Abstract
Rhupus syndrome, a rare entity, is the co-existence of systemic lupus erythematosus (SLE) with rheumatoid arthritis (RA). It manifests as more RA and less SLE related damages. The duration of the disease is longer than typical RA or SLE. Controversies exist regarding the definition of Rhupus. The incidence of Rhupus in patients with arthritis is 0.01%–0.2% and <2% in patients with connective tissue diseases. However, we report a rare case of rhupus in a 55-year-old lady with polyarthritis and joint deformities of 6 year duration, presenting with features of lupus erythematosus.
Keywords: Rare, rheumatoid arthritis co-existent with lupus erythematosus, rhupus
Introduction
Peter Schur coined the term “rhupus” in 1971 to describe patients who satisfy the criteria for both systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA).[1] Rhupus syndrome is a rare condition and has lesser visceral organ involvement as compared with SLE.[2] The syndrome is manifested by patients coincidentally sharing features of both RA and SLE but cannot be combined as a unique clinical, pathologic, or immunologic syndrome. The exact etiology and triggers of rhupus remain unknown till date with limited studies suggesting the combined role of genetic, immunological, hormonal, and environmental factors in the progression of the disease.[3] It is important to categorically differentiate the patients with rhupus because their therapy and outcome differ from those having RA or SLE alone.[4] Herein, we report one such rare case.
Case Report
A 55-year-old lady presented with symmetric polyarthritis involving multiple small and large joints with deformity of upper limbs for 6 years, dark colored facial rash, and multiple red raised scaly lesions over the upper back and chest of 2 months duration and fever of ten days duration. Polyarthritis was associated with joint swelling, tenderness, and deformities. Patient gave history of the facial rash starting with redness and swelling of the entire face that after ten to fifteen days became dark colored. There was history of appearance of red raised scaly itchy lesions over upper back and chest at the same time that increased in size and number over the next 2 months. There was history of exacerbation of skin lesions on sun exposure. Patient also had moderate to high grade fever since ten days that was intermittent, not associated with chills and rigor and came down with medication. There was no history of recurrent oral ulcers, cough, chest pain, palpitations, pain abdomen, or seizures.
General and systemic examination was essentially normal. Dermatological examination revealed involvement of face including forehead, nose, bilateral malar region, and ears in the form of multiple discrete hyperpigmented plaques [Figure 1]. There was sparing of the nasolabial folds and retro auricular region. The skin over the chest and right shoulder was involved in form of multiple scaly papules and multiple coalescing scaly plaques. Post inflammatory hyperpigmented macules were seen in the areas adjoining the plaques [Figure 2]. Mucosal examination was normal.
Figure 1.

Involvement of face including forehead, nose, bilateral malar region, and ears in the form of multiple discrete, hyperpigmented plaques
Figure 2.

Multiple coalescing scaly plaques present over back
Musculoskeletal examination revealed swelling with associated tenderness in bilateral proximal interphalangeal joints and all large joints.
Investigations revealed normocytic, normochromic anemia, raised ESR and C-reactive protein (24 mg/L), a positive direct Coomb's test, rheumatoid factor positive, microalbuminuria, anti-CCP was positive (30 μ/ml) and normal complement levels. Skin biopsy showed mild focal basal layer degeneration, focal dyskeratotic keratinocytes, and perivascular inflammatory infiltrate in superficial dermis [Figure 3]. DIF was negative for IgG, IgM, C3, and IgA. Other connective tissue disease (CTD) markers including ANA were negative. Radiograph of both hands and wrists showed periarticular osteopenia and early erosions of the base of proximal phalanges of bilateral 2nd digits, features suggesting inflammatory polyarthritis of both hands [Figure 4]. She was diagnosed as a case of Rhupus (Rheumatoid arthritis with SLE) and managed with a short course of oral cortico steroids for her skin lesions, hydroxychloroquine, methotrexate, calcium, and Vitamin D supplementation and bisphosphonates. She has shown dramatic improvement in skin rashes and arthritis and is currently on regular follow-up.
Figure 3.
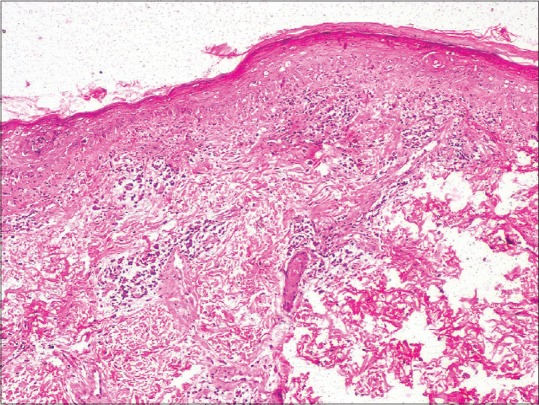
(H and E, ×100). Skin biopsy showed mild focal basal layer degeneration, focal dyskeratotic keratinocytes, and perivascular inflammatory infiltrate in superficial dermis
Figure 4.

Radiograph of both hands and wrists showed periarticular osteopenia and early erosions of the base of proximal phalanges of bilateral 2nd digits
Discussion
Overlap syndromes have been defined as entities satisfying the classification criteria of at least two CTDs occurring at the same or at different times in the same patient. Rhupus is one such condition with the co-existence of SLE and rheumatoid arthritis with a prevalence varying from 0.01% to 2%. Among genetic factors, HLA-DR alleles have been strongly associated with rhupus, being present in nearly 67% of the reported cases.[3,4]
There is a role of the immune system that has been confirmed by the presence of antibodies and immune complexes in serum profile. A glance through the previous case series has revealed the possibility of anti-CCP and C-RP as markers for the diagnosis of rhupus.[3]
RA is a progressive inflammatory autoimmune disease with articular and systemic effects. Its exact cause is unknown, but genetic and environmental factors are contributory. T-cells, B-cells, and the orchestrated interaction of pro-inflammatory cytokines play key roles in the pathophysiology of RA. Predominant role of Th 1 pathway is there with release of cytokines such as IL-17, TNF-α, IL-6, and IL-1, which cause synovial inflammation. However, the exact patho-aetiology of SLE remains elusive. An extremely complicated and multifactorial interaction among various genetic and environmental factors is probably involved. The loss of immune tolerance, increased antigenic load, defective B-cell suppression, and the shifting of Th1 to Th2 immune responses lead to B-cell hyperactivity and the production of pathogenic autoantibodies. Hence, the coexistence of both these entities with different pathogenesis is unique.[5]
Specific antibody profiles and imaging studies assist in making the diagnosis of Rhupus syndrome.
Rhupus patients have been found to have a lower incidence of malar rash, hemolytic anemia, and renal and neurological involvement compared with the SLE group. In addition, rhupus patients rarely have severe renal disorders such as nephrotic syndrome and renal insufficiency. The SLEDAI score that is an indicator of disease activity in SLE, initial corticosteroid dosages, and the requirement of methylprednisolone pulse therapy have been found to be lower in the rhupus patients.[6] Previous studies have also shown that rhupus patients have a lower incidence of visceral organ involvement compared with SLE patients without RA.[2]
Many authors have classified Rhupus syndrome as a subset of SLE with severe arthritis. SLE shows 3 types of articular involvement: intermittent non-erosive polyarthritis usually found in the hands, wrists, and knees; non-erosive deforming arthritis referred to as Jaccoud's joint; and arthritis with joint deformities and specific erosion, i.e., Rhupus syndrome.[7,8] Most patients with SLE have transient, migratory, and reversible arthritis without erosion.
Some rheumatologists suggest that the presence of rheumatoid nodules in SLE patients could be a risk factor for Rhupus syndrome.[9] Tani et al. also found an association of rheumatoid factor positivity and joint erosion in SLE patients.[10]
Conclusion
Rhupus syndrome is a special overlap syndrome of RA and SLE that is manifested characteristically by more RA and less SLE-associated damage.
The treatment and prognosis of Rhupus syndrome have been found to be different from that of RA or SLE. Thus, proper recognition and an early diagnosis of Rhupus syndrome are important for choosing suitable therapies and improving patient prognosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Schur PH. Systemic lupus erythematosus. In: Beeson PB, McDermott W, editors. Cecil-loeb Textbook of Medicine. 13th ed. Philadelphia, PA: W.B. Saunders; 1971. p. 821. [Google Scholar]
- 2.Simón JA, Granados J, Cabiedes J, Morales JR, Varela JA. Clinical and immunogenetic characterization of Mexican patients with 'rhupus'. Lupus. 2002;11:287–92. doi: 10.1191/0961203302lu189oa. [DOI] [PubMed] [Google Scholar]
- 3.Al Fadhli S, Nizam R. Rhupus: A crosswalk between lupus and rheumatoid arthritis. OA Arthritis. 2014;2:3. [Google Scholar]
- 4.Panush RS, Edwards NL, Longley S, Webster E. 'Rhupus' syndrome. Arch Intern Med. 1988;148:1633–6. [PubMed] [Google Scholar]
- 5.Mok CC, Lau CS. Pathogenesis of systemic lupus erythematosus. J Clin Pathol. 2003;56:481–90. doi: 10.1136/jcp.56.7.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li J, Wu H, Huang X, Xu D, Zheng W, Zhao Y, et al. Clinical analysis of 56 patients with rhupus syndrome: Manifestations and comparisons with systemic lupus erythematosus: A retrospective case-control study. Medicine (Baltimore) 2014;93:e49. doi: 10.1097/MD.0000000000000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pipili C, Sfritzeri A, Cholongitas E. Deforming arthropathy in systemic lupus erythematosus. Eur J Intern Med. 2008;19:482–7. doi: 10.1016/j.ejim.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 8.Santiago MB. Miscellaneous non-inflammatory musculoskeletal conditions. Jaccoud's arthropathy. Best Pract Res Clin Rheumatol. 2011;25:715–25. doi: 10.1016/j.berh.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 9.Richter Cohen M, Steiner G, Smolen JS, Isenberg DA. Erosive arthritis in systemic lupus erythematosus: Analysis of a distinct clinical and serological subset. Br J Rheumatol. 1998;37:421–4. doi: 10.1093/rheumatology/37.4.421. [DOI] [PubMed] [Google Scholar]
- 10.Tani C, D'Aniello D, Delle Sedie A, Carli L, Cagnoni M, Possemato N, et al. Rhupus syndrome: Assessment of its prevalence and its clinical and instrumental characteristics in a prospective cohort of 103 SLE patients. Autoimmun Rev. 2013;12:537–41. doi: 10.1016/j.autrev.2012.09.004. [DOI] [PubMed] [Google Scholar]


