Abstract
Objective
Our primary objective was to examine the global paediatric workforce and to better understand geographic differences in the number of paediatricians globally. Secondary objectives were to describe paediatric workforce expectations, who provides children with preventative care and when children transition out of paediatric care.
Design
Survey of identified paediatric leaders in each country.
Setting
Paediatric association leaders worldwide.
Main outcome measures
Paediatrician numbers, provision of primary care for children, age of transition to adult care.
Results
Responses were obtained from 121 countries (73% of countries approached). The number of paediatricians per 100 000 children ranged from a median of 0.5 (IQR 0.3–1.4) in low-income countries to 72 (IQR 4–118) in high-income countries. Africa and South-East Asia reported the lowest paediatrician density (median of 0.8 paediatricians per 100 000 children, IQR 0.4–2.6 and median of 4, IQR 3–9, respectively) and fewest paediatricians entering the workforce. 82% of countries reported transition to adult care by age 18% and 39% by age 15. Most countries (91%) but only 64% of low-income countries reported provision of paediatric preventative care (p<0.001, Cochran-Armitage trend test). Systems of primary care provision varied widely. A majority of countries (63%) anticipated increases in their paediatric workforce in the next decade.
Conclusions
Paediatrician density mirrors known inequities in health provider distribution. Fewer paediatricians are entering the workforce in areas with already low paediatrician density, which may exacerbate disparities in child health outcomes. In some regions, children transition to adult care during adolescence, with implications for healthcare training and delivery. Paediatrician roles are heterogeneous worldwide, and country-specific strategies should be used to address inequity in child health provision.
Keywords: paediatric staffing, health service
What is already known on this topic?
Significant discrepancy between burden of disease and distribution of health professionals has been documented.
Various structures are in place for paediatric care across the globe.
The global distribution of paediatricians, their role in providing care to children and the structure for child health systems in various countries are not known.
What this study hopes to add?
There are inequities in both paediatrician distribution and numbers of new paediatricians entering the workforce in areas with high child mortality.
Most countries provide some regular primary care for children, but the systems to provide that care are highly variable.
In many areas, children transition from paediatric care in early adolescence, with implications for training and care delivery.
Introduction
The discrepancy between the global burden of disease and the distribution of health professionals has been well-described.1–9 Areas with the highest disease burden have the lowest percentage of health professionals, exacerbating the impact of the health workforce deficit. The WHO has identified an index of 4.45 health workers (physicians, nurses and midwives) per 1000 population necessary to meet the Sustainable Development Goals (SDGs) by 2030.6 Countries are called on to set specific targets for numbers of health workers including physicians and health specialists depending on their needs and health services structure.
Child health was a focal point in the Millennium Development Goals and continues to be important in the SDGs. Epidemiological shifts towards non-communicable diseases, a renewed focus on optimising child development, the unique health needs of adolescents and emphasis on reducing morbidity not just mortality, all require renewed deliberation about how healthcare for children is delivered and advanced.10–12 Differing health system designs lead to wide variability in the roles that paediatricians and other child health providers fill in supporting the health of a country’s children. Understanding those roles is vital to providing equitable and quality healthcare and to developing appropriate training competencies for all child health professionals.
Some regional efforts have been undertaken to understand where paediatricians are working and what roles they play, but the paediatric workforce worldwide has not been previously described.6 13–15 Similarly, while health systems have been described on country and sometimes regional levels, a global understanding of healthcare systems for children and their variation can provide valuable information for potential reforms at country level.
The goal of this study was to examine the global status of the paediatric workforce and to better understand geographic differences in the types of work that paediatricians undertake in the provision of child healthcare. Our objectives were to identify the number of paediatricians globally, examine paediatric workforce expectations, understand who provides children with regular promotive and preventative care and to learn when children transition out of paediatric care to adult care.
Methods
Survey development
An online survey was developed using REDCap, an electronic survey tool.16 The survey queried the number of paediatricians per country, expected workforce changes, primary care provision for children and age of transition to adult care (online supplementary file 1). Faculty at Boston Children’s Hospital initially piloted the survey with cognitive interviewing to improve question clarity. The refined survey was further piloted and edited with paediatric leaders within the Global Paediatric Education Consortium representing Europe, Asia, Africa and the Middle East.17 As the internationally agreed on languages for communication between paediatric societies in the International Paediatric Association (IPA) are English, French and Spanish, the final survey was translated into French and Spanish by DR Interpreting, Inc. Translated surveys were sent to native French and Spanish speakers to confirm accuracy of the translation.
bmjpo-2018-000397supp001.docx (319.3KB, docx)
Patient and public involvement
Patients and the public were not directly involved in the design of this study.
Study sample
The survey was distributed to identified paediatric leaders with a goal of attaining one response per country or economy. Countries and economies for inclusion were defined as the 193 UN member countries plus the 5 World Bank Economies (Hong Kong, Macau, Palestine, Puerto Rico and Taiwan) with populations of over 500 000 people, for a total of 198 countries and economies. The survey was initially distributed in May 2015 via email to the lead delegates from the 121 countries with active membership in the IPA at that time. Regional and subspecialty societies that did not function at the country level were excluded. The survey was sent to non-respondents each week for three consecutive weeks. In a second phase, contact was made with paediatric leaders within the non-responding countries as well as an additional 45 countries in which paediatric leadership was identified through contacts known to the author group, networks from the Global Paediatric Education Consortium, International Paediatric Academic Leaders Association, Harvard University, the American Academy of Paediatrics Section of International Child Health or through contacts with country Ministries of Health. Paediatric leaders from non-responding countries who were in attendance at the International Paediatric Congress in August 2016 were also identified and approached.
A majority of countries (73) had a single response. Of those countries with duplicate responses to the survey, 30 had only one complete response and 17 required further review by the authors (BH and CR). Of those, seven countries had identical duplicate responses or the response that was most complete was selected. Ten countries were contacted to clarify duplicate responses and nine clarified. One country had two responses with some variation, and the respondents could not be reached for clarification; for that country, the response from the president of the country’s paediatric association was used.
Country statistics for populations under age 18 were obtained from publicly available Unicef country statistics.18 Income and gross domestic product (GDP) classifications were based on 2016 World Bank groupings.
Statistical analysis
Paediatric workforce characteristics were described using frequencies, medians and IQRs where appropriate. Comparisons between regions were calculated using Kruskal-Wallis tests and Fisher’s exact tests, while comparisons between GDP categories were calculated using Cuzick’s non-parametric tests for trend and Cochran-Armitage trend tests. Data were analysed using Stata (Stata 2015. Stata Statistical Software: Release 14. College Station, Texas, USA).
The study protocol was reviewed by the Institutional Review Board at Boston Children’s Hospital and deemed not human subjects research.
Results
Responses were received from 95 (79%) of the 121 countries with IPA membership and 121 (73%) of the 166 total countries and economies for which a contact was identified (online supplementary file 2). In total, this represented 61% of the global 198 countries and economies. Eight countries responded in French, 10 in Spanish and the remainder in English.
bmjpo-2018-000397supp002.pdf (141.3KB, pdf)
There were 32 countries for whom no contact was identified and therefore no survey sent and 45 countries that did not respond to the survey (table 1). No contact identified and non-responder countries did not vary significantly from responder countries by GDP (p=0.18, Fisher’s exact test), but did vary by region (p=0.002, Fisher’s exact test), with more no contact identified countries located in the Western Pacific and more non-responders in Africa. Countries with no contact identified had significantly smaller populations than those targeted, with a median population of 274 000 as compared with a median population of 10 million in responder countries (p<0.001, Kruskal-Wallis test).
Table 1.
Characteristics of responder, non-responder and no contact identified groups
| Responder | Non-responder | No contact identified | P value | |
| Countries, no. (%) | 121 (61) | 45 (23) | 32 (16) | |
| GDP classification† | 0.18* | |||
| Low income, no. (%) | 14 (12) | 12 (27) | 5 (16) | |
| Lower middle income, no. (%) | 30 (25) | 12 (27) | 8 (25) | |
| Upper middle income, no. (%) | 34 (28) | 12 (27) | 12 (38) | |
| High income, no. (%) | 43 (36) | 9 (20) | 7 (22) | |
| Region‡ | 0.002* | |||
| Africa, no. (%) | 23 (19) | 17 (38) | 7 (21) | |
| South-East Asia, no. (%) | 8 (7) | 1 (2) | 1 (3) | |
| South and Central America, no. (%) | 19 (16) | 8 (18) | 5 (16) | |
| Western Pacific, no. (%) | 12 (10) | 4 (9) | 13 (41) | |
| Eastern Mediterranean, no. (%) | 15 (12) | 6 (13) | 0 | |
| North America, no. (%) | 3 (2) | 1 (2) | 0 | |
| Europe, no. (%) | 41 (34) | 8 (18) | 6 (19) | |
| Country population,§ median in thousands (IQR) | 10 824 (4503–43 417) | 7237 (2175–17 468) | 274 (98–1208) | <0.001** |
| Country population<18 years,¶ median in thousands (IQR) | 3744 (1081–14 144) | 3248 (798-9 500) | 113 (27–581) | 0.08** |
| Number of physicians per 100 000 population,†† median (IQR) | 158 (43–290) | 62 (8–241) | 46 (19–147) | 0.002** |
*P values were calculated using Fisher’s exact tests for categorical variables.
**P values were calculated using Kruskal-Wallis tests for continuous variables (based on Χ2 statistics with 2 df).
†World Bank list of economies (2017) (internet). World Bank. Available from: http://databank.worldbank.org/data/download/site-content/CLASS.xls.
‡Region classification based on ‘WHO regional offices’. WHO, 2017, www.who.int/about/regions/en/.
§Population, total (18 September 2017). Retrieved 9 October 2017, from https://data.worldbank.org/indicator/SP.POP.TOTL.
¶The State of the World’s Children 2016 Statistical Tables (27 June 2016). Retrieved 31 October 2017, from https://data.unicef.org/resources/state-worlds-children-2016-statistical-tables/.
††The 2016 update, Global Health Workforce Statistics, WHO, Geneva (http://www.who.int/hrh/statistics/hwfstats/).
GDP, gross domestic product.
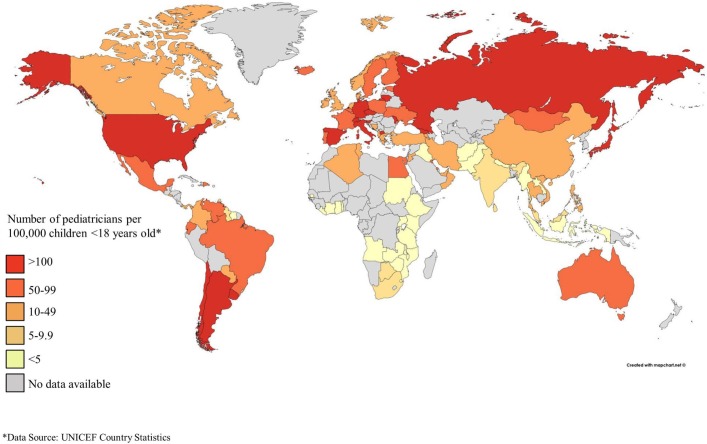
The number of paediatricians reported was normalised against the population of children under 18 years old in each country to obtain a paediatrician density ratio (figure 1). Paediatrician density varied significantly by GDP, ranging from a median of 0.5 paediatricians per 100 000 children in low-income countries to a median of 72 paediatricians per 100 000 children in high-income countries (p<0.001, non-parametric trend test, table 2). In addition, significant variability was seen by region (p<0.001, Kruskal-Wallis test, table 3). The lowest density was seen in Africa (median of 0.8 paediatricians per 100 000 children, IQR 0.4–2.6) and South-East Asia (median of 4 paediatricians per 100 000 children, IQR 3–9) as compared with a global median of 32 paediatricians per 100 000 children (IQR 5–74 and 59 and 87 per 100 000 children (IQR 38 109, and 49–135) in North America and Europe, respectively.
Figure 1.
Pediatrician density per 100 000 children <18 years old*.
Table 2.
Results by GDP classification
| World (n=121) | Low Income (n=14) |
Lower Middle Income (n=30) | Upper Middle Income (n=34) | High Income (n=43) |
P value | |
| Number of paediatricians per country, median (IQR) | 650 (180–3500) | 70 (25–200) | 600 (250–5000) | 1700 (256-6000) | 1400 (500-3,500) | <0.001** |
| Number of paediatricians per 100 000 children<18 years†, median (IQR) | 32 (5–74) | 0.5 (0.3–1.4) | 6 (3–32) | 30 (15–60) | 72 (44–118) | <0.001** |
| Number of new paediatricians entering the workforce each year per 100 000 children<18 years in country†, median (IQR) | 1.44 (0.42–3.07) | 0.08 (0.03–0.18) | 0.45 (0.02–0.93) | 1.36 (0.57–2.09) | 3.10 (2.05–4.06) | 0.01** |
| Number of countries reporting transition from paediatric care‡ | ||||||
| by age 12 years, no. (%) | 3 (3) | 0 | 3 (10) | 0 | 0 | 0.13* |
| by age 15 years, no. (%) | 47 (39) | 9 (64) | 15 (50) | 13 (39) | 10 (23) | 0.002* |
| by age 18 years, no. (%) | 98 (82) | 14 (100) | 27 (90) | 26 (79) | 31 (72) | 0.01* |
| by age 21 years, no. (%) | 118 (98) | 14 (100) | 30 (100) | 33 (100) | 41 (95) | 0.18* |
| Countries reporting regular paediatric promotive and preventive care received, no. (%) | 110 (91) | 9 (64) | 26 (87) | 33 (97) | 42 (98) | <0.001* |
| Percentage of primary care provided by non-physician, median (IQR) | 28 (9–58) | 82 (70–85) | 34 (11–61) | 28.5 (2–51) | 24 (9–45) | 0.01** |
| Percentage of primary care provided by general physician, family doctor or medical officer, median (IQR) | 21 (11–36) | 12 (7–16) | 24 (14–42) | 18 (10–27) | 23 (10–36) | 0.76** |
| Percentage of primary care provided by paediatrician, median (IQR) | 33 (13–57) | 17 (8–22) | 30 (12–49) | 44 (23–56) | 46 (7–73) | 0.04** |
| Number of physicians per 100 000 population,§ median (IQR) | 158.1 (43.4–290.0) | 6.6 (3.0–12.0) | 76.6 (20.1–154.6) | 158.1 (85.4–246.3) | 299 (196.4–379.1) | <0.001** |
*P values were calculated using Cuzick’s nonparametric tests for trend for continuous variables (based on Z statistics with 1 df).
**P values were calculated using Cochran-Armitage trend tests for categorical variables (based on χ² statistics with 1 df).
†The State of the World’s Children 2016 Statistical Tables (27 June 2016). Retrieved 31 October 2017, from https://data.unicef.org/resources/state-worlds-children-2016-statistical-tables/
‡Age of transition from paediatric care not reported by one country in the upper middle income group.
§The 2016 update, Global Health Workforce Statistics, WHO, Geneva (http://www.who.int/hrh/statistics/hwfstats/).
GDP, gross domestic product.
Table 3.
Results by region
| World (n=121) |
Africa (n=23) |
South-East Asia (n=8) | South and Central America (n=19) | Western Pacific (n=12) | Eastern Mediterranean (n=15) | North America (n=3) | Europe (n=41) | P value | |
| GDP classification† | <0.001* | ||||||||
| Low income, no. (%) | 14 (12) | 11 (48) | 1 (13) | 1 (5) | 0 | 1 (7) | 0 | 0 | |
| Lower middle income, no. (%) | 30 (25) | 6 (26) | 6 (75) | 4 (21) | 5 (42) | 5 (33) | 0 | 4 (10) | |
| Upper middle income, no. (%) | 34 (28) | 5 (22) | 1 (13) | 12 (63) | 1 (8) | 4 (27) | 1 (33) | 10 (24) | |
| High income, no. (%) | 43 (36) | 1 (4) | 0 | 2 (11) | 6 (50) | 5 (33) | 2 (67) | 27 (66) | |
| Number of paediatricians per country, median (IQR) | 650 (180-3,500) | 70 (23-167) | 500 (320-3,700) | 1200 (30-5,500) | 2900 (600–5600) | 650 (425–3000) | 25 000 (2667–80 000) | 1545 (500-4500) | <0.001** |
| Number of paediatricians per 100 000 children<18 years,‡ median (IQR) | 32 (5–74) | 0.8 (0.4–2.6) | 4 (3–9) | 47 (9–64) | 32 (17–64) | 25 (5–49) | 59 (38–109) | 87 (49–135) | <0.001** |
| Number of new paediatricians entering the workforce each year per 100 000 children<18 years in country,‡ median (IQR) | 1.44 (0.42–3.07) | 0.08 (0.04–0.14) | 0.42 (0.35–0.79) | 1.47 (1.05–2.67) | 1.44 (0.60–3.06) | 0.80 (0.37–2.19) | 5.61 (1.66–9.57) | 3.08 (1.86–4.05) | <0.001** |
| Transition from paediatric care§ | |||||||||
| by age 12 years, no. (%) | 3 (3) | 1 (4) | 0 | 2 (11) | 0 | 0 | 0 | 0 | 0.25* |
| by age 15 years, no. (%) | 47 (39) | 16 (70) | 6 (75) | 8 (44) | 1 (8) | 11 (73) | 0 | 5 (12) | <0.001* |
| by age 18 years, no. (%) | 98 (82) | 23 (100) | 7 (88) | 15 (83) | 8 (67) | 15 (100) | 2 (67) | 29 (71) | <0.001* |
| by age 21 years, no. (%) | 118 (98) | 23 (100) | 8 (100) | 18 (100) | 11 (92) | 15 (100) | 2 (67) | 41 (100) | 0.01* |
| Countries reporting regular paediatric promotive and preventive care received, no. (%) | 110 (91) | 19 (83) | 7 (88) | 19 (100) | 11 (92) | 10 (67) | 3 (100) | 41 (100) | 0.002* |
| Percentage of primary care provided by non-physician, median (IQR) | 28 (9–58) | 81 (53–85) | 50 (35–68) | 32 (17–61) | 11 (5–27) | 9 (17–26) | 30 (12–32) | 13 (3–33) | <0.001** |
| Percentage of primary care provided by general physician, family doctor or medical officer, median (IQR) | 20 (11–36) | 17 (12–25) | 17 (11–38) | 18 (12–28) | 36 (15–46) | 21 (14–24) | 17 (17–17) | 22 (9–49) | 0.83** |
| Percentage of primary care provided by paediatrician, median (IQR) | 33 (13–59) | 3 (2–16) | 27 (20–33) | 26 (23–55) | 50 (46–71) | 59 (47–69) | 51 (51–51) | 48 (26–71) | <0.001‡ |
| Number of physicians per 100 000 population,¶ (median, IQR) | 158.1 (43.4–290.0) | 12.0 (5.5–37.2) | 39.2 (23.6–64.7) | 117.9 (81.7–116.5) | 175 (114.5–257.5) | 154.6 (85.4–196.4) | 247.7 (207.1–255.4) | 331.1 (277.7–403.5) | <0.001** |
*P values were calculated using Fisher’s exact tests for categorical variables.
**P values were calculated using Kruskal-Wallis tests for continuous variables (based on χ² statistics with 6 df).
†World Bank list of economies (2017) (internet). World Bank. Available from: http://databank.worldbank.org/data/download/site-content/CLASS.xls.
‡The State of the World’s Children 2016 Statistical Tables (27 June 2016). Retrieved 31 October 2017, from https://data.unicef.org/resources/state-worlds-children-2016-statistical-tables/.
§Age of transition from paediatric care not reported by one country in the South and Central America region.
¶The 2016 update, Global Health Workforce Statistics, WHO, Geneva (http://www.who.int/hrh/statistics/hwfstats/).
GDP, gross domestic product.
The number of new paediatricians entering the workforce also varied by GDP classification (p=0.01, non-parametric trend test) and by region (p<0.001, Kruskal-Wallis test). In low-income countries, the paediatric workforce gained a median of 10 new paediatricians per year or 0.08 per 100 000 children, while in high-income countries, the median was 60 new paediatricians per year or 3 per 100 000 children (table 2). In Africa, countries anticipated a median of 5 new paediatricians (0.08 per 100 000 children) per year as compared with a global median of 30 (1.44 paediatricians per 100 000 children) (table 3).
Age of transition out of paediatric care did not vary by GDP (table 2) but did vary by region (p<0.001, Fisher’s exact test, table 3). Notably, in South-East Asia, Africa and the Eastern Mediterranean, over 65% of countries reported that children transitioned from paediatric care by age 15 years, whereas less than 45% of countries reported transition by age 15 in South and Central America and less than 15% in Europe, North America and the Western Pacific.
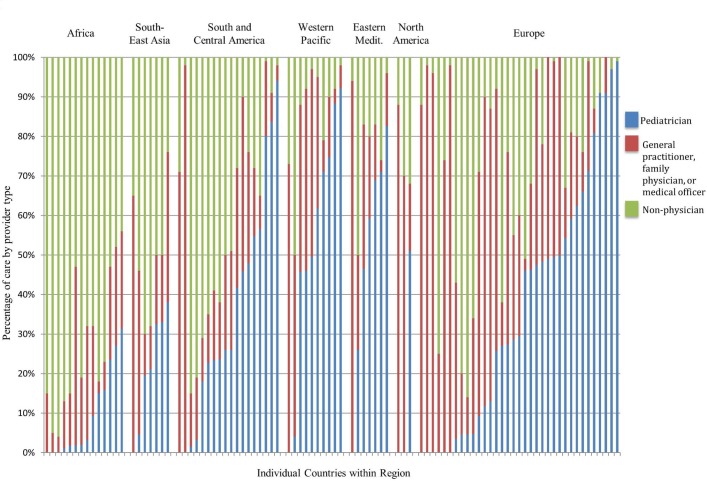
Most countries (91%) responded affirmatively when asked ‘do children in your country receive regular preventative and promotive care throughout childhood (well-child checks, growth monitoring, nutrition assessment, parenting advice, anticipatory guidance, immunization) by either a physician or non-physician health care provider?’ This rate was considerably lower in low-income countries, where only 64% of countries reported regular primary care (p<0.001, Cochran-Armitage trend test, table 2). The type of provider seen for primary paediatric care varied (figure 2). Worldwide, children see non-physicians as the primary care provider a median of 28% of the time (table 2, table 3, IQR 9%–59%). If children saw a physician, that person was a paediatrician (rather than general physician, family physician or medical officer), a median of 33% of the time.
Figure 2.
Type of provider seen for primary care.
Discussion
This international survey of paediatricians is the first, to our knowledge, to report data on paediatrician density and the roles that paediatricians play in provision of care for children on a global scale. This study identified wide variability in paediatrician density, consistent with health workforce findings of physicians as a whole.5 8 19 Areas with the highest burden of paediatric mortality and morbidity had the lowest paediatrician density and paediatricians are joining the workforce at lower rates in those same regions, which may exacerbate inequities in child health. One reason for this inequity may be the existence of a training capacity gap, with fewer avenues to train paediatricians or fewer opportunities for employment in areas with an already low workforce. Some high-income countries have already undertaken more detailed analysis of their paediatric workforce and used this to inform investment and education policy.14 20–24
Another explanation could be the impact of internal or external migration on access to paediatric care. Both have multiple drivers, including job satisfaction, healthy work environment, adequate supplies, feeling of support and appropriate recognition.2 25 26 Within countries, there is often a significant misdistribution of healthcare professionals towards large, wealthy urban areas.1 2 25 27 More detailed data on intranational distribution of paediatricians would be valuable in understanding and seeking to address these disparities of access. Migration between countries has also been well documented.1 2 8 26 While there are no clear data on the impact of this ‘brain drain’ in paediatrics, in both the USA and UK, it is estimated that one-third of the paediatrician workforce are international medical graduates.28 29 Specific efforts to reverse these trends include a focus on providing access to medical training to students from low-resource settings, as exemplified by the Latin American School of Medicine (ELAM) in Cuba, and efforts to develop paediatric residency programmes in low-income and middle-income countries.30 31 Additional efforts to improve salaries, work environments and career opportunities may also be effective means of decreasing external migration and encouraging a trend towards a more equitable distribution of paediatricians globally.32–34
This study identified that many children transition from paediatric care to adult care by age 15, relatively early in adolescence. Age of transition varied by region but not by country income, suggesting that it may be more associated with cultural or professional norms around transition to adulthood rather than workforce planning. Improved understanding of the systems of care for adolescents is critical among UN, WHO and Lancet Commission calls for increased focus, expertise and research on adolescent-specific care.10–12 With early transition to adult care, advancing the adolescent health agenda may require a defined framework for adolescent services and multisectoral approach that engages youth within their communities.
Our study demonstrated that while most countries offered some form of broadly defined preventive care to children, this primary care role is often filled by non-physicians or generalists. In both high-income and low-income countries, task shifting and task sharing have been important and often successful methods for improving access to care and addressing health costs while retaining quality of care.35–39 Most countries continue to explore the appropriate skills mix for providing care, particularly in community settings. Optimising this skills mix will require interprofessional collaboration and training to promote successful multidisciplinary primary care. System planning needs to account for and support the primary role of family and the informal care structures that may exist in communities. A thoughtful country-level approach is required to balance development of preventive and community interventions, alongside secondary and tertiary level services with appropriate referral structures.
Workforce studies, including this one, may not capture all of the specific roles that health professionals play, including leadership in healthcare systems, policy and government; educators and researchers in universities and community advocates. A robust national workforce strategy needs to account for these roles, and country-level human resources for health planning should establish a target density for the paediatrician workforce in relation to their expected roles within the system. For example, the role of a paediatrician in even high density, high-income countries such as the USA, UK and Australia is by design quite different, with paediatricians providing primary care in the former, and secondary and tertiary care in the latter. Clear understanding and designation of tasks such as provision of primary care and age of transition to adult care would need to be considered in order to appropriately define paediatric workforce requirements. Analysis of skills mix needs should also incorporate anticipated epidemiological changes including a reduction in infectious causes of under-5 mortality, an increase in the proportion of neonatal mortality and a shift towards chronic diseases in children.12 40 As countries work to scale-up their healthcare workforce, these baseline data can help inform development strategies.41 42
This study has several limitations. We found no validated tool that would appropriately meet our study objective, therefore developed the survey de novo. Despite piloting the survey among multiple countries, cultures and languages, it is possible that some terms, while commonly used, may have been interpreted differently in different settings, particularly among respondents for whom French, English or Spanish was not their native language. All data were collected as survey responses, usually from a single representative in each country. While we targeted experts at the national paediatric association level who would have knowledge of the state of paediatrics and child health in that nation, responses could vary among individuals particularly for more subjective questions. While we achieved a high level of response globally, there were regional gaps, with particular low responses from West Africa and the Western Pacific. Countries with low physician density and population were similarly under-represented in this sample. These challenges may have been due to language or internet access difficulties, absence of or less active national paediatric organisation or simply limited paediatric presence in those countries. This study was focused on paediatricians, a small component in any country of the human workforce related to child health and health systems. However, paediatricians are important resources for countries, with substantial understanding of child health needs who can also help support country development of child health services and provide guidance for the continuum of care for children and families.
Conclusion
As the global community seeks universal health coverage and works to address the known shortage in healthcare workers, care should be taken to meet the health workforce needs of the world’s children and adolescents. Clarification of paediatrician roles and accompanying skill mix is important in developing health workforce capacity to meet those needs. This study described the state of the paediatric workforce worldwide with notable variability in paediatrician density and roles in different countries. A training capacity gap in countries with high disease burdens may exacerbate the problem of a small workforce relative to healthcare needs. These findings highlight the need for country specific child health workforce strategies, assisted by the development of standardised tools to monitor healthcare capacity and outcomes as countries focus on meeting the SDGs for child health.
Supplementary Material
Acknowledgments
The authors wish to thank Edgar Vesga for his assistance with survey implementation, members of the Global Pediatric Education Consortium who piloted the survey, Julie Hurlbut for assistance with data analysis, tables and figures, Lisa Asaro and David Wypij for assistance with statistical analysis and Judith Palfrey for editing.
Footnotes
Patient consent for publication: Not required.
Contributors: BDH and CMR conceptualised and designed the study, designed the data collection instruments, coordinated and supervised data collection, drafted the initial manuscript and reviewed and revised the manuscript. WN, RA and KDF coordinated data collection, reviewed and revised the manuscript. HPH assisted with design of the data collection instrument including piloting and reviewed and revised the manuscript. WJK advised the international approach, aided with data collection, reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Chen C, Buch E, Wassermann T, et al. . A survey of Sub-Saharan African medical schools. Hum Resour Health 2012;10:4 10.1186/1478-4491-10-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kasper J, Bajunirwe F. Brain drain in sub-Saharan Africa: contributing factors, potential remedies and the role of academic medical centres. Arch Dis Child 2012;97:973–9. 10.1136/archdischild-2012-301900 [DOI] [PubMed] [Google Scholar]
- 3. Liu JX, Goryakin Y, Maeda A, et al. . Global Health Workforce Labor Market Projections for 2030. Hum Resour Health 2017;15:11 10.1186/s12960-017-0187-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baker T. Pediatric emergency and critical care in low-income countries. Paediatr Anaesth 2009;19:23–7. 10.1111/j.1460-9592.2008.02868.x [DOI] [PubMed] [Google Scholar]
- 5. Shehu BB, Ameh EA. Poverty and disease burden vs medical education in sub-Saharan Africa. Ann Afr Med 2007;6:139–41. 10.4103/1596-3519.55706 [DOI] [PubMed] [Google Scholar]
- 6. WHO. Health workforce Requirements for Universal health coverage and the sustainable development goals: Human Resources for Health Oberserver Series, 2016:17. [Google Scholar]
- 7. Pozo-Martin F, Nove A, Lopes SC, et al. . Health workforce metrics pre- and post-2015: a stimulus to public policy and planning. Hum Resour Health 2017;15:14 10.1186/s12960-017-0190-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crisp N, Chen L. Global supply of health professionals. N Engl J Med 2014;370:950–7. 10.1056/NEJMra1111610 [DOI] [PubMed] [Google Scholar]
- 9. Frenk J, Chen L, Bhutta ZA, et al. . Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010;376:1923–58. 10.1016/S0140-6736(10)61854-5 [DOI] [PubMed] [Google Scholar]
- 10. Patton GC, Sawyer SM, Santelli JS, et al. . Our future: a Lancet commission on adolescent health and wellbeing. Lancet 2016;387:2423–78. 10.1016/S0140-6736(16)00579-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Every Woman Every Child: The Global Strategy for Women’ s, Children’ s and Adolescents’ Health (2016-2030), 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kyu HH, Pinho C, Wagner JA, et al. . Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: Findings from the global burden of disease 2013 study. JAMA Pediatr 2016;170:267–87. 10.1001/jamapediatrics.2015.4276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Esso D, del Torso S, Hadjipanayis A, et al. . Paediatric primary care in Europe: variation between countries. Arch Dis Child 2010;95:791–5. 10.1136/adc.2009.178459 [DOI] [PubMed] [Google Scholar]
- 14. Woodhead M. China to train 22,000 more paediatricians in next four years. BMJ 2016;352:i1376 10.1136/bmj.i1376 [DOI] [PubMed] [Google Scholar]
- 15. Ehrich JH, Tenore A, del Torso S, et al. . Diversity of pediatric workforce and education in 2012 in Europe: a need for unifying concepts or accepting enjoyable differences?. J Pediatr 2015;167:471–6. 10.1016/j.jpeds.2015.03.031 [DOI] [PubMed] [Google Scholar]
- 16. Harris PA, Taylor R, Thielke R, et al. . Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Pediatric Education Consortium. http://www.globalpediatrics.org/
- 18. UNICEF. Country Statistics. 2015. https://wwwuniceforg/statistics/index_countrystatshtml.
- 19. WHO. Global strategy on human resources for health: workforce 2030, 2016. [Google Scholar]
- 20. Ranson MK, Chopra M, Atkins S, et al. . Priorities for research into human resources for health in low- and middle-income countries. Bull World Health Organ 2010;88:435–43. 10.2471/BLT.09.066290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McColgan M, Winch R, Clark SJ, et al. . The changing UK paediatric consultant workforce: report from the Royal College of Paediatrics and Child Health. Arch Dis Child 2017;102:170–3. 10.1136/archdischild-2016-312055 [DOI] [PubMed] [Google Scholar]
- 22. Freed GL, Moran LM, Van KD, et al. . Current workforce of general pediatricians in the United States. Pediatrics 2016;137:e20154242 10.1542/peds.2015-4242 [DOI] [PubMed] [Google Scholar]
- 23. Mullan F, Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. Lancet 2007;370:2158–63. 10.1016/S0140-6736(07)60785-5 [DOI] [PubMed] [Google Scholar]
- 24. Hu KJ, Sun ZZ, Rui YJ, et al. . Shortage of paediatricians in China. Lancet 2014;383:954 10.1016/S0140-6736(14)60482-7 [DOI] [PubMed] [Google Scholar]
- 25. Leu HI, Chang WT, Lin MH, et al. . Urban-Rural Disparity in Geographical and Temporal Availability of Pediatric Clinics: A Nationwide Survey in Taiwan. Pediatr Neonatol 2017;58 10.1016/j.pedneo.2016.07.008 [DOI] [PubMed] [Google Scholar]
- 26. Bundred P, Gibbs T. Medical migration and Africa: an unwanted legacy of educational change. Med Teach 2007;29:893–6. 10.1080/01421590701814278 [DOI] [PubMed] [Google Scholar]
- 27. Shipman SA, Lan J, Chang CH, et al. . Geographic maldistribution of primary care for children. Pediatrics 2011;127:19–27. 10.1542/peds.2010-0150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Academy of Pediatrics Committee on Pediatric Workforce. Pediatrician workforce statement. Pediatrics 2005;116:263–9. 10.1542/peds.2005-0873 [DOI] [PubMed] [Google Scholar]
- 29. RCPCH. RCPCH Medical Workforce Census 2013, 2014. [Google Scholar]
- 30. Huish R. Going where no doctor has gone before: The role of cuba’s latin american school of medicine in meeting the needs of some of the world’s most vulnerable populations. Public Health 2008;122:552–7. 10.1016/j.puhe.2008.03.001 [DOI] [PubMed] [Google Scholar]
- 31. Ganapathi L, Martins Y, Schumann D, et al. . Overcoming challenges to develop pediatric postgraduate training programs in low- and middle-income countries. Educ Health 2014;27:277–82. 10.4103/1357-6283.152189 [DOI] [PubMed] [Google Scholar]
- 32. Aluttis C, Bishaw T, Frank MW. The workforce for health in a globalized context-global shortages and international migration. Glob Health Action 2014;7:23611 10.3402/gha.v7.23611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Taylor AL, Hwenda L, Larsen BI, et al. . Stemming the brain drain--a WHO global code of practice on international recruitment of health personnel. N Engl J Med 2011;365:2348–51. 10.1056/NEJMp1108658 [DOI] [PubMed] [Google Scholar]
- 34. Dayrit M, Taylor A, Taylor A, Yan J, et al. . WHO code of practice on the international recruitment of health personnel. Bull World Health Organ 2008;86:739 10.2471/BLT.08.058578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Penazzato M, Davies MA, Apollo T, et al. . Task shifting for the delivery of pediatric antiretroviral treatment: a systematic review. J Acquir Immune Defic Syndr 2014;65:414–22. 10.1097/QAI.0000000000000024 [DOI] [PubMed] [Google Scholar]
- 36. Sanne I, Orrell C, Fox MP, et al. . Nurse versus doctor management of HIV-infected patients receiving antiretroviral therapy (CIPRA-SA): a randomised non-inferiority trial. Lancet 2010;376:33–40. 10.1016/S0140-6736(10)60894-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lynch S, Ford N, van Cutsem G, et al. . Public health. Getting HIV treatment to the most people. Science 2012;337:298–300. 10.1126/science.1225702 [DOI] [PubMed] [Google Scholar]
- 38. WHO. Treat, Train, Retain. The AIDS and health workforce plan, 2006. [Google Scholar]
- 39. Fulton BD, Scheffler RM, Sparkes SP, et al. . Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Hum Resour Health 2011;9:1 10.1186/1478-4491-9-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kanyuka M, Ndawala J, Mleme T, et al. . Malawi and millennium development goal 4: A countdown to 2015 country case study. Lancet Glob Health 2016;4 e201–e214. 10.1016/S2214-109X(15)00294-6 [DOI] [PubMed] [Google Scholar]
- 41. Mullan F, Frehywot S, Omaswa F, et al. . Medical schools in sub-Saharan Africa. Lancet 2011;377:1113–21. 10.1016/S0140-6736(10)61961-7 [DOI] [PubMed] [Google Scholar]
- 42. Haley CA, Vermund SH, Moyo P, et al. . Impact of a critical health workforce shortage on child health in Zimbabwe: a country case study on progress in child survival, 2000-2013. Health Policy Plan 2017;32:czw162 10.1093/heapol/czw162 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2018-000397supp001.docx (319.3KB, docx)
bmjpo-2018-000397supp002.pdf (141.3KB, pdf)