HIV-positive men who participated in a brief online behavioral intervention reported less sexual risk behavior than men who did not participate.
Keywords: HIV, Gay and bisexual men, Sexual risk, Intervention
Abstract
Background
HIV disproportionately affects sexual minority men, and developing strategies to reduce transmission risk is a public health priority.
Purpose
The goal was to empirically test a newly developed, Information, Motivation, Behavioral skills (IMB) theoretically derived, online HIV sexual risk reduction intervention (called HINTS) among a sample of sexual minority men living with HIV.
Methods
Participants were 167 men randomized to either the four-session online HINTS intervention or to a time-matched, online control condition. Participants were assessed at baseline and at 6-month follow-up for demographic, medical and psychosocial factors, and sexual risk behavior. Analyses examined group differences in incidence rates of condomless anal sex (CAS) at follow-up with all male sex partners and by partner serostatus, either seroconcordant or serodiscordant for HIV infection.
Results
Men assigned to the HINTS intervention reported decreased CAS with serodiscordant partners, a behavior that confers high risk of HIV transmission, compared to the control group. Men assigned to the HINTS intervention also reported increased CAS with seroconcordant partners, a behavior indicative of serosorting. Although the IMB model did not appear to mediate these intervention effects, some IMB components were associated with behavioral outcomes at 6-month follow-up.
Conclusions
A new group-based sexual risk reduction intervention conducted exclusively online was successful in reducing HIV transmission risk behavior in a sample of gay and bisexual men living with HIV. Future work should consider utilizing this intervention with other groups living with HIV, perhaps in combination with biomedical HIV prevention strategies.
Introduction
The number of new HIV infections in the USA has remained stable at around 50,000 cases per year (Centers for Disease Control and Prevention [CDC] [1, 2]). However, men who have sex with men (MSM) are disproportionately affected by HIV infection in the USA. MSM, the majority of whom identify as gay or bisexual, comprise less than 5% of the U.S. population, yet account for over 75% of new male HIV infections each year [2]. At the same time, since the advent of highly active antiretroviral therapy, MSM with HIV infection in the USA are now living longer, healthier lives. With the number of new infections at a plateau and fewer HIV-associated deaths reported (World Health Organization [WHO] [3]), innovations in HIV prevention strategies are greatly needed to reduce HIV transmission.
The use of secondary HIV prevention strategies is a national public health priority. Although the CDC recommends abstinence from anal sex as the most effective way to prevent HIV transmission [4], a large majority of MSM with HIV do not report the intention to abstain from sex entirely, and even fewer follow through on such intentions [5]. As a result, secondary prevention strategies for MSM have tended to adopt a risk reduction approach. Two commonly endorsed behavioral strategies to reduce transmission risk among MSM include serosorting practices and condom use. These transmission risk reduction behavioral strategies remain vital for MSM with HIV infection even with the advent of new biomedical HIV prevention strategies, including pharmacological treatment as prevention (TasP) or pre-exposure prophylaxis (PrEP), for MSM without HIV infection [6, 7].
Serosorting refers to the practice of limiting condomless sexual encounters to partners believed to be of the same serostatus, with the intention of reducing HIV transmission risk [4]. Although there are other safety concerns associated with serosorting behaviors [3, 8], it is a commonly endorsed strategy in MSM with and without HIV infection [9], and is recommended as a harm reduction strategy in certain circumstances [3]. Condom use is another widely endorsed secondary prevention strategy [5], which has been shown to substantially decrease the risk of HIV transmission in MSM [10]. The efficacy of condom use is well documented and long established [11, 12], and consistent condom use is strongly recommended by both the CDC [4] and the WHO [3] to reduce HIV transmission risk in MSM. Despite the existence of these risk reduction strategies, many MSM with HIV infection continue to engage in sexual behaviors associated with a high risk of transmission (e.g., condomless anal intercourse with serodiscordant partners) [13, 14]. Consequently, reducing risky sexual behaviors in this population has been an important target for secondary prevention efforts.
Meta-analytic evidence indicates that interventions aimed at sexual risk reduction among individuals with HIV infection can be successful, and that these efforts are more effective when based on established health behavior theories [15–17]. One model of HIV preventive behavior with strong empirical support is the Information-Motivation-Behavioral Skills (IMB) model [18, 19]. The IMB model suggests that HIV prevention information, motivation, and behavioral skills are fundamental prerequisites to changes in sexual risk behaviors. Information concerning HIV risk-reduction and the motivation to practice preventive measures are directly relevant to behavioral change, and may also be expressed indirectly through behavioral skills. Well-informed and motivated individuals can apply successful behavioral skills (e.g., condom negotiation) in order to initiate and maintain risk reduction strategies (e.g., consistent condom use). Studies using the IMB model to predict sexual risk in MSM have reported somewhat mixed findings [20–22], but the IMB model has received considerable empirical support among individuals with HIV infection [19, 23]. Furthermore, the IMB model has been used to guide the development and implementation of successful secondary prevention interventions targeting sexual risk [24–27]. It is noteworthy that to date, these interventions have relied on face-to-face delivery, and few have capitalized on novel technological interfaces.
The Internet has changed the way many people live their lives, especially with regards to connecting with others. Some have suggested that gay and bisexual men adopt new technologies at faster rates than the general population [28]. There have been many social benefits resulting from greater Internet usage, but its proliferation has also been associated with increased sexually transmitted infections and HIV transmission risk [29–31]. Several studies have documented the increased frequency with which MSM seek sex partners online, and more recently through mobile applications (apps), which are now believed to be the leading modality by which men meet other men for sex in the USA, even overtaking gay bars [32–34]. Other studies have found increased rates of condomless anal intercourse among MSM meeting partners online [33, 35]. While the Internet has become a means for people of all genders and sexual preferences to connect with romantic and sexual partners, these findings suggest that the Internet may offer a unique venue for providing interventions to reduce HIV transmission risk behavior among at-risk gay and bisexual men.
Research investigating web-based interventions that specifically target sexual minority men has grown, though it still remains a relatively small empirical base. Recently, several online interventions delivered to young MSM have been shown to be feasible and acceptable, and have successfully enhanced HIV knowledge and motivation to use condoms, as well as achieving reductions in reported condomless sex acts [36–40]. Notably, many of these interventions focused on primary HIV prevention and did not include MSM living with HIV [41]. One recent online secondary prevention study based on a different model of health behavior (i.e., social cognitive theory) implemented tailored risk reduction messages regarding HIV status disclosure and condom usage and found decreased rates of condomless sex as rates of disclosure increased [42]. However, there were no significant differences between the intervention and control groups, suggesting tailored messages provided minimal benefit beyond that conferred by self-monitoring and risk assessment. Considering the potential risks associated with online partner seeking, empirical studies utilizing online interfaces to target sexual transmission risk in men living with HIV is an important area for intervention.
The purpose of the current study was to conduct a field test of a newly developed, brief, exclusively online sexual risk reduction intervention called the HIV Internet Sex (HINTS) study. A group-based intervention was developed through formative research with men living with HIV who had a history of risky sexual behavior and online partner seeking. The IMB model served as a theoretical framework for the intervention development. Unlike some previous online interventions that utilized the IMB model and targeted HIV-negative individuals [36, 40], HINTS was specifically designed for sexual minority men living with HIV. Gay and bisexual men living with HIV were randomized to either HINTS or a comparison control condition, and our primary hypothesis was that men assigned to HINTS would report increased sexual risk reduction practices, such as reductions in condomless anal sex (CAS) with all male partners and especially with HIV-negative or status unknown partners in the 6 months following the study, as compared to the men assigned to the control group. Given that some prior sexual risk reduction interventions among MSM living with HIV have also reported increased serosorting behavior as secondary outcome [43, 44], we also predicted that men assigned to HINTS would show increased use of this risk reduction strategy compared to men in the control group. Finally, as an exploratory aim, we hypothesized that the main theoretical components of the IMB model would mediate the intervention effects on our primary sexual risk reduction outcomes.
Methods
Participant Recruitment
Men were recruited for the HINTS study using online and offline methods. Recruitment ads instructed potential participants to call the HINTS screening phone line. Study staff conducted a brief phone call with interested participants to assess eligibility. Inclusion criteria included: (a) being at least 18 years old; (b) self-identifying as gay or bisexual; (c) living with HIV/AIDS, (d) reporting at least one instance of using the Internet to meet a potential sex partner, and (e) reporting at least one instance of CAS with a male partner. Filler questions were included in the screening assessment to limit potential participants’ ability to detect eligibility criteria. Eligible participants were then provided with information about the study. If they agreed to participate, they provided their email address to receive study-related information.
Procedure
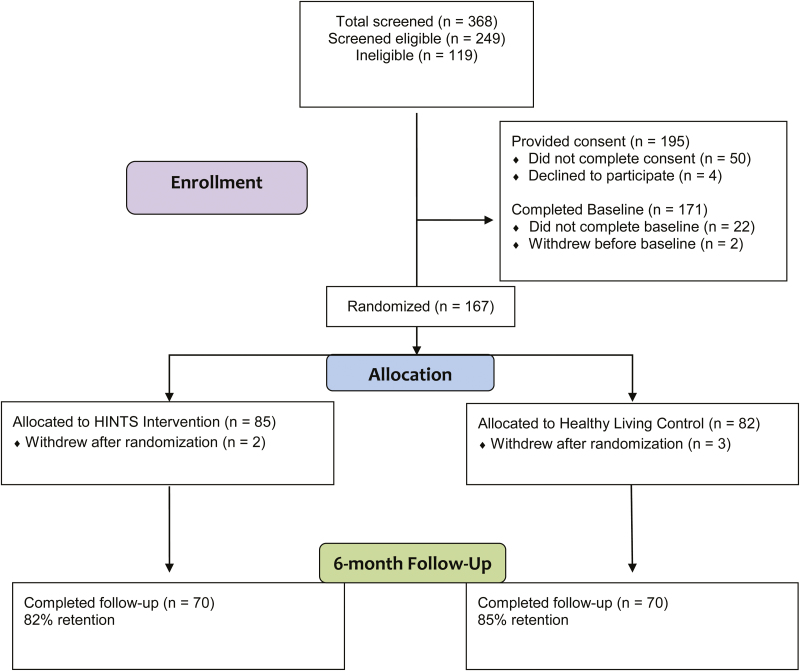
Participants were emailed a unique link and password to their online consent form. Once participants consented to participate in the study, they were sent a link to the baseline survey. Surveys were administered using LimeSurvey [45], a free online open-source survey service. Once the baseline survey was completed, participants were randomized using a computer-generated randomization program to either the HINTS intervention or to a time-matched control condition. Participants were blind to randomization status. Men also provided their physical addresses in order to receive a free headset to better participate in the online groups. Men were assigned to an online group and emailed their four-session group schedule. Group sessions were 45 min in duration and occurred in sequential order (Sessions 1–4). Groups were scheduled twice per week over two consecutive weeks, and participants were assigned to groups by start time (e.g., 12 pm ET, 7 pm ET). In addition to their group schedule, participants were emailed a reminder the day before their scheduled group session to promote attendance. Group interaction included a combination of voice chat and typed chat with facilitators. Follow-up measures were administered 6 months from the time of participants’ baseline surveys and included the same measures, as well as a satisfaction survey for the group interventions. Our university’s Institutional Review Board approved all study procedures. Fig. 1 displays participant flow through the study from screening to follow up. Our ClinicalTrials.gov number is NCT#02887508.
Fig. 1.
Participant flow through enrollment, randomization, and follow-up.
HINTS Intervention
Intervention content was developed using both formative focus groups and individual interviews with gay and bisexual men living with HIV in Atlanta, GA. In each session, facilitators presented information, motivational skills, and behavioral strategies related to a specific topic relevant to online partner seeking and HIV transmission risk reduction. Online interactive polls were included throughout each session to assess participants’ experiences and stimulate discussion. At the end of each session, participants were given an assignment to apply discussion topics to their own online experiences between sessions, in order to promote continuity and engagement.
Group facilitators included two clinical psychology graduate students and two community-based counselors, all of whom had specialized training for working with populations affected by HIV. All facilitators were female. Group facilitators were trained together on delivery of the HINTS and control interventions. Group sessions were recorded and reviewed by the principal investigator, a licensed psychologist and the project manager, a licensed social worker, to monitor intervention fidelity. Additionally, the study team met weekly for supervision to discuss any pertinent issues regarding intervention delivery.
In Session 1, group facilitators and group members introduced themselves. The facilitators presented an overview of the HINTS intervention, then discussed the first HINTS topic: meeting people (including sexual partners) via the Internet. Participants were asked about their experiences of meeting others online and shared instances in which they had encountered a deceptive person or profile online. Facilitators also incorporated relevant video clips during the session to promote discussion. The main goal of this session was to highlight the possibility that potential sex partners might misrepresent their personal information (including serostatus) online. The session ended with a brief review of the topic and discussion, and an assignment to look for deceptive information online to discuss during the next session
In Session 2, the facilitators reviewed the assignment on deception from the previous session, and introduced the topic of HIV serostatus disclosure with partners met online. Participants discussed when and how to address serostatus with potential sex partners, the pros and cons of doing so, and how to manage possible rejections following discussion of HIV status. The main goal of this session was to enhance motivation and behavioral strategies for engaging in a productive dialogue about HIV serostatus. The session ended with an overview of the day’s topics and an assignment to consider online serostatus disclosure for the next session’s discussion.
Session 3 followed a similar format. Discussion began with the assignment on serostatus disclosure from the previous session. The facilitators then introduced material regarding condom negotiation and condom use with partners met online. Topics of discussion included when to discuss condom use preferences with a potential sex partner, how to make condom use more enjoyable during sex, and how best to maintain sexual health. The main goal of this session was to increase motivation and discuss behavioral skills to effectively engage sex partners in using condoms. The session concluded with a brief review of the discussion topics and an assignment regarding online condom negotiation to be shared in the next session.
In Session 4, the group discussed their experiences with the condom negotiation assignment from the previous session. Following this discussion, the facilitators discussed safety when actually meeting potential sex partners met online. Participants shared strategies for maintaining safety when meeting an online acquaintance in person, such as first meeting in a public and well-lit area, letting a friend or family member know where he would be meeting the person, and having an “escape plan.” The goal of this session was to reinforce the topics presented in earlier sessions and how to more safely put them into practice in real-life settings. The session ended with an overview of the entire HINTS program, and participants were invited to provide feedback about what they found most useful during the intervention.
Healthy Living Comparison Condition
The Healthy Living comparison condition followed the same format as HINTS; facilitators presented information, motivational skills, and behavioral skills strategies, but sessions were tailored to address nonsexual health-related topics relevant to individuals living with HIV. Sessions were adapted from a similar control condition implemented in previous studies, and addressed the topics of (a) nutrition and healthy eating, (b) portion control, (c) exercise and staying active, (d) stress reduction to maintain health [46]. As with the HINTS sessions, videos and poll questions were integrated to stimulate discussion during the groups. All control sessions were time-matched with the intervention group sessions.
Measures
Demographic Information
Demographic characteristics including age, sexual identity, sexual orientation, marital status, education level, and income were collected from all participants at baseline.
Psychosocial Variables
Depressive symptoms were assessed using the 20-item Center for Epidemiological Studies of Depression Scale (CES-D; [47]). Participants endorsed how often they experienced each symptom characteristic of depression in the past week on a scale: 0 (no days), 1 (1–2 days), 2 (3–4 days), and 3 (5–7 days). Total scores range from 0 to 60, and a score of 16 indicates a potential clinical level of depression (baseline α = .931).
The Alcohol Use Disorders Identification Test (AUDIT; [48]) was used to assess alcohol use and related problems. The AUDIT includes 10 items that assess frequency of drinking, alcohol dependency, and problems caused by alcohol use. The AUDIT was designed for use in primary care settings to identify individuals at risk for alcohol-related problems. Scores on the AUDIT range from 0 to 40, and a score of 8 or higher is indicative of at-risk drinking. Reliability of the AUDIT in the present sample was acceptable (baseline α = .861).
Information, Motivation, and Behavioral Skills
The IMB measures employed have been used by our research team in prior studies. Knowledge pertinent to the HINTS intervention was assessed using four questions tailored to session content. Participants responded yes, no, or don’t know to each of the following: (a) Can finding out the HIV status of a potential sex partner met online have health benefits? (b) Does trusting people met online pose risks to a person’s health and safety? (c) Can using condoms help prevent STDs that could complicate one’s health? (d) When deciding to meet someone met online in person, should a person offer to meet in a public place during the daytime? Internal consistency between these Yes/No items at 6-month follow-up was low (KR20 = .360).
Motivation was assessed using 10 questions assessing participants’ intention/willingness to practice risk reduction skills (e.g., condom use, serostatus disclosure, strategic positioning, viral load tracking) when meeting sex partner online. Participants responded to each question using a scale from 0 (Definitely will not do) to 5 (Definitely will do). A composite score was calculated by averaging participants’ responses across questions (6-month follow-up α = .833).
Behavioral skills were assessed using a series of vignettes with content specific to meeting sex partners online. Story content included feeling lonely and logging onto a men’s dating site and chatting with someone who clearly wants to hook up; or going out feeling buzzed after a few drinks and instant messaging with someone who wants to meet for sex. Participants were asked to vividly imagine each story and rate their confidence in their ability to engage safety skills using a scale from 0 (Cannot do at all) to 10 (Certain can do). A composite score was calculated by averaging responses across questions (6-month follow-up α = .977).
Sexual Behavior
At baseline and 6-month follow-up, participants self-reported their total number of male sex partners during the past 6 months and how many of those partners they met online. Participants reported male sex partner serostatus (HIV-positive vs. HIV-negative/unknown) and the number of times they had CAS with partners in each serostatus category. CAS with partners living with HIV (seroconcordant) was measured to assess extent of serosorting as an outcome measure, while CAS with partners without HIV or whose HIV-status was unknown (serodiscordant) was measured to assess HIV transmission risk behavior as an outcome measure. This method of dichotomizing sexual behavior by partner serostatus followed conventions set by previous research on sexual risk behavior [49, 50]. An open response format was used to control for response bias and allowed participants to freely enter their number of sex partners and occasions of CAS. Survey software tracked participant responses and prompted participants with their previous entries for subsequent questions regarding the number of times they engaged in CAS. This method of assessing sexual behavior has been used successfully in several prior studies [51–53].
Data Analyses
Baseline characteristics, including demographic, health, psychosocial, and sexual behavior variables for the intervention and control groups were compared to assess the success of randomization. Primary study analyses were analyzed among participants who completed 6-month follow-up surveys (N = 140, 84% of randomized sample). Missing data was minimal (6%) at follow-up. Standard power analyses confirmed sufficient sample size to test our main hypotheses. All analyses were carried out using SPSS, version 21.0.
Analyses were conducted to compare IMB and sexual behavior variables from baseline to 6-month follow-up between groups. ANCOVAs were used to examine changes in the IMB variables over time. Primary outcomes consisted of sexual risk behavior (i.e., CAS) reported at 6-month follow-up. Incidence of CAS was operationalized as count data, which tend to exhibit a strong positive skew and over dispersion [54]. As a result, a negative binomial distribution was applied to analyze CAS with (a) all male sex partners and then (b) seronegative/unknown male sex partners and (c) seropositive male sex partners. Multivariate analyses were conducted analyzing effects of study condition (intervention vs. control), and controlling for baseline sexual behavior, and a priori psychosocial covariates (e.g., age, depression, alcohol use). Results from the multivariate models are reported as exponentiated beta coefficients representing incident rate ratios (IRRs) with 95% confidence intervals for each predictor. The exponentiated beta coefficients serve as a measure of effect size in negative binomial distribution analyses.
As an exploratory aim, we also examined the effects of the theoretical variables (IMB measures) on sexual behavior outcomes to identify potential mediators of primary study effects and also associations with study outcomes at follow-up. Multivariate analyses, including bootstrapping to assess indirect effects, were conducted including our measures of information, motivation, and behavioral skills to examine whether intervention effects on sexual behavior were explained by these theoretical variables. We also analyzed associations between the IMB constructs and sexual behavior at 6-month follow-up controlling for baseline sexual behavior in these analyses.
Results
Participant Characteristics
Recruitment commenced in May 2012, with the 6-month follow-up assessments concluding by January 2014. Table 1 presents sample characteristics at baseline for both the intervention and control groups. There were no significant differences in demographic or psychosocial characteristics at baseline, except for self-identified sexual orientation with more men identifying as bisexual in the HINTS group than the control group (p = .046). There were no significant differences in years since diagnosis, HIV medication usage, CD4 cell counts, or viral load status between the groups. Two participants identified as transgender gay men and were included in the analyses. A total of 167 gay/bisexual men living with HIV were randomized to either the HINTS intervention (n = 85) or to the Healthy Living control condition (n = 82).
Table 1.
Demographic, health, psychosocial, and sexual behavior characteristics for the entire sample at baseline
| Total sample (N = 167) | Intervention group (n = 85) | Control group (n = 82) | p value for differences by condition | |
|---|---|---|---|---|
| Mean (SD) or percentage | ||||
| Age | 44.7 (10.8) | 43.7 (11.4) | 45.7 (10.1) | .230 |
| Race/ethnicity | .548 | |||
| White | 58% | 55% | 60% | |
| Black/African American | 25% | 25% | 24% | |
| Hispanic/Latino | 14% | 14% | 13% | |
| Asian/Pacific Islander | 2% | 4% | 0% | |
| Biracial/Mixed Ethnicity | 2% | 2% | 2% | |
| Male Gender Identification | 99% | 99% | 99% | 1.00 |
| Transgender | 1% | 1% | 1% | |
| Sexual Orientation | .046 | |||
| Gay or homosexual | 92% | 88% | 96% | |
| Bisexual | 8% | 12% | 4% | |
| Married or living with a partner | 20% | 20% | 21% | .988 |
| Education | .613 | |||
| High school or less | 17% | 19% | 16% | |
| Beyond high school | 83% | 81% | 84% | |
| Income | .510 | |||
| $0–$10,000 | 18% | 14% | 22% | |
| $11,000–$20,000 | 23% | 25% | 21% | |
| $21,000–$30,000 | 16% | 14% | 18% | |
| $31,000–$40,000 | 14% | 14% | 13% | |
| $41,000–$50,000 | 7% | 9% | 4% | |
| Over $50,000 | 21% | 21% | 21% | |
| Employment Status | .845 | |||
| Unemployed | 18% | 19% | 17% | |
| Working | 42% | 39% | 45% | |
| Receiving disability | 31% | 33% | 29% | |
| Student | 5% | 5% | 6% | |
| Retired | 4% | 5% | 2% | |
| Health Characteristics | ||||
| Years since HIV Diagnosis | 12.0 (9.4) | 12.4 (9.7) | 11.7 (9.1) | .644 |
| Most recent CD4 cell count | 644.8 (257.5) | 643.7 (271.9) | 646.1 (242.6) | .958 |
| Currently taking HIV medications | 93% | 93% | 94% | .802 |
| Undetectable viral load (baseline) | 74% | 73% | 76% | .725 |
| Undetectable viral load (6 months) | 75% | 73% | 80% | .543 |
| Psychosocial variables | ||||
| Depression (CES-D score) | 17.0 (12.4) | 18.4 (12.8) | 15.6 (11.9) | .148 |
| Problem drinking (AUDIT score) | 5.7 (6.1) | 5.4 (6.5) | 5.9 (5.7) | .633 |
CES-D Center for Epidemiological Studies of Depression Scale; SD standard deviation.
Study Participation, Retention, and Satisfaction
Participants in the HINTS conditions attended an average of 2.2 (SD = 1.8) out of four sessions. Participants in the Healthy Living control conditions attended an average of 2.7 sessions (SD = 1.6). There was no significant difference for group attendance between conditions, F(1,165) = 3.16, p = .077. The modal number of sessions attended by both groups was four sessions. Retention rate was approximately 84%, with 140 of 167 participants (70 in each condition) available at 6-month follow-up. No significant differences in attrition were observed between groups.
Participants were asked to rate their satisfaction using the following scale: 0) Unsatisfied; 1) Somewhat unsatisfied; 2) Somewhat satisfied; 3) Satisfied. Overall, participants in the HINTS intervention reported a mean satisfaction of 2.72 (SD = 0.7), while participants in the control condition reported a mean satisfaction of 2.57 (SD = 0.9). At 6-month follow-up, 97% of participants in the HINTS intervention and 84% in the control condition agreed that study participation was worth their time.
Main Effects Analyses
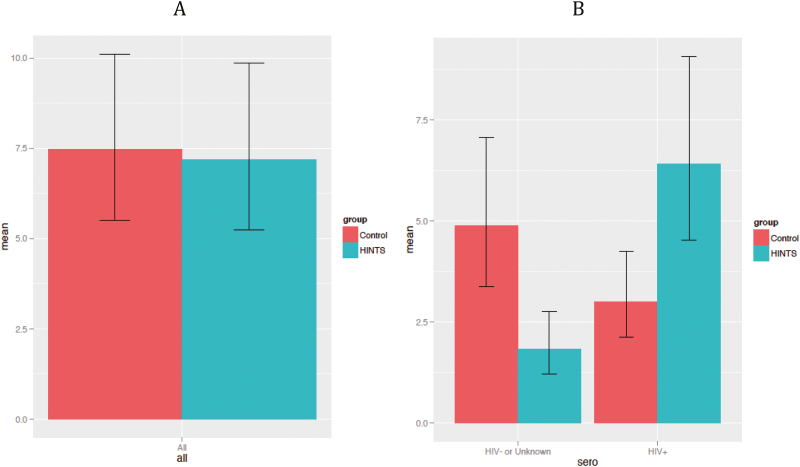
Descriptive statistics for the IMB variables and the sexual behavior outcomes at baseline and 6-month follow-up are presented in Table 2. ANCOVA analyses controlling for baseline data, showed no significant change between groups in the IMB variables at 6-month follow-up (all p’s > .05). Participants in the HINTS intervention reported more male sex partners at 6 months compared to the control condition, controlling for baseline number of partners (IRR: 1.81; 95% CI: 1.23–2.68; p = .003). Participants in HINTS similarly reported meeting more sex partners online at 6-month follow-up (IRR: 2.72; 95% CI: 1.79–4.14; p < .001). While no changes in CAS with all male partners were observed between groups, we observed different patterns of CAS with partners based on their serostatus between the HINTS and control groups. Thus, the following main effects analyses were conducted to explore these changes while controlling for covariates and exploring for potential IMB mediators assessed at 6-month follow-up. Results of the main effects analyses are presented in Table 3 and are depicted in Fig. 2.
Table 2.
Descriptive statistics of IMB and sexual behavior outcomes of the HINTS Intervention compared to the healthy living control group at baseline and 6-month follow-up
| Outcome | HINTS intervention | Control group | p-value* | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6-month follow-up | Baseline | 6-month follow-up | ||||||
| M | SD | M | SD | M | SD | M | SD | ||
| I: Knowledge | 3.49 | 0.6 | 3.47 | 0.9 | 3.49 | 0.8 | 3.66 | 0.7 | .540 |
| M: Intentions | 4.26 | 0.9 | 4.25 | 1.0 | 4.13 | 1.0 | 4.16 | 1.0 | .805 |
| Behavior: Efficacy | 7.03 | 2.3 | 7.08 | 2.5 | 6.60 | 2.3 | 6.86 | 2.4 | .742 |
| Exp(B) (95% CI); p** | |||||||||
| Number male sex partners | 4.97 | 6.5 | 4.89 | 13.1 | 4.69 | 6.3 | 2.58 | 3.2 | 1.81 (1.23–2.68); p = .003 |
| Sex partners met online | 3.46 | 5.1 | 3.95 | 12.4 | 2.97 | 4.3 | 1.46 | 2.4 | 2.72 (1.79–4.14); p < .001 |
| CAS – All partners | 9.34 | 16.4 | 6.40 | 14.8 | 11.32 | 19.1 | 8.90 | 18.1 | 0.91 (0.63–1.30); p = .589 |
| CAS – HIV-/unknown | 3.70 | 6.33 | 1.54 | 4.1 | 5.31 | 11.2 | 3.58 | 13.3 | 0.33 (0.20–0.53); p < .001 |
| CAS – HIV+ | 7.17 | 16.0 | 4.86 | 13.4 | 8.02 | 17.3 | 5.32 | 12.0 | 1.61 (1.08–2.40); p = .020 |
CAS condomless anal sex; IMB Information, Motivation, Behavioral skills.
*Analysis of covariance results controlling for baseline levels.
**Negative binomial regression results, controlling for baseline levels reported as incident rate ratio.
Table 3.
Results of the negative binomial models of the main effects of the intervention on sexual risk behavior (condomless anal sex) with all sexual partners, and with sexual partners by serostatus
| Sexual risk behavior outcome at 6-month follow-up | Model predictor | B | IRR | CI95%lo | CI95%hi | p |
|---|---|---|---|---|---|---|
| Condomless anal sex – All partners | CES-D | −0.022 | 0.979 | 0.959 | 0.999 | .038 |
| Age | −0.033 | 0.967 | 0.942 | 0.994 | .015 | |
| AUDIT | −0.043 | 0.958 | 0.913 | 1.005 | .078 | |
| Condition | −0.037 | 0.964 | 0.610 | 1.522 | .874 | |
| Baseline risk behavior – All partners | 0.030 | 1.030 | 1.014 | 1.047 | <.001 | |
| Condomless anal sex - HIV-/unknown partners | CES-D | −0.013 | 0.987 | 0.962 | 1.012 | .304 |
| Age | −0.014 | 0.987 | 0.953 | 1.021 | .436 | |
| AUDIT | −0.008 | 0.992 | 0.936 | 1.050 | .772 | |
| Condition | −0.985 | 0.373 | 0.207 | 0.672 | .001 | |
| Baseline risk behavior – HIV-/unknown partners | 0.048 | 1.049 | 1.014 | 1.085 | .006 | |
| Condomless anal sex – HIV+ partners | CES-D | −0.011 | 0.989 | 0.967 | 1.011 | .333 |
| Age | −0.034 | 0.966 | 0.940 | 0.993 | .014 | |
| AUDIT | −0.039 | 0.962 | 0.911 | 1.014 | .151 | |
| Condition | 0.762 | 2.142 | 1.268 | 3.617 | .004 | |
| Baseline risk behavior – HIV+ partners | 0.042 | 1.043 | 1.022 | 1.064 | <.001 |
CES-D Center for Epidemiological Studies of Depression Scale; IRR incident rate ratios.
Fig. 2.
Marginal mean incidence of condomless anal sex at 6-month follow-up by experimental condition across (A) all male sex partners and (B) by sex partner serostatus. HINTS HIV Internet Sex Study (experimental condition).
Sexual Risk Behavior With all Male Sex Partners
Experimental condition (HINTS vs. Healthy Living control) was not a significant predictor of incidence of CAS with all male sex partners regardless of serostatus (IRR: 0.964; 95% CI: 0.610–1.522; p = .874), when controlling for age, depression, alcohol use, and sexual risk behavior reported at baseline, indicating that receiving the HINTS intervention did not significantly predict total frequency of CAS with all male sexual partners.
Sexual Risk Behavior With Serodiscordant Male Sex Partners
To assess for HIV transmission risk behavior as an outcome, incidence of CAS with serodiscordant (HIV-negative/serostatus unknown) sex partners reported at 6-month follow-up was examined. Participants in the HINTS intervention reported significantly reduced sexual risk behavior with serodiscordant partners at follow-up (IRR: 0.373; 95% CI: 0.207–0.672; p = .001), when controlling for age, depression, alcohol use, and baseline sexual risk behavior. Men who participated in the HINTS intervention were 62.7% less likely to engage in CAS with a serodiscordant partner at follow-up than men assigned to the control condition.
Sexual Risk Behavior With Seroconcordant Male Sex Partners
Finally, incidence of CAS with seroconcordant sex partners reported at 6-month follow-up was examined. This outcome is consistent with serosorting behavior, which was hypothesized to increase following intervention. Participation in the HINTS intervention was significantly associated with increased incidence of CAS with sex partners living with HIV at follow-up (IRR: 2.142; 95% CI: 1.268–3.617; p = .004). Men who participated in the HINTS intervention were more than twice as likely to engage in CAS with seroconcordant partners compared to men assigned to the control condition.
Theoretical IMB Analyses
Because the IMB variables did not significantly change during the intervention as noted above, conditions were not met for potential mediation effects of these theoretical constructs on our sexual behavior outcomes. Further, using formal mediation analyses with 1,000 bootstrap samples, we did not see evidence for any indirect effects of the IMB constructs on CAS for all partners (Information: B[SE] = −0.28 [0.77], 95% CI: −1.40–0.53; Motivation: B [SE] = −0.08 [0.55], 95% CI: −1.43–0.98; Behavioral Skills: B [SE] = −0.07 [0.45], 95% CI: −1.23–0.68), for HIV-/unknown partners (Information: B [SE] = 0.06 [0.30], 95% CI: −0.41–0.53; Motivation: B [SE] = −0.02 [0.36], 95% CI: −0.87–0.68; Behavioral Skills: B [SE] = −0.08 [0.34], 95% CI: −0.93–0.53), and for HIV+ partners (Information: B [SE] = −0.40 [0.40], 95% CI: −1.49–0.10; Motivation: B [SE] = −0.03 [0.25], 95% CI: −0.59–0.56; Behavioral Skills: B [SE] = 0.06 [0.32], 95% CI: −0.58–0.83).
We then examined the association of the information, motivation, and behavioral skills variables at 6-month follow-up with the primary study outcomes (CAS with all male sex partners, CAS with serodiscordant partners, and CAS with seroconcordant partners). Table 4 presents the results of these analyses. Motivation (IRR: 0.485; 95% CI: 0.292–0.803; p = .005) and behavioral skills (IRR: 0.749; 95% CI: 0.607–0.926; p = .007) at 6 months were significantly associated with decreases in incidence of CAS with serodiscordant partners. Motivation at 6 months was also significantly associated with increases in CAS with seroconcordant partners (IRR: 0.634; 95% CI: 0.419–0.960; p = .031).
Table 4.
Results of the negative binomial models of the mediating effects of IMB variables on sexual risk behavior (condomless anal sex) with all sexual partners, and with sexual partners by serostatus
| Sexual risk behavior outcome at 6-month follow-up | Model predictor | B | IRR | CI95%lo | CI95%hi | p |
|---|---|---|---|---|---|---|
| Condomless anal sex – All partners | CES-D | −0.039 | 0.962 | 0.940 | 0.984 | .001 |
| Age | −0.040 | 0.961 | 0.932 | 0.991 | .011 | |
| AUDIT | −0.040 | 0.961 | 0.913 | 1.011 | .126 | |
| Condition | 0.323 | 1.382 | 0.825 | 2.315 | .219 | |
| Baseline risk behavior – All partners | 0.019 | 1.019 | 1.003 | 1.035 | .019 | |
| Information | 0.193 | 1.213 | 0.773 | 1.903 | .401 | |
| Motivation | −0.337 | 0.714 | 0.480 | 1.064 | .098 | |
| Behavioral Skills | −0.127 | 0.880 | 0.759 | 1.021 | .092 | |
| Condomless anal sex - HIV-/unknown partners | CESD | −0.021 | 0.979 | 0.951 | 1.009 | .166 |
| Age | −0.026 | 0.975 | 0.930 | 1.022 | .286 | |
| AUDIT | −0.063 | 0.939 | 0.872 | 1.012 | .098 | |
| Condition | −0.397 | 0.672 | 0.330 | 1.369 | .274 | |
| Baseline risk behavior – HIV-/unknown partners | 0.036 | 1.037 | 0.997 | 1.076 | .068 | |
| Information | 0.053 | 1.054 | 0.624 | 1.781 | .843 | |
| Motivation | −0.725 | 0.485 | 0.292 | 0.803 | .005 | |
| Behavioral Skills | −0.289 | 0.749 | 0.607 | 0.926 | .007 | |
| Condomless anal sex – HIV+ partners | CESD | −0.013 | 0.987 | 0.963 | 1.011 | .279 |
| Age | −0.053 | 0.949 | 0.920 | 0.978 | .001 | |
| AUDIT | −0.020 | 0.980 | 0.923 | 1.040 | .502 | |
| Condition | 0.922 | 2.514 | 1.444 | 4.376 | .001 | |
| Baseline risk behavior – HIV+ partners | 0.040 | 1.041 | 1.020 | 1.061 | <.001 | |
| Information | 0.214 | 1.239 | 0.751 | 2.043 | .401 | |
| Motivation | −0.455 | 0.634 | 0.419 | 0.960 | .031 | |
| Behavioral Skills | 0.163 | 1.177 | 0.991 | 1.396 | .063 |
Discussion
The goal of this study was to empirically test a newly developed online HIV sexual risk reduction intervention (called HINTS) among a sample of gay and bisexual men living with HIV who meet sex partners online. HINTS is a four-session, group-based behavioral intervention delivered exclusively online and developed using the IMB model of health behavior change [18, 19]. HINTS differs from previous online sexual risk reduction interventions in that it targets MSM living with HIV across a range of ages, is based on the IMB model of health behavior change, and includes information pertinent to online partner seeking. Sessions consisted of health and Internet safety-related information, as well as presentation and discussion of scenarios to enhance motivation and provide the behavioral skills necessary to reduce sexual risk behavior. A total of 167 men (85 assigned to HINTS and 82 assigned to a Healthy Living control condition) participated in the study. Condomless anal sex (CAS) with male partners was assessed at baseline (preintervention) and at 6-month follow-up. We also assessed IMB variables as potential mediators of intervention effects on sexual risk behavior.
Although the HINTS intervention did not have a significant impact on frequency of CAS when examining sexual risk behavior across all male partners, there were significant intervention effects when tested separately by partner serostatus. Men assigned to the HINTS intervention were significantly less likely to engage in CAS with male partners who were either HIV-negative or whose HIV serostatus was unknown, as compared to men assigned to the Healthy Living control condition. For men living with HIV, CAS with serodiscordant partners confers the greatest risk of HIV transmission [13, 14]. The reduced frequency of this behavior among men who received the HINTS intervention indicates significant alterations in sexual transmission risk behavior, a finding with important clinical and public health implications. Motivation and behavioral skills assessed at 6 months were related to the decreased incidence of CAS with serodiscordant partners. Thus, it appears that having a greater level of motivation for reducing sexual risk and the important skills for enacting safer sex practices is associated with decreased HIV transmission risk behavior. However, these IMB variables did not change due to the HINTS intervention and cannot explain the change in CAS based on HINTS group participation. These IMB findings relate to other previous work linking the components of the IMB model to health behavioral outcomes [20–23].
Information did not have a significant impact in our model, perhaps due to the low reliability of our measure or, more likely, due to the established knowledge base of our sample. In fact, it is quite possible that methodological issues (e.g., reliability, validity) related to all three of our IMB outcome measures may have led to not observing a change in the IMB components as a result of the HINTS intervention. We utilized the IMB theoretical model for developing the HINTS intervention content during in-person interviews and face-to-face focus groups, but perhaps did not adapt existing measures used in our prior work adequately for online use. Thus, the existing measures simply may not have been sensitive enough to assess what participants were really getting from the HINTS intervention that led to the reductions in sexual risk behavior. Future work should look to tailor measures specifically to intervention content administered online.
Men assigned to HINTS also showed greater frequency of CAS with partners living with HIV at follow-up compared to men assigned to the Healthy Living control condition. This result suggests that men who received the HINTS intervention engaged in serosorting behavior with greater frequency than men in the control condition. Serosorting is a commonly endorsed strategy in MSM with and without HIV infection because it is perceived to reduce HIV transmission [9], and serosorting frequency has been shown to increase during some behavioral risk reduction interventions [38, 39]. Motivation level at 6 months was also related to increased incidence of CAS with seroconcordant partners. It appears that having a greater level of motivation for reducing sexual risk is associated with increased serosorting behavior, but again since motivation level did not significantly change due to the HINTS intervention, it cannot explain the increases in serosorting behavior. Regardless, participation in the HINTS intervention promoted serosorting behavior among the participants, perhaps reducing subsequent HIV transmission risk.
Although serosorting can help reduce HIV transmission risk compared to CAS with serodiscordant partners [55], it is important to note that it is also associated with a number of significant health risks, including increased risk for contracting bacterial and viral sexually transmitted infections, and risk of “superinfection” with multiple strains of HIV [55–59]. These health risks, and the potential for increased stigma that may result from serosorting, highlight the limitations of the current findings and the need for future studies to address the unique risks associated with distinct sexual behaviors. In addition, recent evidence suggests that serosorting may be most relevant for MSM with undetectable viral loads [60]. Incorporating conversations around viral load status into sexual decision-making (e.g., viral-sorting) would also be an important aspect of sexual risk reduction to explore in the future.
Some additional limitations are worth noting. The sample was drawn primarily from the East Coast and the Midwest due to logistical difficulties associated with running groups in different time zones. However, the study effectively engaged participants from both urban and rural areas, and the exclusively online nature of the intervention allowed sexual minority men in underserved areas to participate. Participants’ sexual behavior data must be interpreted with some caution, as it was collected online via self-report, which may have resulted in biased reporting. However, this strategy has been successfully used in previous work, and prompts were incorporated to help ensure valid data collection. Use of biomedical prevention strategies (e.g., TasP or PrEP) by participants’ partners was not evaluated in this study, and will be important to account for in the future. HIV treatment is a critical component of recent primary and secondary prevention efforts, and should be incorporated into the development of future risk reduction strategies. Recent recommendations now call for the use of combined bio-behavioral prevention interventions [7], and the brief, online HINTS intervention seems uniquely poised for this role. This study also examined only gay and bisexual men, and therefore cannot be generalized to all MSM, women, transgender individuals, or other people living with HIV. Since our HINTS intervention was specifically developed using input from gay and bisexual men living with HIV and was designed to address transmission risk factors relevant to this group, it is unclear how effective it would be in other populations affected by HIV infection. Although sexual minority men represent the group with the greatest incidence of HIV transmission in the USA, it will be important to assess secondary transmission risk among women and other key groups in future work.
Conclusion
Our novel, theoretically driven, brief group intervention called HINTS was successful in reducing specific HIV transmission risk behaviors, as well as increasing serosorting behavior in a sample of gay and bisexual men who meet their sex partners online. Some components of the IMB model were related to observed changes in sexual risk behavior, but did not explain the main intervention effects. Although these effects were evident at 6-month follow-up, it will be important to examine the durability of the HIV risk reduction and serosorting behaviors over longer periods of time in future work. Use of social media and other forms of Internet-based technology (such as mobile apps) to follow individuals over longer intervals may help to promote and maintain these significant benefits. Given that the HINTS intervention is brief and readily accessible online, its future use is warranted in combination with biomedical strategies.
Funding
This study was funded by an NIMH research grant (R34MH087120). This research was also partially supported by an NIMH training grant (T32MH074387).
Compliance with Ethical Standards
Disclosure of Potential Conflicts of Interest
Conflict of Interest: D.G.C. and S.C.K. have received research grants from NIMH. All other authors declare that they have no conflict of interest.
Research involving Human Participants and/or Animals
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. Centers for Disease Control and Prevention (CDC). HIV Surveillance Report: Diagnoses of HIV Infection and AIDS in the United States and Dependent Areas, 25, 2013. [Google Scholar]
- 2. Centers for Disease Control and Prevention (CDC). HIV Surveillance Report: HIV Among Gay and Bisexual Men, 2015a. http://www.cdc.gov/hiv/group/msm/index.html. Accessed October 7, 2015.
- 3. World Health Organization. Department of HIV/AIDS. Guidelines: Prevention and Treatment of HIV and Other Sexually Transmitted Infections Among Men who have Sex with Men and Transgender People: Recommendations for a Public Health Approach. Geneva, Switzerland: World Health Organization, 2011. [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention (CDC). Serosorting Among Gay, Bisexual and Other Men Who Have Sex With Men 2015b. http://www.cdc.gov/msmhealth/Serosorting.htm. Accessed October 7, 2015.
- 5. McFarland W, Chen YH, Nguyen B et al. Behavior, intention or chance? a longitudinal study of HIV seroadaptive behaviors, abstinence and condom use. AIDS Behav. 2012;16(1):121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. IAPAC. Controlling the HIV Epidemic with Antiretrovirals: International Association of Physicians in AIDS Care, Consensus Statement ― 6 July 2012, 2012. www.iapac.org.
- 7. Marrazzo JM, del Rio C, Holtgrave DR et al. ; International Antiviral Society-USA Panel HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society-USA Panel. JAMA. 2014;312(4):390–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilson DP, Regan DG, Heymer KJ, Jin F, Prestage GP, Grulich AE. Serosorting may increase the risk of HIV acquisition among men who have sex with men. Sex Transm Dis. 2010;37(1):13–17. [DOI] [PubMed] [Google Scholar]
- 9. Snowden JM, Wei C, McFarland W, Raymond HF. Prevalence, correlates and trends in seroadaptive behaviours among men who have sex with men from serial cross-sectional surveillance in San Francisco, 2004-2011. Sex Transm Infect. 2014;90(6):498–504. [DOI] [PubMed] [Google Scholar]
- 10. Smith DK, Herbst JH, Zhang X, Rose CE. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015;68(3):337–344. [DOI] [PubMed] [Google Scholar]
- 11. Baral SD, Wirtz A, Sifakis F, Johns B, Walker D, Beyrer C. The highest attainable standard of evidence (HASTE) for HIV/AIDS interventions: toward a public health approach to defining evidence. Public Health Rep. 2012;127(6):572–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Weller SC, Davis-Beaty K. Condom effectiveness in reducing heterosexual HIV transmission (Review). Cochrane Database Syst Rev. 2002;1(1):CD003255. [DOI] [PubMed] [Google Scholar]
- 13. Crepaz N, Marks G, Liau A et al. ; HIV/AIDS Prevention Research Synthesis (PRS) Team Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. AIDS. 2009;23(13):1617–1629. [DOI] [PubMed] [Google Scholar]
- 14. Pantalone DW, Huh D, Nelson KM, Pearson CR, Simoni JM. Prospective predictors of unprotected anal intercourse among HIV-seropositive men who have sex with men initiating antiretroviral therapy. AIDS Behav. 2014;18(1):78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Crepaz N, Lyles CM, Wolitski RJ et al. ; HIV/AIDS Prevention Research Synthesis (PRS) Team Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20(2):143–157. [DOI] [PubMed] [Google Scholar]
- 16. Johnson BT, Carey MP, Chaudoir SR, Reid AE. Sexual risk reduction for persons living with HIV: research synthesis of randomized controlled trials, 1993 to 2004. J Acquir Immune Defic Syndr. 2006;41(5):642–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Crepaz N, Tungol-Ashmon MV, Higa DH et al. A systematic review of interventions for reducing HIV risk behaviors among people living with HIV in the United States, 1988-2012. AIDS. 2014;28(5):633–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–474. [DOI] [PubMed] [Google Scholar]
- 19. Fisher JD, Fisher WA, Shuper PA. The information-motivation-behavioral skills model of HIV prevention behavior. In: DiClemente RJ, Crosby RA, Kegler MC, eds. Emerging Theories in Health Promotion Practice and Research. San Francisco, CA: Jossey-Bass; 2009:21–63. [Google Scholar]
- 20. Benotsch EG, Nettles CD, Wong F et al. Sexual risk behavior in men attending Mardi Gras celebrations in New Orleans, Louisiana. J Community Health. 2007;32(5):343–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fisher CM. Are information, motivation, and behavioral skills linked with HIV-related sexual risk among young men who have sex with men? J HIV AIDS Soc Serv. 2011;10(1):5–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kalichman SC, Picciano JF, Roffman RA. Motivation to reduce HIV risk behaviors in the context of the information, motivation and behavioral skills (IMB) model of HIV prevention. J Health Psychol. 2008;13(5):680–689. [DOI] [PubMed] [Google Scholar]
- 23. Kiene SM, Fisher WA, Shuper PA et al. Understanding HIV transmission risk behavior among HIV-infected South Africans receiving antiretroviral therapy: an information–motivation–behavioral skills model analysis. Health Psychol. 2013;32(8):860–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cornman DH, Kiene SM, Christie S et al. Clinic-based intervention reduces unprotected sexual behavior among HIV-infected patients in KwaZulu-Natal, South Africa: results of a pilot study. J Acquir Immune Defic Syndr. 2008;48(5):553–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Illa L, Echenique M, Jean GS et al. Project ROADMAP: reeducating older adults in maintaining AIDS prevention: a secondary intervention for older HIV-positive adults. AIDS Educ Prev. 2010;22(2):138–147. [DOI] [PubMed] [Google Scholar]
- 26. Margolin A, Avants SK, Warburton LA, Hawkins KA, Shi J. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health Psychol. 2003;22(2):223–228. [PubMed] [Google Scholar]
- 27. Purcell DW, Latka MH, Metsch LR et al. ; INSPIRE Study Team Results from a randomized controlled trial of a peer-mentoring intervention to reduce HIV transmission and increase access to care and adherence to HIV medications among HIV-seropositive injection drug users. J Acquir Immune Defic Syndr. 2007;46(suppl 2):S35–S47. [DOI] [PubMed] [Google Scholar]
- 28. Grov C, Ventuneac A, Rendina HJ, Jimenez RH, Parsons JT. Perceived importance of five different health issues for gay and bisexual men: implications for new directions in health education and prevention. Am J Mens Health. 2013;7(4):274–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. J Acquir Immune Defic Syndr. 2007;44(2):235–243. [DOI] [PubMed] [Google Scholar]
- 30. McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000;284(4):443–446. [DOI] [PubMed] [Google Scholar]
- 31. Rosser BR, Oakes JM, Horvath KJ, Konstan JA, Danilenko GP, Peterson JL. HIV sexual risk behavior by men who use the Internet to seek sex with men: results of the Men’s INTernet Sex Study-II (MINTS-II). AIDS Behav. 2009;13(3):488–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Arch Sex Behav. 2002;31(2):177–183. [DOI] [PubMed] [Google Scholar]
- 33. Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. 2006;33(9):576–584. [DOI] [PubMed] [Google Scholar]
- 34. Rosser BS, West W, Weinmeyer R. Are gay communities dying or just in transition? An International consultation from the Eighth AIDS Impact Conference examining structural change in gay communities. AIDS Care. 2008;20(5):588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Navejas M, Neaigus A, Torian L, Murrill C. Participation in online and offline HIV prevention among men who have sex with men who use the internet to meet sex partners in New York City. AIDS Behav. 2012;16(2):389–395. [DOI] [PubMed] [Google Scholar]
- 36. Lelutiu-Weinberger C, Pachankis JE, Gamarel KE, Surace A, Golub SA, Parsons JT. Feasibility, acceptability, and preliminary efficacy of a live-chat social media intervention to reduce HIV risk among young men who have sex with men. AIDS Behav. 2015;19(7):1214–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Muessig KE, Baltierra NB, Pike EC, LeGrand S, Hightow-Weidman LB. Achieving HIV risk reduction through HealthMpowerment.org, a user-driven eHealth intervention for young Black men who have sex with men and transgender women who have sex with men. Digit Cult Educ. 2014;6(3):164–182. [PMC free article] [PubMed] [Google Scholar]
- 38. Mustanski B, Garofalo R, Monahan C, Gratzer B, Andrews R. Feasibility, acceptability, and preliminary efficacy of an online HIV prevention program for diverse young men who have sex with men: the keep it up! intervention. AIDS Behav. 2013;17(9):2999–3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mustanski B, Greene GJ, Ryan D, & Whitton SW. Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: the Queer Sex Ed intervention. J Sex Res. 2015;52(2):220–230. [DOI] [PubMed] [Google Scholar]
- 40. Schonnesson LN, Bowen AM, Williams ML. Project SMART: preliminary results from a test of the efficacy of a Swedish Internet-Based HIV Risk-Reduction Intervention for men who have sex with men. Arch Sex Behav. 2016;45(6):1501–1511. [DOI] [PubMed] [Google Scholar]
- 41. Muessig KE, Nekkanti M, Bauermeister J, Bull S, Hightow-Weidman LB. A systematic review of recent smartphone, Internet and Web 2.0 interventions to address the HIV continuum of care. Curr HIV/AIDS Rep. 2015;12(1):173–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Milam J, Morris S, Jain S et al. ; CCTG 592 Team Randomized controlled trial of an internet application to reduce HIV transmission behavior among HIV infected men who have sex with men. AIDS Behav. 2016;20(6):1173–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Morin SF, Shade SB, Steward WT et al. ; Healthy Living Project Team A behavioral intervention reduces HIV transmission risk by promoting sustained serosorting practices among HIV-infected men who have sex with men. J Acquir Immune Defic Syndr. 2008; 49(5):544–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sikkema KJ, Abler L, Hansen NB et al. Positive choices: outcomes of a brief risk reduction intervention for newly HIV-diagnosed men who have sex with men. AIDS Behav. 2014;18(9):1808–1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schmitz C. LimeSurvey: An Open Source Survey Tool. Hamburg, Germany: LimeSurvey Project Team; https://www.limesurvey.org, 2015. [Google Scholar]
- 46. Kalichman SC, Cherry C, Kalichman MO et al. Randomized clinical trial of HIV treatment adherence counseling interventions for people living with HIV and limited health literacy. J Acquir Immune Defic Syndr. 2013;63(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 48. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
- 49. Hatzenbuehler ML, O’Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Safren SA, O’Cleirigh C, Skeer MR et al. Demonstration and evaluation of a peer-delivered, individually-tailored, HIV prevention intervention for HIV-infected MSM in their primary care setting. AIDS Behav. 2011;15(5):949–958. [DOI] [PubMed] [Google Scholar]
- 51. Kalichman SC, Cherry C, White D et al. Sexual HIV transmission and antiretroviral therapy: a prospective cohort study of behavioral risk factors among men and women living with HIV/AIDS. Ann Behav Med. 2011;42(1):111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kalichman SC, Eaton L, White D et al. Beliefs about treatments for HIV/AIDS and sexual risk behaviors among men who have sex with men, 1997-2006. J Behav Med. 2007;30(6):497–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Coxe S, West SG, Aiken LS. The analysis of count data: a gentle introduction to poisson regression and its alternatives. J Pers Assess. 2009;91(2):121–136. [DOI] [PubMed] [Google Scholar]
- 55. Kennedy CE, Bernard LJ, Muessig KE et al. Serosorting and HIV/STI Infection among HIV-Negative MSM and transgender people: a systematic review and meta-analysis to inform WHO guidelines. J Sex Transm Dis. 2013;2013(2):583627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Grewal R, Allen VG, Gardner S et al. ; OHTN Cohort Study Research Team Serosorting and recreational drug use are risk factors for diagnosis of genital infection with chlamydia and gonorrhoea among HIV-positive men who have sex with men: results from a clinical cohort in Ontario, Canada. Sex Transm Infect. 2017;93(1):71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Marcus U, Schmidt AJ, Hamouda O. HIV serosorting among HIV-positive men who have sex with men is associated with increased self-reported incidence of bacterial sexually transmissible infections. Sex Health. 2011;8(2):184–193. [DOI] [PubMed] [Google Scholar]
- 58. Poudel KC, Poudel-Tandukar K, Yasuoka J, Jimba M. HIV superinfection: another reason to avoid serosorting practice. Lancet. 2007;370(9581):23. [DOI] [PubMed] [Google Scholar]
- 59. van der Helm JJ, Prins M, del Amo J et al. ; CASCADE Collaboration The hepatitis C epidemic among HIV-positive MSM: incidence estimates from 1990 to 2007. AIDS. 2011;25(8):1083–1091. [DOI] [PubMed] [Google Scholar]
- 60. Prestage G, Mao L, Kippax S et al. Use of viral load to negotiate condom use among gay men in Sydney, Australia. AIDS Behav. 2009;13(4):645–651. [DOI] [PubMed] [Google Scholar]