Melanoma survivors are at risk to develop another melanoma and the same patterns of sun exposure that caused the initial melanoma contribute to the risk for a second melanoma.1 Despite awareness of the risk of developing another melanoma and the benefit of sun protection in modifying that risk,2 melanoma survivors often engage in unprotected episodes of sun exposure resulting in sunburn.3 While melanoma survivors initially decrease sun exposure following diagnosis, these changes are not maintained.4 This proof-of-concept study paired a wearable UV sensor with a self-report survey to explore sun protection behaviours of melanoma survivors
Melanoma survivors (stages: melanoma-in-situ to Stage IIB) consisting of 24 women and 15 men (n=39), who were diagnosed 4–7 years prior to enrolling in this study, had a mean age of 59 years (range 21–80) with Fitzpatrick skin type 1 (n=4), II (n=11), III (n=11), and IV (n=3). An erythemally-weighted UV sensor (Shade® model V1.00, YouV Labs Inc., NY), which was worn during daylight hours outdoors for 10 days during the summer of 2017 in Chicago, Illinois, reported UV exposure in J/m2 to one decimal point.5 The sensor’s magnetic ring requires affixation to clothing. Since T-shirts are reliably worn by most individuals, participants were informed to affix the sensor on the left anterior chest near to the shoulder as shown to participants in a picture.
Participants completed the Daily Minutes of Unprotected Sun Exposure (MUSE) Inventory, a self-reported online survey of sun-protection behaviours, that asks users to describe their level of clothing coverage across 17 body sites, sun protection behaviour (e.g. sunscreen use, shade-seeking) during self-reported activities,6 and a sunburn experience survey. The median minimal erythema dose for skin types I, II, III and IV are 2.5, 2.8, 3.6 and 4.5 standard erythema dose (SED).7 We clustered MUSE reported events with UV-exposure data derived from the sensor in instances when a user exceeded their daily MED. Northwestern University’s Institutional Review Board (STU00201983) approved this protocol.
During 307 of 390 possible days, UV-exposure was detected a median of 18% (IQR: 11%) of daylight hours. Technical problems led to data failure for 13% of all participant-days (50 days). During 40 days, participants had no exposure, forgot to wear the sensor, engaged in aquatic activities or wore it inappropriately. The median UV-exposure recorded over 10 days by each participant was 24.8 J/m2 (IQR: 34.3 J/m2) with a range of 1.0–227.4 J/m2. The median of maximum UV-exposure recorded in a single-day by each participant was 124.9 J/m2 (IQR: 140 J/m2) with a range of 1.0–600.0 J/m2.
Eighteen percent (7/39) of participants received at least one day of UV exposure that exceeded the MED for their respective Fitzpatrick skin type. (Fig 1) For participants who exceeded their daily MED, time-paired data from the MUSE inventory and the UV-sensor indicated that sunscreen use occurred in all but one of the high exposure days (7/8). Sunscreen was not reapplied on 50% of the days and sunburn was reported by one who exceeded their MED and failed to reapply sunscreen. Hats with a brim and sunglasses were each worn during 50% of the UV exposure events.
Figure 1.
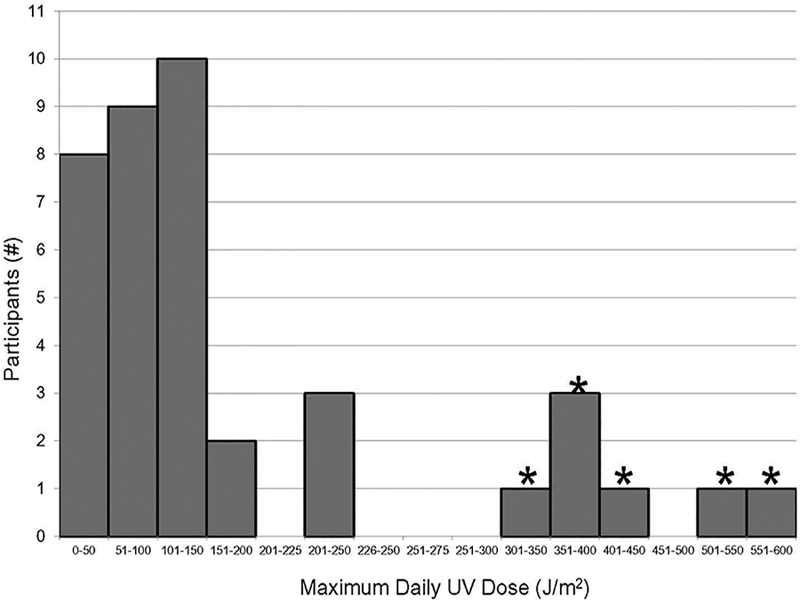
Maximum daily ultraviolet exposure in melanoma survivors. Participants exceeding their MED are indicated by asterisk.
During exit interviews, participants were given a report of their daily UV exposure. Five participants (13%) expressed surprise at their amount of UV exposure. All five had exceeded their MED on at least one day.
This study is limited by a small sample size and short duration of wear of the UV sensor. Furthermore, UV exposure recorded by the sensor will vary by the anatomic location of the sensor.7 While participants were informed and shown where to place the sensor, daily validation of sensor placement was not performed. Additionally, the sensor was not waterproof; therefore, it was not used during aquatic activities.
While objective measures of sun exposure, such as UV dosimeters, are rarely used in both clinical and real-world scenarios, the potential benefit of wearable UV sensor is to inform people, particularly those at-risk of developing skin cancer, of their cumulative UV exposure and to alert them when they approach sufficient exposure to sunburn. Knowledge of personal UV exposure may improve understanding of melanoma survivors regarding the amount of sun exposure they are receiving and in what circumstances. Enhancing melanoma survivors’ awareness of impending sunburn may improve adherence to sun protection in this at-risk population. With increasing ambient temperatures due to climate change, people in temperate climates may spend more days outdoors and wearable UV sensors may help to attenuate sunburn risk.
Acknowledgment
Relevant Disclosures: No conflicts of interest
Funding: Dr. Xu acknowledges support from the Foglia Family Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (T32 AR060710). Dr. Stump is supported by the National Cancer Institute (T32 CA193193). Dr. Robinson acknowledges support from the National Cancer Institute (R01 CA154908). Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR001422. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
YouV Labs Inc., New York, NY donated 20 Shade® sensors for use in this study and provided data management.
References
- 1.Kricker BK, Armstrong C, Goumas M, Litchfield CB, Begg AJ, Hummer LD, et al. 2007. Ambient UV, personal sun exposure and risk of multiple primary melanomas. Cancer Causes Control 2007; 18, 3 (Apr 2007), 295–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol 2011;29:257–263. [DOI] [PubMed] [Google Scholar]
- 3.Lee TK, Brazier AS, Shoveller JA, Gallagher RP. Sun-related behaviour after a diagnosis of cutaneous malignant melanoma. Melanoma Res 2007; 17:1 (Feb 2007), 51–55. [DOI] [PubMed] [Google Scholar]
- 4.Idorn LW, Datta P, Heydenreich J, Philipsen PA, Wulf HC. A 3-year follow-up of sun behaviour in patients with cutaneous malignant melanoma. JAMA Dermatol 2014;150:163–168. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee S, Hoch E, Kaplan P, ELP D. A Comparative Study of Wearable Ultraviolet Radiometers Proceedings of IEEE Life Sciences Sydney, Australia: IEEE; 2017. [Google Scholar]
- 6.Stump T, Aspinwall L, Gray E, Xu S, Maganti N, Leachman S et al. Daily Minutes of Sun Exposure (MUSE) Inventory: Measure description and comparisons to UV sensor and sun protection survey data. Prev Med Reports 2018;11:305–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diffey B Sun Protection: a risk management approach IOP Publishing, Bristol, 2017, pp 5.5–6 [Google Scholar]


