Abstract
Background
Rapid Eye Movement sleep deprivation (REMSD) of rats causes inflammation of the liver and apoptotic cell death of neurons and hepatocytes. Studies also suggest that REM sleep deprivation can cause muscle as well as cardiac injury and neurodegenerative diseases.
Objective and methods
The aim of this research was to determine whether REM sleep deprivation of rats would increase the levels of reactive oxygen species (ROS) in the hepatocytes and create oxidative stress in them. We selectively deprived the rats for REM sleep using the standard flower pot method.
Results
We observed that when rats were subjected to REM sleep deprivation, the levels of ROS in their hepatocytes increased ~184.33% compared to large platform control (LPC) group by day 9 of deprivation, but it returned towards normal level (~49.27%) after recovery sleep for 5 days. Nitric oxide synthase (iNOS) gene expression and protein levels as determined by real-time PCR and western blot analysis respectively were found to be elevated in hepatocytes of REM sleep deprived rats as compared to the LPC group. The level of nitric oxide (NO) in the hepatocytes of REMSD rats also increased by ~404.40% as compared to the LPC group but sleep recovery for 5 days normalized the effect (~135.35% compared to LPC group). We used a large platform control group as a reference group to compare with the REM sleep deprived group as the effect on the hepatocytes of both LPC group and cage control groups were not significantly different.
Discussion
We have analyzed the oxidative stress generated in the hepatocytes of rats due to REM sleep deprivation and further consequences of it. REMS deprivation not only increased the levels of ROS in the hepatocytes but also induced iNOS and NO in them. REM sleep deprived hepatocytes became more susceptible to oxidative stresses on further exposures. Furthermore, our study has great pathological and physiological.
Keywords: Reactive Oxygen Species; Nitric Oxide; Nitric Oxide Synthase; Catalase; Sleep, REM
INTRODUCTION
Sleep is a natural physiological process which is needed for the survival of most of the living beings studied so far1. During sleep, repair of damaged tissue and organs takes place and therefore its deficiency increases the risk of heart and kidney diseases, high blood pressure, diabetes, and stroke2-5. In mammals, sleep is broadly categorized as two types, namely non-rapid eye movement sleep (NREM) and rapid eye movement sleep (REM). REM sleep is reported in all mammals and birds except few exceptions and seems necessary for the maintenance of certain essential body functions like memory consolidation6,7, brain maturation, spatial memory acquisition8, and maintenance of body physiology9. Prolonged loss of REM sleep can alter blood-brain barrier functions10 and can be fatal11,12. In terms of energy metabolism, there is no difference between wakefulness and when the animal is in REM sleep, which constitutes approximately 1/3rd of total sleep13. But extended sleep deprivation experiments in animals have shown that during sleep there is decreased cerebral glucose utilization14.
Most of the studies on REM sleep deprivation have analyzed the biochemical changes that take place in the brain and neurons11-13. Reports also suggest that REMSD can cause apoptosis of neuronal cells15,16 and muscle and cardiac injuries17,18, but what happens to other organs has remained unexplored? ROS are generated when metabolic processes take place in the tissues and the body has a natural system to maintain the balance using anti-oxidants present in the system or available from dietary sources.
The production of excessive ROS due to uncontrolled metabolic processes under stressful conditions can lead to a state, where maintenance and recovery to normal physiological levels become difficult. This can ultimately lead to cell death and tissue disintegration. Studies for testing the relationship between sleep and restoration of normal functioning of the body has been primarily done using total sleep deprivation. Some studies have indicated that ROS are generated due to sleep deprivation which is responsible for alteration of body physiology while others have shown no conclusive evidence of the generation of ROS due to total sleep deprivation.
One study, implicating the involvement of ROS, has reported that lipid peroxidation levels increased in the hippocampus of rodents due to sleep deprivation19, while other study showed that the antioxidant levels decreased in peripheral tissues of animals that were deprived of total sleep for 5 and 10 days and it was restored to normal levels only after rebound recovery sleep16. There are reports of increased superoxide dismutase (SOD) activity in rats which were subjected to total sleep loss (3-14 days) in comparison to control groups20. Some other studies suggest that sleep deprivation creates stress like conditions coupled with oxidative stress leading to decreased levels of glutathione in the whole brain21 and reduced SOD activity in the hippocampus and brainstem22.
Interestingly, there exists contradicting reports giving no conclusive evidence of oxidative damage either in the brain or peripheral tissues such as liver after either short-term (8hrs) or long-term (3-14 days) sleep deprivation. No increase in antioxidant enzymes like SOD, Catalase, Glutathione peroxidase or Malondialdehyde activity has been reported23. It was shown that prolonged wakefulness activates an adaptive stress pathway termed as the unfolded protein response, which momentarily protects against the detrimental consequences of ROS24-26 A recent report has shown a sharp increase in lipid peroxidation in the hepatocytes of sleep deprived rats25. Liver, being the metabolic hub, contributes significantly to the maintenance of body physiology26. Since hepatocytes are known to be involved in metabolism, detoxifying endo- and xenobiotics and synthesis of many proteins like albumin etc.27-29. Hence, we undertook this study to find out whether REMSD of rats would generate ROS in the hepatocytes of the liver and how the ROS generated in them would affect its physiological response.
Our previous study had shown that REM sleep deprivation induced acute phase response in the liver, increased the synthesis of pro-inflammatory cytokines like Interleukin (IL)1β, IL-6 and IL-12 and increased the levels of liver toxicity marker enzymes, alanine transaminase and aspartic transaminase circulating in the blood30IL-6 and IL-12 circulating in the blood of REM sleep deprived rats increased in proportion to the extent of sleep loss. But in contrast the levels of IFN-\u03b3 and a ~200. kDa protein, identified by N-terminal sequencing to be alpha-1-inhibitor-3(A1I3. In the present study, we have shown that REMSD of rats affects the level of ROS in the hepatocytes, increases the expression of NOS gene and the levels of the corresponding protein. Interestingly, we have also observed that the hepatocytes from REM sleep deprived rats become more susceptible to ROS upon further exposure. We also observed the increased production of NO by the hepatocytes after REM sleep deprivation.
MATERIALS AND METHODS
Male Wistar rats weighing between 220-260 gm were used in this study. Animals were housed in the institutional animal house facility with a 12 hr L:D cycle (lights on at 7.00 am). Food and water were provided ad libtium. All experiments were conducted as per the protocol approved by the University's Institutional Animal Ethics Committee.
Methods used for REM sleep deprivation and recovery
Animals were REM sleep deprived by the most widely used flower-pot method31,32. In this method, rats were kept individually on a small raised platform (6.5 cm diameter) surrounded by water in a bucket compared to LPC group where individual rats were kept on a bigger platform of 12.5 cm diameter under identical condition. Cage control (CC) rats were housed in cages under laboratory condition.
Although the animals kept on the small platform (6.5 cm diameter) could sit, crouch and have non-REM sleep, but due to the requirement of postural muscle atonia during REM sleep, they were unable to maintain their extended relaxed body posture on the small platform and tended to fall into the surrounding water. As a result, they wake up at the onset or prior to the appearance of REM sleep and thus are deprived of it. After stipulated days of deprivation, the recovery groups of rats were allowed to sleep uninterrupted in individual cages with a sufficient supply of food and water. The rats were sacrificed on different days (4th, 9th days) of REMSD and after 5 days of recovery and their hepatocytes were isolated for further analysis.
Hepatocytes preparation
Hepatocytes were isolated from the liver of male Wistar rats from CC, LPC, and REM sleep deprived groups by a method used by Shen et al.33. Briefly, the abdomens of the rats were opened through a midline incision. The portal cannula was then placed on a suitable platform and liver was perfused with 0.02% EDTA (Sigma, cat No E9884) solution at 37º C, with a flow rate of 30 ml per minute for 15 minutes. Subsequently, collagenase II (3U/ml; Sigma, cat No C2674) in PBS solution (37°C) was recirculated through the liver at the same flow rate for 15 minutes. After perfusion, liver capsules were disrupted and digested, liver parenchyma was suspended in the ice-cold Hank's balanced salt solution (Sigma, cat no H6648). The resulting cell suspension was washed by centrifugation at 500rpm for 5 min 2-3 times and further centrifuged over 30% percoll (Sigma, P1644) at 100g for 5 min to obtain pure hepatocytes. The viability of the hepatocytes thus obtained as measured by trypan blue exclusion was ≥ 95%.
ROS measurement and optimization of dose for creating oxidative stress
Total ROS level in the hepatocytes obtained from CC, LPC and REMSD group of rats were estimated after labeling with 2',7'-dichlorodihydrofluorescein diacetate (DCF-DA, Sigma, Cat No D6883 ), which is a cell-permeable dye that becomes fluorescent after oxidation by different ROS such as hydroxyl radical, hydrogen peroxide, or peroxynitrite. Briefly, hepatocytes from different groups of rats were treated with 10µM-DCF-DA for 30 min followed by either measurement of ROS level or treatment with different doses 50-500µM of H2O2 (Sigma Aldrich, Cat No 04078) or 10-100mU/ml Xanthine (Sigma, Cat No X0626) /Xanthine oxidase (Sigma, Cat. no X1875) for induction of ROS.
Specific ROS inhibitors were also optimized for effective concentrations by treating the cells with 100-500U/ml Catalase (Sigma, cat No-C1345) and 10-50mU/ml Oxypurinol (Sigma, Cat No O6881). Whenever, ROS inhibitors have used the hepatocytes were treated with them first before DCF-DA treatment, following H2O2 or Xanthine/Xanthine oxidase treatments to induce oxidative stress condition similar to the protocol described for mouse osteoblasts and Human MG63 cells34the roles of ROS in RANKL expression and signaling mechanisms through which ROS regulates RANKL genes are not known. Here we report that increased intracellular ROS levels by H2O2 or xanthine/xanthine oxidase-generated superoxide anion stimulated RANKL mRNA and protein expression in human osteoblast-like MG63 cell line and primary mouse bone marrow stromal cells and calvarial osteoblasts. Further analysis revealed that ROS promoted phosphorylation of cAMP response element-binding protein (CREB. The cells were harvested at the indicated time points after incubation, washed three times with phosphate-buffered saline, and immediately analyzed by Flow cytometer using 488-nm excitation beam. The signals were obtained using a 530-nm bandpass filter (FL-1 channel) for DCF. Each determination is based on the mean fluorescence intensity of 5,000 cells.
Assay for hepatocellular NO production
Hepatocytes were seeded in24-well, flat-bottom plates (Falcon) at 105 cells/well and incubated at 37°C in humidified 5%CO2 conditions with and without 1µg/ml lipopolysaccharides (Sigma, Cat no L 2630). NO was measured indirectly by determination of the concentration of nitrite. Briefly, 100-µl aliquots were removed from hepatocytes cultures and incubated with an equal volume of Griess reagent (1%sulfanilamide,0.1%N-1-naphthyl ethylenediamine dihydrochloride in 2.5% phosphoric acid) from Sigma, Cat No G4410 for 10 min at 37°C. Absolute values of NO were determined using sodium nitrite as standard. Absorbance was read at 550 nm on a microtiter plate reader.
Isolation of RNA and TaqMan Real-time PCR
RNA was isolated from hepatocytes harvested from CC, LPC and REM sleep deprived group of rats and stored in RNA later (Sigma-Aldrich, Cat. R0901) using RNA purification kit (RNeasy Mini Kit, Qiagen, Germany). RNA concentrations and integrity was assessed by Nanodrop and Agilent 2100 Bioanalyzer (Agilent Technologies, Massy, France). Total RNA isolated from the hepatocytes were converted to cDNA using the reverse transcription PCR kit (Applied Biosystems, United States). GADPH served as a housekeeping gene while CC group served as calibrator Probes (Reporter dye FAM-labeled on 5' end and quencher VIC labeled on 3' end), PCR master mix, and PCR plate/tubes were obtained from Applied Biosystems, United States and it was used following the manufacturer's instructions. The catalogue numbers of gene probes were glyceraldehyde 3 phosphate dehydrogenase (GAPDH, Rn01749022_g1), iNOS (Rn02132634_s1) and master mix (Rn99999916-g1).
Western Blot Analysis
Western blotting was performed using a method described previously35HEK293, HeLa, and NIH-3T3 cells, we show that the anti-apoptotic protein Bcl-2 significantly inhibits transcriptional activation of various transcription factors, including NF kappa B, AP1, CRE, and NFAT. A Bcl-2 mutant lacking its BH4 domain (Delta BH4. Primary antibody (Santacruz Biotechnology, Inc, USA) used was at 1/1000 dilutions in 0.1% PBS-tween 20, whereas secondary antibody (Santacruz Biotechnology, Inc, USA) horseradish peroxidase-conjugated was used at 1/5000 dilutions in the same buffer. After following the published procedure the membranes were developed using enhanced chemiluminescence (ECL) reagent (Promega) and photographed using software (Photo and Imaging 2.0; Hewlett-Packard). The analysis of the images was performed with imaging software (Photoshop 8.0; Adobe).
Statistical Analysis
We used LPC group of rats for comparative analysis as statistically CC and LPC control groups were found not to be significantly different (Tukey posthoc analysis followed by ANOVA). We used SPSS (Version 2.7.2) for one-way ANOVA and Tukey's HSD posthoc test for measuring out the effect across treatment groups. The p values ≥ 0.05 were considered significant.
RESULTS
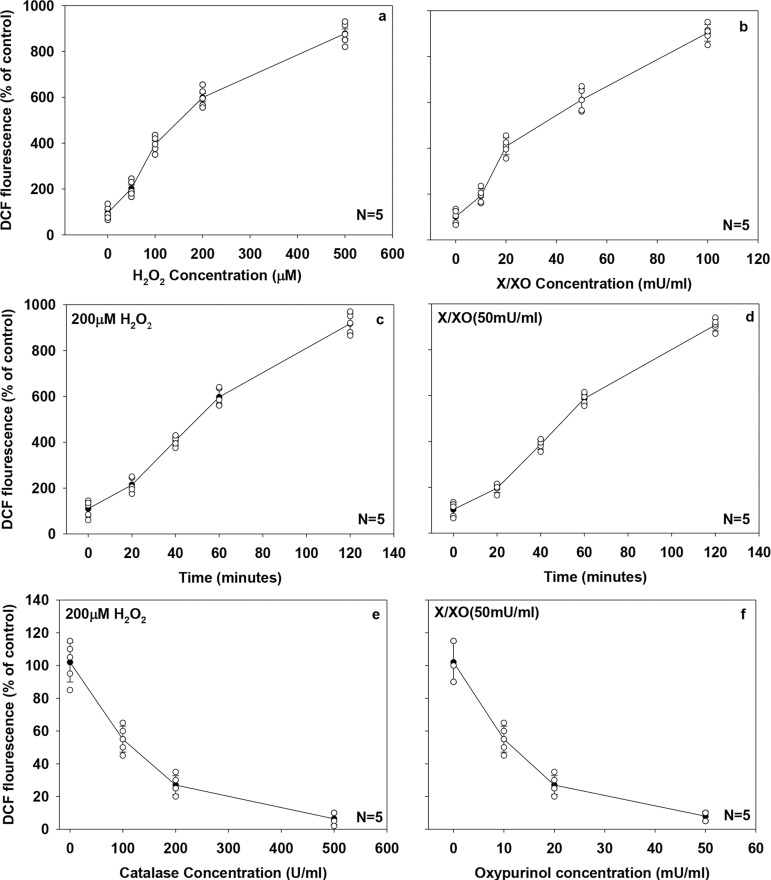
Optimization of dose for induction of ROS using H2O2and Xanthine/Xanthine oxidase and it's suppression by Catalase or Oxypurinol treatment
We treated normal hepatocytes with different concentration of H2O2 or Xanthine/Xanthine oxidase in order to generate reactive oxygen species. Intracellular ROS level increased in a dose-dependent manner with treatments of different concentrations of H2O2 (50-500µM, Fig. 1a, ANOVA, F=354.91, df=4, p<0.001) or Xanthine/Xanthine oxidase (10-100 mU/ml, Fig. 1b, ANOVA, F=374.83, df=4, p<0.001). Based on the result obtained in this experiment we selected the dose of 200µM of H2O2 and 50 mU/ml of Xanthine/Xanthine oxidase to be optimal for the induction of oxidative stress in the hepatocytes. (Fig. 1a, 1b). Then we treated the normal hepatocytes with 200µM-H2O2 or 50 mU/ml- Xanthine/Xanthine oxidase for different time points ranging from 20-120 minutes to determine the optimal time required to induce maximum oxidative stress and observed that 60 minutes is quite sufficient to induce effective ROS production. (Fig. 1c, ANOVA, F=410.21, df=4, p<0.001 and Fig. 1d, ANOVA, F=864.77, df=4, p<0.001). Further, to establish the effective concentrations of ROS inhibitors like Catalase or Oxypurinol which were needed to scavenge the ROS that will be generated. We first, treated the normal hepatocytes with different doses of Catalase (100-500U/ml) or Oxypurinol (10-50µM) followed by treatment with 200µM-H2O2 or 50 mU/ml- Xanthine/Xanthine oxidase for 60 minutes. The doses of Catalase at 500U/ml, (Fig. 1e, 1f ANOVA, F=135.71, df=3, p<0.001) or Oxypurinol at 50µM, (Fig. 1f, ANOVA, F=128.36,df=3, p<0.001) were found to be quite effective in scavenging the ROS generated by treatments with H2O2 (200µM) or Xanthine/Xanthine oxidase (50 mU/ml) for 60 minutes, respectively. Therefore, these doses were used for further ROS stimulation and scavenging experiments. Our results showed that we were able to selectively induce the production of ROS after H2O2 (200µM) or Xanthine/Xanthine oxidase (50 mU/ml) treatment for 60 minutes and could quench them effectively by using specific ROS inhibitors like Catalase (500U/ml) or Oxypurinol (50µM).
Figure 1.
Optimization of ROS level induction and suppression in normal rat hepatocytes by H2O2, X/XO, catalase and oxypurinol. Hepatocytes, isolated from rat were loaded with 10 µM 2, 7-DCF-DA for 30 min and then treated with (a), 50-500 µM H2O2 for 1 h; (b), 10-100 µM xanthine (X) and 10-100 milliunits/ml Xanthine oxidase (XO) for 1 h; (c), 200 µM H2O2 for 20-120 min; (d), 50 µM-X and 50 milliunits/ml-XO for 20-120 min; (e), the hepatocytes were treated with different amount of catalase (100-500U/ml) after 200µM H2O2 induction for an hour and (f), scavenging of ROS production induced by 50mU X/XO for an hour using oxypurinol (10-50 mU/ml). ROS levels were then determined by FAC calibur as described under “Experimental Procedures.” Each point represents the mean ±S.E. of eight determinations from five (N=5) different cell samples. Each determination is the mean DCF fluorescence intensity of 5,000 cells.
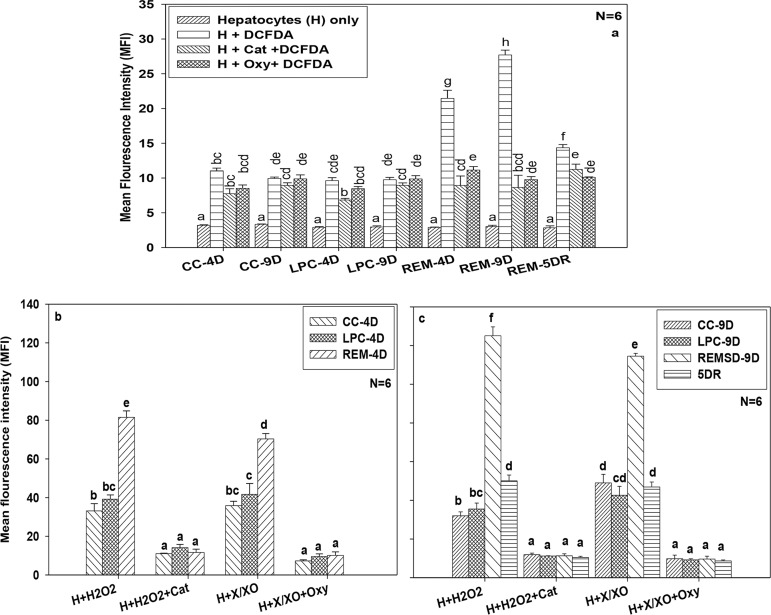
ROS production in hepatocytes by REM sleep deprivation
ROS levels increased significantly with an increase in the number of days of REM sleep deprivation. We used LPC group of rats for comparative analysis as statistically there was no significant difference between CC and LPC control groups ruling out that experimental procedure of keeping rats on the large platform rather than in the cage itself had any effect (Fig. 2a, ANOVA, p<0.05). We observed ~123.04% change in production of ROS in the hepatocytes of the experimental group kept on small platform (6.5 cm diameter) on day 4 of deprivation which increased to~184.33 % on day 9 of deprivation compared to rats kept on LPC group. Sleep recovery of 5 days showed a reduction in the levels of ROS (~49.27% change) in the experimental group when compared to LPC control group indicating the redressal effects (Fig. 2a, ANOVA F=216.92, df=27, p<0.001). At the same time, when we exposed the hepatocytes collected from different groups of rats with ROS quenchers (500U/ml Catalase or 50µM Oxypurinol) which are known to reduce the oxidative stress, we got reduced levels of ROS in hepatocytes after days of deprivation (Fig. 2a, ~30.51% change in the presence of ROS quencher relative to ~123.04% change without it as compared to LPC) and after 9 days of deprivation (Fig. 2a, ~3.35% change in the presence of ROS quencher relative to ~184.33% change without it as compared to LPC). This confirmed that ROS were generated in the hepatocytes due to REMSD which further got quenched by inhibitors like Catalase or Oxypurinol.
Figure 2.
Effect of REM sleep deprivation on ROS production in hepatocytes. Measurement of ROS in hepatocytes from cage control, large platform control, REM sleep deprived group and recovery group of rats. (a), Measurement of ROS in different control groups and REM sleep deprived group of rats treated with scavengers like catalase and oxypurinol after 4 day, 9 days of REM sleep deprivation and 5day of sleep recovery. Differential productions of ROS in progression with REM sleep deprivation compared with control and simultaneously treated with catalase and oxypurinol after 4day of sleep deprivation (b), and 9 day of REMSD and 5day of sleep recovery after 9days of REMSD (c), similarly treated with catalase and oxypurinol. Each vertical bar represents the mean of 6 individual samples with standard error. Treatments that don't share a letter, are statistically different in Tukey post-hoc analysis followed by one way ANOVA across treatment groups. [CC=Cage control, LPC=Large platform control, REM= Rapid eye movement sleep deprivation. H=Hepatocytes, DCFDA= dichlorodihydrofluorescein diacetate, Cat= catalase (200U/ml), Oxy=Oxypurinol (50µM), X/XO=Xanthine/xanthine oxidase (50mU/ ml), H2O2=Hydrogen peroxide 200µM), 4D- after 4 days from start of experiment, 9D- after 9 days from start of experiment, 5DR- After 5 days of REM sleep recovery i.e. rats were allowed to sleep in cages for 5 days].
Sleep loss increased the susceptibility of hepatocytes to further oxidative stress
REM sleep loss not only generated ROS in the hepatocytes of rats but also made them more susceptible to subsequent oxidative stress. We used LPC group of rats for comparative analysis as statistically the effect in CC and LPC control groups were found not to be significantly different. (Fig. 2b, 2c, ANOVA, p<0.05).We report here the increased production of ROS by hepatocytes after 4 day deprivation (~108.03% change) and 9 day deprivation (~252.22% change) compared to LPC group, when hepatocytes were exposed to 200µM-H2O2 for 60 minutes (Fig. 2b, ANOVA F=216.67, df=11, p<0.001 and Fig. 2c, ANOVA F=442.44, df=15, p<0.001). The levels of ROS became normal (~17.49% change compared to LPC) when the similar number of hepatocytes were treated with 500U/ml Catalase (Fig. 2b, 2c). Similarly, when hepatocytes from CC, LPC and REMSD groups after day 4 and 9 of deprivation and after 5Day recovery were treated with 50 mU/ml- Xanthine/Xanthine oxidase, different levels of ROS were induced in them. The levels of ROS observed after 4 days of REM sleep deprivation was~68.88% as compared to LPC group which increased to ~168.76% after 9 days of REM sleep deprivation (Fig. 2b, 2c). The treatment with 50 mU/ml- Xanthine/Xanthine oxidase + 50µM-Oxypurinol reduced the ROS levels on day 4 (~7.03% change) and day 9 (~4.12% change) compared to LPC group of rats (Fig. 2b, 2c). The ROS levels in hepatocytes collected from 5 Day recovery group were similar to that of CC and LPC groups (Fig. 2c). These experiments suggested that REM sleep deprivation made the hepatocytes more susceptible to further oxidative damages.
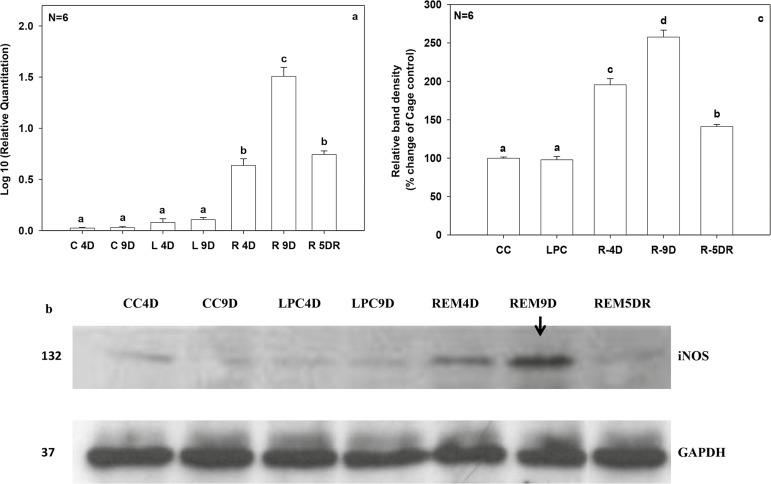
Expression of iNOS gene and protein circulation due to REM sleep deprivation
The iNOS gene expression got affected in hepatocytes of REMSD rats. We used LPC group of rats for comparative analysis as statistically CC and LPC control groups were found not be significantly different (Fig. 3a, 3b, 3c, ANOVA, p<0.05).We found increased expression of iNOS gene by ~7.96fold (log 10 value) by the 4th day of REM sleep deprivation, which increased further upto~14.04 fold (log 10 value) by the 9th day as compared to LPC control. After 5days of recovery sleep, the expression of the iNOS gene improved upto~6.93 fold (log 10 value) compared to LPC control (Fig. 3a, ANOVA F=357.99, df=6, p<0.001). Further, we measured iNOS protein levels in hepatocyte lysate using western blot. Our results show that iNOS protein level increased by~100.8% by 4th day which subsequently increased to ~166.1% by 9 days of REM sleep deprivation compared to that in the LPC group. (Fig. 3b, 3c, ANOVA F=393.94, df=4, p<0.001). The levels of iNOS protein returned to normal levels after 5days of recovery sleep (~46.8% change) compared to LPC controls (Fig. 3b, 3c).
Figure 3.
Measurement of iNOS gene and protein levels in response to REMSD in hepatocytes. (a), The graph shows log fold change in expression pattern of iNOS gene, cage control samples were taken as calibrator while GAPDH was endogenous control for respective genes. (b), Analysis of hepatocytes iNOS protein using WB from CC, LPC and REM sleep deprived and recovery group rats. (c), Densitometric analysis of WB samples for different treatment groups using Image-J software, NIH. Data were represented as relative band density reflected as percentage change of control. Refer figure 2 for statistical and legend details as P value < 0.05 were considered as statistically significant.
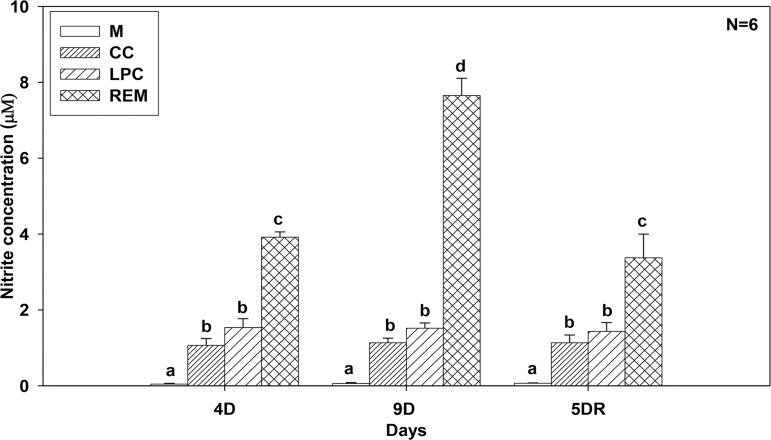
Nitric oxide production in hepatocytes after REMSD
As production of iNOS protein increased in the hepatocytes due to REM sleep loss, we collected the hepatocytes from different groups of rats and measured NO levels in them. Our results show that NO levels were significantly increased in hepatocytes of the REMSD group rats on day 4 (~155.49% change) and day 9 (~404.40% change) than that of LPC group. Further, 5 days of sleep recovery showed redressal effects in terms of NO production but overall NO level was still quite high. (~135.35% change) than of LPC group (Fig. 4, ANOVA F=170.48, df=11, p<0.001). We used LPC group of rats for comparative analysis as statistically CC and LPC groups were found not to be significantly different (Fig. 4, ANOVA, p<0.05).
Figure 4.
Measurement of NO level in hepatocytes in response to REM sleep loss and sleep recovery. Rats were REM sleep deprived of 4 days and 9 days before recovery of 5 days. The hepatocytes were collected from different time points and cultured for nitrite measurement. The X-axis represents the days of REM sleep deprivation and recovery and Y-axis represents the nitrite concentration (µM) in response to REM sleep deprivation. The Kit (Griess reagent kit, Sigma) was used to measure out the levels of nitrite from cultured hepatocytes. [M=Media only, CC=cage control, LPC=large platform control, REM=rapid eye movement), refer figure 2 for statistical details and other legend abbreviation]
DISCUSSION
We subjected the rats to REM sleep deprivation using the flower-pot method and created the LPC and CC groups for comparison. We measured the total ROS level in the hepatocytes of all the groups by using DCF labeling technique. First, we collected the hepatocytes and standardized the method for induction of ROS in them by using H2O2 or Xanthine / Xanthine oxidase and later quenched them by using enzymes like Catalase or Oxypurinol. Lastly, we measured the expression levels of iNOS gene and the protein as well as NO level in hepatocytes after REM sleep deprivation. We used LPC group of rats as a reference group for statistical comparisons as CC and LPC groups had no significant differences in observed parameters. Our findings suggest that REM sleep deprivation of rats can increase ROS production in their hepatocytes which ultimately can induce apoptotic cell death36. Treatment of hepatocytes with H2O2 or Xanthine/Xanthine oxidase can selectively induce production of ROS inside the hepatocytes and it can be quenched by Catalase or Oxypurinol treatment. This gave us a tool to expose the hepatocytes from CC, LPC and REMSD group of rats and investigate how REM sleep deprivation affects their physiology and susceptibility to further oxidative stress.
The oxidative stress created by treatment of hepatocytes with H2O2 or Xanthine/Xanthine oxidase induced the ROS levels to a greater extent in the REMSD group of rats than in the CC and LPC group of rats indicating that REM sleep loss makes the hepatocytes more susceptible to further oxidative stress. Interestingly, when the rats were allowed to have 5 days recovery sleep after REM sleep deprivation their hepatocytes were found not to be as susceptible as before and responded to ROS stress like hepatocytes from CC and LPC groups.
The reason for this is not very clearly understood. Maybe the molecules which are responsible for stress response accumulated during REM sleep deprivation and increased the susceptibility further but they got alleviated to some extent when rats were allowed to have recovery sleep. Other studies have shown increased oxidative stress in brain cells of rats after REMSD20,37, which was also observed in other animal models38. Conditions like obstructive sleep apnea in humans and rodents were found to be positively correlated with increased ROS in the system39,40, and Parkinson disease associated with REM sleep loss was found to contribute to the colon oxidative stress and disruption of mitochondrial function41.
Sleep deprivation was further found to be associated with anxiety-like behavior in rats which can be reduced or prevented by administration of melatonin, which possibly reduces the oxidative stress and maintains the balance between GABAergic and glutamatergic transmission42. Administration of melatonin was found to reduce oxidative stress in rats by blocking down-regulation of γ-aminobutyric acid A-alpha-2 receptors.
These studies suggest that sleep deprivation is somehow directly or indirectly associated with the ROS levels in different tissues. In our previous study, we had also reported that REM sleep deprivation can create inflammation in the liver by increasing the levels of cytokines such as Interleukin-6 (IL-6), IL-12, IL-1β13 indicating that cytokines might be involved in the induction of iNOS genes. Results published by others earlier also suggest that cytokines like tumor necrosis factor alpha (TNF-α), IL-1β, and Interferon-gamma (INF-γ) synergistically activate iNOS gene expression in the liver35.
Lastly, our results show that hepatocytes form REMSD group of rats produced increased levels of NO which was reduced after sleep recovery. Previous studies had shown that NO exerts a protective effect by blocking TNF-α induced apoptosis and hepatotoxicity both in vivo and in vitro, by inhibiting the caspase-3-like protease activity43. Our unpublished results also show that REMSD can cause apoptosis in hepatocytes36. It suggests that might be excess of NO is being produced to counteract the oxidative stress generated due to sleep loss and it protects the hepatocytes from apoptotic death. Our present study is quite unique as it demonstrates that REM sleep deprivation can induce ROS in hepatocytes and make them more susceptible to further oxidative stresses. This shows how important REM sleep is for maintenance of body physiology and survival of animals.
CONCLUSIONS
Our results demonstrate that the REM sleep is very important for the well-being of animals and its loss can't only induce toxicity in the hepatocytes due to the production of ROS but also make them more susceptible to further oxidative stress and death due to apoptosis36. Apart from this, REMSD also can induce iNOS circulation in the system which would increase NO production, which may further affect the well-being of the hepatocytes.
REFERENCES
- 1.Cirelli C, Tononi G. Is sleep essential. PLoS Biol. 2008;6(8):e216. doi: 10.1371/journal.pbio.0060216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018;84:56–66. doi: 10.1016/j.metabol.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 3.Tobaldini E, Costantino G, Solbiati M, Cogliati C, Kara T, Nobili L, et al. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. BNeurosci Biobehav Rev. 2017;74:321–329. doi: 10.1016/j.neubiorev.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Yang H, Haack M, Gautam S, Meier-Ewert HK, Mullington JM. Repetitive exposure to shortened sleep leads to blunted sleep-associated blood pressure dipping. J Hypertens. 2017;35(6):1187–1194. doi: 10.1097/HJH.0000000000001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 6.Graves L, Heller E, Pack A, Abel T. Sleep deprivation selectively impairs memory consolidation for contextual fear conditioning. Learn Mem. 2003;10(3):168–176. doi: 10.1101/lm.48803.LEARNING. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar T, Jha SK. Sleep deprivation impairs consolidation of cued fear memory in rats. PLoS One. 2012;7(10):e47042. doi: 10.1371/journal.pone.0047042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Youngblood BD, Zhou J, Smagin GN, Ryan DH, Harris RB. Sleep deprivation by the "flower pot" technique and spatial reference memory. Physiol Behav. 1997;61(2):249–256. doi: 10.1016/S0031-9384(96)00363-0. [DOI] [PubMed] [Google Scholar]
- 9.Mallick BN, Singh S, Pal D. Role of alpha and beta adrenoceptors in locus coeruleus stimulation-induced reduction in rapid eye movement sleep in freely moving rats. Behav Brain Res. 2005;158:9–21. doi: 10.1016/j.bbr.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Gómez-González B, Hurtado-Alvarado G, Esqueda-León E, Santana-Miranda R, Rojas-Zamorano JA, Velázquez-Moctezuma J. REM sleep loss and recovery regulates blood-brain barrier function. Curr Neurovasc Res. 2013;10(3):197–207. doi: 10.2174/15672026113109990002. [DOI] [PubMed] [Google Scholar]
- 11.Christos GA. Is Alzheimer's disease related to a deficit or malfunction of rapid eye movement (REM) sleep. Med Hypotheses. 1993;41(5):435–439. doi: 10.1016/0306-9877(93)90121-6. [DOI] [PubMed] [Google Scholar]
- 12.Baumann C, Ferini-Strambi L, Waldvogel D, Werth E, Bassetti CL. Parkinsonism with excessive daytime sleepiness--a narcolepsy-like disorder. J Neurol. 2005;252(2):139–145. doi: 10.1007/s00415-005-0614-5. [DOI] [PubMed] [Google Scholar]
- 13.Maquet P. Functional neuroimaging of normal human sleep by positron emission tomography. J Sleep Res. 2000;9(3):207–231. doi: 10.1046/j.1365-2869.2000.00214.x. [DOI] [PubMed] [Google Scholar]
- 14.Everson CA, Smith CB, Sokoloff L. Effects of prolonged sleep deprivation on local rates of cerebral energy metabolism in freely moving rats. Pt 2J Neurosci. 1994;14(11):6769–6778. doi: 10.1523/JNEUROSCI.14-11-06769.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Somarajan BI, Khanday MA, Mallick BN. Rapid Eye Movement Sleep Deprivation Induces Neuronal Apoptosis by Noradrenaline Acting on Alpha1 Adrenoceptor and by Triggering Mitochondrial Intrinsic Pathway. Front Neurol. 2016;7:25–25. doi: 10.3389/fneur.2016.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biswas S, Mishra P, Mallick BN. Increased apoptosis in rat brain after rapid eye movement sleep loss. Neuroscience. 2006;142(2):315–331. doi: 10.1016/j.neuroscience.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 17.Mejri MA, Yousfi N, Hammouda O, Tayech A, Ben Rayana MC, Driss T, et al. One night of partial sleep deprivation increased biomarkers of muscle and cardiac injuries during acute intermittent exercise. J Sports Med Phys Fitness. 2017;57(5):643–651. doi: 10.23736/S0022-4707.16.06159-4. [DOI] [PubMed] [Google Scholar]
- 18.Mônico-Neto M, Dáttilo M, Ribeiro DA, Lee KS, de Mello MT, Tufik S, et al. REM sleep deprivation impairs muscle regeneration in rats. Growth Factors. 2017;35(1):12–18. doi: 10.1080/08977194.2017.1314277. [DOI] [PubMed] [Google Scholar]
- 19.Silva RH, Abílio VC, Takatsu AL, Kameda SR, Grassl C, Chehin AB, et al. Role of hippocampal oxidative stress in memory deficits induced by sleep deprivation in mice. Neuropharmacology. 2004;46(6):895–903. doi: 10.1016/j.neuropharm.2003.11.032. [DOI] [PubMed] [Google Scholar]
- 20.Gopalakrishnan A, Ji LL, Cirelli C. Sleep deprivation and cellular responses to oxidative stress. Sleep. 2004;27(1):27–35. doi: 10.1093/sleep/27.1.27. [DOI] [PubMed] [Google Scholar]
- 21.D'Almeida V, Lobo LL, Hipólide DC, de Oliveira AC, Nobrega JN, Tufik S. Sleep deprivation induces brain region-specific decreases in glutathione levels. Neuroreport. 1998;9(12):2853–2856. doi: 10.1097/00001756-199808240-00031. [DOI] [PubMed] [Google Scholar]
- 22.Ramanathan L, Gulyani S, Nienhuis R, Siegel JM. Sleep deprivation decreases superoxide dismutase activity in rat hippocampus and brainstem. Neuroreport. 2002;13(11):1387–1390. doi: 10.1097/00001756-200208070-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.D'Almeida V, Hipólide DC, Azzalis LA, Lobo LL, Junqueira VB, Tufik S. Absence of oxidative stress following paradoxical sleep deprivation in rats. Neurosci Lett. 1997;235(1-2):25–28. doi: 10.1016/s0304-3940(97)00706-4. [DOI] [PubMed] [Google Scholar]
- 24.Brown MK, Naidoo N. The UPR and the anti-oxidant response: relevance to sleep and sleep loss. Mol Neurobiol. 2010;42(2):103–113. doi: 10.1007/s12035-010-8114-8. [DOI] [PubMed] [Google Scholar]
- 25.Chang HM, Mai FD, Chen BJ, Wu UI, Huang YL, Lan CT, et al. Sleep deprivation predisposes liver to oxidative stress and phospholipid damage: a quantitative molecular imaging study. J Anat. 2008;212(3):295–305. doi: 10.1111/j.1469-7580.2008.00860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rui L. Energy metabolism in the liver. Compr Physiol. 2014;4(1):177–197. doi: 10.1002/cphy.c130024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ménochet K, Kenworthy KE, Houston JB, Galetin A. Simultaneous assessment of uptake and metabolism in rat hepatocytes: a comprehensive mechanistic model. J Pharmacol Exp Ther. 2012;341(1):2–15. doi: 10.1124/jpet.111.187112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rogiers V, Vandenberghe Y, Callaerts A, Verleye G, Cornet M, Mertens K, et al. Phase I and phase II xenobiotic biotransformation in cultures and co-cultures of adult rat hepatocytes. Biochem Pharmacol. 1990;40(8):1701–1706. doi: 10.1016/0006-2952(90)90345-L. [DOI] [PubMed] [Google Scholar]
- 29.Hutson SM, Stinson-Fisher C, Shiman R, Jefferson LS. Regulation of albumin synthesis by hormones and amino acids in primary cultures of rat hepatocytes. Pt 1Am J Physiol. 1987;252(3):E291–E298. doi: 10.1152/ajpendo.1987.252.3.E291. [DOI] [PubMed] [Google Scholar]
- 30.Pandey AK, Kar SK. REM sleep deprivation of rats induces acute phase response in liver: Biochem Biophys Res Commun. Biochem Biophys Res Commun. 2011;410(2):242–246. doi: 10.1016/j.bbrc.2011.05.123. [DOI] [PubMed] [Google Scholar]
- 31.Hicks RA, Okuda A, Thomsen D. Depriving rats of REM sleep: the identification of a methodological problem. Am J Psychol. 1977;90(1):95–102. doi: 10.2307/1421644. [DOI] [PubMed] [Google Scholar]
- 32.van Hulzen ZJ, Coenen AM. Paradoxical sleep deprivation and locomotor activity in rats. Physiol Behav. 1981;27(4):741–744. doi: 10.1016/0031-9384(81)90250-X. [DOI] [PubMed] [Google Scholar]
- 33.Shen L, Hillebrand A, Wang DQ, Liu M. Isolation and primary culture of rat hepatic cells. J Vis Exp. 2012;(64):pii–pii. doi: 10.3791/3917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bai XC, Lu D, Liu AL, Zhang ZM, Li XM, Zou ZP, et al. Reactive oxygen species stimulates receptor activator of NF-kappaB ligand expression in osteoblast. J Biol Chem. 2005;280(17):17497–17506. doi: 10.1074/jbc.M409332200. [DOI] [PubMed] [Google Scholar]
- 35.Massaad CA, Portier BP, Taglialatela G. Inhibition of transcription factor activity by nuclear compartment-associated Bcl-2. J Biol Chem. 2004;279(52):54470–54478. doi: 10.1074/jbc.M407659200. [DOI] [PubMed] [Google Scholar]
- 36.Pandey A, Kumar D, Ray G, Kar S. Biorxiv. 2018. Rapid eye movement sleep deprivation causes apoptotic cell-death of the hepatocytes in rat. [DOI] [Google Scholar]
- 37.Mathangi DC, Shyamala R, Subhashini AS. Effect of REM sleep deprivation on the antioxidant status in the brain of Wistar rats. Ann Neurosci. 2012;19(4):161–164. doi: 10.5214/ans.0972.7531.190405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Villafuerte G, Miguel-Puga A, Rodríguez EM, Machado S, Manjarrez E, Arias-Carrión O. Sleep deprivation and oxidative stress in animal models: a systematic review. Oxid Med Cell Longev. 2015;2015:234952–234952. doi: 10.1155/2015/234952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eisele HJ, Markart P, Schulz R. Obstructive Sleep Apnea, Oxidative Stress, and Cardiovascular Disease: Evidence from Human Studies. Oxid Med Cell Longev. 2015;2015:608438–608438. doi: 10.1155/2015/608438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y, Zhang SX, Gozal D. Reactive oxygen species and the brain in sleep apnea. Respir Physiol Neurobiol. 2010;174(3):307–316. doi: 10.1016/j.resp.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morén C, González-Casacuberta, Navarro-Otano J, Juárez-Flores D, Vilas D, Garrabou G, et al. Colonic Oxidative and Mitochondrial Function in Parkinson's Disease and Idiopathic REM Sleep Behavior Disorder. Parkinsons Dis. 2017;2017 doi: 10.1155/2017/9816095. 9816095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang L, Guo HL, Zhang HQ, Xu TQ, He B, Wang ZH, et al. Melatonin prevents sleep deprivation-associated anxiety-like behavior in rats: role of oxidative stress and balance between GABAergic and glutamatergic transmission. Am J Transl Res. 2017;9(2):2231–2242. [PMC free article] [PubMed] [Google Scholar]
- 43.Taylor BS, Alarcon LH, Billiar TR. Inducible nitric oxide synthase in the liver: regulation and function. Biochemistry (Mosc) 1998;63(7):766–781. [PubMed] [Google Scholar]