In this study, we provide brief messages providers can use when discussing HPV vaccination and guidance for more effectively addressing parents’ questions and concerns about HPV vaccination.
Abstract
Video Abstract
OBJECTIVES:
We sought to identify effective responses to parents’ questions and concerns about human papillomavirus (HPV) vaccine.
METHODS:
In 2017–2018, we surveyed a national sample of 1196 US parents of children aged 9 to 17 years. We recorded brief videos of a pediatrician providing messages that addressed 7 HPV vaccination topics that commonly elicit questions or concerns (eg, recommended age). We randomly assigned parents to 1 of the message topics; parents then viewed 4 videos on that topic in random order and evaluated the messages.
RESULTS:
Parents were more confident in HPV vaccine when they were exposed to messages that addressed lack of knowledge about HPV vaccine (b = 0.13; P = .01), messages that included information about cancer prevention (b = 0.11; P < .001), messages that required a higher reading level (b = 0.02; P = .01), and messages that were longer (b = 0.03; P < .001). Parents were less confident in HPV vaccine when exposed to messages in which urgency was expressed (b = −0.06; P = .005). Analyses conducted by using HPV vaccine motivation as an outcome revealed the same pattern of findings.
CONCLUSIONS:
We provide research-tested messages that providers can use to address parents’ HPV vaccination questions and concerns about 7 common topics. Important principles for increasing message effectiveness are to include information on the benefits of vaccination (including cancer prevention) and avoid expressing urgency to vaccinate when addressing parents' questions or concerns. Additionally, providers may need to be prepared to have longer conversations with parents who express concerns about HPV vaccine, especially regarding safety and side effects.
What’s Known on This Subject:
A variety of messages are available for providers to use when they address parents’ questions and concerns about HPV vaccine. However, little is known about which messages may be more effective.
What This Study Adds:
Parents most often want information about safety, yet this concern is more challenging to address. Effective answers to HPV vaccination questions emphasize benefits (including cancer prevention) but do not to express urgency. We present brief, research-tested messages based on these principles.
Since the vaccine’s introduction >10 years ago, human papillomavirus (HPV) vaccine series completion in the United States has increased to 49% of adolescents aged 13 to 17 in 20171; however, the rate of series completion remains far less than the Healthy People 2020 goal of 80% coverage of adolescents aged 13 to 15,1,2 and follow-through (ie, completion among children who have initiated HPV vaccination) may even be dropping.3 To date, randomized control trials have identified communication techniques providers can use to bring up HPV vaccination and make effective recommendations to parents.4,5 However, little research has been focused on how providers can effectively address questions and ease concerns parents may have after the initial recommendation. Two recent environmental scans of continuing medical education and educational resources about HPV vaccination identified messages developed by the Centers for Disease Control and Prevention (CDC), American Cancer Society, American Academy of Pediatrics, and vaccination experts to help aid providers to communicate information about HPV vaccine.6,7 These messages vary considerably and are focused on how providers can recommend vaccination, answer parents’ concerns or questions, or persuade hesitant parents. To date, little research has been focused on which of these HPV vaccine messages are effective and why.8 We conducted an online video-messaging experiment with parents of preteenagers and teenagers to identify messages that providers can use to effectively address common parental questions and concerns about HPV vaccine and to identify characteristics of messages that explain their greater efficacy.
Methods
Participants
Participants in the study were members of an existing, national online-probability panel of 55 000 US adults who were noninstitutionalized and recruited through address-based sampling.9 Panel members without a computer and Internet access received these resources; those who already had a computer and internet access received points for completing the survey, which could be redeemed for cash, products, or sweepstakes entries. Eligible respondents were parents of at least 1 child aged 9 to 17 years who either had not initiated the HPV vaccine series or had received only the first dose. From November 2017 to January 2018, representatives of the survey company contacted a random sample of 2857 parents via e-mail. Of these parents, 1834 visited the survey Web site and had a child who was of eligible age (9–17 years) and had ≤1 dose of HPV vaccine. Of these respondents, 1313 (72%) met eligibility criteria, provided informed consent, and completed some portion of the survey. After we excluded 50 panelists who did not complete at least two-thirds of the survey, our sample included 1263 parents. The response rate was 61% and based on the American Association for Public Opinion Research response rate 4.10 For the current study, we excluded 67 parents who did not provide data on key variables (eg, confidence and motivation: 30 parents) or were unable to properly view the video messages (37 parents) to arrive at a final analytic sample of 1196 parents. Parents who did not respond to the survey and those who were excluded did not differ from this study’s analytic sample on the key demographics included in our analyses (χ2 and t tests were all P > .05). The University of North Carolina Institutional Review Board approved the study protocol.
Experimental Procedures
More detail about the experimental design appears in the Supplemental Information and is briefly described here. Parents were exposed to 2 different video-messaging experiments during the survey. In the first experiment, we randomly assigned all parents to conditions by employing different vaccine recommendation strategies. In the second experiment, we randomly assigned all parents to messages in which questions or concerns about different HPV vaccine topics were answered (the focus of this study).
Messages
In the experiment, we evaluated 28 messages pertaining to 7 topics about HPV vaccination (4 messages per topic). Four topics were related to lack of knowledge (diseases prevented by HPV vaccine, the age to start HPV vaccine series, vaccinations for boys and girls, and national recommendations for HPV vaccine), and 3 topics were related to concerns (safety and side effects, vaccination for children who are not sexually active, and school requirements for vaccination). We developed these messages from a library of 267 unique messages that were identified in an environmental scan of educational materials about HPV vaccination.7 Each message was coded on 5 characteristics (Table 1; Supplemental Information).
TABLE 1.
HPV Vaccination Topics, Wording, and Characteristics
| Topics | Wording | Characteristics | ||||
|---|---|---|---|---|---|---|
| R | L | C | U | P | ||
| Overall | 7a | 9 | 36%b | 25%c | 71%d | |
| Lack of knowledge | ||||||
| Diseases prevented by HPV vaccine | 1. HPV infection can cause cancer in both men and women. The HPV vaccine will protect your child from many of these cancers. | 5 | 9 | Yes | No | Yes |
| 2. HPV is so common that almost everyone will get it at some point. Most people will never know they are infected. We can prevent it by starting HPV vaccination today. | 7 | 12 | No | Yes | Yes | |
| 3. Over 30 000 Americans get cancer from HPV every year. Most could be prevented with the HPV vaccine. | 7 | 9 | Yes | No | No | |
| 4. HPV is a common virus that millions of people get every year. The HPV vaccine will protect your child from some cancers and genital warts. | 7 | 11 | Yes | No | Yes | |
| The age at which to start the HPV vaccine series | 5. Kids respond more strongly to HPV vaccine when they are younger. This may give better protection against some cancers. | 7 | 7 | Yes | No | No |
| 6. Your kid’s immune system is super powerful at this age. So they will get great protection if we start the HPV vaccine series today. | 7 | 9 | No | Yes | Yes | |
| 7. It is very important to give the HPV vaccine well before exposure to the virus. | 8 | 6 | No | No | No | |
| 8. The younger the better. If we start HPV vaccination at 11 or 12, your kid only needs 2 doses, not 3. | 4 | 8 | No | No | Yes | |
| Vaccination for boys and girls | 9. HPV is a very common virus that infects boys and girls. We can protect your child from the cancers caused by the virus by vaccinating today. | 7 | 11 | Yes | Yes | Yes |
| 10. Only females can get cervical cancer. But the HPV vaccine protects boys and girls from some other cancers, as well as genital warts. | 11 | 10 | Yes | No | No | |
| 11. Men who have HPV probably don’t know it. When boys get the HPV vaccine, they can protect themselves and future partners. | 7 | 9 | No | No | No | |
| 12. HPV infections don’t care if you’re a boy or girl. The virus can cause cancer and many other diseases. | 5 | 8 | Yes | No | Yes | |
| National recommendations for HPV vaccine | 13. The American Academy of Pediatrics recommends giving the HPV vaccine by age 11 or 12. In our practice, we recommend it too. | 9 | 10 | No | No | Yes |
| 14. Guidelines recommend giving the HPV vaccine before age 13. I’ve given the HPV vaccine to my children, and I’d want the same protection for yours. | 8 | 12 | No | No | Yes | |
| 15. Preventive care is important to me. I keep up to date on HPV vaccine guidelines. They show your child is due for the HPV vaccine today. | 7 | 11 | No | Yes | Yes | |
| 16. Experts at the CDC agree that kids should get the HPV vaccine by age 11 or 12 to prevent several cancers. | 8 | 9 | Yes | No | No | |
| Concerns | ||||||
| Safety and side effects | 17. All vaccines can cause minor things, like a sore arm. But I wouldn’t expect to see anything serious. | 9 | 7 | No | No | Yes |
| 18. We have given over 80 million doses of the HPV vaccine in the US since 2006. It’s as safe as the other vaccines I’m recommending today. | 6 | 11 | No | Yes | Yes | |
| 19. My clinic has given thousands of doses of the HPV vaccine, and I’m confident it’s very safe. | 5 | 7 | No | No | Yes | |
| 20. This vaccine is one of the most studied medications on the market. The HPV vaccine is safe, just like the other vaccines we give at this age. | 6 | 10 | No | No | Yes | |
| Vaccination for children not sexually active | 21. This virus is so common that almost everyone is exposed at some point. We are giving the HPV vaccine today so your child will have the best possible protection. | 9 | 11 | No | Yes | Yes |
| 22. Many kids this age are not yet sexually active. Now let’s get your child the HPV vaccine well before any exposure ever takes place. | 6 | 10 | No | No | Yes | |
| 23. We vaccinate kids well before they are exposed to an infection, as with all vaccines. | 9 | 6 | No | No | Yes | |
| 24. This really isn't about sexual activity. The HPV vaccine is about preventing cancer. | 10 | 7 | Yes | No | No | |
| School requirements for vaccination | 25. We can’t wait for schools to know what’s best for your child’s health. | 4 | 5 | No | Yes | Yes |
| 26. School mandates are always incomplete. The HPV vaccine is a very important vaccine that can prevent many cancers. | 9 | 8 | Yes | No | No | |
| 27. My job is to keep your child healthy. And medically, the HPV vaccine is very important. | 6 | 7 | No | No | Yes | |
| 28. School requirements don’t always keep up with medical science. The HPV vaccine is necessary to protect your child’s health. | 10 | 9 | No | No | Yes | |
C, message about cancer prevention; L, length of video message in seconds; P, message contained first-person or second-person pronouns; R, reading level; U, message is urgent.
Median reading level of all messages.
Overall percentage of messages that were about cancer prevention.
Overall percentage of messages in which urgency was expressed.
Overall percentage of messages that contained first-person or second-person pronouns.
Randomization
The survey software randomly assigned parents to receive video messages about 1 of 7 topics about HPV vaccine that parents had reported wanting to learn more about (Supplemental Table 6). Once randomly assigned, parents watched 4 prerecorded video messages about that topic in random order, all of which were delivered by a board-certified female pediatrician (K.T.). After each video message, parents answered questions about how it affected them. After being randomized to conditions, the samples did not differ on key demographics in 9 of 9 tests (χ2 tests and analysis of variance were all P > .05).
Measures
Survey Item Development
Survey items were previously validated in studies of parents, adolescents, and health care providers (P.R., A.M., J.K., N.B., unpublished observations).11–17 When needed, we also adapted items from other sources18–21 or developed new survey items. We cognitively tested the survey instrument with a convenience sample of 16 parents of adolescents who were aged 9 to 17 years to ensure that participants understood the items as we intended. We pretested the instrument with 31 parents from the national panel to ensure proper survey functionality. The full survey instrument is available on request from Dr Brewer.
Outcomes
After each video message, the survey assessed parents’ confidence in and motivation to get HPV vaccines for their children after hearing that message. Items included, “How much would hearing your doctor or health care provider say this increase your confidence in the HPV vaccine?” and “How much would hearing your doctor or health care provider say this make you want to get the [next dose of the] HPV vaccine for your child?” The items had 4-point response scales that ranged from “not at all” (coded as 1) to “a lot” (coded as 4).
Sociodemographic Characteristics
The survey assessed parents’ attitudes toward vaccines in general (4 items; Cronbach’s α = 0.84) and trait reactance (3 items; Cronbach’s α = 0.61).20,22 All items had 5-point responses that ranged from “strongly disagree” (coded as 1) to “strongly agree” (coded as 5). The survey company provided parent's demographic characteristics, including sex, age, race and ethnicity, and education. For demographic and health characteristics of the parent’s index child (ie, reported by the parent), the survey assessed sex, age, and HPV vaccination status (0 doses or ≥1 dose). Sociodemographic characteristics appear in Table 2.
TABLE 2.
Participant Characteristics, N = 1196
| Characteristics | Results |
|---|---|
| Parent | |
| Sex, n (%) | |
| Male | 551 (46) |
| Female | 645 (54) |
| Age, y, mean (SD) | 42.7 (8.1) |
| Race and ethnicity, n (%) | |
| Non-Hispanic white | 839 (70) |
| Non-Hispanic black | 113 (9) |
| Non-Hispanic multiracial or other | 79 (7) |
| Hispanic | 165 (14) |
| Education, n (%) | |
| High school or less | 325 (27) |
| Some college or more | 871 (73) |
| Child | |
| Sex, n (%) | |
| Male | 622 (52) |
| Female | 574 (48) |
| Age, y, mean (SD) | 12.5 (2.7) |
| HPV vaccination status, n (%) | |
| No doses | 719 (60) |
| Initiated series (1 dose) | 477 (40) |
Samples that were randomized to topic conditions did not differ on any key demographics.
Data Analysis
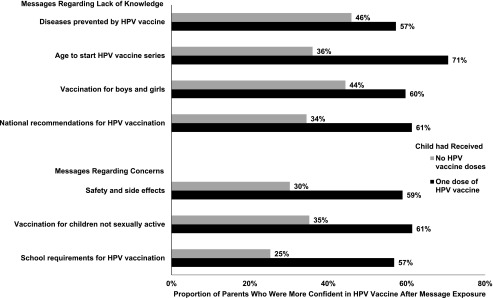
We used Stata 15.1 (Stata Corp, College Station, TX) for analyses. Statistical tests were 2-tailed with a critical Cronbach’s α of 0.05. We calculated the percentage of parents who wanted to learn about the 7 HPV vaccination topics and which topics parents most wanted to learn about from their children’s health care providers (Table 3). We also calculated the percentage of parents who were more confident in HPV vaccine after message exposure (Fig 1). We defined the proportion of parents who were more confident as those who responded with “moderately” or "a lot” to the confidence items. To identify correlates of parents’ confidence in HPV vaccine or motivation to get HPV vaccine for their children, we constructed multilevel linear models to account for within-subject, repeated-measures of study outcomes (Table 4). For each outcome, we first evaluated intercept-only models. Next, we examined each message (level 1 variables) and parental or child sociodemographic characteristics (level 2 variables) as predictors in separate unadjusted models. Any variable with P ≤.10 in the unadjusted models was included in an adjusted multilevel linear model. We report associations as unstandardized regression coefficients (b). We specified unstructured covariance matrices in model estimations and used Huber-White sandwich estimators to account for possible nonnormality in the distribution of the errors in the regression models. Finally, in exploratory analyses, we stratified these models on the child’s HPV vaccination status (Supplemental Table 7).
TABLE 3.
HPV Vaccine Information Wanted From Child’s Health Care Provider
| Topic | Wanted a Little Information, % | Wanted a Lot of Information, % | Wanted the Most Information, % |
|---|---|---|---|
| Safety and side effects | 28 | 40 | 44 |
| Diseases prevented by HPV vaccine | 44 | 40 | 18 |
| Age to start HPV vaccine series | 43 | 39 | 12 |
| Vaccination for boys and girls | 37 | 30 | 8 |
| Vaccination for children not sexually active | 39 | 35 | 7 |
| School requirements for vaccination | 43 | 28 | 6 |
| National recommendations for HPV vaccine | 46 | 35 | 5 |
For last column, parents could choose only 1 topic. Data are for 1189 to 1195 parents (<1% missing).
FIGURE 1.
Proportion of parents who were more confident in HPV vaccine after message exposure.
TABLE 4.
Correlates of Parents’ Confidence in and Motivation to Get HPV Vaccine for Their Children After Message Exposure
| Confidence in HPV Vaccine | Motivation to Get HPV Vaccine | |||||
|---|---|---|---|---|---|---|
| Intercept-Only and Unadjusted Models | Adjusted Model | Intercept-Only and Unadjusted Models | Adjusted Model | |||
| Mean (SD) | b | b | Mean (SD) | b | b | |
| Message characteristics (level 1) | ||||||
| Topics | ||||||
| Lack of knowledge | 2.49 (1.08) | 0.23** | 0.13* | 2.51 (1.08) | 0.27** | 0.17* |
| Concerns | 2.25 (1.08) | Reference | — | 2.24 (1.09) | — | — |
| Reading level required | — | 0.02** | 0.02* | — | 0.02** | 0.01* |
| Length, seconds | — | 0.02** | 0.03** | — | 0.01* | 0.03** |
| About cancer prevention | ||||||
| No | 2.33 (1.09) | Reference | — | 2.33 (1.09) | — | — |
| Yes | 2.45 (1.07) | 0.11** | 0.11** | 2.52 (1.09) | 0.10** | 0.08** |
| Expressed urgency | ||||||
| No | 2.41 (1.08) | Reference | — | 2.42 (1.09) | — | — |
| Yes | 2.35 (1.11) | −0.06* | −0.06* | 2.36 (1.10) | −0.06* | −0.05* |
| Contained first-person or second-person pronouns | ||||||
| No | 2.46 (1.07) | Reference | — | 2.49 (1.09) | — | — |
| Yes | 2.36 (1.09) | −0.05* | −0.02 | 2.37 (1.09) | −0.08** | −0.02 |
| Parent and child characteristics (level 2) | ||||||
| Parent's sex | ||||||
| Male | 2.33 (1.05) | Reference | — | 2.35 (1.04) | — | — |
| Female | 2.44 (1.12) | 0.11 | 0.16* | 2.45 (1.12) | 0.09 | 0.14* |
| Parent's age | — | −0.007* | 0.002 | — | −0.008* | 0.001 |
| Parent's race and ethnicity | ||||||
| Non-Hispanic white | 2.32 (1.08) | Reference | — | 2.33 (1.08) | — | — |
| Non-Hispanic black | 2.63 (1.04) | 0.31* | 0.30* | 2.61 (1.04) | 0.28* | 0.25* |
| Non-Hispanic multiracial or other | 2.62 (1.11) | 0.30* | 0.16 | 2.67 (1.12) | 0.33* | 0.19b |
| Hispanic | 2.47 (1.11) | 0.14 | 0.12 | 2.48 (1.10) | 0.14 | 0.11 |
| Parent's education | ||||||
| High school or less | 2.33 (1.08) | Reference | — | 2.35 (1.08) | — | — |
| Some college or more | 2.41 (1.09) | 0.08 | — | 2.42 (1.09) | 0.08 | — |
| Parent's attitude toward vaccines for adolescents | — | 0.42** | 0.39** | — | 0.44** | 0.39** |
| Parent's trait reactance | — | −0.18* | −0.09* | — | −0.20** | −0.11* |
| Child's sex | ||||||
| Male | 2.43 (1.08) | Reference | — | 2.43 (1.08) | — | — |
| Female | 2.35 (1.10) | −0.08 | — | 2.37 (1.10) | −0.06 | — |
| Child’s age | — | −0.04* | −0.04** | — | −0.04** | −0.04** |
| Child’s HPV vaccination status | ||||||
| No doses | 2.15 (1.06) | Reference | — | 2.16 (1.07) | — | — |
| Initiated series (1 dose) | 2.75 (1.02) | 0.60** | 0.54* | 2.77 (1.02) | 0.61** | 0.54* |
| Intercept | — | 2.39** | 0.73* | — | 2.40** | 0.92* |
Regression coefficients (b) are unstandardized. Confidence and motivation had 4-point response scales of 1 (not at all) to 4 (a lot). Topics for lack of knowledge were: diseases prevented by HPV vaccine, the age to start the HPV vaccine series, vaccination for boys and girls, and national recommendations for HPV vaccination. Topics for concerns were: safety and side effects, vaccination for children not sexually active, and school requirements for HPV vaccination. Parent attitude toward vaccines was assessed by using the Vaccine Confidence Scale that measure attitudes toward adolescent vaccination.22 Parent trait reactance was assessed by using a brief scale that measures resistance that arises when a person feels their autonomy is threatened.20 Intraclass correlation for the confidence model was 0.79, and intraclass correlation for the motivation model was 0.82. —, not applicable.
P < .05; ** P < .001.
Missing cases for each variable ranged from 0% to 2%. We generated 20 data sets using multiple imputation by chained equations to estimate plausible values for missing data23 and used augmented regression procedures to avoid perfect prediction for incomplete categorical variables.24 We report multilevel linear model results from the pooled multiply imputed analyses. To examine the effect of nonresponse, we compared unweighted model results with weighted model results to adjust the sample to reflect the general US population. Because using survey weights did not meaningfully change our findings, we present unweighted analyses.
Results
Interest in HPV Vaccine Topics
Most parents wanted to talk with their children’s health care providers about the 7 HPV vaccine topics, ranging from 68% who wanted to talk about safety and side effects to 84% who wanted to talk about the diseases prevented by HPV vaccine (Table 3). When asked which topic they most wanted information about from their children’s health care providers, parents prioritized safety and side effects (44%), diseases prevented by HPV vaccine (18%), and the age at which to start HPV vaccination (12%). Parents placed the lowest priority on discussing vaccination for boys and girls (8%), vaccination for children who were not sexually active (7%), school requirements for vaccination (6%), and national recommendations for HPV vaccine (5%).
Confidence by HPV Vaccine Topic
Among parents whose children had not yet received HPV vaccine, the proportion who were moderately or a lot more confident in HPV vaccine after message exposure ranged from 25% to 46% (Fig 1). Confidence was highest after the parents were exposed to messages about the diseases prevented by HPV vaccine (46%) and vaccination for boys and girls (44%). Confidence was lowest after parents were exposed to messages about safety and side effects (30%) or school requirements for HPV vaccination (25%). Among parents of children who had initiated the HPV vaccine series, the proportion of those who were more confident in HPV vaccine after message exposure ranged from 57% to 71% (Fig 1). Confidence was highest after parents were exposed to messages about the age to start HPV vaccination (71%). For the other topics, approximately three-fifths of parents were more confident after message exposure.
Correlates of HPV Vaccine Confidence
With respect to message characteristics, parents who were exposed to messages that adressed lack of knowledge (b = 0.13; P = .01) were more confident in HPV vaccine compared with parents who were exposed to messages addressing concerns in adjusted analyses (Table 4). Parents who were exposed to messages that required a higher reading grade level (b = 0.02; P = .01) or messages that were longer (b = 0.03; P < .001) were more confident in HPV vaccine. Additionally, parents who were exposed to messages about cancer prevention (b = 0.11; P < .001) were more confident in HPV vaccine. In contrast, parents who were exposed to messages in which urgency was expressed (b = −0.06; P = .005) had lower confidence in HPV vaccine. Finally, parents who were exposed to messages that contained first-person and second-person pronouns had lower confidence in HPV vaccine, but this association was only significant in bivariate analyses.
With respect to parental characteristics, mothers (b = 0.16; P = .002) and parents who were black (b = 0.30; P = .001) were more confident in HPV vaccine after message exposure than fathers and parents who were white, respectively. Parents who had more positive attitudes toward vaccines (b = 0.39; P < .001) and those with children who had initiated the HPV vaccine series (b = 0.54; P < .001) were more confident in HPV vaccine after message exposure. In contrast, parents who had higher trait reactance (b = −0.09; P = .03) or older children (b = −0.04; P < .001) were less confident in HPV vaccine after message exposure.
Correlates of HPV Vaccine Motivation
Findings for motivation with respect to parents exposed to messages that addressed lack of knowledge (b = 0.17; P = .001), messages that required a higher reading grade level (b = 0.01; P = .03), messages that were longer (b = 0.03; P < .001), messages about cancer prevention (b = 0.08; P < .001), messages in which urgency was expressed (b = −0.05; P = .005), and messages that contained first-person and second-person pronouns were similar to findings for confidence in adjusted analysis (Table 4). Additionally, with respect to parent and child characteristics, our findings for motivation with respect to mothers (b = 0.14; P = .007), parents who were black (b = 0.25; P = .004), parents’ attitudes toward vaccines (b = 0.39; P < .001), parents’ trait reactance (b = −0.11; P = .004), children who had initiated the HPV vaccine series (b = 0.54; P < .001), and older children (b = −0.04; P < .001) were similar to our findings for confidence.
Discussion
Providers’ vaccine recommendations are uniquely powerful in motivating patients to undergo vaccination,25 but little is known about how providers can effectively clarify parents’ questions and ease their concerns after initial recommendations. In our national study, most parents wanted to learn more information from their children’s health care providers about each of the 7 HPV vaccine topics, with a priority on learning more about safety and side effects, diseases prevented by HPV vaccine, and the age at which to start vaccination. Additionally, brief messages that addressed common questions and concerns boosted the confidence of the majority of parents with children who had initiated HPV vaccination. Even among parents who had not initiated HPV vaccination for their children, many reported greater confidence after considering the messages.
Our findings suggest general communication principles when responding to parents’ questions and concerns about HPV vaccination. First, communication regarding HPV vaccine may be more effective if providers include information about cancer prevention. Messages that referred to cancer prevention were more effective in increasing confidence and motivating parents to have their children vaccinated. In addition, messages that referred to cancer prevention worked well among both parents of children who were unvaccinated and parents of children who were vaccinated. Previous studies have drawn the same conclusion,8,26–29 but they have focused on recommendations or general informational statements (rather than addressing questions and concerns) and focused on the prevention of specific cancers in either boys or girls (rather than HPV-related cancer prevention in children in general), had smaller samples, or were reliant on relatively few messages.
Second, urgency is important when first raising the topic of vaccination and when recommending it,4,30 but expressing urgency for vaccination when addressing questions and concerns may be counterproductive. We found that messages that expressed urgency were less effective among parents of unvaccinated children. One reason may be that parents who are hesitant feel inappropriately rushed or that their concerns are not being treated with appropriate care.31 Third, the use of personal pronouns may undermine the impact of explanations. We found that using self-referential language (such as “my clinic,” “we can prevent,” and “your child”) in answers to questions and concerns did not help and could have possibly reduced the impact of messages. Other studies have yielded similarly poor performance of messages about providers getting the vaccine for their own children.8,32
Finally, providers may need to prepare to engage in longer discussions about HPV vaccination when parents express concerns. In our study, parents indicated that they most wanted to speak with their children’s health care providers about the safety and side effects of HPV vaccine. However, messages that addressed low knowledge levels were more effective than messages that addressed concerns. One explanation may be that these topics (safety and side effects, vaccination for children who are not sexually active, and school requirements for HPV vaccination) are inherently challenging to address. Another explanation may be that our brief messages may not have been sufficiently detailed to address these concerns. Patients say that they find value in receiving additional information, such as from fact sheets, and in participating in motivational interviewing.33,34 A final explanation may be that our messages addressing low knowledge more often included information about the benefits of vaccination. As such, reiterating vaccination benefits (including cancer prevention) when addressing concerns may also improve the impact of messages.
The study’s strengths include its large national sample of parents of children who were aged 9 to 17 years and its experimental study design. Parents were exposed to video messages presented by a physician rather than reading message text, which more closely reflects the experience of a clinical visit and lends ecological validity to parental responses. Limitations include our examination of vaccine confidence and perceived motivation as a proxy for behavior intention. Although intention is 1 of the strongest predictors of behavior, barriers to action and other impediments can reduce the strength of the association.35 Future research should be conducted to confirm whether providers easing parents’ concerns in clinical settings yields higher uptake of HPV vaccine. Interventions used to increase parents’ confidence in and motivation to get HPV vaccine alone may not increase vaccine uptake; however, they could be used to increase uptake in combination with clear, strong provider recommendations to get the vaccine, as other studies have shown.4,5,25 The validity of our findings must also be interpreted in light of the fact that parents were exposed to a separate experiment of prerecorded videos of vaccine recommendation strategies before they viewed the messages to which they were randomly assigned in our current study. Although randomization in both experiments revealed no observable selection bias in our 7 topic conditions, parents were likely primed to pay closer attention to our messages, which could have influenced the processing of these messages. Finally, because we assigned parents to view messages about topics they had expressed interest in learning about, the effectiveness of our messages in other contexts remains to be established.
Seven brief messages that providers can use to address parents’ questions and ease concerns are shown in Table 5. For the most part, they are the most effective messages in eliciting confidence and motivation for each HPV vaccine topic. We adjusted the messages in places to align with the previously described communication principles. Providers may take these messages as a starting point and elaborate as needed. In our study, messages elicited higher confidence when they were longer and required a higher reading grade level. We aimed for shorter messages that providers could remember. However, parents seeking information may prefer longer answers (ie, those that translate to a longer discussion). In a study such as ours, the trade-off between a discussion about vaccination and receiving other care may not have been as salient as it would be in a clinical visit. Our study sample was also skewed to parents with higher levels of educational attainment, which could also explain the preference for more complex messages. As a means of conveying complex information about HPV vaccination, providers may consider using validated visual aids in their conversations with parents,36 particularly those who may have lower levels of health literacy.
TABLE 5.
Refined Example Messages Used to Address Parents’ Common Questions and Concerns About HPV Vaccine
| Topic | Example Messages |
|---|---|
| Lack of knowledge | |
| Diseases prevented by HPV vaccine | Over 30 000 Americans get cancer from HPV every year. Most could be prevented with the HPV vaccine. |
| The age to start HPV vaccine series | Kids respond more strongly to the HPV vaccine when they are younger. This may give better protection against some cancers. |
| Vaccination for boys and girls | HPV infections don't care if you're a boy or girl. The virus can cause cancer and many other diseases. |
| National recommendations for HPV vaccine | Experts at the CDC agree that kids should get the HPV vaccine by age 11 or 12 to prevent several cancers. |
| Concerns | |
| Safety and side effects | This vaccine is one of the most studied medications on the market. The HPV vaccine is safe, just like the other vaccines given at this age. |
| Vaccination for children not sexually active | This really isn't about sex. The HPV vaccine is about preventing cancer. |
| School requirements for vaccination | School requirements don't always keep up with medical science. The HPV vaccine is an important vaccine that can prevent many cancers. |
Conclusions
Reasons for the low uptake of HPV vaccination in the United States and other countries are well known and have been known for the last decade.37,38 Previous research has firmly established the importance of a provider’s clear recommendation for increasing vaccine uptake25; however, more work is needed to establish how to communicate information that can be used to effectively address questions and concerns that may come up afterward. In our study, we provide examples of brief messages providers could employ in their discussions with parents about HPV vaccine. We also identify general communication principles, such as including information about the benefits of vaccination and cancer prevention and avoiding expressions of urgency to vaccinate when addressing parents’ questions or concerns.
Glossary
- CDC
Centers for Disease Control and Prevention
- HPV
human papillomavirus
Footnotes
Dr Shah prepared the data, conducted statistical analyses, drafted the initial manuscript, and critically reviewed and revised the manuscript; Drs Brewer, Gilkey, Calo, and Todd and Ms Alton Dailey conceptualized and designed the study, developed the survey instrument, supervised data collection, and critically reviewed and revised the manuscript; Dr Boynton supervised data analyses and critically reviewed and revised the manuscript for important methodological content; Ms Robichaud and Ms Margolis assisted in the conceptualization and development of the survey instrument and data collection and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: Dr Brewer has served on paid advisory boards of or received research grants from Merck, Pfizer, and GlaxoSmithKline; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by the Centers for Disease Control and Prevention (with Dr Brewer as principal investigator; grant 3U48DP005017-03S6) and supported by Cooperative Agreement U48 DP005017-01S8 from the Centers for Disease Control and Prevention and the National Cancer Institute. Dr Shah’s time was partially supported by a National Research Service Award Post-Doctoral Traineeship from the Agency for Healthcare Research and Quality, which was sponsored by the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill (grant T32-HS000032). Funders played no role in (1) the study design; (2) the collection, analysis, and interpretation of data; (3) the writing of the report; or (4) the decision to submit the article for publication. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, or the National Cancer Institute. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Brewer has served on paid advisory boards of and received research grants from Merck, Pfizer, and GlaxoSmithKline; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Walker TY, Elam-Evans LD, Yankey D, et al. . National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(33):909–917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. . National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(29):784–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spencer JC, Brewer NT, Trogdon JG, Wheeler SB, Dusetzina SB. Predictors of human papillomavirus vaccine follow-through among privately insured US patients. Am J Public Health. 2018;108(7):946–950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements versus conversations to improve HPV vaccination coverage: a randomized trial. Pediatrics. 2017;139(1):e20161764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dempsey AF, Pyrznawoski J, Lockhart S, et al. . Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: a cluster randomized clinical trial. JAMA Pediatr. 2018;172(5):e180016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kornides ML, Garrell JM, Gilkey MB. Content of web-based continuing medical education about HPV vaccination. Vaccine. 2017;35(35, pt B):4510–4514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calo WA, Gilkey MB, Malo TL, Robichaud M, Brewer NT. A content analysis of HPV vaccination messages available online. Vaccine. 2018;36(49):7525–7529 [DOI] [PubMed] [Google Scholar]
- 8.Malo TL, Gilkey MB, Hall ME, Shah PD, Brewer NT. Messages to motivate human papillomavirus vaccination: national studies of parents and physicians. Cancer Epidemiol Biomarkers Prev. 2016;25(10):1383–1391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.GfK KnowledgePanel: a methodological overview. 2018. Available at: https://www.gfk.com/fileadmin/user_upload/dyna_content/US/documents/KnowledgePanel_-_A_Methodological_Overview.pdf. Accessed February 22, 2018
- 10.The American Association for Public Opinion Research Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. Oakbrook Terrace, IL: AAPOR; 2015 [Google Scholar]
- 11.Reiter PL, Brewer NT, Gottlieb SL, McRee AL, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69(3):475–480 [DOI] [PubMed] [Google Scholar]
- 12.McRee AL, Brewer NT, Reiter PL, Gottlieb SL, Smith JS. The Carolina HPV immunization attitudes and beliefs scale (CHIAS): scale development and associations with intentions to vaccinate. Sex Transm Dis. 2010;37(4):234–239 [DOI] [PubMed] [Google Scholar]
- 13.Brewer NT, Gottlieb SL, Reiter PL, et al. . Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McRee AL, Reiter PL, Gottlieb SL, Brewer NT. Mother-daughter communication about HPV vaccine. J Adolesc Health. 2011;48(3):314–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015;24(11):1673–1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34(9):1187–1192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kornides ML, McRee AL, Gilkey MB. Parents who decline HPV vaccination: who later accepts and why? Acad Pediatr. 2018;18(2S):S37–S43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention NIS-TEEN hard copy questionnaire. 2010. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NIS/NISTEENPUF10_HHQUEX.pdf. Accessed February 22, 2018
- 19.North Carolina Department of Health and Human Services Calendar year 2013–2014 results: Child health assessment and monitoring program (CHAMP). 2017. Available at: https://schs.dph.ncdhhs.gov/data/champ/201314/topics.htm. Accessed February 22, 2018
- 20.Hall MG, Sheeran P, Noar SM, Ribisl KM, Boynton MH, Brewer NT. A brief measure of reactance to health warnings. J Behav Med. 2017;40(3):520–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brewer NT, Hall MG, Noar SM, et al. . Effect of pictorial cigarette pack warnings on changes in smoking behavior: a randomized clinical trial. JAMA Intern Med. 2016;176(7):905–912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gilkey MB, Magnus BE, Reiter PL, McRee AL, Dempsey AF, Brewer NT. The vaccination confidence scale: a brief measure of parents’ vaccination beliefs. Vaccine. 2014;32(47):6259–6265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–399 [DOI] [PubMed] [Google Scholar]
- 24.White IR, Daniel R, Royston P. Avoiding bias due to perfect prediction in multiple imputation of incomplete categorical variables. Comput Stat Data Anal. 2010;54(10):2267–2275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18(3):149–207 [DOI] [PubMed] [Google Scholar]
- 26.Sperber NR, Brewer NT, Smith JS. Influence of parent characteristics and disease outcome framing on HPV vaccine acceptability among rural, southern women. Cancer Causes Control. 2008;19(1):115–118 [DOI] [PubMed] [Google Scholar]
- 27.McRee AL, Reiter PL, Chantala K, Brewer NT. Does framing human papillomavirus vaccine as preventing cancer in men increase vaccine acceptability? Cancer Epidemiol Biomarkers Prev. 2010;19(8):1937–1944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Juraskova I, Bari RA, O’Brien MT, McCaffery KJ. HPV vaccine promotion: does referring to both cervical cancer and genital warts affect intended and actual vaccination behavior? Womens Health Issues. 2011;21(1):71–79 [DOI] [PubMed] [Google Scholar]
- 29.Porter RM, Amin AB, Bednarczyk RA, Omer SB. Cancer-salient messaging for human papillomavirus vaccine uptake: a randomized controlled trial. Vaccine. 2018;36(18):2494–2500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sturm L, Donahue K, Kasting M, Kulkarni A, Brewer NT, Zimet GD. Pediatrician-parent conversations about human papillomavirus vaccination: an analysis of audio recordings. J Adolesc Health. 2017;61(2):246–251 [DOI] [PubMed] [Google Scholar]
- 31.Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatr. 2012;12(1):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gilkey MB, Zhou M, McRee AL, Kornides ML, Bridges JFP. Parents’ views on the best and worst reasons for guideline-consistent HPV vaccination. Cancer Epidemiol Biomarkers Prev. 2018;27(7):762–767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reno JE, O’Leary S, Garrett K, et al. . Improving provider communication about HPV vaccines for vaccine-hesitant parents through the use of motivational interviewing. J Health Commun. 2018;23(4):313–320 [DOI] [PubMed] [Google Scholar]
- 34.Lockhart S, Dempsey AF, Pyrzanowski J, O’Leary ST, Barnard JG. Provider and parent perspectives on enhanced communication tools for human papillomavirus vaccine-hesitant parents. Acad Pediatr. 2018;18(7):776–782 [DOI] [PubMed] [Google Scholar]
- 35.Sheeran P, Webb TL. The intention–behavior gap. Soc Personal Psychol Compass. 2016;10(9):503–518 [Google Scholar]
- 36.Houts PS, Doak CC, Doak LG, Loscalzo MJ. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence [published correction appears in Patient Educ Couns. 2006;64(1–3):393–394)]. Patient Educ Couns. 2006;61(2):173–190 [DOI] [PubMed] [Google Scholar]
- 37.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45(2–3):107–114 [DOI] [PubMed] [Google Scholar]
- 38.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76–82 [DOI] [PMC free article] [PubMed] [Google Scholar]