Abstract
Background
Uptake of health checks for cardiovascular risk assessment in primary care in England is lower than anticipated. The question-behavior effect (QBE) may offer a simple, scalable intervention to increase health check uptake.
Purpose
The present study aimed to evaluate the effectiveness of enhanced invitation methods employing the QBE, with or without a financial incentive to return the questionnaire, at increasing uptake of health checks.
Methods
We conducted a three-arm randomized trial including all patients at 18 general practices in two London boroughs, who were invited for health checks from July 2013 to December 2014. Participants were randomized to three trial arms: (i) Standard health check invitation letter only; (ii) QBE questionnaire followed by standard invitation letter; or (iii) QBE questionnaire with offer of a financial incentive to return the questionnaire, followed by standard invitation letter. In intention to treat analysis, the primary outcome of completion of health check within 6 months of invitation, was evaluated using a p value of .0167 for significance.
Results
12,459 participants were randomized. Health check uptake was evaluated for 12,052 (97%) with outcome data collected. Health check uptake within 6 months of invitation was: standard invitation, 590 / 4,095 (14.41%); QBE questionnaire, 630 / 3,988 (15.80%); QBE questionnaire and financial incentive, 629 / 3,969 (15.85%). Difference following QBE questionnaire, 1.43% (95% confidence interval −0.12 to 2.97%, p = .070); following QBE questionnaire and financial incentive, 1.52% (−0.03 to 3.07%, p = .054).
Conclusions
Uptake of health checks following a standard invitation was low and not significantly increased through enhanced invitation methods using the QBE.
Keywords: Primary prevention—methods, Cardiovascular diseases, Mass screening—methods, Randomized controlled trial, Electronic health records, Health behavior
In a large randomized controlled trial, enhanced invitation methods based on the question-behavior effect did not increase uptake of health checks
Introduction
A program of health checks for cardiovascular risk assessment has been rolled-out in England [1]. The program aims to identify people who are at increased risk of heart disease, stroke, diabetes or chronic kidney disease, with the intention of delivering individualized interventions to reduce risk. These target conditions are important health priorities in the UK and internationally [2–6]. The English Department of Health estimated that the health check program could potentially prevent 2,000 deaths and 9,500 nonfatal myocardial infarctions and strokes in England each year [1]. The health check is generally conducted by a nurse and includes assessment of blood pressure, smoking, serum total cholesterol and lifestyle behaviors enabling estimation of a cardiovascular disease risk score. Participants are provided with tailored advice according to their level of risk. The health check program was judged to be potentially cost-effective if 75% of eligible participants were to take up the offer of a check [7]. Health checks remain controversial because of the questionable evidence for the effectiveness of a health check program [8, 9], the variable organization and delivery of the program [10] and the small effects it may achieve [11]. Nevertheless, maximizing uptake of health checks remains important for realizing the aims of the health check program and ensuring that the existing health inequalities are not perpetuated.
The population eligible to be offered health checks comprises adults aged 40–74 years who have not been diagnosed with cardiovascular diseases and are not treated for elevated cardiovascular risk [1, 6]. The offer of a free health check is made through a nationally-recommended standard invitation letter, with a reminder letter to nonresponders at 3 months [12]. In most areas, patients are offered a choice of provider which may include local general practices, community pharmacies and outreach services. In addition, general practices may offer patients a health check when they attend the surgery for other reasons; these are referred to as “opportunistic” health checks. Nationally reported data for health check uptake, which include both invited and opportunistic health checks, show that the number of health checks performed as a percent of the number invited is now about 46% in England [13]. Local evaluations have confirmed a pattern of low uptake of health checks [14–16] but there is considerable variation between different areas. In the two London boroughs included in this study, nationally reported data now show health check uptake of 37% and 23%, respectively [13]. Qualitative studies have found that primary care professionals are concerned about potential social inequalities in health check uptake [16]. However, evidence to date is mixed, with two studies finding lower uptake among more deprived individuals [17, 18] and two not finding a significant association between deprivation and health check attendance [19, 20]. Nevertheless, any intervention targeting health check uptake needs to avoid increasing social disparities in uptake,
Given the large number of individuals invited for health checks, interventions to increase uptake need to be low cost and easily scalable. The “Question-Behavior Effect” (QBE) may provide one such method. The QBE is a behavior-change technique that draws on evidence suggesting that asking questions about beliefs towards a behavior increases the likelihood that individuals will later perform that behavior. In an early trial, conducted in a single general practice in rural England, Conner et al. [21] reported that sending a preliminary questionnaire, prior to inviting individuals for a health check, was associated with increased uptake, with rates of 68.3% in the intervention group compared to 53.5% in the control group. A number of mechanisms have been proposed for the operation of the QBE [22]. Recent meta-analyses [22–25], which were published after the inception of this trial, have suggested a range of effect size estimates for the QBE on behaviors similar to health check uptake. These reviews also found publication bias and highlighted methodological weaknesses of some previous studies; consequently, prospectively-registered randomized controlled trials (RCTs) of the QBE with low risk of bias are required to establish whether the QBE can be, “hugely valuable in social policy and public health terms” [25].
The QBE is greater among individuals who return a questionnaire [17] and financial incentives can increase questionnaire response rates [26, 27]. We hypothesized that the QBE might be employed to increase uptake of health checks. We also hypothesized that a financial incentive to return the QBE questionnaire might enhance the effect of the QBE on health check uptake. An incentive may also be particularly attractive to individuals experiencing higher deprivation.
We conducted a RCT with individual participants who were eligible for health checks as the unit of allocation. The trial compared the effects on health check uptake of a standard invitation letter alone; a QBE questionnaire followed by standard invitation 1 week later; a QBE questionnaire, with offer of retail voucher as incentive for questionnaire completion, followed by standard invitation 1 week later. The trial was conducted in a deprived, ethnically diverse area and the association of sociodemographic variables with health check uptake was also evaluated.
Methods
Setting
The trial was conducted in the London Boroughs of Lambeth and Lewisham. These are inner-city areas with significant socioeconomic deprivation and generally young multi-ethnic populations. The population of patients eligible for a health check is defined from analysis of electronic health records of participants registered with general practices in the two boroughs. The recruitment and invitation process is managed through a bespoke management information system called “Health Check Focus” managed by a shared administration team across South London Boroughs (which includes Lambeth and Lewisham). Each month a sample of eligible participants is drawn and included in a pre-notification list (PNL), which is sent to general practices for approval. Once the PNL is approved, all individuals listed are sent a standard health check invitation letter on general practice headed paper by a mailing company.
Trial Design
We conducted a three-arm superiority RCT with equal allocation to each trial arm. The trial interventions comprised: (i) standard invitation letter to attend an NHS health check; (ii) QBE questionnaire followed by standard invitation letter after 7 days; (iii) QBE Questionnaire and offer of a £5 retail voucher as incentive to return the questionnaire followed by standard invitation. Participants in all three trial arms received a standard reminder letter at 3 months if they did not respond to the initial invitation.
General Practice and Individual Participant Recruitment
There were 89 general practices in the two participating Boroughs that were eligible and 18 general practices were invited and agreed to participate in the trial. Participating general practices comprised a non-probability sample, selected by the study team based on their likely preparedness to engage in this research. We compared participating practices with non-trial practices in the same area. Trial practices tended to have larger patient list sizes than non-trial practices but showed similar levels of achievement of clinical performance metrics. Trial practice populations were similar with respect to social and material deprivation and proportion of non-White participants to the entire populations of the two boroughs [28]. Each practice participated in the trial for a minimum of 12 months to allow for seasonal variation in uptake of health checks. The lead GP or senior partner provided written informed consent for the participation of the practice population in the trial because individual patient consent was not feasible. All participants who were eligible to be invited for a health check were included in the trial. There were no exclusion criteria.
Individual participants were randomized to the three trial arms between July 2013 and December 2014. Recruitment and allocation were performed using electronic health records using two different methods. At 12 general practices, allocation was conducted by the research team each month using a randomization list generated by the trial statistician. Each month, all patients included on the practice-approved PNL were assigned simultaneously, using a computer-generated randomization list, stratified by general practice and month using permuted blocks of three. Randomization lists were generated using Stata command “ralloc” in Stata version 12 [29]. This was referred to as the “In-practice Method.” In order to evaluate a potentially more efficient method of delivering the trial, at six general practices, random allocation was programmed into the software of the health check management information system that controlled participant selection for health checks in Lambeth and Lewisham. This was referred to as the “Automated Method.” Simple randomization, stratified by practice and month, was employed to allocate participants to the three trial arms. During the first 2 months of use of the automated recruitment method, review of trial data showed that the correct allocation ratio was not being achieved and this required further adjustment to the software. The first 2 months were therefore considered to act as a pilot study and data from these months were excluded from the main trial analysis. The two randomization methods are compared in detail elsewhere [28].
Sample Size
We estimated that a relevant effect from the intervention would be an increase in uptake of at least 4%, judging that smaller increments would be too small to justify roll-out into the health check program. We estimated that if there were 4,263 participants in each trial arm, with 12,789 in total, this provided over 90% power to detect a difference in uptake of health checks between each active treatment arm and the standard intervention arm of at least 4%. These calculations were based on 5% significance level using a Bonferroni correction for three comparisons (i.e. p = .0167). Calculations were performed in Stata version 12 [29].
Blinding
Participants’ GPs provided consent to their participation in the trial and individual participants were not aware that there were other trial arms. The study team was blind to participant details during trial arm allocation and both allocation methods were considered to provide adequate allocation concealment. The study team was blind to group allocation during extraction of participant outcome data from GP records.
Intervention Rationale and Development
The development of the intervention has been described in more detail elsewhere [28, 30]. Following Conner et al. [17], the QBE questionnaire drew on the Theory of Planned Behavior (TPB) with additional items for anticipated regret [31]. As the present trial was implemented in a deprived area with probable low levels of literacy, questionnaire length was reduced, with two items for the three constructs thought key to the operation of the QBE (attitudes, intentions and anticipated regret) and one item each for subjective norms and perceived behavioral control (PBC). Attitudes items were, “For me, going for a Health Check in the next few weeks would be…” (rated “very worrying” to “very reassuring”) and, “For me, going for a Health Check in the next few weeks would be…,” rated “very bad” to “very good.” Intentions items were “I intend to go for a Health Check in the next few weeks,” rated from “strongly disagree” to “strongly agree” and, “Will I go for a Health Check in the next few weeks?” rated from “definitely no” to “definitely yes.” Anticipated regret was tapped with the items, “If I did not go for a Health Check in the next few weeks, I would feel regret” and “If I did not go for a Health Check in the next few weeks, I would later wish I had,” both rated “strongly disagree” to “strongly agree.” The PBC item was, “I’m confident I can go for a Health Check in the next few weeks,” (“strongly disagree” to “strongly agree”) while the subjective norms item was, “People who are important to me would (“completely disapprove” to “completely approve”) … of me having a Health Check in the next few weeks.” All items were rated on seven-point scales. The Flesch reading ease score was 80.1 and the Flesch-Kincaid grade level was 5.9. Questions were presented to be legible and clear to all readers in accordance with guidelines [32]. Table 1 shows all questions included in the questionnaire and corresponding constructs. The full, formatted questionnaire is shown in Supplementary Materials 1.
Table 1.
Intervention Questionnaire Items
| Construct | Item |
|---|---|
| Intentions | I intend to go for a Health Check in the next few weeks … strongly disagree/ strongly agree |
| Attitudes | For me, going for a Health Check in the next few weeks would be… very bad/ very good |
| Anticipated regret | If I did not go for a Health Check in the next few weeks, I would feel regret… strongly disagree/ strongly agree |
| Intentions | Will I go for a Health Check in the next few weeks? Definitely no/ definitely yes |
| Anticipated regret | If I did not go for a Health Check in the next few weeks, I would later wish I had … strongly disagree/ strongly agree |
| Attitudes | For me, going for a Health Check in the next few weeks would be… very worrying/ very reassuring |
| PBC (Self-efficacy) | I’m confident I can go for a Health Check in the next few weeks… strongly disagree/ strongly agree |
| Subjective norms | People who are important to me would… completely disapprove/ completely approve … of me going for a Health Check in the next few weeks |
A systematic review, including 94 trials with a pooled total of 160,004 participants, found that the odds of returning a postal questionnaire were almost doubled if a financial incentive was offered [26]. As the QBE is greater among individuals who return a questionnaire [17], incentivizing questionnaire return may increase the size of any effect of distributing a questionnaire on uptake of health checks. A meta-analysis of 85,671 participants in 88 randomized trials of financial incentives to increase response rates for mailed questionnaires reported a significant increase in response rates for incentives up to the value of $5 [27]. Participants were offered a £5 retail voucher known as “Love2Shop” that could be redeemed at a wide range of retail outlets appealing to a broad demographic.
The QBE questionnaire was sent out on un-headed paper, together with a covering letter headed with the logo of the participating Borough, signed by the health check programme clinical lead. A pre-paid envelope was included for questionnaire return.
Outcome Assessment
Outcome data were extracted from participant electronic health records by members of the research team using nationally specified READ codes (a coded thesaurus of clinical terms used consistently within the NHS on electronic patient records) to record completion of a health check. At the time of data extraction, participants’ postcodes were linked to the Indices of Multiple Deprivation 2010 score (IMD 2010) as a marker of deprivation. Data for gender, year of birth and practice-recorded ethnicity were also extracted. Data were extracted in a single batch for each practice between June 1, 2015 and July 2, 2015.
Analysis
Risk differences were estimated by fitting a marginal model with binomial family and identity link using the method of generalized estimating equations (GEE). A value of p < .0167 was used for significance to allow for multiple comparisons. Secondary analyses evaluated sub-groups of gender, age (40 to 59 and 60 to 74 years), ethnicity, and deprivation quintile.
Analyses also explored questionnaire return by trial arm and whether individuals who completed the questionnaire were more likely to subsequently attend a health check and to assess whether the impact of offering an incentive for return differed across deprivation quintile. Covariates in logistic models included the stratification variables month of invitation, year, questionnaire return (y/n), treatment arm, deprivation quintile and arm by deprivation quintile interaction. Robust variance estimates allowed for clustering by family practice. A Complier-Average Causal Effect (CACE) analysis was also performed to estimate the effect of the intervention on health check uptake in “compliers.” Compliers are defined as participants who returned a QBE questionnaire in either of the intervention arms, or who “would have” returned a questionnaire if they were in the standard invitation arm. Compliance status could be observed directly in the intervention trial arms but compliance status was latent or unobservable in the standard treatment trial arm. Use of randomization ensured that, on average, the proportion of compliers in the control group is the same as that in the treatment group. This means that we can estimate the proportion of unobserved compliers in the control group from the proportion observed in the treatment group. This analysis followed the approach laid out in Dunn et al [33]. As no participants were lost to follow up we were able to estimate the intervention effect without taking into account the missing data mechanism. An estimate of the standard error for the statistic was obtained through bootstrapping.
Analyses were conducted to evaluate possible associations of questionnaire constructs with subsequent health check uptake. If none of the constructs were significantly associated with uptake, then this would limit the potential impact of the QBE, which some hypothesize operates by making such beliefs more accessible. For intentions, attitudes and anticipated regret, pairwise correlations of relevant questionnaire items were evaluated prior to constructing scale scores as means of two items for further use in the analyses. Although correlations for the intentions and anticipated regret items were acceptable (r = .69 and r = .72, respectively), that for the attitudes items was lower (r = .53). These two items were therefore treated separately in further analyses, with the item rated “very worrying” to “very reassuring” reflecting affective attitudes and that rated “very bad” to “very good” reflecting instrumental attitudes. The association of each construct with health check uptake was evaluated in a logistic model, with the construct fitted as a linear predictor. Robust standard errors were estimated.
Research Ethics
The protocol for the trial was reviewed by the London Bridge Research Ethics Committee and approved on March 7 2013 (Reference 13/LO/0197). The London Bridge Research Ethics Committee is part of the Research Ethics Service of the National Health Service, Health Research Authority in England. It was not considered feasible to obtain individual participant consent for randomization. Obtaining consent, through a postal invitation, from individual participants before entering the study would have vitiated the QBE, as well as resulting in a sample that was likely to be highly biased with respect to the propensity to return a questionnaire or to participate in a health check. For this reason, we obtained consent from the senior partner at each general practice that participated in the study. This approach is commonly used in cluster randomized trials. Obtaining consent from an individual who has a stewardship role in respect of a group of individual participants was judged to be acceptable by the UK Medical Research Council in its recommendations on ethical issues in cluster randomization [34]. The approach was also applicable to the present study in which individual participant randomization was used.
Results
Main Trial Results
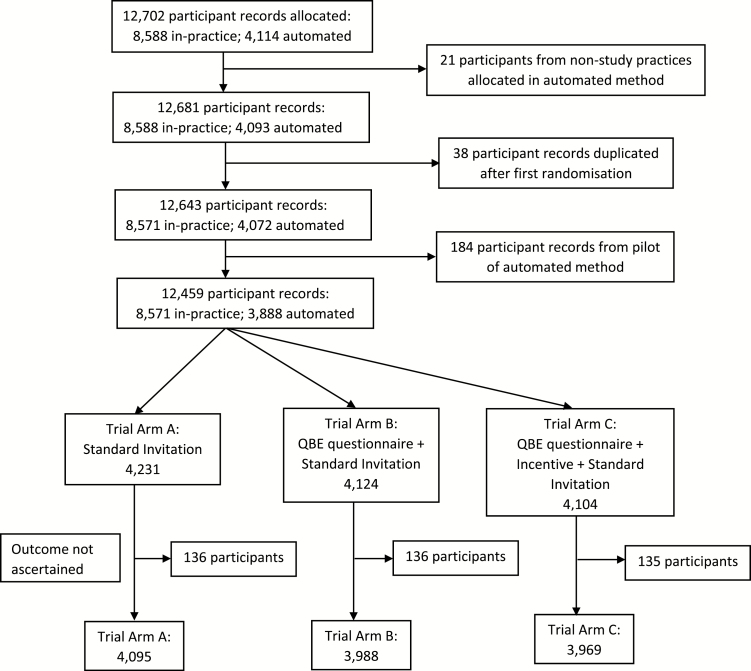
There were 18 general practices recruited into the trial. Trial practices generally had larger list sizes than non-trial practices in the same area but were similar in terms of area deprivation and proportion of ethnic minorities. Figure 1 shows the flow of participants through the trial. There were 12,702 participants recruited but 21 participants were found to be registered with non-trial practices and were excluded leaving 12,681 participants. Records for 38 participants were found to be duplicated after their first allocation, these were also excluded. There were 184 participants included in the pilot of the automated randomization procedure who were not eligible for the trial. There were then 12,459 participants randomized in the trial. The median number of participants per general practice was 711 and ranged from 189 to 1,220.
Fig. 1.
Flow of individuals throughout the study from identification, randomization, and follow-up at 6 months.
Participant characteristics are shown in Table 2. There was a higher proportion of men (52%) than women (44%) invited (with 4% “not known”); the median age of participants was 45 (interquartile range 40, 54) reflecting the demographic distribution of the registered population of the area. Trial participants lived in areas with generally high deprivation with 29.4% in the most deprived quintile for England, 51.2% in the second most deprived quintile and none of the participants in the least deprived quintile for England. There were 35.9% White, 19.5% Black African / Caribbean and 19.6% mixed ethnicity participants.
Table 2.
Baseline Characteristics of the Study Population
| Characteristic | Standard (4,231) | QBE (4,124) | QBE + Inc. (4,104) | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Gender | Female | 1,857 | (43.9) | 1,783 | (43.2) | 1,809 | (44.1) |
| Male | 2,211 | (52.3) | 2,180 | (52.9) | 2,135 | (52.0) | |
| Missing | 163 | (3.9) | 161 | (3.9) | 160 | (3.9) | |
| Age | median (IQR) | 46 | (40–54) | 45 | (40–54) | 45 | (40–54) |
| Age group | 40–59 | 3,501 | (82.8) | 3,431 | (83.2) | 3,414 | (83.2) |
| 60–74 | 567 | (13.4) | 532 | (12.9) | 530 | (12.9) | |
| Missing | 163 | (3.9) | 161 | (3.89 | 160 | (3.9) | |
| Ethnicity | White | 1,502 | (35.5) | 1,477 | (35.8) | 1,489 | (36.3) |
| African / Caribbean | 797 | (18.8) | 822 | (19.9) | 813 | (19.8) | |
| Asian | 197 | (4.7) | 224 | (5.4) | 248 | (6.0) | |
| Mixed | 861 | (20.4) | 806 | (19.5) | 769 | (18.7) | |
| Other | 98 | (2.3) | 99 | (2.4) | 95 | (2.3) | |
| Missing | 776 | (18.3) | 696 | (16.9) | 690 | (16.8) | |
| IMD quintile | Most deprived | 1,214 | (28.7) | 1,224 | (29.7) | 1,225 | (29.9) |
| 4 | 2,183 | (51.6) | 2,128 | (51.6) | 2,068 | (50.4) | |
| 3 | 365 | (8.6) | 367 | (8.9) | 381 | (9.3) | |
| 2 | 11 | (0.3) | 16 | (0.4) | 14 | (0.3) | |
| Least deprived | 0 | 0 | 0 | ||||
| Missing | 458 | (10.8) | 389 | (9.4) | 416 | (10.1) | |
Standard Standard Invitation; QBE Question-Behavior Effect questionnaire; Inc. Incentive; IQR Interquartile range; IMD Indices of Multiple Deprivation. Figures are frequencies (column percent) except where indicated.
At the time of data extraction, it was not possible to search for outcome data for a small number of participants. The patient identifying records for each month’s allocations remained at general practices and at the time of data extraction a small number of spreadsheets were found to be missing. The 407 participants with missing outcome data amounted to 3.3% of all trial participants and 4.8% of participants recruited through the in-practice recruitment method. These participants were excluded from trial analyses, leaving 12,052 participants for further analysis (Fig. 1).
Health check uptake was evaluated for 12,052 participants (Table 3). In the standard invitation trial arm, 590/4,095 (14.4%) of participants were recorded as attending a health check within 6 months of first invitation. With the pre-invitation QBE questionnaire 630/3,988 (15.8%) attended for a health check within 6 months of the invitation. With the QBE questionnaire and the offer of a financial incentive to return the questionnaire 629/3,969 (15.9%) attended for a health check within 6 months of invitation. The risk difference associated with QBE questionnaire versus standard invitation was 1.43% (95% confidence interval [CI] −0.12% to 2.97%, p = .070) and for the QBE questionnaire and offer of financial incentive was 1.52% (−0.03% to 3.07%, p = .054). The estimated difference in health check uptake between the QBE with incentive trial arm and QBE alone was 0.01% (−1.58 to 1.59%, p = .995). QBE questionnaires were returned by 917/ 3,988 (23.0%) in the QBE Questionnaire trial arm and by 974/ 3,969 (24.5%) in the QBE Questionnaire and Incentive trial arm. The questionnaire return rate was 1.42% (−0.4% to 3.26%, p = .132) higher in the trial arm offered an incentive to return the questionnaire. Questionnaire return was significantly associated with female gender, older age and lower levels of deprivation.
Table 3.
Uptake of Health Checks Within 6 Months of Randomization by Trial Arm
| Trial arm | Number of participants | Number of checks within 6 months | Differencea in uptake (95% confidence interval) | p valueb |
|---|---|---|---|---|
| Standard invitation (Standard) | 4,095 | 590 (14.41) | — | |
| Question behavior-effect questionnaire (QBE) | 3,988 | 630 (15.80) | 1.43 (−0.12 to 2.97) | .070 |
| QBE questionnaire and offer of incentive (QBE & Inc.) | 3,969 | 629 (15.85) | 1.52 (−0.03 to 3.07) | .054 |
| Total | 12,052 | 1,849 (15.34) |
QBE Question-Behavior Effect.
aAdjusted for month and year of randomization and clustering by practice.
b p value of <.0167 required for significance because of multiple comparisons.
Demographic Variables Associated With Health Check Uptake
Health check uptake was lower in men than women (adjusted odds ratio 0.74, 95% CI 0.69 to 0.80, p < .001) (Table 4). Health check uptake was higher in participants aged 60 years and older (1.43, 1.20 to 1.71, p < .001) than in those aged 40 to 59 years. Compared to participants of “White” ethnicity in this trial, participants of Black African or Caribbean ethnicity (2.15, 1.86 to 2.49, p < .001), Asian (2.03, 1.63 to 2.67, p < .001) or Mixed ethnicity (3.09, 2.07 to 4.62, p < .001) had higher uptake of health checks. Lower levels of deprivation tended to be associated with higher uptake of health checks but this was only significant for the fourth highest quintile in which there were only 41 participants. There was no clear evidence that the association of deprivation varied by trial arm. A test of the interaction of trial arm with deprivation quintile gave a p value of .067.
Table 4.
Association of Case-Mix Variables With Health Check Uptake Within 6 Months of Randomization
| Uptake of health checks at 6 months after randomization | |||||||
|---|---|---|---|---|---|---|---|
| N | n | % | Odds ratio | (95% CI) | p value | ||
| Trial arm | Standard | 4,095 | 590 | 14 | Ref. | ||
| QBE | 3,988 | 630 | 16 | 1.13 | (1.00 to 1.27) | .042 | |
| QBE & Inc. | 3,969 | 629 | 16 | 1.13 | (1.02 to 1.26) | .018 | |
| Gender | Female | 5,449 | 992 | 18 | Ref. | ||
| Male | 6,526 | 857 | 13 | 0.74 | (0.69 to 0.80) | <.001 | |
| Missing | 77 | 0 | 0 | — | |||
| Age group | 40–59 | 10,346 | 1,530 | 15 | Ref. | ||
| 60–74 | 1,629 | 319 | 20 | 1.43 | (1.20 to 1.71) | <.001 | |
| Missing | 77 | 0 | 0 | — | |||
| Ethnicity | White | 4,468 | 490 | 11 | Ref. | ||
| African / Caribbean | 2,432 | 491 | 20 | 2.15 | (1.86 to 2.49) | <.001 | |
| Asian | 669 | 132 | 20 | 2.03 | (1.63 to 2.67) | <.001 | |
| Mixed | 2,436 | 662 | 27 | 3.09 | (2.07 to 4.62) | <.001 | |
| Other | 292 | 38 | 13 | 1.28 | (0.88 to 1.85) | .194 | |
| Missing | 1,755 | 36 | 2 | 0.15 | (0.07 to 0.34) | <.001 | |
| IMD quintile | Most deprived | 3,663 | 550 | 15 | Ref. | ||
| 4 | 6,379 | 993 | 16 | 1.09 | (0.95 to 1.24) | .215 | |
| 3 | 1,113 | 193 | 17 | 1.15 | (0.95 to 1.39) | .156 | |
| 2 | 41 | 13 | 32 | 2.78 | (1.87 to 4.12) | <.001 | |
| Missing | 856 | 100 | 12 | ||||
QBE Question-Behavior Effect. Adjusted for calendar month and clustering by practice (GEE method, robust standard errors), missing IMD quintile omitted. p value of .0167 required for significance for trial arm comparison. Test for interaction of Trial Arm and IMD quintile, p = .067. Odds ratios were adjusted for each of the variables shown.
Health check uptake was higher in participants who returned the QBE questionnaire. In the two intervention trial arms (QBE and QBE & Incentive), 32.5% and 32.8% of participants who returned the QBE questionnaire subsequently attended a health check respectively. A “per-protocol” analysis estimated an increase in uptake of 17.9% for QBE and 18.3% for QBE & Incentive compared to Standard Invitation only. However, these estimates may be biased because these include a minority of randomized participants in the intervention trial arms but all participants in the control trial arm. In order to obtain an improved estimate of the effect of completing and returning the QBE questionnaire, a Complier-Average Causal Effect (CACE) analysis was performed [30] (Table 5). The CACE analysis estimated the difference in health check uptake to be 6.0% greater in the QBE arm compared to Standard Invitation (95% CI: 0.8% to 11.3%; p = .024) and 5.9% greater in the QBE + Incentive compared to Standard Invitation (95% CI: 0.8% to 10.9%; p = .022) (Table 5). Questionnaire return was associated with older age, female gender, and lower levels of deprivation but there was no evidence that questionnaire return was more frequent in the trial arm that was offered an incentive (Test for interaction of trial arm and deprivation category, p = .734).
Table 5.
Complier-Average Causal Effect Analysis: Compliers (Return of Questionnaire) and Uptake of Health Checks Within 6 Months of Randomization by Trial Arm
| Trial arm | Number of compliers (%) | Number of non-compliers (%) | All (%) |
|---|---|---|---|
| Uptake % | Uptake % | Uptake % | |
| Standard | NK | NK | 4095 (100) |
| NK | NK | 14.4 | |
| QBE | 917 (23.0) | 3,071 (77.0) | 3,988 (100) |
| 32.5 | 10.8 | 15.8 | |
| QBE & Inc. | 974 (24.5) | 2,995 (75.5) | 3,969 (100) |
| 32.8 | 10.4 | 15.9 |
QBE Question-Behavior Effect; NK not known. Complier-Average Causal Effect analysis estimated an increase of 6.0% (95% CI: 0.8% to 11.3%; p = .024) in health checks in QBE arm compared to Standard Invitation, and 5.9% (95% CI: 0.8% to 10.9%; p = .022) in the QBE & Inc. compared to Standard Invitation.
Table 6 presents adjusted odds ratios associating questionnaire responses with health check uptake. Each of the constructs predicted uptake, with participants with higher intentions, more positive instrumental and affective attitudes, higher levels of PBC, perceiving greater social approval for having a check and anticipating more regret (AR) for not having a check being more likely to have a health check. The largest point estimate was for the association of intentions, followed by those for subjective norms, PBC and instrumental attitudes while AR and affective attitudes appeared to be the weakest predictors, but CIs were overlapping.
Table 6.
Odds Ratios for Uptake of Health Checks per Unit Increase in each Questionnaire Construct
| Odds ratioa | 95% Confidence interval | p value | |
|---|---|---|---|
| Intentions | 1.37 | 1.27 to 1.48 | <.001 |
| Attitude: instrumental | 1.26 | 1.16 to 1.36 | <.001 |
| Anticipated regret | 1.14 | 1.08 to 1.19 | <.001 |
| Attitude: affective | 1.16 | 1.08 to 1.25 | <.001 |
| Perceived Behavioral Control | 1.26 | 1.17 to 1.36 | <.001 |
| Subjective Norms | 1.26 | 1.13 to 1.42 | <.001 |
Odds ratios were estimated from a model including each construct.
aAdjusted for each construct shown and clustering by general practice.
Discussion
Main Findings
This study revealed an enhanced invitation method using the QBE was not associated with increased uptake of health checks. The CACE analysis provided an intervention effect estimate for comparable groups, finding an approximate 6% increase in uptake among those who returned the questionnaire. Offering a financial incentive for questionnaire return was not associated with greater return of the QBE Questionnaire, nor with increased uptake of heath checks. Positive responses to the QBE questionnaire items were associated with a greater uptake of the offer of a health check, with the strongest association being observed for intentions.
These findings must be viewed in the context of low overall uptake of health checks in trial participants. For the first 6 months, following a standard invitation letter sent through the population-based call-recall system, uptake was 14%. This low level of response to a standard invitation was confirmed in data from the health check management information system. Trial data for health check uptake only included health checks performed in response to an invitation letter. Nationally reported data for health check uptake are inflated by additional inclusion of completed health checks that are performed opportunistically by health care providers in individuals who may not have received an invitation letter.
Question-Behavior Effect
The research provided no evidence that an invitation method based on the QBE could be associated with an increase in health check uptake that could be of clinical or public health importance [35]. There was no evidence that offering a financial incentive to return the QBE questionnaire might increase the level of response to this invitation method. The 1.4%–1.5% increase in uptake achieved in this trial contrasts with increases of 3%–4% in uptake achieved in another recent study through simple modifications to the health check invitation letter based on behavioral insights [18].
The trial results are in contrast to earlier study findings regarding the positive impact of the QBE on health check uptake [17]. The previous study used a longer questionnaire, was located in a single general practice and was conducted more than 20 years ago. It is possible that the reduction in the number of items or slight changes in the constructs tapped could explain the difference in effects. A recent systematic review did not find that the number of questionnaire items affected the magnitude of the observed QBE [25].
This is one of the largest trials conducted using the QBE and the results add to the weight of evidence against a quantitatively important impact of an intervention based on the QBE [22, 35]. Indeed, the effect of QBE interventions on uptake in our trial (odds ratio approximately 1.13) was highly consistent with the effect of the QBE on screening uptake (d = 0.06 is approximately equivalent to an odds ratio of 1.11 [36]), reported in a recent review of RCTs of QBE interventions [24]. Recent reviews suggest that the QBE is smaller in randomized controlled studies such as ours, when there is a longer time interval between questioning and behavior [22], in studies conducted with non-student samples, in non-laboratory settings and when the intervention is delivered by mail [25]. These factors may constrain the potential of the QBE as a public health intervention.
The association of health check uptake with QBE questionnaire return might be explained in several different ways. This might be interpreted as evidence of the QBE at work, with stronger evidence of an effect among those who responded to the QBE intervention. A second alternative is that return of the QBE questionnaire, and attendance for a health check, are both predicted by similar underlying psychological factors. These might include, for example, attaching high importance to health. A third explanation could be that questionnaire returners and health check attendees share certain demographic characteristics, which might make these behaviors easier to perform. The similarity of demographic factors predicting both health check uptake and questionnaire return, including older age and lower levels of deprivation, might lend support to these second two explanations, with health check uptake being substantially higher in questionnaire returners.
Previous studies and the present results suggest that the QBE best increases behavior in participants with a positive reaction to the behavior. Among questionnaire respondents, views about health checks were largely positive but only a small proportion of study participants returned the questionnaire. Questionnaire nonrespondents may have had less positive views about health checks. Combining the QBE with a motivational intervention to increase positive intentions and attitudes might better support health check uptake [37].
Incentivizing Questionnaire Return
The research found that a financial incentive was not effective at increasing questionnaire return for this behavior as a means to potentially increase the QBE. The finding contrasts in some ways with that of several recent QBE trials. Both a sticky note with a thank you message [38, 39] and a £5 love to shop voucher [39] increased questionnaire return rates but did not increase rates of performance of the behavior (influenza vaccination; bowel screening kit return; attendance for cervical screening). Thus while incentives may be useful in relation to returning questionnaires there is little evidence that this translates into a strengthening of the QBE.
The gift voucher used here was exchangeable at a broad variety of common shops. However, some participants may have been unaware of its wide validity, resulting in it being less attractive than intended. The incentive was conditional on questionnaire return. Larger benefits have been found for unconditional incentives, provided at the time the survey is distributed [26]. However, unconditional incentives may not be feasible when targeting large groups of patients. It is possible that the incentive “crowded out” motivation among individuals who would have returned the questionnaire for altruistic reasons. The reduction in response due to crowding out may have been countered by an increase in response among less intrinsically motivated individuals, resulting in no significant difference in response rates between the incentive and non-incentivized arms.
Strengths and Limitations of This Research
The trial was pre-registered and conducted in a large number of general practices and the large target sample size for the trial was achieved. The study had sufficient power to detect small increases in uptake of health checks. The trial was conducted in a deprived area of inner London with a young population age-distribution and a high proportion of ethnic minorities. We found that uptake of checks in response to a postal invitation was generally higher in ethnic minority groups, which may reflect on the generally lower levels of education in the local “White” population, with college education being more frequent among those of Black African origin in this locality. This research does not exclude the possibility that an enhanced invitation method based on the QBE might be more effective in more affluent areas with older populations. The conduct of the trial depended on using primary care electronic health records, linked to the health check management information system, to recruit participants, arrange for the delivery of the intervention materials and to ascertain trial outcomes. We conducted extensive checks to ensure that these processes were being implemented as intended. Nevertheless, there was evidence of discrepancies arising in the health check management information system. The numbers of discrepancies recorded was too small to have an influence on the overall results of the study. We used Read codes recorded in electronic health records to ascertain trial outcomes. It is possible that general practices might use non-standard Read codes to identify health checks. However, we searched for the Read codes that were mandated by the health check program and these codes are used for reimbursement of practices for completed health checks. We were not able to include in a process evaluation in order to investigate the weak participant response to the questionnaire and the incentives. We made an assumption that questionnaires and invitation letters were received by participants. It is possible that in deprived areas with mobile populations, some invitation letters were not received by their intended recipients. We did not encounter any appreciable number of letters “returned to sender” but even if some letters were not received, this does not undermine our conclusion that the QBE was not effective in the present context.
Conclusions
An enhanced invitation method using the QBE was not associated with increased uptake of health checks in primary care, nor was a financial incentive to return the QBE questionnaire associated with increased uptake. Overall uptake of health checks in response to an invitation was low and our results do not exclude the possibility of an effect of the intervention in the context of higher overall uptake. In the present context, low health check uptake might be explained by service organization and delivery factors that impede the ease with which people can obtain a health check [28].
Supplementary Material
Supplementary material is available at Annals of Behavioral Medicine online.
Acknowledgments
The trial is funded by the National Institute for Health Research (NIHR) Health Technology Assessment Programme (11/129/61). C. Burgess and A. S. Forster were also supported by the Guy’s and St. Thomas’ Charity (grant no. G100702). M. C. Gulliford was supported by the NIHR Biomedical Research Centre at Guy’s and St Thomas’ Hospitals. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. A. S. Forster is funded by a Cancer Research UK Cancer Prevention Fellowship (C49896/A17429).
Conflict of Interest Authors Lisa McDermott, Victoria Cornelius, Alison J. Wright, Caroline Burgess, Alice S. Forster, Mark Ashworth, Bernadette Khoshaba, Philippa Clery, Frances Fuller, Jane Miller, Hiten Dodhia, Caroline Rudisill, Mark T. Conner, and Martin C. Gulliford declare that they have no conflict of interest.
Compliance with ethical standards
Ethical Approval The protocol for the study was approved by the London Bridge Research Ethics Committee on March 7, 2013 (reference 13/LO/0197). The protocol for the trial has been reported previously [27]. All pro cedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declar ation and its later amendments or comparable ethical standards. Trial registration: Current Controlled Trials ISRCTN42856343. Date registered March 21, 2013.
References
- 1. Department of Health. Putting Prevention First. NHS Health Check: Vascular Risk Assessment. Best Practice Guidance. London, UK: Department of Health; 2009. [Google Scholar]
- 2. British Heart Foundation. Cardiovsacular Disease Statistics UK Factsheet. London, UK: British Heart Foundation; 2014. [Google Scholar]
- 3. Diabetes UK. Diabetes Prevalence 2014. London, UK: Diabetes UK; 2015. [Google Scholar]
- 4. National Institute for Health and Care Excellence. Chronic kidney disease in adults: assessment and management Clinical Guideline [CG182]. 2014. Available at www.nice.org.uk/cg182. Accessed 1 July 2017. [Google Scholar]
- 5. Aitken GR, Roderick PJ, Fraser S, et al. Change in prevalence of chronic kidney disease in England over time: comparison of nationally representative cross-sectional surveys from 2003 to 2010. BMJ Open. 2014;4(9):e005480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dregan A, Stewart R, Gulliford MC. Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study. Age Ageing. 2013;42(3):338–345. [DOI] [PubMed] [Google Scholar]
- 7. Department of Health. Economic Modelling For Vascular Checks. London, UK: Department of Health; 2008. [Google Scholar]
- 8. Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ. 2012;345: e7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Capewell S, McCartney M, Holland W. NHS Health Checks–a naked emperor?J Public Health (Oxf). 2015;37(2):187–192. [DOI] [PubMed] [Google Scholar]
- 10. Nicholas JM, Burgess C, Dodhia H, et al. Variations in the organization and delivery of the ‘NHS health check’ in primary care. J Public Health (Oxf). 2013;35(1):85–91. [DOI] [PubMed] [Google Scholar]
- 11. Chang KC, Lee JT, Vamos EP, et al. Impact of the National Health Service Health Check on cardiovascular disease risk: a difference-in-differences matching analysis. CMAJ. 2016;188(10):E228–E238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. NHS. NHS Health Check 2017. Available at www.healthcheck.nhs.uk. Accessed 4 January 2017.
- 13. Dalton AR, Bottle A, Okoro C, Majeed A, Millett C. Uptake of the NHS Health Checks programme in a deprived, culturally diverse setting: cross-sectional study. J Public Health (Oxf). 2011;33(3):422–429. [DOI] [PubMed] [Google Scholar]
- 14. Artac M, Dalton AR, Majeed A, Car J, Huckvale K, Millett C. Uptake of the NHS Health Check programme in an urban setting. Fam Pract. 2013;30(4):426–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dalton AR, Bottle A, Okoro C, Majeed A, Millett C. Implementation of the NHS Health Checks programme: baseline assessment of risk factor recording in an urban culturally diverse setting. Fam Pract. 2011;28(1):34–40. [DOI] [PubMed] [Google Scholar]
- 16. Usher-Smith JA, Mant J, Martin A, et al. NHS health check programme rapid evidence synthesis 2017. Available at http://www.healthcheck.nhs.uk/commissioners_and_providers/evidence/
- 17. Attwood S, Morton K, Sutton S. Exploring equity in uptake of the NHS Health Check and a nested physical activity intervention trial. J Public Health (Oxf). 2016;38(3):560–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sallis A, Bunten A, Bonus A, James A, Chadborn T, Berry D. The effectiveness of an enhanced invitation letter on uptake of National Health Service Health Checks in primary care: a pragmatic quasi-randomised controlled trial. BMC Fam Pract. 2016;17:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cochrane T, Gidlow CJ, Kumar J, Mawby Y, Iqbal Z, Chambers RM. Cross-sectional review of the response and treatment uptake from the NHS Health Checks programme in Stoke on Trent. J Public Health (Oxf). 2013;35(1):92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Krska J, du Plessis R, Chellaswamy H. Implementation of NHS Health Checks in general practice: variation in delivery between practices and practitioners. Prim Health Care Res Dev. 2016;17(4):385–392. [DOI] [PubMed] [Google Scholar]
- 21. Conner M, Godin G, Norman P, Sheeran P. Using the question-behavior effect to promote disease prevention behaviors: two randomized controlled trials. Health Psychol. 2011;30(3):300–309. [DOI] [PubMed] [Google Scholar]
- 22. Wilding S, Conner M, Sandberg T, et al. The question-behavior effect: a theoretical and methodological review and meta-analysis. Eur Rev Soc Psychol. 2016;27(1):196–230. [Google Scholar]
- 23. Spangenberg ER, Kareklas I, Devezer B, Sprott DE. A meta-analytic synthesis of the question–behavior effect. J Consum Psychol. 2016;26(3):441–458. [Google Scholar]
- 24. Rodrigues AM, O’Brien N, French DP, Glidewell L, Sniehotta FF. The question-behavior effect: genuine effect or spurious phenomenon? A systematic review of randomized controlled trials with meta-analyses. Health Psychol. 2015;34(1):61–78. [DOI] [PubMed] [Google Scholar]
- 25. Wood C, Conner M, Miles E, et al. The impact of asking intention or self-prediction questions on subsequent behavior: a meta-analysis. Pers Soc Psychol Rev. 2016;20(3):245–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Edwards PJ, Roberts I, Clarke MJ, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009;3: MR000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Edwards P, Cooper R, Roberts I, Frost C. Meta-analysis of randomised trials of monetary incentives and response to mailed questionnaires. J Epidemiol Community Health. 2005;59(11):987–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McDermott L, Wright AJ, Cornelius V, et al. Enhanced invitation methods and uptake of health checks in primary care: randomised controlled trial and cohort study using electronic health records. Health Technol Assess. 2016;20(84):1–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stata Corporation. Stata Statistical Software. Vol. 12.1 College Station, TX: Stata Press; 2012. [Google Scholar]
- 30. Forster AS, Burgess C, McDermott L, et al. Enhanced invitation methods to increase uptake of NHS health checks: study protocol for a randomized controlled trial. Trials. 2014;15:342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sandberg T, Conner M. A mere measurement effect for anticipated regret: impacts on cervical screening attendance. Br J Soc Psychol. 2009;48(Pt 2):221–236. [DOI] [PubMed] [Google Scholar]
- 32. Sensory Trust. Sensory Trust Information Sheet. Bodelva, Cornnwall, UK: Sensory Trust; 2013. [Google Scholar]
- 33. Dunn G, Maracy M, Dowrick C, et al. ; ODIN group. Estimating psychological treatment effects from a randomised controlled trial with both non-compliance and loss to follow-up. Br J Psychiatry. 2003;183(4):323–331. [DOI] [PubMed] [Google Scholar]
- 34. Medical Research Council. Cluster randomised trials: Methodological and ethical considerations. London: Medical Research Council; 2009. Available at https://www.cebma.org/wp-content/uploads/Cluster-randomised-trials-Methodological-and-ethical-considerations.pdf [Google Scholar]
- 35. Rodrigues AM, French DP, Sniehotta FF. Commentary: The impact of asking intention or self-prediction questions on subsequent behavior: a meta-analysis. Front Psychol. 2016;7:879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19(22):3127–3131. [DOI] [PubMed] [Google Scholar]
- 37. Ayres K, Conner M, Prestwich A, et al. Exploring the question-behaviour effect: randomized controlled trial of motivational and question-behaviour interventions. Br J Health Psychol. 2013;18(1):31–44. [DOI] [PubMed] [Google Scholar]
- 38. Conner M, Sandberg T, Nekitsing C, et al. Varying cognitive targets and response rates to enhance the question-behaviour effect: An 8-arm Randomized Controlled Trial on influenza vaccination uptake. Soc Sci Med. 2017;180:135–142. [DOI] [PubMed] [Google Scholar]
- 39. Conner M, Wilding S, Sandberg T, et al. Testing the mechanisms underlying the question-behavior effect: Two dismantling trials. In preparation.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.