SF. Iron deficiency anemia. Nutrition Clinical Practice 2008;23(2):128-41. [DOI: 10.1177/0884533608314536] [PMID: ] [DOI] [PubMed] [Google Scholar]
Covidence 2017 [Computer program]
- Covidence systematic review software. Melbourne, Australia: Veritas Health Innovation, 2017.Available at www.covidence.org.
Dalmiya 2009
- Dalmiya N, Darnton-Hill I, Schultink W, Shrimpton R. Multiple micronutrient supplementation during pregnancy: a decade of collaboration in action. Food and Nutrition Bulletin 2009;30(4 Suppl 4):S477-9. [DOI: 10.1177/15648265090304S401] [PMID: ] [DOI] [PubMed] [Google Scholar]
De‐Regil 2011
- De-Regil LM, Jefferds MED, Sylvetsky AC, Dowswell T. Intermittent iron supplementation for improving nutrition and developmental outcomes in children under 12 years of age. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD009085.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
De‐Regil 2015
- De-Regil LM, Peña-Rosas JP, Fernández-Gaxiola AC, Rayco-Solon P. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database of Systematic Reviews 2015, Issue 12. [DOI: 10.1002/14651858.CD007950.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG, editor(s). Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
DeMaeyer 1989
- DeMaeyer EM. Preventing and controlling iron deficiency anaemia through primary health care. World Health Organization: Geneva; 1989.
Gajida 2010
- Gajida AU, IIiyasu Z, Zoakah Al. Malaria among antenatal clients attending primary health care facilities in Kano state, Nigeria. Annals of African Medicine 2010;9(3):188-93. [DOI: 10.4103/1596-3519.68352] [PMID: ] [DOI] [PubMed] [Google Scholar]
GRADEpro 2015 [Computer program]
- GRADEpro GDT. Version accessed 06 December 2017. Hamilton (ON): GRADE Working Group, McMaster University (developed by Evidence Prime), 2015.Available at gradepro.org.
Green 2017
- Green R, Datta Mitra A. Megaloblastic anemias: nutritional and other causes. Medical Clinics of North America 2017;101(2):297-317. [10.1016/j.mcna.2016.09.013] [PMID: ] [DOI] [PubMed] [Google Scholar]
Grossetta Nardini 2017 [Computer program]
- Yale MeSH Analyzer. Grossetta Nardini HK, Wang L, Version accessed 11 January 2017. New Haven (CT): Cushing/Whitney Medical Library, 2017.Available at mesh.med.yale.edu/.
Herbert 1987
- Herbert V. The 1986 Herman award lecture. Nutrition science as a continually unfolding story: the folate and vitamin B-12 paradigm. American Journal of Clinical Nutrition 1987;46(3):387-402. [DOI: 10.1093/ajcn/46.3.387] [PMID: 3307371 ] [DOI] [PubMed] [Google Scholar]
Hercberg 1992
- Hercberg S, Galan P. Nutritional anaemias. Baillieres Clinical Haematology 1992;5(1):143-68. [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG, editor(s). Chapter 16: Special topics in Statistics. In: Higgins JPT, Green E, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Jimenez 2010
- Jimenez C, Leets I, Puche R, Anzola E, Montilla R, Parra C, et al. A single dose of vitamin A improves haemoglobin concentration, retinol status and phagocytic function of neutrophils in preschool children. British Journal of Nutrition 2010;103(6):798-802. [DOI: 10.1017/S000711450999276] [PMID: ] [DOI] [PubMed] [Google Scholar]
Khan 2005
- Khan NC, Thanh HTK, Berger J, Hoa PT, Quang ND, Smitasiri S, et al. Community mobilization and social marketing to promote weekly iron-folic acid supplementation: a new approach toward controlling anemia among women of reproductive age in Vietnam. Nutrition Reviews 2005;63(12 Pt 2):S87-94. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kontic‐Vucinic 2006
- Kontic-Vucinic O, Sulovic N, Radunovic N. Micronutrients in women's reproductive health: II. Minerals and trace elements. International Journal of Fertility and Women's Medicine 2006;51(3):116-24. [PMID: ] [PubMed] [Google Scholar]
Kumar 2007
- Kumar A, Valecha N, Jain T, Dash AP. Burden of malaria in India: retrospective and prospective view. American Journal of Tropical Medicine and Hygiene 2007;77(Suppl 6):69-78. [PMID: ] [PubMed] [Google Scholar]
Lynch 2007
- Lynch S. Iron metabolism. In: Kraemer K, Zimmermann MB, editors(s). Nutritional Anemia. Basel: Sight and Life Press, 2007:59-76. [Google Scholar]
Margetts 2007
- Margetts BM, Tallant A, Armstrong E. Weekly iron and folic acid supplementation for women of reproductive age: a review of published studies. Desk review prepared for WPRO. WHO Western Pacific Regional Office; 2007.
Martinez‐de Villareal 2001
- Martinez-de Villareal LE, Limón-Benavides C, Valdez-Leal R, Sánchez-Peña MA, Villareal-Pérez JZ. Impact of weekly administration of folic acid on folic acid blood levels [Efecto de la administración semanalde ácido fólico sobre los valores sanguíneos]. Salud Pública de México 2001;43(2):103-7. [PubMed] [Google Scholar]
Martinez‐de Villareal 2002
- Martinez-de Villareal LE, Pérez JZ, Vázquez PA, Herrera RH, Campos M del R, López RA, et al. Decline of neural tube defects cases after a folic acid campaign in Nuevo León, México. Teratology 2002;66(5):249-56. [DOI: 10.1002/tera.10094] [PMID: 12397633] [DOI] [PubMed] [Google Scholar]
McLean 2008
- McLean E, De Benoist B, Allen LH. Review of the magnitude of folate and vitamin B12 deficiencies worldwide. Food and Nutrition Bulletin 2008;29(2 Suppl 1):S38-51. [DOI: 10.1177/15648265080292S107] [PMID: ] [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [PMC2707599] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norsworthy 2004
- Norsworthy B, Skeaff CM, Adank C, Green TJ. Effects of once-a-week or daily folic acid supplementation on red blood cell folate concentrations in women. European Journal of Clinical Nutrition 2004;58(3):548-54. [DOI: 10.1038/sj.ejcn.1601843] [PMID: 14985695] [DOI] [PubMed] [Google Scholar]
Oates 2007
- Oates PS. The relevance of the intestinal crypt and enterocyte in regulating iron absorption. Pflugers Archiv: European Journal of Physiology 2007;455(2):201-13. [DOI: 10.1007/s00424-007-0264-9] [PMID: 17473933 ] [DOI] [PubMed] [Google Scholar]
Okabe 2011
- Okebe JU, Yahav D, Shbita R, Paul M. Oral iron supplementation for preventing or treating anaemia among children in malaria-endemic areas. Cochrane Database of Systematic Reviews 2011, Issue 10. [DOI: 10.1002/14651858.CD006589.pub3] [DOI] [PubMed] [Google Scholar]
Oppenheimer 2001
- Oppenheimer SJ. Iron and its relation to immunity and infectious disease. Journal of Nutrition 2001;131(2):616S-35S. [DOI: 10.1093/jn/131.2.616S] [PMID: 11160594] [DOI] [PubMed] [Google Scholar]
Paulino 2005
- Paulino LS, Angeles-Agdeppa I, Etorma UM, Ramos AC, Cavalli-Sforza T. Weekly iron-folic acid supplementation to improve iron status and prevent pregnancy anemia in Filipino women of reproductive age. Nutrition Reviews 2005;63(Suppl 2):S109-15. [DOI: 10.1111/j.1753-4887.2005.tb00156.x] [PMID: 16466086] [DOI] [PubMed] [Google Scholar]
Peña‐Rosas 2015
- Peña-Rosas JP, De-Regil LM, Gomez-Malave H, Flores-Urrutia MC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 10. [DOI: 10.1002/14651858.CD009997.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prentice 2007
- Prentice AM, Ghattas H, Doherty C, Cox SE. Iron metabolism and malaria. Food and Nutrition Bulletin 2007;28(4 Suppl 4):S524-39. [DOI: 10.1177/15648265070284S406] [PMID: 18297891] [DOI] [PubMed] [Google Scholar]
Ramakrishnan 2002
- Ramakrishnan U. Prevalence of micronutrient malnutrition worldwide. Nutrition Reviews 2002;60(Suppl 5):S46-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
Reeves 2011
- Reeves BC, Deeks JJ, Higgins JPT, Wells GA. Chapter 13: Including non-randomized studies. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ryan 2016
- Ryan R, Hill S, Cochrane Consumers and Communication Group. How to GRADE the quality of the evidence Version 3.0 (Approved S Hill). cccrg.cochrane.org/author-resources (accessed prior to 1 November 2018).
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings’ tables. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Soekarjo 2001
- Soekarjo DD, De Pee S, Bloem MW, Tjiong R, Yip R, Schreurs WH, et al. Socio-economic status and puberty are the main factors determining anaemia in adolescent girls and boys in East Java, Indonesia. European Journal of Clinical Nutrition 2001;55(11):932-9. [DOI] [PubMed] [Google Scholar]
Stoltzfus 2003
- Stoltzfus RJ. Iron deficiency: global prevalence and consequences. Food and Nutrition Bulletin 2003;24(4 Suppl 2):S99-103. [DOI: 10.1177/15648265030244S206] [PMID: ] [DOI] [PubMed] [Google Scholar]
Viteri 1995
- Viteri FE, Xunian L, Tolomei K, Martin A. True absorption and retention of supplemental iron is more efficient when iron is administered every three days rather than daily to iron-normal and iron-deficient rats. Journal of Nutrition 1995;125(1):82-91. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Viteri 2005
- Viteri FE, Berger J. Importance of pre-pregnancy and pregnancy iron status: can long-term weekly preventive iron and folic acid supplementation achieve desirable and safe status? Nutrition Reviews 2005;63(Suppl 2):S65-76. [DOI: 10.1111/j.1753-4887.2005.tb00163.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 2001
- World Health Organization. Iron Deficiency Anaemia: Assessment, Prevention and Control. A Guide for Programme Managers. Geneva: World Health Organization, 2001. [WHO/NHD/01.3] [Google Scholar]
WHO 2011a
- World Health Organization. Serum Retinol Concentrations for Determining the Prevalence of Vitamin A Deficiency in Populations. Geneva (CH): World Health Organization, 2011. [WHO/NMH/NHD/MNM/11.3] [Google Scholar]
WHO 2011b
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Geneva (CH): World Health Organization, 2011. [WHO/NMH/NHD/MNM/11.1 ] [Google Scholar]
WHO 2011c
- World Health Organization. Serum Ferritin Concentrations for the Assessment of Iron Status and Iron Deficiency in Populations. Geneva (CH): World Health Organization, 2011. [WHO/NMH/NHD/MNM/11.2] [Google Scholar]
WHO 2011d
- World Health Organization. Guideline: Intermittent Iron and Folic Acid Supplementation in Menstruating Women. Geneva (CH): World Health Organization, 2011. [NBK200783] [WHO/NMH/NHD/MNM/09.2] [PubMed] [Google Scholar]
WHO 2014
- World Health Organization. Global Nutrition Targets 2025: Anaemia Policy Brief. Geneva (CH): World Health Organization, 2014. [Google Scholar]
WHO 2015
- World Health Organization. The Global Prevalence of Anaemia in 2011. Geneva: World Health Organization, 2015. [ ISBN: 9789241564960] [Google Scholar]
WHO‐WPRO 2011
- World Health Organization. Weekly Iron and Folic Acid Supplementation Programmes for Women of Reproductive Age: an Analysis of Best Programme Practices (WHO Position Statement). Manila: World Health Organization Regional Office for the Western Pacific, 2011. [ISBN: 9789290615231] [Google Scholar]
Yip 1988
- Yip R, Dallman PR. The roles of inflammation and iron deficiency as causes of anemia. American Journal of Clinical Nutrition 1988;48(5):1295-300. [DOI: 10.1093/ajcn/48.5.1295] [PMID: 3189219 ] [DOI] [PubMed] [Google Scholar]
Yip 1994
- Yip R. Iron deficiency: contemporary scientific issues and international programmatic approaches. Journal of Nutrition 1994;124(Suppl 8):1479S-90S. [DOI: 10.1093/jn/124.suppl_8.1479S] [PMID: 8064407 ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Fernández‐Gaxiola 2011a
- Fernández-Gaxiola AC, De-Regil LM. intermittent iron supplementation for reducing anaemia and its associated impairments in menstruating women. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD009218.pub2] [DOI] [PubMed] [Google Scholar]
Fernández‐Gaxiola 2011b
- Fernández-Gaxiola AC, De-Regil LM, Nasser M. Intermittent iron supplementation for reducing anaemia and its associated impairments in menstruating women. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009218] [DOI] [PubMed] [Google Scholar]


