Abstract
The safety of minimally invasive distal pancreatectomy (MIDP) and open distal pancreatectomy (ODP) regarding oncological outcomes of pancreatic ductal adenocarcinoma (PDAC) remains inconclusive. Therefore, the aim of this study was to examine the oncological safety of MIDP and ODP for PDAC. Major databases including PubMed, Embase, Science Citation Index Expanded, and the Cochrane Library were searched for studies comparing outcomes in patients undergoing MIDP and ODP for PDAC from January 1994 to August 2018. In total, 11 retrospective comparative studies with 4829 patients (MIDP: 1076, ODP: 3753) were included. The primary outcome was long-term survival, including 3-year overall survival (OS) and 5-year OS. The 3-year OS (hazard ratio (HR): 1.03, 95% confidence interval (CI): 0.89, 1.21; P = 0.66) and 5-year OS (HR: 0.91, 95% CI: 0.65, 1.28; P = 0.59) showed no significant differences between the two groups. Furthermore, the positive surgical margin rate (weighted mean difference (WMD): 0.71, 95% CI: 0.56, 0.89, P = 0.003) was lower in the MIDP group. However, patients in the MIDP group had less intraoperative blood loss (WMD: −250.03, 95% CI: −359.68, −140.39; P < 0.00001), a shorter hospital stay (WMD: −2.76, 95% CI: −3.73, −1.78; P < 0.00001) and lower morbidity (OR: 0.57, 95% CI: 0.46, 0.71; P < 0.00001) and mortality (OR: 0.50, 95% CI: 0.31, 0.81, P = 0.005) than patients in the ODP group. The limited evidence suggested that MIDP might be safer with regard to oncological outcomes in PDAC patients. Therefore, future high-quality studies are needed to examine the oncological safety of MIDP.
Introduction
Pancreatic cancer is the fourth leading cause of cancer-related death among men and women in the USA and will become the second most deadly cancer in the near future1,2. Surgical resection remains the main treatment for pancreatic cancer3. The first minimally invasive distal pancreatectomy (MIDP) was reported in 1994. With the development of advanced technology, minimally invasive techniques have increasingly been used in pancreatic surgery4. MIDP is regarded as a safe and feasible procedure for pancreatic surgery5–7. However, one study showed that almost one-third of European pancreatic surgeons considered MIDP inferior to open distal pancreatectomy (ODP) in terms of oncological outcomes8. Furthermore, almost 21% of pancreatic surgeons considered the minimally invasive approach contraindicated for pancreatic ductal adenocarcinoma (PDAC)9. Moreover, some studies have shown that MIDP was not usually performed in clinical practice10.
Previously, a Cochrane review was published that describes all types of pancreatic cancer11. However, the oncological safety of MIDP for PDAC is still not clear. At present, some high-quality studies focusing on PDAC have been published, including one propensity score-matched study performed in Europe12. Thus, we conducted a systematic review and meta-analysis to evaluate the oncological safety of MIDP for PDAC.
Materials and Methods
Literature search
A systematic literature search was performed in PubMed, Embase, Science Citation Index Expanded, and the Cochrane Library to identify and retrieve studies published from January 1994 to August 2018 that examined distal pancreatectomy for PDAC (last search on August 8, 2018). The following medical search headings were used: (“Pancreatic Cancer” or “Pancreatic ductal adenocarcinoma” or “Pancreatic adenocarcinoma”) and (“Left pancreatectomy” or “Distal Pancreatectomy” or “Pancreatectomy”) and (“Laparoscopy” or “Laparoscopic-assisted” or “Laparoscopic” or “Robotic” or “Robot-assisted” or “Mini-invasive” or “Minimally invasive”). The language of full text articles was limited to English. In addition, the references of all selected articles were screened for any potential eligible studies.
Study selection
Studies were included in the meta-analysis if they met the following criteria: (1) human study; (2) published in English; (3) if studies were reported by the same institution (and/or authors), the study with either the larger sample size or higher quality was included. Studies meeting the following criteria were excluded: (1) case reports, letters, editorials, expert opinions and abstracts; (2) benign or other malignant tumors were included without reporting PDAC separately.
Qualitative assessment of the studies selected
The risk of bias of included nonrandomized studies was evaluated according to the risk of bias in nonrandomized studies of interventions (ROBINS-I) tool13.
Data extraction and synthesis
Each study was evaluated by two independent reviewers (Du-Jiang Yang and Jun-Jie Xiong) for inclusion or exclusion from the review. Disagreements between the reviewers were resolved by consensus and by consultation with a third reviewer (Hui-Min Lu) when necessary. Data were collected by two independent researchers using standardized forms. The study characteristics, quality assessment, and intraoperative and postoperative outcomes were included. The means of outcomes were used for the meta-analysis unless otherwise mentioned. Furthermore, the means and standard deviations or medians and ranges were reported14.
The following data were extracted from each study: author, year, country, study design, study duration, number of patients, age, sex, body mass index, tumor size, operation time, intraoperative blood loss, hospital stay, morbidity, postoperative pancreatic fistula (POPF) occurrence, mortality, positive surgical margin rate, lymph nodes harvested, perineural and lymphovascular invasion, multivisceral resection, positive lymph nodes, recurrence, adjuvant therapy and follow-up time.
Outcomes of interest and definitions
Minimally invasive was defined as a laparoscopic, robotic, laparoscopic-assisted or robot-assisted procedure. The primary outcome was overall survival (OS) time, which was defined as the time from the operation until death or the final follow-up evaluation. The secondary outcomes included operative time, intraoperative blood loss, hospital stay, morbidity, POPF occurrence, mortality, positive surgical margin, lymph nodes harvested, recurrence, perineural and lymphovascular invasion, multivisceral resection, positive lymph nodes, and adjuvant therapy. The operative time was defined as the interval from incision to suturing of the skin. Intraoperative blood loss was defined as the blood loss during surgery. The hospital stay was defined as the length from patient admission to discharge from the hospital. Morbidity was defined as all complications that occurred during the hospital stay or within 90 days after surgery. POPF occurrence was defined according to the International Study Group of Pancreatic Fistula (ISGPF)15. Mortality was defined as the number of deaths occurring during hospitalization or within 30 days after surgery. A positive surgical margin was defined as tumor in the transection and circumferential margins with a distance from the margin to the tumor of <1 mm12,16,17 or <0 mm18,19. Lymph nodes harvested was defined as the number of lymph nodes obtained during the operation. Recurrence was defined as local recurrence or distant metastasis. Adjuvant therapy was defined as the number of patients who received adjuvant therapy including postoperative radiation or chemotherapy.
Statistical analysis
A meta-analysis was performed using Review Manager Version 5.3 software (The Cochrane Collaboration, Oxford, UK). Variables are expressed as weighted mean differences (WMDs) or odds ratios (ORs) as appropriate, with their corresponding 95% confidence interval (CI). For continuous and categorical variables, treatment effects are expressed as WMDs and ORs with corresponding 95% CIs. For the survival analysis, we extracted data from the survival curve using a method reported in a previous study, and hazard ratios (HRs) were used for the quantitative analysis20. A Chi-square test was used to assess heterogeneity, with P < 0.1 considered significant. I2 values were used to evaluate statistical heterogeneity; an I2 value of 50% or more indicated the presence of heterogeneity21. The fixed-effects model was initially used for all outcomes, while the random-effects model was used if the test suggested rejection of the assumption of homogeneity22. Descriptive methods were used if the data were inappropriate for meta-analysis. A sensitivity analysis was performed by removing individual studies from the data set and analyzing the effect on the overall results to identify sources of heterogeneity. A funnel plot was constructed to evaluate potential publication bias based on the OS and positive surgical margin rate23.
Results
Description of the included studies
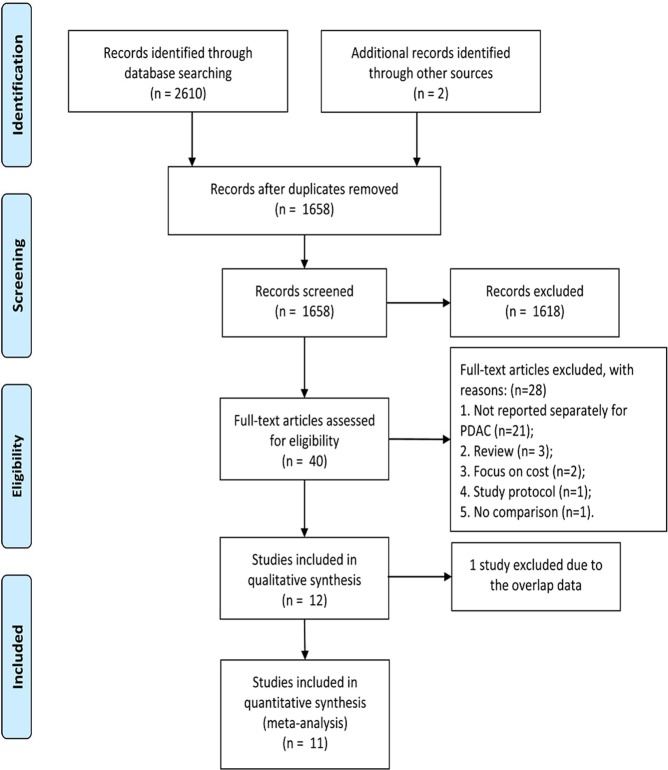
The reporting of this systematic review was in accordance with the PRISMA Statement24. A flow diagram of the study is shown in Fig. 1. In total, 2612 studies were identified from the electronic databases, and 954 studies were excluded because they were duplicate publications. Finally, the full texts of 40 studies11,12,16–19,25–58 were screened for eligibility; however, 28 studies were excluded for various reasons11,25,27–35,38,39,41–43,45–48,50–55,57,58 (Supplementary Materials). Only 12 studies12,16–19,26,36,37,40,44,49,56 were included for further analysis. However, two studies36,49 originated from the National Cancer Database (NCDB). Finally, the study by Kantor49 was excluded because of irrelevant data. In total, 11 studies12,16–19,26,36,37,40,44,56 with 4829 patients (MIDP: 1076, ODP: 3753) were included in the meta-analysis. The study characteristics are shown in Table 1. The studies originated from the United States (4 studies)18,26,36,44, China (2 studies)17,56, Korea37, the UK16, France40, Italy19, and Europe12. The tumor size, which was reported in 10 studies, was larger in patients who underwent ODP than in those who underwent MIDP (WMD: −0.45, 95% CI: −0.85, −0.05; P = 0.03). All included studies were retrospective comparative studies. The risk of bias in included studies was evaluated by the ROBINS-I tool (Table 2). Based on the ROBINS-I assessment, two studies12,37 were considered to have low risk, four studies17,18,26,40 were considered to have moderate risk, and five studies16,19,36,44,56 were considered to have serious risk of bias. Perioperative and tumor outcomes are shown in Tables 3 and 4. The results of the meta-analysis are shown in Table 5 and the Supplementary Materials.
Figure 1.
Flow chart for study search (PRISMA diagram). (PDAC = pancreatic ductal adenocarcinoma).
Table 1.
Characteristics of the included studies.
| Author | Year | Country | Study duration | Design | No of patients | Age (year) | Sex (F/M) | BMI (kg/m2) | Tumor size (cm) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | |||||
| Kooby18 | 2010 | USA | 2000–2008 | Retro | 23 | 70 | 64.6 ± 12.3 | 65.9 ± 11.1 | 12/11 | 43/27 | 28.5 ± 5.7 | 25.8 ± 4.6 | 3.6 ± 1.3 | 3.5 ± 1.4 |
| Magge26 | 2013 | USA | 2002–2010 | Retro | 28 | 34 | 67 + 11.6 | 66 ± 11.7 | 19/9 | 21/13 | 26.7 ± 1.3 | 26.5 ± 0.7 | 3.7 ± 1.3 | 4.5 ± 1.9 |
| Rehman16 | 2014 | UK | 2008–2011 | Retro | 8 | 14 | 64.2 | 64 | 3/8 | 13/1 | NR | NR | 2.4 ± 0.9 | 3.4 ± 1.4 |
| Sharpe36 | 2015 | USA | 2010–2011 | Retro | 144 | 625 | 67.7 ± 10.1 | 65.6 ± 10.5 | NR | NR | NR | NR | 3.7 ± 1.9 | 4.2 ± 3.2 |
| Shin37 | 2015 | Korea | 2006–2013 | PSM | 70 | 80 | 61 ± 7.8 | 65 ± 6 | 23/47 | 32/48 | 24.1 ± 2.1 | 23.1 ± 2.2 | 3 ± 1.35 | 3.5 ± 2.25 |
| Sulpice40 | 2015 | French | 2007–2012 | Retro | 347 | 2406 | 60.6 ± 14.7 | 64.5 ± 12.0 | 196/151 | 1236/1170 | NR | NR | NR | NR |
| Zhang17 | 2015 | China | 2003–2013 | Retro | 17 | 34 | 60 ± 7.75 | 64 ± 9 | 6/11 | 15/19 | 23.4 ± 4.7 | 23.7 ± 2.4 | 3.5 ± 0.8 | 3.9 ± 0.9 |
| Stauffer19 | 2016 | Italy | 1995–2014 | Retro | 44 | 28 | 72 ± 5.8 | 67.3 ± 6.8 | 18/26 | 12/16 | 28.3 ± 7.7 | 26.1 ± 4.3 | 3.6 ± 1.2 | 4.5 ± 2.5 |
| Bauman44 | 2017 | USA | 2005–2014 | Retro | 33 | 46 | 66 ± 2 | 66 ± 2 | 16/17 | 28/18 | 26.2 ± 0.8 | 27.8 ± 0.9 | 3.3 ± 0.3 | 4.0 ± 0.4 |
| Hilst12 | 2017 | European | 2007–2015 | PSM | 340 | 340 | 68 ± 10 | 68 ± 10 | 164/176 | 157/183 | 25 ± 3.7 | 25 ± 4.4 | 3.5 ± 1.5 | 3 ± 1.6 |
| Zhang56 | 2017 | China | 2010–2014 | Retro | 22 | 76 | 55.2 ± 13.1 | 59.8 ± 9.0 | 13/9 | 46/30 | 23.9 ± 2.7 | 23.7 ± 3.3 | 3.6 ± 1.3 | 4.4 ± 1.4 |
No = Number; F = Female; M = Man; BMI = Body mass index; MIDP = Minimally invasive distal pancreatectomy; ODP = Open distal pancreatectomy; Retro = Retrospective; PSM = Propensity score matching; NR = Not report; Data shown represents mean ± standard deviation.
Table 2.
Risk of bias for included studies.
| ROBINS-I | Kooby18 | Magge26 | Rehman16 | Sharpe36 | Shin37 | Sulpice40 | Zhang17 | Stauffer19 | Bauman44 | Hilst12 | Zhang56 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bias due to confounding | L | L | S | S | L | M | L | S | S | L | S |
| Bias in selection of participants into the study | M | L | L | L | L | L | L | L | L | L | L |
| Bias in measurement of interventions | L | L | L | L | L | M | L | L | L | L | L |
| Bias due to departures from intended interventions | M | M | M | L | L | M | M | M | M | L | M |
| Bias due to missing data | L | L | L | L | L | L | L | L | L | L | L |
| Bias in measurement of outcomes | L | L | L | L | L | L | L | L | M | L | L |
| Bias in selection of the reported result | L | M | M | M | L | M | M | M | M | L | M |
| Overall | M | M | S | S | L | M | M | S | S | L | S |
ROBINS-I = Risk of bias in non-randomized studies of interventions; L = Lower; M = Moderate; S = Serious.
Table 3.
Perioperative outcomes.
| Author | Operation time(min) | Intraoperative blood loss(mL) | Hospital stay(days) | Morbidity | POPF | Mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | |
| Kooby18 | 238.4 ± 68 | 216 ± 69 | 422 ± 473 | 751 ± 853 | 7.4 ± 3.4 | 9.4 ± 4.7 | NR | NR | NR | NR | 0 | 2 |
| Magge26 | 294 ± 126.9 | 317 ± 134.1 | 290 ± 317.5 | 570 ± 466.5 | 6 ± 2 | 8 ± 2.2 | 11 | 17 | 6 | 10 | NR | NR |
| Rehman16 | 396.5 ± 58.5 | 287 ± 60 | 349.25 ± 47.5 | 686.3 ± 288.8 | 8.75 ± 2.25 | 12.75 ± 3.75 | 3 | 3 | 2 | 3 | 1 | 1 |
| Sharpe36 | NR | NR | NR | NR | 6.8 ± 4.6 | 8.9 ± 7.5 | NR | NR | NR | NR | 0 | 10 |
| Shin37 | 239 ± 45.3 | 254 ± 76.3 | NR | NR | 9 ± 4 | 12 ± 20 | NR | NR | 13 | 8 | 0 | 1 |
| Sulpice40 | NR | NR | NR | NR | 14.9 ± 8.9 | 19.6 ± 14.6 | 117 | 1142 | NR | NR | 9 | 135 |
| Zhang17 | 190 ± 72.5 | 245 ± 66.25 | 50 ± 117.5 | 400 ± 950 | 13 ± 4.5 | 15.5 ± 8.5 | NR | NR | 9 | 16 | 0 | 1 |
| Stauffer19 | 254 ± 70.3 | 266 ± 68.7 | 332 ± 440 | 874 ± 541.7 | 5.1 ± 2.5 | 9.4 ± 5.3 | 6 | 7 | 6 | 2 | 1 | 0 |
| Bauman44 | 234 ± 12 | 252 ± 12 | 310 ± 68 | 597 ± 95 | 7.6 ± 1.4 | 9 ± 0.7 | 17 | 32 | 8 | 16 | 1 | 7 |
| Hilst12 | 240 ± 85.18 | 230 ± 80 | 200 ± 251.9 | 300 ± 259.3 | 8 ± 4.4 | 9 ± 5.2 | NR | NR | 65 | 67 | 7 | 8 |
| Zhang56 | 188 ± 39 | 160 ± 35 | 210 ± 130 | 240 ± 120 | NR | NR | NR | NR | 8 | 19 | 0 | 0 |
POPF = Postoperative pancreatic fistula; MIDP = Minimally invasive distal pancreatectomy; ODP = Open distal pancreatectomy; NR = Not reported; Data shown represents mean ± standard deviation.
Table 4.
Tumor outcomes.
| Author | Positive surgical margin | Lymph nodes harvested | Recurrence | Adjuvant chemotherapy | Perineural and lymfovascular invasion | Positive lymphnodes | Vascular resection | Follow-up (M) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | MIDP | ODP | ||
| Kooby18 | 6 | 24 | 14.0 ± 8.6 | 12.3 ± 8.3 | NR | NR | 13 | 45 | NR | NR | NR | NR | NR | NR | 82 |
| Magge26 | 4 | 4 | 11 ± 8.9 | 12 ± 9.6 | 2 | 1 | 25 | 29 | NR | NR | 13 | 13 | NR | NR | 60 |
| Rehman16 | 1 | 2 | 15 ± 6.5 | 13.5 ± 6.5 | NR | NR | 4 | 9 | NR | NR | 4 | 9 | NR | NR | 60 |
| Sharpe36 | 17 | 127 | 14.9 ± 10 | 13.3 ± 9.9 | NR | NR | 3 | 69 | NR | NR | 68 | 304 | NR | NR | NR |
| Shin37 | 17 | 13 | 12 ± 5.5 | 10 ± 10.5 | 35 | 48 | 55 | 55 | NR | NR | NR | NR | NR | NR | 60 |
| Sulpice40 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 2 | 96 | 60 |
| Zhang17 | 1 | 5 | 9 ± 2.5 | 8 ± 5 | 11 | 16 | 13 | 26 | 12 | 25 | NR | NR | 0 | 1 | NR |
| Stauffer19 | 2 | 5 | 25.9 ± 7.2 | 12.7 ± 7.3 | NR | NR | 31 | 18 | NR | NR | NR | NR | 3 | 2 | 60 |
| Bauman44 | 6 | 6 | 14.5 ± 1.1 | 17.5 ± 1.2 | 10 | 24 | 20 | 29 | NR | NR | NR | NR | NR | NR | 60 |
| Hilst12 | 122 | 152 | 14 ± 10.4 | 22 ± 12.6 | NR | NR | 165 | 159 | 164 | 210 | NR | NR | 19 | 38 | 82 |
| Zhang56 | 2 | 10 | 11.2 ± 4.6 | 14.4 ± 5.5 | NR | NR | NR | NR | NR | NR | 8 | 31 | NR | NR | 50 |
MIDP = Minimally invasive distal pancreatectomy; ODP = Open distal pancreatectomy; NR = Not reported; M = Months; Data shown represents mean ± standard deviation.
Table 5.
Results of meta-analysis comparing MIDP versus ODP for PDAC.
| Outcome of interest | No. of studies | No. of patients | OR/WMD/HR | 95%CI | P value | Heterogeneity P value | I 2 |
|---|---|---|---|---|---|---|---|
| Primary outcome | |||||||
| 3-OS | 9 | 3988 | 1.03 | 0.89,1.21 | 0.66 | 0.67 | 0% |
| 5-OS | 4 | 3044 | 0.91 | 0.65,1.28 | 0.59 | 0.35 | 9% |
| Secondary outcomes | |||||||
| Operation time | 9 | 1307 | 5.98 | −13.15, 25.11 | 0.54 | <0.00001 | 88% |
| Intraoperative blood loss | 8 | 1157 | −250.04 | −359.69, −140.39 | <0.00001 | <0.00001 | 92% |
| Hospital stay | 10 | 4731 | −2.50 | −3.36, −1.63 | <0.00001 | <0.00001 | 79% |
| Morbidity | 5 | 2988 | 0.57 | 0.46, 0.71 | <0.00001 | 0.69 | 0% |
| POPF | 7 | 1152 | 1.10 | 0.82, 1.47 | 0.54 | 0.56 | 0% |
| Mortality | 10 | 4767 | 0.50 | 0.31, 0.81 | 0.005 | 0.84 | 0% |
| Positive surgical margin | 10 | 2076 | 0.71 | 0.56, 0.89 | 0.003 | 0.39 | 6% |
| Lymph nodes harvested | 10 | 2076 | 0.40 | −2.36, 3.16 | 0.78 | <0.00001 | 95% |
| Recurrence | 4 | 342 | 0.74 | 0.47, 1.18 | 0.21 | 0.14 | 46% |
| Adjuvant therapy | 9 | 1978 | 0.94 | 0.75, 1.18 | 0.59 | 0.13 | 36% |
| Positive lymphnodes | 4 | 951 | 0.95 | 0.69, 1.31 | 0.76 | 0.80 | 0% |
| Vascular resection | 4 | 3556 | 0.36 | 0.22, 0.60 | <0.00001 | 0.30 | 19% |
| Perineural and lymfovascular invasion | 2 | 731 | 0.59 | 0.44, 0.79 | 0.0005 | 0.55 | 0% |
MIDP = Minimally invasive distal pancreatectomy; ODP = Open distal pancreatectomy; OR = Odds ratio; WMD = Weighted Mean Difference; HR = Hazard ratio; PDAC = Pancreatic ductal adenocarcinoma; 3-OS = 3 year overall survival; 5-OS = 5 year overall survival; POPF = Postoperative pancreatic fistula.
Results of the meta-analysis
Primary outcomes
The OS was reported in ten studies12,16–19,26,37,40,44,56. However, the OS could not be extracted from the survival curve in a study by Staffer19. Finally, nine studies reported 3-year OS, and four studies reported 5-year OS. No statistically significant differences were observed in 3-year OS (HR: 1.03, 95% CI: 0.89, 1.21; P = 0.66) or 5-year OS (HR: 0.91, 95% CI: 0.65, 1.28; P = 0.59) between the two groups.
Secondary outcomes
A positive surgical margin was reported in all included studies. The pooled analysis suggested that MIDP was associated with a lower rate of positive surgical margins (OR: 0.71, 95% CI: 0.56, 0.89; P = 0.003). According to the different definitions, the MIDP group also had a lower rate of positive surgical margins for a margin to tumor distance <1 mm12,16,17 (OR: 0.66, 95% CI: 0.49, 0.89; P = 0.006). However, no significant difference was observed for a margin to tumor distance <0 mm18,19 (OR: 0.49, 95% CI: 0.20, 1.20; P = 0.12) between the two groups. Only two studies12,17 reported perineural and lymphovascular invasion; the MIDP group had less perineural and lymphovascular invasion (OR: 0.59, 95% CI: 0.44, 0.79; P = 0.0005) than the ODP group. Positive lymph nodes were reported in four studies16,26,36,56; however, no significant difference was found in this outcome between the two groups (OR: 0.95, 95% CI: 0.69, 1.31; P = 0.76). The rate of the recurrence was not significantly different (OR: 0.74, 95% CI: 0.47, 1.18; P = 0.21) between groups according to the pooled results of 4 studies17,26,37,59. Unfortunately, only one study reported multivisceral resection, and no difference (ODP: −32.1% vs MIDP: −38.6%, P = 0.66) was found between the two groups. MIDP was associated with less intraoperative blood loss (WMD: −250.03, 95% CI: −359.68, −140.39; P < 0.00001), shorter hospital stay (WMD: −2.76, 95% CI: −3.73, −1.78; P < 0.00001), and lower morbidity (OR: 0.57, 95% CI: 0.46, 0.71; P < 0.00001) and mortality (OR: 0.50; 95% CI: 0.31, 0.81; P = 0.005) than ODP. However, no significant difference was observed in operative time (WMD: 5.98, 95% CI: −13.15, 25.11; P = 0.54), POPF occurrence (OR: 1.10; 95% CI: 0.82, 1.47; P = 0.54), number of lymph nodes harvested (WMD: 0.40, 95% CI: −2.36, 3.16; P = 0.78), recurrence (OR: 0.74, 95% CI: 0.47, 1.18; P = 0.21) and adjuvant therapy (OR: 0.94; 95% CI: 0.75, 1.18; P = 0.59) between the two groups.
Sensitivity analysis
A sensitivity analysis was conducted by changing the type of effects model or excluding individual studies from the outcome analysis. The results in operation time were different in the fixed and random effects models. Although high heterogeneity was found for blood loss, this result was presented in both the fixed and random effects models. The heterogeneity was large for hospital stay; however, the heterogeneity was zero when two studies (Sulipice40 and Bauman59 were excluded.
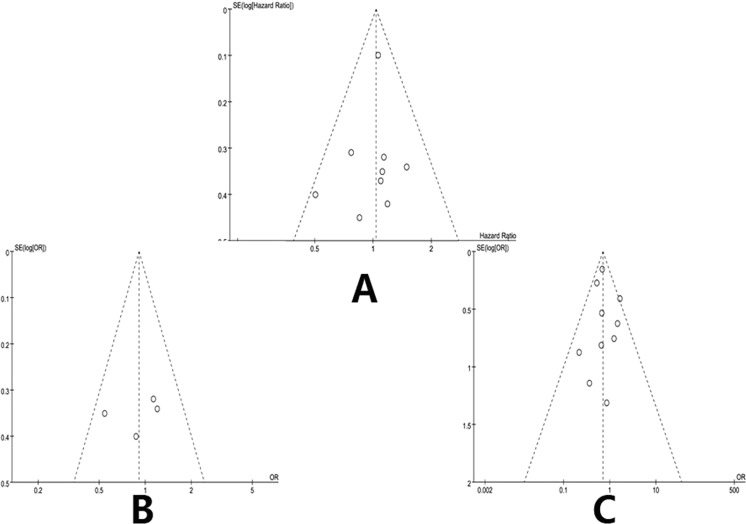
Publication bias
Funnel plots based on the 3-year OS, 5-year OS and positive surgical margins are shown in Fig. 2. No study was outside the limits of the 95% CI; therefore, no evidence of publication bias was present.
Figure 2.
Funnel plot to investigate publication bias. (A) Funnel plot based on 3 year overall survival. (B) Funnel plot based on 5 year overall survival. (C) Funnel plot based on positive surgical margin.
Discussion
MIDP has been performed for more than a decade, and the technical feasibility, safety and clinical benefit have been well documented by many studies comparing it to ODP34,60,61. However, some centers still favor adopting a conventional, open approach for PDAC62,63.This systematic review and meta-analysis suggested that the OS and oncologic outcomes are not significantly different between the MIDP and ODP groups. Although the pooled results were mainly based on nonrandomized data, the results suggested that MIDP did not adversely affect long-term survival in PDAC patients. Furthermore, the MIDP group also had a lower rate of positive surgical margins and less perineural and lymphovascular invasion. Therefore, MIDP might be feasible and safe regarding long-term survival and oncological outcomes in PDAC patients.
Currently, the rate of long-term survival after distal resection for PDAC patients remains poor. Despite the significant improvement in operative skill for MIDP, the long-term survival is still not different between the two groups of PDAC patients. Radical surgical resection remains the only potentially curative treatment for patients with resectable PDAC64. A recent review from a large randomized trial involving resection of PDAC showed positive margin rates ranging from 0% to 83%65. The finding in the current report is consistent with those in the published literature30. Importantly, the MIDP results in fewer resections with positive margins than ODP. This advantage might be due to the clearer view and more elaborate procedure of MIDP. However, the rate of positive margin resection in present study should be interpreted with caution because margin status was influenced by the use of different definitions and pathologic assessment methods. Furthermore, conclusions may vary by pathologists and institutions due to the absence of standardized pathology assessment and reporting. Moreover, surgeons determine which method is more suitable for the PDAC patients before surgery. Therefore, patients with less extensive cancer may undergo MIDP, and patients with more extensive cancer would undergo ODP16,36.
Regarding other oncological outcomes, no significant differences were found for recurrence, lymph nodes harvested and positive lymph nodes. The extent of the lymphadenectomy determined the number of retrieved lymph nodes. According to one report, at least 12 lymph nodes should be evaluated histologically to determine metastatic disease and adequately stage PDAC patients66. Moreover, according to the consensus of the International Study Group on Pancreatic Surgery (ISGPS), a standard lymphadenectomy with resection of lymph node stations 10, 11, and 18 is recommended for cancer of the body and tail of the pancreas67. In most included studies, the mean number of harvested lymph nodes was greater than 12. In present study, no significant difference was observed in the number of harvested lymph nodes between the two groups. Based on this finding, MIDP is a reasonable procedure for PDAC patients.
No difference was observed in some clinical outcomes. However, MIDP is associated with a steep learning curve. This observation potentially affected several outcomes, including operative time, blood loss and the length of hospital stay16. Therefore, the hospital stay and blood loss were decreased in the MIDP group. Moreover, MIDP was associated with significantly lower morbidity and mortality rates than ODP. Our results are consistent with those of many studies. The technical feasibility, safety and clinical benefit have been well confirmed by various matched comparison studies34,60,61. Thus, MIDP might be safer with regard to oncological outcomes in PDAC patients.
However, our study has some limitations. First, all of the included studies were retrospective, which could lead to inevitable selection bias toward resection of larger or locally advanced tumors via the open approach, especially in the earlier years of the study period. Second, the follow-up time differed and was relatively short in some studies. Therefore, the long-term survival was difficult to accurately estimate. Third, the definitions of some outcomes were different among studies.
Conclusion
In summary, the meta-analysis demonstrated that MIDP might be safer with regard to the oncological outcomes of PDAC patients. However, these results need to be confirmed in a future prospective randomized trial.
Supplementary Information
Acknowledgements
This work is supported by the Sichuan Provincial Department of Science and Technology Supporting Project (Grant Number: 2018SZ0174, Sichuan, China). This meta-analysis was registered at https://www.crd.york.ac.uk/prospero/under registration number CRD42018106941.
Author Contributions
Du-Jiang Yang, Jun-Jie Xiong and Wei-Ming Hu designed the study. Du-Jiang Yang and Jun-Jie Xiong performed the study and wrote the paper. Hui-Min Lu and Yi Wei assessed the study and collected the data. Ling Zhang and Shan Lu analyzed the data. Wei-Ming Hu reviewed the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Du-Jiang Yang and Jun-Jie Xiong contributed equally.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-37617-0.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2.Rahib L, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Research. 2014;74:2913–2921. doi: 10.1158/0008-5472.CAN-14-0155. [DOI] [PubMed] [Google Scholar]
- 3.Gao JJ, et al. Standardization of perioperative management on hepato-biliary-pancreatic surgery. Drug Discov Ther. 2012;6:108–111. [PubMed] [Google Scholar]
- 4.Soper NJ, Brunt LM, Dunnegan DL, Meininger TA. Laparoscopic distal pancreatectomy in the porcine model. Surgical Endoscopy. 1994;8:57–60. doi: 10.1007/BF02909495. [DOI] [PubMed] [Google Scholar]
- 5.Kim SC, et al. Comparative analysis of clinical outcomes for laparoscopic distal pancreatic resection and open distal pancreatic resection at a single institution. Surgical Endoscopy and Other Interventional Techniques. 2008;22:2261–2268. doi: 10.1007/s00464-008-9973-1. [DOI] [PubMed] [Google Scholar]
- 6.Mehta SS, Doumane G, Mura T, Nocca D, Fabre JM. Laparoscopic versus open distal pancreatectomy: a single-institution case-control study. Surgical Endoscopy. 2012;26:402–407. doi: 10.1007/s00464-011-1887-7. [DOI] [PubMed] [Google Scholar]
- 7.Melotti G, et al. Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. Annals of Surgery. 2007;246:77–82. doi: 10.1097/01.sla.0000258607.17194.2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rooij TD, et al. Pan-European survey on the implementation of minimally invasive pancreatic surgery with emphasis on cancer. Hpb the Official Journal of the International Hepato Pancreato Biliary Association. 2016;18:170. doi: 10.1016/j.hpb.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van HJ, et al. Worldwide survey on opinions and use of minimally invasive pancreatic resection. Hpb the Official Journal of the International Hepato Pancreato Biliary Association. 2017;19:190. doi: 10.1016/j.hpb.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 10.Mabrut JY, et al. Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery. 2005;137:597–605. doi: 10.1016/j.surg.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Riviere D, et al. Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Database of Systematic Reviews. 2016;4:CD011391. doi: 10.1002/14651858.CD011391.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van HJ, et al. Minimally Invasive versus Open Distal Pancreatectomy for Ductal Adenocarcinoma (DIPLOMA): A Pan-European Propensity Score Matched Study. Annals of Surgery. 2017;17:S20. doi: 10.1016/j.amsu.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Sterne JA, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Bmj. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xiong JJ, et al. Meta-analysis of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Br J Surg. 2014;101:1196–1208. doi: 10.1002/bjs.9553. [DOI] [PubMed] [Google Scholar]
- 15.Bassi C, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 16.Rehman S, et al. Oncological Feasibility of Laparoscopic Distal Pancreatectomy for Adenocarcinoma: A Single-Institution Comparative Study. World Journal of Surgery. 2014;38:476–483. doi: 10.1007/s00268-013-2268-2. [DOI] [PubMed] [Google Scholar]
- 17.Zhang M, et al. LDP vs ODP for pancreatic adenocarcinoma: a case matched study from a single-institution. Bmc Gastroenterology. 2015;15:1–8. doi: 10.1186/s12876-014-0226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kooby DA, et al. A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg. 2010;210:779–785. doi: 10.1016/j.jamcollsurg.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 19.Stauffer JA, Coppola A, Mody K, Asbun HJ. Laparoscopic Versus Open Distal Pancreatectomy for Pancreatic Adenocarcinoma. World Journal of Surgery. 2016;40:1477–1484. doi: 10.1007/s00268-016-3412-6. [DOI] [PubMed] [Google Scholar]
- 20.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Statistics in Medicine. 2004;23:2815–2834. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dersimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7:177. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.Sterne JAC, Egger M, Smith GD. Investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101–105. doi: 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Medicine3, e123–130 (2009). [PMC free article] [PubMed]
- 25.Vijan SS, et al. Laparoscopic vs open distal pancreatectomy: a single-institution comparative study. Arch Surg. 2010;145:616–621. doi: 10.1001/archsurg.2010.120. [DOI] [PubMed] [Google Scholar]
- 26.Magge D, et al. Comparative Effectiveness of Minimally Invasive and Open Distal Pancreatectomy for Ductal Adenocarcinoma. JAMA Surgery. 2013;148:525–531. doi: 10.1001/jamasurg.2013.1673. [DOI] [PubMed] [Google Scholar]
- 27.Duran H, et al. Does robotic distal pancreatectomy surgery offer similar results as laparoscopic and open approach? A comparative study from a single medical center. International Journal of Medical Robotics + Computer Assisted Surgery Mrcas. 2014;10:280. doi: 10.1002/rcs.1569. [DOI] [PubMed] [Google Scholar]
- 28.Hu M, et al. Laparoscopic versus open distal splenopancreatectomy for the treatment of pancreatic body and tail cancer: a retrospective, mid-term follow-up study at a single academic tertiary care institution. Surgical Endoscopy. 2014;28:2584–2591. doi: 10.1007/s00464-014-3507-9. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Y, Chen X, Sun D. Laparoscopic versus open distal pancreatectomy: a single-institution comparative study. World Journal of Surgical Oncology. 2014;12:327–327. doi: 10.1186/1477-7819-12-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adam MA, et al. Minimally Invasive Distal Pancreatectomy for Cancer: Short-Term Oncologic Outcomes in 1,733 Patients. World Journal of Surgery. 2015;39:2564–2572. doi: 10.1007/s00268-015-3138-x. [DOI] [PubMed] [Google Scholar]
- 31.Braga M, et al. Results of 100 consecutive laparoscopic distal pancreatectomies: postoperative outcome, cost-benefit analysis, and quality of life assessment. Surgical Endoscopy. 2015;29:1871–1878. doi: 10.1007/s00464-014-3879-x. [DOI] [PubMed] [Google Scholar]
- 32.De RT, et al. A nationwide comparison of laparoscopic and open distal pancreatectomy for benign and malignant disease. Journal of the American College of Surgeons. 2015;220:263–270. doi: 10.1016/j.jamcollsurg.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 33.Khaled YS, et al. A Case-matched Comparative Study of Laparoscopic Versus Open Distal Pancreatectomy. Surgical Laparoscopy Endoscopy & Percutaneous Techniques. 2015;25:363–367. doi: 10.1097/SLE.0000000000000179. [DOI] [PubMed] [Google Scholar]
- 34.Lee SY, et al. Distal pancreatectomy: a single institution’s experience in open, laparoscopic, and robotic approaches. J Am Coll Surg. 2015;220:18–27. doi: 10.1016/j.jamcollsurg.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 35.Ricci C, et al. Laparoscopic Distal Pancreatectomy in Benign or Premalignant Pancreatic Lesions: Is It Really More Cost-Effective than Open Approach? Journal of Gastrointestinal Surgery Official Journal of the Society for Surgery of the Alimentary Tract. 2015;19:1415. doi: 10.1007/s11605-015-2841-0. [DOI] [PubMed] [Google Scholar]
- 36.Sharpe SM, et al. The laparoscopic approach to distal pancreatectomy for ductal adenocarcinoma results in shorter lengths of stay without compromising oncologic outcomes. American Journal of Surgery. 2015;209:557–563. doi: 10.1016/j.amjsurg.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 37.Shin SH, et al. A comparative study of laparoscopic vs. open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity score-matched analysis. Journal of the American College of Surgeons. 2015;220:177. doi: 10.1016/j.jamcollsurg.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 38.De RT, et al. Outcomes of Distal Pancreatectomy for Pancreatic Ductal Adenocarcinoma in the Netherlands: A Nationwide Retrospective Analysis. Annals of Surgical Oncology. 2016;23:585–591. doi: 10.1245/s10434-015-4930-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iype, S. et al. Short-term and long-term outcomes of distal pancreatectomy. Hpb18 (2016).
- 40.Sulpice L, et al. Laparoscopic Distal Pancreatectomy for Pancreatic Ductal Adenocarcinoma: Time for a Randomized Controlled Trial? Results of an All-inclusive National Observational Study. Annals of Surgery. 2016;262:868. doi: 10.1097/SLA.0000000000001479. [DOI] [PubMed] [Google Scholar]
- 41.Zhang YH, Zhang CW, Hu ZM, Hong DF. Pancreatic cancer: Open or minimally invasive surgery? World journal of gastroenterology. 2016;22:7301. doi: 10.3748/wjg.v22.i32.7301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anderson KL, Adam MA, Thomas S, Roman SA, Sosa JA. Impact of minimally invasive vs. open distal pancreatectomy on use of adjuvant chemoradiation for pancreatic adenocarcinoma. American Journal of Surgery. 2017;213:601–605. doi: 10.1016/j.amjsurg.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 43.Aprea G, et al. Laparoscopic distal pancreatectomy in elderly patients: is it safe? Aging Clinical & Experimental Research. 2017;29:41–45. doi: 10.1007/s40520-016-0677-4. [DOI] [PubMed] [Google Scholar]
- 44.Bauman MD, et al. Laparoscopic distal pancreatectomy for pancreatic cancer is safe and effective. Surgical Endoscopy & Other Interventional Techniques. 2017;32:1–9. doi: 10.1007/s00464-017-5633-7. [DOI] [PubMed] [Google Scholar]
- 45.Conlon, K. C. et al. Minimally invasive pancreatic resections: cost and value perspectives. HPB19 (2017). [DOI] [PubMed]
- 46.De Rooij T, et al. Minimally invasive versus open distal pancreatectomy (LEOPARD): study protocol for a randomized controlled trial. Trials. 2017;18:166. doi: 10.1186/s13063-017-1892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gabriel E, Thirunavukarasu P, Attwood K, Nurkin SJ. National disparities in minimally invasive surgery for pancreatic tumors. Surgical Endoscopy and Other Interventional Techniques. 2017;31:398–409. doi: 10.1007/s00464-016-4987-6. [DOI] [PubMed] [Google Scholar]
- 48.Joliat G-R, Demartines N, Halkic N, Petermann D, Schaefer M. Short-term outcomes after distal pancreatectomy: Laparotomy vs. laparoscopy - A single-center series. Annals of Medicine and Surgery. 2017;13:1–5. doi: 10.1016/j.amsu.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kantor O, et al. Laparoscopic Distal Pancreatectomy for Cancer Provides Oncologic Outcomes and Overall Survival Identical to Open Distal Pancreatectomy. Journal of Gastrointestinal Surgery. 2017;21:1620–1625. doi: 10.1007/s11605-017-3506-y. [DOI] [PubMed] [Google Scholar]
- 50.Nassour I, et al. Conversion of Minimally Invasive Distal Pancreatectomy: Predictors and Outcomes. Annals of Surgical Oncology. 2017;24:3725–3731. doi: 10.1245/s10434-017-6062-5. [DOI] [PubMed] [Google Scholar]
- 51.Ome Y, et al. Laparoscopic radical antegrade modular pancreatosplenectomy for left-sided pancreatic cancer using the ligament of Treitz approach. Surgical Endoscopy. 2017;31:1–2. doi: 10.1007/s00464-017-5561-6. [DOI] [PubMed] [Google Scholar]
- 52.Plotkin A, et al. Reduced morbidity with minimally invasive distal pancreatectomy for pancreatic adenocarcinoma. Hpb the Official Journal of the International Hepato Pancreato Biliary Association. 2017;19:279. doi: 10.1016/j.hpb.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 53.Rosok BI, et al. Minimally invasive distal pancreatectomy. Hpb. 2017;19:205–214. doi: 10.1016/j.hpb.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 54.Wellner, U. F. et al. Laparoscopic versus open distal pancreatectomy-a propensity score-matched analysis from the German StuDoQ|Pancreas registry. International Journal of Colorectal Disease, 1–8 (2017). [DOI] [PubMed]
- 55.Xourafas D, Ashley SW, Clancy TE. Comparison of Perioperative Outcomes between Open, Laparoscopic, and Robotic Distal Pancreatectomy: an Analysis of 1815 Patients from the ACS-NSQIP Procedure-Targeted Pancreatectomy Database. Journal of Gastrointestinal Surgery. 2017;21:1442–1452. doi: 10.1007/s11605-017-3463-5. [DOI] [PubMed] [Google Scholar]
- 56.Zhang A, Wang Y, Hu C, Shen Y, Zheng S. Laparoscopic versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a single-center experience. Journal of Zhejiang University-science B. 2017;18:532–538. doi: 10.1631/jzus.B1600541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fisher, A. V. et al. Analysis of 90-day cost for open versus minimally invasive distal pancreatectomy. Hpb (2018). [DOI] [PubMed]
- 58.Raoof M, et al. Propensity score-matched comparison of oncological outcomes between laparoscopic and open distal pancreatic resection. British Journal of Surgery. 2018;105:578–586. doi: 10.1002/bjs.10747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bauman MD, et al. Laparoscopic distal pancreatectomy for pancreatic cancer is safe and effective. Surgical Endoscopy and Other Interventional Techniques. 2017;32:53–61. doi: 10.1007/s00464-017-5633-7. [DOI] [PubMed] [Google Scholar]
- 60.Eom BW, et al. Clinical outcomes compared between laparoscopic and open distal pancreatectomy. Surgical Endoscopy and Other Interventional Techniques. 2008;22:1334–1338. doi: 10.1007/s00464-007-9660-7. [DOI] [PubMed] [Google Scholar]
- 61.Soh YF, et al. Perioperative outcomes of laparoscopic and open distal pancreatectomy: our institution’s 5-year experience. Asian J Surg. 2012;35:29–36. doi: 10.1016/j.asjsur.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 62.Marangos IP, et al. Laparoscopic resection of exocrine carcinoma in central and distal pancreas results in a high rate of radical resections and long postoperative survival. Surgery. 2012;151:717–723. doi: 10.1016/j.surg.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 63.Deoliveira ML, et al. Assessment of Complications After Pancreatic Surgery A Novel Grading System Applied to 633 Patients Undergoing Pancreaticoduodenectomy. Annals of Surgery. 2006;244:931–939. doi: 10.1097/01.sla.0000246856.03918.9a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wagner M, et al. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. British Journal of Surgery. 2004;91:586–594. doi: 10.1002/bjs.4484. [DOI] [PubMed] [Google Scholar]
- 65.Butturini G, et al. Influence of resection margins and treatment on survival in patients with pancreatic cancer: meta-analysis of randomized controlled trials. Archives of Surgery. 2008;143:75–83. doi: 10.1001/archsurg.2007.17. [DOI] [PubMed] [Google Scholar]
- 66.Slidell MB, et al. Impact of Total Lymph Node Count and Lymph Node Ratio on Staging and Survival after Pancreatectomy for Pancreatic Adenocarcinoma: A Large, Population-Based Analysis. Annals of Surgical Oncology. 2008;15:165–174. doi: 10.1245/s10434-007-9587-1. [DOI] [PubMed] [Google Scholar]
- 67.Tol JAMG, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: A consensus statement by the International Study Group on Pancreatic Surgery (ISGPS) Surgery. 2014;156:591–600. doi: 10.1016/j.surg.2014.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.