Significance Statement
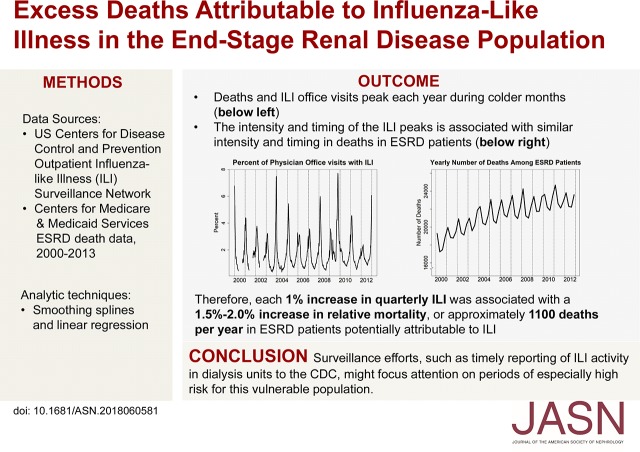
The seasonality of influenza activity contributes to seasonal patterns in morbidity and mortality, particularly among vulnerable populations such as patients with ESRD. However, the relationship between seasonal fluctuations of influenza-like illness (ILI), which encompasses a wide range of respiratory infections, and seasonal patterns of mortality in patients with ESRD has not been explicitly examined. Using data from a Centers for Disease Control and Prevention (CDC) ILI surveillance network and the Medicare ESRD database, the authors found that community ILI activity is associated with seasonal variation in mortality among patients with ESRD, and likely contributes to >1000 deaths per year. Greater emphasis on surveillance efforts, such as timely reporting to the CDC of ILI activity within dialysis units, and study of treatment and containment strategies during high-risk periods, may be warranted.
Keywords: ESRD, influenza, influenza-like illness, mortality
Visual Abstract
Abstract
Background
Morbidity and mortality vary seasonally. Timing and severity of influenza seasons contribute to those patterns, especially among vulnerable populations such as patients with ESRD. However, the extent to which influenza-like illness (ILI), a syndrome comprising a range of potentially serious respiratory tract infections, contributes to mortality in patients with ESRD has not been quantified.
Methods
We used data from the Centers for Disease Control and Prevention (CDC) Outpatient Influenza-like Illness Surveillance Network and Centers for Medicare and Medicaid Services ESRD death data from 2000 to 2013. After addressing the increasing trend in deaths due to the growing prevalent ESRD population, we calculated quarterly relative mortality compared with average third-quarter (summer) death counts. We used linear regression models to assess the relationship between ILI data and mortality, separately for quarters 4 and 1 for each influenza season, and model parameter estimates to predict seasonal mortality counts and calculate excess ILI-associated deaths.
Results
An estimated 1% absolute increase in quarterly ILI was associated with a 1.5% increase in relative mortality for quarter 4 and a 2.0% increase for quarter 1. The average number of annual deaths potentially attributable to ILI was substantial, about 1100 deaths per year.
Conclusions
We found an association between community ILI activity and seasonal variation in all-cause mortality in patients with ESRD, with ILI likely contributing to >1000 deaths annually. Surveillance efforts, such as timely reporting to the CDC of ILI activity within dialysis units during influenza season, may help focus attention on high-risk periods for this vulnerable population.
Seasonal variation in morbidity and mortality has long been a subject of scientific investigation, with some studies reported almost a century ago.1–4 In the 1960s and 1970s, the seasonal pattern in mortality from cardiovascular causes was a particular focus of study.3,5 Because cardiovascular-related and other deaths were more frequent during winter, ambient temperature was initially proposed as the putative mechanism,5 but investigators soon hypothesized a link between the seasonal incidence of respiratory diseases and certain causes of mortality.3 In the ensuing decades, a wealth of reports suggested that influenza, the archetypal seasonal respiratory infectious disease, was associated with morbidity and mortality.6–10 Changes in the inflammatory milieu may be partly responsible for a putative link between influenza and mortality,11 but this remains insufficiently understood.
Influenza is not the only infectious agent responsible for serious respiratory tract infections. A syndrome known as influenza-like illness (ILI), defined by the US Centers for Disease Control and Prevention (CDC) as a fever higher than 37.8°C plus a cough and/or sore throat, can develop in response to infection with a wide range of agents, including influenza, respiratory syncytial virus, rhinovirus, coronavirus, adenovirus, parainfluenza, and many others.12,13 ILI is of sufficient public-health importance that the CDC closely monitors its epidemiology.14
Seasonal variation in mortality in patients receiving hemodialysis was recently described,15–17 but the underlying mechanism for these patterns has not been elucidated. Seasonal variation in mortality in patients with ESRD could be linked to the seasonality of ILI activity, but to our knowledge has never been examined explicitly. We hypothesized that seasonal fluctuations in ILI activity would be reflected in corresponding changes in the patterns of death in patients with ESRD treated with dialysis or kidney transplant.
Methods
Data Sources and Study Population
We used data from the US Outpatient Influenza-like Illness Surveillance Network (ILINet), a mechanism by which the CDC monitors influenza and ILI activity.14 This network comprises over 2700 health care providers in the United States, encompassing over 30 million patient visits each year. Weekly data on physician visits and ILI activity in the community (defined as the percentage of patient visits to health care providers for ILI) are reported to the CDC, including numbers of patients, by age. These data result in estimates of the percentage of visits to health care providers because of ILI, and are reported nationally and locally.
We used the Centers for Medicare & Medicaid Services (CMS) ESRD data from 2000 to 2013 to calculate total numbers of deaths among patients with ESRD by quarter, from the fourth quarter (Q4) of 2000 to Q4 of 2012. Death information was obtained from the ESRD Death Notification (form CMS-2746), which is submitted to the CMS within 30 days of a death. These data were supplemented with information from the CMS enrollment database, inpatient claims, and the Social Security Death Master File.
Statistical Analyses
Assessing the association between ILI incidence and mortality required the following: (1) addressing secular changes in the size of the ESRD population between 2000 and 2012, and selecting a reference standard against which we could compare seasonal mortality counts; (2) addressing comparability of time intervals in the CDC and ESRD data; (3) assessing the relation between the CDC ILI data and mortality; (4) predicting seasonal mortality counts; and (5) estimating the number of deaths potentially associated with changes in ILI. Below we outline how we handled each of these problems.
To address secular changes in the size of the prevalent ESRD population (the “denominator population”), which increased by 62% over the study period, and the associated change in the death rates over this period, we fit a cubic smoothing spline to the yearly death counts for the third quarter (Q3) of each year from 2000 to 2012. The “smoothness” of the resulting line is determined by a smoothing parameter ranging from 0 (linear fit between each point) to 1 (least squares linear fit through all points); a value of 0.6 was chosen by visual inspection to allow for minor nonlinearity. We chose Q3 as our reference standard because the lowest number of deaths typically occur over the summer, and it is a period when relatively less ILI circulates in the community. Next, we divided each quarter’s deaths by the estimated number of deaths from the smoothed spline function, resulting in a series of values that measured the relative discrepancy from the underlying time trend across Q3 of each year from 2000 to 2012. We then subtracted 1 from each value and multiplied by 100. The resulting values represent quarterly relative mortality, expressed as percent increase (or decrease) compared with the average Q3 death counts, after removal of the death trend due to the annual increase in the prevalent ESRD population.
Second, we aggregated the weekly ILI data into quarters. An average quarterly ILI burden was estimated by averaging the national weekly ILI estimates derived from the CDC from 2000 to 2012. ILI estimates during July to September were not collected from 2000 to 2002, so values were imputed from the average of the remaining nonmissing Q3s.
Third, to assess the relationship between the CDC ILI data and mortality, we used Q4 of each year and the first quarter (Q1) of the following year (the influenza season) to create regression models to predict Q4 and Q1 deaths using Q4 and Q1 ILI estimates. We then used these models to predict seasonal mortality counts and calculate excess deaths associated with ILI for each influenza season. To do so, we estimated two linear regression models: (1) a regression of Q4 relative mortality on Q4 ILI, and (2) a corresponding regression of Q1 relative mortality on Q1 ILI. These models generated predicted change in relative mortality (as a percentage of average Q3 mortality) for a one-unit absolute (as opposed to relative) percentage point change in ILI incidence, separately for Q4 and Q1. Predicted death counts for Q4 and Q1 were obtained by multiplying the estimated number of deaths from the smoothed spline function (representing average Q3 mortality counts after removing trend) by 1 plus the regression-predicted percent change in relative mortality. Finally, we estimated the number of deaths associated with an increase (or decrease) in ILI values each year, by first subtracting the average summer (Q3) ILI percentage from each Q4 and Q1 ILI percentage. We then multiplied each resulting Q4 and Q1 ILI value by the appropriate parameter estimates from the regression models and, in the final step, multiplied these estimates by the smoothed spline values (representing average number of Q3 deaths) to give an estimate of the number of “excess” deaths associated with ILI for each season.
To test the robustness of our findings, we performed two separate sensitivity analyses. First, we assessed the effect of adding estimates of the percentage of patients with ESRD who received the influenza vaccination from 2000 to 2012 (US Renal Data System reference tables 2012, 2013, and 2014; https://www.usrds.org/archive.aspx). Second, we assessed the effect of adding estimates of influenza vaccine effectiveness (https://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm) to our regression models for Q4 and Q1. Because estimates of vaccine effectiveness were available only beginning in 2004, we limited the vaccine effectiveness models to 2004–2012.
Results
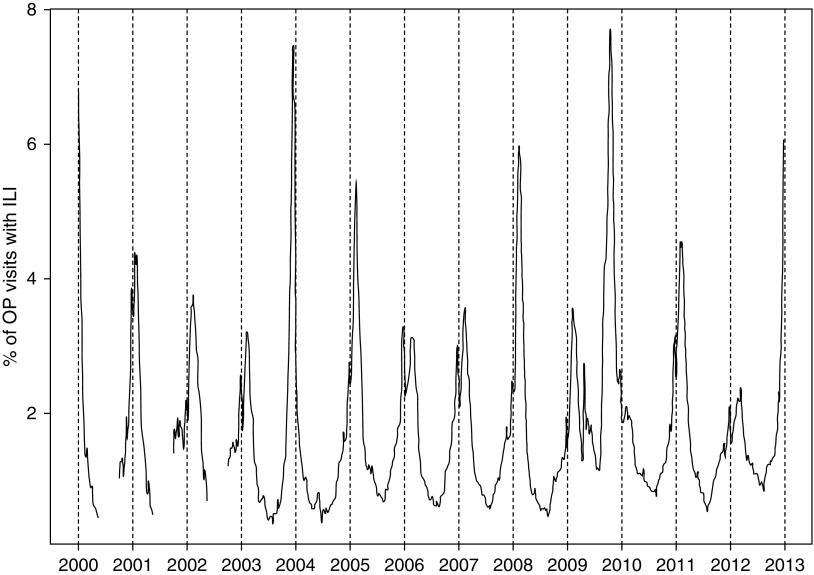
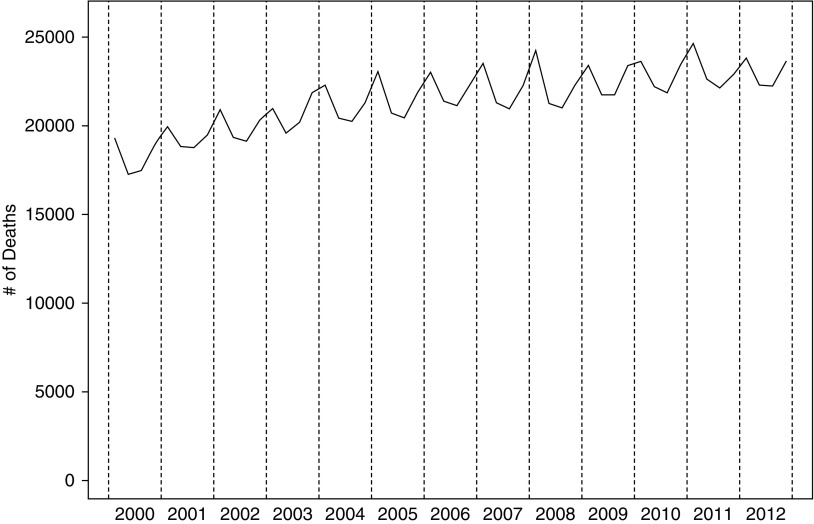
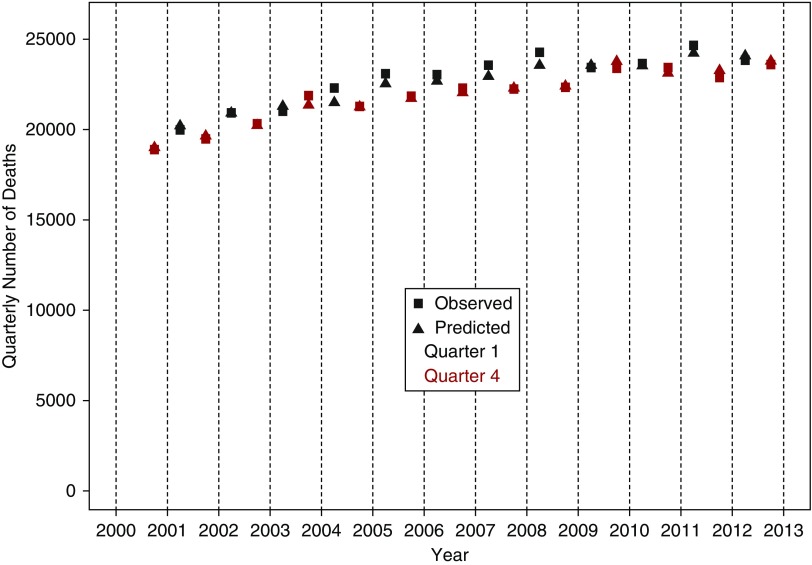
The pattern of ILI activity over time is shown in Figure 1, illustrating the known strong seasonality. The overall trend in quarterly deaths among patients with ESRD, 2000–2012, is shown in Figure 2. The annual increase in the number of deaths is largely due to the overall increase of the ESRD population, from 390,158 in 2000 to 678,383 in 2014.18 Figure 2 also illustrates how death counts vary by season, with the highest death counts in Q1 and the lowest in Q3.
Figure 1.
The intensity and timing of outpatient visits for influenza-like illness vary year to year. CDC percentage of outpatient visits for influenza-like illness. OP, outpatient.
Figure 2.
Death counts among patients with ESRD are seasonal, with higher counts during colder months. Quarterly death counts among patients with ESRD, 2000–2013.
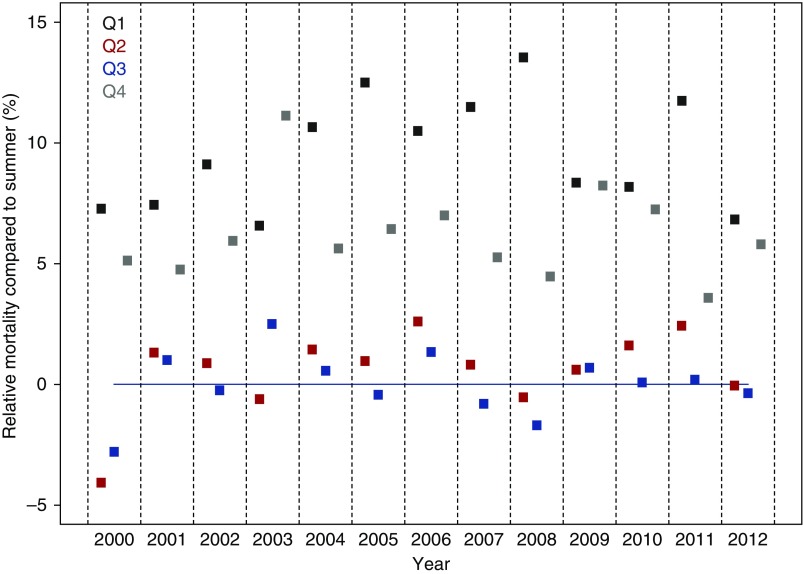
Relative seasonal mortality, or the mortality in a given calendar quarter relative to the referent group (in this case, the Q3 average after removing the underlying increasing trend), is shown in Figure 3. Each quarter’s value can be considered the relative mortality compared with the average summer (Q3) mortality, expressed as a percentage. Q4 (Q4year, blue) and Q1 (Q1year+1, black) correspond to each influenza season, and demonstrate higher relative mortality than for quarter 2 and Q3 for each year examined. In most cases, relative mortality was highest in Q1. In some years, relative mortality was similar for Q4year and Q1year+1. Regression models for Q4 and Q1 estimated that a 1% absolute increase in Q4 ILI was associated with a 1.5% (95% confidence interval, 0.6% to 2.4%) increase in Q4 relative mortality (relative to the average Q3 death count), and that a 1% absolute increase in Q1 ILI was associated with a 2.0% (95% confidence interval, 0.2% to 3.9%) increase in Q1 relative mortality.
Figure 3.
After standardizing death counts to “average summer,” the intensity and timing of death counts among patients with ESRD become apparent. Relative quarterly mortality, by quarter, compared with Q3, after accounting for death trends over time.
Observed versus predicted death counts for Q4 and Q1 for each year (Figure 4) indicated relatively good prediction of the death counts from the ILI values. The mean absolute difference between observed and predicted counts was 211 and 306 deaths for Q4 and Q1, respectively.
Figure 4.
Predicted death counts among patients with ESRD are relatively close to observed death counts. Observed versus predicted death counts in the fall (Q4) and winter (Q1) among patients with ESRD, 2000–2013.
Annual deaths potentially attributable to ILI (Table 1) averaged >1000 (average Q4 deaths, 341; average Q1 deaths, 711; total, 1052), and ranged from a minimum of 633 (2011–2012) to a maximum of 1604 (2009–2010). Notable influenza seasons with respect to distribution of deaths in Q1 versus Q4 were 2003–2004 and 2009–2010, when most ILI activity occurred in Q4, with resulting low ratios of 0.26 and 0.34, respectively. Regarding total number of excess deaths, the highest seasons were, in decreasing order, 2009–2010 (1604 total deaths), 2007–2008 (1441 total deaths), and 2010–2011 (1348 total deaths).
Table 1.
Quarterly ILI percent and relative mortality percent, and estimated excess deaths, by influenza season
| Influenza Season | Q4 | Q1 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Relative Mortality | Relative Mortality | Total | Q1/Q4 Excess | ||||||
| ILI Percent | Percent | Excess Deaths | ILI Percent | Percent | Excess Deaths | Excess Deaths | 95% CI | Death Ratioa | |
| 2000–2001 | 1.76 | 5.12 | 221 | 2.84 | 7.44 | 690 | 911 | 141 to 1681 | 3.12 |
| 2001–2002 | 1.75 | 4.75 | 226 | 2.93 | 9.10 | 747 | 973 | 148 to 1799 | 3.31 |
| 2002–2003 | 1.60 | 5.94 | 190 | 2.39 | 6.57 | 563 | 753 | 119 to 1387 | 2.96 |
| 2003–2004 | 3.57 | 11.11 | 770 | 1.43 | 10.65 | 198 | 968 | 323 to 1610 | 0.26 |
| 2004–2005 | 1.58 | 5.61 | 194 | 3.47 | 12.49 | 1029 | 1223 | 157 to 2290 | 5.30 |
| 2005–2006 | 1.85 | 6.42 | 279 | 2.67 | 10.49 | 718 | 997 | 167 to 1829 | 2.57 |
| 2006–2007 | 1.78 | 7.00 | 262 | 2.69 | 11.48 | 737 | 999 | 162 to 1839 | 2.81 |
| 2007–2008 | 1.59 | 5.25 | 206 | 3.84 | 13.53 | 1235 | 1441 | 178 to 2708 | 6.00 |
| 2008–2009 | 1.24 | 4.47 | 98 | 2.51 | 8.33 | 679 | 777 | 91 to 1464 | 6.93 |
| 2009–2010 | 4.67 | 8.24 | 1196 | 1.87 | 8.17 | 408 | 1604 | 510 to 2697 | 0.34 |
| 2010–2011 | 1.80 | 7.24 | 281 | 3.36 | 11.74 | 1067 | 1348 | 195 to 2505 | 3.80 |
| 2011–2012 | 1.47 | 3.58 | 176 | 1.96 | 6.82 | 457 | 633 | 106 to 1162 | 2.60 |
95% CI, 95% confidence interval.
Ratio of Q1 excess deaths to Q4 excess deaths.
When the percentage of patients with ESRD vaccinated and vaccine effectiveness were added, separately, to the Q4 and Q1 models, the ILI parameter estimates changed little (<10% and <5%, respectively); corresponding P values for percentage vaccinated and vaccine effectiveness were nonsignificant.
Discussion
Seasonal variability of health events and outcomes has long been established in the general population and is increasingly recognized as an important phenomenon in patients with kidney disease, including those receiving dialysis.15–17 The duration and intensity of influenza seasons have been identified as contributors to this seasonal increase in health risks,6–8,19–23 especially among vulnerable populations, such as patients with ESRD, in whom the effectiveness of influenza vaccinations is reduced.24–27 However, the contribution of ILI to mortality in the ESRD population has not specifically been quantified. Given that viral infections are likely associated with hospitalizations and death attributed to ostensibly noninfectious causes, we hypothesized that seasonal patterns in ILI might be associated with mortality in patients with ESRD. Using detailed information collected by the CDC on ILI combined with quarterly mortality data for patients with ESRD, we found an association between severity and timing of ILI activity and mortality. The estimated excess mortality was substantial, averaging approximately 1100 deaths, or approximately 2.4% of all deaths per influenza season. These findings suggest that protection against, surveillance of, and, where possible, treatment of infections due to influenza and related viral respiratory illnesses may constitute an opportunity to reduce deaths in patients with ESRD.
Influenza and, more generally, ILI-related mortality disproportionately affect vulnerable populations such as the elderly, those with chronic diseases, and those characterized by immunocompromised states.28–30 Patients with ESRD constitute just such an at-risk population for a variety of reasons. First, they often have multiple high-risk comorbid conditions, including diabetes mellitus, cardiac diseases, and pulmonary diseases,31,32 reducing “physiologic reserve”33 in the setting of acute medical stressors. Second, they generally have reduced immunologic function, in the form of impaired T cell–mediated immunity, B cell (humoral) immunity, antigen presentation by dendritic cells, and impaired phagocytic and function in cells of mononuclear origin.34 An additional contribution to impaired immunologic function is the state of chronic inflammation that characterizes patients receiving maintenance dialysis.35 Third, close proximity to others who have viral illnesses for prolonged periods of time, as typically occurs in thrice-weekly in-center maintenance hemodialysis, is a risk factor for diseases transmitted via respiratory droplets.
If ILI meaningfully contributes to excess deaths in the ESRD population, as this study suggests, greater emphasis on monitoring, prevention (when possible), and treatment may be warranted. The CDC ILINet36 tracks and provides timely reports of ILI incidence in the general population. ILIs reflect a set of symptoms that may be caused by a wide array of viruses, including rhinovirus, adenovirus, respiratory syncytial virus, parainfluenza virus, and human metapneumovirus, as well as influenza (which could account for 10%–50% of all ILI37–39). Any or all of these viruses may be associated with poor outcomes in chronically ill populations, such as the ESRD population. The nephrology community should consider the potential merits of tracking ILI within individual dialysis units, in a fashion analogous to that undertaken by the CDC in primary care practices nationwide. This type of surveillance initiative might provide dialysis unit–specific data on ILI incidence, which could be used to conduct epidemiologic studies, guide quality improvement efforts (e.g., isolating patients with suspected ILI within dialysis units), and ultimately, inform disease-management strategies.
Prevention is a challenging issue because most ILI is not influenza. Even in the case of influenza, only about two thirds of patients on dialysis receive the vaccination annually,40,41 and further, the vaccine appears to be substantially less effective in this population.40 Unfortunately, although the CDC recommends influenza vaccinations for patients with CKD,42 the optimal vaccination strategy is unknown.43 For example, immunity resulting from single-dose vaccines may wane before the end of an influenza season, leading to suggestions that patients on dialysis should receive high-dose or adjuvanted influenza vaccines.44,45 Given that vaccines have not been developed for the majority of viruses responsible for ILI, the nephrology community should expect at most a modest benefit from any dialysis population–wide influenza vaccination program, as well as supporting future efforts to explore the immune response to vaccinations in such patients.
Treatment and containment approaches could entail, first, on-site rapid detection and identification of influenza and other ILIs in patients receiving maintenance dialysis, followed by physical isolation of the affected patient within the dialysis unit. In addition to potentially hastening treatment for ILI among those affected, use of protective barriers (e.g., masks) and greater discipline in comprehensive disinfection of the dialysis station might prevent the spread of viral upper respiratory infections. Such interventions, if successfully implemented, might confer benefits well beyond those associated solely with mortality. Reduction in community-wide ILI burden might reduce morbid events and hospitalizations, especially for patients at risk for cardiopulmonary events such as acute myocardial infarction or exacerbations of chronic obstructive pulmonary disease or asthma.7,46–48
These findings have potential implications for epidemiologic and health services studies designed to evaluate clinical outcomes over time. The variability in timing and severity of each influenza season (and resulting ILI incidence) can affect morbidity and mortality events, and investigators should consider accounting for ILI in their analyses.49
This study should be evaluated in light of the following limitations. We used an ecologic study design owing to the sources of exposure (CDC ILINet) and death (ESRD) data included in the analysis. As such, the opportunity for residual confounding cannot be ruled out. Our measure of mortality was on the basis of total quarterly death counts and did not take into consideration cause of death. Possibly, some causes of death that may occur more frequently in colder months could be unrelated to ILI; for example, falls resulting in severe fractures that lead to death or other trauma-related deaths. We elected to perform an analysis using quarters because of uncertainty in the temporal relationship between ILI infection and various causes of death. As a result, our aggregation of ILI data and mortality data into quarterly measurements lacks fine granularity. Finally, although these data may be the best source of ILI information available, they may not accurately reflect actual ILI incidence, particularly at local or regional levels. Because behavior and activity patterns of patients with ESRD likely vary somewhat from those of the general population, patterns of exposure to ILI might differ in patients with ESRD relative to community-dwelling individuals with intact kidney function.
In summary, we found evidence that community ILI activity is associated with seasonal variation in all-cause mortality in patients with ESRD. Surveillance efforts, such as near real-time reporting of ILI activity to the CDC, may be useful in focusing attention on periods of high risk for this vulnerable population.
Disclosures
K.J.R. is employed by Research Triangle Institute. G.M.C. has received a research grant and consulting fees from Amgen. B.D.B. owns stock in, and is employed by Amgen. M.A.B. has received research grants from Amgen and AstraZeneca, has ownership or partnership in NoviSci, and has received consulting fees from AbbVie, Amgen, Merck, RxAnte, CERobs, Genentech, Outcomes Insight, and TargetPharma. J.L. has received consulting fees from Fibrogen. W.C.W. has received consulting fees from Akebia, Amgen, AstraZeneca, Bayer, Daichii-Sankyo, Fibrogen, Relpysa, Vifor FMC Renal Pharma, and ZS Pharma. T.S. has received research grants (National Institute on Aging: R01/R56 AG023178, AG056479); owns stock in Novartis, Roche, BASF, AstraZeneca, and Novo Nordisk; and is involved in the Center for Pharmacoepidemiology, whose current members are GlaxoSmithKline, UCB BioSciences, Merck, and Shire. K.L.M. owns stock in, and is employed by Amgen. C.A.H. has received a research grant from Amgen and consulting fees from AstraZeneca and Fibrogen. A.J.C. has received consulting fees from Fibrogen and is employed by NxStage. D.T.G., A.A., and J.B.W. declare no conflicts of interest.
The authors thank Chronic Disease Research Group colleagues Anne Shaw, for assistance with manuscript preparation, and Nan Booth, MSW, MPH, ELS, for assistance with manuscript editing.
Acknowledgments
D.T.G., K.J.R., M.A.B., J.L., and J.B.W. made substantial contributions to conception and design. D.T.G., K.J.R., G.M.C., B.D.B., M.A.B., J.L.,W.C.W., T.S., K.L.M., C.A.H., A.A., A.J.C., and J.B.W. made substantial contributions to analysis and interpretation of data. D.T.G. and J.B.W. drafted the article, and K.J.R., G.M.C., B.D.B., M.A.B., J.L., W.C.W., T.S., K.L.M., C.A.H., A.A., and A.J.C. revised it critically for important intellectual content. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
This work was supported by Amgen, Inc., Thousand Oaks, California. The contract provides for the Minneapolis Medical Research Foundation authors to have final determination of manuscript content.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Collins SD: Public health weekly reports for November 11, 1932. Public Health Rep 47: 2159–2189, 1932 [PMC free article] [PubMed] [Google Scholar]
- 2.Bean WB, Mills CA: Coronary occlusion, heart failure, and environmental temperatures. Am Heart J 16: 701–713, 1938 [Google Scholar]
- 3.Anderson TW, Le Riche WH: Cold weather and myocardial infarction. Lancet 1: 291–296, 1970 [DOI] [PubMed] [Google Scholar]
- 4.Brookhart MA, Rothman KJ: Simple estimators of the intensity of seasonal occurrence. BMC Med Res Methodol 8: 67, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rose G: Cold weather and ischaemic heart disease. Br J Prev Soc Med 20: 97–100, 1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reichert TA, Simonsen L, Sharma A, Pardo SA, Fedson DS, Miller MA: Influenza and the winter increase in mortality in the United States, 1959-1999. Am J Epidemiol 160: 492–502, 2004 [DOI] [PubMed] [Google Scholar]
- 7.Warren-Gash C, Smeeth L, Hayward AC: Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: A systematic review. Lancet Infect Dis 9: 601–610, 2009 [DOI] [PubMed] [Google Scholar]
- 8.Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR: Acute myocardial infarction and influenza: A meta-analysis of case-control studies. Heart 101: 1738–1747, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simonsen L, Taylor RJ, Viboud C, Miller MA, Jackson LA: Mortality benefits of influenza vaccination in elderly people: An ongoing controversy. Lancet Infect Dis 7: 658–666, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Jackson LA, Jackson ML, Nelson JC, Neuzil KM, Weiss NS: Evidence of bias in estimates of influenza vaccine effectiveness in seniors. Int J Epidemiol 35: 337–344, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Corrales-Medina VF, Madjid M, Musher DM: Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis 10: 83–92, 2010 [DOI] [PubMed] [Google Scholar]
- 12.Monto AS: Epidemiology of viral respiratory infections. Am J Med 112[Suppl 6A]: 4S–12S, 2002 [DOI] [PubMed] [Google Scholar]
- 13.Mahony JB: Detection of respiratory viruses by molecular methods. Clin Microbiol Rev 21: 716–747, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention: Influenza (Flu): Overview of Influenza Surveillance in the United States, 2012. Available at: https://www.cdc.gov/flu/weekly/pdf/overview.pdf. Accessed October 22, 2018
- 15.Usvyat LA, Carter M, Thijssen S, Kooman JP, van der Sande FM, Zabetakis P, et al.: Seasonal variations in mortality, clinical, and laboratory parameters in hemodialysis patients: A 5-year cohort study. Clin J Am Soc Nephrol 7: 108–115, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guinsburg AM, Usvyat LA, Etter M, Xu X, Thijssen S, Marcelli D, et al.: Monitoring Dialysis Outcomes (MONDO) Consortium : Seasonal variations in mortality and clinical indicators in international hemodialysis populations from the MONDO registry. BMC Nephrol 16: 139, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Obi Y, Kalantar-Zadeh K, Streja E, Rhee CM, Reddy UG, Soohoo M, et al.: Seasonal variations in transition, mortality and kidney transplantation among patients with end-stage renal disease in the USA. Nephrol Dial Transplant 32[suppl_2]: ii99–ii105, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Renal Data System: 2016 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2016. Available at: https://www.usrds.org/2016/view/Default.aspx. Accessed October 22, 2018
- 19.Nichol KL, Baken L, Nelson A: Relation between influenza vaccination and outpatient visits, hospitalization, and mortality in elderly persons with chronic lung disease. Ann Intern Med 130: 397–403, 1999 [DOI] [PubMed] [Google Scholar]
- 20.Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt K, Iwane M: Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med 348: 1322–1332, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Nichol KL: Influenza vaccination in the elderly: Impact on hospitalisation and mortality. Drugs Aging 22: 495–515, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E: Effectiveness of influenza vaccine in the community-dwelling elderly. N Engl J Med 357: 1373–1381, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL: Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol 1: 274–281, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rautenberg P, Teifke I, Schlegelberger T, Ullmann U: Influenza subtype-specific IgA, IgM and IgG responses in patients on hemodialysis after influenza vaccination. Infection 16: 323–328, 1988 [DOI] [PubMed] [Google Scholar]
- 25.Cavdar C, Sayan M, Sifil A, Artuk C, Yilmaz N, Bahar H, et al.: The comparison of antibody response to influenza vaccination in continuous ambulatory peritoneal dialysis, hemodialysis and renal transplantation patients. Scand J Urol Nephrol 37: 71–76, 2003 [DOI] [PubMed] [Google Scholar]
- 26.Eiselt J, Kielberger L, Rajdl D, Racek J, Pazdiora P, Malánová L: Previous vaccination and age are more important predictors of immune response to influenza vaccine than inflammation and iron status in dialysis patients. Kidney Blood Press Res 41: 139–147, 2016 [DOI] [PubMed] [Google Scholar]
- 27.Moon SJ, Lee SH, Byun YH, Yun GY, Kim SK, Seong BL, et al.: Risk factors affecting seroconversion after influenza A/H1N1 vaccination in hemodialysis patients. BMC Nephrol 13: 165, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Treanor JJ: CLINICAL PRACTICE. Influenza vaccination. N Engl J Med 375: 1261–1268, 2016 [DOI] [PubMed] [Google Scholar]
- 29.Grohskopf LA, Sokolow LZ, Broder KR, Olsen SJ, Karron RA, Jernigan DB, et al.: Prevention and control of seasonal influenza with vaccines. MMWR Recomm Rep 65: 1–54, 2016 [DOI] [PubMed] [Google Scholar]
- 30.Paules C, Subbarao K: Influenza. Lancet 390: 697–708, 2017 [DOI] [PubMed] [Google Scholar]
- 31.Hemmelgarn BR, Manns BJ, Quan H, Ghali WA: Adapting the Charlson Comorbidity Index for use in patients with ESRD. Am J Kidney Dis 42: 125–132, 2003 [DOI] [PubMed] [Google Scholar]
- 32.Liu J, Huang Z, Gilbertson DT, Foley RN, Collins AJ: An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int 77: 141–151, 2010 [DOI] [PubMed] [Google Scholar]
- 33.McDermid RC, Bagshaw SM: Physiological reserve and frailty in critical illness. In: Textbook of Post-ICU Medicine: The Legacy of Critical Care, edited by Stevens R, Hart N, Herridge M, Oxford, UK, Oxford University Press, 2014, pp. 303–316 [Google Scholar]
- 34.Vaziri ND, Pahl MV, Crum A, Norris K: Effect of uremia on structure and function of immune system. J Ren Nutr 22: 149–156, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carrero JJ, Stenvinkel P: Inflammation in end-stage renal disease--what have we learned in 10 years? Semin Dial 23: 498–509, 2010 [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention: Weekly US Influenza Surveillance Report, 2017. Available at: https://www.cdc.gov/flu/weekly/. Accessed October 22, 2018
- 37.van Beek J, Veenhoven RH, Bruin JP, van Boxtel RAJ, de Lange MMA, Meijer A, et al.: Influenza-like illness incidence is not reduced by influenza vaccination in a cohort of older adults, despite effectively reducing laboratory-confirmed influenza virus infections. J Infect Dis 216: 415–424, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zambon MC, Stockton JD, Clewley JP, Fleming DM: Contribution of influenza and respiratory syncytial virus to community cases of influenza-like illness: An observational study. Lancet 358: 1410–1416, 2001 [DOI] [PubMed] [Google Scholar]
- 39.McDonald SA, van Boven M, Wallinga J: An evidence synthesis approach to estimating the proportion of influenza among influenza-like illness patients. Epidemiology 28: 484–491, 2017 [DOI] [PubMed] [Google Scholar]
- 40.McGrath LJ, Kshirsagar AV, Cole SR, Wang L, Weber DJ, Stürmer T, et al.: Influenza vaccine effectiveness in patients on hemodialysis: An analysis of a natural experiment. Arch Intern Med 172: 548–554, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.US Renal Data System: 2015 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2015. Available at: https://www.usrds.org/2015/view/Default.aspx. Accessed October 22, 2018
- 42.Chi C, Patel P, Pilishvili T, Moore M, Murphy T, Strikas R: Guidelines for Vaccinating Kidney Dialysis Patients and Patients with Chronic Kidney Disease, 2012. Available at: https://www.cdc.gov/dialysis/pdfs/vaccinating_dialysis_patients_and_patients_dec2012.pdf. Accessed October 22, 2018
- 43.Remschmidt C, Wichmann O, Harder T: Influenza vaccination in patients with end-stage renal disease: Systematic review and assessment of quality of evidence related to vaccine efficacy, effectiveness, and safety. BMC Med 12: 244, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mastalerz-Migas A, Steciwko A, Brydak LB: Immune response to influenza vaccine in hemodialysis patients with chronic renal failure. Adv Exp Med Biol 756: 285–290, 2013 [DOI] [PubMed] [Google Scholar]
- 45.Noh JY, Song JY, Choi WS, Lee J, Seo YB, Kwon YJ, et al.: Immunogenicity of trivalent influenza vaccines in patients with chronic kidney disease undergoing hemodialysis: MF59-adjuvanted versus non-adjuvanted vaccines. Hum Vaccin Immunother 12: 2902–2908, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Puig-Barberà J, Natividad-Sancho A, Trushakova S, Sominina A, Pisareva M, Ciblak MA, et al.: Global Influenza Hospital Surveillance Study Group (GIHSN) : Epidemiology of hospital admissions with influenza during the 2013/2014 northern hemisphere influenza season: Results from the global influenza hospital surveillance network. PLoS One 11: e0154970, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pawełczyk M, Kowalski ML: The Role of human parainfluenza virus infections in the immunopathology of the respiratory tract. Curr Allergy Asthma Rep 17: 16, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kwok CS, Aslam S, Kontopantelis E, Myint PK, Zaman MJ, Buchan I, et al.: Influenza, influenza-like symptoms and their association with cardiovascular risks: A systematic review and meta-analysis of observational studies. Int J Clin Pract 69: 928–937, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chertow GM, Liu J, Monda KL, Gilbertson DT, Brookhart MA, Beaubrun AC, et al.: Epoetin alfa and outcomes in dialysis amid regulatory and payment reform. J Am Soc Nephrol 27: 3129–3138, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]