Abstract
Every day, health physicists and physicians are expected to communicate effectively with concerned people, but rarely (if ever) are they given training on how to effectively communicate. In an age of social media, this paper presents the relevance of teachings from an ancient Greek philosopher. Aristotle’s Rhetoric is still considered one of the most influential works on persuasive messaging. He puts the onus of effective communications on the people with the “true” and “just” information to communicate that information clearly to the audience. By communicating with intention—using the persuasive appeals of ethos, pathos, logos, and storytelling—radiation professionals can speak to their expertise in radiation science, while adapting their instructions, presentations, and communications styles to meet the needs of each type of audience: from scientists to concerned citizens, from doctors to first responders, and beyond.
Keywords: National Council on Radiation Protection and Measurements, risk communication, radiation risk, patient protection, health effects
In the age of social media, where immense value is placed on what can be said in 280 characters, it is easy to lose sight of the fact that the measure of effective communication is how well the message is received and understood, not the communicators’ perception of how well they are communicating. So, can 21st century radiation professionals learn from an ancient Greek philosopher? Undoubtedly, yes.
Aristotle’s Rhetoric is still considered one of the most influential works on persuasive messaging. Aristotle puts the onus of effective communications on the people with the “true” and “just” information to communicate that information clearly to the audience (Aristotle et al. 1954). As members of the radiation community, it is our responsibility and duty to communicate radiation protection information successfully to stakeholders. While every person has preferences for how they receive information, there are some overarching practices for effective communication that radiation professionals should implement in order to communicate the complex topics of radiation science and radiation risk.
Except for classroom or professional settings, the majority of radiation communication with the public takes place because someone is concerned about their health or the health of a loved one. People want to know their personal risk from a specific exposure. The desire for personalized information isn’t swayed by the fact that we base risk estimates on population statistics and, at low doses, on the linear nonthreshold model. Our ability to communicate radiation risk is hampered even more by the fact that individuals in a high stress situation typically have a difficult time hearing and remembering information and tend to focus on negative information (Covello 2011).
Because the ability to absorb information is hindered during high stress situations, it becomes crucial to communicate thoughtfully so that the information is received as intended. The same way that medical treatment is tailored to a patient, information needs to be tailored to the recipient. Before you start communicating, you need to (1) understand how your audience prefers to get their information, (2) identify your intended outcome, and (3) decide on the communication techniques that will be most effective. This three-step process is something people do unconsciously all of the time. For example, when you arc making dinner for a group, you know their preferences and allergies (audience preference), decide on a meal (intended outcome), and gather ingredients (tool/techniques) before you start cooking. Similarly, knowing the audience and intended outcome, and choosing communication techniques should be decided before you start communicating.
While each information consumer is different and may have different information needs, Aristotle presents three overarching “appeals” of persuasive messaging: ethos, pathos, and logos. Respectively, “the first depends upon the moral character of the speaker, the second upon putting the hearer into a certain frame of mind, the third upon the speech itself…” (Aristotle et al. 1954).
ETHOS — CREDIBILITY IN COMMUNICATING RADIATION INFORMATION
Ethos is about the credibility of the communicator. More specifically, it is about the inherent credibility and likeability of the communicator before lie or she starts delivering the message. As a radiation professional, you have expertise. This is not in question. But expertise only makes up 15 – 20% of your credibility. Caring and empathy make up about 50% of your credibility, and people judge empathy within the first 9 – 30 s of meeting you (ASTHO 2002; Covello 2009; Covello and Milligan 2010). From physical appearance alone, people will judge trustworthiness in 100 ms (one-tenth of a second) or less (Willis and Todorov 2006). One 2017 study reported that people could make trustworthiness judgements based on 33 ms of viewing a face (South Palomares and Young 2017).
With less than a second to make an impression, the opportunity to influence how others view your credibility happens before you walk in the door. Ethos is clothing, hair, posture, and facial expression from the literal moment a person first sees you. It is the difference between walking into the room staring at a book and walking in and immediately making eye contact. It is the first words that come out of your mouth. It is the difference between starting an interaction with “Umm” or “Hello.”
When you have advanced notice, first impressions should always be thought through. What is the image you want to project? You only get one chance to make a first impression. In radiation, we arc often faced with discussions about people’s health. A good first impression will be a positive, affirming start to what is likely to be an emotional conversation.
PATHOS — EMOTION IN COMMUNICATING RADIATION INFORMATION
Pathos is about tapping into the receivers’ emotions—getting them “into a certain frame of mind”—to illicit a preferred outcome (Aristotle et al. 1954). Typically, pathos is discussed in the context of inspiring large crowds. But, the pathos appeal is about communicating with purpose to move the emotional state of an audience to the place where your message will be best understood and acted upon. Intentional emotional maneuvering can and should be applied to individual interactions.
Most public communication about radiation is with citizens who arc concerned about their health or the health of a loved one. This is especially true in the medical community. As already discussed, the ability for a person to absorb information is greatly reduced when stress levels arc high. The high-stress, doubt, and fear associated with health concerns arc emotional barriers to information consumption. This adds to the already challenging task of communicating information on radiation and medical benefits and risks to concerned patients and family members.
Doctors need to communicate with the intention of reducing the patient’s emotional barriers in order to effectively convey radiation risk information for the purpose of informed decision making. To communicate with intention, you must:
know what you want to accomplish in a specific communication;
identify barriers to accomplishing that goal; and
choose verbal and body language that will help reduce or remove those barriers to success.
Based on this author’s 14 y of radiation communication experience, the best tools for reducing high stress, doubt, and fear are compassion, validation, and commitment: compassion for the audience as individuals, validation of their feelings, and commitment to their cause.
While similar to the Conviction/Compassion/Optimism Concept, the increased emphasis on validation stems from the value individuals place on simply having someone acknowledge their feelings as real and reasonable (Feil 1993: Peters et al. 1997: Hall 2012: Hyer and Covello 2017). A 2014 study used magnetic resonance imaging to study the brain when people perceived their feelings were understood, and when they perceived their feelings were not understood. When participants didn’t feel understood the part of the brain associated with negative affect was activated. When participants felt understood the part of the brain associated with reward and social connection was activated (Morelli et al. 2014).
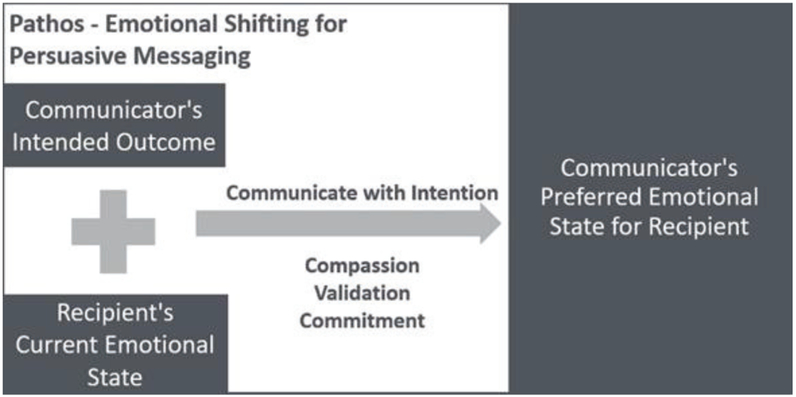
Validating feelings is a very powerful tool for scientists because you can validate a person’s feelings even if the science says that the feelings are unwarranted. When a person feels understood, they are more likely to hear what you have to say because you took the time to understand them. Put simply, “people want to know that you care before they care what you know’’ (WHO 2005). Fig. 1 illustrates effective use of pathos.
Fig. 1.
Simple method for assessing a situation and employing communication techniques to move an information recipient to a preferred emotional state.
LOGOS — LOGTC TN COMMUNTCATTNG RADTATTON INFORMATION
“But all the authority and empathy in the world won’t really help you if people don’t understand what you’re talking about” (Edinger 2013). Logos is about building a logical argument. The most important part to remember about logos is that it isn’t your logic that is important. If you have ethos (credibility), fundamentally people trust that you know what you are talking about. The challenge is figuring out how to effectively communicate your logic and reasoning to the person on the receiving end of the information.
Communicating radiation information is difficult because members of the public do not know if 1 mSv or 10,000 mSv is bad for their health. The unfamiliarity with radiation is one of many reasons that the public perceives radiation exposure as a high-risk scenario whether or not the concern is scientifically warranted (Covello and Sandman 2001; Hyer and Covello 2017). What the public wants to know is “Will I be safe?,” “How concerned should I be?,” and “Will I get cancer?.” When it comes to radiation, the answers to these questions are not black and white. Scientifically, the most accurate answer is probably “It depends.” But “it depends” is not a satisfactory answer to people concerned about their health. Based on experience and common sense, “it depends” leads to increased confusion and more fear — once again hindering your ability to communicate.
One of our greatest opportunities for improving radiation communication is on the topic of uncertainty at low doses. As a radiation community we need to adjust our message for our audience’s knowledge level. We lose credibility when we talk to members of the public, who typically have little knowledge about radiation, like we talk with other members of the professional community.
In 2017, the Journal of Radiological Protection published an article titled “LRPA consultation: is the system of protection ‘fit for purpose’ and can it be readily communicated? Views of the radiation protection professionals.” Written for a radiation-literate audience, this document contained the following technical language about explaining uncertainty of risk at low doses:
“At the dose levels of particular interest it means that the risk of radiation, assuming that there is a risk, is sufficiently low that we have not been able to detect it. However, this should be balanced with the concept that ‘absence of evidence is not necessarily evidence of absence’, and that whilst we have not been able to detect radiation risks around the levels of natural background exposure there are some theoretical reasons to believe that a risk could be present, although at levels that would generally be regarded as very low and which would be undetectable.”
Later in the article—again for a technical audience—the article summarizes what we know about uncertainty at low doses by saying . .whilst we don’t know everything, we do know that at the most relevant exposure levels the risk is bounded and must be quite small, otherwise we would be able to detect it” (Coates and Czarwinski 2018).
When explaining the concept of uncertainty of risk at low doses, is there a way to simplify the language even further for a concerned member of the public? This author would like to propose the following language:
The risk of cancer at low doses is so small that we can’t detect it.
But no one wants to get cancer.
So, we keep radiation doses as low as possible to limit even these small risks.
The radiation community typically discusses cancer risk as a statistical probably, like ×/10,000 or ×/100,000. Try and picture 100,000 people. You know it is a large number, but it may be difficult to visualize because it is beyond what we typically experience in daily life. Numbers around 100 are easier to comprehend because we experience it on a human scale (e.g., a wedding) (Garcia-Retamero and Galesic 2011; Dahlstrom 2014). If we must use large denominators, using examples like the number of people it takes to fill a college or professional football stadium may help put that large denominator in context.
When talking about radiation it is important to remember the person on the other end of that communication. To guide your messaging choices, ask yourself who are you addressing, what are their concerns, what is their technical understanding, and what do they need to know to make informed decisions.
STORYTELLING IN COMMUNICATING RADIATION INFORMATION
The radiation community typically conveys facts when talking about the science and risk of radiation. Presenting facts allows for complete accuracy in the information provided. But are facts the best way to convey information to people who are concerned and need to make informed decisions? Aristotle didn’t think so when he wrote “.. .even if we possessed the most accurate scientific knowledge, we should not find it easy to persuade them by the employment of such knowledge. For scientific discourse is concerned with instruction, but in the case of such persons instruction is impossible; our proofs and arguments must rest on generally accepted principles…’’ (Aristotle et al. 1954)
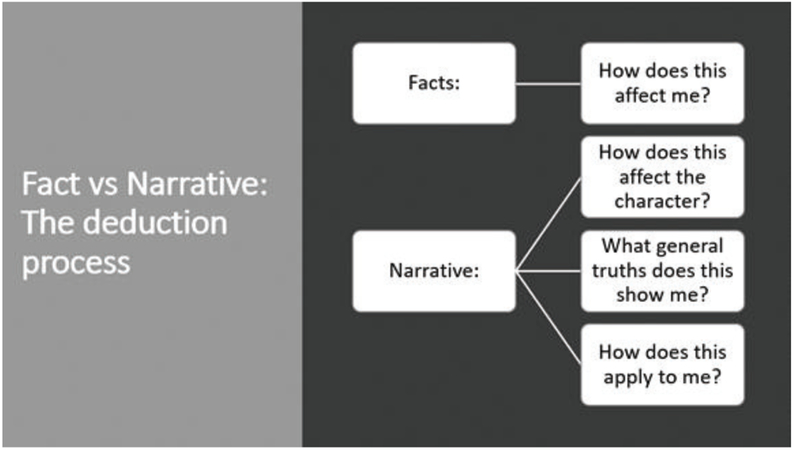
Comprehending facts is a one step process: Does this fact apply to me? Comprehending stories makes the receiver go through a series of deductions to determine if and how the story applies personally. A story or a narrative provides a relatable depiction of an individual experience. This allows the consumer of the information to empathize with the characters, analyze the story, and draw personal connections to how the story applies to his or her life (Altmann et al. 2014; Dahlstrom 2014). Fig. 2 shows the difference in the deduction process when receiving facts versus being told a narrative. Studies have even found that information threaded into a storyline requires less cognitive resources to comprehend (Fisch 2000; Dahlstrom 2010, 2012). Using stories to convey information may be helpful in high-stress situations when cognitive function is impaired.
Fig. 2.
Facts vs. narrative: differences in the deduction process.
Turn on your radio or television news station and you will hear scientific and medical information told through stories all the time. Reporters find one person whose story evokes emotion and epitomizes the scientific or health information they want to convey. Narratives are effective; indeed, studies and experience have found they can rarely be countered by facts (McComas and Shanahan 1999). The anti-vaccination movement in America is an excellent example of how stories that evoke empathy can outweigh facts (Frenkel 2017; Gebelhoff 2018).
Understanding the power of stories, the radiation community should examine where, if at all, there is a place for storytelling in describing radiation risk. For example, after establishing credibility and reducing stress, a doctor could tell a story about a person who had a statistically typical reaction to a procedure. Using case studies may be a useful tool for conveying health risks.
CONCLUSION
Effective radiation communication with the public doesn’t just happen. The process of communicating with intention needs to be taught and practiced. Professional communicators are taught social skills, the importance of body language, ways to show empathy, and how to structure a persuasive argument. Physicians and health physicists are not given in-depth, if any, communication training, yet they are expected to provide professional, quality information to people concerned about their health. As important as it is that the radiation community continues to talk about the importance of good communication, it is equally important to start practicing proven communication techniques.
A simple way to improve radiation communication is to take an active interest in the person on the receiving end. To help you (1) understand how your audience prefers to get their information, (2) identify your intended outcome, and (3) decide on the communication techniques that will be most effective, here are a few questions to ask your audience:
How can I help?
What do you know about the topic?
Who is involved in the decision making? (Remember, most pediatric patients have two caregivers that may have different information preferences.)
What information can I provide that would be most useful to you? Most useful to any joint decision maker?
How do you like to get your information? Verbal? In writing? References? Case Studies?
When faced with an ailing patient, doctors usually have several options for diagnosis and treatment of disease. But doctors consider many factors (i.e., patient age, size, current medication, previous medical history, course of disease) before deciding on a course of action. Similarly, radiation experts need to have a set of tools available for effective communication. Once the tools are available, radiation experts can select the best communication tools based on the information needs, emotional state, and knowledge base of the audience. In other words, for effective radiation risk communication we need to personalize communication like we personalize medical diagnosis and treatment.
REFERENCES
- Altmann U, Bohrn IC, Lubrich O, Menninghaus W, Jacobs AM Fact vs fiction—how paratextual information shapes our reading processes. Soc Cogn Affect Neurosci 9(1):22–29; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aristotle, Roberts WR, Bywater I, Solmsen F Rhetoric. New York: Modern Library; 1954. [Google Scholar]
- Association of State and Territorial Health Officials. Communicating in risk situations. Washington, DC: ASTHO; 2002. [Google Scholar]
- Coates R, Czarwinski R. IRPA consultation: is the system of protection ‘fit for purpose’ and can it be readily communicated? Views of the radiation protection professionals. J Radiol Prot 38:440–455; 2018. [DOI] [PubMed] [Google Scholar]
- Covello VT. Strategies for overcoming challenges to effective risk communication In: Heath RL, O’Hair HD, eds. Handbook of risk and crisis communication. New York: Routledge Taylor and Francis Group; 2009; 143–154. [Google Scholar]
- Covello VT. Risk communication, radiation, and radiological emergencies: strategies, tools and techniques. Health Phys 101:511–530; 2011. [DOI] [PubMed] [Google Scholar]
- Covello VT, Milligan PA. Radiological risk and emergency communications 2010 NRC Regulatory Information Conference. Bethesda, MD: U.S. Nuclear Regulatory Commission; 2010. [Google Scholar]
- Covello V, Sandman PM. Risk communication: evolution and revolution In: Solutions to an environment in peril. Baltimore, MD: John Hopkins University Press; 2001; 164–178. [Google Scholar]
- Dahlstrom MF. The role of causality in information acceptance in narratives: an example from science communication. Commun Res 37(6):857–875; 2010. [Google Scholar]
- Dahlstrom MF. The persuasive influence of narrative causality: Psychological mechanism, strength in overcoming resistance, and persistence over time. Media Psychol 15(3):303–326; 2012. [Google Scholar]
- Dahlstrom MF. Using narratives and storytelling to communicate science with nonexpert audiences. PNAS 111(Suppl 4): 13614–13620; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger S Three elements of great communication, according to Aristotle Boston, MA: Harvard Business Review; (January 17); 2013. [Google Scholar]
- Feil N The validation breakthrough: simple techniques for communicating with people with "Alzheimer’s-type dementia." Baltimore, MD: Health Professions Press; 1993. [Google Scholar]
- Fisch SM. A capacity model of children’s comprehension of educational content on television. Media Psychol 2(1):63–91; 2000. [Google Scholar]
- Frenkel S She warned of ‘peer-to-peer misinformation’ Congress listened. Available at: https://www.nytimes.com/2017/11/12/technology/social-media-disinformation.html. Accessed 12 June 2018 New York: New York Times; (November 12); 2017. [Google Scholar]
- Garcia-Retamero R, Galesic M. Using plausible group sizes to communicate information about medical risks. Patient Educ Coun 84(2):245–250; 2011. [DOI] [PubMed] [Google Scholar]
- Gebelhoff R The anti-vaccine movement shows why Facebook is broken. Available at: https://www.washingtonpost.com/blogs/post-partisan/wp/2018/01/09/the-anti-vaccine-movement-shows-why-facebook-is-broken/?noredirect=on&utm_term=.f68719092b0e. Accessed 12 June 2018 Washington, DC: The Washington Post; (January 9); 2018. [Google Scholar]
- Hall K Understanding validation: a way to communicate acceptance [online]. Available at: https://www.psychologytoday.com/us/blog/pieces-mind/201204/understanding-validation-way-communicate-acceptance. Accessed 12 June 2018 Psychol Today (April 26); 2012. [Google Scholar]
- Hyer RN, Covello VT. Breaking bad news in the high-concern, low trust setting: how to get your story heard. Health Phys 112(2):111–115; 2017. [DOI] [PubMed] [Google Scholar]
- McComas K, Shanahan J. Telling stories about global climate change: measuring the impact of narratives on issue cycles. Commun Res 26(1):30–57; 1999. [Google Scholar]
- Morelli SA, Torre JB, Eisenberger NI The neural bases of feeling understood and not understood. Soc Cogn Affect Neurosci 9(12): 1890–1896; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters RG, Covello VT, McCallum DB. The determinants of trust and credibility in environmental risk communication: an empirical study. Risk Anal 17(1):43–54; 1997. [DOI] [PubMed] [Google Scholar]
- South Palomares JK, Young AW. Facial first impressions of partner preference traits: trustworthiness, status, and attractiveness. Soc Psychol Personality Sci 2017; 10.1177/1948550617732388. [DOI] [Google Scholar]
- Willis J, Todorov A. First impressions: making up your mind after a 100-ms exposure to a face. Psychol Sci 17(7):592–598; 2006. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Effective media communication during public health emergencies: a WHO field guide. Geneva: WHO: 2005. [Google Scholar]