Abstract
Acute uncomplicated diverticulitis (AUD) is generally felt to be caused by obstruction and inflammation of a colonic diverticulum and occurs in about 4–5% of patients with diverticulosis. The cornerstone of AUD treatment has conventionally been antibiotic therapy, but with a paradigm shift in the underlying pathogenesis of the disease from bacterial infection to more of an inflammatory process, as well as concerns about antibiotic overuse, this dogma has recently been questioned. We will review emerging data that supports more selective antibiotic use in this population, as well as newer guidelines that advocate this position as well. While there are no discrete algorithms to guide us, we will attempt to suggest clinical scenarios where antibiotics may reasonably be withheld.
Keywords: Acute uncomplicated diverticulitis, Antibiotics, Colitis, Diverticular disease
Introduction
Diverticulosis coli is defined as the presence of sac-like protrusions in the colonic wall [1]. Over half of adults older than 70 years of age undergoing colonoscopy are noted to have incidental diverticulosis [2]. Manifestations and complications of diverticular disease include acute diverticulitis, symptomatic uncomplicated diverticular disease (with symptoms suggestive of diverticulitis in the absence of overt inflammation), diverticular bleeding, and segmental colitis associated with diverticulosis [1]. Acute diverticulitis, the subject of this article, is the manifestation of mucosal inflammation of a diverticulum [1] and occurs in about 4–5% of patients with diverticulosis [3, 4]. Of those patients, about 85% will have uncomplicated disease [5]. Furthermore, recurrence occurs in about 13.3–23.4% of people with diverticulitis [6, 7, 8, 9]. This is in contrast to earlier studies that estimated a recurrence rate of about 25–45% [10, 11, 12]. Furthermore, fewer than 6% of patients with recurrence develop complications or need for emergent surgical intervention [7, 8, 9]. Acute uncomplicated diverticulitis (AUD) is the most common acute complication of diverticular disease [13].
Pathogenesis
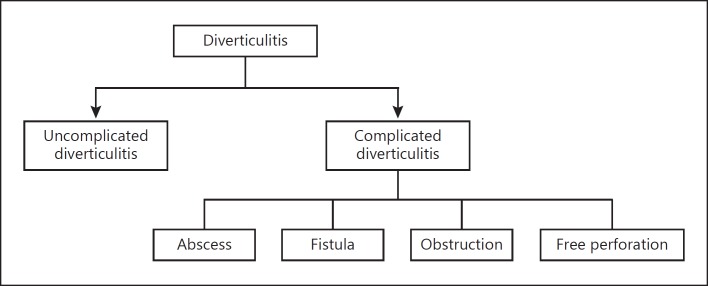
The pathogenesis of diverticulitis is unknown; however, it has been proposed that diverticulitis develops from obstruction of the neck of a diverticulum, leading to bacterial proliferation, local ischemia, and possible micro-perforation [14]. Anaerobic bacteria are the most common organisms identified, including Bacteroides, Peptostreptococcus, Clostridium, and Fusobacterium [14]. Gram-negative aerobes can also be cultured [15]. Complicated diverticulitis (Fig. 1) is defined as the presence of an overt abscess, fistula, stricture, bowel obstruction, or peritonitis with perforation [14]. Free perforation only occurs in 1–2% of patients who present for urgent evaluation [16]. Moreover, colonic obstruction is rare and occurs due to either acute inflammation from edema or abscess formation or stricture formation due to chronic scarring from repeated attacks of acute diverticulitis [16].
Fig. 1.
Classification of diverticulitis.
Demographics and Epidemiology
Diverticulitis was historically thought to be a disease of the elderly; however, the rates of diverticulitis have increased drastically in those younger than 40 years of age [17]. Furthermore, there is a male predominance in the young age group as compared to a female predominance in those greater than 65 years of age [18].
In the United States, acute diverticulitis ranks as the third most common inpatient gastrointestinal diagnosis and one of the most common gastrointestinal diagnoses in the outpatient setting and emergency department [19]. Acute diverticulitis costs about USD 2.6 billion dollars per year in inpatient costs [19].
Presentation
The classic presentation of acute diverticulitis is left lower quadrant abdominal pain, although the presenting symptoms can vary significantly and include abdominal fullness, fever, leukocytosis, change in bowel habit, nausea, vomiting, and urinary symptoms [1, 16]. Furthermore, patients may have right-sided disease (or a redundant sigmoid colon that can drape towards the right) and may present with dominantly right-sided symptoms.
Diagnosis
While in the right-sided clinical setting, it is reasonable and appropriate to diagnose acute diverticulitis empirically, computed tomography (CT) scanning has become the main test used for diagnosis and to assess severity of disease and/or the presence of complications [14, 20]. Colonoscopy is generally avoided in the acute setting due to risk of perforation or exacerbation of disease but, if indicated, is usually performed about 4–6 weeks after resolution of symptoms [14].
Staging
Staging is an important step in the classification of patients and subsequent determination of appropriate management. Several staging systems have been used, including Hinchey, Ambrosetti, and Neff [21, 22, 23].
The Hinchey classification (Table 1) categorizes colonic perforation in diverticular disease [21]. Stage 1 is defined as a small or confined pericolic abscess. Stage 2 is defined as a pelvic abscess. Stage 3 includes a localized perforation, and stage 4 is free perforation [21]. Mortality risk rises from < 5% in patients with stage 1 or 2 diverticulitis to 43% in patients with stage 4 diverticulitis [24].
Table 1.
Acute diverticulitis staging classification
| Stage | Hinchey | Neff | Ambrosetti |
|---|---|---|---|
| 0 | Diverticular wall thickening | ||
| 1 | Small or confined pericolic abscess | Localized pneumoperitoneum or local abscess | Uncomplicated acute diverticulitis |
| 2 | Pelvic abscess | Pelvic abscess | Complicated acute diverticulitis |
| 3 | Localized perforation | Distant abscess | Complicated chronic diverticulitis with fistula or stenosis |
| 4 | Free perforation | Other distant complications | |
Ambrosetti [22] proposed a revised CT classification in 2013 where he defined stage 1 as uncomplicated acute diverticulitis, stage 2 as complicated acute diverticulitis, and stage 3 as complicated chronic diverticulitis with either fistula or stenosis. He further concluded that imaging not only confirms the diagnosis but appropriately stages the severity of disease in order to best guide therapeutic interventions and assess the risk of recurrence [22].
The Neff classification is also based on CT findings [23]. Stage 0 is uncomplicated diverticulitis with CT findings of diverticular wall thickening with increased density of the pericolic fat. Stage 1 is locally complicated diverticulitis with CT findings of localized pneumoperitoneum or local abscess. Stage 2 is a complicated diverticulitis by pelvic abscess and stage 3 by a distant abscess. Lastly, stage 4 is a complicated diverticulitis with other distant complications. This staging classification system was used to successfully select patient populations that can be appropriately treated in the outpatient setting [23].
Management
The treatment of AUD has historically been assumed to include antibiotic treatment, with oral agents for outpatients with milder disease and intravenous administration for more severe episodes. Over the past decade, however, there has been an emerging proposal that perhaps the process was more inflammatory than infectious, as well as an appropriate emphasis on antibiotic restraint due to resistance issues. Randomized controlled trials (RCTs) of withholding antibiotics in defined populations of patients have begun to emerge, and will be reviewed below, but were favorable enough that the recent American Gastroenterological Association's guidelines on the management of acute diverticulitis overtly recommended selective, rather than routine, use of antibiotics in patients with AUD [1]. These RCTs also prompted a change in several European society guidelines. The Danish national guidelines suggested that there is no evidence for the obligate use of antibiotics in AUD, and, therefore, they should be used selectively “depending on the overall condition of the patient and the severity of the infection” [25]. A multidisciplinary working group from the Netherlands concluded in 2013 that there is no evidence for the routine use of antibiotics in patients with mild uncomplicated diverticulitis [26]. They recognized that due to the scarcity of evidence in the treatment of AUD, treatment is mainly guided by the surgeon's personal preference [26]. The Italian Consensus Conference on Diverticular Disease promoted by Gruppo Italiano Malattia Diverticolare (GRIMAD) stated that antibiotics may not improve outcomes in AUD and that they should be used on a “case-by-case” basis [27]. Lastly, the German Society for Gastroenterology, Digestive and Metabolic disease, and the German Society for General and Visceral surgery also recommended against the use of antibiotics in AUD without any risk factors, including immunosuppression [28].
The first RCT published from Sweden and Iceland in 2012 evaluated the necessity of antibiotic use in the recovery from AUD without complications within a 12-month interval [29]. They evaluated 623 patients with CT-proven left-sided AUD. Total duration of antibiotics in the treatment group was at least 7 days and antibiotics included an intravenous administration of a second- or third-generation cephalosporin and metronidazole or carbapenems or pipercillin-tazobactam. Overall rates of complication, including perforation and abscess formation, were low at 1.4%. They found no statistically significant differences between the antibiotic-treated patients (1%) and those not treated with antibiotics (1.9%). Furthermore, there were no differences in the frequency of surgery, length of hospital stay, recurrence of diverticulitis, abdominal pain, or changes in bowel habit. From these results, the authors concluded that, “antibiotic treatment of AUD does not prevent complications, accelerate recovery or prevent recurrence” [29].
The second RCT from the Netherlands evaluated 528 patients with CT-proven left-sided uncomplicated, acute diverticulitis, confirmed within 24 h [30]. Patients randomized to antibiotic treatments received 48 h of intravenous amoxicillin-clavulanic acid after which the route could be changed to oral for a total of 10 days of treatment. Patients were then followed up for 6 months to evaluate for complications. No differences were found between the observation and antibiotic treatment groups in terms of complicated diverticulitis, ongoing diverticulitis, recurrent diverticulitis, sigmoid resection, re-admission, adverse events, and mortality [30]. Importantly, hospital stay was actually significantly shorter in the observation group (2 days) than in the antibiotic treatment group (3 days) with a p = 0.006 [30]. The authors suggested that antibiotics could be eliminated in patients with a “first episode of uncomplicated, left-sided acute diverticulitis” [30].
Additionally, there is a large RCT from Spain that is underway, aiming to evaluate the safety and efficacy of nonantibiotic use in mild acute diverticulitis [31]. The results of this trial, when available, will aid in optimizing current guidelines in the management of AUD.
The above completed RCTs add further evidence to the data set supporting treatment without antibiotics in selected patients with AUD, suggesting that avoidance of antibiotics in AUD does not necessarily lead to more complications, more recurrences, or longer hospitalization stays. Ferrer et al. [32] evaluated a restrictive antibiotic outpatient treatment regimen for mild-to-moderate acute diverticulitis as classified by modified Neff staging. They found that about 88% of patients with mild to moderate AUD were successfully treated as outpatients without complications [32]. A large university hospital in Norway studied 244 patients with AUD of which 177 were treated without antibiotics [33]. They confirmed that management of AUD without antibiotics is safe as only 4% had treatment failure with only 1 fistula (< 1%) as a complication in these treatment failure patients [33]. Similar findings were seen by Mali et al. [34], who evaluated the efficacy of nonantibiotic treatment of AUD in a 30-day follow-up period. Their study found that of 161 patients, none developed complicated diverticulitis or required surgical intervention [34]. In addition, 87% were treated as outpatients and only 3% required inpatient hospital care [34]. This raises another important question in the care of AUD patients: whether outpatient treatment is safe, feasible, and efficacious, and several studies [23, 35, 36] suggest that the treatment of AUD can be safely done as an outpatient. Mizuki et al. [35] evaluated 70 patients with mild-to-moderate AUD. These patients were treated as outpatients with oral antibiotics for 10 days along with diet modification. Sixty-eight patients completed their treatment protocol without any complications [35]. Another large cohort of patients from the Kaiser Permanente Southern California region was evaluated for the effectiveness of outpatient management after the initial episode of diverticulitis. Etzioni et al. [36] studied 693 patients and found a 6% rate of treatment failure. They were able to analyze their cohort for predictors of outpatient treatment failure and found that patients with free air on initial CT scan were at highest risk for treatment failure [36]. Interestingly, age, white blood cell count, and duration of antibiotic therapy were not predictive of treatment failure [36].
Who Should Receive Antibiotic Therapy?
Despite the lack of evidence, there is likely to be agreement that certain patient populations with AUD should definitively receive antibiotics. Immunocompromised patients are a unique population in which AUD is associated with worse outcomes and high mortality due to the inability of these patients to mount an appropriate and effective immune response [37]. Therefore, pregnant patients, chronic kidney disease patients, collagen-vascular disease patients, those on chronic corticosteroid therapy, and septic patients should generally be treated with antibiotics when presenting with AUD [37, 38, 39]. For otherwise healthy patients, however, with a nontoxic presentation of AUD, antibiotic use should be selective [1, 40] and likely adjudicated with a conversation with the patient.
Conclusion
There has been a recent paradigm shift in the treatment of AUD with new evidence supporting nonantibiotic therapy regimens. A number of European guidelines, as well as the most recent American Gastroenterological Association Institute Guidelines on the Management of Acute Diverticulitis, advocate for the selective use of antibiotics, rather than routine use, in patients with AUD [40]. We have also suggested broad parameters in which to consider this conservative approach.
Disclosure Statement
The authors declare that they have no conflicts of interest.
Funding Sources
There are no funding sources for this article.
References
- 1.Strate LL, Peery AF, Neumann I. American Gastroenterological Association Institute Technical Review on the Management of Acute Diverticulitis. Gastroenterology. 2015;149:1950–1976. doi: 10.1053/j.gastro.2015.10.001. e12. [DOI] [PubMed] [Google Scholar]
- 2.Peery AF, Barrett PR, Park D, et al. A high-fiber diet does not protect against asymptomatic diverticulosis. Gastroenterology. 2012;142:266–272. doi: 10.1053/j.gastro.2011.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shahedi K, Fuller G, Bolus R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11:1609–1613. doi: 10.1016/j.cgh.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strate LL, Modi R, Cohen E, et al. Diverticular disease as a chronic illness: evolving epidemiologic and clinical insights. Am J Gastroenterol. 2012;107:1486–1493. doi: 10.1038/ajg.2012.194. [DOI] [PubMed] [Google Scholar]
- 5.Ambrosetti P, Chautems R, Soravia C, et al. Long-term outcome of mesocolic and pelvic diverticular abscesses of the left colon: a prospective study of 73 cases. Dis Colon Rectum. 2005;48:787–791. doi: 10.1007/s10350-004-0853-z. [DOI] [PubMed] [Google Scholar]
- 6.Hall JF, Roberts PL, Ricciardi R, et al. Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 2011;54:283–288. doi: 10.1007/DCR.0b013e3182028576. [DOI] [PubMed] [Google Scholar]
- 7.Eglinton T, Nguyen T, Raniga S, et al. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952–957. doi: 10.1002/bjs.7035. [DOI] [PubMed] [Google Scholar]
- 8.Anaya DA, Flum DR. Risk of emergency colectomy and colostomy in patients with diverticular disease. Arch Surg. 2005;140:681–685. doi: 10.1001/archsurg.140.7.681. [DOI] [PubMed] [Google Scholar]
- 9.Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576–583. doi: 10.1001/archsurg.140.6.576. [DOI] [PubMed] [Google Scholar]
- 10.Parks TG, Connell AM. The outcome in 455 patients admitted for treatment of diverticular disease of the colon. Br J Surg. 1970;57:775–778. doi: 10.1002/bjs.1800571021. [DOI] [PubMed] [Google Scholar]
- 11.Parks TG. Natural history of diverticular disease of the colon. A review of 521 cases. Br Med J. 1969;4:639–642. doi: 10.1136/bmj.4.5684.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munson KD, Hensien MA, Jacob LN, et al. Diverticulitis. A comprehensive follow-up. Dis Colon Rectum. 1996;39:318–322. doi: 10.1007/BF02049475. [DOI] [PubMed] [Google Scholar]
- 13.Isacson D, Andreasson K, Nikberg M, et al. No antibiotics in acute uncomplicated diverticulitis: does it work? Scand J Gastroenterol. 2014;49:1441–1446. doi: 10.3109/00365521.2014.968861. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057–2066. doi: 10.1056/NEJMcp073228. [DOI] [PubMed] [Google Scholar]
- 15.Brook I, Frazier EH. Aerobic and anaerobic microbiology in intra-abdominal infections associated with diverticulitis. J Med Microbiol. 2000;49:827–830. doi: 10.1099/0022-1317-49-9-827. [DOI] [PubMed] [Google Scholar]
- 16.Salem TA, Molloy RG, O'Dwyer PJ. Prospective study on the management of patients with complicated diverticular disease. Colorectal Dis. 2006;8:173–176. doi: 10.1111/j.1463-1318.2005.00865.x. [DOI] [PubMed] [Google Scholar]
- 17.Etzioni DA, Mack TM, Beart RW, Jr, et al. Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210–217. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 18.Kang JY, Hoare J, Tinto A, et al. Diverticular disease of the colon - on the rise: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003;17:1189–1195. doi: 10.1046/j.1365-2036.2003.01551.x. [DOI] [PubMed] [Google Scholar]
- 19.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187.e1–3. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ambrosetti P, Jenny A, Becker C, et al. Acute left colonic diverticulitis - compared performance of computed tomography and water-soluble contrast enema: prospective evaluation of 420 patients. Dis Colon Rectum. 2000;43:1363–1367. doi: 10.1007/BF02236631. [DOI] [PubMed] [Google Scholar]
- 21.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 22.Ambrosetti P. Acute left-sided colonic diverticulitis: clinical expressions, therapeutic insights, and role of computed tomography. Clin Exp Gastroenterol. 2016;9:249–257. doi: 10.2147/CEG.S110428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mora Lopez L, Serra Pla S, Serra-Aracil X, et al. Application of a modified Neff classification to patients with uncomplicated diverticulitis. Color Dis. 2013;15:1442–1447. doi: 10.1111/codi.12449. [DOI] [PubMed] [Google Scholar]
- 24.Schwesinger WH, Page CP, Gaskill HV III, et al. Operative management of diverticular emergencies: strategies and outcomes. Arch Surg. 2000;135:558–562. doi: 10.1001/archsurg.135.5.558. [DOI] [PubMed] [Google Scholar]
- 25.Andersen JC, Bundgaard L, Elbrond H, et al. Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59:C5543. [PubMed] [Google Scholar]
- 26.Andeweg CS, Mulder IM, Felt-Bersma RJ, et al. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg. 2013;30:278–292. doi: 10.1159/000354035. [DOI] [PubMed] [Google Scholar]
- 27.Cuomo R, Barbara G, Pace F, et al. Italian consensus conference for colonic diverticulosis and diverticular disease. United European Gastroenterol J. 2014;2:413–442. doi: 10.1177/2050640614547068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kruis W, Germer CT, Leifeld L, et al. Diverticular disease: guidelines of the German Society of Gastroenterology, Digestive and Metabolic Diseases and the German Society for General and Visceral Surgery. Digestion. 2014;90:190–207. doi: 10.1159/000367625. [DOI] [PubMed] [Google Scholar]
- 29.Chabok A, Pahlman L, Haapaniemi S, et al. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 2012;99:532–539. doi: 10.1002/bjs.8688. [DOI] [PubMed] [Google Scholar]
- 30.Daniels L, Ünlü C, de Korte N, et al. Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg. 2017;104:52–61. doi: 10.1002/bjs.10309. [DOI] [PubMed] [Google Scholar]
- 31.Mora Lopez L, Ruiz-Edo N, Serra Pla S, et al. Multicentre, controlled, randomized clinical trial to compare the efficacy and safety of ambulatory treatment of mild acute diverticulitis without antibiotics with the standard treatment with antibiotics. Int J Colorectal Dis. 2017;32:1509–1516. doi: 10.1007/s00384-017-2879-4. [DOI] [PubMed] [Google Scholar]
- 32.Ferrer EO, Ruiz EN, Hidalgo GLA, et al. Selective non-antibiotic treatment in sigmoid diverticulitis: is it time to change the traditional approach? Tech Coloproctol. 2016;20:309–315. doi: 10.1007/s10151-016-1464-0. [DOI] [PubMed] [Google Scholar]
- 33.Brochmann ND, Schultz JK, Jakobsen GS, Oresland T. Management of acute uncomplicated diverticulitis without antibiotics: a single-centre cohort study. Colorectal Dis. 2016;18:1101–1107. doi: 10.1111/codi.13355. [DOI] [PubMed] [Google Scholar]
- 34.Mali JP, Mentula PJ, Leppaniemi AK, Sallinen VJ. Symptomatic treatment for uncomplicated acute diverticulitis: a prospective cohort study. Dis Colon Rectum. 2016;59:529–534. doi: 10.1097/DCR.0000000000000579. [DOI] [PubMed] [Google Scholar]
- 35.Mizuki A, Nagata H, Tatemichi M, et al. The outpatient management of patients with acute mild-to-moderate colonic diverticulitis. Aliment Pharmacol. 2005;21:889–897. doi: 10.1111/j.1365-2036.2005.02422.x. [DOI] [PubMed] [Google Scholar]
- 36.Etzioni DA, Chiu VY, Cannom RR, et al. Outpatient treatment of acute diverticulitis: rates and predictors of failure. Dis Colon Rectum. 2010;53:861–865. doi: 10.1007/DCR.0b013e3181cdb243. [DOI] [PubMed] [Google Scholar]
- 37.Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284–294. doi: 10.1097/DCR.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 38.Peery AF, Stollman N. Antibiotics for acute uncomplicated diverticulitis: time for a paradigm change? Gastroenterology. 2015;149:1650–1651. doi: 10.1053/j.gastro.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klarenbeek BR, Samuels M, van der Wal MA, et al. Indications for elective sigmoid resection in diverticular disease. Ann Surg. 2010;251:670–674. doi: 10.1097/SLA.0b013e3181d3447d. [DOI] [PubMed] [Google Scholar]
- 40.Stollman N, Smalley W, Hirano I, et al. American Gastroenterological Association Institute Guideline on the Management of Acute Diverticulitis. Gastroenterology. 2015;149:1944–1949. doi: 10.1053/j.gastro.2015.10.003. [DOI] [PubMed] [Google Scholar]