Spousal caregivers who report greater purpose in life have fewer care-related difficulties, especially when care recipients report low purpose in life.
Keywords: Caregiving, Disability, Purpose in life, Spouses
Abstract
Background
Greater feelings of purpose in life are associated with better health and may reduce the negative impact of chronic stress. Yet little is known about how purpose in life may buffer the negative effects of caregiving, a common chronic stressor in middle and later life.
Methods
This cross-sectional study utilized a U.S. sample of 315 spousal caregivers and their partners with functional disability drawn from the 2011 National Health and Aging Trends Study and National Study of Caregiving to examine how both parties’ perceptions of purpose in life are associated with caregivers’ emotional and physical caregiving difficulties. We also evaluated whether care recipients’ purpose in life moderates the association between caregivers’ purpose in life and care-related difficulties. Finally, we considered whether these links differed by caregiver gender. Models controlled for caregivers’ sociodemographics, care tasks, support resources, valued activity participation, and each care partner’s health conditions.
Results
Caregivers’ greater purpose in life was significantly linked to fewer physical caregiving difficulties. Caregivers’ greater purpose in life was significantly associated with fewer emotional care-related difficulties among caregiving wives and when care recipients’ purpose in life was low.
Conclusions
Although the associations between purpose in life and care-related difficulties are likely bidirectional, purpose in life may represent an important resource for combating the adverse consequences of caregiving. This study highlights the value of considering personal resources and their implications for caregivers’ well-being within a dyadic context.
Introduction
Feelings of purpose in life (e.g., the belief that one’s life has direction and meaning) have significant implications for health and well-being in middle and older adulthood [1]. Prospective studies show that a stronger sense of life purpose is linked to a lower incidence of depression [2], sleep disturbances [3, 4], disability [5, 6], cognitive decline [7, 8], myocardial infarction [9], stroke [10], and mortality [6, 11–13]. Greater purpose in life is also associated with reduced health risk according to biological indicators (e.g., C-reactive protein, allostatic load) in cross-sectional [14, 15] and longitudinal [16] research. These health benefits may in part be attributed to less physiological reactivity to stressors [17], along with the use of more proactive coping strategies [18–21] among people who perceive greater life purpose. Consequently, feelings of purpose in life may be a critical psychological resource that buffers the adverse effects of stressors encountered in one’s middle and later years.
One relatively common stressor in midlife and later life is the experience of caring for a partner with functional disability [22]. Nearly 18 million U.S. adults give unpaid care to a person aged 65 years or older due to reduced physical, mental, or cognitive capacities, and spouses are usually first in line to provide this assistance [23, 24]. Although spousal caregiving may be viewed as a natural part of one’s marital commitment, it can take a heavy emotional and physical toll. The vast majority of spousal caregivers live in the same household as their impaired partner, and so they are constantly and chronically exposed to stressors related to caregiving (e.g., care tasks) and their partner’s poor health with potentially few opportunities for respite [23]. Spousal caregivers also typically have limited personal resources to cope with caregiving stress. Compared with nonspouse caregivers (e.g., adult children), caregiving spouses are older and have less education, lower incomes, worse mental and physical health, and fewer sources of social support [23, 25–28]. Strikingly, most caregiving spouses (56%) earn less than $50,000 per year and more than half (58%) report no help from family, friends, or home care aides in managing their care responsibilities [23].
According to stress process models of caregiving, care-related stress often leads to emotional and physical problems [22]. Indeed, national estimates reveal that emotional and physical caregiving difficulties (i.e., self-appraisals of caregiving as emotionally or physically challenging) are prevalent, with roughly one in five U.S. caregivers reporting physical difficulties and two in five reporting emotional difficulties [29, 30]. Such difficulties are operationalized and measured in a number of ways, such as elements of subjective caregiver burden and caregiving strain [24]. The experience of caregiving difficulties is a major public health concern because these difficulties pose substantial threats to caregivers’ long-term well-being including more frequent sleep disturbances and worse self-care behaviors (e.g., smoking, lack of exercise), along with higher rates of depression, chronic health conditions, and mortality [26, 30–32].
Stress process theorists propose, however, that the degree to which caregivers encounter emotional and physical difficulties depends partly on their use and availability of personal resources to cope with care-related stress [22, 33]. Caregivers’ greater feelings of self-efficacy, for example, are concurrently associated with less perceived difficulty with care tasks [34] and have been found to attenuate the impact of caregiving stress on psychological well-being [35] and proinflammatory cytokine interleukin (IL)-6, a known risk biomarker for cardiovascular disease [36]. Likewise, cross-sectional research shows that caregivers’ greater feelings of purpose in life have been linked to lower depressive symptoms [37], less caregiving burden or strain [38, 39], and better overall health [40]. As such, spousal caregivers who report more purpose in life may experience fewer emotional and physical caregiving difficulties. Prior research on caregivers’ purpose in life has largely focused on Asian samples, perhaps due in part to the significance of finding and honoring one’s life purpose and/or to strong norms of family interconnectedness and care in many Eastern cultures [41]. Thus, it is not known whether feelings of purpose in life are linked to outcomes among U.S. caregivers. It is plausible, for instance, that the association between purpose in life and care-related difficulties may be somewhat weaker in the USA than in Asian countries due to less cultural emphasis on the fulfillment of social responsibilities (e.g., caregiving) as a primary contributor to well-being [41]. Nevertheless, given that spousal caregivers often have limited social and financial resources, their feelings of purpose in life may be a key personal resource that attenuates caregiving stress.
Care recipients’ feelings of purpose in life may also be consequential for care-related experiences. Interdependence theory proposes that spouses affect and are affected by one another’s everyday perceptions and behaviors [42]. In accordance with this perspective, studies of care dyads have shown that partners’ personal resources (e.g., self-efficacy, self-esteem, confidence) are associated with better health and well-being within dyads both concurrently [43, 44] and longitudinally [45–48]. A greater sense of life purpose among people with chronic health conditions has been linked to lower depressive symptoms at one point in time [18] and across a 2-year period [49], less disability, fatigue, and perceived decline in health [50, 51], greater psychosocial adjustment to illness [49, 52], and long-term physical and psychological improvements in recovery from surgery [19, 20]. Hence, when care recipients perceive more purpose in life, this may help mitigate caregivers’ emotional and physical care-related challenges. By contrast, when care recipients lack feelings of purpose, this may contribute to greater caregiving difficulties. Providing care for a partner with little hope may be particularly taxing for caregivers, and a caregiver with greater purpose in life may be more resilient when faced with this hardship than a caregiver with less purpose. Under such circumstances, caregivers’ own feelings purpose in life may become an especially critical personal resource in coping with the emotional and physical burdens of the care role.
Stress process perspectives on caregiving hold that men and women may differ in their experience of emotional and physical care-related difficulties [22, 33]. Relative to caregiving men, caregiving women tend to report more burden linked to their care role as well as worse mental and physical health [32, 53]. These gender differences may be partly explained by heightened care-related stressors (e.g., more hours of care and more caregiving tasks) and by fewer social resources (e.g., less help with care tasks or household chores) among caregiving women [53]. Considering women’s greater vulnerabilities to emotional and physical problems from the care role, perceptions of purpose in life within care dyads may be more salient in managing care-related difficulties for caregiving wives than for caregiving husbands.
In this study, we utilized a nationally representative U.S. sample of spousal caregivers and their partners with functional disability to explore the links between both parties’ feelings of purpose in life and caregivers’ emotional and physical caregiving difficulties. We also examined whether these associations differed by caregiver gender.
Study Aims and Hypotheses
This study had two major aims. First, we examined the links between spousal caregivers’ and care recipients’ feelings of purpose in life and caregivers’ reports of emotional and physical difficulties from their care role. On the basis of theoretical and empirical work indicating the stress-buffering role of purpose in life (17–21) and that personal resources in the care dyad may affect caregivers’ experience of care-related difficulties [43–48], we predicted the following:
(1) Caregivers’ greater perceptions of purpose in life will be linked to their own fewer emotional and physical caregiving difficulties.
(2) Care recipients’ greater perceptions of purpose in life will be linked to caregivers’ reports of fewer emotional and physical caregiving difficulties.
(3) These associations will be significantly stronger for caregiving wives than for caregiving husbands.
Second, we considered whether the associations between caregivers’ perceived purpose in life and caregiving difficulties are moderated by care recipients’ reports of purpose in life. To examine this second aim, we made the following predictions:
(4) The association between caregivers’ greater purpose in life and fewer caregiving difficulties will be stronger when care recipients’ reports of purpose in life are low.
(5) This association will be significantly stronger for caregiving wives than for caregiving husbands.
Methods
Participants and Procedures
The sample for this cross-sectional study included 315 community-dwelling adults aged 65 years and older with functional disability and their spousal caregivers drawn from the 2011 National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC). We did not seek ethical approval for this study, as we used publicly available secondary data with no individual identifiers. For this type of study, formal consent is not required.
Participants were eligible for NHATS if they were Medicare enrollees aged 65 years and older, resided in the contiguous USA, and received health-related assistance in the last month with any of the following: mobility, self-care activities (e.g., bathing, dressing), or household chores (e.g., laundry, shopping). Participants were recruited from a Medicare enrollment database using a stratified three-stage sampling design. In total, 14,643 Medicare enrollees were sampled. Of the 12,411 enrollees released to the field, 8,245 (71%) were interviewed in 2011 [54].
NHATS participants were also eligible for NSOC if they had at least one family member or nonpaid unrelated helper who helped them with one or more of the following due to health limitations: mobility, self-care, household chores, and medical care activities (e.g., managing medications). Of the 2,423 NHATS participants who were eligible for NSOC, there were 4,935 eligible caregivers. NHATS participants provided contact information for 3,362 (68.1%) of these caregivers. Of the 3,362 caregivers, 2,007 (59.7%) completed a 30-min telephone interview in the 2011 NSOC.
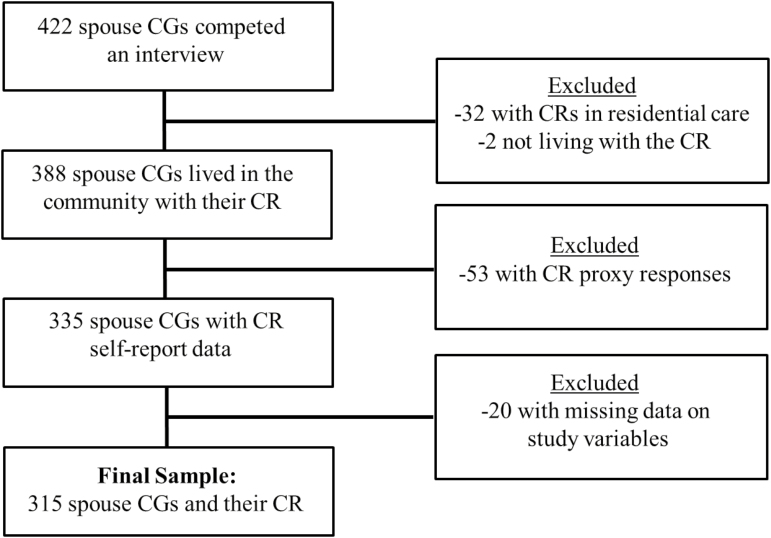
Of the 2,007 caregivers who participated in the NSOC, 422 caregiving spouses were interviewed. Fig. 1 presents a flow chart to illustrate the sample selection for this study. Our interest was in spousal caregivers of community-dwelling older adults who share a household; thus, we removed 32 caregivers whose care recipients lived in a residential care facility and two caregivers who did not live with their care recipient. In total, 388 caregivers lived with their care recipient in the community. We excluded 53 care dyads in which a proxy respondent was used for the care recipient due to illness, cognitive impairment, or problems with speech or hearing. Of the remaining 335 dyads, we removed 20 who were missing data on one or more study variables. Hence, we focused our analysis on 315 spousal caregivers and their care recipients (see Table 1 for background characteristics and scores on key variables). On average, these caregivers had been married to the care recipient for 42.75 years (SD = 17.81, range = 0–72). Compared with the 107 spousal caregivers who were removed, the 315 caregivers in this study were younger (t[418] = −3.05, p = .002), less educated (t[419] = −2.17, p = .03) and cared for care recipients with a higher number of chronic health conditions (t[420] = 3.26, p = .001), less purpose in life (t[88.49] = −2.94, p = .004), and a lower likelihood of having dementia (χ2 [1, N = 421] = 55.02, p < .001). There were no differences in caregivers’ reports of purpose in life or their perceived emotional and physical caregiving difficulties.
Fig. 1.
Flow chart showing selection of the analytic sample for this study. CG caregiver; CR care recipient.
Table 1.
Background characteristics and key variables for spousal caregivers
| Characteristics | Caregivers | |
|---|---|---|
| M | SD | |
| CG Age in years | 73.33 | 8.80 |
| CR Age in years | 76.41 | 7.15 |
| CG Chronic health conditions | 2.06 | 1.44 |
| CR Chronic health conditions | 3.10 | 1.44 |
| CG Valued activity participation | 2.11 | 1.18 |
| CG ADL/IADL assistance | 4.82 | 2.30 |
| CG Medical care activities | 4.78 | 3.12 |
| CG Purpose in life | 3.70 | 0.62 |
| CR Purpose in life | 2.77 | 0.46 |
| CG Emotional caregiving difficulties | 1.19 | 1.59 |
| CG Physical caregiving difficulties | 0.91 | 1.51 |
| Proportions | ||
| CG Female gender | 0.53 | |
| CG Educational attainment | ||
| High school graduate | 0.31 | |
| College graduate | 0.10 | |
| Post graduate | 0.07 | |
| CG Employed for pay | 0.16 | |
| CG Informal support | 0.44 | |
| CG Paid help | 0.17 | |
| CR Racial/ethnic minority | 0.24 | |
| CR Dementia status | 0.09 | |
N = 315 spousal care dyads.
ADL activities of daily living; CG caregiver; CR care recipient; IADL independent activities of daily living; SD standard deviation.
Measures
Purpose in Life
Perceptions of purpose in life were measured with an item adapted from the widely used Ryff Scales of Psychological Well-Being [55]. Caregivers and care recipients reported the extent to which they agreed with the statement, “My life has meaning and purpose”. Responses for caregivers ranged from 1 (disagree strongly) to 4 (agree strongly), whereas responses for care recipients ranged from 1 (agree not at all) to 3 (agree a lot). Mean scores were calculated, with higher scores reflecting greater feelings of purpose in life. The subscale from which this item is derived has shown high test–retest reliability, good construct validity, and strong concurrent correlations between shortened and full versions [56–58]. Although one-item measures are not ideal, single-item indicators of well-being (e.g., life satisfaction) have often demonstrated high validity and reliability [59–61].
Caregiving Difficulties
Consistent with prior research [30, 62], we examined caregivers’ own perceptions of emotional and physical caregiving difficulties. Caregivers were first asked whether it was emotionally or physically difficult to care for their spouse (1 = yes, 0 = no). Next, caregivers who reported difficulties were asked to describe their extent from 1 (a little difficult) to 5 (very difficult). For each type of difficulty, caregivers who did not report difficulties were given a score of zero and caregivers who reported difficulties were given a score based on their degree of difficulties (0 = no difficulty to 5 = high difficulty). Separate scores were calculated for emotional and physical difficulties.
Caregiver Gender
We considered caregiver gender (1 = female, 0 = male) to explore whether the associations in this study differed between caregiving wives and husbands.
Covariates
We controlled for caregivers’ age and educational attainment (1 = no schooling completed to 9 = masters, professional, or doctoral degree), both of which are linked to caregiving difficulties [22, 26]. We also controlled a range of additional factors that are associated with caregiving difficulties: caregivers’ own health conditions [25, 30], caregivers’ valued activity participation [30, 63], caregiving tasks [30, 62, 64], caregivers’ support resources [65], and care recipients’ health conditions and dementia status [28, 30].
Caregivers reported whether they had been diagnosed with seven chronic health conditions: arthritis, cancer, diabetes, heart disease, hypertension, lung disease, and osteoporosis (1 = yes, 0 = no). Summed scores were created.
Caregivers reported whether they participated in four types of activities in the last month: (a) visiting in person with friends/family; (b) attending religious services; (c) participating in club meetings/group activities; and (d) going out for enjoyment. Caregivers were then asked about the importance they placed on each activity (1 = not so important to 3 = very important). Summed scores for valued activity participation were determined from reports that caregivers participated in activities rated as somewhat or very important.
Caregivers indicated (1 = yes, 0 = no) whether they assisted with a series of care tasks. Activities of daily living (ADLs) included: bathing, dressing, eating, toileting, getting in/out of bed, and mobility inside and outside the house. Independent activities of daily living (IADLs) included: laundry, shopping, preparing meals, banking, and managing money. Medical care activities included: keeping track of medications, giving shots or injections, managing medical tasks (e.g., ostomy care, intravenous (IV), testing blood), helping with exercises, helping with a special diet, caring for skin wounds/sores, caring for teeth/dentures, caring for feet (e.g., clipping nails), ordering medication, scheduling medical appointments, speaking to medical providers, helping to change/add a health insurance or prescription drug plan, and other medical insurance matters. Summed scores were created for total ADL/IADL assistance and medical care activities.
Caregivers’ support resources were considered with two separate items. Informal support was assessed from caregivers’ reports on whether they have friends or family members who help them care for the care recipient (1 = yes, 0 = no). Paid help was measured with one item asking whether caregivers had used a paid helper to assist with care tasks within the past year (1 = yes, 0 = no).
Care recipients reported whether they had been diagnosed with eight chronic health conditions: arthritis, cancer, diabetes, heart disease, hypertension, lung disease, osteoporosis, and stroke (1 = yes, 0 = no). Summed scores were calculated. Care recipients’ dementia status (1 = dementia, 0 = no dementia) was determined from a self-reported physician diagnosis of Alzheimer’s disease or dementia.
Analytic Strategy
We estimated hierarchical linear regression models in SAS 9.4. Although we used data from both the caregiver and the care recipient as predictors, the outcome was caregivers’ reports of caregiving difficulties. Thus, the caregiver was the unit of analysis rather than the care dyad and the assumption of independence of observations was not violated [66]. In Step 1, we entered the covariates along with caregiver gender. We added caregivers’ and care recipients’ reports of purpose in life in Step 2 to examine their independent associations with caregiving difficulties. In Step 3, we entered two interaction terms (Caregiver Purpose in Life × Caregiver Gender; Care Recipient Purpose in Life × Caregiver Gender) to determine whether the associations between caregivers’ and care recipients’ reports of purpose in life and caregiving difficulties differed by caregiver gender. In Step 4, we entered an interaction term (Caregiver Purpose in Life × Care Recipient Purpose in Life) to examine whether the association between caregivers’ reports of purpose in life and care-related difficulties was moderated by care recipients’ reports of purpose in life. Interaction terms analyzed in Step 3 were not included in Step 4. In Step 5, we entered a three-way interaction term (Caregiver Purpose in Life × Care Recipient Purpose in Life × Caregiver Gender) to examine whether the moderating effect of care recipients’ reports of purpose in life differed by caregiver gender. The final model included all possible two-way interactions within the three-way interaction. Continuous variables were mean centered.
To explore the significant moderating effects of care recipients’ reports of purpose in life, we evaluated the statistical significance of the links between caregivers’ purpose in life and caregiving difficulties at one standard deviation above and below the mean of care recipients’ reports to represent high and low scores, respectively [67]. To adjust for multiple model comparisons, we used a Bonferroni correction (α/n, where α = .05 and n = 2 models) such that p values equal to or less than .025 were considered statistically significant.
Observations from NHATS and NSOC are weighted to adjust for different probabilities of sample selection and nonresponse. We focused on caregivers as the unit of analysis, and so we used the NSOC analytic weight in the models with statistical procedures to account for the complex survey design [68].
Results
Bivariate correlations among study variables were examined in preliminary analyses (see Table 2). Caregivers’ perceptions of purpose in life were significantly negatively correlated with emotional (r = −.27, p < .001) and physical (r = −.24, p < .001) caregiving difficulties. Likewise, care recipients’ greater perceptions of purpose in life were significantly correlated with fewer emotional caregiving difficulties (r = −.11, p = .05) and marginally correlated with fewer physical caregiving difficulties (r = −.11, p = .06). Caregivers’ and care recipients’ reports of purpose in life were significantly positively correlated (r = .19, p = .001).
Table 2.
Pearson correlations among key study variables
| Variable | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. CG Age | |||||
| 2. CG Gender (female) | −.31** | ||||
| 3. CG Purpose in life | −.02 | −.04 | |||
| 4. CR Purpose in life | −.08 | −.05 | .19** | ||
| 5. CG Emotional caregiving difficulties | −.09 | .29** | −.27** | −.11* | |
| 6. CG Physical caregiving difficulties | −.03 | .24** | −.24** | −.11 | .54** |
N = 315 spousal care dyads.
CG caregiver; CR care recipient.
*p ≤ .05. **p ≤ .001.
We also considered bivariate links between caregivers’ purpose in life and model covariates. Caregivers’ greater purpose in life was linked to their own fewer chronic health conditions (r = −.15, p = .01) and greater participation in valued activities (r = .15, p = .01), demonstrating that the purpose in life measure has construct validity.
Independent t-tests revealed no significant differences between caregiving wives and husbands in caregiver or care recipient reports of purpose in life. Wives, however, reported significantly more emotional (t[301.06] = 5.53, p < .001) and physical (t[291.87] = 4.38, p < .001) care-related difficulties.
Parameter estimates from the hierarchical models are shown in Table 3. We present unstandardized and standardized coefficients along with the accounted variance from each step of the models for emotional and physical caregiving difficulties.
Table 3.
Associations between perceptions of purpose in life within spousal care dyads and caregivers’ caregiving difficulties
| Predictor | Emotional caregiving difficulties | Physical caregiving difficulties | ||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | β | ΔR 2 | B | SE | β | ΔR 2 | |
| Step 1 | .18 | .15 | ||||||
| CG Age | −.01 | .01 | −.05 | −.003 | .01 | −.02 | ||
| CG Gender (female) | .56* | .23 | .18 | .26 | .23 | .09 | ||
| CG Educational attainment | .13** | .05 | .17 | .10 | .05 | .13 | ||
| CG Chronic health conditions | .17* | .07 | .16 | .16 | .07 | .16 | ||
| CG Valued activity participation | .02 | .10 | .01 | −.06 | .09 | −.05 | ||
| CG ADL/IADL assistance | .01 | .04 | .01 | .06 | .05 | .09 | ||
| CG Medical care activities | .09** | .03 | .18 | .10*** | .03 | .21 | ||
| CG Informal support | −.12 | .16 | −.04 | .15 | .18 | .05 | ||
| CG Paid help | .16 | .26 | .04 | .06 | .24 | .02 | ||
| CR Dementia status | .37 | .31 | .06 | .04 | .29 | .01 | ||
| CR Chronic health conditions | .13* | .05 | .12 | .08 | .06 | .08 | ||
| Step 2 | .05 | .03 | ||||||
| CG Purpose in life | −.52*** | .14 | −.20 | −.39* | .17 | −.16 | ||
| CR Purpose in life | −.29 | .25 | −.09 | −.28 | .28 | −.09 | ||
| Step 3 | .02 | .004 | ||||||
| CG Purpose in life × CG Gender | −.78** | .28 | −.22 | −.25 | .29 | −.08 | ||
| CR Purpose in life × CG Gender | .48 | .51 | .10 | .39 | .47 | .09 | ||
| Step 4 | .03 | .004 | ||||||
| CG Purpose in life × CR Purpose in life | .80** | .29 | .18 | .31 | .33 | .07 | ||
| Step 5 | .03 | .004 | ||||||
| CG Purpose in life × CR Purpose in life × CG Gender | −1.30 | .58 | −.24 | .16 | .73 | .03 | ||
| Total R2 | .28 | .20 | ||||||
Parameters are presented at each step of the model. Interaction terms in Step 3 were not included in Step 4. Step 5 included all possible two-way interaction terms within the three-way interaction.
N = 315 spousal care dyads.
CG caregiver; CR care recipient; ADL/IADL activities of daily living/instrumental activities of daily living.
*p ≤ .025. **p ≤ .01. ***p ≤ .001.
Perceptions of Purpose in Life Within Care Dyads and Caregiving Difficulties
Emotional Difficulties
As shown in Table 3, higher caregiver purpose in life was linked to significantly fewer emotional caregiving difficulties (B = −.52, β = −.20, p = .001). This association was moderated by caregiver gender (B = −.78, β = −.22, p = .01). Specifically, caregivers’ greater purpose in life was significantly associated with fewer emotional difficulties for caregiving wives (B = −.90, β = −.35, p < .001) but not for caregiving husbands (B = −.12, β = −.05, p = .56). In other words, for caregiving wives, a 1-point increase in purpose in life scores was associated with .90 less emotional difficulties (on a scale from 0 to 5). Care recipients’reports of purpose in life were not significantly linked to emotional caregiving difficulties.
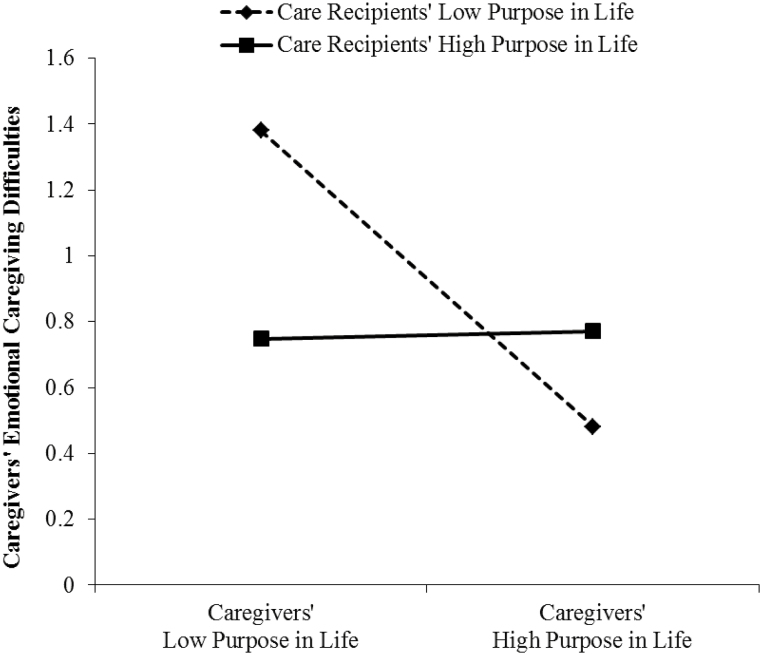
The association between caregivers’ own purpose in life and emotional caregiving difficulties was moderated by care recipients’ reports of purpose in life (B = .80, β = .18, p = .01). Caregivers’ greater feelings of purpose were significantly associated with fewer emotional difficulties when care recipients perceived low (B = −.73, β = −.28, p < .001) rather than high (B = .02, β = .01, p = .94) levels of purpose in life (Fig. 2). Therefore, when care recipients reported low life purpose, a 1-point increase in caregivers’ own purpose in life scores was associated with .73 less emotional difficulties (on a scale from 0 to 5).
Fig. 2.
The moderating effect of care recipients’ perceptions of purpose in life on the association between caregivers’ own perceptions of purpose in life and their emotional caregiving difficulties.
Physical Difficulties
Table 3 shows that caregivers’ own greater purpose in life was significantly associated with fewer physical caregiving difficulties (B = −.39, β = −.16, p = .02). Thus, a 1-point increase in caregivers’ purpose in life scores was associated with .39 less physical caregiving difficulties (on a scale from 0 to 5). This link did not differ by caregiver gender. Care recipients’ reports of purpose in life were not significantly associated with physical care-related difficulties. Likewise, the association between caregivers’ own purpose in life and their physical caregiving difficulties was not moderated by care recipients’ perceptions of purpose in life.
Discussion
This study provides evidence that perceptions of purpose in life within spousal care dyads are linked to caregivers’ experience of emotional and physical caregiving difficulties. We extend research on the caregiving stress process by demonstrating that caregivers’ and care recipients’ reports of their life purpose appear to be important psychosocial resources for spousal caregivers, independent of their sociodemographics, care activities, support resources, valued activity participation, and both care partners’ health conditions. Overall, findings imply that caregivers’ greater feelings of purpose in life are associated with fewer caregiving difficulties, but these associations are partly shaped by gender and by care recipients’ views of their own life purpose.
With regard to emotional caregiving difficulties, we found significant gender differences.
Specifically, caregivers’ stronger sense of purpose in life was linked to fewer emotional care-related difficulties for caregiving wives but not for caregiving husbands. These findings may be partly explained by gender distinctions in caregiving styles. Men typically maintain a sense of emotional detachment from caregiving, but women are often emotionally entrenched in the care situation [69]. Supporting this perspective, caregiving wives in this study reported significantly greater emotional care-related difficulties than caregiving husbands. Consequently, whereas husbands tend to draw on practical assistance (e.g., help with care tasks) from family members in managing their care role [69], wives may need to rely on personal resources (e.g., purpose in life) more frequently to cope with the emotional challenges of caregiving.
For both wives and husbands, however, caregivers who perceived more purpose in life reported significantly fewer physical caregiving difficulties. There are at least two possible reasons for this finding. First, the psychological benefits of purpose in life may make care tasks less of a physical effort. In accord with this possibility, those with a stronger sense of purpose tend to have more energy and may be more adept at proactively coping with challenges [18–21]. Second, spousal caregivers with more purpose in life may take better care of their own health, which renders them better able to perform their care tasks. Research indicates that people with greater life purpose have higher sleep quality and fewer sleep disturbances [3, 4], and engage in more frequent behaviors (e.g., exercise, regular check-ups) to promote and sustain good health [70–74]. Contrary to our hypothesis, the link between caregivers’ purpose in life and physical caregiving difficulties was not significantly stronger for caregiving wives than for caregiving husbands. Thus, despite prior studies showing women’s higher susceptibility to physical problems experienced in the care role [32, 53], the present findings suggest that both wives and husbands who report more purpose perceive less difficulty with physical aspects of caregiving.
The association between caregivers’ reports of purpose in life and emotional caregiving difficulties varied by care recipients’ perceived purpose in life. More precisely, when care recipients reported low levels of purpose in life, caregivers’ greater perceptions of their own life purpose were associated with fewer emotional care-related difficulties. By contrast, when care recipients reported high levels of purpose, caregivers’ own views of purpose were unrelated to these difficulties. As such, spousal caregivers’ feelings of purpose in life may become a more salient personal resource in managing the emotional burdens of caregiving when their care recipient lacks this resource.
We speculate that several factors may account for this finding. Previous research has shown that exposure to the care recipient’s suffering—including a loss of fulfillment or engagement with life—is linked to caregivers’ elevated psychological distress [75, 76]. It is plausible, then, that caregivers’ own strong feelings of purpose may make them more resilient to the negative emotional consequences of their partner’s low sense of purpose. Additionally, given the interdependence in mental health within spousal care dyads [43, 46], such resilience among caregivers may help to prevent further deterioration in care recipients’ well-being that could exacerbate emotional caregiving difficulties. Interestingly, there were no significant gender differences, indicating that both wives’ and husbands’ perceptions of purpose in life may help to counteract the adverse emotional implications of their partner’s diminished sense of purpose. It is worth noting that this pattern was not found for physical caregiving difficulties. One possible explanation is that, although care recipients’ low sense of life purpose may be emotionally distressing, these feelings are unlikely to have a direct impact on the everyday physical challenges of caregiving (e.g., helping the care recipient in and out of bed).
The cross-sectional nature of this study raises the question of whether spousal caregivers who experience more caregiving difficulties tend to perceive their lives as less purposeful due to compromised emotional and/or physical capacities. Research indicates, for example, that adults with minor depression report significantly less purpose in life relative to community averages [77]. Furthermore, there may be reciprocal associations between caregivers’ feelings purpose in life and care-related difficulties. Future work is needed to elucidate understanding of how the associations in this study develop over time.
Strengths of this study include a nationally representative sample of spousal caregivers and their partners with functional disability, data from both partners in the caregiving dyad, and the exploration of couple-level patterns of purpose in life and their associations with caregivers’ reports of emotional and physical care-related difficulties. Importantly, models controlled for sociodemographics, care activities, support resources, caregivers’ valued activity participation, and both care partners’ health conditions. Hence, caregivers’ and care recipients’ views of purpose in life demonstrated robust and independent associations with caregiving difficulties. Finally, the sample included a roughly equal proportion (47%) of caregiving men, who continue to be underrepresented in the literature despite comprising nearly half of spousal caregivers [23]. This study therefore sheds light on gender differences in the linkages between psychosocial resources within spousal care dyads and spouses’ caregiving difficulties.
Along with these strengths, we acknowledge several limitations. First, this study is cross-sectional, and so we are not able to determine causal associations. Second, consistent with other population-based studies [3, 16, 24], caregivers reported relatively low levels of care-related difficulties and high levels of purpose in life on average. As a consequence, the findings may not generalize to samples that tend to be highly distressed (e.g., dementia caregivers). Moreover, the restricted response range may have truncated the associations in this study; thus, our findings could be an underestimate of the links between purpose in life within spousal care dyads and caregivers’ care-related difficulties. Third, compared with the larger NSOC sample of spousal caregivers, caregivers in this study cared for partners with a higher number of chronic conditions and less purpose in life. The findings may therefore only apply to spousal caregivers of care recipients with higher medical morbidity and lower life purpose. Fourth, several key variables were assessed with a single item, limiting reliability and validity. Finally, the effect sizes were small to medium, accounting for 2%–5% of the variance in caregiving outcomes. Still, even small effects may have a large clinical and public health impact [78]. Taken as a whole, this study yields valuable insights and lays groundwork for subsequent studies to gain more in-depth knowledge of how purpose in life within spousal care dyads may contribute to spouses’ care-related experiences.
Conclusions
In summary, this study demonstrates that perceptions of purpose in life provide an important resource in the context of caregiving. The findings identify each partner’s views of purpose in life as personal resources for spousal caregivers, bolstering a growing literature that underscores the interdependence within couples managing chronic illness and disability [79, 80].
Spouses play a vital role in supporting older persons with functional disability so they can remain living in their own homes and communities [23]. Yet spouses also face heightened emotional and physical vulnerabilities to care-related stressors [23, 25–27]. Consequently, more research is needed to determine ways to minimize spouses’ caregiving difficulties. This study suggests that strategies to enhance and maintain caregivers’ feelings of purpose in their lives may be beneficial, perhaps particularly when care recipients lack a strong sense of purpose. Although additional work is needed to evaluate the clinical applications of this study, the present findings set the stage for future research to explore how perceptions of purpose in life within spousal care dyads may inform the development of proactive educational programs and interventions to support the health and well-being of caregiving spouses.
Compliance with Ethical Standards Statements
Conflict of Interest: Authors Polenick, Kales, and Birditt declare that they have no conflict of interest.
Authors’ Contributions: Author Polenick conceptualized and planned the study, conducted the statistical analyses, and wrote the paper. Authors Kales and Birditt assisted with the interpretation of the findings and critically revised the paper.
Ethical Approval: The authors did not seek ethical approval for this study, as publicly available secondary data were used with no individual identifiers. For this type of study, formal consent is not required.
Informed Consent: The National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC) obtained signed informed consent from participants prior to data collection.
Acknowledgments
Data from this study were presented in part at the Annual Meeting of the American Association of Geriatric Psychiatry, Dallas, TX, March 25, 2017. The National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC) are sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. This work was supported by training grant T32 MH073553-11 from the National Institute of Mental Health (Stephen J. Bartels, Principal Investigator).
References
- 1. Roepke AM, Jayawickreme E, Riffle OM. Meaning and health: a systematic review. Appl Res Qual Life. 2014;9:1055–1079. [Google Scholar]
- 2. Wood AM, Joseph S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten year cohort study. J Affect Disord. 2010;122(3):213–217. [DOI] [PubMed] [Google Scholar]
- 3. Kim ES, Hershner SD, Strecher VJ. Purpose in life and incidence of sleep disturbances. J Behav Med. 2015;38(3):590–597. [DOI] [PubMed] [Google Scholar]
- 4. Phelan CH, Love GD, Ryff CD, Brown RL, Heidrich SM. Psychosocial predictors of changing sleep patterns in aging women: a multiple pathway approach. Psychol Aging. 2010;25(4):858–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boyle PA, Buchman AS, Bennett DA. Purpose in life is associated with a reduced risk of incident disability among community-dwelling older persons. Am J Geriatr Psychiatry. 2010;18(12):1093–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zaslavsky O, Rillamas-Sun E, Woods NF et al. Association of the selected dimensions of eudaimonic well-being with healthy survival to 85 years of age in older women. Int Psychogeriatr. 2014;26(12):2081–2091. [DOI] [PubMed] [Google Scholar]
- 7. Boyle PA, Buchman AS, Wilson RS, Yu L, Schneider JA, Bennett DA. Effect of purpose in life on the relation between Alzheimer disease pathologic changes on cognitive function in advanced age. Arch Gen Psychiatry. 2012;69(5):499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilson RS, Boyle PA, Segawa E et al. The influence of cognitive decline on well-being in old age. Psychol Aging. 2013;28(2):304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C. Purpose in life and reduced risk of myocardial infarction among older U.S. adults with coronary heart disease: a two-year follow-up. J Behav Med. 2013;36(2):124–133. [DOI] [PubMed] [Google Scholar]
- 10. Kim ES, Sun JK, Park N, Peterson C. Purpose in life and reduced incidence of stroke in older adults: ‘The Health and Retirement Study’. J Psychosom Res. 2013;74(5):427–432. [DOI] [PubMed] [Google Scholar]
- 11. Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosom Med. 2009;71(5):574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Koizumi M, Ito H, Kaneko Y, Motohashi Y. Effect of having a sense of purpose in life on the risk of death from cardiovascular diseases. J Epidemiol. 2008;18(5):191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Krause N. Meaning in life and mortality. J Gerontol B Psychol Sci Soc Sci. 2009;64(4):517–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Friedman EM, Hayney M, Love GD, Singer BH, Ryff CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychol. 2007;26(3):305–313. [DOI] [PubMed] [Google Scholar]
- 15. Friedman EM, Ryff CD. Living well with medical comorbidities: a biopsychosocial perspective. J Gerontol B Psychol Sci Soc Sci. 2012;67(5):535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zilioli S, Slatcher RB, Ong AD, Gruenewald TL. Purpose in life predicts allostatic load ten years later. J Psychosom Res. 2015;79(5):451–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ishida R, Okawa M. Effects of a firm purpose in life on anxiety and sympathetic nervous activity caused by emotional stress: assessment by psycho-physiological method. Stress Health. 2006;22(4):275–281. [Google Scholar]
- 18. Peter C, Müller R, Post MW, van Leeuwen CM, Werner CS, Geyh S; Swiss Spinal Cord Injury Cohort Study Group Depression in spinal cord injury: assessing the role of psychological resources. Rehabil Psychol. 2015;60(1):67–80. [DOI] [PubMed] [Google Scholar]
- 19. Smith BW, Zautra AJ. Purpose in life and coping with knee-replacement surgery: occupation, participation and health. Occup Ther J Res. 2000;20(1 suppl 1):S96–S99. [Google Scholar]
- 20. Smith BW, Zautra AJ. The role of purpose in life in recovery from knee surgery. Int J Behav Med. 2004;11(4):197–202. [DOI] [PubMed] [Google Scholar]
- 21. Sougleris C, Ranzijn R. Proactive coping in community-dwelling older Australians. Int J Aging Hum Dev. 2011;72(2):155–168. [DOI] [PubMed] [Google Scholar]
- 22. Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ.. Profiles in Caregiving: The Unexpected Career. San Diego, CA: Academic Press; 1995. [Google Scholar]
- 23. Reinhard SC, Levine C, Samis S.. Family Caregivers Providing Complex Chronic Care to Their Spouses. Washington, DC: American Association of Retired Persons and United Hospital Fund; 2014. http://www.aarp.org/content/dam/aarp/research/public_policy_institute/health/2014/family-caregivers-providing-complex-chronic-care-spouses-AARP-ppi-health.pdf. [Google Scholar]
- 24. Schulz R, Eden J.. Families Caring for an Aging America. Washington, DC: The National Academies Press; 2016. http://www.nap.edu/23606 [PubMed] [Google Scholar]
- 25. Navaie-Waliser M, Feldman PH, Gould DA, Levine C, Kuerbis AN, Donelan K. When the caregiver needs care: the plight of vulnerable caregivers. Am J Public Health. 2002;92(3):409–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2007;62(2):P126–P137. [DOI] [PubMed] [Google Scholar]
- 27. Pinquart M, Sörensen S. Spouses, adult children, and children-in-law as caregivers of older adults: a meta-analytic comparison. Psychol Aging. 2011;26(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Oldenkamp M, Hagedoorn M, Slaets J, Stolk R, Wittek R, Smidt N. Subjective burden among spousal and adult-child informal caregivers of older adults: results from a longitudinal cohort study. BMC Geriatr. 2016;16(1):208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. National Alliance for Caregiving and the American Association of Retired Persons Public Policy Institute. Caregiving in the US; 2012. http://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf. [Google Scholar]
- 30. Spillman BC, Wolff J, Freedman VA et al. Informal Caregiving for Older Americans: An Analysis of the 2011 National Study of Caregiving. Washington, DC: U.S. Department of Health and Human Services; 2014. [Google Scholar]
- 31. Perkins M, Howard VJ, Wadley VG et al. Caregiving strain and all-cause mortality: evidence from the REGARDS study. J Gerontol B Psychol Sci Soc Sci. 2013;68(4):504–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003;129(6):946–972. [DOI] [PubMed] [Google Scholar]
- 33. Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–594. [DOI] [PubMed] [Google Scholar]
- 34. Giovannetti ER, Wolff JL, Xue QL et al. Difficulty assisting with health care tasks among caregivers of multimorbid older adults. J Gen Intern Med. 2012;27(1):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Romero-Moreno R, Losada A, Mausbach BT, Márquez-González M, Patterson TL, López J. Analysis of the moderating effect of self-efficacy domains in different points of the dementia caregiving process. Aging Ment Health. 2011;15(2):221–231. [DOI] [PubMed] [Google Scholar]
- 36. Mausbach BT, von Känel R, Roepke SK et al. Self-efficacy buffers the relationship between dementia caregiving stress and circulating concentrations of the proinflammatory cytokine interleukin-6. Am J Geriatr Psychiatry. 2011;19(1):64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chow EO, Ho HC. The relationship between psychological resources, social resources, and depression: results from older spousal caregivers in Hong Kong. Aging Ment Health. 2012;16(8):1016–1027. [DOI] [PubMed] [Google Scholar]
- 38. Chow EO, Ho CYH. Caregiver strain, age, and psychological well-being of older spousal caregivers in Hong Kong. J Soc Work. 2015;15(5):479–497. [Google Scholar]
- 39. Okamoto K, Harasawa Y. Predictor of increase in caregiver burden for disabled elderly at home. Arch Gerontol Geriatr. 2009;49(1):129–131. [DOI] [PubMed] [Google Scholar]
- 40. Stetz KM. The relationship among background characteristics, purpose in life, and caregiving demands on perceived health of spouse caregivers. Sch Inq Nurs Pract. 1989;3(2):133–153. [PubMed] [Google Scholar]
- 41. Ryff CD, Love GD, Miyamoto Y et al. Culture and the promotion of well-being in east and west: understanding varieties of attunement to the surrounding context. In: Fava GA, Ruini C, eds. Increasing Psychological Well-being in Clinical and Educational Settings: Interventions and Cultural Contexts. New York: Springer; 2014:1–19. [Google Scholar]
- 42. Rusbult CE, Van Lange PAM. Why we need interdependence theory. Soc Pers Psychol Comp. 2008;2(5):2049–2070. [Google Scholar]
- 43. Chung ML, Bakas T, Plue LD, Williams LS. Effects of self-esteem, optimism, and perceived control on depressive symptoms in stroke survivor-spouse dyads. J Cardiovasc Nurs. 2016;31(2):E8–E16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lyons KS, Vellone E, Lee CS et al. A dyadic approach to managing heart failure with confidence. J Cardiovasc Nurs. 2015;30(4suppl 1):S64–S71. [DOI] [PubMed] [Google Scholar]
- 45. Gere J, Martire LM, Keefe FJ, Stephens MA, Schulz R. Spouse confidence in self-efficacy for arthritis management predicts improved patient health. Ann Behav Med. 2014;48(3):337–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kershaw T, Ellis KR, Yoon H, Schafenacker A, Katapodi M, Northouse L. The interdependence of advanced cancer patients’ and their family caregivers’ mental health, physical health, and self-efficacy over time. Ann Behav Med. 2015;49(6):901–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Li LW, McLaughlin SJ. Caregiver confidence: does it predict changes in disability among elderly home care recipients? Gerontologist. 2012;52(1):79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rohrbaugh MJ, Shoham V, Coyne JC, Cranford JA, Sonnega JS, Nicklas JM. Beyond the “self” in self-efficacy: spouse confidence predicts patient survival following heart failure. J Fam Psychol. 2004;18(1):184–193. [DOI] [PubMed] [Google Scholar]
- 49. Dezutter J, Luyckx K, Wachholtz A. Meaning in life in chronic pain patients over time: associations with pain experience and psychological well-being. J Behav Med. 2015;38(2):384–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Harrison TC, Stuifbergen AK. Life purpose: effect on functional decline and quality of life in polio survivors. Rehabil Nurs. 2006;31(4):149–154. [DOI] [PubMed] [Google Scholar]
- 51. Schleicher H, Alonso C, Shirtcliff EA, Muller D, Loevinger BL, Coe CL. In the face of pain: the relationship between psychological well-being and disability in women with fibromyalgia. Psychother Psychosom. 2005;74(4):231–239. [DOI] [PubMed] [Google Scholar]
- 52. Schnoll RA, Harlow LL, Brower L. Spirituality, demographic and disease factors, and adjustment to cancer. Cancer Pract. 2000;8(6):298–304. [DOI] [PubMed] [Google Scholar]
- 53. Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):P33–P45. [DOI] [PubMed] [Google Scholar]
- 54. Montaquila J, Freedman VA, Edwards B, Kasper JD.. National Health and Aging Trends Study Round 1 Sample Design and Selection. NHATS Technical Paper #1. Baltimore, MD: Johns Hopkins University School of Public Health; 2012. https://www.nhats.org/scripts/sampling/NHATS%20Round%201%20Sample%20Design%2005_10_12.pdf. [Google Scholar]
- 55. Ryff C, Almeida DM, Ayanian JS et al. Midlife Development in the United States (MIDUS2), 2004–2006: Documentation of Scales, All Parts (ICPSR 4652) Inter-University Consortium for Political and Social Research. Ann Arbor, MI; 2006. [Google Scholar]
- 56. Cooke PJ, Melchert TP, Connor K. Measuring well-being: a review of instruments. Couns Psychol. 2016;44(5):730–757. [Google Scholar]
- 57. Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57(6):1069–1081. [Google Scholar]
- 58. Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–727. [DOI] [PubMed] [Google Scholar]
- 59. Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS. Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res. 2014;14:398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Cheung F, Lucas RE. Assessing the validity of single-item life satisfaction measures: results from three large samples. Qual Life Res. 2014;23(10):2809–2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lucas RE, Donnellan MB. Estimating the reliability of single-item life satisfaction measures: results from four national panel studies. Soc Indic Res. 2012;105(3):323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016;176(3):372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Schüz B, Czerniawski A, Davie N et al. Leisure time activities and mental health in informal dementia caregivers. Appl Psychol Health Well Being. 2015;7(2):230–248. [DOI] [PubMed] [Google Scholar]
- 64. Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2003;58(2):P112–P128. [DOI] [PubMed] [Google Scholar]
- 65. Zarit SH, Femia EE. A future for family care and dementia intervention research? Challenges and strategies. Aging Ment Health. 2008;12(1):5–13. [DOI] [PubMed] [Google Scholar]
- 66. Kenny DA, Cook W. Partner effects in relationship research: conceptual issues, analytic difficulties, and illustrations. Pers Relatsh. 1999;6(4):433–448. [Google Scholar]
- 67. Aiken LS, West SG.. Multiple Regression: Testing and Interpreting Interactions. London: Sage Publications; 1991. [Google Scholar]
- 68. Kasper JD, Freedman VA, Spillman B.. National Study of Caregiving User Guide. Baltimore, MD: Johns Hopkins University School of Public Health; 2013. https://www.nhats.org/scripts/documents%5CNSOC_Round_1_User_Guide.pdf. [Google Scholar]
- 69. Thompson EH. What’s Unique About Men’s Caregiving? Men as Caregivers: Theory, Research, and Service Implications. New York: Springer; 2002: 20–47. [Google Scholar]
- 70. Holahan CK, Holahan CJ, Suzuki R. Purposiveness, physical activity, and perceived health in cardiac patients. Disabil Rehabil. 2008;30(23):1772–1778. [DOI] [PubMed] [Google Scholar]
- 71. Holahan CK, Holahan CJ, Velasquez KE, Jung S, North RJ, Pahl SA. Purposiveness and leisure-time physical activity in women in early midlife. Women Health. 2011;51(7):661–675. [DOI] [PubMed] [Google Scholar]
- 72. Holahan CK, Suzuki R. Motivational factors in health promoting behavior in later aging. Act Adapt Aging. 2006;30(1):47–60. [Google Scholar]
- 73. Hooker SA, Masters KS. Purpose in life is associated with physical activity measured by accelerometer. J Health Psychol. 2016;21(6):962–971. [DOI] [PubMed] [Google Scholar]
- 74. Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proc Natl Acad Sci USA. 2014;111(46):16331–16336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Monin JK, Levy BR, Kane HS. To love is to suffer: older adults’ daily emotional contagion to perceived spousal suffering. J Gerontol B Psychol Sci Soc Sci. 2017;72(3):383–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Monin JK, Schulz R. Interpersonal effects of suffering in older adult caregiving relationships. Psychol Aging. 2009;24(3):681–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Nierenberg AA, Rapaport MH, Schettler PJ et al. Deficits in psychological well-being and quality-of-life in minor depression: implications for DSM-V. CNS Neurosci Ther. 2010;16(4):208–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Rutledge T, Loh C. Effect sizes and statistical testing in the determination of clinical significance in behavioral medicine research. Ann Behav Med. 2004;27(2):138–145. [DOI] [PubMed] [Google Scholar]
- 79. Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull. 2007;133(6):920–954. [DOI] [PubMed] [Google Scholar]
- 80. Revenson T, Griva K, Luszczynska A et al. Caregiving as a dyadic process. In: Revenson T, Griva K, Luszczynska A. et al. eds. Caregiving in the Illness Context. London: Palgrave MacMillian; 2016:25–37. [Google Scholar]