Abstract
IMPORTANCE
Previous analyses of obesity trends among children and adolescents showed an increase between 1988–1994 and 1999–2000, but no change between 2003–2004 and 2011–2012, except for a significant decline among children aged 2 to 5 years.
OBJECTIVES
To provide estimates of obesity and extreme obesity prevalence for children and adolescents for 2011–2014 and investigate trends by age between 1988–1994 and 2013–2014.
DESIGN, SETTING, AND PARTICIPANTS
Children and adolescents aged 2 to 19 years with measured weight and height in the 1988–1994 through 2013–2014 National Health and Nutrition Examination Surveys.
EXPOSURES
Survey period.
MAIN OUTCOMES AND MEASURES
Obesity was defined as a body mass index (BMI) at or above the sex-specific 95th percentile on the US Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts. Extreme obesity was defined as a BMI at or above 120% of the sex-specific 95th percentile on the CDC BMI-for-age growth charts. Detailed estimates are presented for 2011–2014. The analyses of linear and quadratic trends in prevalence were conducted using 9 survey periods. Trend analyses between 2005–2006 and 2013–2014 also were conducted.
RESULTS
Measurements from 40 780 children and adolescents (mean age, 11.0 years; 48.8% female) between 1988–1994 and 2013–2014 were analyzed. Among children and adolescents aged 2 to 19 years, the prevalence of obesity in 2011–2014 was 17.0% (95% CI, 15.5%−18.6%) and extreme obesity was 5.8% (95% CI, 4.9%−6.8%). Among children aged 2 to 5 years, obesity increased from 7.2% (95% CI, 5.8%−8.8%) in 1988–1994 to 13.9% (95% CI,10.7%−17.7%) (P < .001) in 2003–2004 and then decreased to 9.4% (95% CI, 6.8%−12.6%)(P = .03) in 2013–2014. Among children aged 6 to 11 years, obesity increased from 11.3% (95% CI, 9.4%−13.4%) in 1988–1994 to 19.6% (95% CI, 17.1%−22.4%) (P < .001) in 2007–2008, and then did not change (2013–2014: 17.4% [95% CI, 13.8%−21.4%]; P = .44). Obesity increased among adolescents aged 12 to 19 years between 1988–1994 (10.5% [95% CI, 8.8%−12.5%]) and 2013–2014 (20.6% [95% CI, 16.2%−25.6%]; P < .001) as did extreme obesity among children aged 6 to 11 years (3.6% [95% CI, 2.5%−5.0%] in 1988–1994 to 4.3% [95% CI,3.0%−6.1%] in 2013–2014; P = .02) and adolescents aged 12 to 19 years (2.6% [95% CI,1.7%−3.9%] in 1988–1994 to 9.1% [95% CI, 7.0%−11.5%] in 2013–2014; P < .001). No significant trends were observed between 2005–2006 and 2013–2014 (P value range, .09-.87).
CONCLUSIONS AND RELEVANCE
In this nationally representative study of US children and adolescents aged 2 to 19 years, the prevalence of obesity in 2011–2014 was 17.0% and extreme obesity was 5.8%. Between 1988–1994 and 2013–2014, the prevalence of obesity increased until 2003–2004 and then decreased in children aged 2 to 5 years, increased until 2007–2008 and then leveled off in children aged 6 to 11 years, and increased among adolescents aged 12 to 19 years.
Obesity and extreme obesity in children and adolescents are associated with elevated blood pressure and abnormal fasting glucose1 and, long-term, often tracks into adulthood.2 In adults, obesity can result in increased morbidity and mortality.3,4 Obesity in children and adolescents is defined based on body mass index (BMI; calculated as weight in kilograms divided by height in meters squared).5 The most recent estimate for the prevalence of child and adolescent obesity in the United States is 17% and is based on data for 2011–2014.6
Many trend analyses have been published on obesity among children and adolescents based on different time periods. These include analyses of increasing trends between 1963–1965 and 1988–1994,7,8 1971–1975 and 1988–1994,9 1988–1994 and 1999–2000,10 1999–2000 and 2007–2008,11 1999–2000 and 2009–2010,12,13 and 1999–2000 and 2011–2012.14 Analyses of obesity trends in children and adolescents between 2003–2004 and 2011–201215 and between 1999–2000 and 2013–20146 showed an increase between 1999–2000 and 2013–2014 but no change between 2003–2004 and 2013–2014. Age-specific trend analyses of obesity prevalence between 2003–2004 and 2011–2012 showed no significant change in children aged 6 to 11 years or in adolescents aged 12 to 19 years, but a decrease in children aged 2 to 5 years.15 Trend analyses showing an increase in extreme obesity prevalence between 1999–2000 and 2011–2012 also have been published.14
Using data from the 2013–2014 National Health and Nutrition Examination Survey (NHANES), the purpose of this study was to investigate age-specific trends in the prevalence of obesity and extreme obesity in children and adolescents. Only some7–11,14,15 of the published analyses included age-specific trends and no analyses of total or age-specific trends have been analyzed for data between 1988–1994 and all the NHANES surveys since 1999–2000. To have sufficient power to fully investigate differences in trends by age and because no analyses of obesity or extreme obesity among children and adolescents have included trends from 1988–1994 to the present, this study focused on trends for that period. Detailed subgroup estimates for child and adolescent obesity and extreme obesity prevalence are also presented for 2011–2014.
Methods
Details about NHANES are available elsewhere.16 In brief, NHANES is a nationally representative, cross-sectional survey of the civilian, noninstitutionalized US population, with both interview and examination components.17 A complex probability sample, NHANES includes oversampling of certain subgroups. In 2013–2014, non-Hispanic black, non-Hispanic Asian, and Hispanic individuals, among other demographic groups, were oversampled. Beginning in 1999, NHANES has been continuously collecting data and releasing it publicly every 2 years. Prior to the continuous survey, 3 NHANES were conducted, including in 1988–1994 (NHANES III). The NHANES participants aged 18 years or older provided consent, children and adolescents aged 7 to 17 years provided documented assent, and parental permission was obtained for those younger than 18 years. NHANES was approved by the National Center for Health Statistics research ethics review board. In 2013–2014, 76% of children and adolescents aged 1 to 19 years selected for the survey participated in the examination component of the survey.18 Comparable numbers for this age group for 1988–1994, 1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, and 2011–2012 ranged between 77% and 87%.18
During the examination component of NHANES 2013–2014, standardized measurements of weight and height were obtained. Standardized measurement procedures were used between 1988 and 2014. Child and adolescent obesity was defined as a BMI at or above the sex-specific 95th percentile on the US Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts.19,20 Extreme obesity was defined as a BMI at or above 120% of the sex-specific 95th percentile on the CDC BMI-for-age growth charts.21,22
Demographic covariates included sex, age, race/Hispanic origin, and education level of the household head. Age was reported during the NHANES examination and was grouped as children aged 2 to 5 years and 6 to 11 years and adolescents aged 12 to 19 years. During the interview, participants or proxy respondents (such as parents) were asked to report race and Hispanic origin. Data on race/Hispanic origin were categorized as non-Hispanic white, non-Hispanic black, non-Hispanic Asian, Hispanic, and other for 2011–2014. For trend analyses, race and Hispanic origin was categorized as non-Hispanic white, non-Hispanic black, Mexican American, and other because reliable estimates for non-Hispanic Asian and Hispanic were not possible across all the survey periods. Individuals reporting multiple races were categorized as other and were included in the analyses of the entire population but not shown separately. Education level of the household head was categorized as less than a high school degree, a high school degree (including those who received a general equivalency diploma), and greater than a high school degree.
Estimates of prevalence and 95% confidence intervals were examined by sex, age group, race/Hispanic origin, and education level of the household head using data from NHANES 2011–2014 (4 years of data). Combining 2 cycles of NHANES data increases the efficiency of the prevalence estimates by increasing the sample size. Demographic differences in obesity and extreme obesity among US children and adolescents for 2011–2014 were tested using logistic regression models.
The 2-year cycles of NHANES were used for trend tests of obesity and extreme obesity to increase the number of time points. Analyses of both unadjusted and adjusted trends in obesity and extreme obesity prevalence were conducted using the following periods: 1988–1994, 1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012, and 2013–2014.
Overall and age-specific trends in obesity and extreme obesity prevalence among children and adolescents aged 2 to 19 years were conducted. Unadjusted trends as well as trends adjusted for sex, race/Hispanic origin, and education level of the household head were tested using logistic regression models in which the survey period was treated as a continuous variable using the midpoint of the period as the time point. Linear trends were tested separately and quadratic trends were tested with both linear and quadratic terms included in the models. If the quadratic term was significant in the model that contained the linear term, then the model with the quadratic term was the better fit. If a quadratic trend was found, Joinpoint software was used to find the inflection point and differences in slopes between the 2 segments were tested using piecewise linear regression.23 Unadjusted linear trend analyses during the most recent decade (2005–2006 to 2013–2014) also were conducted. Significance was assessed using the Satterthwaite-adjusted F test.24
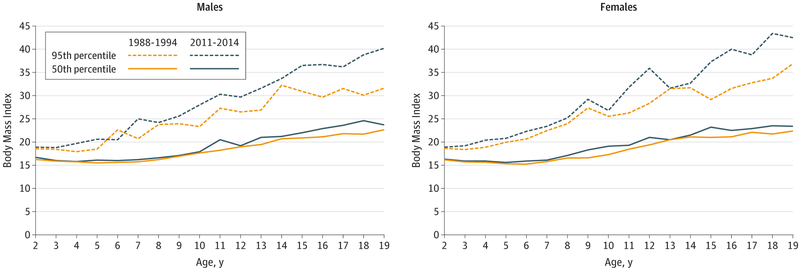
To characterize the shift in the distribution of BMI over time, the internal sex-and age-specific values of the 50th and 95th percentiles of BMI are presented for 1988–1994 and 2011–2014. Because BMI varies with age in children and adolescents, percentiles are presented by single year of age. Percentiles are shown graphically for males and females.
All estimated prevalences, standard errors, and percentiles were based on weighted data. The NHANES examination sample weights adjusted for oversampling, nonresponse, and noncoverage. Standard errors were estimated using Taylor series linearization.25 The complex sample design was incorporated in the standard error estimates and all statistical testing. Confidence intervals were constructed using the approach described by Korn and Graubard.26 In testing for differences or trends, a 2-sided P value of .05 was used to assess statistical significance. No adjustments were made for multiple comparisons. Analyses were conducted using SAS version 9.3 (SAS Institute Inc), SUDAAN version 11.0 (RTI International), and Joinpoint version 3.0.1 (National Cancer Institute).
Results
Obesity Prevalence in 2011–2014
Among children and adolescents aged 2 to 19 years in 2011–2014, 139 of 7017 (2%) were missing values for weight, height, or both and were not included in the analysis. Of these 139 children and adolescents, 18 (13%) were pregnant. The un-weighted sample sizes in 2011–2014 appear in Table 1 by sex, age, and race/Hispanic origin. In the analyses that included education level of the household head, an additional 224 (3%) children and adolescents were excluded due to missing data.
Table 1.
Unweighted Sample Sizes for Children and Adolescents Aged 2 to 19 Years by Sex, Age Group, and Race/Hispanic Origin: NHANES 2011–2014
| No. of Participants by Race/Hispanic Origin | |||||
|---|---|---|---|---|---|
| Age Group, y |
All Groupsa |
Non-Hispanic | Hispanic | ||
| White | Black | Asian | |||
| All participants | |||||
| 2–19 | 6878 | 1647 | 1910 | 728 | 2178 |
| 2–5 | 1714 | 390 | 485 | 175 | 547 |
| 6–11 | 2562 | 638 | 714 | 236 | 810 |
| 12–19 | 2602 | 619 | 711 | 317 | 821 |
| Males | |||||
| 2–19 | 3507 | 865 | 986 | 358 | 1094 |
| 2–5 | 867 | 188 | 260 | 83 | 279 |
| 6–11 | 1315 | 340 | 361 | 119 | 417 |
| 12–19 | 1325 | 337 | 365 | 156 | 398 |
| Females | |||||
| 2–19 | 3371 | 782 | 924 | 370 | 1084 |
| 2–5 | 847 | 202 | 225 | 92 | 268 |
| 6–11 | 1247 | 298 | 353 | 117 | 393 |
| 12–19 | 1277 | 282 | 346 | 161 | 423 |
Abbreviation: NHANES, National Health and Nutrition Examination Surveys.
Includes race/Hispanic origin groups not shown separately.
Weighted estimates of obesity and extreme obesity prevalence appear in Table 2 by sex, age, and race/Hispanic origin in 2011–2014. Among children and adolescents aged 2 to 19 years, the prevalence of obesity in 2011–2014 was 17.0%6 (95% CI, 15.5%−18.6%) and extreme obesity was 5.8% (95% CI, 4.9%−6.8%). Among children aged 2 to 5 years, the prevalence of obesity was 8.9% (95% CI, 7.1%−11.0%), it was 17.5% (95% CI, 15.2%−20.1%) among children aged 6 to 11 years, and it was 20.5% (95% CI, 17.8%−23.5%) among adolescents aged 12 to 19 years. Estimates of obesity and extreme obesity by age group and education level of the household head appear in eTable 1 in the Supplement.
Table 2.
Weighted Prevalence of Obesity and Extreme Obesity in US Children and Adolescents Aged 2 to 19 Years by Sex, Age, and Race/Hispanic Origin: NHANES 2011–2014
| Weighted Prevalence by Age Group, % (95% CI) | ||||
|---|---|---|---|---|
| 2–19 y | 2–5 y | 6–11 y | 12–19y | |
| Obesity (BMI at or above the sex-specific 95th percentile on the CDC BMI-for-age growth charts) | ||||
| All race/Hispanic origin groupsa | ||||
| Both sexes | 17.0 (15.5–18.6) | 8.9 (7.1–11.0) | 17.5 (15.2–20.1) | 20.5 (17.8–23.5) |
| Males | 16.9 (15.1–19.0) | 9.2 (6.5–12.4) | 17.6 (14.6–20.9) | 20.1 (16.8–23.6) |
| Females | 17.1 (15.1–19.3) | 8.6 (6.2–11.6) | 17.5 (14.9–20.3) | 21.0 (17.3–25.2) |
| Non-Hispanic white | ||||
| Both sexes | 14.7 (12.3–17.3) | 5.2 (3.1–8.3) | 13.6 (9.8–18.3) | 19.6 (14.7–25.3) |
| Males | 14.3 (11.2–17.9) | 6.1 (2.6–12.0)b | 13.0 (9.0–17.9) | 18.7 (13.0–25.7) |
| Females | 15.1 (11.7–19.1) | 4.4 (2.0–8.2) | 14.4 (9.3–20.9) | 20.4 (13.6–28.8) |
| Non-Hispanic black | ||||
| Both sexes | 19.5 (17.1–22.2) | 10.4 (7.5–14.0) | 21.4 (17.5–25.8) | 22.6 (18.0–27.8) |
| Males | 18.4 (16.1–21.0) | 9.0 (4.8–14.9) | 21.2 (16.6–26.5) | 20.9 (16.4–25.9) |
| Females | 20.7 (17.1–24.6) | 11.9 (8.0–16.8) | 21.6 (16.8–27.0) | 24.4 (18.4–31.3) |
| Non-Hispanic Asian | ||||
| Both sexes | 8.6 (6.4–11.2) | 5.0 (1.6–11.3)b,c | 9.8 (6.1–14.9) | 9.4 (6.4–13.2) |
| Males | 11.8 (8.3–16.1) | 4.8 (0.7–15.2)b,c | 14.7 (7.9–24.1) | 12.9 (8.0–19.1) |
| Females | 5.3 (2.9–8.6) | 5.1 (0.9–15.3)b,c | 4.7 (1.6–10.2)b,c | 5.7 (2.7–10.5) |
| Hispanic | ||||
| Both sexes | 21.9 (20.0–23.9) | 15.6 (12.5–19.2) | 25.0 (22.0–28.1) | 22.8 (19.5–26.3) |
| Males | 22.4 (19.9–24.9) | 16.7 (12.0–22.2) | 25.8 (20.7–31.4) | 22.7 (18.7–27.1) |
| Females | 21.4 (18.8–24.1) | 14.6 (9.4–21.2) | 24.1 (19.9–28.7) | 22.8 (18.5–27.7) |
| Extreme obesity (BMI at or above 120% of the sex-specific 95th percentile on the CDC BMI-for-age growth charts) | ||||
| All race/Hispanic origin groupsa | ||||
| Both sexes | 5.8 (4.9–6.8) | 1.7 (1.0–2.7) | 5.6 (4.5–6.9) | 7.8 (6.3–9.6) |
| Males | 5.7 (4.7–6.9) | 1.3 (0.7–2.3) | 5.8 (4.2–7.7) | 7.7 (5.9–9.8) |
| Females | 5.9 (4.7–7.3) | 2.1 (1.0–3.9)b | 5.5 (4.3–6.9) | 8.0 (5.8–10.7) |
| Non-Hispanic white | ||||
| Both sexes | 4.4 (3.2–6.0) | 1.0 (0.2–2.9)b,c | 3.4 (1.6–6.4)b | 6.7 (4.6–9.2) |
| Males | 3.9 (2.5–5.9) | 0.3 (0–2.5)b,c | 3.4 (1.2–7.2)b | 5.9 (3.7–9.0) |
| Females | 5.0 (3.3–7.2) | 1.8 (0.3–5.7)b,c | 3.4 (1.7–6.2) | 7.4 (4.1–12.3) |
| Non-Hispanic black | ||||
| Both sexes | 8.6 (6.8–10.8) | 2.1 (0.7–4.8)b,c | 8.8 (6.5–11.6) | 11.6 (8.5–15.4) |
| Males | 8.4 (6.6–10.4) | 1.9 (0.4–5.5)b,c | 9.3 (5.8–14.1) | 10.7 (7.7–14.3) |
| Females | 8.9 (6.3–12.1) | 2.2 (0.6–5.9)b,c | 8.2 (5.4–11.9) | 12.7 (8.1–18.5) |
| Non-Hispanic Asian | ||||
| Both sexes | 1.3 (0.5–2.8)b | 0.50 (0.01–3.04)b,c | 1.0 (0.2–3.3)b,c | 2.0 (0.6–4.5)b,c |
| Males | 2.2 (0.8–4.7)b,c | 0.99 (0.01–6.18)b,c | 1.4 (0.1–5.8)b,c | 3.3 (0.9–8.6)b,c |
| Females | 0.43 (0.04–1.77)b,c | 0d | 0.6 (0–4.2)b,c | 0.52 (0.01–3.23)b,c |
| Hispanic | ||||
| Both sexes | 7.6 (6.3–9.2) | 3.0 (1.3–5.6)b | 9.3 (7.4–11.5) | 8.8 (6.8–11.2) |
| Males | 8.0 (6.0–10.3) | 3.2 (1.5–6.0)b,c | 9.6 (6.8–13.1) | 9.2 (6.2–13.1) |
| Females | 7.3 (5.4–9.5) | 2.7 (0.6–7.5)b,c | 8.9 (6.3–12.2) | 8.3 (5.7–11.7) |
Abbreviations: BMI, body mass index; CDC, Centers for Disease Control and Prevention; NHANES, National Health and Nutrition Examination Surveys.
Includes race/Hispanic origin groups not shown separately.
The relative standard errors are greater than 30%.
The number of cases is less than 10.
The 95% confidence interval cannot be calculated because the number of cases is 0.
In 2011–2014, there were significant differences in obesity and extreme obesity prevalence by age, race/Hispanic origin, and education level of household head. The odds ratios (ORs) from logistic regression models containing all 4 demographic covariates appear in eTable 2 in the Supplement. The odds of obesity were significantly higher among children aged 6 to 11 years (17.5% [95% CI, 15.2%−20.1%]; OR, 2.29 [95% CI,1.73–3.03]) and adolescents aged 12 to 19 years (20.5% [95% CI,17.8%−23.5%]; OR, 2.82 [95% CI, 2.08–3.84]) compared with children aged 2 to 5 years (8.9%; 95% CI, 7.1%−11.0%). The odds of obesity also were higher among non-Hispanic black children and adolescents (19.5% [95% CI, 17.1%−22.2%]; OR, 1.34 [95% CI, 1.03–1.75]) and Hispanic children and adolescents(21.9% [95% CI, 20.0%−23.9%]; OR, 1.48 [95% CI, 1.23–1.78]) compared with non-Hispanic white children and adolescents(14.7%; 95% CI, 12.3%−17.3%).
In contrast, the odds for obesity were lower for non-Hispanic Asian children and adolescents (8.6% [95% CI, 6.4%−11.2%]; OR, 0.57 [95% CI, 0.39–0.82]) compared with non-Hispanic white children and adolescents. The odds of obesity were higher among children and adolescents in households headed by individuals with less than a high school degree (21.0% [95% CI, 18.5%−23.8%]; OR, 1.41 [95% CI, 1.13–1.75]) or a high school degree (22.2% [95% CI, 19.1%−25.5%]; OR, 1.61 [95% CI, 1.27–2.04]) compared with those in households in which the household head had greater than a high school degree (14.1%; 95% CI, 12.0%−16.4%). Findings were the same in relation to extreme obesity.
Trend Analyses
Among the 3598 children and adolescents aged 2 to 19 years in 2013–2014, 75 (2%) were missing values of weight, height, or both and were not included in the analysis. Of these 75 children and adolescents, 10 (13%) were pregnant. Analyses that included education level of the household head excluded an additional 93 children and adolescents (3%) due to missing data. Measurements from 40 780 children and adolescents (mean age, 11.0 years; 48.8% female) between 1988–1994 and 2013–2014 were analyzed.
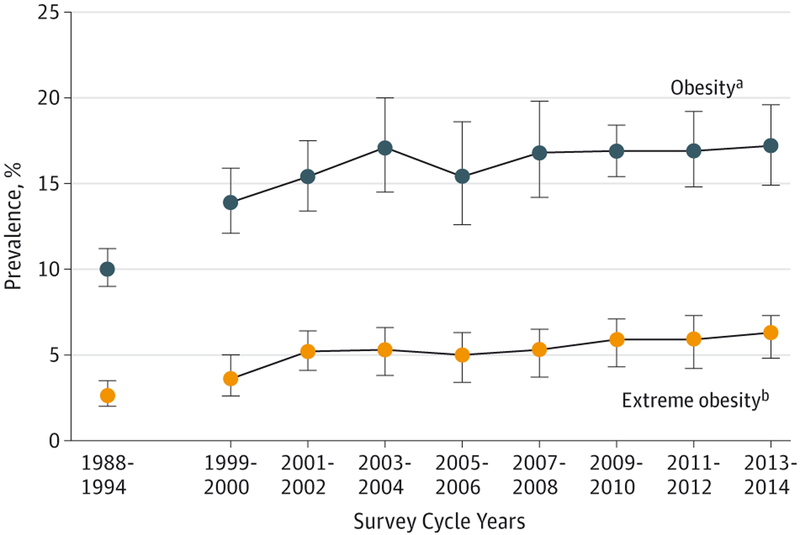
Unadjusted trends in prevalence of obesity and extreme obesity appear in Figure 1 (children and adolescents aged 2–19 years) and by age group in Table 3 and in eFigures 1 and 2 in the Supplement. Among children and adolescents aged 2 to 19 years, there was a significant quadratic trend in obesity (P = .004) suggesting a change in slope (Figure 1 and Table 3) between 1988–1994 and 2013–2014. The Joinpoint analysis and piecewise regression analysis found an inflection point at 2003–2004 and a significant difference (P = .01) in slopes before and after this period. Obesity increased until 2003–2004 (slope, 0.51 [95% CI, 0.35 to 0.67]; P < .001) and did not change after that period (slope, 0.08 [95% CI, −0.15 to 0.30]; P = .49). The prevalence of extreme obesity increased between 1988–1994 and 2013–2014 (linear P < .001). In the models adjusted for sex, age, race/Hispanic origin, and education level of the household head, results related to obesity and extreme obesity did not change (eTable 3 in the Supplement).
Figure 1.
Prevalence of Obesity and Extreme Obesity in US Children and Adolescents Aged 2 to 19 Years From 1988–1994 Through 2013–2014
Data are from the National Health and Nutrition Examination Surveys. The error bars indicate 95% confidence intervals. The prevalence estimates are weighted.
a Defined as at or above the sex-specific 95th percentile on the US Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts.
b Defined as at or above 120% of the sex-specific 95th percentile on the CDC BMI-for-age growth charts.
Table 3.
Age-Specific Trends in Obesity and Extreme Obesity Prevalence in US Children and Adolescents for 1988–1994 Through 2013–2014a
| Ages 2–19 y | Ages 2–5 y | Ages 6–11 y | Ages 12–19 y | |||||
|---|---|---|---|---|---|---|---|---|
| Survey Year | Unweighted Sample Size |
Weighted Prevalence, % (95% CI) |
Unweighted Sample Size |
Weighted Prevalence, % (95% CI) |
Unweighted Sample Size |
Weighted Prevalence, % (95% CI) |
Unweighted Sample Size |
Weighted Prevalence, % (95% CI) |
| Obesity (BMI at or above the sex-specific 95th percentile on the CDC BMI-for-age growth charts) | ||||||||
| 1988–1994 | 10 777 | 10.0 (9.0–11.2) | 4373 | 7.2 (5.8–8.8) | 3279 | 11.3 (9.4–13.4) | 3125 | 10.5 (8.8–12.5) |
| 1999–2000 | 4039 | 13.9 (12.1–15.9) | 726 | 10.3 (7.0–14.6) | 1048 | 15.1 (12.2–18.3) | 2265 | 14.8 (12.9–16.9) |
| 2001–2002 | 4261 | 15.4(13.4–17.5) | 795 | 10.6 (7.0–15.1) | 1165 | 16.2 (12.9–20.1) | 2301 | 16.7 (14.3–19.2) |
| 2003–2004 | 3961 | 17.1 (14.5–20.0) | 819 | 13.9 (10.7–17.7) | 982 | 18.8 (16.1–21.7) | 2160 | 17.4 (13.9–21.3) |
| 2005–2006 | 4207 | 15.4 (12.6–18.6) | 952 | 10.7 (8.4–13.3) | 1114 | 15.1 (11.0–20.1) | 2141 | 17.8 (14.0–22.0) |
| 2007–2008 | 3249 | 16.8 (14.2–19.8) | 853 | 10.1 (7.7–12.9) | 1197 | 19.6 (17.1–22.4) | 1199 | 18.1 (14.6–22.0) |
| 2009–2010 | 3408 | 16.9 (15.4–18.4) | 903 | 12.1 (9.8–14.8) | 1213 | 18.0 (15.9–20.3) | 1292 | 18.4 (15.7–21.3) |
| 2011–2012 | 3355 | 16.9 (14.8–19.2) | 871 | 8.4 (5.8–11.7) | 1268 | 17.7 (14.4–21.5) | 1216 | 20.5 (16.9–24.4) |
| 2013–2014 | 3523 | 17.2 (14.9–19.6) | 843 | 9.4 (6.8–12.6) | 1294 | 17.4 (13.8–21.4) | 1386 | 20.6 (16.2–25.6) |
| P value for trend | ||||||||
| Linear | <.001 | .29 | <.001 | <.001 | ||||
| Quadratic | .004 | .001 | .03 | .25 | ||||
| Extreme obesity (BMI at or above 120% of the sex-specific 95th percentile on the CDC BMI-for-age growth charts) | ||||||||
| 1988–1994 | 10 777 | 2.6 (2.0–3.5) | 4373 | 1.3 (0.6–2.5)b | 3279 | 3.6 (2.5–5.0) | 3125 | 2.6 (1.7–3.9) |
| 1999–2000 | 4039 | 3.6 (2.6–5.0) | 726 | 1.7 (0.6–3.8)b | 1048 | 3.1 (1.8–5.0) | 2265 | 5.0 (3.5–6.9) |
| 2001–2002 | 4261 | 5.2 (4.1–6.4) | 795 | 2.7 (0.9–6.0)b | 1165 | 6.2 (4.4–8.6) | 2301 | 5.4 (4.1–6.9) |
| 2003–2004 | 3961 | 5.1 (3.8–6.6) | 819 | 2.8 (1.5–4.8) | 982 | 5.3 (4.0–6.9) | 2160 | 5.9 (4.1–8.2) |
| 2005–2006 | 4207 | 4.7 (3.4–6.3) | 952 | 1.5 (0.7–2.9)b | 1114 | 3.9 (2.6–5.6) | 2141 | 6.7 (4.8–9.0) |
| 2007–2008 | 3249 | 4.9 (3.7–6.5) | 853 | 1.8 (0.6–3.9)b | 1197 | 5.7 (4.3–7.5) | 1199 | 5.9 (3.9–8.6) |
| 2009–2010 | 3408 | 5.6 (4.3–7.1) | 903 | 2.7 (1.6–4.1) | 1213 | 5.1 (3.7–6.8) | 1292 | 7.4 (4.8–10.8) |
| 2011–2012 | 3355 | 5.6 (4.2–7.3) | 871 | 1.6 (0.7–3.2)b | 1268 | 6.9 (5.2–8.9) | 1216 | 6.6 (4.4–9.5) |
| 2013–2014 | 3523 | 6.0(4.8–7.3) | 843 | 1.7 (0.8–3.3)b | 1294 | 4.3 (3.0–6.1) | 1386 | 9.1 (7.0–11.5) |
| P value for trend | ||||||||
| Linear | <.001 | .59 | .02 | <.001 | ||||
| Quadratic | .17 | .16 | .35 | .37 | ||||
Abbreviations: BMI, body mass index; CDC, Centers for Disease Control and Prevention.
Data are from the National Health and Nutrition Examination Surveys. P values are from logistic regression models.
Relative standard errors are greater than 30% but less than 40%.
There was a significant quadratic trend in obesity prevalence between 1988–1994 and 2013–2014 among children aged 2 to 5 years (P = .001) (Table 3). The Joinpoint analysis and the piecewise regression analysis found an inflection point in 2003–2004 and a significant difference (P < .001) in the slope before and after this period. The prevalence of obesity increased until 2003–2004 (slope, 0.42 [95% CI, 0.23 to 0.62], P < .001) and then decreased (slope, −0.33 [95% CI, −0.63 to −0.04]; P = .03). There was no change in extreme obesity prevalence in this age group between 1988–1994 and 2013–2014 (P = .59). The results related to obesity and extreme obesity did not change in the models adjusted for sex, race/Hispanic origin, and education level of the household head (eTable 3 in the Supplement).
There was a significant quadratic trend in obesity among children aged 6 to 11 years (P = .03; Table 3). The Joinpoint analysis identified a potential inflection point at 2007–2008; however, the piecewise regression analysis did not find a significant difference (P = .06) in slope before and after this period. The prevalence of obesity increased between 1988–1994 and 2007–2008 (slope, 0.44 [95% CI, 0.26 to 0.61]; P < .001) but did not change after that period (slope, −0.23 [95% CI, −0.82 to 0.36]; P = .44). Extreme obesity increased between 1988–1994 and 2013–2014 (linear P = .02). The results related to obesity and extreme obesity did not change in the models adjusted for sex, race/Hispanic origin, and education level of the household head (eTable 3 in the Supplement).
Among adolescents, there was a significant increasing linear trend for both obesity (P < .001) and extreme obesity (P < .001), but no quadratic trends between 1988–1994 and 2013–2014 (Table 3). The results related to obesity and extreme obesity did not change in the models adjusted for sex, race/Hispanic origin, and education level of the household head (eTable 3 in the Supplement).
No unadjusted or adjusted linear trends in obesity or extreme obesity prevalence during the last decade (2005–2006 through 2013–2014) were significant for any age group (eTable 4 in the Supplement).
The sex-and age-specific values of the 50th and 95th percentiles of BMI in 1988–1994 and 2011–2014 appear in Figure 2. For example, in 1988–1994, the 95th percentile of BMI among 17-year-old males was 31.5 (ie, 5% of males had a BMI >31.5), and in 2011–2014 the 95th percentile was 36.2 (ie, 5% of males had a BMI >36.2). Change over time in the 95th percentile for both males and females increased with age. Among males, the 95th percentiles of BMI in 1988–1994 were generally lower than in 2011–2014. Among females, there was little difference between the 95th percentiles in 1988–1994 and 2011–2014 until they reached the age of 10 years (BMI unit range, 0.3–1.8) compared with the ages of 11 to 19 years during which the majority of values in 1988–1994 compared with 2011–2014 were 5.5 or more BMI units lower. In contrast, little change can be seen in the 50th percentiles of BMI over time, illustrating the increased skewness of the BMI distribution among older children and adolescents.
Figure 2.
Weighted Estimates for US Children and Adolescents Aged 2 to 19 Years in the 50th and 95th Percentiles of Body Mass Index From 1988–1994 and 2011–2014
Data are from the National Health and Nutrition Examination Surveys.
Discussion
Trends in child and adolescent obesity varied by age. During an approximately 25-year period (1988–1994 through 2013–2014), the prevalence increased until 2003–2004 but then decreased among children aged 2 to 5 years. Among children aged 6 to 11 years, the prevalence increased until 2007–2008 and then leveled off. Among adolescents aged 12 to 19 years, obesity prevalence increased between 1988–1994 and 2013–2014. Trends in extreme obesity prevalence showed no change between 1988–1994 and 2013–2014 among children aged 2 to 5 years, whereas it increased among children aged 6 to 11 years and among adolescents aged 12 to 19 years. No significant changes in either obesity or extreme obesity were seen between 2005–2006 and 2013–2014, suggesting any recent changes among adolescents were small.
Other research conducted in the United States has shown declines in obesity prevalence among children aged 2 to 5 years. Data on low-income preschool-aged children who participate in federal nutrition programs,27 clinical data on children who participate in Kaiser Permanente in southern California,28 and children in a health maintenance organization in Boston, Massachusetts29 have also shown small decreases in obesity prevalence among preschool-aged children.
Studies of trends in obesity prevalence among US adolescents have shown inconsistent results. Results based on the Youth Risk Behavioral Surveillance System (YRBS) found a significant linear increase in obesity prevalence based on self-reported weight and height between 1999 and 2013.30 Similar to the results from YRBS, NHANES showed an increase in prevalence among adolescents between 1999 and 2012,14 but no significant changes were found in this study between 2005–2006 and 2013–2014. On the other hand, data from electronic health records in southern California showed a significant decline (4.5%) in obesity prevalence between 2008 and 2013 among adolescents.28
Studies conducted in children and adolescents suggest that those with very high BMIs (based on varying definitions) are at a higher risk for elevated blood pressure, abnormal glucose, and abnormal lipids.22,31,32 In addition, research has shown low health-related quality-of-life levels in children and adolescents with extreme obesity33 and weight-based victimization in children and adolescents with obesity.34
Body mass index is an imperfect measure of body fat and health risk. There are racial and ethnic differences in body fat at the same BMI level.35,36 Among children and adolescents, the definition of obesity is statistical.19 Children and adolescents are compared with a group of US children in the 1960s to early 1990s, so the prevalence of obesity is dependent on the characteristics of the age-specific population during that period. In addition, among young children, small changes in weight can lead to relatively large changes in BMI percentile.
Strengths and Limitations
A strength of NHANES is that weight and height are measured rather than reported. Research has shown that adolescents and adults underreport weight and overreport height, which leads to biased (lower) BMI values.37 Parental report of weight and height can result in underreporting of height, which results in biased (higher) BMI values.38 NHANES measurements are standardized over time and transferred directly from the scale and stadiometer into the database, reducing the potential for recording errors.
Study limitations also need to be considered. NHANES sample sizes for some demographic subgroups, as well as the number of primary sampling units, are small. Although NHANES is released every 2 years and the estimates based on those 2 years are nationally representative, the NHANES survey design is based on 4 years of data collection.16 Combining multiple survey cycles is recommended for many analyses, such as estimates of conditions with low prevalence (<5%).39 Estimates based on 4 years of data have a greater number of degrees of freedom, larger sample sizes (denominators), and greater numbers of cases (numerator), and are therefore more stable than the estimates based on 2 years of data, particularly when examining subgroups. For example, the sample size was 31 with only 4 degrees of freedom for non-Hispanic Asian females aged 2 to 5 years with measured weight and height and fewer than 10 obese persons in 2013–2014 compared with a sample size of 92 with 15 degrees of freedom for this subgroup using 4 years of data from 2011–2014. Even with combined data, there were still subgroups in which the number of cases was less than 10, especially for extreme obesity. As a result, detailed estimates of obesity by subgroup were based on 4 years of NHANES data, similar to a recent publication.6
The current analysis contains multiple statistical significance tests to determine the trends and differences. Multiple statistical tests can result in some outcomes being statistically significant merely by chance. Consequently, the results presented should be interpreted with this in mind.
Conclusions
In this nationally representative study of US children and adolescents aged 2 to 19 years, the prevalence of obesity in 2011–2014 was 17.0% and extreme obesity was 5.8%. Between 1988–1994 and 2013–2014, the prevalence of obesity increased until 2003–2004 and then decreased in children aged 2 to 5 years, increased until 2007–2008 and then leveled off in children aged 6 to 11 years, and increased among adolescents aged 12 to 19 years.
Supplementary Material
Footnotes
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: The findings and conclusions reported in this article are those of the authors and not necessarily those of the US Centers for Disease Control and Prevention (CDC).
Additional Information: The National Center for Health Statistics and the CDC had a role in the design and conduct of the National Health and Nutrition Examination Surveys and in the collection and management of the data; however, the National Center for Health Statistics and the CDC had no role in the analysis and interpretation of the data; in the preparation of the manuscript; or in the decision to submit the manuscript for publication.
REFERENCES
- 1.Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192. [DOI] [PubMed] [Google Scholar]
- 2.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res. 1998;6(suppl 2):51S–209S. [PubMed] [Google Scholar]
- 5.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(suppl 4):S193–S228. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015; 219(219):1–8. [PubMed] [Google Scholar]
- 7.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101(3 pt 2):497–504. [PubMed] [Google Scholar]
- 8.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents: the National Health and Nutrition Examination Surveys, 1963 to 1991. Arch Pediatr Adolesc Med. 1995;149(10):1085–1091. [DOI] [PubMed] [Google Scholar]
- 9.Ogden CL, Troiano RP, Briefel RR, Kuczmarski RJ, Flegal KM, Johnson CL. Prevalence of overweight among preschool children in the United States, 1971 through 1994. Pediatrics. 1997;99(4):E1. [DOI] [PubMed] [Google Scholar]
- 10.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288(14):1728–1732. [DOI] [PubMed] [Google Scholar]
- 11.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. [DOI] [PubMed] [Google Scholar]
- 12.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012;(82):1–8. [PubMed] [Google Scholar]
- 14.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr. 2014;168(6):561–566. [DOI] [PubMed] [Google Scholar]
- 15.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: sample design, 2011–2014. Vital Health Stat 2. 2014;162(162):1–33. [PubMed] [Google Scholar]
- 17.CDC National Center for Health Statistics. National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation. http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed May 6, 2016.
- 18.CDC National Center for Health Statistics. National Health and Nutrition Examination Survey: response rates and population totals. http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm. Accessed May 6, 2016.
- 19.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 2010;(25):1–5. [PubMed] [Google Scholar]
- 20.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;246(246):1–190. [PubMed] [Google Scholar]
- 21.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(5):1314–1320. [DOI] [PubMed] [Google Scholar]
- 22.Kelly AS, Barlow SE, Rao G, et al. ; American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young, Council on Nutrition, Physical Activity and Metabolism, and Council on Clinical Cardiology. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–1712. [DOI] [PubMed] [Google Scholar]
- 23.Neter J, Wasserman W, Kutner MH. Applied Linear Statistical Models. 2nd ed. Hinsdale, IL: Irwin; 1985. [Google Scholar]
- 24.Skinner CJ, Holt D, Smith TMF. Analysis of Complex Surveys. Chichester, England: John Wiley & Sons; 1989. [Google Scholar]
- 25.Wolters KM. Introduction to Variance Estimation. New York, NY: Springer-Verlag; 1982. [Google Scholar]
- 26.Korn EL, Graubard BI. Confidence intervals for proportions with small expected number of positive counts estimated from survey data. Survey Methodology. 1998;23:193–201. [Google Scholar]
- 27.Centers for Disease Control and Prevention. Vital signs: obesity among low-income, preschool-aged children—United States, 2008–2011. MMWR Morbid Mortal Weekly Rep. 2013;62(31):629–634. [PMC free article] [PubMed] [Google Scholar]
- 28.Koebnick C, Mohan YD, Li X, Young DR. Secular trends of overweight and obesity in young southern Californians 2008–2013. J Pediatr. 2015;167(6):1264–1271.e2, e1262. [DOI] [PubMed] [Google Scholar]
- 29.Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012;129(5):823–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kann L, Kinchen S, Shanklin SL, et al. ; Centers for Disease Control and Prevention (CDC). Youth risk behavior surveillance—United States, 2013. MMWR Suppl. 2014;63(4):1–168. [PubMed] [Google Scholar]
- 31.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–17.e2. [DOI] [PubMed] [Google Scholar]
- 32.Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373(14):1307–1317. [DOI] [PubMed] [Google Scholar]
- 33.Modi AC, Loux TJ, Bell SK, Harmon CM, Inge TH, Zeller MH. Weight-specific health-related quality of life in adolescents with extreme obesity. Obesity (Silver Spring). 2008;16(10):2266–2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Puhl RM, Peterson JL, Luedicke J. Weight-based victimization: bullying experiences of weight loss treatment-seeking youth. Pediatrics. 2013;131(1):e1–e9. [DOI] [PubMed] [Google Scholar]
- 35.Flegal KM, Ogden CL, Yanovski JA, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. 2010;91(4):1020–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flegal KM, Shepherd JA, Looker AC, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009;89(2):500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8(4):307–326. [DOI] [PubMed] [Google Scholar]
- 38.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: the impact of parent-reported height and weight. Obesity (Silver Spring). 2009;17(8):1574–1580. [DOI] [PubMed] [Google Scholar]
- 39.Johnson CL, Paulose-Ram R, Ogden CL, et al. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital Health Stat 2. 2013;161(161):1–24. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.