Abstract
Selective dorsal rhizotomy is a key technique in the surgical management of spasticity in patients with cerebral palsy. The technique evolved from the late 1800s when pioneers like Dana and Abbe performed dorsal rhizotomy in their treatment of refractory pain. These surgeons noted a reduction in muscle tone associated with the operation. When Sherrington then published his Nobel prize-winning work on the corticospinal tract and its role in the neuromuscular system in the 1890s, the course was set for modifying spasticity by aiming surgery at the dorsal roots. This procedure underwent multiple modifications through the next century and today it is, arguably, the most commonly performed operation to treat cerebral palsy children with spasticity. Selective dorsal rhizotomy is a technique that still teaches us a great deal about neurophysiology on a daily basis and it is thanks to the pioneers, described in this article, that we have this tool in our armamentarium.
Electronic supplementary material
The online version of this article (10.1007/s13311-018-00690-4) contains supplementary material, which is available to authorized users.
Key·Words: Selective dorsal rhizotomy, History, Evolution, Techniques, Spasticity.
Introduction
Selective dorsal rhizotomy (SDR) forms the cornerstone of the armamentarium of the neurosurgeon who ventures into the realm of dealing with spasticity. Since Sherrington [1–7] and his Nobel prize-winning research on the neuromuscular system, muscle tone, and the pathogenesis of spasticity in the late nineteenth century, the dorsal afferent pathway and its role in the control of muscle tone in mammals has received much attention. It is exactly this dorsal feedback system that is the main target in managing spasticity when performing selective dorsal rhizotomies. Today, the common perception is that there are two schools of thought when it comes to SDR: the “Peacock-school” and the “Park-school”. This is because modern variations of the technique of SDR are largely those developed by Warwick Peacock at Red Cross War Memorial Children’s Hospital, in Cape Town, South Africa [8], and later modified by Dr. Tae Sung Park from St. Louis in the USA, where, after learning the technique of SDR from Dr. Peacock, he modified it to a limited level exposure of the conus during the procedure [9]. It is in fact not a new technique as such—as this is where it all started with Fasano and Gros [10, 11].
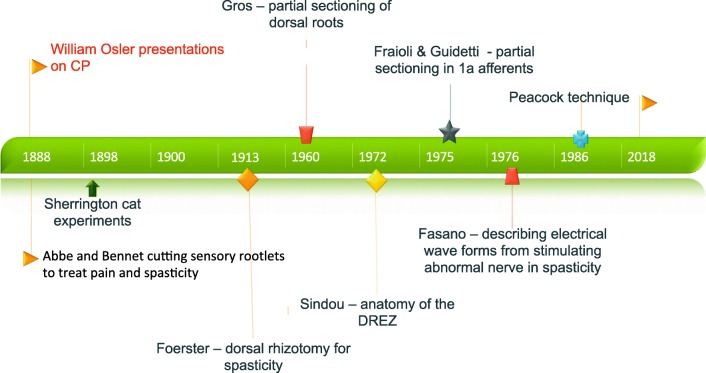
Like most things in surgery, there was always someone who thought about it earlier and then it was forgotten.In the case of SDR, the history and evolution of the technique is a fascinating review of our current understanding, or lack thereof, on spasticity and its pathogenesis. In this review, the focus will be on this journey of exploration of the nervous system and how this led to the techniques of SDR as we use it today to treat spastic, diplegic cerebral palsy. Figure 1 will illustrate a timeline of innovation in SDR.
Fig. 1.
Timeline of SDR techniques and innovation
Historical Aspects
The first reported use of posterior rhizotomy was by Abbe for pain management in the 1880s [12]. Bennett [13] also performed this technique for pain and showed relief of spasticity at the same time. He gave credit for the procedure to Dana [12] in this historic manuscript. Lorenz [14] introduced peripheral neurectomy as a means to treat spasticity in 1887, when he started performing obturator neurectomy as a means of reducing hip adductor spasticity.Due to the debilitating flailing legs, caused by unopposed hip abduction, this technique has been out of favor for many years [15]. The technique was again introduced in 1976 by Gros in Montpellier [16] and further developed by the group of Sindou [17, 18] in Lyon.
The original focus, in the late 1800s, on the peripheral nerve changed again when Sherington [14] published his work on neural control of movement in the 1890s, for which he received the Nobel prize. Sherrington [19] showed that sectioning of the corticospinal tracts could cause decerebrate rigidity in cats and that there was a reduction in muscle tone in these cats once the posterior roots were divided. This led to the early belief that spasticity is the result of injury to the corticospinal tract. We know, however, today that spasticity is not caused by injury to the corticospinal tracts, but by the closely related reticulospinal and vestibulospinal-tract injuries rather [20].
In the early 1900s, Foerster [21] reported on his first dorsal rhizotomies to treat spasticity in humans. He divided the whole of the dorsal nerve root from T12 to S2 [22], with the use of nerve stimulation to identify the nerve root level as well as to differentiate motor from sensory nerve roots [23]. Aware that control of knee extension is key to standing posture and gait, he purposefully spared the L4 nerve root in an attempt to preserve knee extension strength.Complications with his technique include severe sensory loss, bladder denervation, trophic changes, and proprioception difficulties [11, 22, 24]; as a result, the technique fell from favor until revived by Gros [24] in the 1960’s.
Gros [16, 24], from Montpellier, refined the procedure by sectioning only four fifths of the dorsal root fascicles.This approach was accompanied by unpredictable postoperative weakness and, in many patients, persistence of spasticity. Gros [22] started using electromyography intraoperatively to help identify the abnormal rootlets,while sparing the dorsal rootlets that were clearly involved in postural control and gait and they performed the procedure via a laminectomy of T11 to L1 in a lateral position [22].They dissected the dorsal nerve root at the level of the conus and then separated the dorsal nerve root into separate fascicles. The number of fascicles that were cut depended on the degree of selectivity wished for the muscle groups involved. As an example, they would aim to keep more rootlets for the gastrocnemius muscles, while they would sacrifice more rootlets for the hip adductor muscles [22]. During the stimulation process, they would use a continuous stimulation at 4 Hz, with each square wavelength being 1 msec. Amplitude of 1 V was used at each fascicle. A physical therapist would help the surgeon assess which of the stimulated rootlets cause abnormal muscle contraction in the muscles and to determine which rootlets impair the patient’s function [11, 22]. Emphasis was placed on the clinical evaluation of the patient, so asymmetrical rhizotomies were common practice if the clinical picture required it [22]. Gros [22] also reported suprasegmental effects from dorsal rhizotomy, where the patients would have associated reduction in upper limb spasticity after undergoing lower limb dorsal rhizotomy.
During the same time period Sindou [25], who was trained by Gros, developed a keen interest in the dorsal root entry zone (DREZ). Sindou described the anatomy and developed the DREZotomy technique for pain management and he noted that, by creating a lesion in the DREZ up to 5 mm in depth, spasticity is reduced. Sindou [26] also performed dorsal rhizotomies using the same principles as Gros and applied electrophysiological principles of Fasano, but did not divide the dorsal root into separate fascicles.They made a qualitative decision on division percentage, and not quantitative as Gros, by means of individual fascicle stimulation [22].
During this same period [10, 27], Fasano started using and describing electrophysiological evaluations in more detail during the rhizotomy procedure to perform selective fascicular sectioning and therefore only cut the fascicles that presumably contribute to the abnormal muscular tone. Fasano described electrophysiological features of abnormal nerve inhibition. He thought that this was due to the loss of suprasegmental inhibition of the alfa-gamma muscle loop. The features that Fasano [28] found to be indicative of abnormal neuromuscular reaction to an electrical stimulation were: abnormal threshold to a train of stimuli, spread to muscles that were not primarily innervated and crossover activation. In using these electrophysiological principles he felt that patients had less sensory deficits (including proprioception), less weakness with greater functional improvement after SDR. He also used a conus-level approach as that which was described by Foerster and Gros [29].
Modern SDR
Warwick Peacock, from Red Cross War Memorial Children’s Hospital in Cape Town, went on to modify the procedure by changing the short segment lumbar laminectomy to a long segment exposure (L2–L5 laminectomy) and he is generally credited with the modern revival of SDR for managing spasticity. His main concern that led him to a cauda equina level approach was the high incidence of bladder and bowel deficits with the conus-level approach used by other groups up to that time [8]. Peacock performed a L2 to L5 laminectomy and then SDR on L2 to S1. The technique entails using selective dorsal fascicular sectioning as based on electromyographical (EMG) findings, Fasano’s principles of EMG interpretation, and the clinical pattern of spasticity [8, 24, 30–33]. Peacock noted that he always left S2 intact if there was any anal sphincter innervation from it, even when S2 would also show abnormal triceps surae activity.
Although never deemed necessary by Peacock and the Cape Town team that continued his legacy, many international colleagues who adopted the Peacock technique for SDR kept children in a whole spinal plaster cast for a period of 6 weeks after surgery. The concerns raised by Steinbok and other authors [34–38] regarding increased spinal deformities due to the multilevel laminectomies did not help the cause. SDR was later further modified by doing a laminotomy procedure with a high-speed drill that allowed for replacement of the laminae postoperative and reattachment of the paraspinal muscles. This would also negate the concern of spinal deformities after SDR. These concerns were, however proven to be unfounded on long-term follow-up studies [30, 39, 40].
Tae Sung Park, from St. Louis, visited Warwick Peacock in the 1980s and learned the technique for SDR but later modified the procedure back to the original conus-level exposure, using ultrasound to determine this point following a T12 to L1/2 laminectomy [9, 41]. EMG is then used to confirm the level of nerve root and a percentage of the dorsal root is sectioned.
Marc Sindou from Lyon, France, agreed with the technique of cauda equina exposure to identify the nerve at the exit foramina but was concerned about the long segment exposure required by the Peacock technique (L2–S2). Sindou and Georgoulis [42] then developed the Keyhole interlaminar dorsal rhizotomy (KIDr) technique in 2014, which allows them minimal spinal ligamentous injury, while still allowing accurate nerve root identification at the exit foraminae. Currently, this center performs all their SDR’s using this approach [42]. They have also done away with a whole spine plaster cast for 6 weeks, as done before, in using this technique.
A key factor in SDR evolution is most certainly the advancements in intraoperative neuromonitoring. Abbott and colleagues [43, 44] in New York continued to describe and find ways of protecting the pudendal plexus during SDR. They showed how they identify the S2 innervation of the pudendal plexus by using electrophysiological principles of constant EMG monitoring and compound muscle action potentials (CMAP). They also found that outcomes on ankle spasticity were better if they strive to include S2 in the sectioning, even if only partial [44].
Questions regarding the usefulness and indeed the need of intraoperative neuromonitoring and the technique of fascicular dissection have been asked many times [41, 45–48]. On the one side of the argument, Nishida and colleagues [49] wrote that neurophysiological testing may have a significant impact on outcomes of SDR. They measure and describe in great detail these electrophysiological reflexes, while Steinbok [46] showed an improvement in function in lower limbs, of about 90%, independent of the emphasis that was placed on neuromonitoring and the fascicular dissection techniques. Warf and colleagues [47] also showed that a SDR technique without fascicular dissection or neurophysiological monitoring can be effective in a resource-scarce environment. Steinbok [50] also showed that SDR without neuromonitoring is equally safe and yields similar results to SDR with the use of neurophysiological mapping. Fukuhara and colleagues [51, 52] have, however, shown on histological studies (where they show micro-architectural changes in nerve fascicles involved with abnormal spastic muscles), that there is a role for fascicular dissection and stimulation to evaluate each fascicle within the dorsal root to determine its role in abnormal spasticity and, therefore, the need to cut it. Careful manipulation is needed because even gentle fascicular dissection and manipulation can lead to electrical aberrations, which may be misleading [53].
One unifying point of the selection criteria of Foerster, Gros, Sindou, Fasano, Peacock, and Abbott [8, 23, 26–28] was their selection criteria and more specifically their view on exclusion criteria for SDR: truncal weakness and dystonia or athetosis. These characteristics all lead to inability to rehabilitate as the weakness is exacerbated and the dystonic or dynamic movement component is unmasked by SDR. The ideal patient is an ambulant child with cerebral palsy of the spastic diplegia subtype, without any dystonic features or truncal weakness. This is still true for most units today and a thorough clinical examination by an experienced team should still be the gold standard in patient selection. As is clear from a review article by Grunt et al. [54], there is still significant variation in the selection criteria for SDR. Various approaches are currently explored; such as Intrathecal Baclofen trial to evaluate SDR candidacy (unpublished but it is experimental in the UK), but no consensus standard criteria exist as yet.
Evolution of Our Understanding of the Physiology of Spasticity
Sherrington’s [19] studies on cats were the groundbreaking work that started our understanding of the physiological principles of muscle tone and spasticity. Before this, there has been posterior rhizotomies performed, but mainly for pain. Many authors noted a reduction in muscle tone as well [12, 13]. The early theory on muscle tone still rested on the concept of a receptor inside the muscle spindle as well as its afferent fiber (Ia) which is inside the posterior nerve root [24]. This reflex arc then excites the alfa-motor neuron in the spinal cord to induce a contraction. Spasticity is then thought to result from a loss of inhibition of this reflex mechanism [24]. In other words: the muscle spindle will continue to contract if the higher centers (brain and spinal cord) do not fulfill its “dampening” effect on the monosynaptic reflex arc.
Today, most authors do not accept the original argument of hyperexcitability of the gamma-loop as a valid explanation for spasticity [24, 55]. We know today that Sherrington sectioned through the reticulospinal tracts as well as the corticospinal tracts in his cat experiments, and it is this reticulospinal tract injury, and likely vestibulospinaltract injury, that led to spasticity in mammals [20]. Various authors are also looking at more peripheral explanations for spasticity. Different types of inhibition have been described by Myklebust et al. [55]: reciprocal Ia inhibition; presynaptic inhibition; recurrent inhibition; group II afferent inhibition and Golgi tendon organ inhibition [24]. The interneuron, that acts on the Ia afferent, is also influenced by corticospinal tracts [56]. Myklebust [55] also showed that if there is impaired reciprocal inhibition, abnormal activation of opposing muscle groups will lead to co-contraction or reciprocal activation of muscle. Therefore, reduced presynaptic inhibition of Ia fibers can lead to spasticity. This inhibition is mediated by Gamma amino butyric acid (GABA) [24]. This inhibitory effect of GABA, and the contribution it has on spasticity, is also a target for ongoing research. Key to our understanding of spasticity today is, however, the injury to the reticulospinal tract and its role in dampening of muscle activity [20].
As is evident from the above discussion, we are still far from understanding the exact mechanism of spasticity. There are ample opportunities for further research and management strategies.The major drawback is likely our lack of an adequate computational or animal model of spasticity.
Current Practice in Cape Town
The authors currently perform a classical “Peacock technique” with a laminoplasty technique from L2 to L5 where the laminae are kept attached at the rostral level and reflected during the procedure, to be fixed in place after dural closure. We also perform a “super selective” fascicular sectioning based on detailed electrophysiological mapping techniques and a detailed clinical examination. Selective Botulinum toxin injection as part of the preoperative workup forms part of the decision making process. This allows for testing of the “biomechanical hypothesis” (the theory of the biomechanical cause and therefore the major muscles involved in the movement disorder of the specific patient) before a permanent lesion is created. In this way, the surgeon has time to evaluate weakness and functional deterioration, or improvement prior to committing to SDR or selective peripheral neurotomy (SPN). Combination procedures, where an SDR is followed by SPN to alleviate focal residual spasticity is also an option, as this allows a more conservative approach with the SDR that allows for sparing of quadriceps and tibialis anterior, but the problematic hamstring or gastrocnemius and tibialis posterior spastic component can be treated afterwards with SPN aimed at these muscles in isolation if needed - again, after Botulinum toxin testing.
The Future?
A great deal of work has focused on intraoperative neuromonitoring and its usefulness in surgical decision making during SDR [57]. In the next few years, it is hoped that surgical management will be able to make another quantum leap, where surgery may be able to address the cause of spasticity and not only treat the symptoms. Other strategies, such as stem cells, or neuromodulatory techniques may also hold some new answers. Lesioning techniques, such as SDR, will never be obsolete, as the burden of disease is too great and the cost of newer therapies too high for developing countries to let go of effective lesioning techniques altogether. Further understanding is required in the physiology of spasticity, as well as the ways that one can alter those physiological abnormalities, to improve the function and quality of life in patients with cerebral palsy and other spastic conditions.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Electronic supplementary material
(PDF 2456 kb)
References
- 1.Sherrington CS. On reciprocal innervation of antagonistic muscles. Third note, Proceedings of the Royal Society of London. 1897;60:414–417. doi: 10.1098/rspl.1896.0062. [DOI] [Google Scholar]
- 2.Sherrington CS. On the reciprocal innervation of antagonistic muscles. Fifth note. Proceedings of the Royal Society of London. 1899;64:179–181. doi: 10.1098/rspl.1898.0090. [DOI] [Google Scholar]
- 3.Sherrington CS. On reciprocal innervation of antagonistic muscles.─ Tenth note. Proc. R. Soc. Lond. B. 1907;79:337–349. doi: 10.1098/rspb.1907.0026. [DOI] [Google Scholar]
- 4.Sherrington CS. Reciprocal innervation of antagonistic muscles. Thirteenth note.―On the antagonism between reflex inhibition and reflex excitation. Proc. R. Soc. Lond. B. 1908;80:565–578. doi: 10.1098/rspb.1908.0053. [DOI] [Google Scholar]
- 5.Sherrington CS. Reciprocal innervation of antagonistic muscles. Fourteenth note.-On double reciprocal innervation. Proc. R. Soc. Lond. B. 1909;81:249–268. doi: 10.1098/rspb.1909.0022. [DOI] [Google Scholar]
- 6.Sherrington CS. Flexion-reflex of the limb, crossed extension-reflex, and reflex stepping and standing. The Journal of physiology. 1910;40:28–121. doi: 10.1113/jphysiol.1910.sp001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sherrington CS. Nervous rhythm arising from rivalry of antagonistic reflexes: reflex stepping as outcome of double reciprocal innervation. Proc. R. Soc. Lond. B. 1913;86:233–261. doi: 10.1098/rspb.1913.0020. [DOI] [Google Scholar]
- 8.Peacock WJ, Staudt LA. Selective posterior rhizotomy: evolution of theory and practice. Pediatric neurosurgery. 1991;17:128–134. doi: 10.1159/000120582. [DOI] [PubMed] [Google Scholar]
- 9.Park TS, Gaffney PE, Kaufman BA, Molleston MC. Selective lumbosacral dorsal rhizotomy immediately caudal to the conus medullaris for cerebral palsy spasticity. Neurosurgery. 1993;33:929–934. doi: 10.1227/00006123-199311000-00026. [DOI] [PubMed] [Google Scholar]
- 10.Fasano VA, Barolat-Romana G, Zeme S, Sguazzi A. Electrophysiological assessment of spinal circuits in spasticity by direct dorsal root stimulation. Neurosurgery. 1979;4:146–151. doi: 10.1227/00006123-197902000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Gros C, Ouaknine G, Vlahovitch B, Frerebeau P. La radicotomie sélective postérieure dans le traitement neuro-chirurgical de lhypertonie pyramidale. Neurochirurgie. 1967;13:505. [PubMed] [Google Scholar]
- 12.Abbe R. Resection of the posterior roots of spinal nerves to relieve pain, pain reflex, athetosis, and spastic paralysis: Dana's operation. Med Rec. 1911;79:377–381. [Google Scholar]
- 13.Bennett WH. A case in which acute spasmodic pain in the left lower extremity was completely relieved by sub-dural division of the posterior roots of certain spinal nerves, all other treatment having proved useless. Death from sudden collapse and cerebral hæmorrhage on the twelfth day after the operation, at the commencement of apparent convalescence. Medico-chirurgical transactions. 1889;72:329. doi: 10.1177/095952878907200119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lorenz F. Uber chirurgische Behandlung der angeborenen spastischen Gliedstare. Wien Klin Rdsch. 1887;21:25–27. [Google Scholar]
- 15.Matsuo T, Tada S, Hajime T. Insufficiency of the hip adductor after anterior obturator neurectomy in 42 children with cerebral palsy. Journal of pediatric orthopedics. 1986;6:686–692. doi: 10.1097/01241398-198611000-00008. [DOI] [PubMed] [Google Scholar]
- 16.C.Gros. Spasticity—clinical classification and surgical treatment, Advances and technical standards in neurosurgery, Springer1979, pp. 55–97.
- 17.P. Mertens, M. Sindou. Selective peripheral neurotomies for the treatment of spasticity. Neurosurgery for spasticity, Springer1991, pp. 119–132.
- 18.Sindou M, Abdennebi B, Sharkey P. Microsurgical selective procedures in peripheral nerves and the posterior root-spinal cord junction for spasticity. Stereotactic and Functional Neurosurgery. 1985;48:97–104. doi: 10.1159/000101110. [DOI] [PubMed] [Google Scholar]
- 19.Sherrington C. Decerebrate rigidity, and reflex coordination of movements. The Journal of physiology. 1898;22:319–332. doi: 10.1113/jphysiol.1898.sp000697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheean G. The pathophysiology of spasticity. European journal of neurology. 2002;9:3–9. doi: 10.1046/j.1468-1331.2002.0090s1003.x. [DOI] [PubMed] [Google Scholar]
- 21.P.Foerster. Resection of the posterior spinal nerve-roots in the treatment of gastric crises and spastic paralysis, SAGE Publications, 1911. [PMC free article] [PubMed]
- 22.Privat J, Benezech J, Frerebeau P, Gros C. Sectorial posterior rhizotomy, a new technique of surgical treatment for spasticity. Acta neurochirurgica. 1976;35:181–195. doi: 10.1007/BF01405946. [DOI] [PubMed] [Google Scholar]
- 23.Foerster O. On the indications and results of the excision of posterior spinal nerve roots in men. Surg Gynecol Obstet. 1913;16:463–475. [Google Scholar]
- 24.Smyth MD, Peacock WJ. The surgical treatment of spasticity. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2000;23:153–163. doi: 10.1002/(SICI)1097-4598(200002)23:2<153::AID-MUS3>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 25.Sindou M. Microsurgical DREZotomy (MDT) for pain, spasticity, and hyperactive bladder: a 20-year experience. Acta neurochirurgica. 1995;137:1–5. doi: 10.1007/BF02188771. [DOI] [PubMed] [Google Scholar]
- 26.Sindou M, Fischer G, Goutelle A, Schott B, Mansuy L. La radicellotomie postérieure sélective dans le traitement des spasticités. Rev Neurol. 1974;130:201–216. [PubMed] [Google Scholar]
- 27.Fasano V, Broggi G, Barolat-Romana G, Sguazzi A. Surgical treatment of spasticity in cerebral palsy. Pediatric Neurosurgery. 1978;4:289–305. doi: 10.1159/000119785. [DOI] [PubMed] [Google Scholar]
- 28.Abbott R, Forem SL, Johann M. Selective posterior rhizotomy for the treatment of spasticity: a review. Child's Nervous System. 1989;5:337–346. doi: 10.1007/BF00271889. [DOI] [PubMed] [Google Scholar]
- 29.Barolat G. Dorsal selective rhizotomy through a limited exposure of the cauda equina at L-1. Journal of neurosurgery. 1991;75:804–807. doi: 10.3171/jns.1991.75.5.0804. [DOI] [PubMed] [Google Scholar]
- 30.Langerak NG, Lamberts RP, Fieggen AG, Peter JC, Peacock WJ, Vaughan CL. Selective dorsal rhizotomy: long-term experience from Cape Town. Child's Nervous System. 2007;23:1003–1006. doi: 10.1007/s00381-007-0383-9. [DOI] [PubMed] [Google Scholar]
- 31.Langerak NG, Lamberts RP, Fieggen AG, Peter JC, Peacock WJ, Vaughan CL. Functional status of patients with cerebral palsy according to the International Classification of Functioning, Disability and Health model: a 20-year follow-up study after selective dorsal rhizotomy. Archives of physical medicine and rehabilitation. 2009;90:994–1003. doi: 10.1016/j.apmr.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 32.N.G.Langerak, R.P.Lamberts, A.G.Fieggen, J.C.Peter, L.van derMerwe, W.J.Peacock, C.L.Vaughan. A prospective gait analysis study in patients with diplegic cerebral palsy 20 years after selective dorsal rhizotomy, DOI (2008). [DOI] [PubMed]
- 33.Langerak NG, Tam N, Vaughan CL, Fieggen AG, Schwartz MH. Gait status 17–26 years after selective dorsal rhizotomy. Gait & posture. 2012;35:244–249. doi: 10.1016/j.gaitpost.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 34.Steinbok P, Hicdonmez T, Sawatzky B, Beauchamp R, Wickenheiser D. Spinal deformities after selective dorsal rhizotomy for spastic cerebral palsy. Journal of Neurosurgery: Pediatrics. 2005;102:363–373. doi: 10.3171/jns.2005.102.2.0363. [DOI] [PubMed] [Google Scholar]
- 35.Golan JD, Hall JA, O'Gorman G, Poulin C, Benaroch TE, Cantin M-A, Farmer J-P. Spinal deformities following selective dorsal rhizotomy. Journal of Neurosurgery: Pediatrics. 2007;106:441–449. doi: 10.3171/ped.2007.106.6.441. [DOI] [PubMed] [Google Scholar]
- 36.Turi M, Kalen V. The risk of spinal deformity after selective dorsal rhizotomy. Journal of Pediatric Orthopaedics. 2000;20:104. [PubMed] [Google Scholar]
- 37.Johnson MB, Goldstein L, Thomas SS, Piatt J, Aiona M, Sussman M. Spinal deformity after selective dorsal rhizotomy in ambulatory patients with cerebral palsy. Journal of Pediatric Orthopaedics. 2004;24:529–536. doi: 10.1097/01241398-200409000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Steinbok P. Selective dorsal rhizotomy for spastic cerebral palsy: a review. Child's nervous system. 2007;23:981–990. doi: 10.1007/s00381-007-0379-5. [DOI] [PubMed] [Google Scholar]
- 39.van Schie PE, Schothorst M, Dallmeijer AJ, Vermeulen RJ, van Ouwerkerk WJ, Strijers RL, Becher JG. Short-and long-term effects of selective dorsal rhizotomy on gross motor function in ambulatory children with spastic diplegia. Journal of Neurosurgery: Pediatrics. 2011;7:557–562. doi: 10.3171/2011.2.PEDS10452. [DOI] [PubMed] [Google Scholar]
- 40.Langerak NG, Vaughan CL, Hoffman EB, Figaji AA, Fieggen AG, Peter JC. Incidence of spinal abnormalities in patients with spastic diplegia 17 to 26 years after selective dorsal rhizotomy. Child's Nervous System. 2009;25:1593–1603. doi: 10.1007/s00381-009-0993-5. [DOI] [PubMed] [Google Scholar]
- 41.Park TS, Johnston JM. Surgical techniques of selective dorsal rhizotomy for spastic cerebral palsy. Neurosurgical focus. 2006;21:1–6. [PubMed] [Google Scholar]
- 42.Sindou M, Georgoulis G. Keyhole interlaminar dorsal rhizotomy for spastic diplegia in cerebral palsy. Acta neurochirurgica. 2015;157:1187–1196. doi: 10.1007/s00701-015-2453-1. [DOI] [PubMed] [Google Scholar]
- 43.Huang JC, Deletis V, Vodusek DB, Abbott R. Preservation of pudendal afferents in sacral rhizotomies. Neurosurgery. 1997;41:411–415. doi: 10.1097/00006123-199708000-00015. [DOI] [PubMed] [Google Scholar]
- 44.Lang FF, Deletis V, Cohen HW, Velasquez L, Abbott R. Inclusion of the S2 dorsal rootlets in functional posterior rhizotomy for spasticity in children with cerebral palsy. Neurosurgery. 1994;34:847–853. doi: 10.1227/00006123-199405000-00009. [DOI] [PubMed] [Google Scholar]
- 45.Steinbok P, Kestle JR. Variation between centers in electrophysiologic techniques used in lumbosacral selective dorsal rhizotomy for spastic cerebral palsy. Pediatric neurosurgery. 1996;25:233–239. doi: 10.1159/000121131. [DOI] [PubMed] [Google Scholar]
- 46.Steinbok P, Gustavsson B, Kestle JR, Reiner A, Cochrane DD. Relationship of intraoperative electrophysiological criteria to outcome after selective functional posterior rhizotomy. Journal of neurosurgery. 1995;83:18–26. doi: 10.3171/jns.1995.83.1.0018. [DOI] [PubMed] [Google Scholar]
- 47.Sacco DJ, Tylkowski CM, Warf BC. Nonselective partial dorsal rhizotomy: a clinical experience with 1-year follow-up. Pediatric neurosurgery. 2000;32:114–118. doi: 10.1159/000028914. [DOI] [PubMed] [Google Scholar]
- 48.Pollack MA. Limited benefit of electrophysiological studies during dorsal rhizotomy. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 1994;17:553–555. doi: 10.1002/mus.880170514. [DOI] [PubMed] [Google Scholar]
- 49.T.Nishida, B.Storrs. Electrophysiological monitoring in selective posterior rhizotomy for spasticity: principles, techniques and interpretation of responses, Neurosurgery for Spasticity, Springer1991, pp. 159–163.
- 50.Steinbok P, Tidemann AJ, Miller S, Mortenson P, Bowen-Roberts T. Electrophysiologically guided versus non-electrophysiologically guided selective dorsal rhizotomy for spastic cerebral palsy: a comparison of outcomes. Child's Nervous System. 2009;25:1091–1096. doi: 10.1007/s00381-009-0908-5. [DOI] [PubMed] [Google Scholar]
- 51.Fukuhara T, Najm IM, Levin KH, Luciano MG, Brant CL. Nerve rootlets to be sectioned for spasticity resolution in selective dorsal rhizotomy. Surgical neurology. 2000;54:126–133. doi: 10.1016/S0090-3019(00)00282-2. [DOI] [PubMed] [Google Scholar]
- 52.Fukuhara T, Nakatsu D, Namba Y, Yamadori I. Histological evidence of intraoperative monitoring efficacy in selective dorsal rhizotomy. Child's Nervous System. 2011;27:1453–1458. doi: 10.1007/s00381-011-1462-5. [DOI] [PubMed] [Google Scholar]
- 53.Logigian EL, Soriano SG, Herrmann DN, Madsen JR. Gentle dorsal root retraction and dissection can cause areflexia: implications for intraoperative monitoring during “selective” partial dorsal rhizotomy. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2001;24:1352–1358. doi: 10.1002/mus.1155. [DOI] [PubMed] [Google Scholar]
- 54.Grunt S, Fieggen AG, Vermeulen RJ, Becher JG, Langerak NG. Selection criteria for selective dorsal rhizotomy in children with spastic cerebral palsy: a systematic review of the literature. Developmental Medicine & Child Neurology. 2014;56:302–312. doi: 10.1111/dmcn.12277. [DOI] [PubMed] [Google Scholar]
- 55.Myklebust BM, Gottlieb GL, Penn RD, Agarwal GC. Reciprocal excitation of antagonistic muscles as a differentiating feature in spasticity, Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology. Society. 1982;12:367–374. doi: 10.1002/ana.410120409. [DOI] [PubMed] [Google Scholar]
- 56.Burke D. Spasticity as an adaptation to pyramidal tract injury. Advances in neurology. 1988;47:401–423. [PubMed] [Google Scholar]
- 57.G.Georgoulis, A.Brînzeu, M.Sindou. Dorsal rhizotomy for children with spastic diplegia of cerebral palsy origin: usefulness of intraoperative monitoring. Journal of Neurosurgery: Pediatrics, DOI (2018) 1–13. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 2456 kb)